Multiple Myeloma and Thrombosis: Prophylaxis and Risk Prediction Tools
Abstract
1. Introduction
2. Understanding the Complex Procoagulant Profile of the MM Patient
2.1. Patient-Related Risk Factors
2.2. Disease-Specific Risk Factors and the Search for a Biomarker
2.3. Treatment-Related Risk Factors
3. Risk Assessment Tools
3.1. Guidelines and Clinical Practice
3.2. Risk Assessment Models
4. Thromboprophylaxis: To DOAC or Not To DOAC?
5. Conclusions and Recommendations
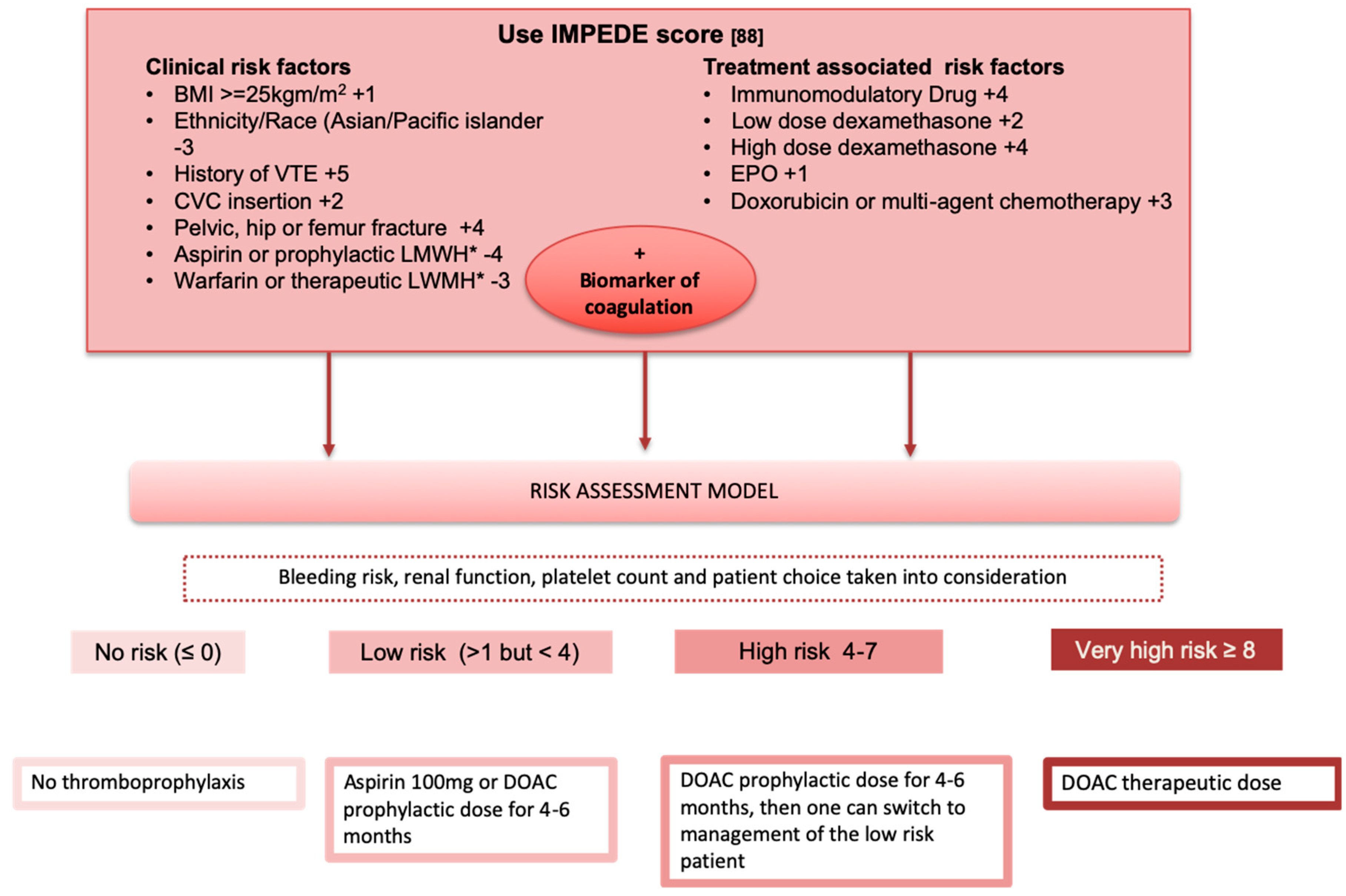
Potential Algorithm for Risk Stratification of Patients
Funding
Conflicts of Interest
References
- Cesarman-Maus, G.; Braggio, E.; Fonseca, R. Thrombosis in multiple myeloma (MM). Hematology 2012, 17 (Suppl. 1), S177–S180. [Google Scholar] [CrossRef] [PubMed]
- Falanga, A.; Marchetti, M. Venous thromboembolism in the hematologic malignancies. J. Clin. Oncol. 2009, 27, 4848–4857. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, V.; Za, T.; Rossi, E. Venous thromboembolism in multiple myeloma. Semin. Thromb. Hemost. 2014, 40, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Kristinsson, S.Y. Thrombosis in multiple myeloma. Hematol. Am. Soc. Hematol. Educ. Program 2010, 2010, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Leleu, X.; Rodon, P.; Hulin, C.; Daley, L.; Dauriac, C.; Hacini, M.; Decaux, O.; Eisemann, J.C.; Fitoussi, O.; Lioure, B.; et al. MELISSE, a large multicentric observational study to determine risk factors of venous thromboembolism in patients with multiple myeloma treated with immunomodulatory drugs. Thromb. Haemost. 2013, 110, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Kristinsson, S.Y.; Pfeiffer, R.M.; Bjorkholm, M.; Schulman, S.; Landgren, O. Thrombosis is associated with inferior survival in multiple myeloma. Haematologica 2012, 97, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Schoen, M.W.; Luo, S.; Gage, B.; Carson, K.R.; Sanfilippo, K.M. Association of venous thromboembolism with increased mortality in patients with multiple myeloma. J. Clin. Oncol. 2018. [Google Scholar] [CrossRef]
- Khorana, A.A.; Dalal, M.R.; Lin, J.; Connolly, G.C. Health care costs associated with venous thromboembolism in selected high-risk ambulatory patients with solid tumors undergoing chemotherapy in the United States. Clin. Outcomes Res. 2013, 5, 101–108. [Google Scholar] [CrossRef]
- Lee, A.Y. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J. Clin. Oncol. 2009, 27, 4895–4901. [Google Scholar] [CrossRef]
- Rajkumar, S.V. Value and Cost of Myeloma Therapy. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 662–666. [Google Scholar] [CrossRef]
