Population Pharmacokinetics of Vincristine Related to Infusion Duration and Peripheral Neuropathy in Pediatric Oncology Patients
Abstract
1. Introduction
2. Results
2.1. Study Population
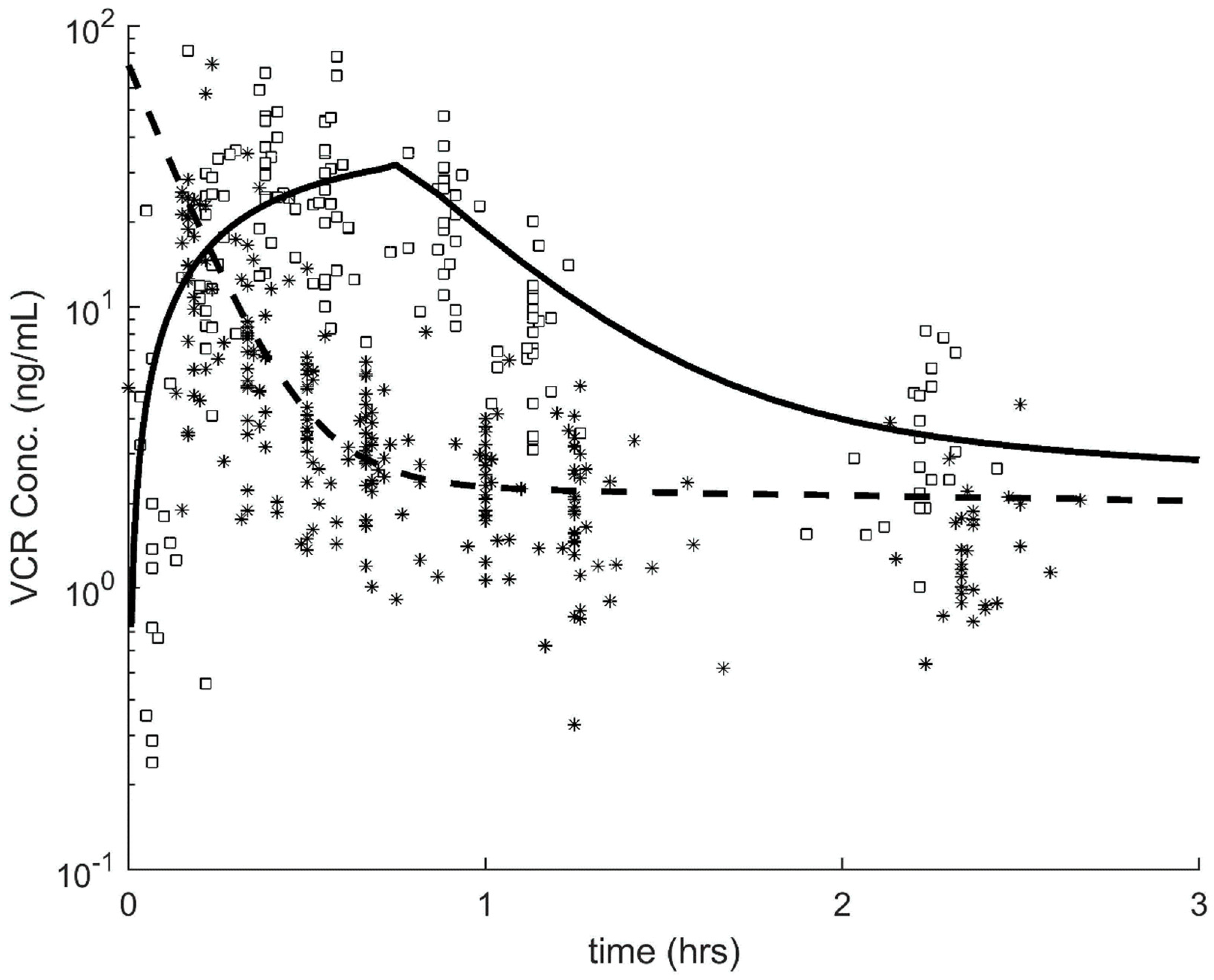
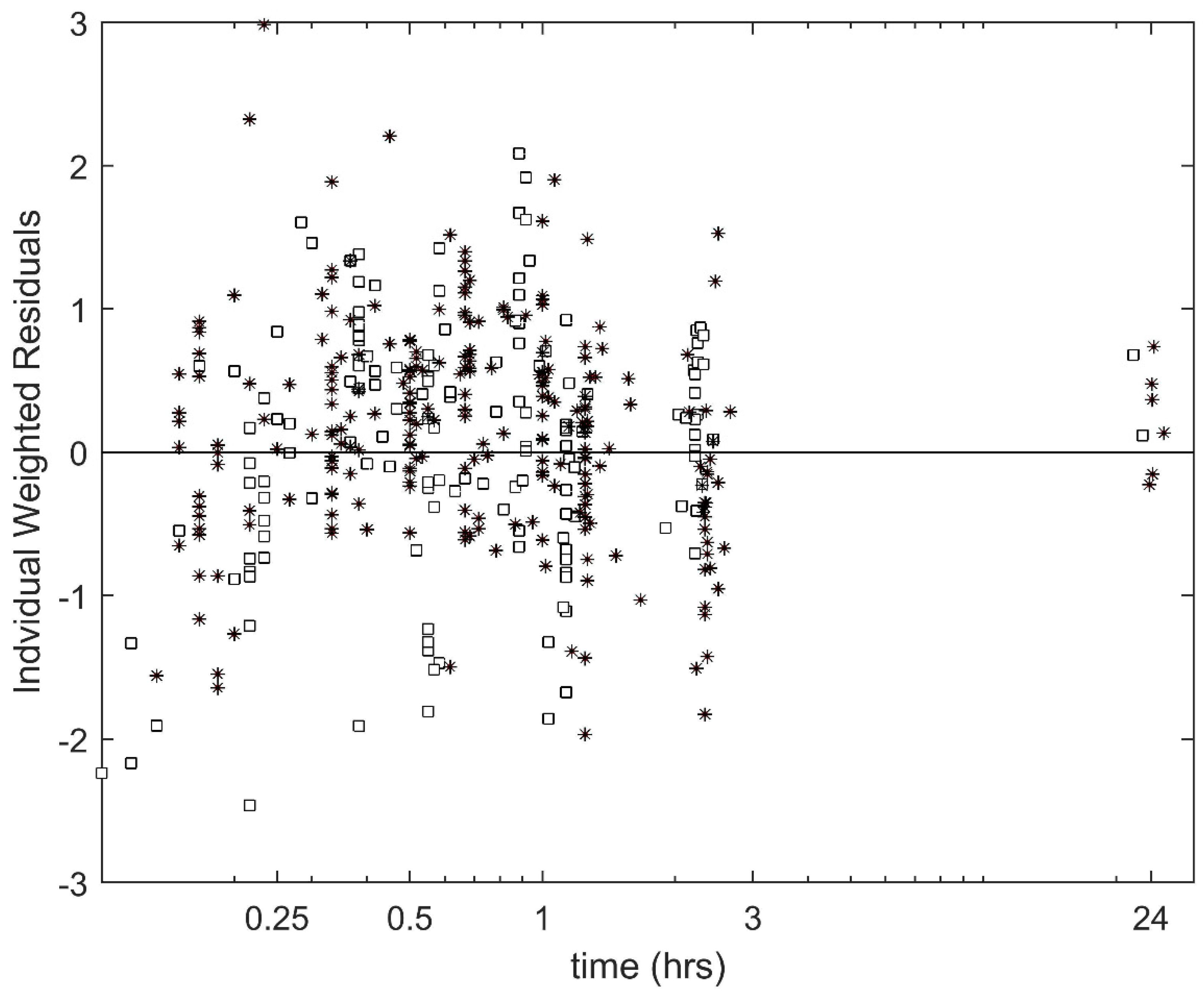
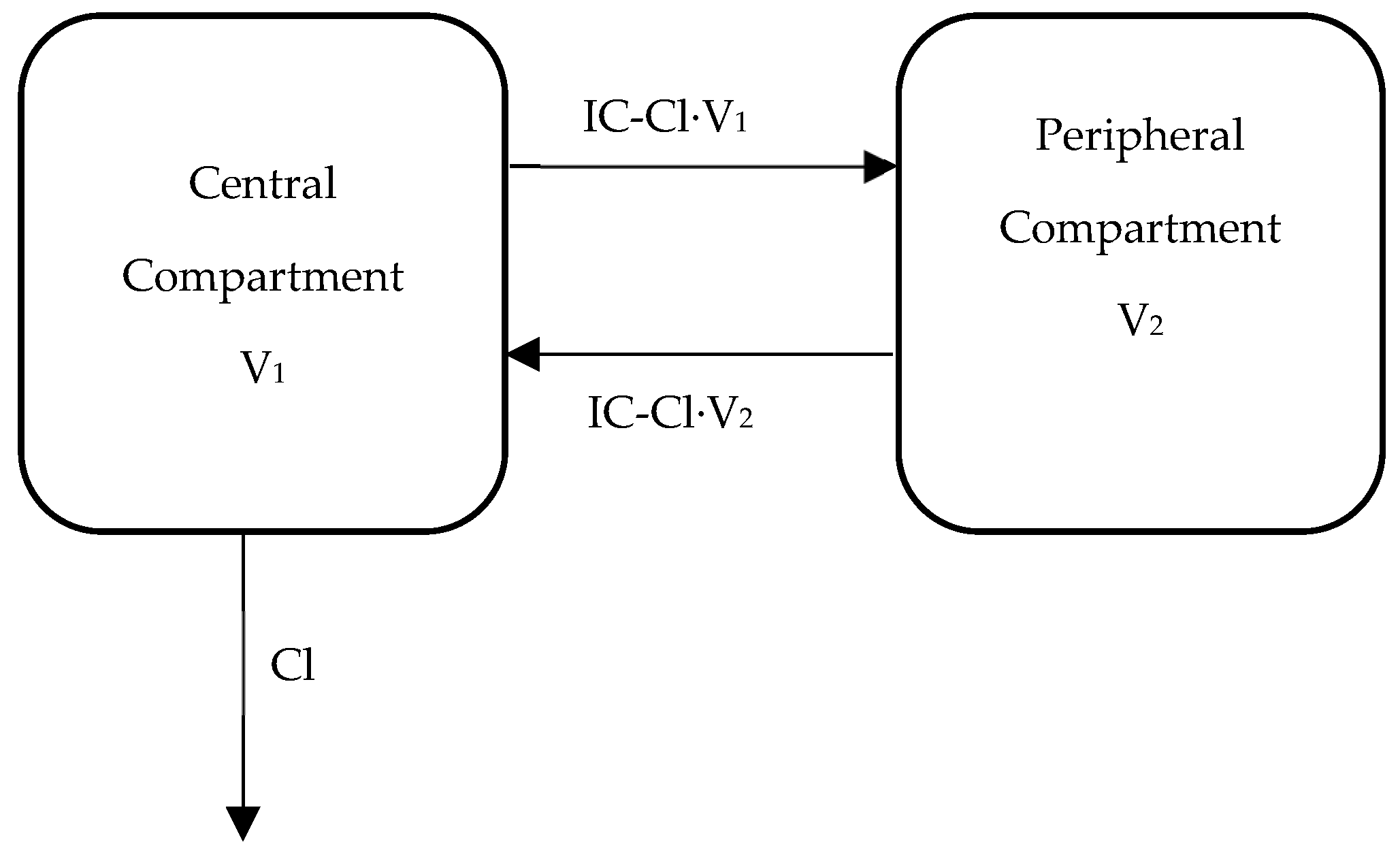
2.2. Population Pharmacokinetics of VCR
2.3. Association between PK Parameters and VIPN
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Pharmacokinetic Sampling
4.3. Assessment of VIPN
4.4. Quantification of Plasma VCR Concentrations
4.5. Pharmacokinetic Analysis
4.6. Concurrent Azole Antifungal Treatment
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- van de Velde, M.E.; Kaspers, G.L.; Abbink, F.C.H.; Wilhelm, A.J.; Ket, J.C.F.; van den Berg, M.H. Vincristine-induced peripheral neuropathy in children with cancer: A systematic review. Crit. Rev. Oncol. Hematol. 2017, 114, 114–130. [Google Scholar] [CrossRef] [PubMed]
- Coccia, P.F.; Altman, J.; Bhatia, S.; Borinstein, S.C.; Flynn, J.; George, S.; Goldsby, R.; Hayashi, R.; Huang, M.S.; Johnson, R.H.; et al. Adolescent and young adult oncology clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2012, 10, 1112–1150. [Google Scholar] [CrossRef]
- Stryckmans, P.A.; Lurie, P.M.; Manaster, J.; Vamecq, G. Mode of action of chemotherapy in vivo on human acute leukemia—II. Vincristine. Eur. J. Cancer 1973, 9, 613–620. [Google Scholar] [CrossRef]
- Dennison, J.B.; Jones, D.R.; Renbarger, J.L.; Hall, S.D. Effect of CYP3A5 expression on vincristine metabolism with human liver microsomes. J. Pharmacol. Exp. Ther. 2007, 321, 553–563. [Google Scholar] [CrossRef]
- Bloemhof, H.; Van Dijk, K.N.; De Graaf, S.S.; Vendrig, D.E.; Uges, D.R. Sensitive method for the determination of vincristine in human serum by high-performance liquid chromatography after on-line column-extraction. J. Chromatogr. 1991, 572, 171–179. [Google Scholar] [CrossRef]
- Crom, W.R.; De Graaf, S.S.; Synold, T.; Uges, D.R.; Bloemhof, H.; Rivera, G.; Christensen, M.L.; Mahmoud, H.; Evans, W.E. Pharmacokinetics of vincristine in children and adolescents with acute lymphocytic leukemia. J. Pediatr. 1994, 125, 642–649. [Google Scholar] [CrossRef]
