Ruxolitinib-Associated Infections in Polycythemia Vera: Review of the Literature, Clinical Significance, and Recommendations
Simple Summary
Abstract
1. Risk of Infections in Myeloproliferative Neoplasm (MPN)
2. Therapy Management of Polycythemia Vera and the Current Role of Ruxolitinib Treatment
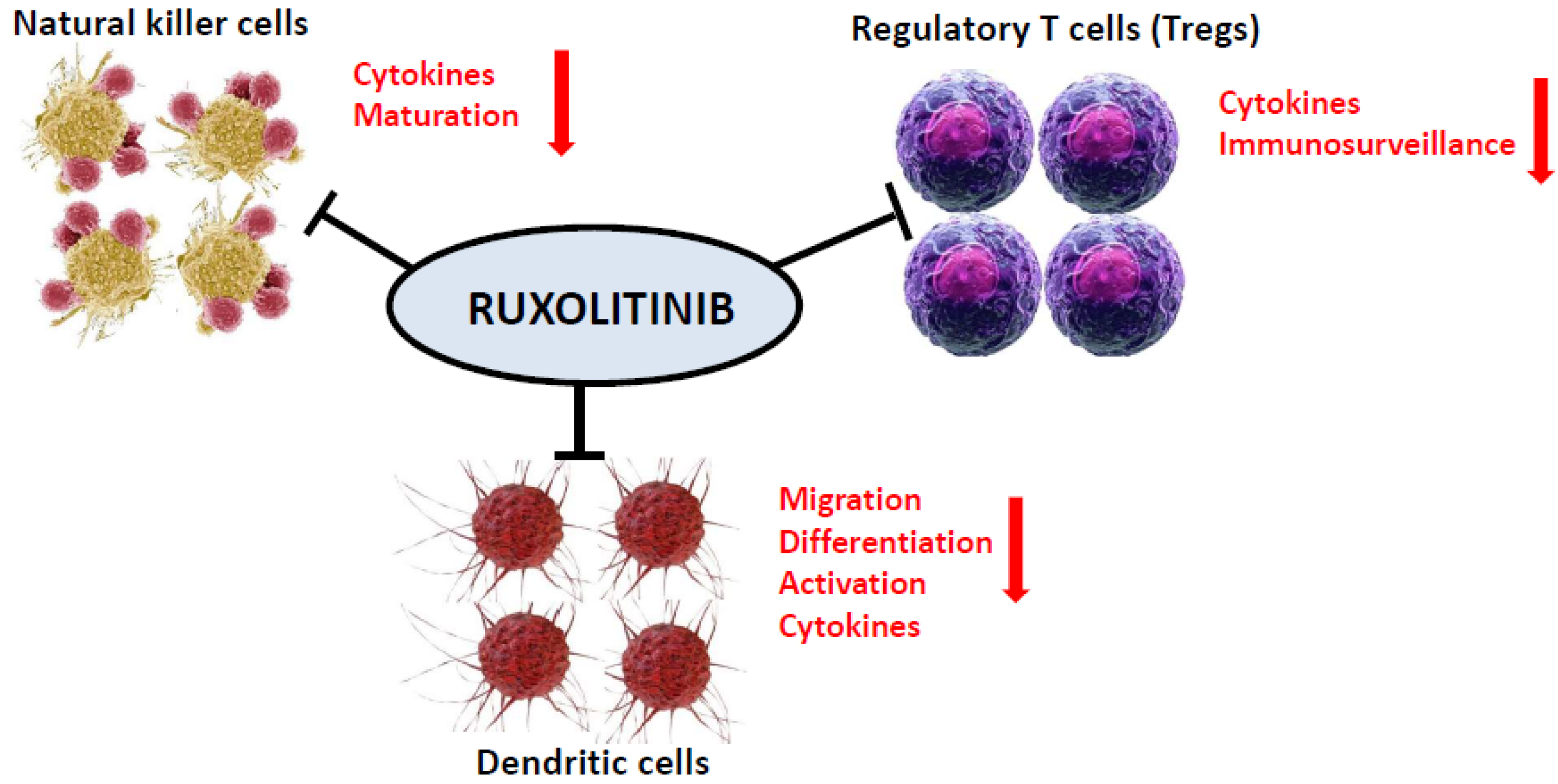
3. Mechanism of the Immunosuppressive Effect of JAK Inhibition
3.1. Dendritic Cells (DC)
3.2. Natural Killer (NK) Cells
3.3. T Regulatory (Treg) Cells
4. Infections in MPN Related to Ruxolitinib Treatment with a Special Focus on Polycythemia Vera
4.1. Infections Associated with Ruxolitinib in the COMFORT-I, COMFORT-II, and the JUMP Studies and in a Retrospective Analysis in Myelofibrosis
4.2. Infections Associated with Ruxolitinib in the RESPONSE and RELIEF Phase III Trials in Polycythemia Vera
4.3. Ruxolitinib-Associated Infections Reported in Literature Reviews or Case Reports in MPN
5. Ruxolitinib and COVID-19
6. Summary and Recommendations for Avoiding Complications from Ruxolitinib-Associated Infections with a Special Focus on Polycythemia Vera
7. Conclusions
Funding
Conflicts of Interest
References
- Hultcrantz, M.; Wilkes, S.R.; Kristinsson, S.Y.; Andersson, T.M.-L.; Derolf, Å.R.; Eloranta, S.; Samuelsson, J.; Landgren, O.; Dickman, P.W.; Lambert, P.C.; et al. Risk and cause of death in patients diagnosed with myeloproliferative neoplasms in Sweden between 1973 and 2005: A population-based study. J. Clin. Oncol. 2015, 33, 2288–2295. [Google Scholar] [CrossRef]
- Landtblom, A.R.; Andersson, T.M.L.; Dickman, P.W.; Smedby, K.E.; Eloranta, S.; Batyrbekova, N.; Samuelsson, J.; Björkholm, M.; Hultcrantz, M. Risk of Infections in Patients with Myeloproliferative Neoplasms-A Population-Based Cohort Study of 8363 Patients. Leukemia 2020. [Google Scholar] [CrossRef]
- Crodel, C.C.; Jentsch-Ullrich, K.; Koschmieder, S.; Kämpfe, D.; Griesshammer, M.; Döhner, K.; Jost, P.J.; Wolleschak, D.; Isfort, S.; Stegelmann, F.; et al. Frequency of infections in 948 MPN patients: A prospective multicenter patient-reported pilot study. Leukemia 2020, 34, 1949–1953. [Google Scholar] [CrossRef]
- Griesshammer, M.; Gisslinger, H.; Mesa, R. Current and future treatment options for polycythemia vera. Ann. Hematol. 2015, 94, 901–910. [Google Scholar] [CrossRef]
- Barbui, T.; Tefferi, A.; Vannucchi, A.M.; Passamonti, F.; Silver, R.T.; Hoffman, R.; Verstovsek, S.; Mesa, R.; Kiladjian, J.-J.; Hehlmann, R.; et al. Philadelphia chromosome-negative classical myeloproliferative neoplasms: Revised management recommendations from European LeukemiaNet. Leukemia 2018, 32, 1057–1069. [Google Scholar] [CrossRef]
- Griesshammer, M.; Sadjadian, P. The BCR-ABL1-negative myeloproliferative neoplasms: A review of JAK inhibitors in the therapeutic armamentarium. Expert Opin. Pharmacother. 2017, 18, 1929–1938. [Google Scholar] [CrossRef]
