Primary Granulocyte Colony-Stimulating Factor Prophylaxis in Metastatic Pancreatic Cancer Patients Treated with FOLFIRINOX as the First-Line Treatment
Abstract
Simple Summary
Abstract
1. Introduction
2. Method
2.1. Study Population
2.2. Study Design
2.3. G-CSF Agents
2.4. Statistical Analysis
2.5. Ethics Statement
3. Results
3.1. Characteristics of the Patients
3.2. AEs
3.3. Efficacy
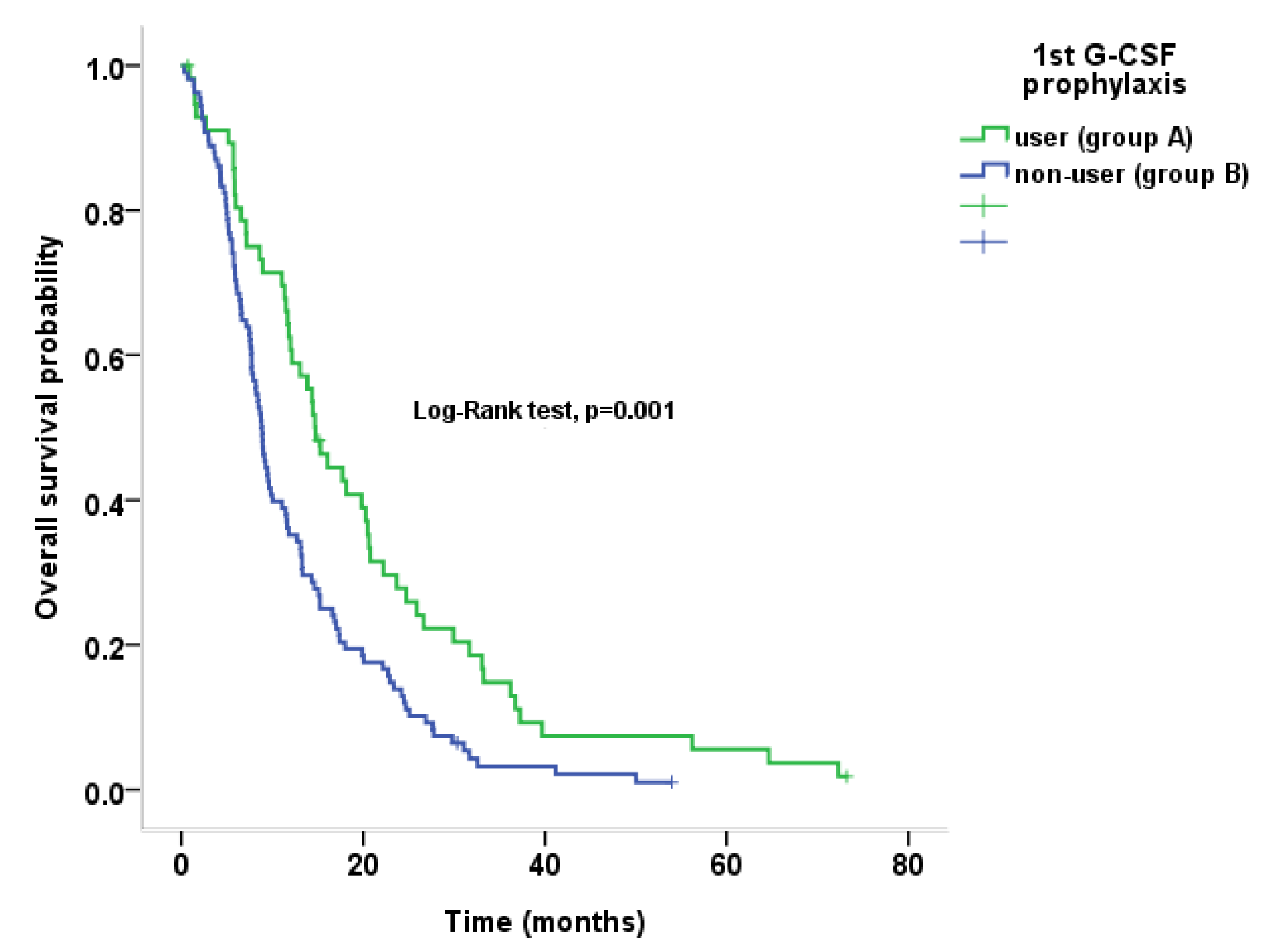
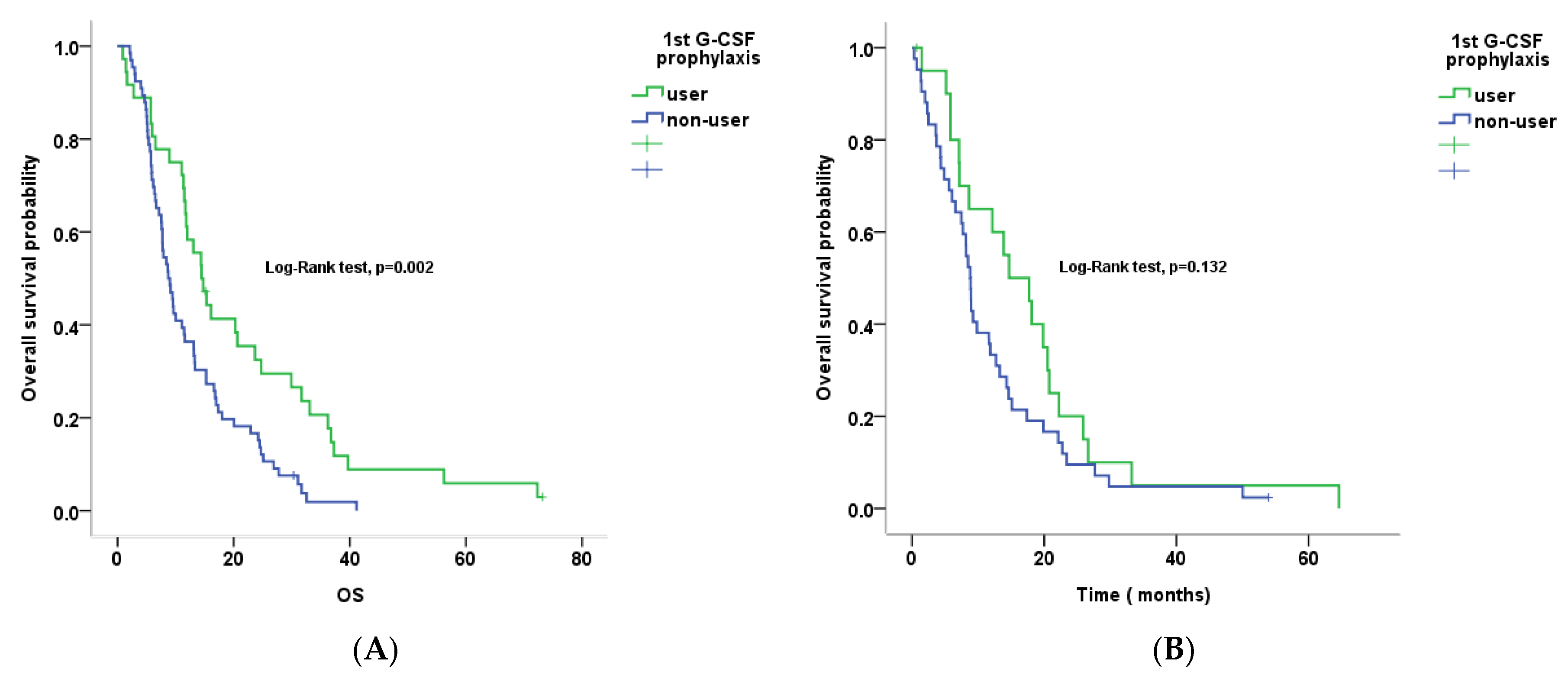
3.4. Primary G-CSF Prophylaxis and Clinical Outcomes by Age Group
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Gaduputi, V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J. Oncol. 2019, 10, 10–27. [Google Scholar] [CrossRef] [PubMed]
- Neoptolemos, J.P.; Kleeff, J.; Michl, P.; Costello, E.; Greenhalf, W.; Palmer, H.D. Therapeutic developments in pancreatic cancer: Current and future perspectives. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 333–348. [Google Scholar] [CrossRef] [PubMed]
- Perkhofer, L.; Ettrich, T.J.; Seufferlein, T. Pancreatic cancer: Progress in systemic therapy. Gastrointest. Tumors 2014, 1, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Desseigne, F.; Ychou, M.; Bouché, O.; Guimbaud, R.; Bécouarn, Y.; Adenis, A.; Raoul, J.L.; Gourgou-Bourgade, S.; de la Fouchardière, C.; et al. Folfirinox versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 2011, 364, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Hammel, P.; Hebbar, M.; Abdelghani, M.B.; Wei, A.C.; Raoul, J.L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. Folfirinox or gemcitabine as adjuvant therapy for pancreatic cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.F.; Li, G.J.; Zhao, H. Efficacy and toxicity of different chemotherapy regimens in the treatment of advanced or metastatic pancreatic cancer: A network Meta-analysis. J. Cell Biochem. 2018, 119, 511–523. [Google Scholar] [CrossRef]