- Huang, H.; Li, H.; Li, D. Effect of serum monoclonal protein concentration on haemostasis in patients with multiple myeloma. Blood Coagul. Fibrinolysis 2015, 26, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Kwaan, H.C. Hyperviscosity in plasma cell dyscrasias. Clin. Hemorheol. Microcirc. 2013, 55, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, A.; Rajkumar, S.V.; San Miguel, J.F.; Larocca, A.; Niesvizky, R.; Morgan, G.; Landgren, O.; Hajek, R.; Einsele, H.; Anderson, K.C.; et al. International Myeloma Working Group consensus statement for the management, treatment, and supportive care of patients with myeloma not eligible for standard autologous stem-cell transplantation. J. Clin. Oncol. 2014, 32, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Kleber, M.; Engelhardt, M.; Zweegman, S.; Gay, F.; Kastritis, E.; van de Donk, N.W.; Bruno, B.; Sezer, O.; Broijl, A.; et al. European Myeloma Network guidelines for the management of multiple myeloma-related complications. Haematologica 2015, 100, 1254–1266. [Google Scholar] [CrossRef]
- Palumbo, A.; Rajkumar, S.V.; Dimopoulos, M.A.; Richardson, P.G.; San Miguel, J.; Barlogie, B.; Harousseau, J.; Zonder, J.A.; Cavo, M.; Zangari, M.; et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia 2008, 22, 414–423. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Leleu, X.; Palumbo, A.; Moreau, P.; Delforge, M.; Cavo, M.; Ludwig, H.; Morgan, G.J.; Davies, F.E.; Sonneveld, P.; et al. Expert panel consensus statement on the optimal use of pomalidomide in relapsed and refractory multiple myeloma. Leukemia 2014, 28, 1573–1585. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Palumbo, A.; Attal, M.; Beksac, M.; Davies, F.E.; Delforge, M.; Einsele, H.; Hajek, R.; Harousseau, J.L.; da Costa, F.L.; et al. Optimizing the use of lenalidomide in relapsed or refractory multiple myeloma: Consensus statement. Leukemia 2011, 25, 749–760. [Google Scholar] [CrossRef]
- Palumbo, A.; Cavo, M.; Bringhen, S.; Zamagni, E.; Romano, A.; Patriarca, F.; Rossi, D.; Gentilini, F.; Crippa, C.; Galli, M.; et al. Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: A phase III, open-label, randomized trial. J. Clin. Oncol. 2011, 29, 986–993. [Google Scholar] [CrossRef]
- Larocca, A.; Cavallo, F.; Bringhen, S.; Di Raimondo, F.; Falanga, A.; Evangelista, A.; Cavalli, M.; Stanevsky, A.; Corradini, P.; Pezzatti, S.; et al. Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood 2012, 119, 933–939. [Google Scholar] [CrossRef]
- Fotiou, D.; Gerotziafas, G.; Kastritis, E.; Dimopoulos, M.A.; Terpos, E. A review of the venous thrombotic issues associated with multiple myeloma. Expert Rev. Hematol. 2016, 9, 695–706. [Google Scholar] [CrossRef]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Cancer-Associated Venous Thromboembolic Disease. Available online: www.nccn.org/professionals/physician_gls/pdf/vte.pdf (accessed on 12 December 2019).