- Bose, P.; Verstovsek, S. JAK2 inhibitors for myeloproliferative neoplasms: What is next? Blood 2017, 130, 115–125. [Google Scholar] [CrossRef]
- Verstovsek, S.; Mesa, R.A.; Gotlib, J.; Levy, R.S.; Gupta, V.; DiPersio, J.F.; Catalano, J.V.; Deininger, M.; Miller, C.; Silver, R.T.; et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N. Engl. J. Med. 2012, 366, 799–807. [Google Scholar] [CrossRef]
- Harrison, C.; Kiladjian, J.J.; Al-Ali, H.K.; Gisslinger, H.; Waltzman, R.; Stalbovskaya, V.; McQuitty, M.; Hunter, D.S.; Levy, R.; Knoops, L.; et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N. Engl. J. Med. 2012, 366, 787–798. [Google Scholar] [CrossRef]
- Vannucchi, A.M.; Kiladjian, J.J.; Griesshammer, M.; Masszi, T.; Durrant, S.; Passamonti, F.; Harrison, C.N.; Pane, F.; Zachee, P.; Mesa, R.; et al. Ruxolitinib versus standard therapy for the treatment of polycythaemia vera. N. Engl. J. Med. 2015, 372, 426–435. [Google Scholar] [CrossRef]
- Passamonti, F.; Griesshammer, M.; Palandri, F.; Egyed, M.; Benevolo, G.; Devos, T.; Callum, J.; Vannucchi, A.M.; Sivgin, S.; Bensasson, C.; et al. Ruxolitinib for the treatment of inadequately controlled polycythaemia vera without splenomegaly (RESPONSE-2): A randomised, open-label, phase 3b study. Lancet Oncol. 2017, 18, 88–99. [Google Scholar] [CrossRef]
- Mesa, R.; Vannucchi, A.M.; Yacoub, A.; Zachee, P.; Garg, M.; Lyons, R.; Koschmieder, S.; Rinaldi, C.; Byrne, J.; Hasan, Y.; et al. The efficacy and safety of continued hydroxycarbamide therapy versus switching to ruxolitinib in patients with polycythaemia vera: A randomized, double-blind, double-dummy, symptom study (RELIEF). Br. J. Haematol. 2017, 176, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Curto-Garcia, N.; Baxter, J.; Harris, E.; McMullin, M.F.; Mead, A.; Yap, C.; Boucher, R.; Fox, S.; Harrison, C. Molecular analysis in MAJIC-PV correlation with clinical endpoints. EHA Libr. 2019, 267361, S1607. [Google Scholar] [CrossRef]
- Barosi, G.; Birgegard, G.; Finazzi, G.; Griesshammer, M.; Harrison, C.; Hasselbalch, H.; Kiladijan, J.-J.; Lengfelder, E.; Mesa, R.; Mc Mullin, M.F.; et al. A unified definition of clinical resistance and intolerance to hydroxycarbamide in polycythaemia vera and primary myelofibrosis: Results of a european LeukemiaNet (ELN) consensus process. Br. J. Haematol. 2010, 148, 961–963. [Google Scholar] [CrossRef] [PubMed]
- Leonard, W.J. Type I cytokines and interferons. In Fundamental Immunology, 4th ed.; Lippincott Raven: Philadelphia, PA, USA, 1997. [Google Scholar]
- Leonard, W.J.; Shores, E.W.; Love, P.E. Role of the common cytokine receptor gamma chain in cytokine signaling and lymphoid development. Immunol. Rev. 1995, 148, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Ghoreschi, K.; Laurence, A.; O’Shea, J.J. Janus kinases in immune cell signalling. Immunol. Rev. 2009, 228, 273–287. [Google Scholar] [CrossRef]
