Validation of the 2018 FIGO Classification for Cervical Cancer: Lymphovascular Space Invasion Should Be Considered in IB1 Stage
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
2.1. Population Characteristics
2.2. FIGO Stage Modification
2.3. Survical Outcomes
3. Discussion
4. Materials and Methods
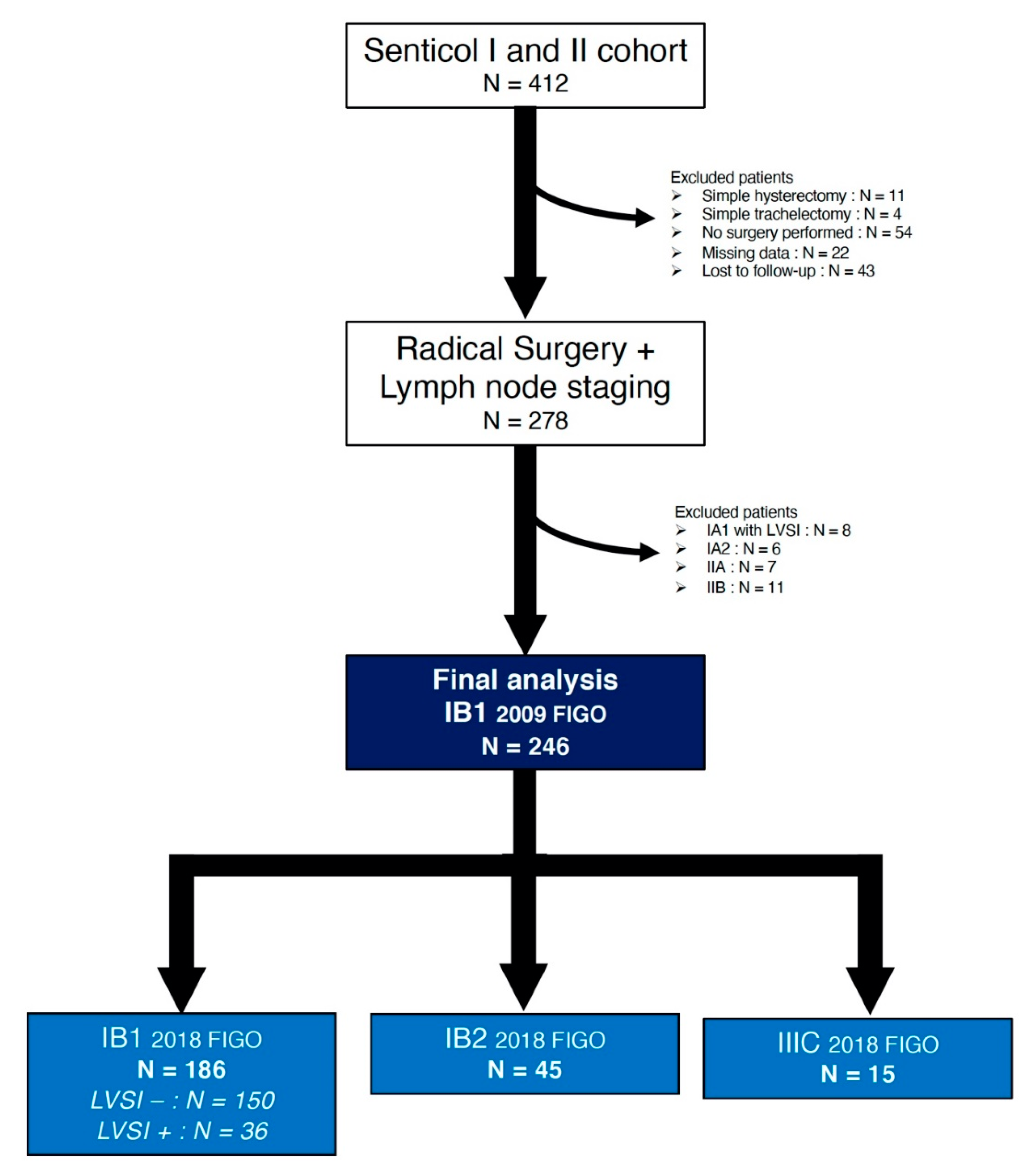
4.1. Patient Selection
4.2. Data Analysis
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Koh, W.-J.; Abu-Rustum, N.R.; Bean, S.; Bradley, K.; Campos, S.M.; Cho, K.R.; Chon, H.S.; Chu, C.; Clark, R.; Cohn, D.; et al. Cervical Cancer, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. JNCCN 2019, 17, 64–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLachlan, J.; Boussios, S.; Okines, A.; Glaessgen, D.; Bodlar, S.; Kalaitzaki, R.; Taylor, A.; Lalondrelle, S.; Gore, M.; Kaye, S.; et al. The Impact of Systemic Therapy beyond First-line Treatment for Advanced Cervical Cancer. Clin. Oncol. 2017, 29, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Cibula, D.; Pötter, R.; Planchamp, F.; Avall-Lundqvist, E.; Fischerova, D.; Haie Meder, C.; Köhler, C.; Landoni, F.; Lax, S.; Lindegaard, J.C.; et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients with Cervical Cancer. Int. J. Gynecol. Cancer 2018, 28, 641. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, O.K.; Chen, J.; Dodson, M.; Lee, C.M.; Gaffney, D.K. Prognostic significance of histology and positive lymph node involvement following radical hysterectomy in carcinoma of the cervix. Am. J. Clin. Oncol. 2009, 32, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Xia, X.; Xu, H.; Wang, Z.; Liu, R.; Hu, T.; Li, S. Analysis of Prognostic Factors Affecting the Outcome of Stage IB-IIB Cervical Cancer Treated by Radical Hysterectomy and Pelvic Lymphadenectomy. Am. J. Clin. Oncol. 2016, 39, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.H.; Kim, Y.S.; Nam, J.-H. Prognostic significance of lymph node ratio in node-positive cervical cancer patients. Medicine (Baltimore) 2018, 97, e11711. [Google Scholar] [CrossRef]
- Kwon, J.; Eom, K.-Y.; Kim, Y.S.; Park, W.; Chun, M.; Lee, J.; Kim, Y.B.; Yoon, W.S.; Kim, J.H.; Choi, J.H.; et al. The Prognostic Impact of the Number of Metastatic Lymph Nodes and a New Prognostic Scoring System for Recurrence in Early-Stage Cervical Cancer with High Risk Factors: A Multicenter Cohort Study (KROG 15-04). Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2018, 50, 964–974. [Google Scholar] [CrossRef]
- Sartori, E.; Tisi, G.; Chiudinelli, F.; La Face, B.; Franzini, R.; Pecorelli, S. Early stage cervical cancer: Adjuvant treatment in negative lymph node cases. Gynecol. Oncol. 2007, 107, S170–S174. [Google Scholar] [CrossRef]