- Gidding, C.E.; Meeuwsen-de Boer, G.J.; Koopmans, P.; Uges, D.R.; Kamps, W.A.; de Graaf, S.S. Vincristine pharmacokinetics after repetitive dosing in children. Cancer Chemother. Pharmacol. 1999, 44, 203–209. [Google Scholar] [CrossRef]
- Guilhaumou, R.; Simon, N.; Quaranta, S.; Verschuur, A.; Lacarelle, B.; Andre, N.; Solas, C. Population pharmacokinetics and pharmacogenetics of vincristine in paediatric patients treated for solid tumour diseases. Cancer Chemother. Pharmacol. 2011, 68, 1191–1198. [Google Scholar] [CrossRef]
- Groninger, E.; Meeuwsen-De Boer, G.J.; De Graaf, S.S.; Kamps, W.A.; De Bont, E.S. Vincristine induced apoptosis in acute lymphoblastic leukaemia cells: A mitochondrial controlled pathway regulated by reactive oxygen species? Int. J. Oncol. 2002, 21, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- Groninger, E.; Meeuwsen-de Boar, T.; Koopmans, P.; Uges, D.; Sluiter, W.; Veerman, A.; Kamps, W.; de Graaf, S. Pharmacokinetics of vincristine monotherapy in childhood acute lymphoblastic leukemia. Pediatr. Res. 2002, 52, 113–118. [Google Scholar] [CrossRef]
- Moore, A.S.; Norris, R.; Price, G.; Nguyen, T.; Ni, M.; George, R.; Van, B.K.; Duley, J.; Charles, B.; Pinkerton, R. Vincristine pharmacodynamics and pharmacogenetics in children with cancer: A limited-sampling, population modelling approach. J. Paediatr. Child Health 2011, 47, 875–882. [Google Scholar] [CrossRef]
- Plasschaert, S.L.A.; Groninger, E.; Boezen, M.; Kema, I.; De Vries, E.G.E.; Uges, D.; Veerman, A.J.P.; Kamps, W.A.; Vellenga, E.; De Graaf, S.S.; et al. Influence of functional polymorphisms of the MDR1 gene on vincristine pharmacokinetics in childhood acute lymphoblastic leukemia. Clin. Pharmacol. Ther. 2004, 76, 220–229. [Google Scholar] [CrossRef]
- Egbelakin, A.; Ferguson, M.J.; MacGill, E.A.; Lehmann, A.S.; Topletz, A.R.; Quinney, S.K.; Li, L.; McCammack, K.C.; Hall, S.D.; Renbarger, J.L. Increased risk of vincristine neurotoxicity associated with low CYP3A5 expression genotype in children with acute lymphoblastic leukemia. Pediatr. Blood Cancer 2011, 56, 361–367. [Google Scholar] [CrossRef]