- Chin, V.; Nagrial, A.; Sjoquist, K.; O’Connor, C.A.; Chantrill, L.; Biankin, A.V.; Scholten, R.J.; Yip, D. Chemotherapy and radiotherapy for advanced pancreatic cancer. Cochrane Database Syst. Rev. 2018, 3, Cd011044. [Google Scholar] [CrossRef]
- Ozaka, M.; Ishii, H.; Sato, T.; Ueno, M.; Ikeda, M.; Uesugi, K.; Sata, N.; Miyashita, K.; Mizuno, N.; Tsuji, K.; et al. A phase Ii study of modified folfirinox for chemotherapy-naïve patients with metastatic pancreatic cancer. Cancer Chemother. Pharmacol. 2018, 81, 1017–1023. [Google Scholar] [CrossRef]
- Yoshida, K.; Iwashita, T.; Uemura, S.; Maruta, A.; Okuno, M.; Ando, N.; Iwata, K.; Kawaguchi, J.; Mukai, T.; Shimizu, M. A multicenter prospective phase Ii study of first-line modified folfirinox for unresectable advanced pancreatic cancer. Oncotarget 2017, 8, 111346–111355. [Google Scholar] [CrossRef]
- Wang, Z.Q.; Zhang, F.; Deng, T.; Zhang, L.; Feng, F.; Wang, F.H.; Wang, W.; Wang, D.S.; Luo, H.Y.; Xu, R.H.; et al. The efficacy and safety of modified folfirinox as first-line chemotherapy for Chinese patients with metastatic pancreatic cancer. Cancer Commun. 2019, 39, 26. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, J.D.; Rogers, J.E.; Hess, K.R.; Wolff, R.A.; Varadhachary, G.R.; Javle, M.M.; Shroff, R.T.; Ho, L.; Fogelman, D.R.; Raghav, K.P.S.; et al. Modified folfirinox in pancreatic cancer patients age 75 or older. Pancreatology 2020, 20, 501–504. [Google Scholar] [CrossRef]
- Junior, U.P.L.S.; Rother, E.T.; Maluf, F.C.; Bugano, D.D.G. Meta-analysis of modified folfirinox regimens for patients with metastatic pancreatic cancer. Clin. Colorectal Cancer 2018, 17, 187–197. [Google Scholar] [CrossRef]
- Baldini, C.; Escande, A.; Bouché, O.; el Hajbi, F.; Volet, J.; Bourgeois, V.; Vantroys, T.R.; Ploquin, A.; Desauw, C.; Hebbar, M. Safety and efficacy of folfirinox in elderly patients with metastatic or locally advanced pancreatic adenocarcinoma: A retrospective analysis. Pancreatology 2017, 17, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Peter, H.; Macintyre, J.; Kawamura, C.; Maldonado, J.C.; Ernani, V.; Loaiza-Bonilla, A.; Narayanan, G.; Ribeiro, A.; Portelance, L.; Merchan, J.R. A retrospective study of neoadjuvant folfirinox in unresectable or borderline-resectable locally advanced pancreatic adenocarcinoma. BMC Cancer 2012, 12, 1–7. [Google Scholar]
