Nuclear Receptor Binding Protein 2 Is Downregulated in Medulloblastoma, and Reduces Tumor Cell Survival upon Overexpression
Abstract
1. Introduction
2. Results
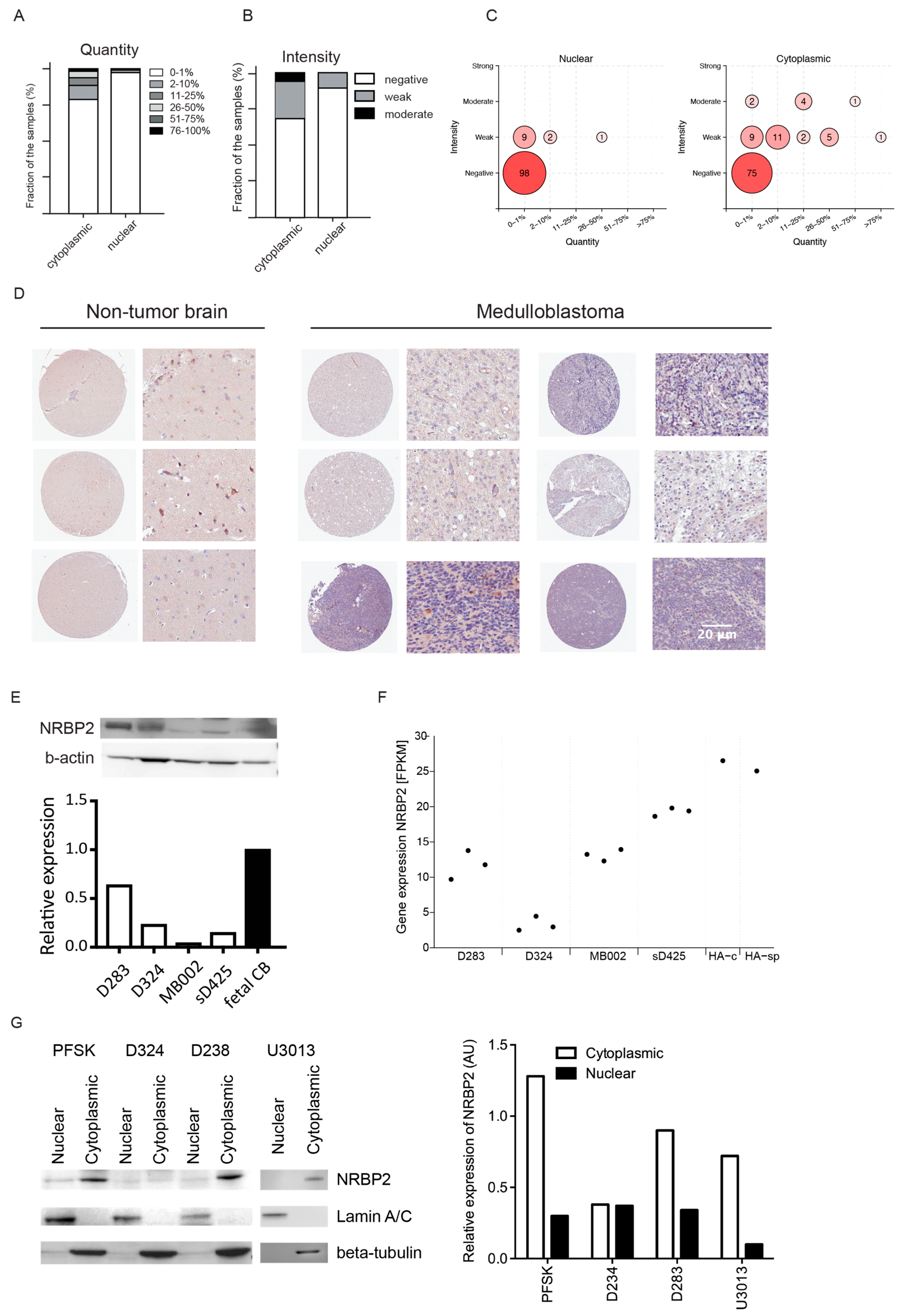
2.1. Low Level of NRBP2 Expression in Human Brain Tumors
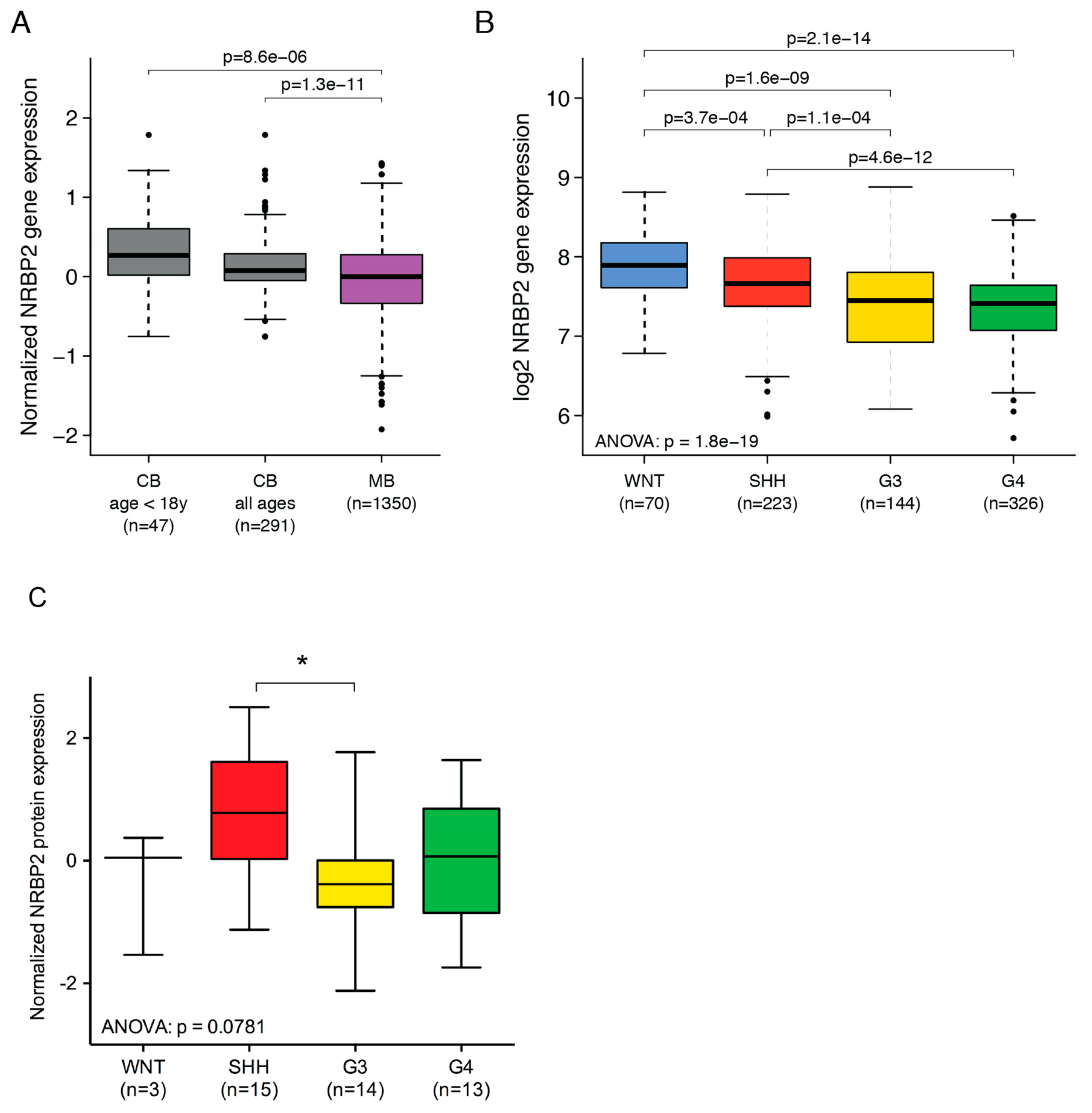
2.2. Cytoplasmic Localization of NRBP2 in Brain Tumor Cell Lines
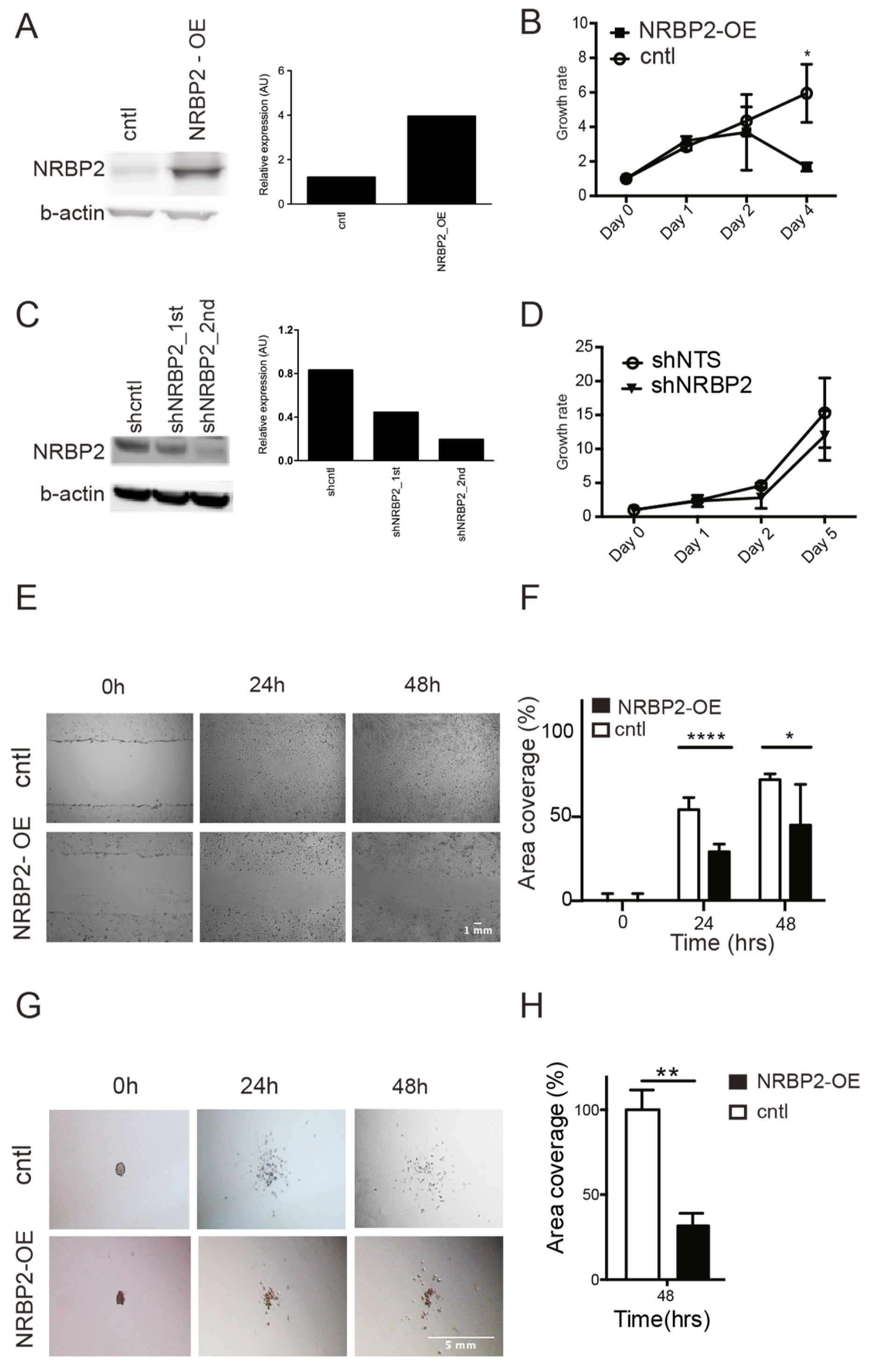
2.3. Reduced NRBP2 Expression in Medulloblastoma Patients Compared to Normal Cerebellum
2.4. NRBP2 Expression Is Repressed in Medulloblastoma Cell Lines by Epigenetic Factors
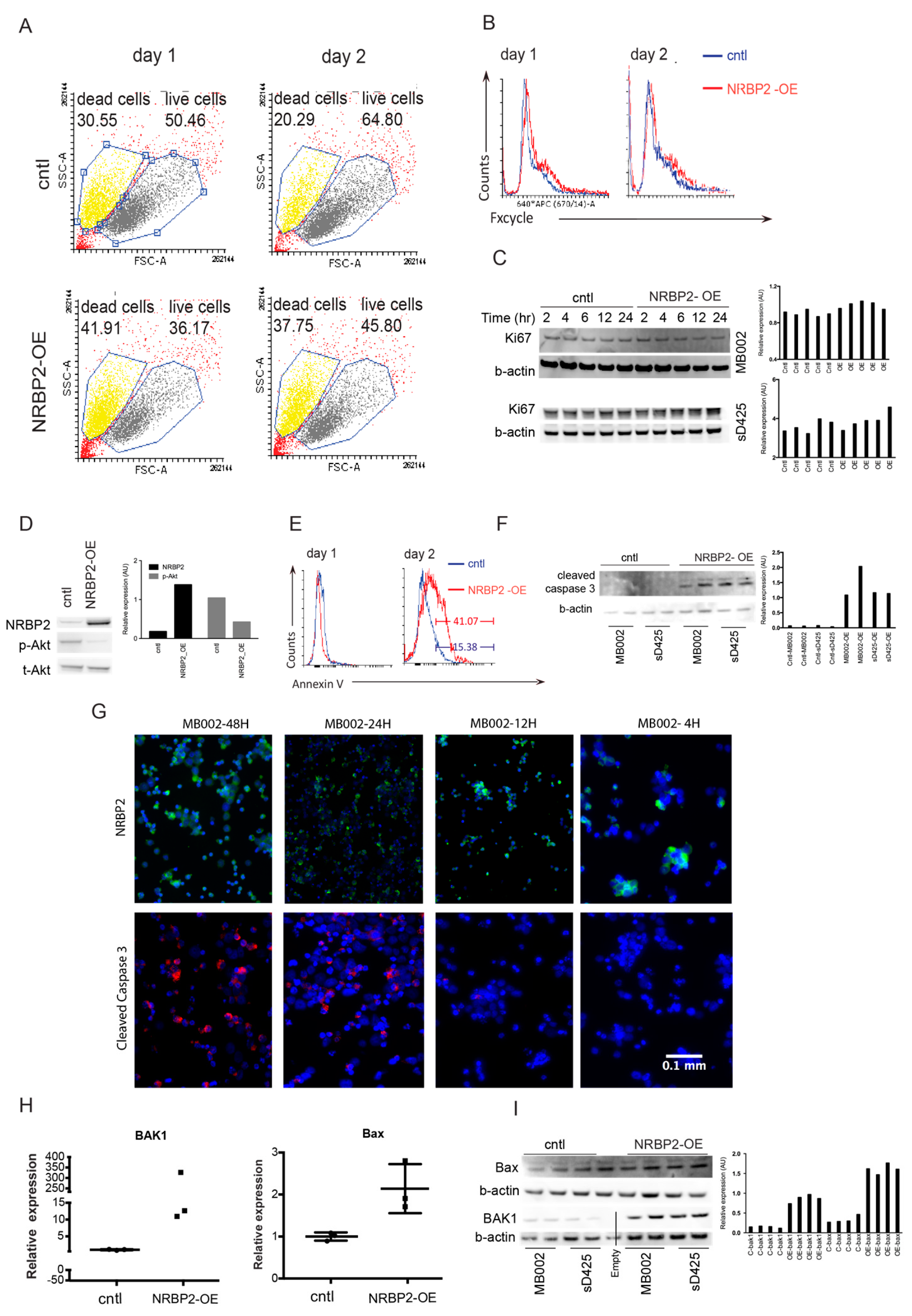
2.5. Overexpression of NRBP2 Leads to a Reduction in Cell Numbers, Impaired Migration, and Inhibits Invasion In Vitro
2.6. Overexpression of NRBP2 Causes Cell Death in Medulloblastoma Cells
3. Discussion
4. Materials and Methods
4.1. Tissue Microarrays and Analysis
4.2. Cell Culture
4.3. Subcellular Fractionation
4.4. Database Mining
4.5. Treatment with Epigenetic Modifier Drugs
4.6. siRNA Transfection
4.7. RT-qPCR
4.8. Plasmid Transfection
4.9. Lentivirus Transduction
4.10. Cell Growth Assay
4.11. Scratch Assay
4.12. Invasion Assay
4.13. Flow Cytometry
4.14. Western Blot
4.15. Cell Cytospin and Immunofluorescence
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pizer, B.L.; Clifford, S.C. The potential impact of tumour biology on improved clinical practice for medulloblastoma: Progress towards biologically driven clinical trials. Br. J. Neurosurg. 2009, 23, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.D.; Northcott, P.A.; Korshunov, A.; Remke, M.; Cho, Y.J.; Clifford, S.C.; Eberhart, C.G.; Parsons, D.W.; Rutkowski, S.; Gajjar, A.; et al. Molecular subgroups of medulloblastoma: The current consensus. Acta Neuropathol. 