- Lavoie Smith, E.M.; Li, L.; Hutchinson, R.J.; Ho, R.; Burnette, W.B.; Wells, E.; Bridges, C.; Renbarger, J. Measuring vincristine-induced peripheral neuropathy in children with acute lymphoblastic leukemia. Cancer Nurs. 2013, 36, E49–E60. [Google Scholar] [CrossRef]
- Diouf, B.; Crews, K.R.; Lew, G.; Pei, D.; Cheng, C.; Bao, J.; Zheng, J.J.; Yang, W.; Fan, Y.; Wheeler, H.E.; et al. Association of an inherited genetic variant with vincristine-related peripheral neuropathy in children with acute lymphoblastic leukemia. JAMA J. Am. Med. Assoc. 2015, 313, 815–823. [Google Scholar] [CrossRef]
- Gidding, C.E.; Kellie, S.J.; Kamps, W.A.; De Graaf, S.S. Vincristine revisited. Crit. Rev. Oncol. Hematol. 1999, 29, 267–287. [Google Scholar] [CrossRef]
- Frost, B.M.; Lonnerholm, G.; Koopmans, P.; Abrahamsson, J.; Behrendtz, M.; Castor, A.; Forestier, E.; Uges, D.R.; de Graaf, S.S. Vincristine in childhood leukaemia: No pharmacokinetic rationale for dose reduction in adolescents. Acta Paediatr. 2003, 92, 551–557. [Google Scholar] [CrossRef]
- Kellie, S.J.; Koopmans, P.; Earl, J.; Nath, C.; Roebuck, D.; Uges, D.R.A.; De Graaf, S.S.N. Increasing the dosage of vincristine: A clinical and pharmacokinetic study of continuous-infusion vincristine in children with central nervous system tumors. Cancer 2004, 100, 2637–2643. [Google Scholar] [CrossRef]
- Pinkerton, C.R.; McDermott, B.; Philip, T.; Biron, P.; Ardiet, C.; Vandenberg, H.; Brunat-Mentigny, M. Continuous vincristine infusion as part of a high dose chemoradiotherapy regimen: Drug kinetics and toxicity. Cancer Chemother. Pharmacol. 1988, 22, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Groninger, E.; Meeuwsen-de Boer, T.; Koopmans, P.; Uges, D.; Sluiter, W.; Veerman, A.; Kamps, W.; de Graaf, S. Vincristine pharmacokinetics and response to vincristine monotherapy in an up-front window study of the Dutch Childhood Leukaemia Study Group (DCLSG). Eur. J. Cancer 2005, 41, 98–103. [Google Scholar] [CrossRef]
