Periodontal Diseases as Putative Risk Factors for Head and Neck Cancer: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Results
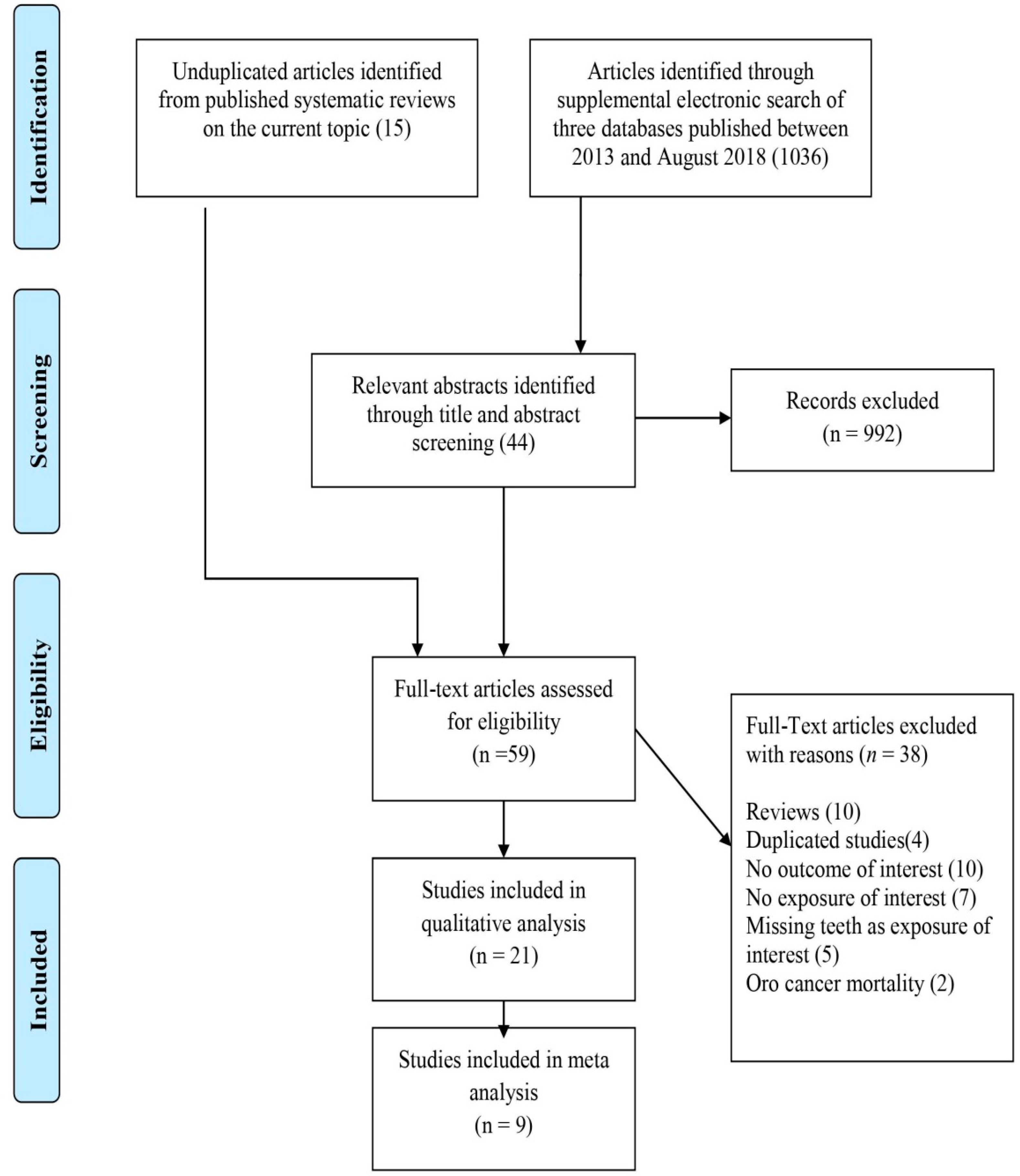
2.1. Study Selection
2.2. Characteristics of the Included Studies
2.2.1. Case Control Studies
2.2.2. Cohort Studies
2.3. Periodontal Disease Measurements
