Oncologic Benefit of Adjuvant Chemoradiation after D2 Gastrectomy: A Stepwise Hierarchical Pooled Analysis and Systematic Review
Abstract
1. Introduction
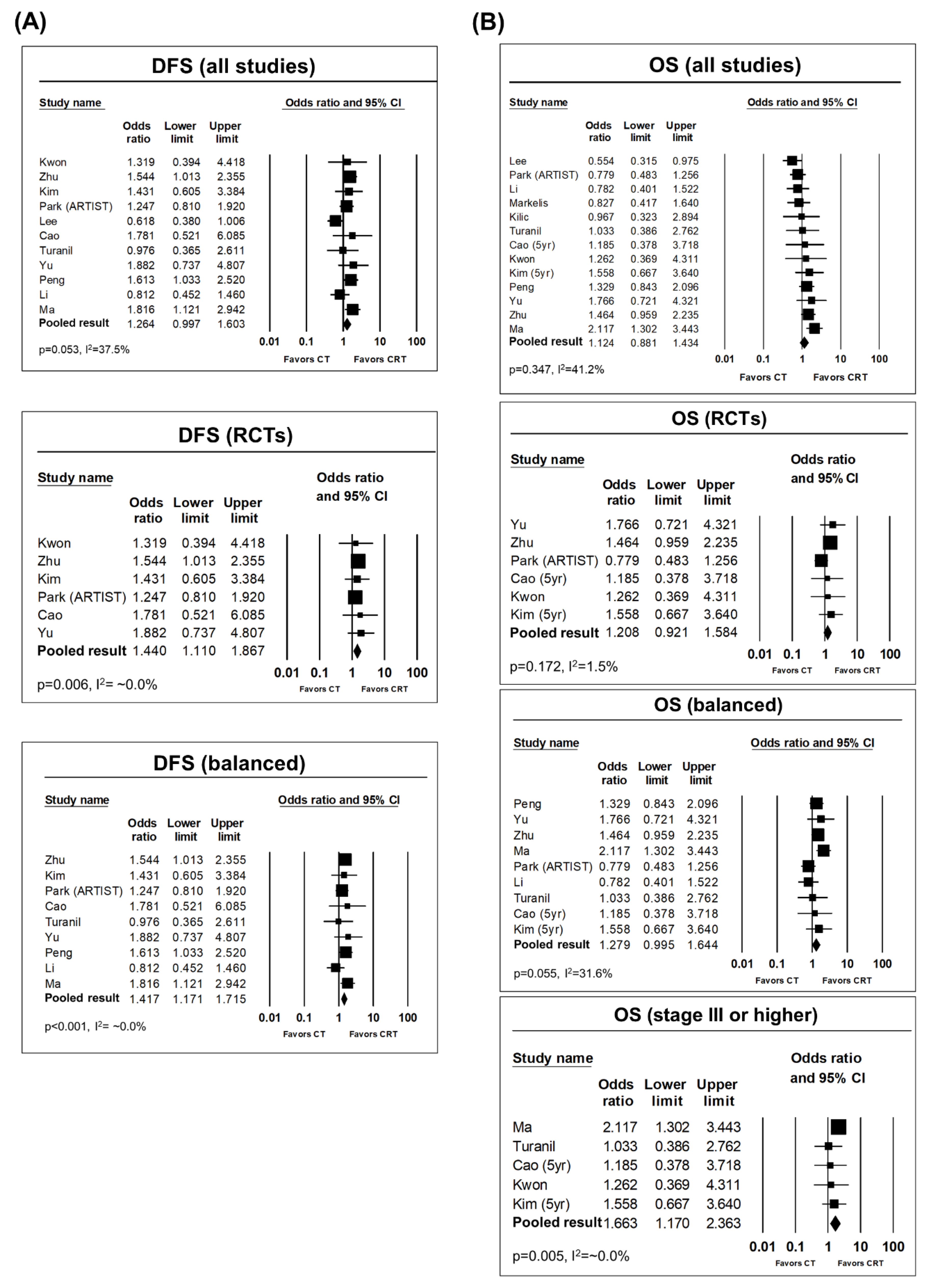
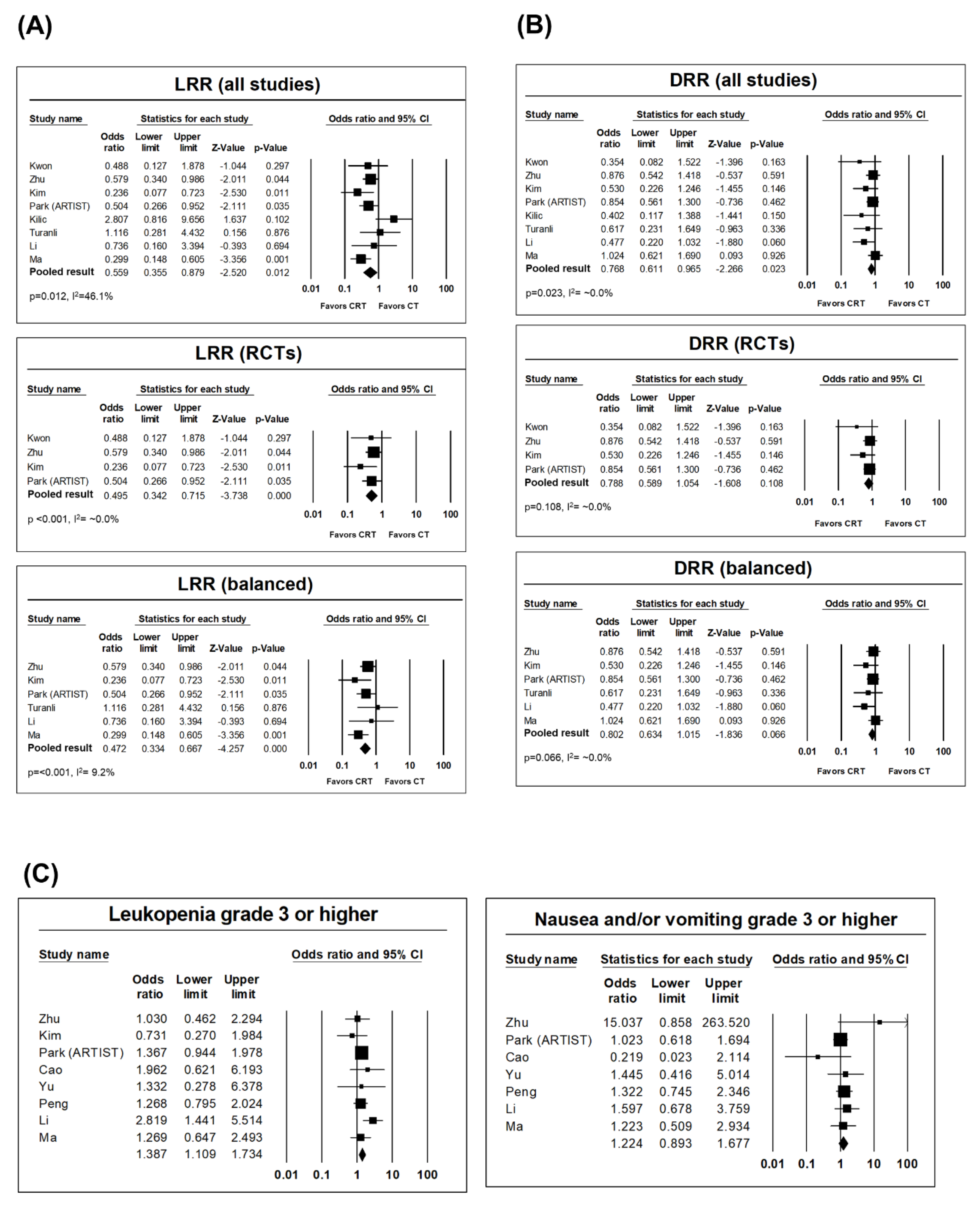
2. Results
3. Discussion
3.1. Clinical Interpretation of Pooled Results and Related Literature
3.2. Practical Implication and Future Perspectives
3.3. Limitations
4. Methods
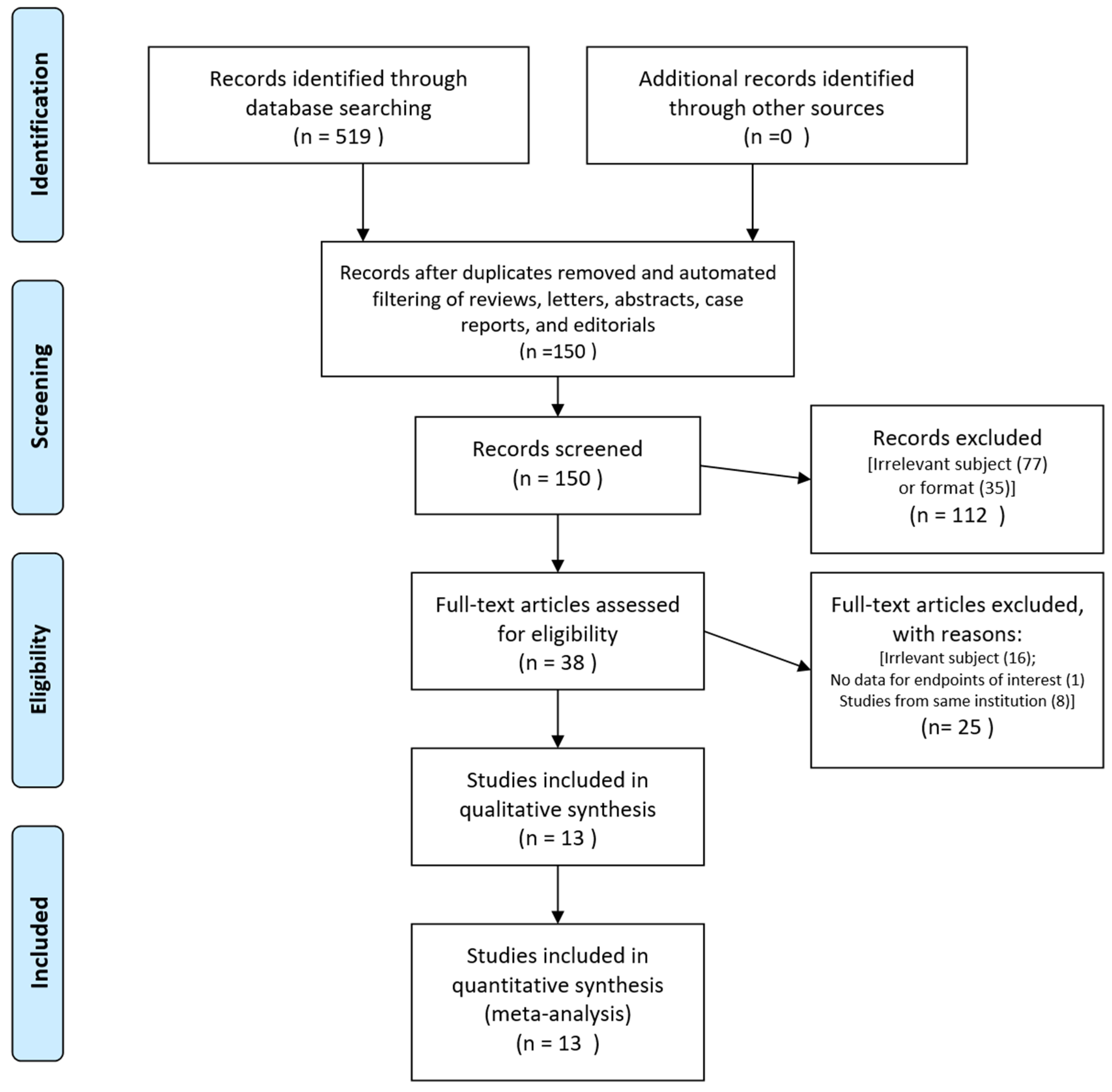
4.1. Inclusion Process and Criteria
4.2. Data Collection and Quality Assessment
4.3. Statistical Analyses
4.4. Ethical Consideration
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Association, J.G.C. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric. Cancer 2017, 20, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Guideline Committee of the Korean Gastric Cancer Association (KGCA), Development Working Group & Review Panel. Korean Practice Guideline for Gastric Cancer 2018: An evidence-based, multi-disciplinary approach. J. Gastric Cancer 2019, 19, 1–48. [Google Scholar] [CrossRef]
- De Manzoni, G.; Marrelli, D.; Baiocchi, G.L.; Morgagni, P.; Saragoni, L.; Degiuli, M.; Donini, A.; Fumagalli, U.; Mazzei, M.A.; Pacelli, F. The Italian Research Group for Gastric Cancer (GIRCG) guidelines for gastric cancer staging and treatment: 2015. Gastric Cancer 2017, 20, 20–30. [Google Scholar] [CrossRef]
- Allum, W.; Meyer, H.; Garofalo, A.; Schuhmacher, J.; Demanzoni, G.; Degiuli, M.; Kulig, J.; van de Velde, C.; Roukos, D.; Barr, H. Gastric cancer in Europe: European union network of excellence (EUNE) for gastric cancer steering group. Br. J. Surg. 2008, 95, 406–408. [Google Scholar]
- Degiuli, M.; Sasako, M.; Ponti, A.; Vendrame, A.; Tomatis, M.; Mazza, C.; Borasi, A.; Capussotti, L.; Fronda, G.; Morino, M. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br. J. Surg. 2014, 101, 23–31. [Google Scholar] [CrossRef]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef]
