Survival Improvement over Time of 960 s-AML Patients Included in 13 EORTC-GIMEMA-HOVON Trials
Simple Summary
Abstract
1. Introduction
2. Results
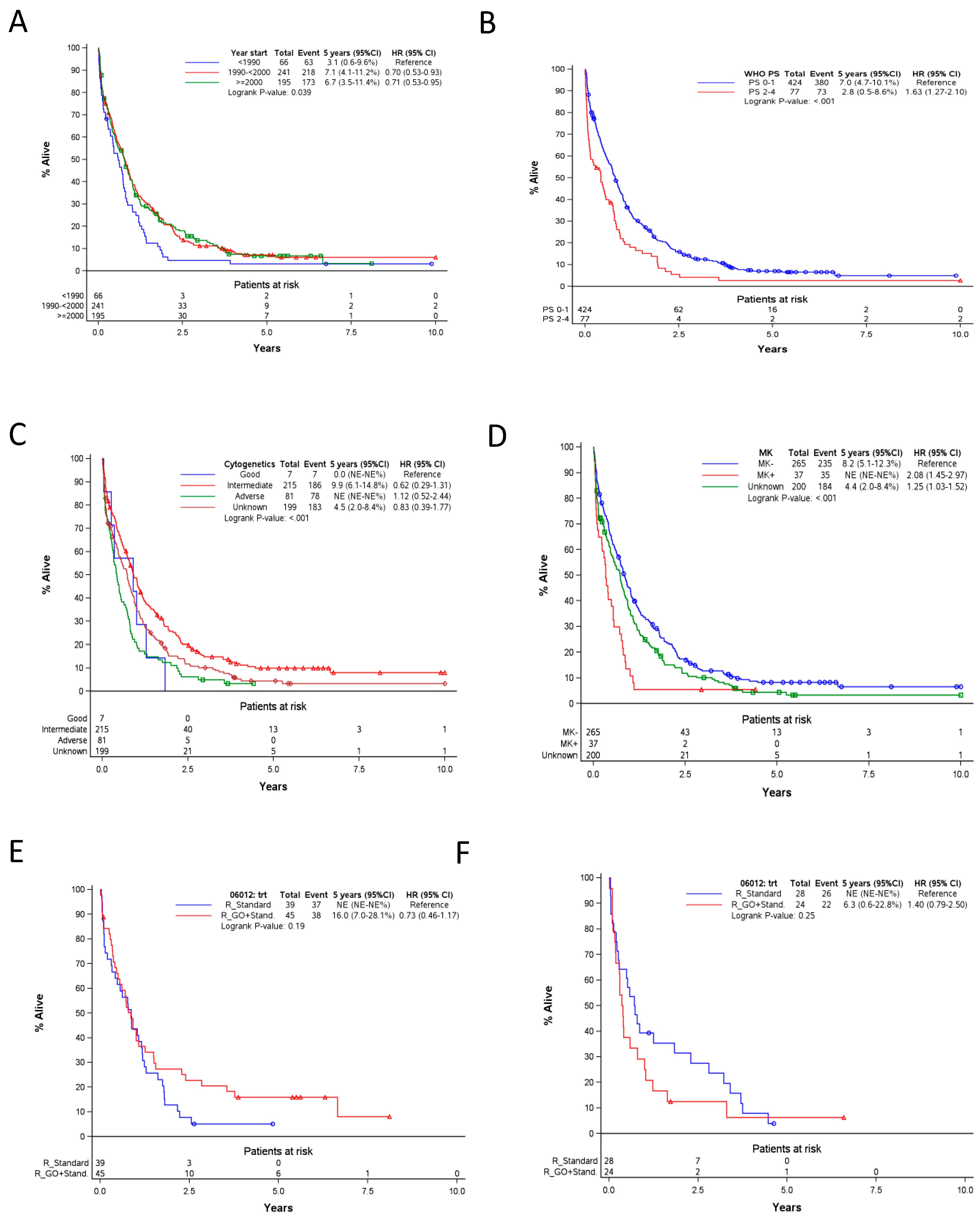
2.1. Patients and Overall Survival (OS) in the Whole Cohort
2.2. Outcomes in Patients ≤ 60 Years Old with Secondary Acute Myeloid Leukemia (s-AML) Occurring after MDS or Other Malignancies
2.2.1. General Characteristics and Outcomes
2.2.2. Factors Affecting OS
2.2.3. Impact of allo-SCT and auto-SCT on OS
2.3. Outcomes in Patients > 60 Years Old with s-AML Occurring after MDS or Other Malignancies
2.3.1. General Characteristics and Outcomes
2.3.2. Factors Associated with OS
3. Discussion
4. Patients and Methods
4.1. Patients, Treatment, Data Management and Methods
4.2. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ertz-Archambault, N.; Kosiorek, H.; Taylor, G.E.; Kelemen, K.; Dueck, A.; Castro, J.; Marino, R.; Gauthier, S.; Finn, L.; Sproat, L.Z.; et al. Association of Therapy for Autoimmune Disease With Myelodysplastic Syndromes and Acute Myeloid Leukemia. JAMA Oncol. 2017, 3, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Leone, G.; Mele, L.; Pulsoni, A.; Equitani, F.; Pagano, L. The incidence of secondary leukemias (Review). Haematologica 1999, 84, 937–945. [Google Scholar] [PubMed]
- Hulegardh, E.; Nilsson, C.; Lazarevic, V.; Garelius, H.; Antunovic, P.; Rangert Derolf, A.; Mollgard, L.; Uggla, B.; Wennstrom, L.; Wahlin, A.; et al. Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: A report from the Swedish Acute Leukemia Registry. Am. J. Hematol. 2015, 90, 208–214. [Google Scholar] [CrossRef]
- Rampal, R.; Ahn, J.; Abdel-Wahab, O.; Nahas, M.; Wang, K.; Lipson, D.; Otto, G.A.; Yelensky, R.; Hricik, T.; McKenney, A.S.; et al. Genomic and functional analysis of leukemic transformation of myeloproliferative neoplasms. Proc. Natl. Acad. Sci. USA 2014, 111, E5401–E5410. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Wang, F.; Kantarjian, H.; Doss, D.; Khanna, K.; Thompson, E.; Zhao, L.; Patel, K.; Neelapu, S.; Gumbs, C.; et al. Preleukaemic clonal haemopoiesis and risk of therapy-related myeloid neoplasms: A case-control study. Lancet. Oncol. 2017, 18, 100–111. [Google Scholar] [CrossRef]
- Boddu, P.; Kantarjian, H.M.; Garcia-Manero, G.; Ravandi, F.; Verstovsek, S.; Jabbour, E.; Borthakur, G.; Konopleva, M.; Bhalla, K.N.; Daver, N.; et al. Treated secondary acute myeloid leukemia: A distinct high-risk subset of AML with adverse prognosis. Blood Adv. 2017, 1, 1312–1323. [Google Scholar] [CrossRef]
- Granfeldt Ostgard, L.S.; Medeiros, B.C.; Sengelov, H.; Norgaard, M.; Andersen, M.K.; Dufva, I.H.; Friis, L.S.; Kjeldsen, E.; Marcher, C.W.; Preiss, B.; et al. Epidemiology and Clinical Significance of Secondary and Therapy-Related Acute Myeloid Leukemia: A National Population-Based Cohort Study. J. Clin. Oncol. 2015, 33, 3641–3649. [Google Scholar] [CrossRef]