2.4. Data Adjustment for Confounding Factors
2.5. Quality of Studies
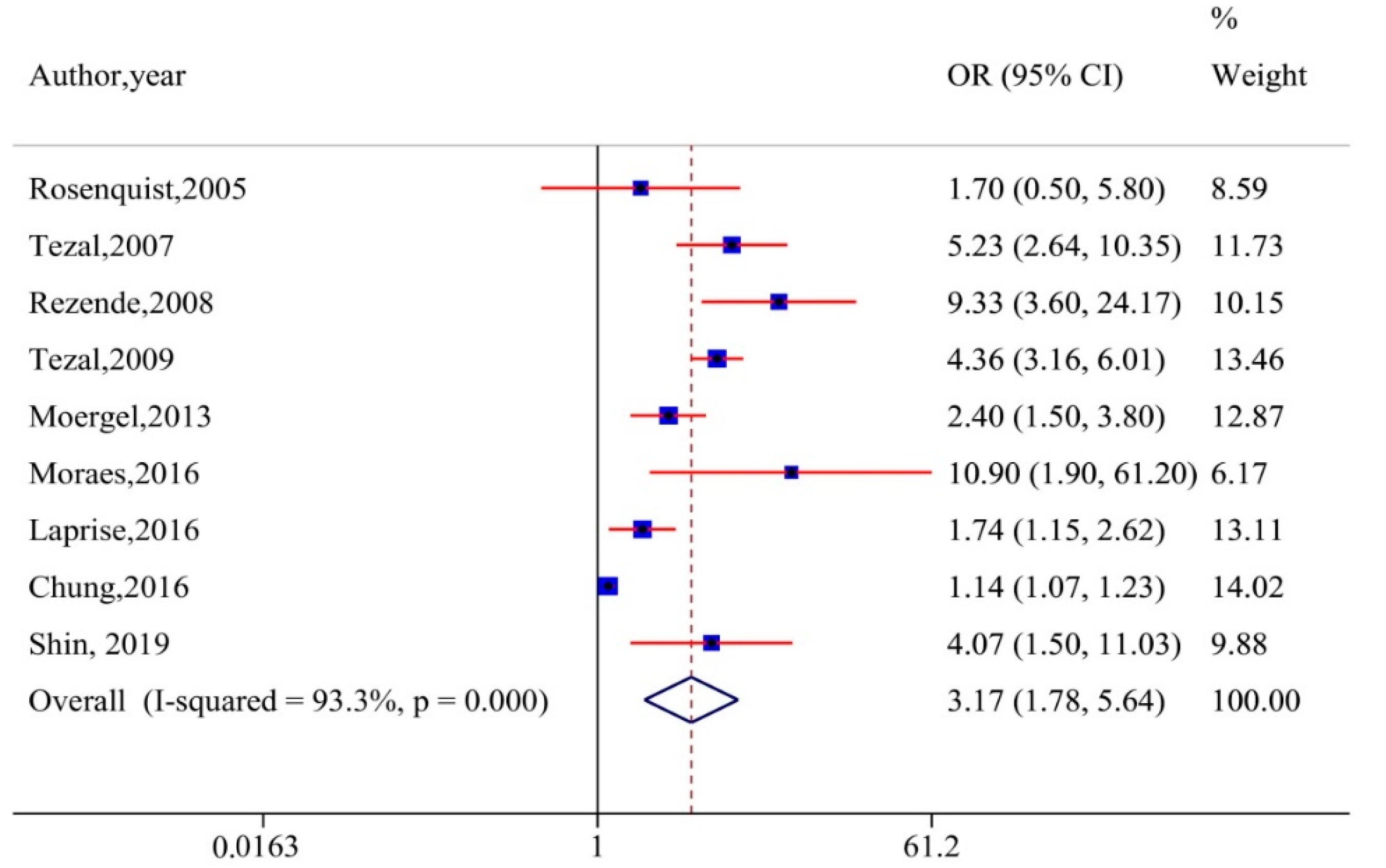
2.6. Meta-Analysis
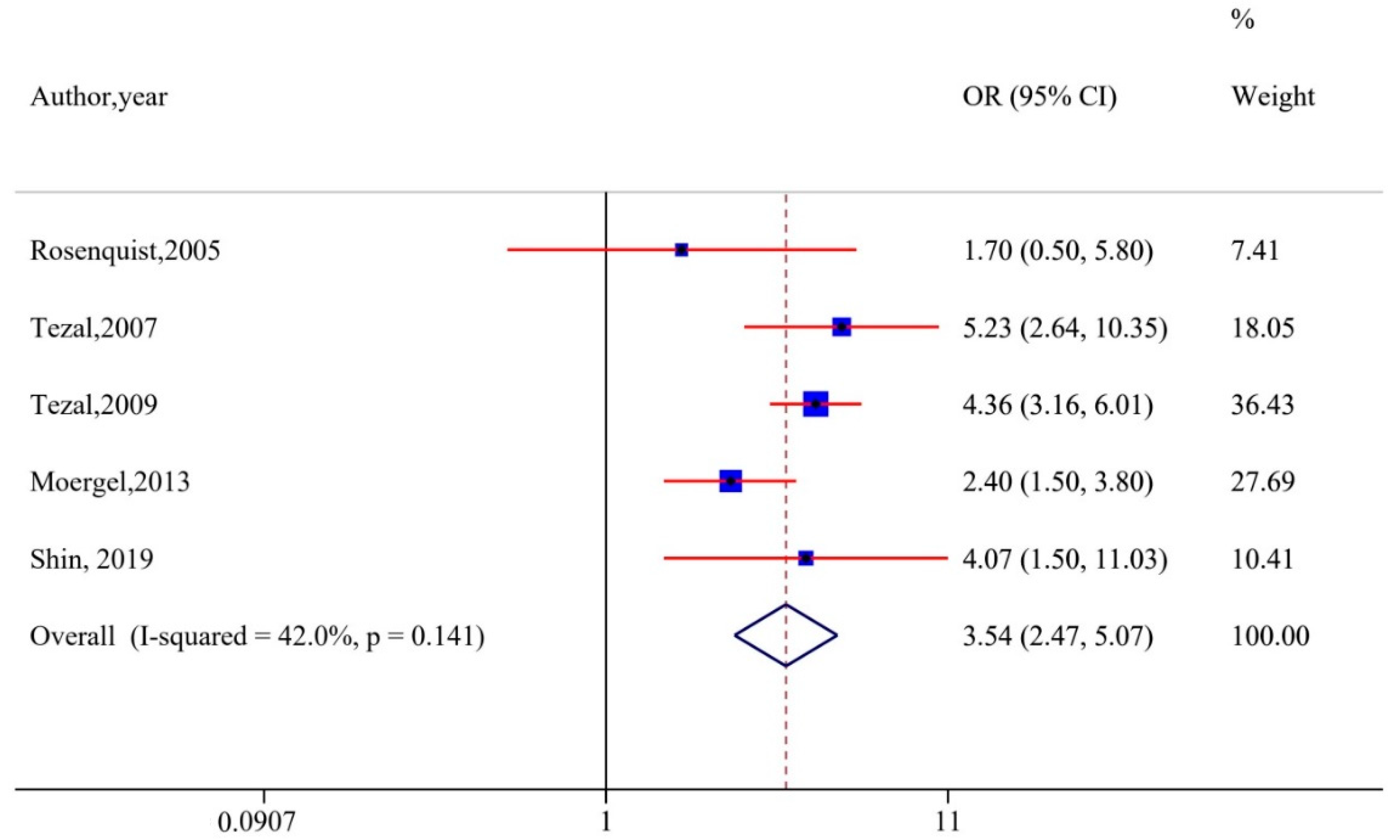
2.7. Sub-Group Analysis and Sensitivity Analysis
2.8. Publication Bias
3. Discussion
4. Limitations
5. Materials and Methods
5.1. Literature Search and Selection
- P—Any population.