- Jansen, E.; Boot, H.; Dubbelman, R.; Verheij, M.; Cats, A. Postoperative chemoradiotherapy in gastric cancer—A phase I–II study of radiotherapy with dose escalation of weekly cisplatin and daily capecitabine chemotherapy. Ann. Oncol. 2010, 21, 530–534. [Google Scholar] [CrossRef]
- Sasako, M.; Sakuramoto, S.; Katai, H.; Kinoshita, T.; Furukawa, H.; Yamaguchi, T.; Nashimoto, A.; Fujii, M.; Nakajima, T.; Ohashi, Y. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J. Clin. Oncol. 2011, 29, 4387–4393. [Google Scholar] [CrossRef]
- Noh, S.H.; Park, S.R.; Yang, H.K.; Chung, H.C.; Chung, I.J.; Kim, S.W.; Kim, H.H.; Choi, J.H.; Kim, H.K.; Yu, W. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1389–1396. [Google Scholar] [CrossRef]
- Macdonald, J.S.; Smalley, S.R.; Benedetti, J.; Hundahl, S.A.; Estes, N.C.; Stemmermann, G.N.; Haller, D.G.; Ajani, J.A.; Gunderson, L.L.; Jessup, J.M.; et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N. Engl. J. Med. 2001, 345, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lim, D.H.; Kim, S.; Park, S.H.; Park, J.O.; Park, Y.S.; Lim, H.Y.; Choi, M.G.; Sohn, T.S.; Noh, J.H.; et al. Phase III trial comparing capecitabine plus cisplatin versus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: The ARTIST trial. J. Clin. Oncol. 2012, 30, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.; Verheij, M.; Allum, W.; Cunningham, D.; Cervantes, A.; Arnold, D. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2016, 27, v38–v49. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Comprehensive Network. NCCN Guidelines Version 4.2019 Gastric Cancer. Available online: https://www.nccn.org/professionals/physician_gls/pdf/gastric.pdf (accessed on 30 January 2020).