- Baron, F.; Stevens-Kroef, M.; Kicinski, M.; Meloni, G.; Muus, P.; Marie, J.P.; Halkes, C.J.M.; Thomas, X.; Vrhovac, R.; Albano, F.; et al. Impact of Induction Regimen and of Allogeneic Hematopoietic Cell Transplantation on Outcome in Younger Adults Patients with Acute Myeloid Leukemia with a Monosomal Karyotype. Haematologica 2019, 104, 1168–1175. [Google Scholar] [CrossRef]
- Willemze, R.; Suciu, S.; Meloni, G.; Labar, B.; Marie, J.P.; Halkes, C.J.; Muus, P.; Mistrik, M.; Amadori, S.; Specchia, G.; et al. High-Dose Cytarabine in Induction Treatment Improves the Outcome of Adult Patients Younger Than Age 46 Years with Acute Myeloid Leukemia: Results of the EORTC-GIMEMA AML-12 Trial. J. Clin. Oncol. 2014, 32, 219–228. [Google Scholar] [CrossRef]
- Amadori, S.; Suciu, S.; Willemze, R.; Mandelli, F.; Selleslag, D.; Stauder, R.; Ho, A.; Denzlinger, C.; Leone, G.; Fabris, P.; et al. Sequential administration of gemtuzumab ozogamicin and conventional chemotherapy as first line therapy in elderly patients with acute myeloid leukemia: A phase II study (AML-15) of the EORTC and GIMEMA leukemia groups. Haematologica 2004, 89, 950–956. [Google Scholar]
- Savani, B.N.; Labopin, M.; Boumendil, A.; Ehninger, G.; Ganser, A.; Ayuk, F.; Stelljes, M.; Finke, J.; Beelen, D.W.; Niederwieser, D.; et al. Allogeneic hematopoietic stem cell transplantation for secondary acute myeloid leukemia-a report from the Acute Leukemia Working Party of the EBMT. Blood 2015, 126, 63. [Google Scholar] [CrossRef]
- Sengsayadeth, S.; Gatwood, K.S.; Boumendil, A.; Labopin, M.; Finke, J.; Ganser, A.; Stelljes, M.; Ehninger, G.; Beelen, D.; Niederwieser, D.; et al. Conditioning intensity in secondary AML with prior myelodysplastic syndrome/myeloproliferative disorders: An EBMT ALWP study. Blood Adv. 2018, 2, 2127–2135. [Google Scholar] [CrossRef] [PubMed]
- Othus, M.; Kantarjian, H.; Petersdorf, S.; Ravandi, F.; Godwin, J.; Cortes, J.; Pierce, S.; Erba, H.; Faderl, S.; Appelbaum, F.R.; et al. Declining rates of treatment-related mortality in patients with newly diagnosed AML given ‘intense’ induction regimens: A report from SWOG and MD Anderson. Leukemia 2014, 28, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Gooley, T.A.; Chien, J.W.; Pergam, S.A.; Hingorani, S.; Sorror, M.L.; Boeckh, M.; Martin, P.J.; Sandmaier, B.M.; Marr, K.A.; Appelbaum, F.R.; et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N. Engl. J. Med. 2010, 363, 2091–2101. [Google Scholar] [CrossRef]