2012, 123, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Kool, M.; Korshunov, A.; Remke, M.; Jones, D.T.; Schlanstein, M.; Northcott, P.A.; Cho, Y.J.; Koster, J.; Schouten-van Meeteren, A.; van Vuurden, D.; et al. Molecular subgroups of medulloblastoma: An international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 2012, 123, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Vladoiu, M.C.; El-Hamamy, I.; Donovan, L.K.; Farooq, H.; Holgado, B.L.; Sundaravadanam, Y.; Ramaswamy, V.; Hendrikse, L.D.; Kumar, S.; Mack, S.C.; et al. Childhood cerebellar tumours mirror conserved fetal transcriptional programs. Nature 2019. [Google Scholar] [CrossRef] [PubMed]
- Swartling, F.J.; Bolin, S.; Phillips, J.J.; Persson, A.I. Signals that regulate the oncogenic fate of neural stem cells and progenitors. Exp. Neurol. 2014, 260, 56–68. [Google Scholar] [CrossRef]
- Demoulin, J.B.; Enarsson, M.; Larsson, J.; Essaghir, A.; Heldin, C.H.; Forsberg-Nilsson, K. The gene expression profile of PDGF-treated neural stem cells corresponds to partially differentiated neurons and glia. Growth Factors 2006, 24, 184–196. [Google Scholar] [CrossRef]
- Larsson, J.; Forsberg, M.; Brannvall, K.; Zhang, X.Q.; Enarsson, M.; Hedborg, F.; Forsberg-Nilsson, K. Nuclear receptor binding protein 2 is induced during neural progenitor differentiation and affects cell survival. Mol. Cell Neurosci. 2008, 39, 32–39. [Google Scholar] [CrossRef]
- Hooper, J.D.; Baker, E.; Ogbourne, S.M.; Sutherland, G.R.; Antalis, T.M. Cloning of the cDNA and localization of the gene encoding human NRBP, a ubiquitously expressed, multidomain putative adapter protein. Genomics 2000, 66, 113–118. [Google Scholar] [CrossRef]