- Cooke, E.W.; Pappas, L.; Gaffney, D.K. Does the revised International Federation of Gynecology and Obstetrics staging system for endometrial cancer lead to increased discrimination in patient outcomes? Cancer 2011, 117, 4231–4237. [Google Scholar] [CrossRef]
- Rosendahl, M.; Høgdall, C.K.; Mosgaard, B.J. Restaging and Survival Analysis of 4036 Ovarian Cancer Patients According to the 2013 FIGO Classification for Ovarian, Fallopian Tube, and Primary Peritoneal Cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2016, 26, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, N.; Berek, J.S.; Cuello Fredes, M.; Denny, L.A.; Grenman, S.; Karunaratne, K.; Kehoe, S.T.; Konishi, I.; Olawaiye, A.B.; Prat, J.; et al. Revised FIGO staging for carcinoma of the cervix uteri. Int. J. Gynaecol. Obstet. 2019, 145, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Herr, D.; König, J.; Heilmann, V.; Koretz, K.; Kreienberg, R.; Kurzeder, C. Prognostic impact of satellite-lymphovascular space involvement in early-stage cervical cancer. Ann. Surg. Oncol. 2009, 16, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Qiu, S.; Ding, Y.; Zhang, Q.; Si, L.; Lv, S.; Liu, L. Prognostic value of lymphovascular space invasion in patients with early stage cervical cancer in Jilin, China: A retrospective study. Medicine (Baltim.) 2019, 98, e17301. [Google Scholar] [CrossRef] [PubMed]
- Creasman, W.T.; Kohler, M.F. Is lymph vascular space involvement an independent prognostic factor in early cervical cancer? Gynecol. Oncol. 2004, 92, 525–529. [Google Scholar] [CrossRef]
- Obrzut, B.; Semczuk, A.; Naróg, M.; Obrzut, M.; Król, P. Prognostic Parameters for Patients with Cervical Cancer FIGO Stages IA2-IIB: A Long-Term Follow-Up. Oncology 2017, 93, 106–114. [Google Scholar] [CrossRef]
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; González-Martín, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.R.; et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, Treatment and Follow-up. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2016, 26, 2–30. [Google Scholar] [CrossRef] [Green Version]
- Margolis, B.; Cagle-Colon, K.; Chen, L.; Tergas, A.I.; Boyd, L.; Wright, J.D. Prognostic significance of lymphovascular space invasion for stage IA1 and IA2 cervical cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2020, 30, 735–743. [Google Scholar] [CrossRef]
- Delgado, G.; Bundy, B.; Zaino, R.; Sevin, B.U.; Creasman, W.T.; Major, F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: A Gynecologic Oncology Group study. Gynecol. Oncol. 1990, 38, 352–357. [Google Scholar] [CrossRef]