- Canaani, J.; Beohou, E.; Labopin, M.; Ghavamzadeh, A.; Beelen, D.; Hamladji, R.M.; Niederwieser, D.; Volin, L.; Markiewicz, M.; Arnold, R.; et al. Trends in patient outcome over the past two decades following allogeneic stem cell transplantation for acute myeloid leukaemia: An ALWP/EBMT analysis. J. Intern. Med. 2019, 285, 407–418. [Google Scholar] [CrossRef]
- Vulaj, V.; Perissinotti, A.J.; Uebel, J.R.; Nachar, V.R.; Scappaticci, G.B.; Crouch, A.; Bixby, D.L.; Burke, P.W.; Maillard, I.; Talpaz, M.; et al. The FOSSIL Study: FLAG or standard 7+3 induction therapy in secondary acute myeloid leukemia. Leuk Res. 2018, 70, 91–96. [Google Scholar] [CrossRef]
- Baron, F.; Labopin, M.; Savani, B.N.; Beohou, E.; Niederwieser, D.; Eder, M.; Potter, V.; Kroger, N.; Beelen, D.; Socie, G.; et al. Graft-versus-host disease and graft-versus-leukaemia effects in secondary acute myeloid leukaemia: A retrospective, multicentre registry analysis from the Acute Leukaemia Working Party of the EBMT. Br. J. Haematol. 2020, 188, 428–437. [Google Scholar] [CrossRef]
- Lancet, J.E.; Uy, G.L.; Cortes, J.E.; Newell, L.F.; Lin, T.L.; Ritchie, E.K.; Stuart, R.K.; Strickland, S.A.; Hogge, D.; Solomon, S.R.; et al. CPX-351 (cytarabine and daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia. J. Clin. Oncol. 2018, 36, 2684–2692. [Google Scholar] [CrossRef]
- Versluis, J.; Hazenberg, C.L.; Passweg, J.R.; van Putten, W.L.; Maertens, J.; Biemond, B.J.; Theobald, M.; Graux, C.; Kuball, J.; Schouten, H.C.; et al. Post-remission treatment with allogeneic stem cell transplantation in patients aged 60 years and older with acute myeloid leukaemia: A time-dependent analysis. Lancet Haematol. 2015, 2, e427–e436. [Google Scholar] [CrossRef]
- Huls, G.; Chitu, D.A.; Havelange, V.; Jongen-Lavrencic, M.; van de Loosdrecht, A.A.; Biemond, B.J.; Sinnige, H.; Hodossy, B.; Graux, C.; Kooy, R.V.M.; et al. Azacitidine maintenance after intensive chemotherapy improves DFS in older AML patients. Blood 2019, 133, 1457–1464. [Google Scholar] [CrossRef]
- Amadori, S.; Suciu, S.; Stasi, R.; Salih, H.R.; Selleslag, D.; Muus, P.; De Fabritiis, P.; Venditti, A.; Ho, A.D.; Lubbert, M.; et al. Sequential combination of gemtuzumab ozogamicin and standard chemotherapy in older patients with newly diagnosed acute myeloid leukemia: Results of a randomized phase III trial by the EORTC and GIMEMA consortium (AML-17). J. Clin. Oncol. 2013, 31, 4424–4430. [Google Scholar] [CrossRef] [PubMed]
- De Witte, T.; Suciu, S.; Meert, L.; Halkes, C.; Selleslag, D.; Bron, D.; Amadori, S.; Willemze, R.; Muus, P.; Baron, F. Idarubicin and cytarabine in combination with gemtuzumab ozogamicin (IAGO) for untreated patients with high-risk MDS or AML evolved from MDS: A phase II study from the EORTC and GIMEMA Leukemia Groups (protocol 06013). Ann. Hematol. 2015, 94, 1981–1989. [Google Scholar] [CrossRef] [PubMed]