- Reiterer, V.; Eyers, P.A.; Farhan, H. Day of the dead: Pseudokinases and pseudophosphatases in physiology and disease. Trends Cell Biol. 2014, 24, 489–505. [Google Scholar] [CrossRef]
- Wilson, C.H.; Crombie, C.; van der Weyden, L.; Poulogiannis, G.; Rust, A.G.; Pardo, M.; Gracia, T.; Yu, L.; Choudhary, J.; Poulin, G.B.; et al. Nuclear receptor binding protein 1 regulates intestinal progenitor cell homeostasis and tumour formation. EMBO J. 2012, 31, 2486–2497. [Google Scholar] [CrossRef]
- Zhang, L.; Ge, C.; Zhao, F.; Zhang, Y.; Wang, X.; Yao, M.; Li, J. NRBP2 Overexpression Increases the Chemosensitivity of Hepatocellular Carcinoma Cells via Akt Signaling. Cancer Res. 2016, 76, 7059–7071. [Google Scholar] [CrossRef] [PubMed]
- Weishaupt, H.; Johansson, P.; Sundstrom, A.; Lubovac-Pilav, Z.; Olsson, B.; Nelander, S.; Swartling, F.J. Batch-normalization of cerebellar and medulloblastoma gene expression datasets utilizing empirically defined negative control genes. Bioinformatics 2019, 35, 3357–3364. [Google Scholar] [CrossRef] [PubMed]
- Cavalli, F.M.G.; Remke, M.; Rampasek, L.; Peacock, J.; Shih, D.J.H.; Luu, B.; Garzia, L.; Torchia, J.; Nor, C.; Morrissy, A.S.; et al. Intertumoral Heterogeneity within Medulloblastoma Subgroups. Cancer Cell 2017, 31, 737–754. [Google Scholar] [CrossRef] [PubMed]
- Archer, T.C.; Ehrenberger, T.; Mundt, F.; Gold, M.P.; Krug, K.; Mah, C.K.; Mahoney, E.L.; Daniel, C.J.; LeNail, A.; Ramamoorthy, D.; et al. Proteomics, Post-translational Modifications, and Integrative Analyses Reveal Molecular Heterogeneity within Medulloblastoma Subgroups. Cancer Cell 2018, 34, 396–410. [Google Scholar] [CrossRef]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.E.; Sumer, S.O.; Aksoy, B.A.; Jacobsen, A.; Byrne, C.J.; Heuer, M.L.; Larsson, E.; et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012, 2, 401–404. [Google Scholar] [CrossRef]