- Moorcraft, S.Y.; Khan, K.; Peckitt, C.; Watkins, D.; Rao, S.; Cunningham, D.; Chau, I. FOLFRINOX for locally advanced or metastatic pancreatic ductal adenocarcinoma: The Royal Marsden experience. Clin. Colorectal Cancer 2014, 13, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Yau, L.; Nakov, R.; Krendyukov, A. Overall survival and risk of second malignancies with cancer chemotherapy and G-Csf support. Ann. Oncol. 2018, 29, 1903–1910. [Google Scholar] [CrossRef]
- Lyman, G.H.; Reiner, M.; Morrow, P.K.; Crawford, J. The effect of filgrastim or pegfilgrastim on survival outcomes of patients with cancer receiving myelosuppressive chemotherapy. Ann. Oncol. 2015, 26, 1452–1458. [Google Scholar] [CrossRef]
- Lyman, G.H.; Dale, D.C.; Culakova, E.; Poniewierski, M.S.; Wolff, D.A.; Kuderer, N.M.; Huang, M.; Crawford, J. The impact of the granulocyte colony-stimulating factor on chemotherapy dose intensity and cancer survival: A systematic review and meta-analysis of randomized controlled trials. Ann. Oncol. 2013, 24, 2475–2484. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Dale, D.C.; Crawford, J.; Lyman, G.H. Impact of primary prophylaxis with granulocyte colony-stimulating factor on febrile neutropenia and mortality in adult cancer patients receiving chemotherapy: A systematic review. J. Clin. Oncol. 2007, 25, 3158–3167. [Google Scholar] [CrossRef]
- Lalami, Y.; Klastersky, J. Impact of chemotherapy-induced neutropenia (CIN) and febrile neutropenia (FN) on cancer treatment outcomes: An overview about well-established and recently emerging clinical data. Crit. Rev. Oncol. Hematol. 2017, 120, 163–179. [Google Scholar] [CrossRef]