- McLornan, D.P.; Khan, A.A.; Harrison, C.N. Immunological Consequences of JAK Inhibition: Friend or Foe? Curr. Hematol. Malig. Rep. 2015, 10, 370–379. [Google Scholar] [CrossRef]
- Parampalli, Y.S.; Stübig, T.; Cornez, I.; Alchalby, H.; Schönberg, K.; Rudolph, J.; Triviai, I.; Wolschke, C.; Heine, A.; Brossart, P.; et al. JAK1/2 inhibition impairs T cell function in vitro and in patients with myeloproliferative neoplasms. Br. J. Haematol. 2015, 169, 824–833. [Google Scholar] [CrossRef]
- Elli, E.M.; Baratè, C.; Mendicino, F.; Palandri, F.; Palumbo, G.A. Mechanisms Underlying the Anti-inflammatory and Immunosuppressive Activity of Ruxolitinib. Front. Oncol. 2019, 9, 1186. [Google Scholar] [CrossRef]
- Heine, A.; Held, S.A.; Daecke, S.N.; Wallner, S.; Yajnanarayana, S.P.; Kurts, C.; Wolf, D.; Brossart, P. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood 2013, 122, 1192–1202. [Google Scholar] [CrossRef]
- Rudolph, J.; Heine, A.; Quast, T.; Kolanus, W.; Trebicka, J.; Brossart, P.; Wolf, D. The JAK inhibitor ruxolitinib impairs dendritic cell migration via off-target inhibition of ROCK. Leukemia 2016, 30, 2119–2123. [Google Scholar] [CrossRef]
- Schönberg, K.; Rudolph, J.; Vonnahme, M.; Yajnanarayana, S.P.; Cornez, I.; Hejazi, M.; Manser, A.R.; Uhrberg, M.; Verbeek, W.; Koschmieder, S.; et al. JAK inhibition impairs NK cell function in myeloproliferative neoplasms. Cancer Res. 2015, 75, 2187–2199. [Google Scholar] [CrossRef] [PubMed]
- Massa, M.; Rosti, V.; Campanelli, R.; Fois, G.; Barosi, G. Rapid and long-lasting decrease of T-regulatory cells in patients with myelofibrosis treated with ruxolitinib. Leukemia 2014, 28, 449–451. [Google Scholar] [CrossRef]
- Keohane, C.; Kordasti, S.Y.; Seidl, T.; Abellan, P.P.; Thomas, N.S.B.; Harrison, C.N.; McLornan, D.P.; Mufti, G.J. JAK inhibition induces silencing of T helper cytokine secretion and a profound reduction in T regulatory cells. BJM 2015, 171, 60–73. [Google Scholar] [CrossRef]
- Zeiser, R.; von Bubnoff, N.; Butler, J.; Mohty, M.; Niederwieser, D.; Or, R.; Szer, J.; Wagner, E.M.; Zuckerman, T.; Mahuzier, B.; et al. Ruxolitinib for glucocorticoid-refractory acute graft versus-host disease. N. Engl. J. Med. 2020, 382, 1800–1810. [Google Scholar] [CrossRef]
- Vannucchi, A.M.; Sordi, B.; Morettini, A.; Nozzoli, C.; Poggesi, L.; Pieralli, F.; Bartoloni, A.; Atanasio, A.; Miselli, F.; Paoli, C.; et al. Compassionate use of JAk1/2 inhibitor ruxolitinib for severe COVID-19: A prospective observational trial. Leukemia 2020, 1–13. [Google Scholar] [CrossRef]
