A 30-Year Long-Term Experience in Appendix Neuroendocrine Neoplasms—Granting a Positive Outcome
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Immunohistochemistry
4.3. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Connor, S.J.; Hanna, G.B.; Frizelle, F.A. Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7970 appendectomies. Dis. Colon Rectum 1998, 41, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Moertel, C.G.; Dockerty, M.B.; Judd, E.S. Carcinoid tumors of the vermiform appendix. Cancer 1968, 21, 270–278. [Google Scholar] [CrossRef]
- Modlin, I.M.; Lye, K.D.; Kidd, M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003, 97, 934–959. [Google Scholar] [CrossRef]
- Landry, C.S.; Woodall, C.; Scoggins, C.R.; McMasters, K.M.; Martin, R.C., 2nd. Analysis of 900 appendiceal carcinoid tumors for a proposed predictive staging system. Arch. Surg. 2008, 143, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Pape, U.F.; Niederle, B.; Costa, F.; Gross, D.; Kelestimur, F.; Kianmanesh, R.; Knigge, U.; Oberg, K.; Pavel, M.; Perren, A.; et al. ENETS Consensus Guidelines for Neuroendocrine Neoplasms of the Appendix (Excluding Goblet Cell Carcinomas). Neuroendocrinology 2016, 103, 144–152. [Google Scholar] [CrossRef]
- Yao, J.C.; Hassan, M.; Phan, A.; Dagohoy, C.; Leary, C.; Mares, J.E.; Abdalla, E.K.; Fleming, J.B.; Vauthey, J.N.; Rashid, A.; et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008, 26, 3063–3072. [Google Scholar] [CrossRef]
- Clift, A.K.; Frilling, A. Neuroendocrine, goblet cell and mixed adeno-neuroendocrine tumours of the appendix: Updates, clinical applications and the future. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 237–247. [Google Scholar] [CrossRef]
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef]
- Goede, A.C.; Caplin, M.E.; Winslet, M.C. Carcinoid tumour of the appendix. Br. J. Surg. 2003, 90, 1317–1322. [Google Scholar] [CrossRef]
- Modlin, I.M.; Kidd, M.; Latich, I.; Zikusoka, M.N.; Shapiro, M.D. Current status of gastrointestinal carcinoids. Gastroenterology 2005, 128, 1717–1751. [Google Scholar] [CrossRef]