- Wang, F.H.; Shen, L.; Li, J.; Zhou, Z.W.; Liang, H.; Zhang, X.T.; Tang, L.; Xin, Y.; Jin, J.; Zhang, Y.J. The Chinese Society of Clinical Oncology (CSCO): Clinical guidelines for the diagnosis and treatment of gastric cancer. Cancer Commun. 2019, 39, 10. [Google Scholar] [CrossRef]
- Yoo, C.; Noh, S.H.; Shin, D.; Choi, S.; Min, J. Recurrence following curative resection for gastric carcinoma. Br. J. Surg. 2000, 87, 236–242. [Google Scholar] [CrossRef]
- Park, S.H.; Sohn, T.S.; Lee, J.; Lim, D.H.; Hong, M.E.; Kim, K.-M.; Sohn, I.; Jung, S.H.; Choi, M.G.; Lee, J.H. Phase III trial to compare adjuvant chemotherapy with capecitabine and cisplatin versus concurrent chemoradiotherapy in gastric cancer: Final report of the adjuvant chemoradiotherapy in stomach tumors trial, including survival and subset analyses. J. Clin. Oncol. 2015, 33, 3130–3136. [Google Scholar] [CrossRef]
- Zhu, W.G.; Xua, D.F.; Pu, J.; Zong, C.D.; Li, T.; Tao, G.Z.; Ji, F.Z.; Zhou, X.L.; Han, J.H.; Wang, C.S. A randomized, controlled, multicenter study comparing intensity-modulated radiotherapy plus concurrent chemotherapy with chemotherapy alone in gastric cancer patients with D2 resection. Radiother. Oncol. 2012, 104, 361–366. [Google Scholar] [CrossRef]
- Ma, G.F.; Zhang, H.G.; Liu, J.; Chen, Y.X.; Xiao, H.; Wang, X.F.; He, J.; Zeng, Z.C.; Sun, J.; Liu, T.S. Benefit of adjuvant chemoradiotherapy in patients with pathological stage III gastric cancer. Cancer Manag. Res. 2019, 11, 6029. [Google Scholar] [CrossRef]
- Turanli, S.; Atalay, C.; Berberoglu, U.; Gulben, K. Adjuvant chemoradiation versus chemotherapy for stage III gastric cancer after surgery with curative intent. J. Cancer Res. Ther. 2015, 11, 369. [Google Scholar] [CrossRef]
- Kim, T.H.; Park, S.R.; Ryu, K.W.; Kim, Y.-W.; Bae, J.-M.; Lee, J.H.; Choi, I.J.; Kim, Y.-J.; Kim, D.Y. Phase 3 trial of postoperative chemotherapy alone versus chemoradiation therapy in stage III-IV gastric cancer treated with R0 gastrectomy and D2 lymph node dissection. Int. J. Radiat. Biol. Phys. 2012, 84, e585–e592. [Google Scholar] [CrossRef]
- Trip, A.K.; Nijkamp, J.; van Tinteren, H.; Cats, A.; Boot, H.; Jansen, E.P.M.; Verheij, M. IMRT limits nephrotoxicity after chemoradiotherapy for gastric cancer. Radiother Oncol. 2015, 114, 421–426. [Google Scholar] [CrossRef]
- Boda-Heggemann, J.; Weiss, C.; Schneider, V.; Hofheinz, R.-D.; Haneder, S.; Michaely, H.; Wertz, H.; Ronellenfitsch, U.; Hochhaus, A.; Wenz, F. Adjuvant IMRT/XELOX radiochemotherapy improves long-term overall-and disease-free survival in advanced gastric cancer. Strahlenther. Onkol. 2013, 189, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Ringash, J.; Perkins, G.; Brierley, J.; Lockwood, G.; Islam, M.; Catton, P.; Cummings, B.; Kim, J.; Wong, R.; Dawson, L. IMRT for adjuvant radiation in gastric cancer: A preferred plan? Int. J. Radiat. Biol. Phys. 2005, 63, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Markelis, R.; Endzinas, Ž.; Kiudelis, M.; Grižas, S.; Pundzius, J.; Saladžinskas, Ž.; Juozaitytė, E.; Inčiūra, A.; Pranys, D.; Maleckas, A. Adjuvant therapy after curative resection with D2 lymphadenectomy for gastric cancer: Results of a prospective clinical trial. Medicina 2009, 45, 460. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.C.; Kim, M.C.; Kim, K.H.; Jang, J.S.; Oh, S.Y.; KIM, S.H.; Kwon, K.A.; Lee, S.; Lee, H.S.; KIM, H.J. Adjuvant chemoradiation versus chemotherapy in completely resected advanced gastric cancer with D2 nodal dissection. Asia Pac. J. Clin. Oncol. 2010, 6, 278–285. [Google Scholar] [CrossRef]
- Kilic, L.; Ordu, C.; Ekenel, M.; Yildiz, I.; Keskin, S.; Sen, F.; Gural, Z.; Asoglu, O.; Kizir, A.; Aykan, F. Comparison of two different adjuvant treatment modalities for pN3 gastric cancer patients after D2 lymph node dissection: Can we avoid radiotherapy in a subgroup of patients? Med. Oncol. 2013, 30, 660. [Google Scholar] [CrossRef]
- Lee, S.J.; Sohn, T.S.; Lee, J.; Park, S.H.; Park, J.O.; Do Hoon, L.; Park, Y.S.; Lim, H.Y.; Choi, M.G.; Lee, J.H. Adjuvant chemoradiation with 5-fluorouracil/leucovorin versus S-1 in gastric cancer patients following D2 lymph node dissection surgery: A feasibility study. Anticancer Res. 2014, 34, 6585–6591. [Google Scholar]
- Cao, X.G. Efficacy and adverse reactions of chemoradiotherapy after D2 radical resection for advanced gastric cancer. J. Pract. Oncol. 2015, 30, 533–536. [Google Scholar]
- Yu, J.W.; Hao, J.Q.; Hu, Z.G.; Qian, L.T. Chemoradiotherapy vs pure chemotherapy for local progressive gastric cancer following D2 lymph node dissection: A comparison of effectiveness. Acad. J. Second Mil. Med. Univ. 2016, 37, 177–183. [Google Scholar]