- Lee, J.C.; Kim, J.W.; Ahn, S.; Kim, H.W.; Lee, J.; Kim, Y.H.; Paik, K.H.; Kim, J.; Hwang, J.H. Optimal dose reduction of folfirinox for preserving tumour response in advanced pancreatic cancer: Using cumulative relative dose intensity. Eur. J. Cancer 2017, 76, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Sohal, D.P.S.; Kennedy, E.B.; Khorana, A.; Copur, M.S.; Crane, C.H.; Garrido-Laguna, I.; Krishnamurthi, S.; Moravek, C.; O’Reilly, E.M.; Philip, P.A.; et al. Metastatic pancreatic cancer: Asco clinical practice guideline update. J. Clin. Oncol. 2018, 36, 2545–2556. [Google Scholar] [CrossRef] [PubMed]
- Okusaka, T.; Ikeda, M.; Fukutomi, A.; Ioka, T.; Furuse, J.; Ohkawa, S.; Isayama, H.; Boku, N. Phase Ii study of folfirinox for chemotherapy-naïve Japanese patients with metastatic pancreatic cancer. Cancer Sci. 2014, 105, 1321–1326. [Google Scholar] [CrossRef]
- Muranaka, T.; Kuwatani, M.; Komatsu, Y.; Sawada, K.; Nakatsumi, H.; Kawamoto, Y.; Yuki, S.; Kubota, Y.; Kubo, K.; Kawahata, S.; et al. Comparison of efficacy and toxicity of folfirinox and gemcitabine with Nab-paclitaxel in unresectable pancreatic cancer. J. Gastrointest. Oncol. 2017, 8, 566–571. [Google Scholar] [CrossRef] [PubMed]
| Variables | 1st G-CSF User (n = 57) | 1st G-CSF Non-User (n = 108) | All Patients (n = 165) | p Value |
|---|---|---|---|---|
| Age, median (range, yr) | 61.1 (41–80) | 61.5 (29–79) | 61.4 (29–80) | 0.856 |
| Sex, no. (%) | 0.637 | |||
| Female | 19 (33.3) | 40 (37.0) | 59 (35.8) | |
| Male | 38 (66.7) | 68 (63.0) | 106 (64.2) | |
| BMI, median (range, kg/m2) | 23.3 (15.4–29.1) | 22.7 (15.0–29.3) | 23.0 (15.0–29.3) | 0.147 |
| ECOG performance status | 0.095 | |||
| 0–1 | 51 (89.5) | 104 (96.3) | 155 (93.9) | |
| 2 | 6 (10.5) | 4 (3.7) | 10 (6.1) | |
| Primary site, no. (%) | 0.098 | |||
| Head and neck | 20 (35.1) | 48 (44.4) | 68 (41.2) | |
| Body | 5 (8.8) | 19 (17.6) | 24 (14.5) | |
| Tail | 30 (52.6) | 39 (36.1) | 69 (41.8) | |
| Multicentric | 1 (1.8) | 2 (1.9) | 3 (1.8) | |
| Site of metastasis, no. (%) * | 0.874 | |||