- Lowenberg, B.; Suciu, S.; Archimbaud, E.; Haak, H.; Stryckmans, P.; de Cataldo, R.; Dekker, A.W.; Berneman, Z.N.; Thyss, A.; van der Lelie, J.; et al. Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy--the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: Final report. European Organization for the Research and Treatment of Cancer and the Dutch-Belgian Hemato-Oncology Cooperative Hovon Group. J. Clin. Oncol. 1998, 16, 872–881. [Google Scholar] [PubMed]
- Zittoun, R.A.; Mandelli, F.; Willemze, R.; de Witte, T.; Labar, B.; Resegotti, L.; Leoni, F.; Damasio, E.; Visani, G.; Papa, G.; et al. Autologous or allogeneic bone marrow transplantation compared with intensive chemotherapy in acute myelogenous leukemia. N. Engl. J. Med. 1995, 332, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Baron, F.; Efficace, F.; Cannella, L.; Willemze, R.; Vignetti, M.; Muus, P.; Marie, J.P.; Ferrero, D.; Fazi, P.; La Sala, E.; et al. Long-term follow-up of a trial comparing post-remission treatment with autologous or allogeneic bone marrow transplantation or intensive chemotherapy in younger acute myeloid leukemia patients. Haematologica 2019. [Google Scholar] [CrossRef]
- Hengeveld, M.; Suciu, S.; Karrasch, M.; Specchia, G.; Marie, J.P.; Muus, P.; Petti, M.C.; Rotoli, B.; Amadori, S.; Fioritoni, G.; et al. Intensive consolidation therapy compared with standard consolidation and maintenance therapy for adults with acute myeloid leukaemia aged between 46 and 60 years: Final results of the randomized phase III study (AML 8B) of the European Organization for Research and Treatment of Cancer (EORTC) and the Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto (GIMEMA) Leukemia Cooperative Groups. Ann. Hematol. 2012, 91, 825–835. [Google Scholar] [CrossRef]
- De Witte, T.; Suciu, S.; Peetermans, M.; Fenaux, P.; Strijckmans, P.; Hayat, M.; Jaksic, B.; Selleslag, D.; Zittoun, R.; Dardenne, M.; et al. Intensive chemotherapy for poor prognosis myelodysplasia (MDS) and secondary acute myeloid leukemia (sAML) following MDS of more than 6 months duration. A pilot study by the Leukemia Cooperative Group of the European Organisation for Research and Treatment in Cancer (EORTC-LCG). Leukemia 1995, 9, 1805–1811. [Google Scholar]
- Amadori, S.; Suciu, S.; Jehn, U.; Stasi, R.; Thomas, X.; Marie, J.P.; Muus, P.; Lefrere, F.; Berneman, Z.; Fillet, G.; et al. Use of glycosylated recombinant human G-CSF (lenograstim) during and/or after induction chemotherapy in patients 61 years of age and older with acute myeloid leukemia: Final results of AML-13, a randomized phase-3 study. Blood 2005, 106, 27–34. [Google Scholar] [CrossRef]