- Gidding, C.E.; Fock, J.M.; Begeer, J.H.; Koopmans, P.; Meeuwsen-de Boer, G.J.; Kamps, W.A.; Uges, D.R.A.; De Graaf, S.S.N. Vincristine disposition and neurotoxicity in children. In Proceedings of the Annual Meeting-American Society of Clinical Oncology, Los Angeles, CA, USA, 16–19 May 1998. Abstract N22-2068-ASCO 1998. 16-5-1998. [Google Scholar]
- van Schie, R.M.; Bruggemann, R.J.; Hoogerbrugge, P.M.; Te Loo, D.M. Effect of azole antifungal therapy on vincristine toxicity in childhood acute lymphoblastic leukaemia. J. Antimicrob. Chemother. 2011, 66, 1853–1856. [Google Scholar] [CrossRef]
- Moriyama, B.; Henning, S.A.; Leung, J.; Falade-Nwulia, O.; Jarosinski, P.; Penzak, S.R.; Walsh, T.J. Adverse interactions between antifungal azoles and vincristine: Review and analysis of cases. Mycoses 2012, 55, 290–297. [Google Scholar] [CrossRef]
- Nikanjam, M.; Sun, A.; Albers, M.; Mangalindin, K.; Song, E.; Vempaty, H.; Sam, D.; Capparelli, E.V. Vincristine-associated Neuropathy with Antifungal Usage: A Kaiser Northern California Experience. J. Pediatr. Hematol. 2018, 40, e273–e277. [Google Scholar] [CrossRef]
- Science, M.; Robinson, P.D.; MacDonald, T.; Rassekh, S.R.; Dupuis, L.L.; Sung, L. Guideline for primary antifungal prophylaxis for pediatric patients with cancer or hematopoietic stem cell transplant recipients. Pediatr. Blood Cancer 2014, 61, 393–400. [Google Scholar] [CrossRef]
- Bruggemann, R.J.; Alffenaar, J.W.; Blijlevens, N.M.; Billaud, E.M.; Kosterink, J.G.; Verweij, P.E.; Burger, D.M. Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents. Clin. Infect. Dis. 2009, 48, 1441–1458. [Google Scholar] [CrossRef]
- Chan, J.D. Pharmacokinetic drug interactions of vinca alkaloids: Summary of case reports. Pharmacotherapy 1998, 18, 1304–1307. [Google Scholar]
- Thummel, K.E.; Shen, D.D.; Podoll, T.D.; Kunze, K.L.; Trager, W.F.; Hartwell, P.S.; Raisys, V.A.; Marsh, C.L.; McVicar, J.P.; Barr, D.M.; et al. Use of midazolam as a human cytochrome P450 3A probe: I. In vitro-in vivo correlations in liver transplant patients. J. Pharmacol. Exp. Ther. 1994, 271, 549–556. [Google Scholar]