- E—Exposed to periodontal diseases.
- C—Not exposed to periodontal disease,
- O—Head and neck cancer,
5.2. Eligibility Criteria
Observational studies (both case control and cohort) that assessed the association between any measure of periodontal status with HNC were included if they met the following criteria: (1) Controls and cases were clearly defined and (2) hazard ratios (HRs), odds ratios (ORs), or risk ratios (unadjusted/adjusted) and related 95% confidence intervals (CIs) were reported, or else the figures that can help to determine any of these ratios were present in the article.
5.3. Data Extraction
5.4. Quality of Studies
5.5. Data Analysis
6. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S68–S77. [Google Scholar] [CrossRef] [PubMed]
- Wilton, J.M.; Griffiths, G.S.; Curtis, M.A.; Maiden, M.F.; Gillett, I.R.; Wilson, D.T.; Sterne, J.A.; Johnson, N.W. Detection of high-risk groups and individuals for periodontal diseases. Systemic predisposition and markers of general health. J. Clin. Periodontol. 1988, 15, 339–346. [Google Scholar] [CrossRef]
- Johnson, N.W.; Griffiths, G.S.; Wilton, J.M.; Maiden, M.F.; Curtis, M.A.; Gillett, I.R.; Wilson, D.T.; Sterne, J.A. Detection of high-risk groups and individuals for periodontal diseases. Evidence for the existence of high-risk groups and individuals and approaches to their detection. J. Clin. Periodontol. 1988, 15, 276–282. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, S.K.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45 (Suppl. 20), s1–s8. [Google Scholar] [CrossRef]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Arigbede, A.O.; Babatope, B.O.; Bamidele, M.K. Periodontitis and systemic diseases: A literature review. J. Indian Soc. Periodontol. 2012, 16, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Onate, M.D.; Pauley, K.M.; Bhattacharyya, I.; Cha, S. Presence of Porphyromonas gingivalis in gingival squamous cell carcinoma. Int. J. Oral Sci. 2011, 3, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Al-Hebshi, N.N.; Nasher, A.T.; Maryoud, M.Y.; Homeida, H.E.; Chen, T.; Idris, A.M.; Johnson, N.W. Inflammatory bacteriome featuring Fusobacterium nucleatum and Pseudomonas aeruginosa identified in association with oral squamous cell carcinoma. Sci. Rep. 2017, 7, 1834. [Google Scholar] [CrossRef]
- Bracci, P.M. Oral Health and the Oral Microbiome in Pancreatic Cancer: An Overview of Epidemiological Studies. Cancer J. 2017, 23, 310–314. [Google Scholar] [CrossRef]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Cognetti, D.M.; Weber, R.S.; Lai, S.Y. Head and neck cancer: An evolving treatment paradigm. Cancer 2008, 113, 1911–1932. [Google Scholar] [CrossRef]
- Gopinath, D.; Menon, R.K.; Banerjee, M.; Botelho, M.G.; Johnson, N.W. Culture-independent studies on bacterial dysbiosis in oral and oropharyngeal squamous cell carcinoma: A systematic review. Crit. Rev. Oncol. Hematol. 2019, 139, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Michaud, D.S.; Fu, Z.; Shi, J.; Chung, M. Periodontal Disease, Tooth Loss, and Cancer Risk. Epidemiol. Rev. 2017, 39, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Beltran-Aguilar, E.D.; Eke, P.I.; Thornton-Evans, G.; Petersen, P.E. Recording and surveillance systems for periodontal diseases. Periodontology 2012, 60, 40–53. [Google Scholar] [CrossRef] [PubMed]
- Leroy, R.; Eaton, K.A.; Savage, A. Methodological issues in epidemiological studies of periodontitis--how can it be improved? BMC Oral Health 2010, 10, 8. [Google Scholar] [CrossRef]
- Periodontal Disease. Available online: https://www.nidcr.nih.gov/research/data-statistics/periodontal-disease (accessed on 15 March 2020).