- Peng, J.; Wei, Y.; Zhou, F.; Dai, J.; Zhong, Y.; Xie, C.; Qin, Y.; Gong, J.; Xiong, B.; Zhou, Y. D2-resected stage IIIc gastric cancer patients benefit from adjuvant chemoradiotherapy. Cancer Med. 2016, 5, 2773–2780. [Google Scholar] [CrossRef]
- Li, Q.; Li, G.; Palmer, J.D.; Zhang, Z. Lymph node burden as a predictive factor for selective chemoradiotherapy in patients with locally advanced gastric cancer after a D2 dissection. Amer. J. Clin. Oncol. 2017, 40, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Stahl, M.; Walz, M.K.; Riera-Knorrenschild, J.; Stuschke, M.; Sandermann, A.; Bitzer, M.; Wilke, H.; Budach, W. Preoperative chemotherapy versus chemoradiotherapy in locally advanced adenocarcinomas of the oesophagogastric junction (POET): Long-term results of a controlled randomised trial. Eur. J. Cancer (Oxford, England: 1990) 2017, 81, 183–190. [Google Scholar] [CrossRef]
- Klevebro, F.; Alexandersson von Döbeln, G.; Wang, N.; Johnsen, G.; Jacobsen, A.B.; Friesland, S.; Hatlevoll, I.; Glenjen, N.I.; Lind, P.; Tsai, J.A.; et al. A randomized clinical trial of neoadjuvant chemotherapy versus neoadjuvant chemoradiotherapy for cancer of the oesophagus or gastro-oesophageal junction. Ann. Oncol. 2016, 27, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.H.; Song, K.Y.; Jeon, H.M.; Park, C.H.; Jacks, L.M.; Gonen, M.; Shah, M.A.; Brennan, M.F.; Coit, D.G.; Strong, V.E. Is gastric cancer different in Korea and the United States? Impact of tumor location on prognosis. Ann. Surg. Oncol. 2014, 21, 2332–2339. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.S.; Lim, J.S.; Noh, S.H.; Hyung, W.J.; An, J.Y.; Lee, Y.C.; Rha, S.Y.; Lee, C.G.; Koom, W.S. Patterns of regional recurrence after curative D2 resection for stage III (N3) gastric cancer: Implications for postoperative radiotherapy. Radiother Oncol. 2012, 104, 367–373. [Google Scholar] [CrossRef]
- Brady, L.W.; Perez, C.A.; Wazer, D.E. Perez & Brady’s Principles and Practice of Radiation Oncology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Kwong, D.; Sham, J.; Choy, D. The effect of loco-regional control on distant metastatic dissemination in carcinoma of the nasopharynx: An analysis of 1301 patients. Int. J. Radiat. Biol. Phys. 1994, 30, 1029–1036. [Google Scholar] [CrossRef]
- Vicini, F.A.; Kestin, L.; Huang, R.; Martinez, A. Does local recurrence affect the rate of distant metastases and survival in patients with early-stage breast carcinoma treated with breast-conserving therapy? Cancer 2003, 97, 910–919. [Google Scholar] [CrossRef]
- Oba, K.; Paoletti, X.; Alberts, S.; Bang, Y.J.; Benedetti, J.; Bleiberg, H.; Catalano, P.; Lordick, F.; Michiels, S.; Morita, S. Disease-free survival as a surrogate for overall survival in adjuvant trials of gastric cancer: A meta-analysis. J. Natl. Cancer Inst. 2013, 105, 1600–1607. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, D.; Yang, L.; Chi, Y.; Tang, Y.; Li, N.; Wang, S.; Song, Y.; Liu, Y.; Liu, W. S-1 chemotherapy and intensity-modulated radiotherapy after D1/D2 lymph node dissection in patients with node-positive gastric cancer: A phase I/II study. Br. J. Cancer 2018, 118, 338–343. [Google Scholar] [CrossRef]
- Moningi, S.; Ajani, J.A.; Badgwell, B.D.; Murphy, M.B.; Ikoma, N.; Mansfield, P.F.; Ho, J.C.; Suh, Y.; Crane, C.; Herman, J.M. IMRT reduces acute toxicity in patients treated with preoperative chemoradiation for gastric cancer. Adv. Radiat. Oncol. 2019, 5, 369–376. [Google Scholar] [CrossRef]
- Wang, J.; Tian, Y.; Tang, Y.; Wang, X.; Li, N.; Ren, H.; Fang, H.; Feng, Y.; Wang, S.; Song, Y. A phase II prospective nonrandomized trial of magnetic resonance imaging-guided hematopoietic bone marrow-sparing radiotherapy for gastric cancer patients with concurrent chemotherapy. Onco Targets Ther. 2016, 9, 2701. [Google Scholar] [CrossRef] [PubMed]
- Leone, P.; Vacca, A.; Dammacco, F.; Racanelli, V. Common variable immunodeficiency and gastric malignancies. Int. J. Mol. Sci. 2018, 19, 451. [Google Scholar] [CrossRef] [PubMed]
- Yap, Y.L.; So, J.B. Gastric adenocarcinoma occurring in a young patient with common variable immunodeficiency syndrome. Singap. Med. J. 2009, 50, e201–e203. [Google Scholar]
- Wasserstein, R.L.; Lazar, N.A. The ASA statement on p-values: Context, process, and purpose. Am. Stat. 2016, 70, 129–133. [Google Scholar] [CrossRef]
- Basta, Y.L.; Baur, O.L.; van Dieren, S.; Klinkenbijl, J.H.; Fockens, P.; Tytgat, K.M. Is there a benefit of multidisciplinary cancer team meetings for patients with gastrointestinal malignancies? Ann. Surg. Oncol. 2016, 23, 2430–2437. [Google Scholar] [CrossRef]