- Gao, J.; Aksoy, B.A.; Dogrusoz, U.; Dresdner, G.; Gross, B.; Sumer, S.O.; Sun, Y.; Jacobsen, A.; Sinha, R.; Larsson, E.; et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013, 6, pl1. [Google Scholar] [CrossRef]
- Batora, N.V.; Sturm, D.; Jones, D.T.; Kool, M.; Pfister, S.M.; Northcott, P.A. Transitioning from genotypes to epigenotypes: Why the time has come for medulloblastoma epigenomics. Neuroscience 2014, 264, 171–185. [Google Scholar] [CrossRef]
- Hovestadt, V.; Jones, D.T.; Picelli, S.; Wang, W.; Kool, M.; Northcott, P.A.; Sultan, M.; Stachurski, K.; Ryzhova, M.; Warnatz, H.J.; et al. Decoding the regulatory landscape of medulloblastoma using DNA methylation sequencing. Nature 2014, 510, 537–541. [Google Scholar] [CrossRef]
- Bandopadhayay, P.; Bergthold, G.; Nguyen, B.; Schubert, S.; Gholamin, S.; Tang, Y.; Bolin, S.; Schumacher, S.E.; Zeid, R.; Masoud, S.; et al. BET bromodomain inhibition of MYC-amplified medulloblastoma. Clin. Cancer Res. 2014, 20, 912–925. [Google Scholar] [CrossRef]
- Ivanov, D.P.; Coyle, B.; Walker, D.A.; Grabowska, A.M. In vitro models of medulloblastoma: Choosing the right tool for the job. J. Biotechnol. 2016, 236, 10–25. [Google Scholar] [CrossRef]
- Jones, D.T.; Jager, N.; Kool, M.; Zichner, T.; Hutter, B.; Sultan, M.; Cho, Y.J.; Pugh, T.J.; Hovestadt, V.; Stutz, A.M.; et al. Dissecting the genomic complexity underlying medulloblastoma. Nature 2012, 488, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Pugh, T.J.; Weeraratne, S.D.; Archer, T.C.; Pomeranz Krummel, D.A.; Auclair, D.; Bochicchio, J.; Carneiro, M.O.; Carter, S.L.; Cibulskis, K.; Erlich, R.L.; et