- Greenblatt, D.J.; Ehrenberg, B.L.; Culm, K.E.; Scavone, J.M.; Corbett, K.E.; Friedman, H.L.; Harmatz, J.S.; Shader, R.I. Kinetics and EEG effects of midazolam during and after 1-minute, 1-hour, and 3-hour intravenous infusions. J. Clin. Pharmacol. 2004, 44, 605–611. [Google Scholar] [CrossRef]
- Chang, T.K.; Weber, G.F.; Crespi, C.L.; Waxman, D.J. Differential activation of cyclophosphamide and ifosphamide by cytochromes P-450 2B and 3A in human liver microsomes. Cancer Res. 1993, 53, 5629–5637. [Google Scholar]
- Boddy, A.V.; Yule, S.M.; Wyllie, R.; Price, L.; Pearson, A.D.; Idle, J.R. Comparison of continuous infusion and bolus administration of ifosfamide in children. Eur. J. Cancer 1995, 31, 785–790. [Google Scholar] [CrossRef]
- Guilhaumou, R.; Solas, C.; Bourgarel-Rey, V.; Quaranta, S.; Rome, A.; Simon, N.; Lacarelle, B.; Andre, N. Impact of plasma and intracellular exposure and CYP3A4, CYP3A5, and ABCB1 genetic polymorphisms on vincristine-induced neurotoxicity. Cancer Chemother. Pharmacol. 2011, 68, 1633–1638. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, L.S.; Marais, L.; Tanner, L. Comparison of two chemotherapy-induced peripheral neuropathy measurement approaches in children. Support. Care Cancer 2014, 22, 359–366. [Google Scholar] [CrossRef] [PubMed]
- van Hasselt, J.G.; van Eijkelenburg, N.K.; Beijnen, J.H.; Schellens, J.H.; Huitema, A.D. Design of a drug-drug interaction study of vincristine with azole antifungals in pediatric cancer patients using clinical trial simulation. Pediatr. Blood Cancer 2014, 61, 2223–2229. [Google Scholar] [CrossRef] [PubMed]
- EORTC-58081-CLG Translational Research—Observational Study for Identification of New Possible Prognostic Factors and Future Therapeutic Targets in Children with Acute Lymphoblastic Leukaemia (ALL). Available online: https://www.eortc.org/research_field/clinical-detail/58081/ (accessed on 3 July 2020).