- Zeng, X.T.; Deng, A.P.; Li, C.; Xia, L.Y.; Niu, Y.M.; Leng, W.D. Periodontal disease and risk of head and neck cancer: A meta-analysis of observational studies. PLoS ONE 2013, 8, e79017. [Google Scholar] [CrossRef]
- Yao, Q.W.; Zhou, D.S.; Peng, H.J.; Ji, P.; Liu, D.S. Association of periodontal disease with oral cancer: A meta-analysis. Tumour Biol. 2014, 35, 7073–7077. [Google Scholar] [CrossRef]
- Javed, F.; Warnakulasuriya, S. Is there a relationship between periodontal disease and oral cancer? A systematic review of currently available evidence. Crit. Rev. Oncol. Hematol. 2016, 97, 197–205. [Google Scholar] [CrossRef]
- Chung, S.D.; Tsai, M.C.; Huang, C.C.; Kao, L.T.; Chen, C.H. A population-based study on the associations between chronic periodontitis and the risk of cancer. Int. J. Clin. Oncol. 2016, 21, 219–223. [Google Scholar] [CrossRef]
- Nwizu, N.N.; Marshall, J.R.; Moysich, K.; Genco, R.J.; Hovey, K.M.; Mai, X.; LaMonte, M.J.; Freudenheim, J.L.; Wactawski-Wende, J. Periodontal Disease and Incident Cancer Risk among Postmenopausal Women: Results from the Women’s Health Initiative Observational Cohort. Cancer Epidemiol. Biomarkers. Prev. 2017, 26, 1255–1265. [Google Scholar] [CrossRef]
- Michaud, D.S.; Kelsey, K.T.; Papathanasiou, E.; Genco, C.A.; Giovannucci, E. Periodontal disease and risk of all cancers among male never smokers: An updated analysis of the Health Professionals Follow-up Study. Ann. Oncol. 2016, 27, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Michaud, D.S.; Liu, Y.; Meyer, M.; Giovannucci, E.; Joshipura, K. Periodontal disease, tooth loss, and cancer risk in male health professionals: A prospective cohort study. Lancet. Oncol. 2008, 9, 550–558. [Google Scholar] [CrossRef]
- Laprise, C.; Shahul, H.P.; Madathil, S.A.; Thekkepurakkal, A.S.; Castonguay, G.; Varghese, I.; Shiraz, S.; Allison, P.; Schlecht, N.F.; Rousseau, M.-C.; et al. Periodontal diseases and risk of oral cancer in Southern India: Results from the HeNCe Life study. Int. J. Cancer 2016, 139, 1512–1519. [Google Scholar] [CrossRef]
- Mazul, A.L.; Taylor, J.M.; Divaris, K.; Weissler, M.C.; Brennan, P.; Anantharaman, D.; Abedi-Ardekani, B.; Olshan, A.F.; Zevallos, J.P. Oral health and human papillomavirus-associated head and neck squamous cell carcinoma. Cancer 2017, 123, 71–80. [Google Scholar] [CrossRef]
- Moergel, M.; Kammerer, P.; Kasaj, A.; Armouti, E.; Alshihri, A.; Weyer, V.; Al-Nawas, B. Chronic periodontitis and its possible association with oral squamous cell carcinoma—A retrospective case control study. Head Face Med. 2013, 9, 39. [Google Scholar] [CrossRef] [PubMed]
- Moraes, R.C.; Dias, F.L.; Figueredo, C.M.; Fischer, R.G. Association between Chronic Periodontitis and Oral/Oropharyngeal Cancer. Braz. Dental. J. 2017, 27, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Hashim, D.; Sartori, S.; Brennan, P.; Curado, M.P.; Wunsch-Filho, V.; Divaris, K.; Olshan, A.F.; Zevallos, J.P.; Winn, D.M.; Franceschi, S.; et al. The role of oral hygiene in head and neck cancer: Results from International Head and Neck Cancer Epidemiology (INHANCE) consortium. Ann. Oncol. 2016, 27, 1619–1625. [Google Scholar] [CrossRef]
- Tezal, M.; Sullivan, M.A.; Reid, M.E.; Marshall, J.R.; Hyland, A.; Loree, T.; Lillis, C.; Hauck, L.; Wactawski-Wende, J.; Scannapieco, F.A.; et al. Chronic periodontitis and the risk of tongue cancer. Arch. Otolaryngol. 2007, 133, 450–454. [Google Scholar] [CrossRef]
- Tezal, M.; Sullivan, M.A.; Hyland, A.; Marshall, J.R.; Stoler, D.; Reid, M.E.; Loree, R.L.; Rigual, R.N.; Merzianu, M.; Hauck, L.; et al. Chronic periodontitis and the incidence of head and neck squamous cell carcinoma. Cancer Epidemiol. Biomarkers Prev. 2009, 18, 2406–2412. [Google Scholar] [CrossRef]
- Rosenquist, K.; Wennerberg, J.; Schildt, E.B.; Bladstrom, A.; Goran Hansson, B.; Andersson, G. Oral status, oral infections and some lifestyle factors as risk factors for oral and oropharyngeal squamous cell carcinoma. A population-based case-control study in southern Sweden. Acta Otolaryngol. 2005, 125, 1327–1336. [Google Scholar] [CrossRef]
- Garrote, L.F.; Herrero, R.; Reyes, R.M.; Vaccarella, S.; Anta, J.L.; Ferbeye, L.; Muñoz, N.; Franceschi, S. Risk factors for cancer of the oral cavity and oro-pharynx in Cuba. Br. J. Cancer 2001, 85, 46–54. [Google Scholar] [CrossRef]