- Niederle, M.B.; Niederle, B. Diagnosis and treatment of gastroenteropancreatic neuroendocrine tumors: Current data on a prospectively collected, retrospectively analyzed clinical multicenter investigation. Oncologist 2011, 16, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Pape, U.F.; Perren, A.; Niederle, B.; Gross, D.; Gress, T.; Costa, F.; Arnold, R.; Denecke, T.; Plockinger, U.; Salazar, R.; et al. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology 2012, 95, 135–156. [Google Scholar] [CrossRef]
- McCusker, M.E.; Cote, T.R.; Clegg, L.X.; Sobin, L.H. Primary malignant neoplasms of the appendix: A population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer 2002, 94, 3307–3312. [Google Scholar] [CrossRef]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; the WHO Classification of Tumours Editorial Board; et al. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.H.; Shia, J.; Soslow, R.A.; Dhall, D.; Wong, W.D.; O’Reilly, E.; Qin, J.; Paty, P.; Weiser, M.R.; Guillem, J.; et al. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am. J. Surg. Pathol. 2008, 32, 1429–1443. [Google Scholar] [CrossRef]
- Kanthan, R.; Saxena, A.; Kanthan, S.C. Goblet cell carcinoids of the appendix: Immunophenotype and ultrastructural study. Arch. Pathol. Lab. Med. 2001, 125, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Edge, S.B. AJCC Cancer Staging Manual, Eighth Edition Manual; Springer: New York, NY, USA, 2017. [Google Scholar]
- National Comprehensive Cancer Network (NCCN). Neuroendocrine and Adrenal Tumors (Version 1.2019); Harborside Press: New York, NY, USA, 2019. [Google Scholar]
- Singh, H.; Koomson, A.S.; Decker, K.M.; Park, J.; Demers, A.A. Continued increasing incidence of malignant appendiceal tumors in Canada and the United States: A population-based study. Cancer 2020, 126, 2206–2216. [Google Scholar] [CrossRef]
- Addiss, D.G.; Shaffer, N.; Fowler, B.S.; Tauxe, R.V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 1990, 132, 910–925. [Google Scholar] [CrossRef]
