MicroRNA-199b Downregulation Confers Resistance to 5-Fluorouracil Treatment and Predicts Poor Outcome and Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer Patients
Abstract
1. Introduction
2. Experimental Section
2.1. Cell Cultures and Transfection
2.2. Patient Samples and Pathologic Response
2.3. Nucleic Acid Isolation
2.4. Quantification of miRNA Expression Levels
2.5. Cell Viability Assay
2.6. Analysis of Caspase Activation
2.7. Western Blot Analysis
2.8. Statistical Analysis
3. Results
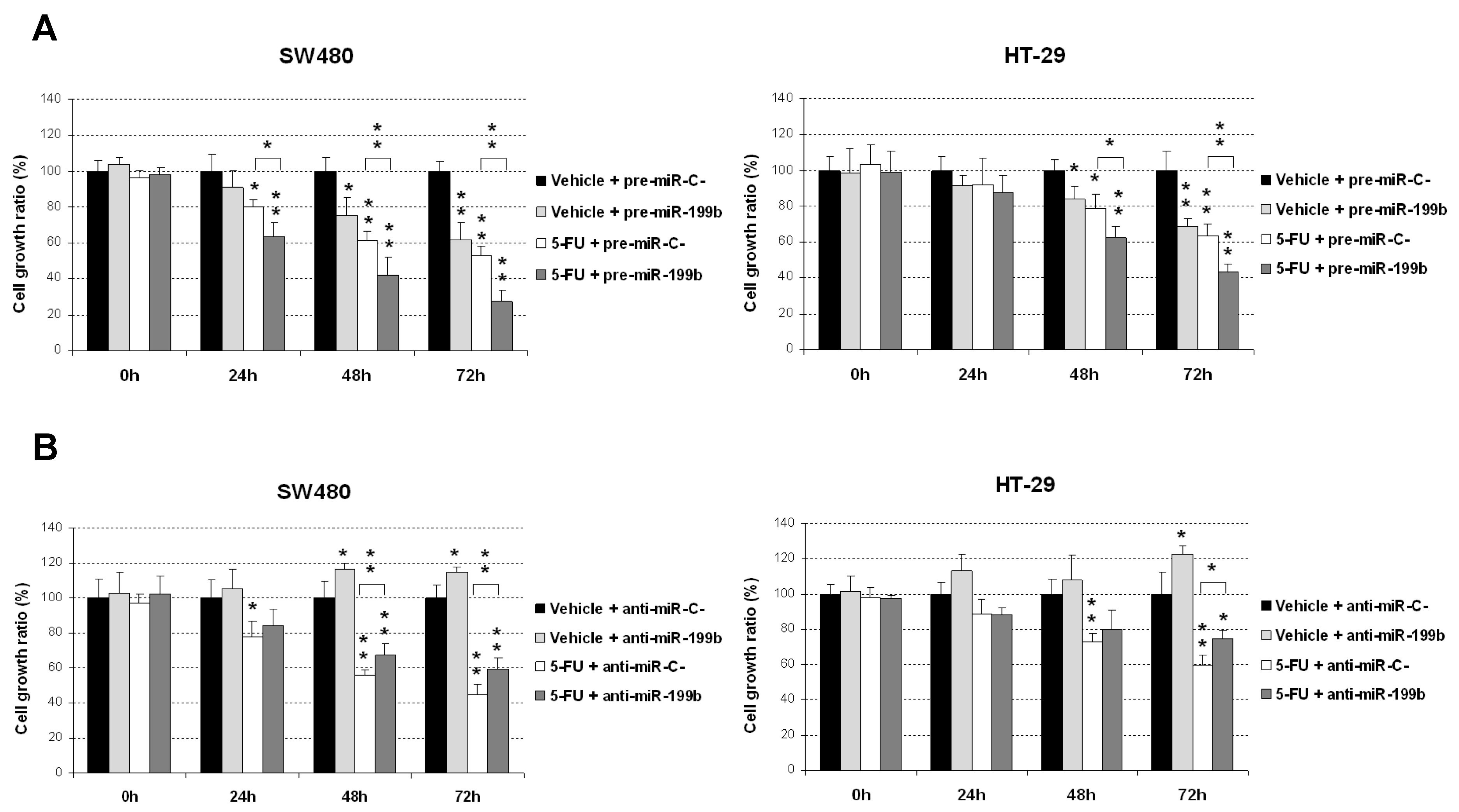
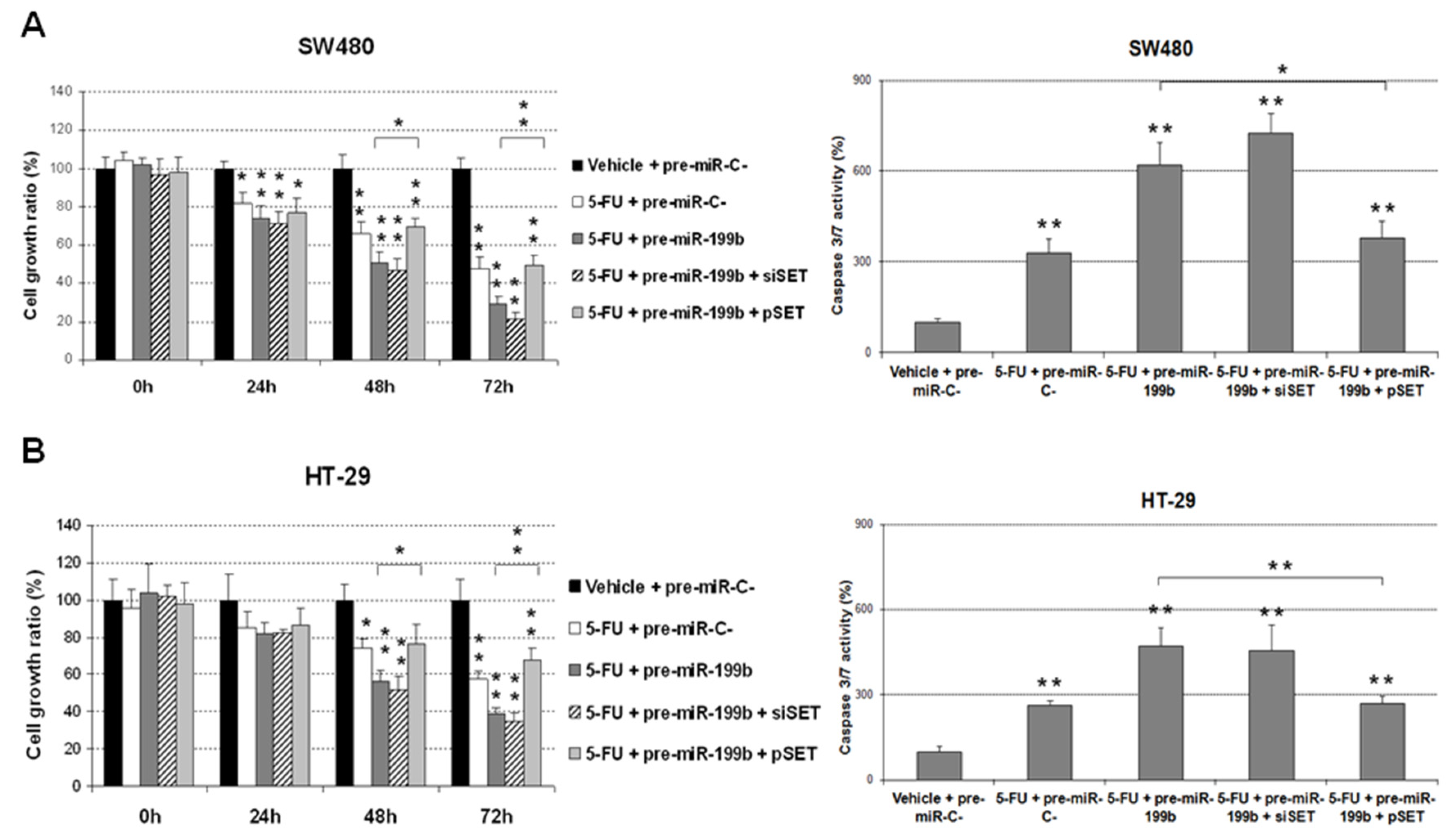
3.1. MiR-199b Sensitizes to 5-FU Treatment in a SET-Dependent Manner
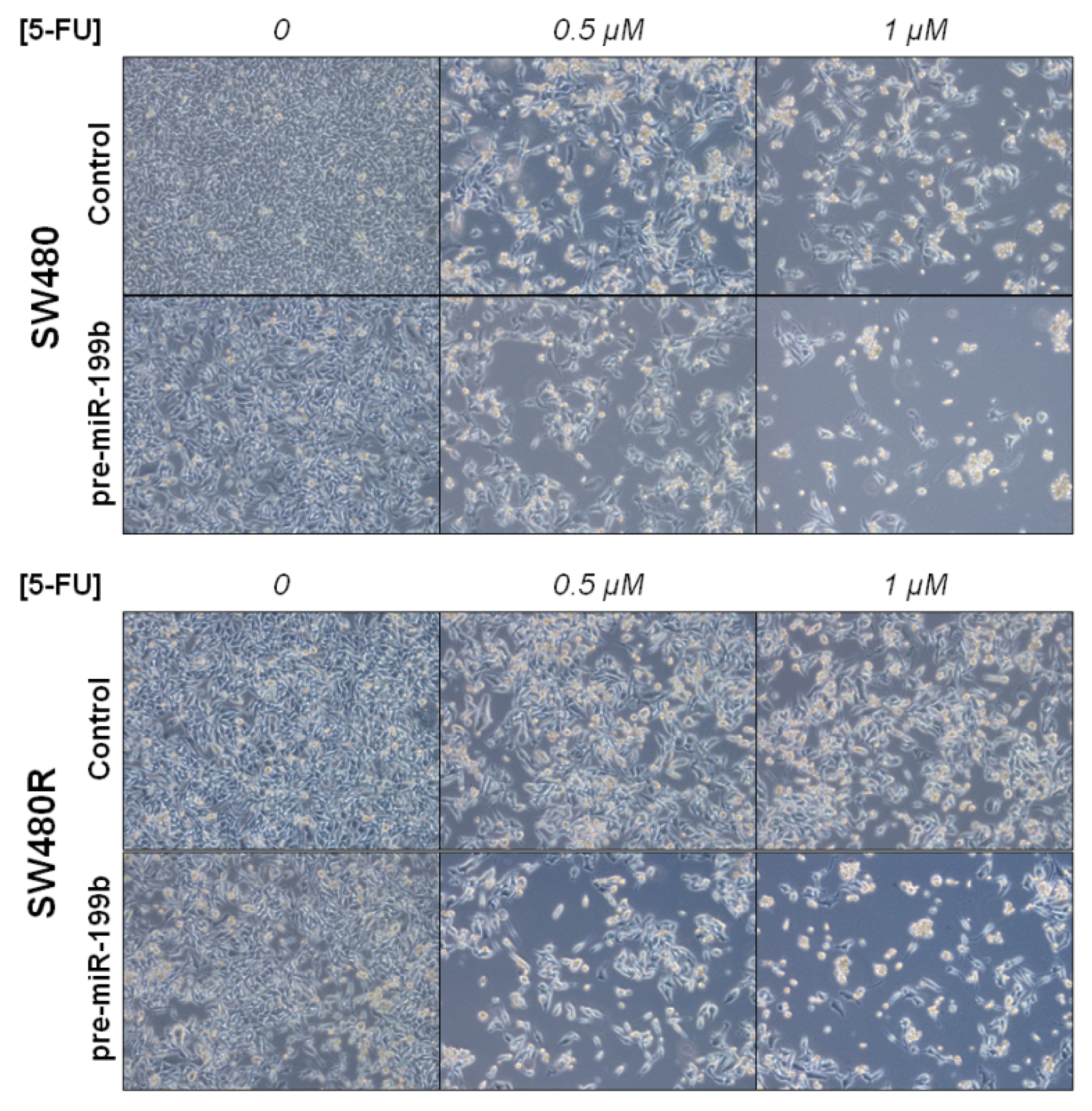
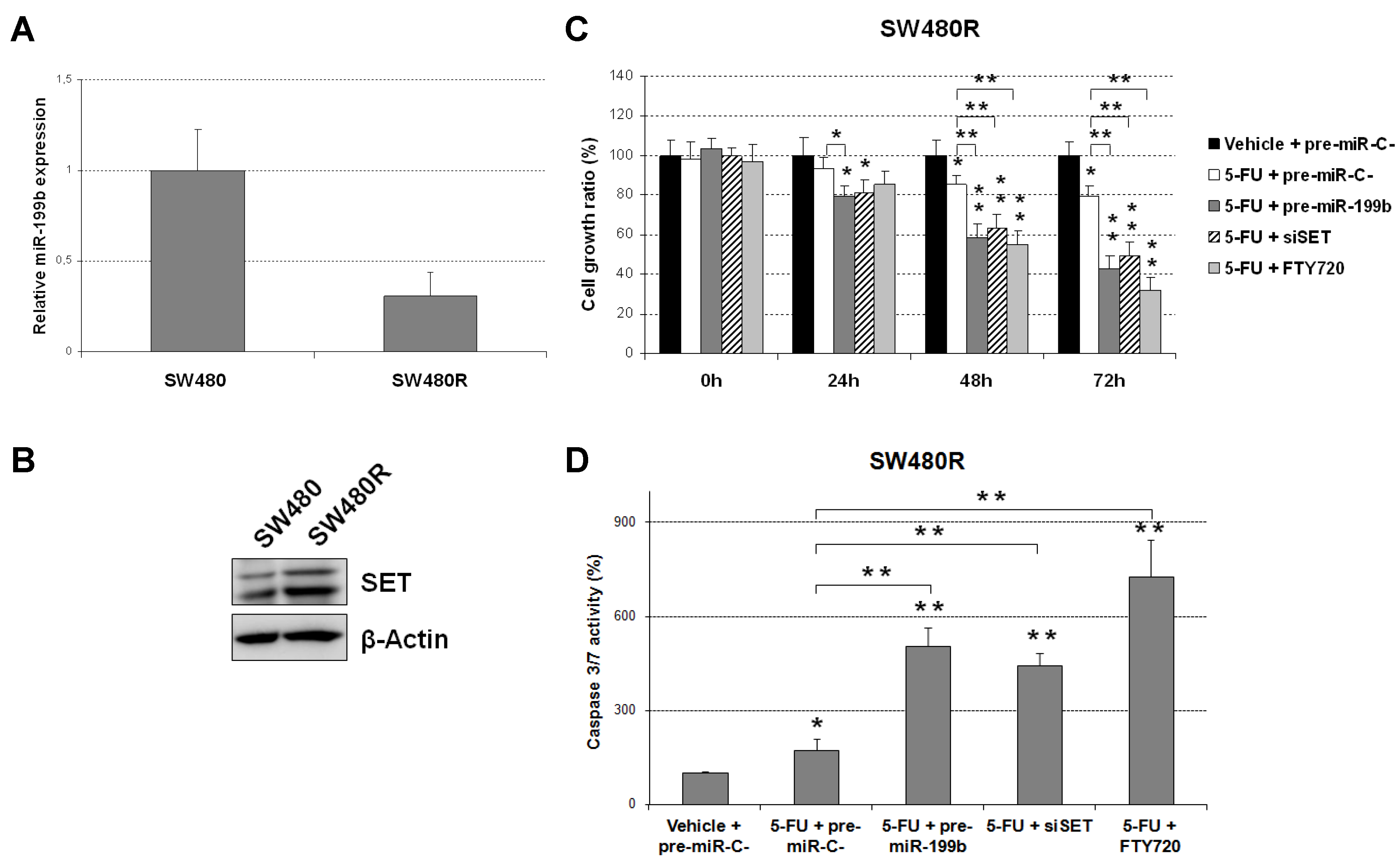
3.2. The miR-199b/SET Axis Emerges as a Novel Target to Overcome 5-FU Resistance
3.3. Prevalence of miR-199b Downregulation and Its Association with Molecular and Clinical Parameters
3.4. MiR-199b Predicts Pathological Response to Neoadjuvant CRT in Locally Advanced Rectal Cancer
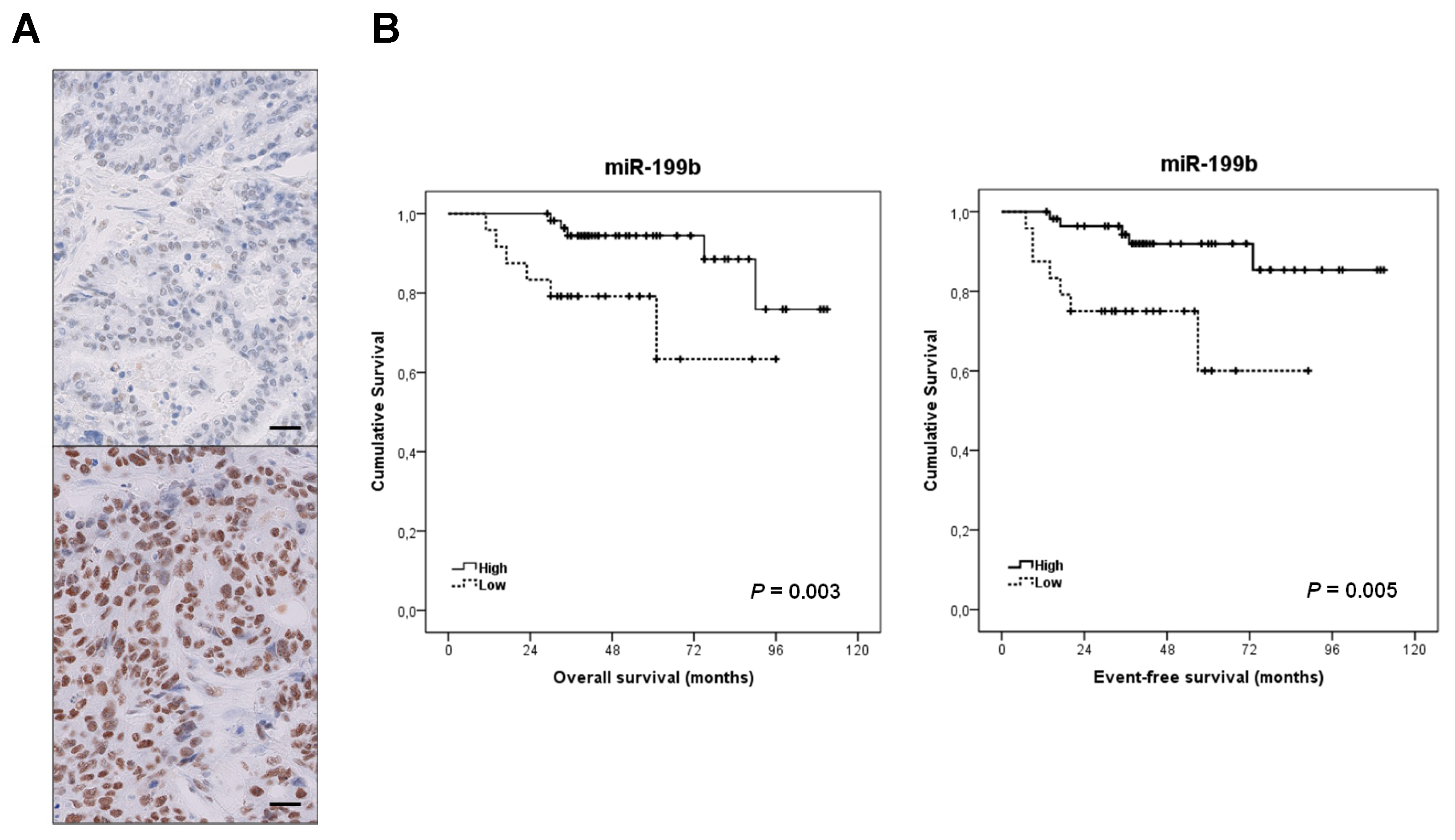
3.5. Clinical Significance of miR-199b Downregulation in Locally Advanced Rectal Cancer
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Kloor, M.; Pox, C.P. Colorectal cancer. Lancet 2014, 383, 1490–1502. [Google Scholar] [CrossRef]
- Sauer, D.M.R.; Becker, H.; Hohenberger, W.; Rödel, C.; Wittekind, C.; Fietkau, R.; Martus, P.; Tschmelitsch, J.; Hager, E.; Hess, C.F.; et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 2004, 351, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.H.; Harling, H.; Kirkeby, L.T.; Wille-Jørgensen, P.; Mocellin, S. Postoperative adjuvant chemotherapy in rectal cancer operated for cure. Cochrane Database Syst. Rev. 2012, 3, CD004078. [Google Scholar] [CrossRef] [PubMed]
- Hofheinz, R.-D.; Wenz, F.; Post, S.; Matzdorff, A.; Laechelt, S.; Hartmann, J.T.; Müller, L.; Link, H.; Moehler, M.; Kettner, E.; et al. Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: A randomised, multicentre, non-inferiority, phase 3 trial. Lancet Oncol. 2012, 13, 579–588. [Google Scholar] [CrossRef]