al. Medulloblastoma exome sequencing uncovers subtype-specific somatic mutations. Nature 2012, 488, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Karagianni, P.; Wong, J. HDAC3: Taking the SMRT-N-CoRrect road to repression. Oncogene 2007, 26, 5439–5449. [Google Scholar] [CrossRef] [PubMed]
- Castelo-Branco, G.; Lilja, T.; Wallenborg, K.; Falcao, A.M.; Marques, S.C.; Gracias, A.; Solum, D.; Paap, R.; Walfridsson, J.; Teixeira, A.I.; et al. Neural stem cell differentiation is dictated by distinct actions of nuclear receptor corepressors and histone deacetylases. Stem. Cell Rep. 2014, 3, 502–515. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chu, M.; Wang, S.; Chan, D.; Qi, S.; Wu, M.; Zhou, Z.; Nishi, E.; Qin, J.; Wong, J. Identification and characterization of nardilysin as a novel dimethyl H3K4-binding protein involved in transcriptional regulation. J. Biol. Chem. 2012, 287, 10089–10098. [Google Scholar] [CrossRef]
- Vescovi, A.L.; Galli, R.; Reynolds, B.A. Brain tumour stem cells. Nat. Rev. Cancer 2006, 6, 425–436. [Google Scholar] [CrossRef]
- Bergstrom, T.; Forsberg-Nilsson, K. Neural stem cells: Brain building blocks and beyond. Ups. J. Med. Sci. 2012, 117, 132–142. [Google Scholar] [CrossRef]
- Swartling, F.J. Myc proteins in brain tumor development and maintenance. Ups. J. Med. Sci. 2012, 117, 122–131. [Google Scholar] [CrossRef]
- Dietzmann, K.; Kirches, E.; von, B.; Jachau, K.; Mawrin, C. Increased human polo-like kinase-1 expression in gliomas. J. Neurooncol. 2001, 53, 1–11. [Google Scholar] [CrossRef]