- Chang, J.S.; Lo, H.I.; Wong, T.Y.; Huang, C.C.; Lee, W.T.; Tsai, S.T.; Chen, K.C.; Yen, C.J.; Wu, Y.H.; Hsueh, W.T.; et al. Investigating the association between oral hygiene and head and neck cancer. Oral Oncol. 2013, 49, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, W.; Pohlabeln, H.; Foraita, R.; Nelis, M.; Lagiou, P.; Lagiou, A.; Bouchardy, C.; Slamova, A.; Schejbalova, M.; Merletti, F.; et al. Oral health, dental care and mouthwash associated with upper aerodigestive tract cancer risk in Europe: The ARCAGE study. Oral Oncol. 2014, 50, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Talamini, R.; Vaccarella, S.; Barbone, F.; Tavani, A.; La Vecchia, C.; Herrero, R.; Muñoz, N.; Franceschi, S. Oral hygiene, dentition, sexual habits and risk of oral cancer. Br. J. Cancer 2000, 83, 1238–1242. [Google Scholar] [CrossRef] [PubMed]
- Rezende, C.P.; Ramos, M.B.; Daguila, C.H.; Dedivitis, R.A.; Rapoport, A. Oral health changes in with oral and oropharyngeal cancer. Braz. J. Otorhinolaryngol. 2008, 74, 596–600. [Google Scholar] [CrossRef]
- Balaram, P.; Sridhar, H.; Rajkumar, T.; Vaccarella, S.; Herrero, R.; Nandakumar, A.; Ravichandran, K.; Ramdas, K.; Sankaranarayanan, V.; Gajalakshmi, V.; et al. Oral cancer in southern India: The influence of smoking, drinking, paan-chewing and oral hygiene. Int. J. Cancer 2002, 98, 440–445. [Google Scholar] [CrossRef]
- Eliot, M.N.; Michaud, D.S.; Langevin, S.M.; McClean, M.D.; Kelsey, K.T. Periodontal disease and mouthwash use are risk factors for head and neck squamous cell carcinoma. Cancer Causes Control 2013, 24, 1315–1322. [Google Scholar] [CrossRef]
- Shin, Y.J.; Choung, H.W.; Lee, J.H.; Rhyu, I.C.; Kim, H.D. Association of Periodontitis with Oral Cancer: A Case-Control Study. J. Dent. Res. 2019, 98, 526–533. [Google Scholar] [CrossRef]
- Chang, J.S.; Tsai, C.R.; Chen, L.T.; Shan, Y.S. Investigating the Association Between Periodontal Disease and Risk of Pancreatic Cancer. Pancreas 2016, 45, 134–141. [Google Scholar] [CrossRef]
- Sinha, D.N.; Gupta, P.C.; Ray, C.S.; Singh, P.K. Prevalence of smokeless tobacco use among adults in WHO South-East Asia. Indian J. Cancer 2012, 49, 342. [Google Scholar] [CrossRef]
- Dalton, J.E.; Bolen, S.D.; Mascha, E.J. Publication Bias: The Elephant in the Review. Anesth. Analg. 2016, 123, 812–813. [Google Scholar] [CrossRef] [PubMed]
- Buhlin, K.; Gustafsson, A.; Andersson, K.; Hakansson, J.; Klinge, B. Validity and limitations of self-reported periodontal health. Community Dent. Oral Epidemiol. 2002, 30, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Vered, Y.; Sgan-Cohen, H.D. Self-perceived and clinically diagnosed dental and periodontal health status among young adults and their implications for epidemiological surveys. BMC Oral Health 2003, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Connor Gorber, S.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [PubMed]
- Page, R.C.; Eke, P.I. Case definitions for use in population-based surveillance of periodontitis. J. Periodontol. 2007, 78, 1387–1399. [Google Scholar] [CrossRef] [PubMed]
- Savage, A.; Eaton, K.A.; Moles, D.R.; Needleman, I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J. Clin. Periodontol. 2009, 36, 458–467. [Google Scholar] [CrossRef]
- Armitage, G.C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef]
- Bueno, A.C.; Ferreira, R.C.; Cota, L.O.; Silva, G.C.; Magalhaes, C.S.; Moreira, A.N. Comparison of different criteria for periodontitis case definition in head and neck cancer individuals. Support. Care Cancer 2015, 23, 2599–2604. [Google Scholar] [CrossRef]
- Holtfreter, B.; Albandar, J.M.; Dietrich, T.; Dye, B.A.; Eaton, K.A.; Eke, P.I.; Papapanou, P.P.; Kocher, T. Joint EU/USA Periodontal Epidemiology Working Group. Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies: Proposed standards from the Joint EU/USA Periodontal Epidemiology Working Group. J. Clin. Periodontol. 2015, 42, 407–412. [Google Scholar] [CrossRef]
- Deschamps-Lenhardt, S.; Martin-Cabezas, R.; Hannedouche, T.; Huck, O. Association between periodontitis and chronic kidney disease: Systematic review and meta-analysis. Oral Dis. 2018, 25, 385–402. [Google Scholar] [CrossRef]