- Baker, H.A.; Brown, A.R.; Mahnken, J.D.; Shireman, T.I.; Webb, C.E.; Lipe, B.C. Application of risk factors for venous thromboembolism in patients with multiple myeloma starting chemotherapy, a real-world evaluation. Cancer Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Paludo, J.; Mikhael, J.R.; LaPlant, B.R.; Halvorson, A.E.; Kumar, S.; Gertz, M.A.; Hayman, S.R.; Buadi, F.K.; Dispenzieri, A.; Lust, J.A.; et al. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed lenalidomide-refractory multiple myeloma. Blood 2017, 130, 1198–1204. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, C. Thrombotic Events in Patients with Myeloma Treated with Immunomodulatory Drugs; Results of the Myeloma XI Study. Blood 2017, 130, 553. [Google Scholar]
- Ay, C.; Dunkler, D.; Simanek, R.; Thaler, J.; Koder, S.; Marosi, C.; Zielinski, C.; Pabinger, I. Prediction of venous thromboembolism in patients with cancer by measuring thrombin generation: Results from the Vienna Cancer and Thrombosis Study. J. Clin. Oncol. 2011, 29, 2099–2103. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D.; Adams, V.R. Incidence and Risk Factors of Thromboembolism with Multiple Myeloma in the Presence of Death as a Competing Risk: An Empirical Comparison of Statistical Methodologies. Healthcare 2016, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Bagratuni, T.; Kastritis, E.; Politou, M.; Roussou, M.; Kostouros, E.; Gavriatopoulou, M.; Eleutherakis-Papaiakovou, E.; Kanelias, N.; Terpos, E.; Dimopoulos, M.A. Clinical and genetic factors associated with venous thromboembolism in myeloma patients treated with lenalidomide-based regimens. Am. J. Hematol. 2013, 88, 765–770. [Google Scholar] [CrossRef]
- Anaissie, E.J.; Coleman, E.A.; Goodwin, J.A.; Kennedy, R.L.; Lockhart, K.D.; Stewart, C.B.; Coon, S.K.; Bailey, C.; Barlogie, B. Prophylactic recombinant erythropoietin therapy and thalidomide are predictors of venous thromboembolism in patients with multiple myeloma: Limited effectiveness of thromboprophylaxis. Cancer 2012, 118, 549–557. [Google Scholar] [CrossRef]
- Chalayer, E.; Tardy-Poncet, B.; Karlin, L.; Chapelle, C.; Montmartin, A.; Piot, M.; Guyotat, D.; Collet, P.; Lecompte, T.; Tardy, B. Thrombin generation in newly diagnosed multiple myeloma during the first three cycles of treatment: An observational cohort study. Res. Pract. Thromb. Haemost. 2019, 3, 89–98. [Google Scholar] [CrossRef]
- Knight, R.; DeLap, R.J.; Zeldis, J.B. Lenalidomide and venous thrombosis in multiple myeloma. N. Engl. J. Med. 2006, 354, 2079–2080. [Google Scholar] [CrossRef]
- Galli, M.; Elice, F.; Crippa, C.; Comotti, B.; Rodeghiero, F.; Barbui, T. Recombinant human erythropoietin and the risk of thrombosis in patients receiving thalidomide for multiple myeloma. Haematologica 2004, 89, 1141–1142. [Google Scholar]
- Cortelezzi, A.; Moia, M.; Falanga, A.; Pogliani, E.M.; Agnelli, G.; Bonizzoni, E.; Gussoni, G.; Barbui, T.; Mannucci, P.M.; Group, C.S. Incidence of thrombotic complications in patients with haematological malignancies with central venous catheters: A prospective multicentre study. Br. J. Haematol. 