| Liver | 38 (66.7) | 67 (62.0) | 105 (63.6) | |
| Peritoneal seeding | 13 (22.8) | 26 (24.1) | 39 (23.6) | |
| Distant lymph node | 17 (29.8) | 21 (19.4) | 38 (23.0) | |
| Lung | 12 (21.1) | 20 (18.5) | 32 (19.4) | |
| Others | 13 (22.8) | 21 (19.4) | 34 (20.6) | |
| Metastatic organ, no. (%) | 0.391 | |||
| 1 | 32 (56.1) | 72 (66.7) | 107 (64.8) | |
| 2 | 15 (26.3) | 23 (21.3) | 37 (22.4) | |
| ≥3 | 10 (17.5) | 13 (12.0) | 21 (13.3) | |
| Baseline laboratory values | ||||
| ANC, median (range, g/dL) | 4624 (840–11,297) | 4723 (1,331–12,178) | 4712(840–12,178) | 0.642 |
| Albumin, median (range, g/dL) | 4.1 (2.5–4.7) | 3.9 (2.4–5.0) | 3.9 (2.4–5.0) | 0.544 |
| CA19-9, median (range, U/mL) | 660.0 (5.0–20,000) | 380.0 (5–20,000) | 464.6 (5–20,000) | 0.138 |
| cRDI, median (range) | 80.6 (43.3–102.2) | 73.9 (28.3–109.0) | 76.3 (28.3–109.0) | 0.007 |
| Cycles, median (range) | 9.0 (1–75) | 6.0 (1–31) | 7.0 (1–75) | 0.004 |
| Grade 3–4 Toxicity | 1st G-CSF User (n = 57) | 1st G-CSF Non-User (n = 108) | All Patients (n = 165) | p Value |
|---|---|---|---|---|
| Hematologic | ||||
| Neutropenia | 18/57 (31.6) | 60/108 (55.6) | 78/165 (47.3) | 0.003 |
| Febrile neutropenia | 1/57 (1.8) | 20/108 (18.5) | 21/165 (12.7) | 0.002 |
| Anemia | 3/57 (5.3) | 17/108 (15.7) | 20/165 (12.1) | 0.050 |
| Thrombocytopenia | 2/57 (3.5) | 9/108 (8.3) | 11/165 (6.7) | 0.237 |
| Nonhematologic | ||||
| Fatigue | 1/56 (1.8) | 5/105 (4.8) | 6/161 (3.7) | 0.342 |
| Vomiting | 3/56 (5.4) | 13/105 (12.4) | 16/161 (9.9) | 0.156 |
| Diarrhea | 5/56 (8.9) | 7/105 (6.7) | 12/161 (7.5) | 0.603 |
| Sensory neuropathy | 0/56 (0.0) | 2/105 (1.9) | 2/161 (1.2) | 0.299 |
| Variables | Number of Patients (%) | OS (Median, Months) | 95%CI (Months) | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | p Value | HR | 95% CI | p Value | ||||
| Overall patients | 165 | 11.0 | 9.0–13.1 | ||||||
| Age | |||||||||
| <65 yr | 102 (62) | 11.4 | 9.3–13.5 | ||||||
| ≥65 yr | 63 (38) | 9.2 | 6.1–12.3 | 1.154 | 0.837–1.591 | 0.381 | |||