- Du, C.Z.; Li, J.; Cai, Y.; Sun, Y.S.; Xue, W.C.; Gu, J. Effect of multidisciplinary team treatment on outcomes of patients with gastrointestinal malignancy. World J. Gastroenterol. 2011, 17, 2013–2018. [Google Scholar] [CrossRef] [PubMed]
- Oxenberg, J.; Papenfuss, W.; Esemuede, I.; Attwood, K.; Simunovic, M.; Kuvshinoff, B.; Francescutti, V. Multidisciplinary cancer conferences for gastrointestinal malignancies result in measureable treatment changes: A prospective study of 149 consecutive patients. Ann. Surg. Oncol. 2015, 22, 1533–1539. [Google Scholar] [CrossRef]
- Quéro, L.; Guillerm, S.; Hennequin, C. Neoadjuvant or adjuvant therapy for gastric cancer. World J. Gastrointest. Oncol. 2015, 7, 102–110. [Google Scholar] [CrossRef]
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet (London, England) 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Fuchs, C.S.; Tomasek, J.; Yong, C.J.; Dumitru, F.; Passalacqua, R.; Goswami, C.; Safran, H.; Dos Santos, L.V.; Aprile, G.; Ferry, D.R.; et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): An international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet (London, England) 2014, 383, 31–39. [Google Scholar] [CrossRef]
- Wilke, H.; Muro, K.; Van Cutsem, E.; Oh, S.C.; Bodoky, G.; Shimada, Y.; Hironaka, S.; Sugimoto, N.; Lipatov, O.; Kim, T.Y.; et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): A double-blind, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1224–1235. [Google Scholar] [CrossRef]
- Wei, L.; Sun, J.; Zhang, N.; Zheng, Y.; Wang, X.; Lv, L.; Liu, J.; Xu, Y.; Shen, Y.; Yang, M. Noncoding RNAs in gastric cancer: Implications for drug resistance. Mol. Cancer 2020, 19, 1–17. [Google Scholar] [CrossRef]
- Argentiero, A.; De Summa, S.; Di Fonte, R.; Iacobazzi, R.M.; Porcelli, L.; Da Vià, M.; Brunetti, O.; Azzariti, A.; Silvestris, N.; Solimando, A.G. Gene expression comparison between the lymph node-positive and-negative reveals a peculiar immune microenvironment signature and a theranostic role for WNT targeting in pancreatic ductal adenocarcinoma: A pilot study. Cancers 2019, 11, 942. [Google Scholar] [CrossRef] [PubMed]
- Eggar, M.; Davey Smith, G. Misleading meta-analysis. Lessons from “an effective, safe, simple” intervention that wasn’t. Br. Med. J. 1995, 310, 752–754. [Google Scholar]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Shrier, I.; Boivin, J.-F.; Steele, R.J.; Platt, R.W.; Furlan, A.; Kakuma, R.; Brophy, J.; Rossignol, M. Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles. Am. J. Epidemiol. 2007, 166, 1203–1209. [Google Scholar] [CrossRef]
- Zhou, M.L.; Kang, M.; Li, G.C.; Guo, X.M.; Zhang, Z. Postoperative chemoradiotherapy versus chemotherapy for R0 resected gastric cancer with D2 lymph node dissection: An up-to-date meta-analysis. World J. Surg. Oncol. 2016, 14, 209. [Google Scholar] [CrossRef]
- Huang, Y.Y.; Yang, Q.; Zhou, S.W.; Wei, Y.; Chen, Y.X.; Xie, D.R.; Zhang, B. Postoperative chemoradiotherapy versus postoperative chemotherapy for completely resected gastric cancer with D2 Lymphadenectomy: A meta-analysis. PLoS ONE 2013, 8, e68939. [Google Scholar]
- Ohri, N.; Garg, M.K.; Aparo, S.; Kaubisch, A.; Tome, W.; Kennedy, T.J.; Kalnicki, S.; Guha, C. Who benefits from adjuvant radiation therapy for gastric cancer? A meta-analysis. Int. J. Radiat. Biol. Phys. 2013, 86, 330–335. [Google Scholar] [CrossRef]
- The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 3 February 2020).
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Fixed-Effect Versus Random-Effects Models. In Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Cochran, W.G. The combination of estimates from different experiments. Biometrics 1954, 10, 101–129. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Declaration of Helsinki: Recommendations Guiding Medical Doctors in Biomedical Research Involving Human Subjects. Available online: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/ (accessed on 3 February 2020).
| Author, Year | Affiliation | Study Design | Inclusion Criteria | Inclusion Period | Total No. of Patients | CRT/CT No. | Modality | † Age (Years) | Diffuse Type (%) | T Stage | N Stage |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Markelis, 2009 [25] | Kaunas University, Lithuania | NRCT, prospective | Radical resection and D2 LND I–IV | 2003–2007 | 133 | 63 | FL, 45 Gy/5 weeks | m57.9 | HG 3–4 (78%) | T1–2 (30%); T3–4 (70%) | N0 (29%); N1 (41%); N2 (30%) |
| 70 | 5FU and LV | m62.2 | HG 3–4 (63%) | T1–2 (33%); T3–4 (67%) | N0 (27%); N1 (44%); N2 (29%) | ||||||