- Neben, K.; Korshunov, A.; Benner, A.; Wrobel, G.; Hahn, M.; Kokocinski, F.; Golanov, A.; Joos, S.; Lichter, P. Microarray-based screening for molecular markers in medulloblastoma revealed STK15 as independent predictor for survival. Cancer Res. 2004, 64, 3103–3111. [Google Scholar] [CrossRef]
- Bulstrode, H.; Johnstone, E.; Marques-Torrejon, M.A.; Ferguson, K.M.; Bressan, R.B.; Blin, C.; Grant, V.; Gogolok, S.; Gangoso, E.; Gagrica, S.; et al. Elevated FOXG1 and SOX2 in glioblastoma enforces neural stem cell identity through transcriptional control of cell cycle and epigenetic regulators. Genes Dev. 2017, 31, 757–773. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Yang, Z.; Huang, J.; Chen, H.; Xiang, J.; Li, S.; Chen, C.; He, X.; Lin, F.; Yang, Z.; et al. Nuclear receptor binding protein 1 correlates with better prognosis and induces caspase-dependent intrinsic apoptosis through the JNK signalling pathway in colorectal cancer. Cell Death Dis. 2018, 9, 436. [Google Scholar] [CrossRef] [PubMed]
- Menghi, F.; Jacques, T.S.; Barenco, M.; Schwalbe, E.C.; Clifford, S.C.; Hubank, M.; Ham, J. Genome-wide analysis of alternative splicing in medulloblastoma identifies splicing patterns characteristic of normal cerebellar development. Cancer Res. 2011, 71, 2045–2055. [Google Scholar] [CrossRef] [PubMed]
- Waterland, R.A.; Kellermayer, R.; Rached, M.T.; Tatevian, N.; Gomes, M.V.; Zhang, J.; Zhang, L.; Chakravarty, A.; Zhu, W.; Laritsky, E.; et al. Epigenomic profiling indicates a role for DNA methylation in early postnatal liver development. Hum. Mol. Genet. 2009, 18, 3026–3038. [Google Scholar] [CrossRef]
- Becher, O.J.; Wechsler-Reya, R.J. For pediatric glioma, leave no histone unturned. Science 2014, 346, 1458–1459. [Google Scholar] [CrossRef]