- Ebina, Y.; Yaegashi, N.; Katabuchi, H.; Nagase, S.; Udagawa, Y.; Hachisuga, T.; Saito, T.; Mikami, M.; Aoki, Y.; Yoshikawa, H. Japan Society of Gynecologic Oncology guidelines 2011 for the treatment of uterine cervical cancer. Int. J. Clin. Oncol. 2015, 20, 240–248. [Google Scholar] [CrossRef]
- Weyl, A.; Illac, C.; Lusque, A.; Leray, H.; Vaysse, C.; Martinez, A.; Chantalat, E.; Motton, S. Prognostic value of lymphovascular space invasion in early-stage cervical cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2020, 30, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Boussios, S.; Seraj, E.; Zarkavelis, G.; Petrakis, D.; Kollas, A.; Kafantari, A.; Assi, A.; Tatsi, K.; Pavlidis, N.; Pentheroudakis, G. Management of patients with recurrent/advanced cervical cancer beyond first line platinum regimens: Where do we stand? A literature review. Crit. Rev. Oncol. Hematol. 2016, 108, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-Y.; Kim, Y.T.; Kim, S.; Lee, B.; Lim, M.C.; Kim, J.-W.; Won, Y.-J. Prognosis of Cervical Cancer in the Era of Concurrent Chemoradiation from National Database in Korea: A Comparison between Squamous Cell Carcinoma and Adenocarcinoma. PLoS ONE 2015, 10, e0144887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.L.-Y.; Huang, C.-Y.; Huang, Y.-S.; Chen, R.-J.; Wang, C.-W.; Chen, Y.-H.; Cheng, J.C.-H.; Cheng, A.-L.; Kuo, S.-H. Differential clinical characteristics, treatment response and prognosis of locally advanced adenocarcinoma/adenosquamous carcinoma and squamous cell carcinoma of cervix treated with definitive radiotherapy. Acta Obstet. Gynecol. Scand. 2014, 93, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-Y.; Kim, D.-Y.; Kim, J.-H.; Kim, Y.-M.; Kim, Y.-T.; Nam, J.-H. Outcomes after radical hysterectomy according to tumor size divided by 2-cm interval in patients with early cervical cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2011, 22, 59–67. [Google Scholar] [CrossRef]
- Piver, M.S.; Chung, W.S. Prognostic significance of cervical lesion size and pelvic node metastases in cervical carcinoma. Obstet. Gynecol. 1975, 46, 507–510. [Google Scholar]
- Landoni, F.; Maneo, A.; Colombo, A.; Placa, F.; Milani, R.; Perego, P.; Favini, G.; Ferri, L.; Mangioni, C. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 1997, 350, 535–540. [Google Scholar] [CrossRef]
- Roy, M.; Plante, M. Pregnancies after radical vaginal trachelectomy for early-stage cervical cancer. Am. J. Obstet. Gynecol. 1998, 179, 1491–1496. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef]