- Kraemer, M.; Franke, C.; Ohmann, C.; Yang, Q.; Acute Abdominal Pain Study, G. Acute appendicitis in late adulthood: Incidence, presentation, and outcome. Results of a prospective multicenter acute abdominal pain study and a review of the literature. Langenbecks Arch. Surg. 2000, 385, 470–481. [Google Scholar] [CrossRef]
- Pahlavan, P.S.; Kanthan, R. Goblet cell carcinoid of the appendix. World J. Surg. Oncol. 2005, 3, 36. [Google Scholar] [CrossRef]
- Daskalakis, K.; Alexandraki, K.; Kassi, E.; Tsoli, M.; Angelousi, A.; Ragkousi, A.; Kaltsas, G. The risk of lymph node metastases and their impact on survival in patients with appendiceal neuroendocrine neoplasms: A systematic review and meta-analysis of adult and paediatric patients. Endocrine 2020, 67, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Brighi, N.; La Rosa, S.; Rossi, G.; Grillo, F.; Pusceddu, S.; Rinzivillo, M.; Spada, F.; Tafuto, S.; Massironi, S.; Faggiano, A.; et al. Morphological Factors Related to Nodal Metastases in Neuroendocrine Tumors of the Appendix: A Multicentric Retrospective Study. Ann. Surg. 2020, 271, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Crown, A.; Simianu, V.V.; Kennecke, H.; Lopez-Aguiar, A.G.; Dillhoff, M.; Beal, E.W.; Poultsides, G.A.; Makris, E.; Idrees, K.; Smith, P.M.; et al. Appendiceal Neuroendocrine Tumors: Does Colon Resection Improve Outcomes? J. Gastrointest. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Mirzayans, R.; Andrais, B.; Scott, A.; Paterson, M.C.; Murray, D. Single-cell analysis of p16(INK4a) and p21(WAF1) expression suggests distinct mechanisms of senescence in normal human and Li-Fraumeni Syndrome fibroblasts. J. Cell. Physiol. 2010, 223, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Morisaki, H.; Ando, A.; Nagata, Y.; Pereira-Smith, O.; Smith, J.R.; Ikeda, K.; Nakanishi, M. Complex mechanisms underlying impaired activation of Cdk4 and Cdk2 in replicative senescence: Roles of p16, p21, and cyclin D1. Exp. Cell Res. 1999, 253, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Stein, G.H.; Drullinger, L.F.; Soulard, A.; Dulic, V. Differential roles for cyclin-dependent kinase inhibitors p21 and p16 in the mechanisms of senescence and differentiation in human fibroblasts. Mol. Cell. Biol. 1999, 19, 2109–2117. [Google Scholar] [CrossRef]