- Van Gijn, W.; Marijnen, C.A.; van de Velde, C.J. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12 years follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011, 12, 575–582. [Google Scholar] [CrossRef]
- Sauer, R.; Liersch, T.; Rodel, C. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: Results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J. Clin. Oncol. 2012, 30, 1926–1933. [Google Scholar] [CrossRef]
- Grass, F.; Mathis, K. Novelties in treatment of locally advanced rectal cancer. F1000Researach 2018, 7, 1868. [Google Scholar] [CrossRef]
- MacGregor, T.P.; Maughan, T.S.; Sharma, R.A. Pathological grading of regression following neoadjuvant chemoradiation therapy: The clinical need is now. J. Clin. Pathol. 2012, 65, 867–871. [Google Scholar] [CrossRef]
- Fokas, E.; Liersch, T.; Fietkau, R.; Hohenberger, W.; Beissbarth, T.; Hess, C.; Becker, H.; Ghadimi, M.; Mrak, K.; Merkel, S.; et al. Tumor regression grading after preoperative chemoradiotherapy for locally advanced rectal carcinoma revisited: Updated results of the CAO/ARO/AIO-94 trial. J. Clin. Oncol. 2014, 32, 1554–1562. [Google Scholar] [CrossRef]
- Bosset, J.F.; Collette, L.; Calais, G.; Mineur, L.; Maingon, P.; Radošević-Jelić, L.; Daban, A.; Bardet, E.; Beny, A.; Ollier, J.-C. Chemotherapy with preoperative radiotherapy in rectal cancer. N. Engl. J. Med. 2006, 355, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.K.; Baik, S.H.; Seong, J.S.; Kim, H.; Roh, J.K.; Lee, K.Y.; Sohn, S.K.; Cho, C.H. Oncologic outcomes after neoadjuvant chemoradiation followed by curative resection with tumor-specific mesorectal excision for fixed locally advanced rectal cancer. Ann. Surg. 2006, 244, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, F.; Bengala, C.; Losi, L.; Pagano, M.; Iachetta, F.; Dealis, C.; Jovic, G.; Depenni, R.; Zironi, S.; Falchi, A.M.; et al. Prognostic and predictive value of baseline and posttreatment molecular marker expression in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Kuremsky, J.G.; Tepper, J.E.; McLeod, H.L. Biomarkers for response to neoadjuvant chemoradiation for rectal cancer. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 673–688. [Google Scholar] [CrossRef] [PubMed]