- Verstovsek, S.; Mesa, R.A.; Gotlib, J.; Levy, R.S.; Gupta, V.; DiPersio, J.F.; Catalano, J.V.; Deininger, M.W.N.; Miller, C.B.; Silver, R.T.; et al. Efficacy, safety, and survival with ruxolitinib in patients with myelofibrosis: Results of a median 3-year follow-up of COMFORT-I. Haematologica 2015, 100, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.N.; Vannucchi, A.M.; Kiladjian, J.J.; Al-Ali, H.K.; Gisslinger, H.; Knoops, L.; Cervantes, F.; Jones, M.M.; Sun, K.; McQuitty, M.; et al. Long-term findings from COMFORT-II, a phase 3 study of ruxolitinib vs. best available therapy for myelofibrosis. Leukemia 2016, 30, 1701–1707. [Google Scholar] [CrossRef]
- Al-Ali, H.K.; Griesshammer, M.; le Coutre, P.; Waller, C.F.; Liberati, A.M.; Schafhausen, P.; Tavares, R.; Giraldo, P.; Foltz, L.; Raanani, P.; et al. Safety and efficacy of ruxolitinib in an open-label, multicenter, single-arm phase 3b expanded-access study in patients with myelofibrosis: A snapshot of 1144 patients in the JUMP trial. Haematologica 2016, 101, 1065–1073. [Google Scholar] [CrossRef]
- Polverelli, N.; Breccia, M.; Benevolo, G.; Martino, B.; Tieghi, A.; Latagliata, R.; Sabattini, E.; Riminucci, M.; Godio, L.; Catani, L.; et al. Risk factors for infections in myelofibrosis: Role of disease status and treatment. A multicenter study of 507 patients. Am. J. Hematol. 2017, 92, 37–41. [Google Scholar] [CrossRef]
- Verstovsek, S.; Vannucchi, A.M.; Griesshammer, M.; Masszi, T.; Durrant, S.; Passamonti, F.; Harrison, C.N.; Pane, F.; Zachee, P.; Kirito, K.; et al. Ruxolitinib versus best available therapy in patients with polycythemia vera: 80-week follow-up from the RESPONSE trial. Haematologica 2016, 101, 821–829. [Google Scholar] [CrossRef]
- Kiladjian, J.J.; Zachee, P.; Hino, M.; Pane, F.; Masszi, T.; Harrison, C.N.; Mesa, R.; Miller, C.B.; Passamonti, F.; Durrant, S.; et al. Long-term efficacy and safety of ruxolitinib versus best available therapy in polycythaemia vera (RESPONSE): 5-year follow up of a phase 3 study. Lancet Haematol. 2020, 7, e226–e237. [Google Scholar] [CrossRef]
- Griesshammer, M.; Saydam, G.; Palandri, F.; Benevolo, G.; Egyed, M.; Callum, J.; Devos, T.; Sivgin, S.; Guglielmelli, P.; Bensasson, C.; et al. Ruxolitinib for the treatment of inadequately controlled polycythemia vera without splenomegaly: 80-week follow-up from the RESPONSE-2 trial. Ann. Hematol. 2018, 97, 1591–1600. [Google Scholar] [CrossRef]
- Lussana, F.; Cattaneo, M.; Rambaldi, A.; Squizzato, A. Ruxolitinib-associated infections: A systematic review and meta-analysis. Am. J. Hematol. 2018, 93, 339–347. [Google Scholar] [CrossRef]
- Caocci, G.; Murgia, F.; Podda, L.; Solinas, A.; Atzeni, S.; La Nasa, G. Reactivation of hepatitis B virus infection following ruxolitinib treatment in a patient with myelofibrosis. Leukemia 2014, 28, 225–227. [Google Scholar] [CrossRef]