- Afonso, J.; Longatto-Filho, A.; Martinho, O.; Lobo, F.; Amaro, T.; Reis, R.M.; Santos, L.L. Low RKIP expression associates with poor prognosis in bladder cancer patients. Virchows Arch. 2013, 462, 445–453. [Google Scholar] [CrossRef]
- Martinho, O.; Campos, M.; Ribeiro, G.; Penna, V.; Curcelli, E.C.; Olivieri, M.V.; Morini, S.; Scapulatempo, C.; Abrahao-Machado, L.F.; Reis, R.M. Raf Kinase Inhibitor Protein Expression and Prognostic Value in Soft Tissue Sarcomas. Pathobiology 2016, 83, 41–46. [Google Scholar] [CrossRef]
- Martinho, O.; Gouveia, A.; Silva, P.; Pimenta, A.; Reis, R.M.; Lopes, J.M. Loss of RKIP expression is associated with poor survival in GISTs. Virchows Arch. 2009, 455, 277–284. [Google Scholar] [CrossRef]
- Martinho, O.; Simoes, K.; Longatto-Filho, A.; Jacob, C.E.; Zilberstein, B.; Bresciani, C.; Gama-Rodrigues, J.; Cecconello, I.; Alves, V.; Reis, R.M. Absence of RKIP expression is an independent prognostic biomarker for gastric cancer patients. Oncol. Rep. 2013, 29, 690–696. [Google Scholar] [CrossRef]
- Raquel-Cunha, A.; Cardoso-Carneiro, D.; Reis, R.M.; Martinho, O. Current Status of Raf Kinase Inhibitor Protein (RKIP) in Lung Cancer: Behind RTK Signaling. Cells 2019, 8, 442. [Google Scholar] [CrossRef] [PubMed]
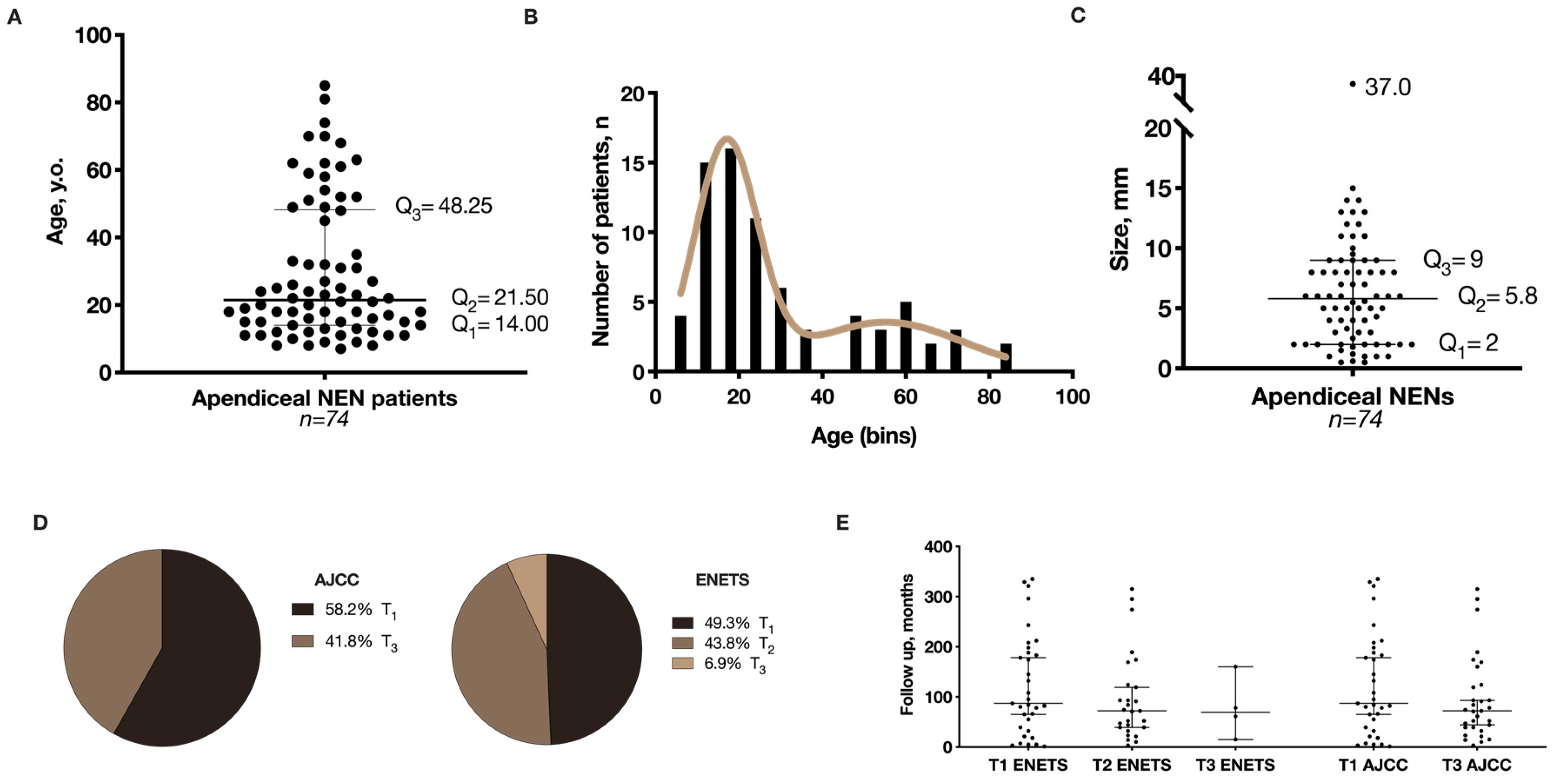
| Number of Appendectomies Performed | 16,936 |
| Number of Patients with Appendix NENs | 74 |
| Incidence of Appendix NENs in Appendectomies | 0.38% |
| Gender | |
| Male, n (%) | 27 (36.5) |
| Female, n (%) | 47 (63.5) |
| Age at diagnosis (median), years | 21.5 |
| <18, (median), years | 12.0 |
| ≥18, (median), years | 31.5 |
| Surgical procedure | |
| Appendicectomy, n | 62 |
| Appendicectomy + right-sided hemicolectomy, n | 3 |
| Colectomy, n | 8 |
| Annexectomy, n | 1 |
| Size | |
| Median, mm | 5.8 |
| Location of the tumor * | |
| Tip of the appendix, n (%) | 54 (76.1) |
| Mid-appendix, n (%) | 13 (18.3) |
| Base of the appendix, n (%) | 4 (5.6) |