- Casado, E.; García, V.M.; Sanchez, J.J.; Blanco, M.; Maurel, J.; Feliu, J.; Fernandez-Martos, C.; De Castro-Carpeño, J.; Castelo, B.; Iniesta, C.B.; et al. A combined strategy of SAGE and quantitative PCR provides a 13-gene signature that predicts preoperative chemoradiotherapy response and outcome in rectal cancer. Clin. Cancer Res. 2011, 17, 4145–4154. [Google Scholar] [CrossRef]
- Bottarelli, L.; De Angelis, G.L.; Azzoni, C.; Di Mario, F.; De’ Angelis, N.; Leandro, G.; Fornaroli, F.; Gaiani, F.; Negri, F. Potential predictive biomarkers in locally advanced rectal cancer treated with preoperative chemo-radiotherapy. Acta Biomed. 2018, 89, 102–106. [Google Scholar]
- Kong, Y.W.; Ferland-McCollough, D.; Jackson, T.; Bushell, M.D. MicroRNAs in cancer management. Lancet Oncol. 2012, 13, e249–e258. [Google Scholar] [CrossRef]
- Azizian, A.; Gruber, J.; Ghadimi, B.M.; Gaedcke, J. MicroRNA in rectal cancer. World J. Gastrointest. Oncol. 2016, 8, 416–426. [Google Scholar] [CrossRef]
- Machackova, T.; Prochazka, V.; Kala, Z.; Slaby, O. Translational Potential of MicroRNAs for Preoperative Staging and Prediction of Chemoradiotherapy Response in Rectal Cancer. Cancers 2019, 11, 1545. [Google Scholar] [CrossRef]
- Shen, Z.-L.; Wang, B.; Jiang, K.-W.; Ye, C.-X.; Cheng, C.; Yan, Y.-C.; Zhang, J.-Z.; Yang, Y.; Gao, Z.-D.; Ye, Y.-J.; et al. Downregulation of miR-199b is associated with distant metastasis in colorectal cancer via activation of SIRT1 and inhibition of CREB/KISS1 signaling. Oncotarget 2016, 7, 35092–35105. [Google Scholar] [CrossRef]