- De Witte, T.; Suciu, S.; Verhoef, G.; Labar, B.; Archimbaud, E.; Aul, C.; Selleslag, D.; Ferrant, A.; Wijermans, P.; Mandelli, F.; et al. Intensive chemotherapy followed by allogeneic or autologous stem cell transplantation for patients with myelodysplastic syndromes (MDSs) and acute myeloid leukemia following MDS. Blood 2001, 98, 2326–2331. [Google Scholar] [CrossRef]
- Mandelli, F.; Vignetti, M.; Suciu, S.; Stasi, R.; Petti, M.C.; Meloni, G.; Muus, P.; Marmont, F.; Marie, J.P.; Labar, B.; et al. Daunorubicin versus mitoxantrone versus idarubicin as induction and consolidation chemotherapy for adults with acute myeloid leukemia: The EORTC and GIMEMA Groups Study AML-10. J. Clin. Oncol. 2009, 27, 5397–5403. [Google Scholar] [CrossRef]
- Jehn, U.; Suciu, S.; Thomas, X.; Lefrere, F.; Muus, P.; Berneman, Z.; Marie, J.P.; Adamo, F.; Fillet, G.; Nobile, F.; et al. Non-infusional vs. intravenous consolidation chemotherapy in elderly patients with acute myeloid leukemia: Final results of the EORTC-GIMEMA AML-13 randomized phase III trial. Leukemia 2006, 20, 1723–1730. [Google Scholar] [CrossRef]
- De Witte, T.; Hagemeijer, A.; Suciu, S.; Belhabri, A.; Delforge, M.; Kobbe, G.; Selleslag, D.; Schouten, H.C.; Ferrant, A.; Biersack, H.; et al. Value of allogeneic versus autologous stem cell transplantation and chemotherapy in patients with myelodysplastic syndromes and secondary acute myeloid leukemia. Final results of a prospective randomized European Intergroup Trial. Haematologica 2010, 95, 1754–1761. [Google Scholar] [CrossRef] [PubMed]
- Grimwade, D.; Hills, R.K.; Moorman, A.V.; Walker, H.; Chatters, S.; Goldstone, A.H.; Wheatley, K.; Harrison, C.J.; Burnett, A.K.; National Cancer Research Institute Adult Leukaemia Working Group. Refinement of cytogenetic classification in acute myeloid leukemia: Determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 2010, 116, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Breems, D.A.; van Putten, W.L.; De Greef, G.E.; Van Zelderen-Bhola, S.L.; Gerssen-Schoorl, K.B.; Mellink, C.H.; Nieuwint, A.; Jotterand, M.; Hagemeijer, A.; Beverloo, H.B.; et al. Monosomal karyotype in acute myeloid leukemia: A better indicator of poor prognosis than a complex karyotype. J. Clin. Oncol. 2008, 26, 4791–4797. [Google Scholar] [CrossRef] [PubMed]
- Lubbert, M.; Suciu, S.; Hagemeijer, A.; Ruter, B.; Platzbecker, U.; Giagounidis, A.; Selleslag, D.; Labar, B.; Germing, U.; Salih, H.R.; et al. Decitabine improves progression-free survival in older high-risk MDS patients with multiple autosomal monosomies: Results of a subgroup analysis of the randomized phase III study 06011 of the EORTC Leukemia Cooperative Group and German MDS Study Group. Ann. Hematol. 2016, 95, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Kalbfleisch, J.D.; Prentice, R.L. The Statistical Analysis of Failure Time Data, 2nd ed.; John Wiley: Hoboken, NJ, USA, 2002. [Google Scholar]

| Variation | Group | All | Age | ||