- Chen, C.C.; Chen, Y.Y.; Huang, C.E. Cryptococcal meningoencephalitis associated with the long-term use of ruxolitinib. Ann. Hematol. 2016, 95, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Lee, C.H.; Pei, S.N. Pulmonary tuberculosis reactivation following ruxolitinib treatment in a patient with primary myelofibrosis. Leuk. Lymphoma 2015, 56, 1528–1529. [Google Scholar] [CrossRef]
- Colomba, C.; Rubino, R.; Siracusa, L.; Lalicata, F.; Trizzino, M.; Titone, L.; Tolomeo, M. Disseminated tuberculosis in a patient treated with a JAK2 selective inhibitor: A case report. BMC Res. Notes 2012, 5, 552. [Google Scholar] [CrossRef]
- Eyal, O.; Flaschner, M.; Yehuda, A.B.; Rund, D. Varicella-zoster virus meningoencephalitis in a patient treated with ruxolitinib. Am. J. Hematol. 2017, 92, E74–E75. [Google Scholar] [CrossRef]
- Goldberg, R.A.; Reichel, E.; Oshry, L.J. Bilateral toxoplasmosis retinitis associated with ruxolitinib. N. Engl. J. Med. 2013, 369, 681–683. [Google Scholar] [CrossRef]
- Hopman, R.K.; Lawrence, S.J.; Oh, S.T. Disseminated tuberculosis associated with ruxolitinib. Leukemia. 2014, 28, 1750–1751. [Google Scholar] [CrossRef] [PubMed]
- Hirano, A.; Yamasaki, M.; Saito, N.; Iwato, K.; Daido, W.; Funaishi, K.; Ishiyama, S.; Deguchi, N.; Taniwaki, M.; Ohashi, N. Pulmonary cryptococcosis in a ruxolitinib-treated patient with primary myelofibrosis. Respir. Med. Case Rep. 2017, 22, 87–90. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Lee, S.R.; Park, Y.; Choi, C.W.; Kim, S.J.; Yhim, H.-Y.; Kim, I.; Oh, D.; Mun, Y.-C.; Lim, S.-N. Efficacy of ruxolitinib in Korean myelofibrosis patients and cases complicated TB lymphadenitis during the treatment. Blood 2013, 122, 1596. [Google Scholar] [CrossRef]
- Kinoshita, M.; Ogawa, Y.; Kawamura, T.; Kirito, K.; Shimada, S. Case of disseminated molluscum contagiosum caused by ruxolitinib, a Janus kinase 1 and 2 inhibitor. J. Dermatol. 2016, 43, 1387–1388. [Google Scholar] [CrossRef]
- Kirito, K.; Sakamoto, M.; Enomoto, N. Elevation of the Hepatitis B Virus DNA during the Treatment of Polycythemia Vera with the JAK Kinase Inhibitor Ruxolitinib. Intern. Med. 2016, 55, 1341–1344. [Google Scholar] [CrossRef]
- Knödler, A.; Schmiedel, S.; Schäfer, G.; Bokemeyer, C.; von Amsberg, G. Pneumocystis jirovecii pneumonia associated with Ruxolitinib therapy in a patient with myelofibrosis. Oncol. Res. Treat. 2014, 37, 164–165. [Google Scholar]
- Kusano, Y.; Terui, Y.; Ueda, K.; Hatake, K. Epstein-Barr virus gastric ulcer associated with ruxolitinib. Ann. Hematol. 2016, 95, 1741–1742. [Google Scholar] [CrossRef] [PubMed]
- Kusano, Y.; Terui, Y.; Ueda, K.; Hatake, K. Klebsiella pneumoniae primary liver abscess associated with ruxolitinib. Ann. Hematol. 2016, 95, 1561–1562. [Google Scholar] [CrossRef]
- Landman, G.W.; Arend, S.M.; van Dissel, J.T. Ruxolitinib can mask symptoms and signs of necrotizing fasciitis. J. Infect. 2013, 66, 296–297. [Google Scholar] [CrossRef]