- Chen, L.-Y.; Zhi, Z.; Wang, L.; Zhao, Y.-Y.; Deng, M.; Liu, Y.-H.; Qin, Y.; Tian, M.-M.; Liu, Y.; Shen, T.; et al. NSD2 circular RNA promotes metastasis of colorectal cancer by targeting miR-199b-5p-mediated DDR1 and JAG1 signalling. J. Pathol. 2019, 248, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Makkinje, A.; Damuni, Z. The myeloid leukemia-associated protein SET is a potent inhibitor of protein phosphatase 2A. J. Biol. Chem. 1996, 271, 11059–11062. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.H.; Chen, K.F. Reprogramming the oncogenic response: SET protein as a potential therapeutic target in cancer. Expert Opin. Ther. Targets 2017, 21, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Cristóbal, I.; Caramés, C.; Rincón, R.; Manso, R.; Madoz-Gúrpide, J.; Torrejón, B.; González-Alonso, P.; Rojo, F.; García-Foncillas, J. Downregulation of microRNA-199b predicts unfavorable prognosis and emerges as a novel therapeutic target which contributes to PP2A inhibition in metastatic colorectal cancer. Oncotarget 2017, 8, 40169–40180. [Google Scholar] [CrossRef]
- Baek, D.W.; Kim, G.; Kang, B.W.; Kim, H.J.; Park, S.Y.; Park, J.S.; Choi, G.-S.; Kang, M.K.; Hur, K.; Kim, J.G. High expression of microRNA-199a-5p is associated with superior clinical outcomes in patients with locally advanced rectal cancer. J. Cancer Res. Clin. Oncol. 2020, 146, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Greenson, J.K.; Bonner, J.D.; Ben-Yzhak, O.; Cohen, H.I.; Miselevich, I.; Resnick, M.B.; Trougouboff, P.; Tomsho, L.D.; Kim, E.; Low, M.; et al. Phenotype of microsatellite unstable colorectal carcinomas: Well-differentiated and focally mucinous tumors and the absence of dirty necrosis correlate with microsatellite instability. Am. J. Surg. Pathol. 2003, 27, 563–570. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real—Time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- McShane, L.M.; Altman, D.G.; Sauerbrei, W.; Taube, S.E.; Gion, M.; Clarck, G.M. Reporting recommendations for tumor marker prognostic studies. J. Clin. Oncol. 2005, 23, 9067–9072. [Google Scholar] [CrossRef]
