PET-FDG: Impetus
Abstract
:1. Introduction
2. Impetus Criteria Description
- Diffuse bone marrow (BM) uptake:
- Deauville criteria:
- 1 No uptake at all
- 2 ≤ mediastinal blood pool uptake
- 3 >mediastinal blood pool uptake, ≤ liver uptake
- 4 > liver uptake +10%
- 5 >> liver uptake (twice)
- A^ appended if there is hypermetabolism in limbs and ribs [10]
- Focal bone lesions (F):
- Lesion number group (x):
- x = 1: no lesions
- x = 2: 1 to 3 lesions
- x = 3: 4 to 10 lesions
- x = 4: >10 lesions
- S: skull
- Sp: spine
- Extra Sp: all the rest
- Hottest focal bone lesion Deauville criteria (target lesion is the hottest area):
- 1 No uptake at all
- 2 ≤ mediastinal blood pool uptake
- 3 > mediastinal blood pool uptake, ≤ liver uptake
- 4 > liver uptake +10%
- 5 >> liver uptake (twice or more)
- Lytic lesions(L) at CT associated to PET:
- Lesion number group (x):
- x = 1: no lesions
- x = 2: 1 to 3 lesions
- x = 3: 4 to 10 lesions
- x = 4: >10 lesions
- Presence of at least one fracture on CT images (Fr)
- Presence of paramedullary disease (PM): a bone lesion involving surrounding soft tissues with bone cortical interruption
- Extramedullary disease (EM):
- Site
- Nodal disease (N) plus site:
- LC: laterocervical
- SC: supraclavicular
- M: mediastinal
- Ax: axillary
- Rp: retroperitoneal
- Mes: mesentery
- In: inguinal
- Extranodal disease (EN) plus site:
- Li: liver
- Mus: muscle
- Spl: spleen
- Sk: skin
- Oth: other
- Plus, Deauville criteria for target EM lesions (target lesion is the hottest area):
- 1 No uptake at all
- 2 ≤ mediastinal blood pool uptake (SUV max)
- 3 > mediastinal blood pool uptake, ≤ liver uptake
- 4 > liver uptake + 10%
- 5 >> liver uptake (twice or more).
3. Concordance Analysis
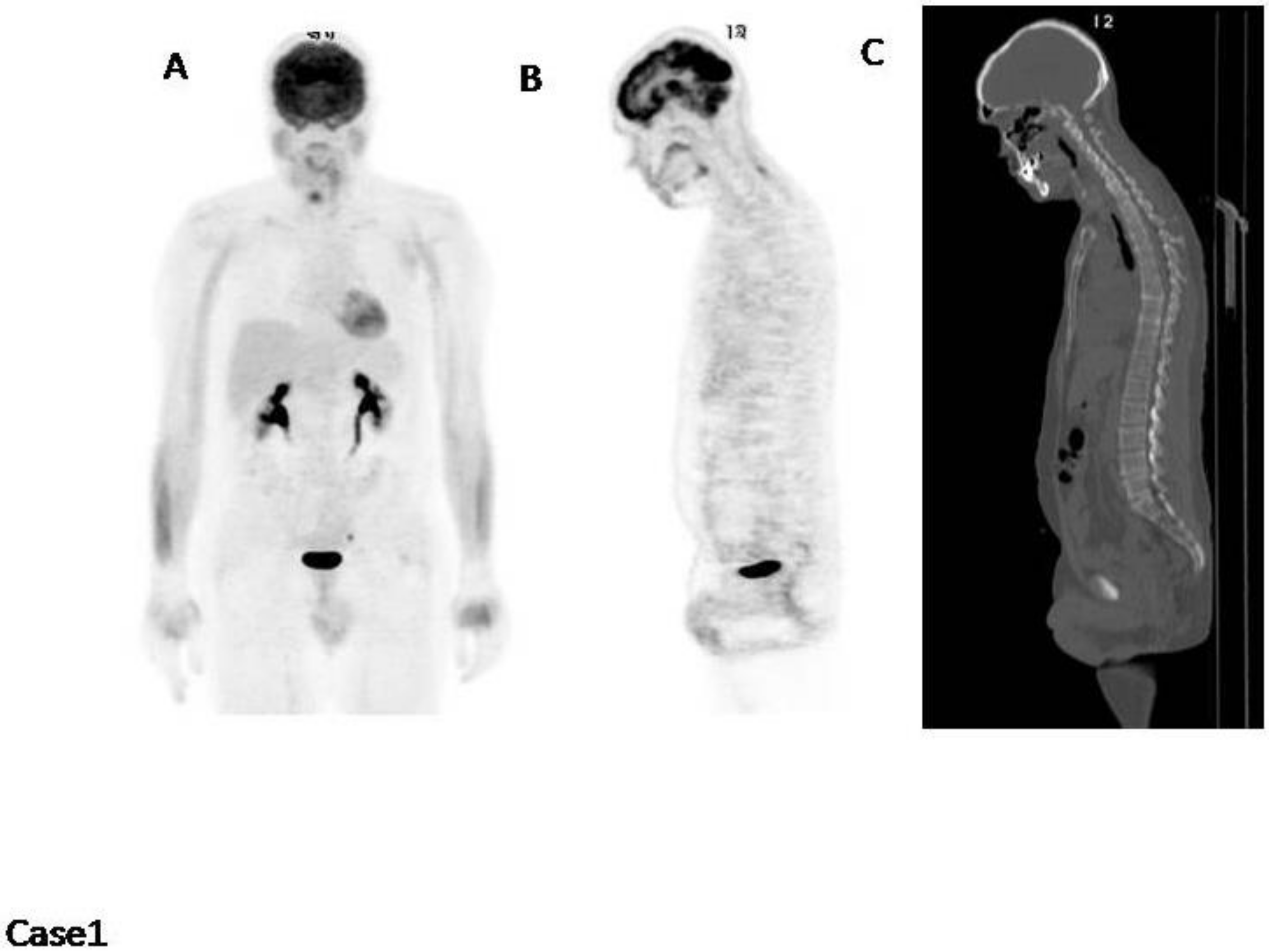
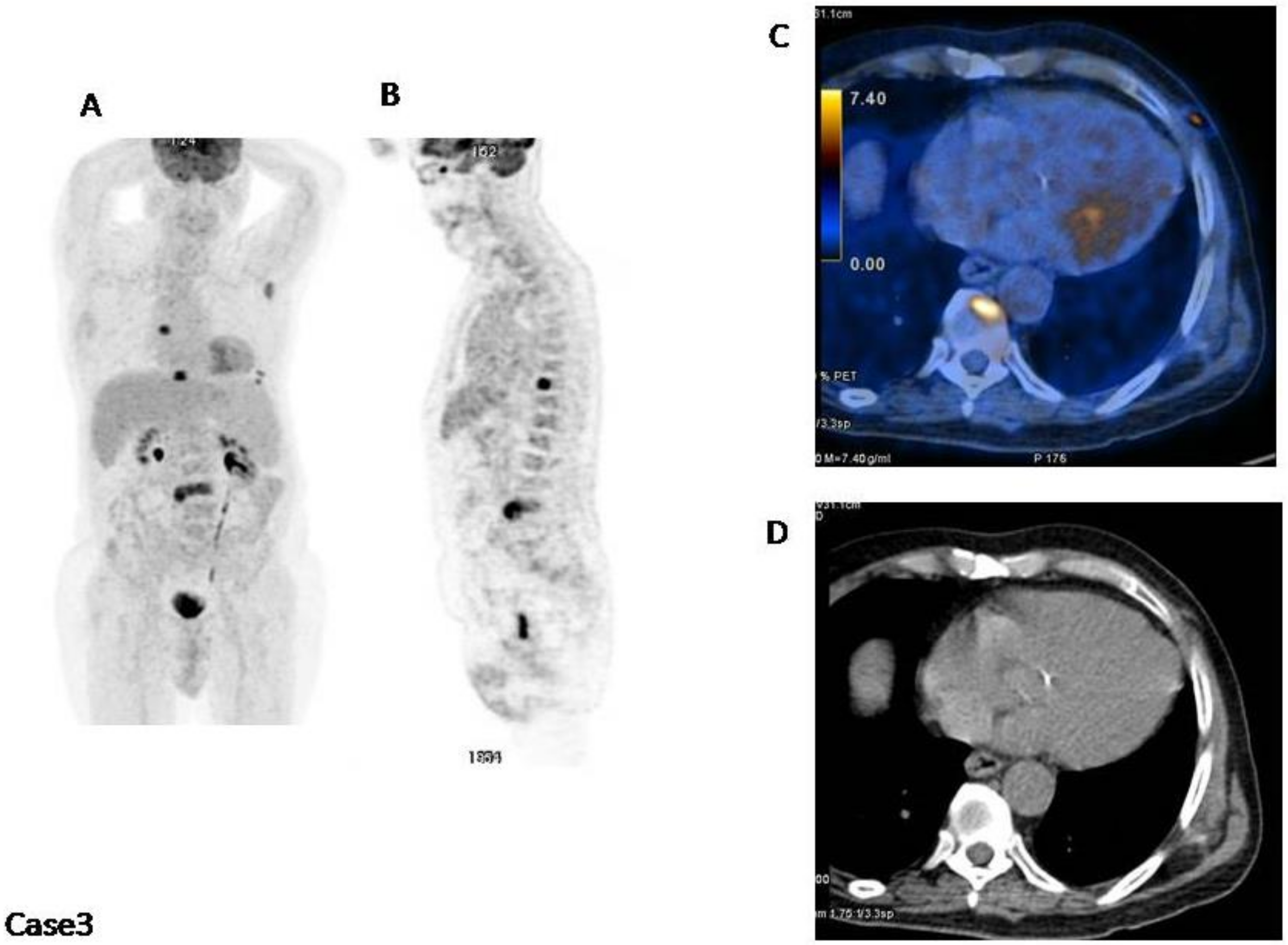
4. Impetus Criteria: Examples of Application
5. Positivity Cut Offs
6. Use of Impetus in Literature