|---|---|---|---|---|---|
| Group A (n = 181) | Group B (n = 186) | Total (n = 367) | 16–45 yrs (n = 127) | 46–60 yrs (n = 240) | |
| Year start of treatment; n (%) | |||||
| <1990 | 10 (5.5) | 16 (8.6) | 26 (7.1) | 13 (10.2) | 13 (5.4) |
| 1990–<2000 | 98 (54.1) | 90 (48.4) | 188 (51.2) | 64 (50.4) | 124 (51.7) |
| ≥2000 | 73 (40.3) | 80 (43.0) | 153 (41.7) | 50 (39.4) | 103 (42.9) |
| Sex, n (%) | |||||
| Male | 109 (60.2) | 74 (39.8) | 183 (49.9) | 65 (51.2) | 118 (49.2) |
| Female | 72 (39.8) | 112 (60.2) | 184 (50.1) | 62 (48.8) | 122 (50.8) |
| Age at Start of Treatment (years) | |||||
| Median (range) | 51 (20–60) | 48 (16–60) | 49 (16–60) | 39.0 (16.0-45.0) | 54.0 (46.0-60.0) |
| 16-45, n (%) | 48 (26.5) | 79 (42.5) | 127 (34.6) | 127 (100.0) | |
| 46-60, n (%) | 133 (73.5) | 107 (57.5) | 240 (65.4) | 240 (100.0) | |
| WHO PS, n (%) | |||||
| 0 | 78 (43.1) | 69 (37.1) | 147 (40.1) | 43 (33.9) | 104 (43.3) |
| 1 | 71 (39.2) | 80 (43.0) | 151 (41.1) | 61 (48.0) | 90 (37.5) |
| 2, 3 or 4 | 32 (17.7) | 36 (19.4) | 68 (18.5) | 22 (17.3) | 46 (19.2) |
| WBC at diagnosis (×109/L) | |||||
| Median (range) | 5.3 (0.6–408.3) | 9.6 (0.5–290.0) | 6.8 (0.5–408.3) | 39.0 (16.0–45.0) | 54.0 (46.0–60.0) |
| <25 | 140 (77.3) | 120 (64.5) | 260 (70.8) | 85 (66.9) | 175 (72.9) |
| ≥25 | 41 (22.7) | 65 (34.9) | 106 (28.9) | 41 (32.3) | 65 (27.1) |
| Cytogenetics Risk Group, n (%) | |||||
| Good | 1 (0.6) | 18 (9.7) | 19 (5.2) | 11 (8.7) | 8 (3.3) |
| Intermediate | 87 (48.1) | 79 (42.5) | 166 (45.2) | 46 (36.2) | 120 (50.0) |
| Adverse | 36 (19.9) | 22 (11.8) | 58 (15.8) | 20 (15.7) | 38 (15.8) |
| Unknown | 57 (31.5) | 67 (36.0) | 124 (33.8) | 50 (39.4) | 74 (30.8) |
| Monosomal Karyotype (MK) Status, n (%) | |||||
| MK− | 108 (59.7) | 108 (58.1) | 216 (58.9) | 68 (53.5) | 148 (61.7) |
| MK+ | 14 (7.7) | 9 (4.8) | 23 (6.3) | 7 (5.5) | 16 (6.7) |
| Unknown | 59 (32.6) | 69 (37.1) | 52 (40.9) | 76 (31.7) | |
| Time From MDS to AML (months) | n = 127 | n = 13 | n = 140 | n = 37 | n = 103 |
| Median (range) | 7.2 (2.1–178.4) | 5.3 | 7.1 (0.4–178.4) | 5.3 (0.7–1.78.4) | 8.0 (0.4–139.7) |
| Time From Other Cancer to AML (years) | |||||
| Median (range) | NA | 3.7 (0.2–30.3) | 3.7 (0.2–30.3) | 3.1 (0.2–30.3) | 4.4 (0.8–22.8) |
| Induction Treatment Intensity | |||||
| Standard | 163 (90.1) | 156 (83.9) | 319 (86.9) | 107 (84.3) | 212 (88.3) |
| Intensive | 18 (9.9) | 30 (16.1) | 48 (13.1) | 20 (15.7) | 28 (11.7) |
| Best Response to Induction Treatment, n (%) | |||||
| No CR/CRi | 87 (49.2) | 65 (34.9) | 154 (42.0) | 41 (32.3) | 113 (47.1) |
| CR/CRi | 92 (50.8) | 121 (65.0) | 213 (58.0) | 86 (67.7) | 127 (53.0)) |
| Auto SCT in CR/CRi, n [%] | 17 [18.5] | 40 [33.1] | 57 [26.8] | 28 [32.6] | 29 [22.8] |