| Sex | |||||||||
| Female | 59 (36) | 11.6 | 7.8–15.3 | ||||||
| Male | 106 (64) | 9.5 | 6.6–12.3 | 1.297 | 0.936–1.797 | 0.118 | |||
| Albumin | |||||||||
| ≥3.5 g/dL | 124 (75) | 12.2 | 10.3–14.0 | ||||||
| <3.5 g/dL | 41 (25) | 6.5 | 4.3–8.7 | 1.864 | 1.295–2.683 | 0.001 | 1.718 | 1.223–2.412 | 0.002 |
| CA 19-9 | |||||||||
| <464.6 U/mL | 78 (50) | 13.0 | 10.9–15.2 | ||||||
| ≥464.6 U/mL | 78 (50) | 8.9 | 8.2–9.6 | 1.166 | 0.845–1.607 | 0.350 | |||
| Primary G-CSF prophylaxis | |||||||||
| Yes | 57 (35) | 14.7 | 12.0–17.4 | ||||||
| No | 108 (65) | 8.8 | 7.9–9.7 | 1.766 | 1.257–2.481 | 0.001 | 1.799 | 1.249–2.591 | 0.002 |
| Dose intensity (cRDI) | |||||||||
| ≥76.3 | 83 (50) | 11.6 | 8.1–15.2 | ||||||
| <76.3 | 82 (50) | 9.5 | 7.1–11.8 | 1.183 | 0.864–1.618 | 0.295 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, J.H.; Shin, D.W.; Kim, J.; Lee, J.-C.; Hwang, J.-H. Primary Granulocyte Colony-Stimulating Factor Prophylaxis in Metastatic Pancreatic Cancer Patients Treated with FOLFIRINOX as the First-Line Treatment. Cancers 2020, 12, 3137. https://doi.org/10.3390/cancers12113137
Jung JH, Shin DW, Kim J, Lee J-C, Hwang J-H. Primary Granulocyte Colony-Stimulating Factor Prophylaxis in Metastatic Pancreatic Cancer Patients Treated with FOLFIRINOX as the First-Line Treatment. Cancers. 2020; 12(11):3137. https://doi.org/10.3390/cancers12113137
Chicago/Turabian StyleJung, Jae Hyup, Dong Woo Shin, Jaihwan Kim, Jong-Chan Lee, and Jin-Hyeok Hwang. 2020. "Primary Granulocyte Colony-Stimulating Factor Prophylaxis in Metastatic Pancreatic Cancer Patients Treated with FOLFIRINOX as the First-Line Treatment" Cancers 12, no. 11: 3137. https://doi.org/10.3390/cancers12113137
APA StyleJung, J. H., Shin, D. W., Kim, J., Lee, J.-C., & Hwang, J.-H. (2020). Primary Granulocyte Colony-Stimulating Factor Prophylaxis in Metastatic Pancreatic Cancer Patients Treated with FOLFIRINOX as the First-Line Treatment. Cancers, 12(11), 3137. https://doi.org/10.3390/cancers12113137