2005, 129, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Zangari, M.; Barlogie, B.; Thertulien, R.; Jacobson, J.; Eddleman, P.; Fink, L.; Fassas, A.; Van Rhee, F.; Talamo, G.; Lee, C.K.; et al. Thalidomide and deep vein thrombosis in multiple myeloma: Risk factors and effect on survival. Clin. Lymphoma 2003, 4, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Auwerda, J.J.; Yuana, Y.; Osanto, S.; de Maat, M.P.; Sonneveld, P.; Bertina, R.M.; Leebeek, F.W. Microparticle-associated tissue factor activity and venous thrombosis in multiple myeloma. Thromb. Haemost. 2011, 105, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Undas, A.; Zubkiewicz-Usnarska, L.; Helbig, G.; Woszczyk, D.; Kozinska, J.; Dmoszynska, A.; Debski, J.; Podolak-Dawidziak, M.; Kuliczkowski, K. Induction therapy alters plasma fibrin clot properties in multiple myeloma patients: Association with thromboembolic complications. Blood Coagul. Fibrinolysis 2015, 26, 621–627. [Google Scholar] [CrossRef]
- Robak, M.; Trelinski, J.; Chojnowski, K. Hemostatic changes after 1 month of thalidomide and dexamethasone therapy in patients with multiple myeloma. Med. Oncol. 2012, 29, 3574–3580. [Google Scholar] [CrossRef][Green Version]
- Carr, M.E., Jr.; Dent, R.M.; Carr, S.L. Abnormal fibrin structure and inhibition of fibrinolysis in patients with multiple myeloma. J. Lab. Clin. Med. 1996, 128, 83–88. [Google Scholar] [CrossRef]
- Carr, M.E., Jr.; Zekert, S.L. Abnormal clot retraction, altered fibrin structure, and normal platelet function in multiple myeloma. Am. J. Physiol. 1994, 266, H1195–H1201. [Google Scholar] [CrossRef]
- Zamagni, E.; Brioli, A.; Tacchetti, P.; Zannetti, B.; Pantani, L.; Cavo, M. Multiple myeloma, venous thromboembolism, and treatment-related risk of thrombosis. Semin. Thromb. Hemost. 2011, 37, 209–219. [Google Scholar] [CrossRef]
- Palumbo, A.; Palladino, C. Venous and arterial thrombotic risks with thalidomide: Evidence and practical guidance. Adv. Drug Saf. 2012, 3, 255–266. [Google Scholar] [CrossRef]
- Baz, R.; Li, L.; Kottke-Marchant, K.; Srkalovic, G.; McGowan, B.; Yiannaki, E.; Karam, M.A.; Faiman, B.; Jawde, R.A.; Andresen, S.; et al. The role of aspirin in the prevention of thrombotic complications of thalidomide and anthracycline-based chemotherapy for multiple myeloma. Mayo Clin. Proc. 2005, 80, 1568–1574. [Google Scholar] [CrossRef]
- Deitcher, S.R.; Erban, J.K.; Limentani, S.A. Acquired free protein S deficiency associated with multiple myeloma: A case report. Am. J. Hematol. 1996, 51, 319–323. [Google Scholar] [CrossRef]
- Gruber, A.; Blasko, G.; Sas, G. Functional deficiency of protein C and skin necrosis in multiple myeloma. Thromb. Res. 1986, 42, 579–581. [Google Scholar] [CrossRef]
- Yasin, Z.; Quick, D.; Thiagarajan, P.; Spoor, D.; Caraveo, J.; Palascak, J. Light-chain paraproteins with lupus anticoagulant activity. Am. J. Hematol. 1999, 62, 99–102. [Google Scholar] [CrossRef]
- Leiba, M.; Malkiel, S.; Budnik, I.; Rozic, G.; Avigdor, A.; Duek, A.; Nagler, A.; Kenet, G.; Livnat, T. Thrombin generation as a predictor of thromboembolic events in multiple myeloma patients. Blood Cells Mol. Dis. 2017, 65, 1–7. [Google Scholar] [CrossRef]
- Dargaud, Y.; Fouassier, M.; Bordet, J.C.; Ducastelle-Lepretre, S.; Dumontet, C.; Moreau, P.; Michallet, M. The challenge of myeloma-related thromboembolic disease: Can thrombin generation assay help physicians to better predict the thromboembolic risk and personalize anti-thrombotic prophylaxis? Leuk. Lymphoma 2019, 1–4. [Google Scholar] [CrossRef]