- Malkan, U.Y.; Haznedaroglu, I.C. A myelofibrosis case that develops mycobacterial infection after ruxolitinib treatment. Int. J. Clin. Exp. Med. 2017, 10, 7304–7307. [Google Scholar]
- Palandri, F.; Polverelli, N.; Catani, L.; Vianelli, L. Ruxolitinib-associated tuberculosis: A case of successful ruxolitinib rechallenge. Ann. Hematol. 2015, 94, 519–520. [Google Scholar] [CrossRef]
- Perricone, G.; Vinci, M.; Pungolino, E. Occult hepatitis B infection reactivation after ruxolitinib therapy. Dig. Liver Dis. 2017, 49, 719. [Google Scholar] [CrossRef] [PubMed]
- Tong, L.X.; Jackson, J.; Kerstetter, J.; Worswick, S.D. Reactivation of herpes simplex virus infection in a patient undergoing ruxolitinib treatment. J. Am. Acad. Dermatol. 2014, 70, e59–e60. [Google Scholar] [CrossRef] [PubMed]
- von Hofsten, J.; Johnsson Forsberg, M.; Zetterberg, M. Cytomegalovirus retinitis in a patient who received ruxolitinib. N. Engl. J. Med. 2016, 374, 296–297. [Google Scholar] [CrossRef]
- Wathes, R.; Moule, S.; Milojkovic, D. Progressive multifocal leukoencephalopathy associated with ruxolitinib. N. Engl. J. Med. 2013, 369, 197–198. [Google Scholar] [CrossRef]
- Wysham, N.G.; Sullivan, D.R.; Allada, G. An opportunistic infection associated with ruxolitinib, a novel Janus kinase 1,2 inhibitor. Chest 2013, 143, 1478–1479. [Google Scholar] [CrossRef]
- Keizer, S.; Gerritsen, R.; Jauw, Y.; Janssen, J.; Koopman, B.; Bresser, P. Fatal tuberculosis during treatment with ruxolitinib. Ned. Tijdschr. Geneeskd. 2015, 159, A8650. [Google Scholar]
- Chan, J.F.; Chan, T.S.; Gill, H.; Lam, F.Y.F.; Trendell-Smith, N.J.; Sridhar, S.; Tse, H.; Lau, S.K.P.; Hung, I.F.N.; Yuen, K.Y.; et al. Disseminated infections with talaromyces marneffei in non-AIDS patients given monoclonal antibodies against CD20 and kinase inhibitors. Emerg. Infect. Dis. 2015, 21, 1101–1106. [Google Scholar] [CrossRef]
- Branco, B.; Metsu, D.; Dutertre, M.; Marchou, B.; Delobel, P.; Recher, C.; Martin-Blondel, G. Use of rifampin for treatment of disseminated tuberculosis in a patient with primary myelofibrosis on ruxolitinib. Ann. Hematol. 2016, 95, 1207–1209. [Google Scholar] [CrossRef] [PubMed]
- Palmason, R.; Linden, O.; Richter, J. Case-report: EBV driven lymphoproliferative disorder associated with Ruxolitinib. BMC Hematol. 2015, 15, 10. [Google Scholar] [CrossRef]
- Shen, C.H.; Hwang, C.E.; Chen, Y.Y.; Chen, C.-C. Hepatitis B virus reactivation associated with ruxolitinib. Ann. Hematol. 2014, 93, 1075–1076. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Feenstra, J.; Georghiou, P.R. Pneumocystis jiroveci pneumonitis complicating ruxolitinib therapy. BMJ Case Rep. 2014, 2014, bcr2014204950. [Google Scholar] [CrossRef] [PubMed]
- Dioverti, M.V.; Abu Saleh, O.M.; Tande, A.J. Infectious complications in patients on treatment with Ruxolitinib: Case report and review of the literature. Infect. Dis. 2018, 50, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Sylvine, P.; Thomas, S.; Pirayeh, E. Infections associated with ruxolitinib: Study in the French Pharmacovigilance database. Ann. Hematol. 2018, 97, 913–914. [Google Scholar] [CrossRef]