- Mumby, M. PP2A: Unveiling a reluctant tumor suppressor. Cell 2007, 130, 21–24. [Google Scholar] [CrossRef]
- Westermarck, J.; Hahn, W.C. Multiple pathways regulated by the tumor suppressor PP2A in transformation. Trends Mol. Med. 2008, 14, 152–160. [Google Scholar] [CrossRef]
- Cristobal, I.; Manso, R.; Rincón, R.; Caramés, C.; Senin, C.; Borrero, A.; Martinez-Useros, J.; Rodríguez, M.; Zazo, S.; Aguilera, O.; et al. PP2A inhibition is a common event in colorectal cancer and its restoration using FTY720 shows promising therapeutic potential. Mol. Cancer Ther. 2014, 13, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Carmen Figueroa-Aldariz, M.; Castañeda-Patlán, M.C.; Santoyo-Ramos, P.; Zentella, A.; Robles-Flores, M. Protein phosphatase 2A is essential to maintain active Wnt signaling and its Aβ tumor suppressor subunit is not expressed in colon cancer cells. Mol. Carcinog 2014, 54, 1430–1441. [Google Scholar] [CrossRef] [PubMed]
- Cristobal, I.; Rincón, R.; Manso, R.; Carames, C.; Zazo, S.; Madoz-Gurpide, J.; Rojo, F.; García-Foncillas, J. Deregulation of the PP2A inhibitor SET shows promising therapeutic implications and determines poor clinical outcome in patients with metastatic colorectal cancer. Clin. Cancer Res. 2015, 21, 347–356. [Google Scholar] [CrossRef]
- Tan, Y.J.; Lee, Y.T.; Petersen, S.H.; Kaur, G.; Kono, K.; Tan, S.C.; Majid, A.M.A.; Oon, C.E. BZD9L1 sirtuin inhibitor as a potential adjuvant for sensitization of colorectal cancer cells to 5-fluorouracil. Ther. Adv. Med. Oncol. 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Chen, Y.; Park, J.; Song, H.-C.; Chen, Y.; Park, J.W.; Joe, Y.; Chung, H.T. CO ameliorates endothelial senescence induced by 5-fluorouracil through SIRT1 activation. Arch. Biochem. Biophys. 2019, 677, 108185. [Google Scholar] [CrossRef] [PubMed]
- Cristóbal, I.; Garcia-Orti, L.; Cirauqui, C.; Cortes-Lavaud, X.; García-Sánchez, A.; Calasanz, M.J.; Odero, M.D. Overexpression of SET is a recurrent event associated with poor outcome and contributes to protein phosphatase 2A inhibition in acute myeloid leukemia. Haematologica 2012, 97, 543–550. [Google Scholar] [CrossRef]