| p-value | 0.017 | 0.0921 | 0.883 | 0.685 | |||||||
| Kwon, 2010 [26] | Dong-A University, South Korea | RCT | R0 resection and D2 LND III–IV | 2002–2004 | 61 | 31 | FP and capecitabine, 45 Gy/5 weeks | ≥60 (25.8%) | 64.5 | AJCC IIIA (36%); IIIB (42%); IV (M0, 23%) | |
| 30 | FP | ≥60 (46.7%) | 43.3 | AJCC IIIA (67%); IIIB (23%); IV (M0, 10%) | |||||||
| p-value | 0.114 | 0.108 | 0.05 | ||||||||
| Zhu, 2012 [18] | Nanjing Medical University, China | RCT | R0 resection and D2 LND IB–IV | 2003–2008 | 351 | 186 | FL and 45 Gy/5 weeks (IMRT) | M56 | NA | AJCC IB–II (30%); III (55%); IV (M0, 14%) | |
| 165 | 5FU and LV | M59 | NA | AJCC IB–II (27%); III (58%); IV (M0, 14%) | |||||||
| p-value | NA | ||||||||||
| Kim, 2012 [21] | NCC, Korea | RCT | R0 resection and D2 LND stage III–IV | 2002–2006 | 110 | 46 | FL and 45 Gy/5 weeks | ≥60 (19.6%) | 56.5 | T2 (30%); T3 (63%); T4 (7%) | N1 (33%); N2 (46%); N3 (22%) |
| 44 | FL | ≥60 (31.8%) | 54.5 | T2 (43%) T3 (50%); T4 (7%) | N0–1 (27%); N2 (50%); N3 (23%) | ||||||
| p-value | 0.23 | 0.978 | 0.465 | 0.483 | |||||||
| Park, 2015, Lee, 2012 (ARTIST) [12,17] | Samsung Medical Center, Korea | RCT | R0 resection and D2 LND IB–IV | 2004–2008 | 458 | 230 | XP and 45 Gy/5 weeks | M56 | 63% | AJCC II (37%); III (31%); IV(M0, 11%) N0 (12%); N1 (57%); N2–3 (32%) | |
| 228 | XP | M56 | 57% | AJCC II (38%); III (29%); IV (12%) N0 (15%); N1 (54%); N2–3 (31%) | |||||||
| p-value | NA | ||||||||||
| Kilic, 2013 [27] | Istanbul University, Turkey | NRCT, retrospective | D2 LND, pTanyN3M0 (R0 77.8% vs. 71.7%, p = 0.61) | 2005–2009 | 71 | 18 | FL and 45 Gy/5 weeks | M46 | 61.1 | T2/3 (89%) T4 (11%) | all N3 |
| 53 | ECF of DCF | M54 | 30.1 | T2/3 (91%) T4 (9%) | all N3 | ||||||
| p-value | 0.1 | 0.02 | 0.72 | ||||||||
| Lee, 2014 [28] | Samsung Medical Center, Korea | NRCT, retrospective | R0 resection and D2 LND IB–IV | 2008–2009 | 405 | 244 | FL and 45 Gy/5 weeks | M53 | Tubular (68.4%) signet ring cell (22.1%) | T1–2 (71%) T3–4 (29%) | N0–2 (56%) N3a (27%) N3b (17%) |
| 161 | S-1 | M57 | Tubular (67.1%) signet ring cell (21.1%) | T1–2 (82%) T3–4 (18%) | N0–2 (78%) N3a (17%) N3b (5%) | ||||||
| p-value | 0.001 | 0.234 | 0.02 | <0.001 | |||||||
| Cao, 2015 [29] | Xinwen Mining Group Central Hospital, China | RCT | R0 resection and D2 LND stage III–IV | 2008–2010 | 50 | 25 | FP and capecitabine CCRT | ≥60 (40%) | LD (68%) | AJCC IIIA (32%); IIIB (40%) | |
| 25 | FP | ≥60 (44%) | LD (60%) | AJCC IIIA (48%); IIIB (32%) | |||||||
| p-value | NS | NS | NS | ||||||||
| Turanli, 2015 [20] | Ankara Oncology Education and Research Hospital, Turkey | NRCT, retrospective | R0 resection and D2 LND III | 2004–2009 | 92 | 71 | FL and 45 Gy/5 weeks | m57.5 | 29.6 | T3 (7%) T4 (89%) | N1 (18%); N2 (40%) N3 (42%) |
| 21 | FL or ECF | m57.5 | 38.1 | T3 (14%) T4 (81%) | N1 (14%); N2 (38%); N3 (47%) | ||||||
| p-value | 0.98 | 0.46 | 0.48 | 0.87 | |||||||
| Yu, 2016 [30] | Anhui University, China | RCT | R0 resection and D2 LND stage II–III | 2010–2011 | 79 | 40 | Capecitabine CCRT (45 Gy) followed by XELOX | ≥60 (57.5%) | HG3–4 (57.5%) | AJCC II (40%) III (60%) N0 (29%) | |
| 39 | XELOX | ≥60 (48.7%) | HG3–4 (64.1%) | AJCC II (36%) III (64%) N0 (31%) | |||||||
| p-value | 0.434 | 0.548 | 0.707 | ||||||||
| Peng, 2016 [31] | Wuhan University, China | NRCT, retrospective | R0 resection and D2 LND stage IIA–IIIC | 2004–2012 | 337 | 124 | FOLFOX or XELOX or capecitabine and 45 Gy/ 5 weeks | M54 | HG 3–4 (78.2%) | AJCC II (36%); IIIA (20%); IIIB (17%) IIIC (27%) | |
| 213 | FOLFOX or XELOX or capecitabine | M56 | HG 3–4 (75.5%) | AJCC II (31%); IIIA (23%); IIIB (20%); IIIC (27%) | |||||||
| p-value | 0.247 | 0.128 | 0.507 | ||||||||
| Li, 2017 [32] | Fudan University, China | NRCT, retrospective | R0 resection and D2 LND IB–IIIC | 2005–2010 | 186 | 93 | 5FU or capecitabine or tegafur and 45–50Gy/5–6 weeks (3D-CRT or IMRT) | m54 | LD (15.1%) | T1–2 (17%) T3 (25%) T4 (58%) | N0 (9%); N1 (17%); N2 (23%); N3 (52%) |
| 93 | 5FU based regimen | m57 | LD (19.4%) | T1–2 (14%) T3 (19%) T4 (67%) | N0 (11%); N1 (22%); N2 (24%); N3 (44%) | ||||||
| p-value | 0.61 | 0.43 | 0.37 | 0.76 | |||||||
| Ma, 2019 [19] | Fudan University, China | NRCT, retrospective, PSM | R0 resection and D2 LND stage III | 2009–2014 | 270 | 135 | Same regimen and 45 Gy/5 weeks, 5–10 Gy boost (3D-CRT or IMRT) | m54.3 | NA | T2 (6%) T3 (16%) T4 (79%) | N0–2 (31%) N3a (45%) N3b (24%) |
| 135 | 5FU or capecitabine or ECF, modified DCF regimen | m54.7 | NA | T2 (3%) T3 (21%) T4 (76%) | N0–2 (30%) N3a (44%) N3b (25%) | ||||||