- Blaizot, A.; Vergnes, J.N.; Nuwwareh, S.; Amar, J.; Sixou, M. Periodontal diseases and cardiovascular events: Meta-analysis of observational studies. Int. Dent. J. 2009, 59, 197–209. [Google Scholar] [PubMed]
- Martin-Cabezas, R.; Seelam, N.; Petit, C.; Agossa, K.; Gaertner, S.; Tenenbaum, H.; Davideau, J.L.; Huck, O. Association between periodontitis and arterial hypertension: A systematic review and meta-analysis. Am. Heart J. 2016, 180, 98–112. [Google Scholar] [CrossRef]
- Berlin-Broner, Y.; Febbraio, M.; Levin, L. Association between apical periodontitis and cardiovascular diseases: A systematic review of the literature. Int. Endod. J. 2017, 50, 847–859. [Google Scholar] [CrossRef] [PubMed]
- Rutter-Locher, Z.; Smith, T.O.; Giles, I.; Sofat, N. Association between Systemic Lupus Erythematosus and Periodontitis: A Systematic Review and Meta-analysis. Front. Immunol. 2017, 8, 1295. [Google Scholar] [CrossRef]
- Liu, L.H.; Li, E.M.; Zhong, S.L.; Li, Y.Q.; Yang, Z.Y.; Kang, R.; Zhao, S.K.; Li, F.T.; Wan, S.P.; Zhao, Z.G. Chronic periodontitis and the risk of erectile dysfunction: A systematic review and meta-analysis. Int. J. Impot. Res. 2017, 29, 43–48. [Google Scholar] [CrossRef]
- Zhao, D.; Khawaja, A.T.; Jin, L.; Li, K.Y.; Tonetti, M.; Pelekos, G. The directional and non-directional associations of periodontitis with chronic kidney disease: A systematic review and meta-analysis of observational studies. J. Periodont. Res. 2018, 53, 682–704. [Google Scholar] [CrossRef]
- Li, S.; Liu, X.; Zhou, Y.; Acharya, A.; Savkovic, V.; Xu, C.; Wu, N.; Deng, Y.; Hu, X.; Li, H.; et al. Shared genetic and epigenetic mechanisms between chronic periodontitis and oral squamous cell carcinoma. Oral Oncol. 2018, 86, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Arora, M.; Weuve, J.; Fall, K.; Pedersen, N.L.; Mucci, L.A. An exploration of shared genetic risk factors between periodontal disease and cancers: A prospective co-twin study. Am. J. Epidemiol. 2010, 171, 253–259. [Google Scholar] [CrossRef]
- da Silva, M.K.; de Carvalho, A.C.G.; Alves, E.H.P.; da Silva, F.R.P.; Pessoa, L.D.S.; Vasconcelos, D.F.P. Genetic Factors and the Risk of Periodontitis Development: Findings from a Systematic Review Composed of 13 Studies of Meta-Analysis with 71,531 Participants. Int. J. Dent. 2017, 2017, 1914073. [Google Scholar] [CrossRef]
- Gopinath, D.; Menon, R.K. Unravelling the molecular signatures in HNSCC: Is the homogenous paradigm becoming obsolete? Oral Oncol. 2018, 82, 19. [Google Scholar] [CrossRef]
- Hwang, I.M.; Sun, L.M.; Lin, C.L.; Lee, C.F.; Kao, C.H. Periodontal disease with treatment reduces subsequent cancer risks. QJM 2014, 107, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Hyde, S.; Dupuis, V.; Mariri, B.P.; Dartevelle, S. Prevention of tooth loss and dental pain for reducing the global burden of oral diseases. Int. Dent. J. 2017, 67 (Suppl. 2), 19–25. [Google Scholar] [CrossRef]
- Zheng, T.Z.; Boyle, P.; Hu, H.F.; Duan, J.; Jian, P.J.; Ma, D.Q.; Shui, L.P.; Niu, S.R.; Scully, C.; MacMahon, B. Dentition, oral hygiene, and risk of oral cancer: A case-control study in Beijing, People’s Republic of China. Cancer Causes Control 1990, 1, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.S.; Hu, X.Y.; Gu, W.J.; Hu, Z.; Wei, B. Tooth loss and risk of head and neck cancer: A meta-analysis. PLoS ONE 2013, 8, e71122. [Google Scholar] [CrossRef]
- Baelum, V.; Luan, W.M.; Chen, X.; Fejerskov, O. Predictors of tooth loss over 10 years in adult and elderly Chinese. Community Dent. Oral Epidemiol. 1997, 25, 204–210. [Google Scholar] [CrossRef]
- Shigli, K.; Hebbal, M.; Angadi, G.S. Relative contribution of caries and periodontal disease in adult tooth loss among patients reporting to the Institute of Dental Sciences, Belgaum, India. Gerodontology 2009, 26, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Chauncey, H.H.; Glass, R.L.; Alman, J.E. Dental caries. Principal cause of tooth extraction in a sample of US male adults. Caries Res. 1989, 23, 200–205. [Google Scholar] [CrossRef]
- Gopinath, D.; Menon, R. C-reactive protein as an individual prognostic marker in oral cancer: Practical considerations. Clin. Otolaryngol. 2018, 43, 1184. [Google Scholar] [CrossRef]