- Anand, K.; Burns, E.A.; Ensor, J.; Rice, L.; Pingali, S.R. Mycobacterial Infections with Ruxolitinib: A Retrospective Pharmacovigilance Review. Clin. Lymphoma Myeloma Leuk. 2020, 20, 18–23. [Google Scholar] [CrossRef]
- Lescuyer, S.; Ledoux, M.P.; Gravier, S.; Natarajan-Ame, S.; Duval, C.; Maloisel, F.; Mauvieux, L.; Toussaint, E.; Fornecker, L.-M.; Herbrecht, R. Tuberculosis and atypical mycobacterial infections in ruxolitinib-treated patients with primary or secondary myelofibrosis or polycythemia vera. Int. J. Infect. Dis. 2019, 80, 134–136. [Google Scholar] [CrossRef]
- La Rosee, F.; Bremer, H.C.; Gehrke, I.; Kehr, A.; Hochhaus, A.; Birndt, S.; Felhauer, M.; Henkes, M.; Kumle, B.; Russo, S.G. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia 2020, 34, 1805–1815. [Google Scholar] [CrossRef]
- Breccia, M.; Piciocchi, A.; DeStefano, V.; Finazzi, G.; Iurlo, A.; Fazi, P.; Soddu, S.; Martino, B.; Palandri, F.; Siragusa, S. COVID-19 in Philadelphia-negative myeloproliferative disorders: A GIMEMA survey. Leukemia 2020. [Google Scholar] [CrossRef]
- Maschmeyer, G.; De Greef, J.; Mellinghoff, S.C.; Nosari, A.; Thiebot-Bertrand, A.; Bergeron, A.; Franquet, T.; Blijlevens, N.M.A.; Maertens, J.A. Infections associated with immunotherapeutic and molecular targeted agents in hematology and oncology. A position paper by the European Conference on Infections in Leukemia (ECIL). Leukemia 2019, 33, 844–862. [Google Scholar] [CrossRef]
- Reinwald, M.; Silva, J.T.; Mueller, N.J.; Fortun, J.; Garzoni, C.; de Fijter, J.W.; Fernandez-Ruiz, M.; Grossi, P.; Aguado, J.M. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: An infectious diseases perspective (Intracellular signalling pathways: Tyrosine kinase and mTOR inhibitors). Clin. Microbiol. Infect. 2018, 24, 53–70. [Google Scholar] [CrossRef]
- Sant’Antonio, E.; Bonifacio, M.; Breccia, M.; Rumi, E. A journey through infectious risk associated with ruxolitinib. Br. J. Haematol. 2019, 187, 286–295. [Google Scholar] [CrossRef]
- Alimam, S.; Harrison, C. Experience with ruxolitinib in the treatment of polycythaemia vera. Ther. Adv. Hematol. 2017, 8, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Impfkommission, S. Empfehlungen der Ständigen Impfkommission (STIKO) am Robert Koch-Institut. Epid. Bull. 2019, 34, 313–364. [Google Scholar]
| Infectious Complication | MPN Subtype | References |
|---|---|---|
| Tuberculosis | PMF | [38,39,42,44,51,52,58,60] |
| Hepatitis B | PMF | [36,53] |
| post-ET myelofibrosis | [62] | |
| PV | [46] | |
| Cryptococcal meningoencephalitis | PMF | [37,64] |
| VZV meningoencephalitis | PV | [40] |
| Toxoplasmosis retinitis | PV | [41] |