- EsPhALL: An Open-Label Study to Evaluate the Safety and Efficacy of IMATINIB with Chemotherapy in Pediatric Patients with Ph+/BCR-ABL+ Acute Lymphoblastic Leukemia (Ph+ALL). 2015. Available online: http://www.skion.nl (accessed on 3 July 2020).
- The EuroNet-PHL-C1 Protocol First International Inter-Group Study for Classical Hodgkin’s Lymphoma in Children and Adolescents. 2012. Available online: https://www.skion.nl (accessed on 3 July 2020).
- The EuroNet-PHL-C2 Protocol Second International Inter-Group Study for Classical Hodgkin’s Lymphoma in Children and Adolescents. Version 3.0. 2016. Available online: https://www.skion.nl (accessed on 3 July 2020).
- The EpSSG Protocol a Protocol for Non Metastatic Rhabdomyosarcoma. Version 1.3. 2012. Available online: https://www.skion.nl (accessed on 3 July 2020).
- SIOP Wilms: Chemotherapy Before and After Surgery in Treating Children with Wilm’s Tumor. 2001. Available online: https://www.skion.nl (accessed on 3 July 2020).
- ACNS0331: A Study Evaluating Limited Target Volume Boost Irradiation and Reduced Dose Craniospinal Radiotherapy (18.00 Gy) and Chemotherapy in Children with Newly Diagnosed Standard Risk Medulloblastoma: A Phase III Double Randomized Trial. 2004. Available online: https://www.skion.nl (accessed on 3 July 2020).
- ACNS0332: Efficacy of Carboplatin Administered Concomitantly with Radiation and Isotretinoin as a Pro-Apoptotic Agent in Other Than Average Risk Medulloblastoma/PNET Patients. 2007. Available online: https://www.skion.nl (accessed on 3 July 2020).
- SIOP LGG: Cooperative Multicenter Study for Children and Adolescents with Low Grade Glioma. 2004. Available online: https://www.skion.nl (accessed on 3 July 2020).
- Skolnik, J.M.; Zhang, A.Y.; Barrett, J.S.; Adamson, P.C. Approaches to clear residual chemotherapeutics from indwelling catheters in children with cancer. Ther. Drug Monit. 2010, 32, 741–748. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, N.C.I. Common Terminology Criteria for Adverse Events (CTCAE) version 4.03. 2010. Available online: https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf (accessed on 3 July 2020).