- Kim, S.I.; Cho, J.H.; Seol, A.; Kim, Y.I.; Lee, M.; Kim, H.S.; Chung, H.H.; Kim, J.-W.; Park, N.H.; Song, Y.-S. Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1-IIA2 cervical cancer. Gynecol. Oncol. 2019, 153, 3–12. [Google Scholar] [CrossRef]
- de Gregorio, A.; Widschwendter, P.; Ebner, F.; Friedl, T.W.P.; Huober, J.; Janni, W.; de Gregorio, N. Influence of the New FIGO Classification for Cervical Cancer on Patient Survival: A Retrospective Analysis of 265 Histologically Confirmed Cases with FIGO Stages IA to IIB. Oncology 2020, 98, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Ayhan, A.; Aslan, K.; Bulut, A.N.; Akilli, H.; Öz, M.; Haberal, A.; Meydanli, M.M. Is the revised 2018 FIGO staging system for cervical cancer more prognostic than the 2009 FIGO staging system for women previously staged as IB disease? Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Machida, H.; Mandelbaum, R.S.; Konishi, I.; Mikami, M. Validation of the 2018 FIGO cervical cancer staging system. Gynecol. Oncol. 2019, 152, 87–93. [Google Scholar] [CrossRef] [PubMed]
- McComas, K.N.; Torgeson, A.M.; Ager, B.J.; Hellekson, C.; Burt, L.M.; Maurer, K.A.; Werner, T.L.; Gaffney, D.K. The variable impact of positive lymph nodes in cervical cancer: Implications of the new FIGO staging system. Gynecol. Oncol. 2020, 156, 85–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cibula, D.; Abu-Rustum, N.R.; Dusek, L.; Zikán, M.; Zaal, A.; Sevcik, L.; Kenter, G.G.; Querleu, D.; Jach, R.; Bats, A.S.; et al. Prognostic significance of low volume sentinel lymph node disease in early-stage cervical cancer. Gynecol. Oncol. 2012, 124, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Guani, B.; Dorez, M.; Magaud, L.; Buenerd, A.; Lecuru, F.; Mathevet, P. Impact of micrometastasis or isolated tumor cells on recurrence and survival in patients with early cervical cancer: SENTICOL Trial. Int. J. Gynecol. Cancer 2019, 29, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Melamed, A.; Margul, D.J.; Chen, L.; Keating, N.L.; Del Carmen, M.G.; Yang, J.; Seagle, B.-L.L.; Alexander, A.; Barber, E.L.; Rice, L.W.; et al. Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. N. Engl. J. Med. 2018, 379, 1905–1914. [Google Scholar] [CrossRef] [PubMed]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arévalo-Serrano, J.; Căpîlna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR study: An international European cohort observational study comparing minimally invasive surgery versus open abdominal radical hysterectomy in patients with stage IB1 cervical cancer. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2020, 30, 1269–1277. [Google Scholar] [CrossRef]