| Allo SCT in CR/CRi, n [%] | 23 [25.0] | 23 [19.0] | 46 [21.6] | 26 [30.2] | 20 [15.7] |
| DFS Status in CR/CRi Patients, n [%] | |||||
| Still in First CR/CRi | 29 [31.5] | 53 [43.8] | 82 38.5] | 48 [55.8] | 34 [26.8] |
| Relapse after CR/CRi | 53 [57.6] | 45 [37.2] | 98 [46.0] | 28 [32.6] | 70 [55.1] |
| Death in CR/CRi | 10 [10.9] | 23 [19.0] | 33 [15.5] | 10 [11.6] | 23 [18.1] |
| Survival Status, n (%) | |||||
| Alive | 42 (23.2) | 65 (34.9) | 107 (29.2) | 55 (43.3) | 52 (21.7) |
| Dead | 139 (76.8) | 121 (65.1) | 260 (70.8) | 72 (56.7) | 188 (78.3) |
| Variable | Category | Hazard Ratio (HR) | 95%CI for HR | p-Value * |
|---|---|---|---|---|
| Model 1 | ||||
| Group | Group A | 1 | ||
| Group B | 0.84 | (0.65, 1.09) | 0.20 | |
| Sex | Male | 1 | ||
| Female | 0.72 | (0.56, 0.93) | 0.01 | |
| WBC (×109/L) | <25 | 1 | ||
| ≥25 | 1.99 | (1.51, 2.62) | <0.001 | |
| Cytogenetics | Good/intermediate | 1 | (<0.001) | |
| Adverse | 2.17 | (1.54, 3.06) | <0.0001 | |
| Unknown | 1.25 | (0.93, 1.67) | 0.14 | |
| Period | <1990 | 1 | (0.005) | |
| 1990 ≤ 2000 | 0.50 | (0.31, 0.80) | 0.003 | |
| ≥2000 | 0.43 | (0.26, 0.70) | 0.0008 | |
| Age (years) | 16–45 | 1 | ||
| 46–60 | 1.65 | (1.24, 2.18) | 0.0005 | |
| Treatment intensity | Standard | 1 | ||
| Intensive | 0.54 | (0.33, 0.87) | 0.01 | |
| Model 2 | ||||
| Group | Group A | 1 | ||
| Group B | 0.82 | (0.63, 1.06) | 0.13 | |
| Sex | Male | 1 | ||
| Female | 0.68 | (0.53, 0.87) | 0.003 | |
| WBC (×109/L) | <25 | 1 | ||
| ≥25 | 2.14 | (1.62, 2.82) | < 0.001 | |
| Cytogenetics | Good/intermediate | 1 | (<0.001) | |
| Adverse | 2.22 | (1.57, 3.12) | <0.0001 | |
| Unknown | 1.27 | (0.95, 1.70) | 0.11 | |
| Period | <1990 | 1 | (0.005) | |
| 1990–<2000 | 0.51 | (0.32, 0.81) | 0.004 | |
| ≥2000 | 0.44 | (0.27, 0.72) | 0.001 | |
| Age/treatment intensity | 16–45 y/Standard | 1 | (0.001) | |
| 16–45 y/Intensive | 0.17 | (0.06, 0.49) | 0.001 | |
| 46–60 y/Standard | 1.41 | (1.06, 1.89) | 0.019 | |
| 46–60 y/Intensive | 1.28 | (0.72, 2.25) | 0.40 | |
| Variable | Group A (n = 327) | Group B (n = 175) | Total (n = 502) |
|---|---|---|---|
| Year start, n (%) | |||
| <1990 | 38 (11.6) | 28 (16.0) | 66 (13.1) |
| 1990 ≤ 2000 | 149 (45.6) | 92 (52.6) | 241 (48.0) |
| ≥2000 | 140 (42.8) | 55 (31.4) | 195 (38.8) |
| Sex, n (%) | |||
| Male | 195 (59.6) | 85 (48.6) | 280 (55.8) |
| Female | 132 (40.4) | 90 (51.4) | 222 (44.2) |
| Age at Start of Induction | |||
| Median (range), years | 68.0 (61.0–85.0) | 68.0 (61.0–85.0) | 68.0 (61.0–85.0) |
| 61–69, n (%) | 191 (58.4) | 115 (65.7) | 306 (61.0) |
| 70–85, n (%) | 136 (41.6) | 60 (34.3) | 196 (39.0) |
| WHO PS, n (%) | |||
| PS 0 | 121 (37.0) | 54 (30.9) | 175 (34.9) |
| PS 1 | 161 (49.2) | 88 (50.3) | 249 (49.6) |
| PS 2, 3 or 4 | 45 (13.7) | 32 (18.3) | 77 (15.3) |