| p-value | 0.74 | 0.305 | 0.081 | ||||||||
| Author, Year | CRT/CT No. | Median Follow-Up (Months, Range) | Median DFS | 3-Year DFS | 5-Year DFS | Median OS (Months) | 3-Year OS | 5-Year OS | Prognosticators (p-Value) | Pattern of Failure | Grade 3–4 Toxicities (CRT vs. CT) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Markelis, 2009 [25] | 63 | 52.4% | Overall incidence: 44.4% vs. 7.1% (p < 0.05) | ||||||||
| 70 | 57.1% | ||||||||||
| 0.039 | |||||||||||
| Kwon, 2010 [26] | 31 | 77.2 (24–92.8) | 80.0% | 76.7% | 80.6% | 70.1% | Overall LRR 12.9% vs. 23.3% (p = 0.335); DM 9.7% vs. 23.3% (p = 0.335) | Neutropenia (48.4% vs. 16.7%); anemia (12.9% vs. 16.7%); N/V (6.5% vs. 13.3%) | |||
| 30 | 75.2% | 59.1% | 76.7% | 70.0% | |||||||
| 0.887 | 0.222 | 0.814 | |||||||||
| Zhu, 2012 [18] | 186 | 42.5 | 50 | 57.5% | 45.2% | 54.0 | 59.7% | 48.4% | UVA, OS: Stage (p < 0.001); LN+ (p = 0.001) | 5-yr LRR 15.6% vs. 24.2% (CRT vs. CT, p = 0.042); 5-yr DM 24.2% vs. 26.7% (p = 0.595) | Leukopenia (7.5% vs. 7.3%); nausea (2.7% vs. 0%); vomiting (1.6% vs. 0%) |
| 165 | 32 | 46.7% | 35.8% | 38.0 | 50.3% | 41.4% | |||||
| 0.029 | 0.122 | ||||||||||
| Kim, 2012 [21] | 46 | 86.7 | 67.4% | 60.9% | 65.2% | Overall LRR 10.9% vs. 34.1% (CRT vs. CT, p = 0.006); Overall DM 32.6% vs. 47.7 (CRT vs. CT, p = 0.288) | Hematologic (19.6% vs. 25%, p = NS); GI toxicity (17.4% vs. 11.4%, p = NS). | ||||
| 44 | 59.1% | 50.0% | 54.6% | ||||||||
| 0.246 | 0.67 | ||||||||||
| Park, 2015 Lee, 2012 (ARTIST) [12,17] | 230 | 7 years | 78.2% | 73.9% | 80.0% | 75.0% | MVA, OS: Stage (p < 0.01); Lauren classification (p = 0.03); LNR (p < 0.01) | Overall LRR 7% vs. 13% (CRT vs. CT, p = 0.0033); DM 24% vs. 27% (p = 0.5568) | Neutropenia (48.4% vs. 40.7%); Nausea (12.3% vs. 12.4%); Vomiting (3.5% vs. 3.1%); One 5 complication in each arm | ||
| 228 | 74.2% | 67.1% | 83.7% | 73.0% | |||||||
| 0.0862 | 0.527 | ||||||||||
| Kilic, 2013 [27] | 18 | 13.8 (6.2–74.1) | 15.2 | 34.2 | 38.8% | MVA, DFS: LNR (p = 0.04) | Overall LRR 33.3% vs. 15.1% (CRT vs. CT, p = 0.63); DM 22.2% vs. 41.5% (CRT vs. CT) | No toxicity related death in both groups | |||
| 53 | 12.5 | 26.8 | 39.6% | ||||||||
| 0.56 | 0.74 | ||||||||||
| Lee, 2014 [28] | 244 | 49 (3.0–62.0) | 73.0% | 79.8% | MVA, DFS: Stage (<0.001); Age (p = 0.006) | Neutropenia 40.2% vs. 8.7% (p < 0.001); all neutropenia was transient. Nausea 5.7% vs. 0% (p = 0.002); vomiting 2.5% vs. 0% (p = 0.085) | |||||
| 161 | 81.4% | 87.7% | |||||||||
| 0.035 | |||||||||||
| Cao, 2015 [29] | 25 | 3 years | 76.0% | 60.0% | 64.0% | Neutropenia 48% vs. 32% (p = 0.016); nausea 4% vs. 16% (p = 0.032); diarrhea 8% vs. 0% (p = 0.025) | |||||
| 25 | 64.0% | 52.0% | 60.0% | ||||||||
| 0.112 | 0.231 | 0.324 | |||||||||
| Turanli, 2015 [20] | 71 | 30 (8–112) | 42.2% | 32.9% | 32.0 | 43.6% | 34.4% | Overall LRR 15.7% vs. 14.3% (CRT vs. CT, p = 0.089); DM 45.1% vs. 57.1% (p = 0.42) | |||
| 21 | 42.8% | 24.1% | 29.0 | 42.8% | 23.8% | ||||||
| 0.8 | 0.74 | ||||||||||
| Yu, 2016 [30] | 40 | 34 | 42.5% | 52.5% | MVA, OS: ECOG (0.016); LN+ (0.035) | Leukopenia (10% vs. 7.7%, p = 0.253); N/V (17.5% vs. 12.8%, p = 0.043) | |||||
| 39 | 28.2% | 38.5% | |||||||||
| 0.238 | 0.235 | ||||||||||
| Peng, 2016 [31] | 124 | 41.1 (14–111.1) | 40.7 | 55.6% | 38.7% | 51.0 | 41.4% | 45.6% | Overall incidence: 36.3% vs. 31.0% (p = 0.338) m/c Cx: Leukopenia or neutropenia (21.7% vs. 14.6%, p = 0.09); nausea (10.4% vs. 8.4%); vomiting (9.6% vs. 7.5%) | ||
| 213 | 31.2 | 43.7% | 31.1% | 48.6 | 34.7% | 37.3% | |||||
| 0.112 | 0.3 | 0.132 | |||||||||
| Li, 2017 [32] | 93 | CRT 28 (5–62) CT 43 (2–63) | 57.0% | 72.8% | Overall LRR 3.2% vs. 4.3% (p = 0.76); DM 12.9% vs. 23.7% (p = 0.18) | Overall incidence: 38.7% vs. 18.3% (p = 0.002); leukopenia 30.1% vs. 10.8%, Nausea (10.8% vs. 5.4%); vomiting (5.4% vs. 5.4%) | |||||
| 93 | 62.0% | 77.4% | |||||||||
| 0.3 | 0.23 | ||||||||||
| Ma, 2019 [19] | 135 | 41 (7–104.2) | 60.7% | 40.7% | M51.2 | 57.0% | 45.2% | MVA, OS: Stage (<0.001); LNR <0.001; total vs. subtotal gastrectomy 0.007); tumor deposit (0.028) | Overall LRR [n = 135 (CRT) 280 (CTx)] 7.4% vs. 21.1% (CRT vs. CT, p < 0.001); Overall DM 21.5% vs. 21.1% (CRT vs. CT, p = 0.924) | Leukopenia (16.3% vs. 13.3%, p = 0.493); anorexia (14.8% vs. 11.1%, p = 0.365); N/V (8.9% vs. 7.4%, p = 0.615) | |
| 135 | 52.6% | 16.3% | M39.3 | 38.5% | 19.3% | ||||||
| <0.01 | <0.01 | ||||||||||
| Studies | No. of Studies | No. of Patients | Heterogeneity p | I2 (%) | Heterogeneity | Pooled Results (95% CI) | p (Pooled Analyses) | Egger’s p | |
|---|---|---|---|---|---|---|---|---|---|