- Lécuru, F.; Mathevet, P.; Querleu, D.; Leblanc, E.; Morice, P.; Daraï, E.; Marret, H.; Magaud, L.; Gillaizeau, F.; Chatellier, G.; et al. Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: Results of the SENTICOL study. J. Clin. Oncol. 2011, 29, 1686–1691. [Google Scholar] [CrossRef]
- Mathevet, P.; Lecuru, F.; Magaud, L.; Bouttitie, F. Sentinel lymph node biopsy for early cervical cancer: Results of a randomized prospective, multicenter study (Senticol 2) comparing adding pelvic lymph node dissection vs sentinel node biopsy only. Gynecol. Oncol. 2017, 145 (Suppl. 1), 2–3. [Google Scholar] [CrossRef]
- Hermanek, P.; Hutter, R.V.; Sobin, L.H.; Wittekind, C. International Union against Cancer. Classification of isolated tumor cells and micrometastasis. Cancer 1999, 86, 2668–2673. [Google Scholar] [CrossRef]
- Corrigendum to “Revised FIGO staging for carcinoma of the cervix uteri” [Int J Gynecol Obstet 145(2019) 129-135]. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2019, 147, 279–280. [CrossRef] [PubMed]

| Variable | Total Population N = 246 | |
|---|---|---|
| N Patients or Median | % or (Range) | |
| Age at diagnosis [years] | ||
| All patients | 42 | (22–85) |
| <50 | 181 | 73.6 |
| 50–70 | 56 | 22.8 |
| >70 | 9 | 3.7 |
| Body Mass-Index [kg/m2] | ||
| All patients | 22.7 | (14.6–41.4) |
| <18.5 | 20 | 8.1 |
| 18.5–25 | 154 | 62.6 |
| <25–30 | 43 | 17.5 |
| >30 | 29 | 11.8 |
| Menopausal status | ||
| Premenopausal | 174 | 70.7 |
| Postmenopausal | 72 | 29.3 |
| Histology | ||
| Squamous cell carcinoma | 166 | 67.5 |
| Adenocarcinoma | 74 | 30.1 |
| Other type | 6 | 2.4 |
| Grade of differenciation | ||
| G1 | 77 | 43.0 |
| G2 | 65 | 36.3 |
| G3 | 37 | 20.7 |
| Not specified | 65 | - |
| Conisation | ||
| Yes | 150 | 61.0 |
| No | 96 | 39.0 |
| Preoperative brachytherapy | ||
| Yes | 66 | 26.8 |
| No | 180 | 73.2 |
| Surgical procedure | ||
| Type of surgery | ||
| Radical Hysterectomy | 199 | 80.9 |
| Radical Trachelectomy | 47 | 19.1 |
| Type of surgical approach | ||
| Minimal Invasive Surgery | 229 | 93.1 |
| Laparotomy | 17 | 6.9 |
| Type of Lymph node staging | ||
| SLN alone | 77 | 31.3 |
| SLN + Pelvic lymphadenectomy | 169 | 68.7 |
| Final pathologic examination | ||
| Tumor size | ||
| <20 mm | 200 | 81.3 |
| ≥20 mm | 46 | 18.7 |
| Deep stromal invasion | ||
| <10 mm | 178 | 80.2 |
| ≥10 mm | 44 | 19.8 |
| Not specified | 24 | - |
| LVSI | ||
| Yes | 57 | 23.2 |
| No | 189 | 76.8 |
| Positive margin | ||
| Yes | 9 | 3.7 |
| No | 237 | 96.3 |
| Patients with ≥1 positive node | ||
| Yes | 15 | 6.1 |
| No | 231 | 93.9 |
| Adjuvant treatment | ||
| None | 186 | 75.6 |
| Brachytherapy | 29 | 11.8 |
| EBRT | 11 | 4.5 |
| CCR | 20 | 8.1 |
| Outcomes | ||
| Recurrence | ||
| None | 226 | 91.5 |
| Nodal | 5 | 2.0 |