| WBCx109/L at diagnosis, n (%) | |||
| <25 | 250 (76.5) | 119 (68.0) | 369 (73.5) |
| 25 ≤ 100 | 65 (19.9) | 41 (23.4) | 106 (21.1) |
| ≥100 | 12 (3.7) | 15 (8.6) | 27 (5.4) |
| Cytogenetics, n (%) | |||
| Good | 1 (0.3) | 6 (3.4) | 7 (1.4) |
| Intermediate | 151 (46.2) | 64 (36.6) | 215 (42.8) |
| Adverse | 50 (15.3) | 31 (17.7) | 81 (16.1) |
| Unknown | 125 (38.2) | 74 (42.3) | 199 (39.6) |
| Monosomal Karyotype (MK) status, n (%) | |||
| MK− | 186 (56.9) | 79 (45.1) | 265 (52.8) |
| MK+ | 16 (4.9) | 21 (12.0) | 37 (7.4) |
| Unknown | 125 (38.2) | 75 (42.9) | 200 (39.8) |
| Time from MDS to AML (months) | |||
| Median (range) | 7.8 (2.1–126.0) | 11.3 (1.1–58.2) | 8.2 (1.1–126.0) |
| Time from Other Cancer to AML (years) | |||
| Median (range) | 6.4 (0.1–38.0) | 6.4 (0.1–38.0) | |
| CR/CRi Status after Induction, n (%) | |||
| No CR/CRi | 188 (57.5) | 90 (51.4) | 278 (54.4) |
| CR/CRi | 139 (42.5) | 85 (48.6) | 224 (44.6) |
| DFS Status in Patients in CR/CRi, n [%] | |||
| Still in CR/CRi | 11 [7.9] | 10 [11.8] | 21 [9.4] |
| Relapse after CR/CRi | 115 [82.7] | 62 [72.9] | 177 [79.0] |
| Death in CR/CRi | 13 [9.4] | 13 [15.3] | 26 [11.6] |
| Survival Status, n (%) | |||
| Alive | 27 (8.3) | 21 (12.0) | 48 (9.6) |
| Dead | 300 (91.7) | 154 (88.0) | 454 (90.4) |
| 5-year Survival Rate (95% CI) | 5% (3–8%) | 9% (5–14%) | 6% (4–9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramadan, S.M.; Suciu, S.; Stevens-Kroef, M.J.P.L.; Willemze, R.; Amadori, S.; de Witte, T.; Löwenberg, B.; Muus, P.; Labar, B.; Meert, L.; et al. Survival Improvement over Time of 960 s-AML Patients Included in 13 EORTC-GIMEMA-HOVON Trials. Cancers 2020, 12, 3334. https://doi.org/10.3390/cancers12113334
Ramadan SM, Suciu S, Stevens-Kroef MJPL, Willemze R, Amadori S, de Witte T, Löwenberg B, Muus P, Labar B, Meert L, et al. Survival Improvement over Time of 960 s-AML Patients Included in 13 EORTC-GIMEMA-HOVON Trials. Cancers. 2020; 12(11):3334. https://doi.org/10.3390/cancers12113334
Chicago/Turabian StyleRamadan, Safaa M., Stefan Suciu, Marian J. P. L. Stevens-Kroef, Roelof Willemze, Sergio Amadori, Theo de Witte, Bob Löwenberg, Petra Muus, Boris Labar, Liv Meert, and et al. 2020. "Survival Improvement over Time of 960 s-AML Patients Included in 13 EORTC-GIMEMA-HOVON Trials" Cancers 12, no. 11: 3334. https://doi.org/10.3390/cancers12113334
APA StyleRamadan, S. M., Suciu, S., Stevens-Kroef, M. J. P. L., Willemze, R., Amadori, S., de Witte, T., Löwenberg, B., Muus, P., Labar, B., Meert, L., de Schaetzen, G., Meloni, G., Leone, G., Vignetti, M., Marie, J.-P., Lübbert, M., & Baron, F. (2020). Survival Improvement over Time of 960 s-AML Patients Included in 13 EORTC-GIMEMA-HOVON Trials. Cancers, 12(11), 3334. https://doi.org/10.3390/cancers12113334