| Histological pattern ** | |
| Insular, n (%) | 58 (82.8) |
| Trabecular / tubular, n (%) | 12 (17.2) |
| Tumor infiltration *** | |
| Submucosa | 16 (21.9) |
| Muscularis propria | 24 (32.9) |
| Subserosa or mesoappendix | 33 (45.2) |
| Lymphovascular invasion *** | |
| Yes | 9 (12.3) |
| No | 64 (87.7) |
| Perineural invasion *** | |
| Yes | 12 (16.4) |
| No | 61 (83.6) |
| Tumor necrosis *** | |
| Yes | 8 (11.0) |
| No | 65 (89.0) |
| Grading of the appendix NENs according to ENETS *** | |
| G1 | 70 (96.0) |
| G2 | 3 (4.0) |
| G3 | 0 (0.0) |
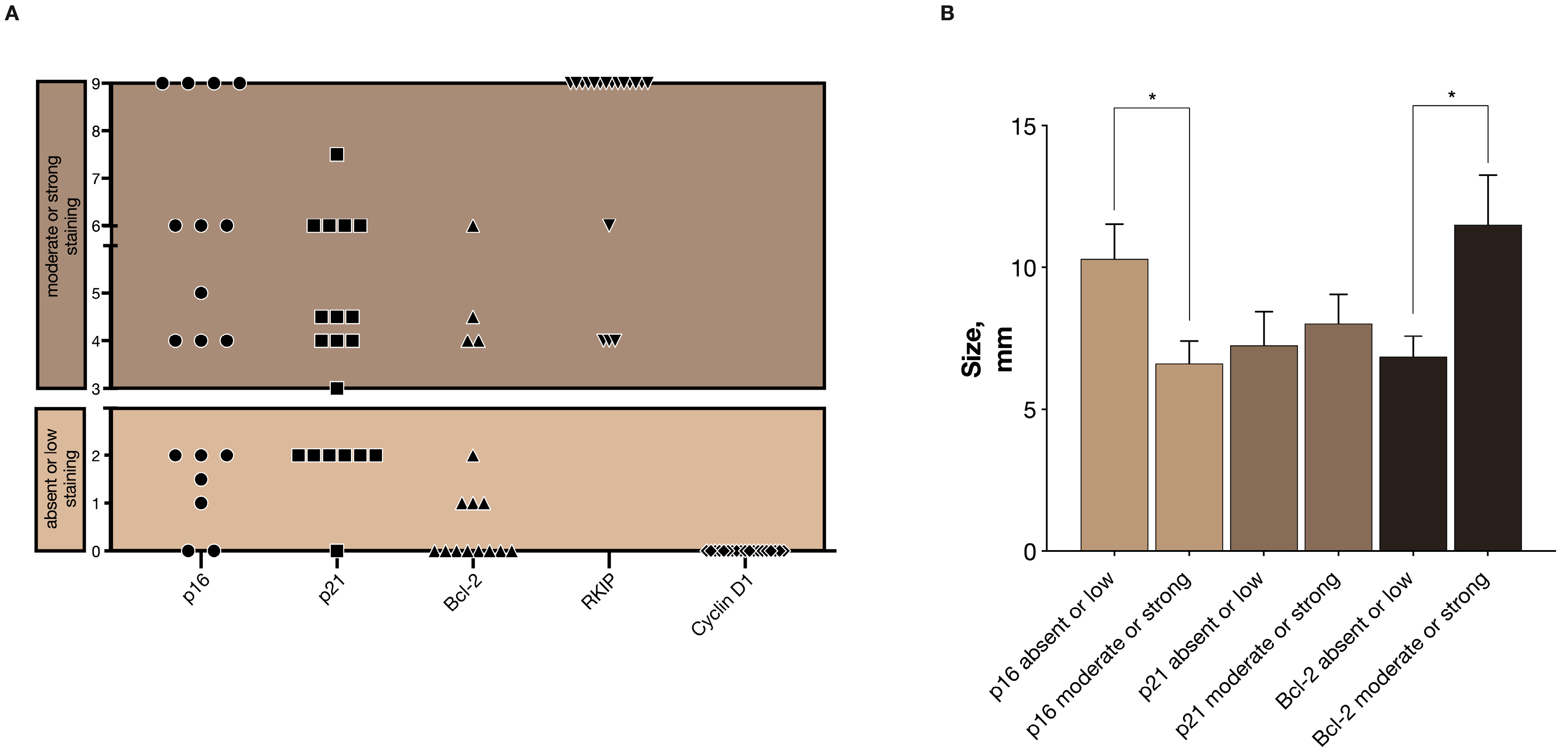
| Molecular Markers | Size (mean ± S.E.M.), mm | p-Value |
|---|---|---|
| p16 score (n) | ||
| Absent or low (4) | 10.29 ± 1.23 | 0.017 |
| Moderate or strong (10) | 6.62 ± 0.78 | |
| p21 score (n) | ||
| Absent or low (3) | 7.25 ± 1.18 | 0.661 |
| Moderate or strong (12) | 8.02 ± 1.04 | |
| Bcl-2 score (n) | ||
| Absent or low (7) | 6.86 ± 0.72 | 0.011 |
| Moderate or strong (3) | 11.50 ± 1.76 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vinagre, J.; Pinheiro, J.; Martinho, O.; Reis, R.M.; Preto, J.; Soares, P.; Lopes, J.M. A 30-Year Long-Term Experience in Appendix Neuroendocrine Neoplasms—Granting a Positive Outcome. Cancers 2020, 12, 1357. https://doi.org/10.3390/cancers12061357
Vinagre J, Pinheiro J, Martinho O, Reis RM, Preto J, Soares P, Lopes JM. A 30-Year Long-Term Experience in Appendix Neuroendocrine Neoplasms—Granting a Positive Outcome. Cancers. 2020; 12(6):1357. https://doi.org/10.3390/cancers12061357
Chicago/Turabian StyleVinagre, João, Jorge Pinheiro, Olga Martinho, Rui Manuel Reis, John Preto, Paula Soares, and José Manuel Lopes. 2020. "A 30-Year Long-Term Experience in Appendix Neuroendocrine Neoplasms—Granting a Positive Outcome" Cancers 12, no. 6: 1357. https://doi.org/10.3390/cancers12061357
APA StyleVinagre, J., Pinheiro, J., Martinho, O., Reis, R. M., Preto, J., Soares, P., & Lopes, J. M. (2020). A 30-Year Long-Term Experience in Appendix Neuroendocrine Neoplasms—Granting a Positive Outcome. Cancers, 12(6), 1357. https://doi.org/10.3390/cancers12061357