- Agarwal, A.; MacKenzie, R.J.; Pippa, R.; Eide, C.A.; Oddo, J.; Tyner, J.W.; Sears, R.; Vitek, M.P.; Odero, M.D.; Christensen, D.J.; et al. Antagonism of SET using OP449 enhances the efficacy of tyrosine kinase inhibitors and overcomes drug resistance in myeloid leukemia. Clin. Cancer Res. 2014, 20, 2092–2103. [Google Scholar] [CrossRef]
- Cristóbal, I.; Madoz-Gúrpide, J.; Manso, R.; González-Alonso, P.; Rojo, F.; García-Foncillas, J. Potential anti-tumor effects of FTY720 associated with PP2A activation: A brief review. Curr. Med. Res. Opin. 2016, 32, 1137–1141. [Google Scholar] [CrossRef]
- Cristóbal, I.; Torrejón, B.; Rubio, J.; Santos, A.; Pedregal, M.; Caramés, C.; Zazo, S.; Luque, M.; Sanz-Alvarez, M.; Madoz-Gúrpide, J.; et al. Deregulation of SET is Associated with Tumor Progression and Predicts Adverse Outcome in Patients with Early-Stage Colorectal Cancer. J. Clin. Med. 2019, 8, 346. [Google Scholar] [CrossRef]
| Parameters | No. Cases | No. miR-199b High (%) | No. miR-199 Low (%) | p | ||
|---|---|---|---|---|---|---|
| MiR-199b | 82 | 58 | (70.7) | 24 | (29.3) | |
| Age | 82 | 58 | 24 | 0.407 | ||
| <70 | 42 | 28 | (48.3) | 14 | (58.3) | |
| ≥70 | 40 | 30 | (51.7) | 10 | (41.7) | |
| ECOG 1 | 82 | 58 | 24 | 0.370 | ||
| 0 | 52 | 35 | (60.3) | 17 | (70.8) | |
| 1–2 | 30 | 23 | (39.7) | 7 | (29.2) | |
| Clinical Stage Pre-CRT 2 | 82 | 58 | 24 | 0.638 | ||
| II | 5 | 4 | (6.9) | 1 | (4.2) | |
| III | 77 | 54 | (93.1) | 23 | (95.8) | |
| Grade Pre-CRT | 73 | 50 | 23 | 0.185 | ||
| Low | 21 | 12 | (24) | 9 | (39.1) | |
| Moderate-High | 52 | 38 | (76) | 14 | (60.9) | |
| ypT 3 | 82 | 58 | 24 | 0.143 | ||
| 0 | 11 | 10 | (17.2) | 1 | (4.2) | |
| 1 | 11 | 10 | (17.2) | 1 | (4.2) | |
| 2 | 26 | 16 | (27.6) | 10 | (41.6) | |
| 3 | 27 | 19 | (32.8) | 8 | (33.4) | |
| 4 | 4 | 2 | (3.4) | 2 | (8.3) | |
| x | 3 | 1 | (1.8) | 2 | (8.3) | |
| ypN 4 | 82 | 58 | 24 | 0.007 | ||