| Pulmonary cryptococcosis | post-PV myelofibrosis | [57] |
| PMF | [43] | |
| Molluscum contagiosum | PV | [45] |
| Pneumocystis jirovecii pneumonia | PMF | [47,63,64] |
| EBV gastric ulcer | PMF | [48] |
| Klebsiella pneumonia liver abscess | PMF | [49] |
| Herpes simplex reactivation | MDS | [54] |
| Cytomegalovirus retinitis | PMF | [55] |
| Progressive multifocal leukoencephalopathy | PMF | [56] |
| Talaromyces marneffei infection | PMF | [59] |
| EBV driven lymphoproliferative disorder | post-PV myelofibrosis | [61] |
| Recommended Actions/Tests | In Detail |
|---|---|
| Accurate history taking at the start and physical examination | Identify risk groups for infections like tuberculosis, identify other reasons for immunosuppression, and identify co-medication [70,71]. |
| Baseline virology | Hepatitis B [70,71]. No consensus in favor of routine testing for HCV and HIV. |
| Hepatitis B screening | Includes HBsAg, anti-HBs, and anti-HBc [70]. If anti-HBc is positive, determine HBV-DNA [72]. |
| Test in hepatitis B virus carriers | Close monitoring of liver function and plasma HBV-DNA level. Referral to a specialist [70]. |
| Test, if tuberculosis is suspected | Tuberculin Skin Test (TST) or (preferably) IFN-γ Release Assay, IGRA (i.e., Quanti-FERON test) [70,72]. |
| Vaccination | Age-appropriate vaccination against influenza, herpes zoster, and pneumococci [3,74]. Vaccination against meningococcal infection in patients with pre-existing comorbidity or the immune system *. |
| Varicella zoster virus (VZV) | No primary but secondary prophylaxis in individual cases. Inform and educate patients to seek immediate medical attention if signs of cutaneous herpes zoster develop [72]. VZV reactivation: consider vaccination against VZV with inactivated vaccine. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sadjadian, P.; Wille, K.; Griesshammer, M. Ruxolitinib-Associated Infections in Polycythemia Vera: Review of the Literature, Clinical Significance, and Recommendations. Cancers 2020, 12, 3132. https://doi.org/10.3390/cancers12113132
Sadjadian P, Wille K, Griesshammer M. Ruxolitinib-Associated Infections in Polycythemia Vera: Review of the Literature, Clinical Significance, and Recommendations. Cancers. 2020; 12(11):3132. https://doi.org/10.3390/cancers12113132
Chicago/Turabian StyleSadjadian, Parvis, Kai Wille, and Martin Griesshammer. 2020. "Ruxolitinib-Associated Infections in Polycythemia Vera: Review of the Literature, Clinical Significance, and Recommendations" Cancers 12, no. 11: 3132. https://doi.org/10.3390/cancers12113132
APA StyleSadjadian, P., Wille, K., & Griesshammer, M. (2020). Ruxolitinib-Associated Infections in Polycythemia Vera: Review of the Literature, Clinical Significance, and Recommendations. Cancers, 12(11), 3132. https://doi.org/10.3390/cancers12113132