| Vaginal | 5 | 2.0 |
| Pelvic | 5 | 2.0 |
| Distant metastases | 6 | 2.4 |
| Status | ||
| Alive | 238 | 96.8 |
| Dead | 8 | 3.2 |
| Predictive Variable | IB1 LVSI− N = 150 | IB1 LVSI+ N = 36 | p | ||
|---|---|---|---|---|---|
| N Patients or Mean ± SD | % or (Range) | N Patients or Mean ± SD | % or (Range) | ||
| Age (years) | |||||
| All patients | 43.8 ± 12.3 | (22–85) | 43.1 ± 12.3 | (26–72) | 0.74 |
| <50 | 112 | 74.7 | 25 | 69.4 | 0.68 |
| 50–70 | 32 | 21.3 | 10 | 27.8 | |
| > 70 | 6 | 4.0 | 1 | 2.8 | |
| BMI [kg/m2] | |||||
| All patients | 23.9 ± 5.2 | (14.6–41.4) | 23.5 ± 4.8 | (17.4–37.7) | 0.72 |
| <18.5 | 10 | 6.7 | 1 | 2.8 | 0.75 |
| 18.5–25 | 97 | 64.7 | 26 | 72.2 | |
| <25–30 | 26 | 17.3 | 5 | 13.9 | |
| >30 | 17 | 11.3 | 4 | 11.1 | |
| Menopausal status | |||||
| Premenopausal | 107 | 71.3 | 25 | 69.4 | 0.83 |
| Postmenopausal | 43 | 28.7 | 11 | 30.6 | |
| Histology | |||||
| Squamous cell carcinoma | 101 | 67.3 | 25 | 69.4 | 0.43 |
| Adenocarcinoma | 46 | 30.7 | 9 | 25.0 | |
| Other type | 3 | 2.0 | 2 | 5.6 | |
| Grade of differenciation | |||||
| G1 | 47 | 45.2 | 10 | 35.7 | 0.22 |
| G2 | 39 | 37.5 | 9 | 32.1 | |
| G3 | 18 | 17.3 | 9 | 32.1 | |
| Not specified | 46 | - | 8 | - | |
| Conisation | |||||
| Yes | 100 | 67.1 | 22 | 61.1 | 0.49 |
| No | 49 | 32.9 | 14 | 38.9 | |
| Preoperative brachytherapy | |||||
| Yes | 47 | 31.3 | 7 | 19.4 | 0.16 |
| No | 103 | 68.7 | 29 | 80.6 | |
| Surgical procedure | |||||
| Type of surgery | |||||
| Radical Hysterectomy | 118 | 78.7 | 30 | 83.3 | 0.53 |
| Radical Trachelectomy | 32 | 21.3 | 6 | 16.7 | |
| Type of surgical approach | |||||
| Minimal Invasive Surgery | 143 | 95.3 | 35 | 97.2 | 0.62 |
| Laparotomy | 7 | 4.7 | 1 | 2.8 | |
| Type of Lymph node staging | |||||
| SLN alone | 58 | 38.7 | 9 | 25.0 | 0.12 |
| SLN + Pelvic lymphadenectomy | 92 | 61.3 | 27 | 75.0 | |
| Final pathologic exam | |||||
| Tumor size (mm) | 2.9 ± 5.2 | (0–18) | 7.5 ± 7.4 | (0–18) | <0.0001 |
| Deep stromal invasion | |||||
| Mean | 2.1 ± 4.9 | (0–20) | 5.4 ± 6.1 | (0–20) | 0.001 |
| <10 mm | 132 | 94.3 | 23 | 67.6 | <0.0001 |
| ≥10 mm | 8 | 5.7 | 11 | 32.4 | |
| Not specified | 10 | - | 2 | - | |
| Positive margin | |||||
| Yes | 5 | 3.3 | 2 | 5.6 | 0.53 |
| No | 145 | 96.7 | 34 | 94.4 | |
| Presence of ITCs | |||||
| Yes | 3 | 2.0 | 1 | 2.8 | 0.77 |
| No | 147 | 98.0 | 35 | 97.2 | |
| Adjuvant treatment | |||||
| None | 136 | 90.7 | 24 | 66.7 | 0.0002 |
| Brachytherapy | 10 | 6.7 | 9 | 25.0 | |
| EBRT | 1 | 0.7 | 3 | 8.3 | |
| CCR | 3 | 2.0 | 0 | 0.0 | |