| N0 | 64 | 50 | (86.2) | 14 | (58.3) | |
| N1 | 14 | 5 | (8.6) | 9 | (37.5) | |
| N2 | 4 | 3 | (5.2) | 1 | (4.2) | |
| Pathological Stage | 82 | 58 | 24 | 0.029 | ||
| yp0 | 11 | 10 | (17.2) | 1 | (4.2) | |
| ypI | 32 | 25 | (43.1) | 7 | (29.2) | |
| ypII | 21 | 15 | (25.9) | 6 | (25) | |
| ypIII | 18 | 8 | (13.8) | 10 | (41.6) | |
| Responders vs. Nonresponders | ||||||
|---|---|---|---|---|---|---|
| MiR-199b Expression | No. Cases | MiR-199b Low (%) | MiR-199b High (%) | p | ||
| Response | 82 | 24 | 58 | 0.004 | ||
| Nonresponse 1 | 37 | 17 | (70.8) | 20 | (34.5) | |
| Response 2 | 45 | 7 | (29.2) | 38 | (65.5) | |
| Response 1 vs. Nonresponse 2 | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| OR 4 | 95% CI 3 | p | HR | 95% CI | p | |||
| Lower | Upper | Lower | Upper | |||||
| Age | 0.192 | 0.095 | ||||||
| <70 | 1.000 | 1.000 | ||||||
| ≥70 | 1.796 | 0.746 to 4.327 | 2.275 | 0.868 to 5.968 | ||||
| Gender | 0.193 | - | ||||||
| Male | 1.000 | |||||||
| Female | 0.549 | 0.222 to 1.354 | - | - | ||||
| Clinical Stage | 0.551 | - | ||||||
| II | 1.000 | |||||||
| III | 1.307 | 0.543 to 3.144 | - | - | ||||
| Grade Pre-CRT 5 | 0.605 | - | ||||||
| Low | 1.000 | |||||||
| Moderate-High | 1.185 | 0.623 to 2.252 | - | - | ||||
| ECOG 6 | 0.501 | - | ||||||
| 0 | 1.000 | |||||||
| 1–2 | 1.364 | 0.553 to 3.363 | - | - | ||||
| MiR-199b | 0.004 | 0.002 | ||||||
| High | 1.000 | 1.000 | ||||||
| Low | 4.614 | 1.642 to 11.969 | 5.332 | 1.813 to 13.679 | ||||
| Parameters | Univariate OS 1 Analysis | Multivariate OS Cox Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| HR 3 | 95% CI 2 | p | HR | 95% CI | p | |||
| Lower | Upper | Lower | Upper | |||||
| Age | 0.261 | 0.184 | ||||||
| <70 | 1.000 | 1.000 | ||||||
| ≥70 | 1.914 | 0.617 to 5.937 | 2.249 | 0.680 to 7.436 | ||||
| Pathological Stage | 0.206 | - | ||||||
| 0–I | 1.000 | |||||||
| II–III | 2.063 | 0.672 to 6.632 | - | - | ||||
| ypT 4 | 0.204 | - | ||||||
| 0–2 | 1.000 | |||||||
| 3–4 | 1.274 | 0.877 to 1.850 | - | - | ||||