- Gilchrist, L.S.; Tanner, L. The pediatric-modified total neuropathy score: A reliable and valid measure of chemotherapy-induced peripheral neuropathy in children with non-CNS cancers. Suppor. Care Cancer 2013, 21, 847–856. [Google Scholar] [CrossRef]
- Damen, C.W.; Israels, T.; Caron, H.N.; Schellens, J.H.; Rosing, H.; Beijnen, J.H. Validated assay for the simultaneous quantification of total vincristine and actinomycin-D concentrations in human EDTA plasma and of vincristine concentrations in human plasma ultrafiltrate by high-performance liquid chromatography coupled with tandem mass spectrometry. Rapid Commun. Mass Spectrom. 2009, 23, 763–774. [Google Scholar] [CrossRef]
| Patient Characteristics | Pharmacokinetic Part of Trial | RCT Part of Trial | ||
|---|---|---|---|---|
| Total (n = 35) | Push Group (n = 20) | 1 h Group (n = 15) | Total Group (n = 90) | |
| Age in years, mean (SD) | 10.06 (5.6) | 10.30 (6.17) | 9.73 (4.85) | 9.17 (5.15) |
| Ancestry, n (%) | ||||
| Caucasian | 30 (86) | 17 (85) | 13 (87) | 73 (81) |
| Non-Caucasian | 5 (14) | 3 (15) | 2 (13) | 17 (19) |
| Sex, n (%) | 50 (56) | |||
| Male | 16 (45) | 9 (45) | 7 (47) | 50 (56) |
| Female | 19 (54) | 11 (55) | 8 (53) | 40 (44) |
| Diagnosis, n (%) | ||||
| ALL | 26 (74) | 12 (60) | 14 (93) | 58 (64) |
| Hodgkin | 6 (17) | 5 (25) | 1 (7) | 18 (20) |
| Medulloblastoma | 1 (3) | 1 (5) | 0 (0) | 2 (2) |
| LGG | 1 (3) | 1 (5) | 0 (0) | 2 (2) |
| Wilms | 1 (3) | 1 (5) | 0 (0) | 8 (9) |
| RMS | 0 (0) | 0 (0) | 0 (0) | 2 (2) |
| Pharmacokinetic Parameter | Base Model | Administration Type | ||
|---|---|---|---|---|
| Population Estimate | RSE (%) | Population Estimate | RSE (%) | |
| Cl (L/hr/m2) | 25.3 | 10.1 | 30.5 | 10.0 |
| V1 (L/m2) | 22.1 | 14.4 | 20.8 | 12.5 |
| IC-Cl (L/hr/m2) | 77.9 | 12.8 | 34.2 | 9.5 |
| beta on IC-CL (push) | 1.13 | 4.5 | ||
| V2 (L/m2) | 358.5 | 11.3 | 127.7 | 19.0 |
| beta on V2 (push) | 1.13 | 19.1 | ||
| Inter-Individual Variability | CV% | CV% | ||
| Cl (L/hr/m2) | 0.51 | 17.4 | 0.52 | 16.9 |
| V1 (L/m2) | 0.62 | 20.7 | 0.55 | 23.9 |
| IC-Cl (L/hr/m2) | 0.67 | 16.7 | 0.48 | 16.4 |
| V2 (L/m2) | 0.48 | 17.4 | 0.41 | 17.0 |
| Residual (CV%) | 0.46 | 4.4 | 0.45 | 4.3 |
| −2-Log-likelihood | 2212.5 | 2174.3 | ||
| Parameter | Total Group | 1 h Infusions | Push Injections | Comparison of Push Injections VS. Push 1 h Infusions | |||||
|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Beta (95% CI) * | 95% CI * | p-Value | |
| Plasma AUC (ng·hr)/mL | 39.78 | 31.91–49.47 | 44.04 | 35.52–57.17 | 38.60 | 30.54–43.66 | −2.13 | −7.97 to 3.71 | 0.46 |
| Peripheral AUC (ng·hr)/mL | 36.71 | 27.48–45.78 | 42.50 | 33.78–55.75 | 35.36 | 26.22–40.97 | −4.18 | −10.26 to 1.90 | 0.17 |
| Plasma Cmax ng/mL | 57.28 | 31.91–74.47 | 30.05 | 21.86–39.07 | 72.44 | 58.64–86.12 | 43.01 | 31.55 to 54.47 | <0.001 |
| Peripheral Cmax ng/mL | 2.87 | 2.24–4.37 | 4.81 | 3.15–6.94 | 2.57 | 1.77–2.92 | −1.79 | −2.63 to −0.94 | <0.001 |