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Rajkumar, S.V.; Dimopolous, M.A.; Palumbo, A.; Blade, J.; Merlini, G.; Mateos, M.V.; Kumar, S.; Hillengass, J.; Kastritis, E.; Richardson, P.; et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014, 15, 538–548. [Google Scholar] [CrossRef]
- Rasche, L.; Angtuaco, E.; McDonald, J.E.; Buros, A.; Stein, C.; Pawlyn, C.; Thanendrarajan, S.; Schinke, C.; Samant, R.; Yaccoby, S.; et al. Low expression of hexokinase-2 is associated with false-negative FDG-positron emission tomography in multiple myeloma. Blood 2017, 130, 30–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abe, Y.; Ikeda, S.; Kitadate, A.; Narita, K.; Kobayashi, H.; Miura, D.; Takeuchi, M.; O’uchi, E.; O’uchi, T.; Matsue, K. Low hexokinase-2 expression-associated false-negative 18F-FDG PET/CT as a potential prognostic predictor in patients with multiple myeloma. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Ntanasis-Stathopoulos, I.; Gavriatopoulou, M.; Dimopoulos, M.A. Pathogenesis of bone disease in multiple myeloma: From bench to bedside. Blood Cancer J. 2018, 8, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimopoulos, M.A.; Terpos, E.; Chanan-Khan, A.; Leung, N.; Ludwig, H.; Jagannath, S.; Niesvizky, R.; Giralt, S.; Fermand, J.P.; Bladé, J.; et al. Renal impairment in patients with multiple myeloma: A consensus statement on behalf of the International Myeloma Working Group. J. Clin. Oncol. 2010, 28, 4976–4984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonti, R.; Larobina, M.; Del Vecchio, S.; De Luca, S.; Fabbricini, R.; Catalano, L.; Pane, F.; Salvatore, M.; Pace, L. Metabolic tumor volume assessed by 18F-FDG PET/CT for the prediction of outcome in patients with multiple myeloma. J. Nucl. Med. 2012, 53, 1829–1835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nanni, C.; Zamagni, E.; Versari, A.; Chauvie, S.; Bianchi, A.; Rensi, M.; Bellò, M.; Rambaldi, I.; Gallamini, A.; Patriarca, F.; et al. Image interpretation criteria for FDG PET/CT in multiple myeloma: A new proposal from an Italian expert panel. IMPeTUs (Italian myeloma criteria for PET USe). Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Barrington, S.F.; Mikhaeel, N.G. When should FDG-PET be used in the modern management of lymphoma? Br. J. Haematol. 2014, 164, 315–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nanni, C.; Versari, A.; Chauvie, S.; Bertone, E.; Bianchi, A.; Rensi, M.; Bellò, M.; Gallamini, A.; Patriarca, F.; Gay, F.; et al. Interpretation criteria for FDG PET/CT in multiple myeloma (IMPeTUs): Final results. IMPeTUs (Italian myeloma criteria for PET USe). Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Abe, Y.; Narita, K.; Kobayashi, H.; Kitadate, A.; Takeuchi, M.; O’uchi, T.; Matsue, K. Medullary Abnormalities in Appendicular Skeletons Detected With 18F-FDG PET/CT Predict an Unfavorable Prognosis in Newly Diagnosed Multiple Myeloma Patients with High-Risk Factors. AJR Am. J. Roentgenol. 2019, 213, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Zamagni, E.; Nanni, C.; Dozza, L.; Carlier, T.; Bailly, C.; Tacchetti, P.; Versari, A.; Chauvie, S.; Gallamini, A.; Attal, M. Standardization of 18F-FDG PET/CT according to Deauville criteria for metabolic complete response definition in newly diagnosed transplant eligible multiple myeloma (mm) patients: Joint analysis of two prospective randomized phase III trials. Blood 2018, 132, 257. [Google Scholar] [CrossRef] [Green Version]
- Shengming, D.; Bin, Z.; Zhou, Y.; Xu, X.; Li, J.; Sang, S.; Zhang, W. The Role of 18F-FDG PET/CT in Multiple Myeloma Staging according to IMPeTUs: Comparison of the Durie–Salmon Plus and Other Staging Systems. Contrast Media Mol. Imaging 2018, 2018, 4198673. [Google Scholar]



© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nanni, C. PET-FDG: Impetus. Cancers 2020, 12, 1030. https://doi.org/10.3390/cancers12041030
Nanni C. PET-FDG: Impetus. Cancers. 2020; 12(4):1030. https://doi.org/10.3390/cancers12041030
Chicago/Turabian StyleNanni, Cristina. 2020. "PET-FDG: Impetus" Cancers 12, no. 4: 1030. https://doi.org/10.3390/cancers12041030
APA StyleNanni, C. (2020). PET-FDG: Impetus. Cancers, 12(4), 1030. https://doi.org/10.3390/cancers12041030