- Paavilainen, L.; Edvinsson, A.; Asplund, A.; Hober, S.; Kampf, C.; Ponten, F.; Wester, K. The impact of tissue fixatives on morphology and antibody-based protein profiling in tissues and cells. J. Histochem. Cytochem. 2010, 58, 237–246. [Google Scholar] [CrossRef]
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K.; Burger, P.C.; Jouvet, A.; Scheithauer, B.W.; Kleihues, P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007, 114, 97–109. [Google Scholar] [CrossRef]
- Spyrou, A.; Kundu, S.; Haseeb, L.; Yu, D.; Olofsson, T.; Dredge, K.; Hammond, E.; Barash, U.; Vlodavsky, I.; Forsberg-Nilsson, K. Inhibition of Heparanase in Pediatric Brain Tumor Cells Attenuates their Proliferation, Invasive Capacity, and In Vivo Tumor Growth. Mol. Cancer 2017, 16, 1705–1716. [Google Scholar] [CrossRef]
- Xie, Y.; Bergstrom, T.; Jiang, Y.; Johansson, P.; Marinescu, V.D.; Lindberg, N.; Segerman, A.; Wicher, G.; Niklasson, M.; Baskaran, S.; et al. The Human Glioblastoma Cell Culture Resource: Validated Cell Models Representing All Molecular Subtypes. EBioMedicine 2015, 2, 1351–1363. [Google Scholar] [CrossRef]
- Bolin, S.; Borgenvik, A.; Persson, C.U.; Sundstrom, A.; Qi, J.; Bradner, J.E.; Weiss, W.A.; Cho, Y.J.; Weishaupt, H.; Swartling, F.J. Combined BET bromodomain and CDK2 inhibition in MYC-driven medulloblastoma. Oncogene 2018, 37, 2850–2862. [Google Scholar] [CrossRef]
- Jin, C.; Yu, D.; Hillerdal, V.; Wallgren, A.; Karlsson-Parra, A.; Essand, M. Allogeneic lymphocyte-licensed DCs expand T cells with improved antitumor activity and resistance to oxidative stress and immunosuppressive factors. Mol. Methods Clin. Dev. 2014, 1, 14001. [Google Scholar] [CrossRef] [PubMed]

| NRBP2 | F 5′-GGCCTCATCAAGATCGGCTC-3′ |
| R 5′-GCAGGTTCCGAAGTTCCTCTC-3′ | |
| NcoR | F 5′-GGAAGACTACCATTACTGCAGCTAACT-3′ |