| DFS, controlled comparisons | |||||||||
| All studies | 11 | 2379 | 0.1 | 37.5% | Medium | OR 1.264 (0.997–1.603) | 0.053 | 0.942 | |
| RCTs | 6 | 1089 | 0.964 | ~0.0% | Very low | OR 1.440 (1.110–1.867) | 0.006 | 0.420 | |
| Balanced | 9 | 1913 | 0.61 | ~0.0% | Very low | OR 1.417 (1.171–1.715) | <0.001 | 0.824 | |
| 3-year DFS, single-arm analysis | |||||||||
| CRT arm | 11 | 1225 | <0.001 | 84.9% | Very high | 62.5% (54.6–69.8) | NA | 0.749 | |
| CT arm | 11 | 1154 | <0.001 | 91.3% | Very high | 57.1% (46.1–67.5) | NA | 0.868 | |
| 5-year DFS, single-arm analysis | |||||||||
| CRT arm | 8 | 848 | <0.001 | 91.1% | Very high | 53.3% (40.9–65.4) | NA | 0.851 | |
| CT arm | 8 | 861 | <0.001 | 93.4% | Very high | 40.9% (27.3–56.0) | NA | 0.748 | |
| OS, controlled comparisons | |||||||||
| All studies | 13 | 2583 | 0.06 | 41.2% | Medium | OR 1.124 (0.881–1.434) | 0.347 | 0.760 | |
| RCTs | 6 | 1089 | 0.406 | 1.5% | Very low | OR 1.208 (0.921–1.584) | 0.172 | 0.622 | |
| Balanced | 9 | 1913 | 0.166 | 31.6% | Medium | OR 1.279 (0.995–1.644) | 0.055 | 0.840 | trimmed value † |
| Stage ≥III | 5 | 563 | 0.662 | ~0.0% | Very low | OR 1.663 (1.170–2.363) | 0.005 | 0.023 | OR 1.963 (1.443–2.671) |
| 3-year OS, single-arm analysis | |||||||||
| CRT arm | 11 | 1235 | <0.001 | 90.8% | Very high | 61.4% (51.1–70.8) | NA | 0.479 | |
| CT arm | 11 | 1208 | <0.001 | 95.0% | Very high | 59.1% (44.4–72.3) | NA | 0.513 | |
| 5-year OS, single-arm analysis | |||||||||
| CRT arm | 8 | 848 | <0.001 | 89.1% | Very high | 55.8% (44.5–66.5) | NA | 0.885 | |
| CT arm | 8 | 861 | <0.001 | 93.9% | Very high | 46.9% (32.0–62.4) | NA | 0.922 | |
| Locoregional recurrence, controlled comparison | |||||||||
| All studies | 8 | 1724 | 0.073 | 46.1% | Medium | OR 0.559 (0.355–0.879) | 0.012 | 0.439 | |
| RCTs | 4 | 960 | 0.569 | ~0.0% | Very low | OR 0.495 (0.342–0.715) | <0.001 | 0.307 | |
| Balanced | 6 | 1592 | 0.357 | 9.2% | Low | OR 0.472 (0.334–0.667) | <0.001 | 0.863 | |
| Locoregional recurrence, single-arm analysis | |||||||||
| CRT arm | 8 | 810 | 0.001 | 70.4% | High | 11.3% (7.5–16.8) | NA | 0.786 | |
| CT arm | 8 | 914 | <0.001 | 73.7% | High | 18.1% (13.1–24.4) | NA | 0.459 | |
| Distant metastasis, controlled comparison | |||||||||
| All studies | 8 | 1724 | 0.504 | ~0.0 | Very low | OR 0.768 (0.611–0.965) | 0.023 | 0.004 | OR 0.837 (0.655–1.070) |
| RCTs | 4 | 960 | 0.511 | ~0.0 | Very low | OR 0.788 (0.589–1.054) | 0.108 | 0.027 | OR 0.814 (0.612–1.083) |
| Balanced | 6 | 1592 | 0.543 | ~0.0 | Very low | OR 0.802 (0.634–1.015) | 0.066 | 0.051 | OR 0.908 (0.710–1.160) |
| Distant metastasis, single-arm analysis | |||||||||
| CRT arm | 8 | 810 | <0.001 | 74.3% | High | 24.1% (18.1–31.2) | NA | 0.621 | |
| CT arm | 8 | 914 | <0.001 | 75.3% | High | 30.9% (24.4–38.3) | NA | 0.069 | 29.0% (22.6–36.3) |
| Complication of grade ≥3 | |||||||||
| Leukopenia | 8 | 1821 | 0.433 | ~0.0 | Very low | OR 1.387 (1.109–1.734) | 0.004 | 0.946 | |
| N/V | 7 | 1731 | 0.406 | 2.5% | Very low | OR 1.224 (0.893–1.677) | 0.209 | 0.617 | |
| Leukopenia, single-arm analysis | |||||||||
| CRT arm | 10 | 1154 | <0.001 | 91.9% | Very high | 26.4% (17.7–37.5) | NA | 0.105 | |
| CT arm | 10 | 1133 | <0.001 | 91.1% | Very high | 15.7% (9.4–25.0) | NA | 0.074 | 17.1% (10.7–26.2) |
| N/V, single-arm analysis | |||||||||
| CRT arm | 9 | 1108 | <0.001 | 72.6% | High | 11.2% (7.8–15.8) | NA | 0.200 | |
| CT arm | 9 | 1089 | 0.005 | 63..8% | High | 11.1% (7.6–16.0) | NA | 0.014 | 11.7% (7.7–17.5) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rim, C.H.; Shin, I.-S.; Lee, H.Y.; Yoon, W.S.; Park, S. Oncologic Benefit of Adjuvant Chemoradiation after D2 Gastrectomy: A Stepwise Hierarchical Pooled Analysis and Systematic Review. Cancers 2020, 12, 2125. https://doi.org/10.3390/cancers12082125
Rim CH, Shin I-S, Lee HY, Yoon WS, Park S. Oncologic Benefit of Adjuvant Chemoradiation after D2 Gastrectomy: A Stepwise Hierarchical Pooled Analysis and Systematic Review. Cancers. 2020; 12(8):2125. https://doi.org/10.3390/cancers12082125
Chicago/Turabian StyleRim, Chai Hong, In-Soo Shin, Hye Yoon Lee, Won Sup Yoon, and Sunmin Park. 2020. "Oncologic Benefit of Adjuvant Chemoradiation after D2 Gastrectomy: A Stepwise Hierarchical Pooled Analysis and Systematic Review" Cancers 12, no. 8: 2125. https://doi.org/10.3390/cancers12082125
APA StyleRim, C. H., Shin, I.-S., Lee, H. Y., Yoon, W. S., & Park, S. (2020). Oncologic Benefit of Adjuvant Chemoradiation after D2 Gastrectomy: A Stepwise Hierarchical Pooled Analysis and Systematic Review. Cancers, 12(8), 2125. https://doi.org/10.3390/cancers12082125