| 2009 FIGO Classification | 2018 FIGO Classification | 2018 FIGO Classification with LVSI Status | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 FIGO | n | Number of events | 5-year DFS | 2018 FIGO | n | Number of events | 5-year DFS | HR | 95% CI | p | 2018 FIGO | n | Number of events | 5-year DFS | HR | 95% CI | p |
| IB1 | 246 | 20 | 90.0% | IB1 | 186 | 11 | 92.9% | 1 | IB1 LVSI− | 150 | 6 | 95.8% | 1 | ||||
| IB1 LVSI+ | 36 | 5 | 82.5% | 3.33 | 1.02–10.91 | 0.047 | |||||||||||
| IB2 | 45 | 8 | 78.6% | 3.31 | 1.33–8.23 | 0.003 | IB2 | 45 | 8 | 78.6% | 4.85 | 1.68–13.98 | 0.003 | ||||
| IIIC | 15 | 1 | 91.7% | 1.09 | 0.14–8.44 | 0.93 | IIIC | 15 | 1 | 91.7% | 1.60 | 0.19–13.27 | 0.66 | ||||
| 2009 FIGO Classification | 2018 FIGO Classification | 2018 FIGO Classification with LVSI Status | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 FIGO | n | Number of events | 5-year DFS | 2018 FIGO | n | Number of events | 5-year DFS | HR | 95% CI | p | 2018 FIGO | n | Number of events | 5-year DFS | HR | 95% CI | p |
| IB1 | 246 | 8 | 96.2% | IB1 | 186 | 4 | 97.3% | 1 | IB1 LVSI− | 150 | 2 | 98.2% | 1 | ||||
| IB1 LVSI+ | 36 | 2 | 94.2% | 3.99 | 0.56–28.34 | 0.17 | |||||||||||
| IB2 | 45 | 4 | 90% | 4.35 | 1.09–17.4 | 0.04 | IB2 | 45 | 4 | 90.0% | 6.96 | 1.27–38.01 | 0.03 | ||||
| IIIC | 15 | 0 | 100% | NA | NA | NA | IIIC | 15 | 0 | 100% | NA | NA | NA | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balaya, V.; Guani, B.; Magaud, L.; Bonsang-Kitzis, H.; Ngô, C.; Mathevet, P.; Lécuru, F.; on behalf of the SENTICOL Group. Validation of the 2018 FIGO Classification for Cervical Cancer: Lymphovascular Space Invasion Should Be Considered in IB1 Stage. Cancers 2020, 12, 3554. https://doi.org/10.3390/cancers12123554
Balaya V, Guani B, Magaud L, Bonsang-Kitzis H, Ngô C, Mathevet P, Lécuru F, on behalf of the SENTICOL Group. Validation of the 2018 FIGO Classification for Cervical Cancer: Lymphovascular Space Invasion Should Be Considered in IB1 Stage. Cancers. 2020; 12(12):3554. https://doi.org/10.3390/cancers12123554
Chicago/Turabian StyleBalaya, Vincent, Benedetta Guani, Laurent Magaud, Hélène Bonsang-Kitzis, Charlotte Ngô, Patrice Mathevet, Fabrice Lécuru, and on behalf of the SENTICOL Group. 2020. "Validation of the 2018 FIGO Classification for Cervical Cancer: Lymphovascular Space Invasion Should Be Considered in IB1 Stage" Cancers 12, no. 12: 3554. https://doi.org/10.3390/cancers12123554
APA StyleBalaya, V., Guani, B., Magaud, L., Bonsang-Kitzis, H., Ngô, C., Mathevet, P., Lécuru, F., & on behalf of the SENTICOL Group. (2020). Validation of the 2018 FIGO Classification for Cervical Cancer: Lymphovascular Space Invasion Should Be Considered in IB1 Stage. Cancers, 12(12), 3554. https://doi.org/10.3390/cancers12123554