| R 5′-CATCCTTGTCCGAGGCAATT-3′ | |
| SMRT | F 5′-GGGTAAATATGACCAGTGGGAAGAG-3′ |
| R 3′-TGGCATTCAGAGGGTTAAAAGC-3′ | |
| BAX | F 5′-CCCGAGAGGTCTTTTTCCGAG-3′ |
| R 5′-CCAGCCCATGATGGTTCTGAT-3′ | |
| BAK1 | F 5′-GTTTTCCGCAGCTACGTTTTT-3′ |
| R 5′-GCAGAGGTAAGGTGACCATCTC-3′ | |
| b-actin | F 5′-CTAAGGCCAACCGTGAAAAG-3′ |
| R 5′-ACCAGAGGCATACAGGGACA-3′ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiong, A.; Roy, A.; Spyrou, A.; Weishaupt, H.; Marinescu, V.D.; Olofsson, T.; Hermanson, O.; Swartling, F.J.; Forsberg-Nilsson, K. Nuclear Receptor Binding Protein 2 Is Downregulated in Medulloblastoma, and Reduces Tumor Cell Survival upon Overexpression. Cancers 2020, 12, 1483. https://doi.org/10.3390/cancers12061483
Xiong A, Roy A, Spyrou A, Weishaupt H, Marinescu VD, Olofsson T, Hermanson O, Swartling FJ, Forsberg-Nilsson K. Nuclear Receptor Binding Protein 2 Is Downregulated in Medulloblastoma, and Reduces Tumor Cell Survival upon Overexpression. Cancers. 2020; 12(6):1483. https://doi.org/10.3390/cancers12061483
Chicago/Turabian StyleXiong, Anqi, Ananya Roy, Argyris Spyrou, Holger Weishaupt, Voichita D. Marinescu, Tommie Olofsson, Ola Hermanson, Fredrik J. Swartling, and Karin Forsberg-Nilsson. 2020. "Nuclear Receptor Binding Protein 2 Is Downregulated in Medulloblastoma, and Reduces Tumor Cell Survival upon Overexpression" Cancers 12, no. 6: 1483. https://doi.org/10.3390/cancers12061483
APA StyleXiong, A., Roy, A., Spyrou, A., Weishaupt, H., Marinescu, V. D., Olofsson, T., Hermanson, O., Swartling, F. J., & Forsberg-Nilsson, K. (2020). Nuclear Receptor Binding Protein 2 Is Downregulated in Medulloblastoma, and Reduces Tumor Cell Survival upon Overexpression. Cancers, 12(6), 1483. https://doi.org/10.3390/cancers12061483