- Loos, B.G. Systemic Markers of Inflammation in Periodontitis. J. Periodontol. 2005, 76 (Suppl. 11S), 2106–2115. [Google Scholar] [CrossRef]
- Moutsopoulos, N.M.; Madianos, P.N. Low-grade inflammation in chronic infectious diseases: Paradigm of periodontal infections. Ann. N. Y. Acad. Sci. 2006, 1088, 251–264. [Google Scholar] [CrossRef]
- Graves, D. Cytokines that promote periodontal tissue destruction. J. Periodontol. 2008, 79, 1585–1591. [Google Scholar] [CrossRef] [PubMed]
- Kuboniwa, M.; Hasegawa, Y.; Mao, S.; Shizukuishi, S.; Amano, A.; Lamont, R.J.; Yilmaz, O.P. gingivalis accelerates gingival epithelial cell progression through the cell cycle. Microbes Infect. 2008, 10, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Nagy, K.N.; Sonkodi, I.; Szoke, I.; Nagy, E.; Newman, H.N. The micoflora associated with human oral carcinomas. Oral Oncol. 1998, 34, 304–308. [Google Scholar] [CrossRef]
- Kostic, A.D.; Chun, E.; Robertson, L.; Glickman, J.N.; Gallini, C.A.; Michaud, M.; Clancy, T.E.; Chung, D.C.; Lochhead, P.; Hold, G.L.; et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013, 14, 207–215. [Google Scholar] [CrossRef]
- Uitto, V.J.; Baillie, D.; Wu, Q.; Gendron, R.; Grenier, D.; Putnins, E.E.; Kanervo, A.; Firth, J.D. Fusobacterium nucleatum increases collagenase 3 production and migration of epithelial cells. Infect. Immun. 2005, 73, 1171–1179. [Google Scholar] [CrossRef]
- Ha, N.H.; Woo, B.H.; Ha, E.S.; Choi, J.I.; Kim, S.J.; Park, B.S.; Lee, J.H.; Park, H.R. Prolonged and repetitive exposure to Porphyromonas gingivalis increases aggressiveness of oral cancer cells by promoting acquisition of cancer stem cell properties. Tumour Biol. 2015, 36, 9947–9960. [Google Scholar] [CrossRef]
- Binder Gallimidi, A.; Fischman, S.; Revach, B.; Bulvik, R.; Maliutina, A.; Rubinstein, A.M.; Nussbaum, G.; Elkin, M. Periodontal pathogens Porphyromonas gingivalis and Fusobacterium nucleatum promote tumor progression in an oral-specific chemical carcinogenesis model. Oncotarget 2015, 6, 22613–22623. [Google Scholar] [CrossRef]
- Ahn, J.; Segers, S.; Hayes, R.B. Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis 2012, 33, 1055–1058. [Google Scholar] [CrossRef]
- Castellarin, M.; Warren, R.L.; Freeman, J.D.; Dreolini, L.; Krzywinski, M.; Strauss, J.; Barnes, R.; Watson, P.; Allen-Vercoe, E.; Moore, R.A.; et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res. 2012, 22, 299–306. [Google Scholar] [CrossRef]
- Brennan, C.A.; Garrett, W.S. Fusobacterium nucleatum-symbiont, opportunist and oncobacterium. Nat. Rev. Microbiol. 2018, 17, 156–166. [Google Scholar] [CrossRef]
- Menon, R.K.; Gopinath, D. Eliminating bias and accelerating the clinical translation of oral microbiome research in oral oncology. Oral Oncol. 2018, 79, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, D.; Thannikunnath, B.V.; Neermunda, S.F. Prevalence of Carcinomatous Foci in Oral Leukoplakia: A Clinicopathologic Study of 546 Indian Samples. J. Clin. Diagn. Res. 2016, 10, ZC78–ZC83. [Google Scholar]
- Song, F.; Parekh, S.; Hooper, L.; Loke, Y.K.; Ryder, J.; Sutton, A.J.; Hing, C.; Kwok, C.S.; Pang, C.; Harvey, I. Dissemination and publication of research findings: An updated review of related biases. Health Technol. Assess. 2010, 14, 1–193. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Sutton, A.J.; Duval, S.J.; Tweedie, R.L.; Abrams, K.R.; Jones, D.R. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000, 320, 1574–1577. [Google Scholar] [CrossRef]
- Xu, S.; Song, M.; Xiong, Y.; Liu, X.; He, Y.; Qin, Z. The association between periodontal disease and the risk of myocardial infarction: A pooled analysis of observational studies. BMC Cardiovasc. Disord. 2017, 17, 50. [Google Scholar] [CrossRef]
- Araujo, M.M.; Martins, C.C.; Costa, L.C.; Cota, L.O.; Faria, R.L.; Cunha, F.A.; Costa, O.F. Association between depression and periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2016, 43, 216–228. [Google Scholar] [CrossRef]
- Preshaw, P.M. Detection and diagnosis of periodontal conditions amenable to prevention. BMC Oral Health 2015, 15, S5. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, K.F. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998, 280, 1690–1691. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]