| ypN 5 | 0.048 | 0.108 | ||||||
| N− | 1.000 | 1.000 | ||||||
| N+ | 3.336 | 1.011 to 11.005 | 2.243 | 0.861 to 4.544 | ||||
| ECOG 6 | 0.434 | - | ||||||
| 0 | 1.000 | |||||||
| 1–2 | 1.549 | 0.518 to 4.632 | - | - | ||||
| MiR-199b | 0.014 | 0.040 | ||||||
| High | 1.000 | 1.000 | ||||||
| Low | 4.036 | 1.328 to 12.261 | 3.478 | 1.059 to 11.425 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cristóbal, I.; Rubio, J.; Santos, A.; Torrejón, B.; Caramés, C.; Imedio, L.; Mariblanca, S.; Luque, M.; Sanz-Alvarez, M.; Zazo, S.; et al. MicroRNA-199b Downregulation Confers Resistance to 5-Fluorouracil Treatment and Predicts Poor Outcome and Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer Patients. Cancers 2020, 12, 1655. https://doi.org/10.3390/cancers12061655
Cristóbal I, Rubio J, Santos A, Torrejón B, Caramés C, Imedio L, Mariblanca S, Luque M, Sanz-Alvarez M, Zazo S, et al. MicroRNA-199b Downregulation Confers Resistance to 5-Fluorouracil Treatment and Predicts Poor Outcome and Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer Patients. Cancers. 2020; 12(6):1655. https://doi.org/10.3390/cancers12061655
Chicago/Turabian StyleCristóbal, Ion, Jaime Rubio, Andrea Santos, Blanca Torrejón, Cristina Caramés, Laura Imedio, Sofía Mariblanca, Melani Luque, Marta Sanz-Alvarez, Sandra Zazo, and et al. 2020. "MicroRNA-199b Downregulation Confers Resistance to 5-Fluorouracil Treatment and Predicts Poor Outcome and Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer Patients" Cancers 12, no. 6: 1655. https://doi.org/10.3390/cancers12061655
APA StyleCristóbal, I., Rubio, J., Santos, A., Torrejón, B., Caramés, C., Imedio, L., Mariblanca, S., Luque, M., Sanz-Alvarez, M., Zazo, S., Madoz-Gúrpide, J., Rojo, F., & García-Foncillas, J. (2020). MicroRNA-199b Downregulation Confers Resistance to 5-Fluorouracil Treatment and Predicts Poor Outcome and Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer Patients. Cancers, 12(6), 1655. https://doi.org/10.3390/cancers12061655