| Total CTCAE Score | Total Ped-mTNS Score | VIPN CTCAE Score No/Yes * | VIPN Ped-mTNS Score No/Yes * | |||||
|---|---|---|---|---|---|---|---|---|
| Beta (95% CI) | p Value | Beta (95% CI) | p Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Cl(L/hr/m2) | 0.00 (−0.04 to 0.05) | 0.90 | 0.02 (−0.09 to 0.14) | 0.70 | 1.01 (0.96–1.06) | 0.74 | 1.05 (0.99–1.12) | 0.11 |
| V1 (L/m2) | −0.00 (−0.06 to 0.09) | 0.96 | −0.03 (−0.19 to 0.13) | 0.72 | 1.00 (0.89–1.11) | 0.93 | 0.98 (0.91–1.07) | 0.98 |
| IC-Cl (L/h/m2) | 0.01 (0.00–0.02) | 0.04 | 0.04 (0.01–0.07) | 0.004 | 1.02 (1.00–1.03) | 0.02 | 1.05 (1.02–1.09) | 0.001 |
| V2 (L/m2) | −0.00 (−0.00 to 0.00) | 0.88 | 0.01 (−0.00 to 0.02) | 0.20 | 1.00 (0.99–1.00) | 0.29 | 1.00 (1.00–1.01) | 0.81 |
| Plasma AUC (ng·h/mL) | −0.01 (−0.06 to 0.03) | 0.54 | −0.06 (−0.16 to 0.05) | 0.27 | 0.97 (0.93–1.02) | 0.21 | 0.95 (0.89–1.02) | 0.18 |
| Peripheral AUC (ng·h/mL) | −0.01 (−0.05 to 0.04) | 0.76 | −0.05 (−0.16 to 0.06) | 0.34 | 0.98 (0.93–1.03) | 0.40 | 0.97 (0.91–1.04) | 0.41 |
| Plasma Cmax (ng/mL) | −0.01 (−0.03 to 0.02) | 0.55 | 0.00 (−0.08 to 0.07) | 0.94 | 0.96 (0.92–1.00) | 0.05 | 0.99 (0.96–1.02) | 0.53 |
| Peripheral Cmax (ng/mL) | −0.00 (−0.36 to 0.35) | 0.99 | −0.31 (−1.27 to 0.65) | 0.52 | 0.97 (0.64–1.47) | 0.89 | 0.96 (0.61–1.49) | 0.85 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van de Velde, M.E.; Panetta, J.C.; Wilhelm, A.J.; van den Berg, M.H.; van der Sluis, I.M.; van den Bos, C.; Abbink, F.C.H.; van den Heuvel-Eibrink, M.M.; Segers, H.; Chantrain, C.; et al. Population Pharmacokinetics of Vincristine Related to Infusion Duration and Peripheral Neuropathy in Pediatric Oncology Patients. Cancers 2020, 12, 1789. https://doi.org/10.3390/cancers12071789
van de Velde ME, Panetta JC, Wilhelm AJ, van den Berg MH, van der Sluis IM, van den Bos C, Abbink FCH, van den Heuvel-Eibrink MM, Segers H, Chantrain C, et al. Population Pharmacokinetics of Vincristine Related to Infusion Duration and Peripheral Neuropathy in Pediatric Oncology Patients. Cancers. 2020; 12(7):1789. https://doi.org/10.3390/cancers12071789
Chicago/Turabian Stylevan de Velde, Mirjam Esther, John Carl. Panetta, Abraham J. Wilhelm, Marleen H. van den Berg, Inge M. van der Sluis, Cor van den Bos, Floor C.H. Abbink, Marry M. van den Heuvel-Eibrink, Heidi Segers, Christophe Chantrain, and et al. 2020. "Population Pharmacokinetics of Vincristine Related to Infusion Duration and Peripheral Neuropathy in Pediatric Oncology Patients" Cancers 12, no. 7: 1789. https://doi.org/10.3390/cancers12071789
APA Stylevan de Velde, M. E., Panetta, J. C., Wilhelm, A. J., van den Berg, M. H., van der Sluis, I. M., van den Bos, C., Abbink, F. C. H., van den Heuvel-Eibrink, M. M., Segers, H., Chantrain, C., van der Werff Ten Bosch, J., Willems, L., Evans, W. E., & Kaspers, G. L. (2020). Population Pharmacokinetics of Vincristine Related to Infusion Duration and Peripheral Neuropathy in Pediatric Oncology Patients. Cancers, 12(7), 1789. https://doi.org/10.3390/cancers12071789