| Author | Year | Design | Population | Cases | Controls | Age Range | PD Assessment | Subtype | OR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Talam-ini [35] | 2000 | case control | Italy | 112 | 125 | 60 (median) | Self-reported gum bleeding | OSCC | 2.4 (1.5–3.8) |
| Garrote [32] | 2001 | case control | Cuba | 150 | 171 | 28–91 | Self-reported gum bleeding | OC/OPC | 2.03 (0.66–6.25) |
| Balaram [37] | 2002 | case control | India | 307 | 291 | 56 (22–85) M | Self-reported gum bleeding | OC | 2.83 (1.71–4.68) |
| Balaram [37] | 2002 | case control | India | 248 | 290 | 58(18–87) F | Self-reported gum bleeding | OC | 3.35 (1.82–6.15) |
| Rosenq-uist [31] # | 2005 | case control | Sweden | 132 | 320 | Ca:33–87/ Co:33–89 | Alveolar bone loss | O/OPSCC | 1.7 (0.5–5.8) |
| Tezal [29] # | 2007 | case control | USA | 51 | 54 | 54.6 ± 15.9 | Alveolar bone loss | Oral tumor | 5.23 (2.64–10.35) |
| Rezende [36] # | 2008 | case control | Brazil | 50 | 50 | >40 | CPITN | O/OPSCC | 9.33 (3.60–24.17) |
| Tezal [30] # | 2009 | case control | USA | 266 | 207 | Ca:56.89 ± 11.73/ Co:54.00 ± 15.45 | Alveolar bone loss | HNSCC | 4.36 (3.16–6.01) |
| Moergel [26] # | 2013 | case control | Germany | 178 | 123 | 60 (mean) | Mean bone loss | OSCC | 2.4 (1.5–3.8) |
| Chang [33] | 2013 | case control | Taiwan | 317 | 296 | Ca-54.6/ Co 53.1 | Self-reported gum bleeding | HNSCC | 3.15 (1.36–7.28) |
| Eliot [38] | 2013 | case control | USA | 513 | 567 | Nil | Self-reported periodontal disease | HNSCC | 1.09 (1.02–1.16) |
| ARCA-GE [34] | 2014 | case control | Europe | 1963 | 1993 | Ca-59.8 ± 10.1/ Co-59.8 ± 11.8 | Self-reported Gum bleeding | Aerodigestive tract | 1.15 (0.81–1.63) |
| INHA-NCE [28] | 2016 | case control | Multi-centric | 2672 | 2634 | 15–80 | Self-reported Gum disease | HNSCC | 1.98 (1.68, 2.35) |
| Moraes [27] # | 2016 | case control | Brazil | 35 | 40 | Ca: 55.1 ± 8.4/ Co:55.4 ± 9.4 | Severity of periodontal diseasemeasured by probe | O/OPC | 10.9 (1.9–61.2) |
| Laprise [24] # | 2016 | case control | India | 306 | 328 | Ca-60 ± 10.8/ Co-59.2 ± 11.3 | Gingival recession | OSCC | 1.74 (1.15–2.62) |
| Mazul [25] | 2017 | case control | USA | 212 | 321 | 20–80 | Self-reported tooth mobility | OC | 1.58 (1.05–2.37) |
| Shin [39] # | 2019 | case control | Korea | 146 | 278 | Ca:63.8/Co:64.4 | Alveolar bone loss | OSCC | 4.066 (1.499 to 11.026) |
| Author | Year | Duration | Population | Cases | Controls | Age Range | PD Assessment | Sub Type | HR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Michaud [23] | 2008 | 18 | USA | 7863 | 40,512 | 40–75 | Self-reported periodontitis | OPC | 1.15 (0.73–1.81) |
| Chung [20] # | 2016 | 5 | Taiwan | 40,140 | 40,140 | 54.1 ± 11.5 | Diagnosis of chronic periodontitis | OC (ICD-9-CM code 140–149) | 1.20 (1.09–1.33) |
| Michaud [22] | 2016 | 26 | USA | 1768 | 17,554 | 40–75 | Self-reported periodontitis | OPC | 2.25 (1.30–3.90) |
| Nwizu [21] | 2017 | USA | 17,103 | 48,766 | 68.3(Mean) | Self-reported periodontitis | Lip, oral cavity and pharynx | 1.10 (0.64–1.87) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gopinath, D.; Kunnath Menon, R.; K. Veettil, S.; George Botelho, M.; Johnson, N.W. Periodontal Diseases as Putative Risk Factors for Head and Neck Cancer: Systematic Review and Meta-Analysis. Cancers 2020, 12, 1893. https://doi.org/10.3390/cancers12071893
Gopinath D, Kunnath Menon R, K. Veettil S, George Botelho M, Johnson NW. Periodontal Diseases as Putative Risk Factors for Head and Neck Cancer: Systematic Review and Meta-Analysis. Cancers. 2020; 12(7):1893. https://doi.org/10.3390/cancers12071893
Chicago/Turabian StyleGopinath, Divya, Rohit Kunnath Menon, Sajesh K. Veettil, Michael George Botelho, and Newell W. Johnson. 2020. "Periodontal Diseases as Putative Risk Factors for Head and Neck Cancer: Systematic Review and Meta-Analysis" Cancers 12, no. 7: 1893. https://doi.org/10.3390/cancers12071893
APA StyleGopinath, D., Kunnath Menon, R., K. Veettil, S., George Botelho, M., & Johnson, N. W. (2020). Periodontal Diseases as Putative Risk Factors for Head and Neck Cancer: Systematic Review and Meta-Analysis. Cancers, 12(7), 1893. https://doi.org/10.3390/cancers12071893