- Zangari, M.; Saghafifar, F.; Anaissie, E.; Badros, A.; Desikan, R.; Fassas, A.; Mehta, P.; Morris, C.; Toor, A.; Whitfield, D.; et al. Activated protein C resistance in the absence of factor V Leiden mutation is a common finding in multiple myeloma and is associated with an increased risk of thrombotic complications. Blood Coagul. Fibrinolysis 2002, 13, 187–192. [Google Scholar] [CrossRef]
- Cini, M.; Zamagni, E.; Valdre, L.; Palareti, G.; Patriarca, F.; Tacchetti, P.; Legnani, C.; Catalano, L.; Masini, L.; Tosi, P.; et al. Thalidomide-dexamethasone as up-front therapy for patients with newly diagnosed multiple myeloma: Thrombophilic alterations, thrombotic complications, and thromboprophylaxis with low-dose warfarin. Eur. J. Haematol. 2010, 84, 484–492. [Google Scholar] [CrossRef]
- Elice, F.; Fink, L.; Tricot, G.; Barlogie, B.; Zangari, M. Acquired resistance to activated protein C (aAPCR) in multiple myeloma is a transitory abnormality associated with an increased risk of venous thromboembolism. Br. J. Haematol. 2006, 134, 399–405. [Google Scholar] [CrossRef]
- Ay, C.; Simanek, R.; Vormittag, R.; Dunkler, D.; Alguel, G.; Koder, S.; Kornek, G.; Marosi, C.; Wagner, O.; Zielinski, C.; et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: Results from the Vienna Cancer and Thrombosis Study (CATS). Blood 2008, 112, 2703–2708. [Google Scholar] [CrossRef]
- Minnema, M.C.; Fijnheer, R.; De Groot, P.G.; Lokhorst, H.M. Extremely high levels of von Willebrand factor antigen and of procoagulant factor VIII found in multiple myeloma patients are associated with activity status but not with thalidomide treatment. J. Thromb. Haemost. 2003, 1, 445–449. [Google Scholar] [CrossRef]
- van Marion, A.M.; Auwerda, J.J.; Lisman, T.; Sonneveld, P.; de Maat, M.P.; Lokhorst, H.M.; Leebeek, F.W. Prospective evaluation of coagulopathy in multiple myeloma patients before, during and after various chemotherapeutic regimens. Leuk. Res. 2008, 32, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Fotiou, D.; Gavriatopoulou, M.; Ntanasis-Stathopoulos, I.; Migkou, M.; Dimopoulos, M.A.; Terpos, E. Updates on thrombotic events associated with multiple myeloma. Expert Rev. Hematol. 2019, 12, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Joseph, L.; Fink, L.M.; Hauer-Jensen, M. Cytokines in coagulation and thrombosis: A preclinical and clinical review. Blood Coagul. Fibrinolysis 2002, 13, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Nomura, S.; Ito, T.; Yoshimura, H.; Hotta, M.; Nakanishi, T.; Fujita, S.; Nakaya, A.; Satake, A.; Ishii, K. Evaluation of thrombosis-related biomarkers before and after therapy in patients with multiple myeloma. J. Blood Med. 2018, 9, 1–7. [Google Scholar] [CrossRef]
- Petropoulou, A.D.; Gerotziafas, G.T.; Samama, M.M.; Hatmi, M.; Rendu, F.; Elalamy, I. In vitro study of the hypercoagulable state in multiple myeloma patients treated or not with thalidomide. Thromb. Res. 2008, 121, 493–497. [Google Scholar] [CrossRef]
- Crowley, M.P.; Kevane, B.; O’Shea, S.I.; Quinn, S.; Egan, K.; Gilligan, O.M.; Ni Ainle, F. Plasma Thrombin Generation and Sensitivity to Activated Protein C Among Patients With Myeloma and Monoclonal Gammopathy of Undetermined Significance. Clin. Appl. Thromb. Hemost 2016, 22, 554–562. [Google Scholar] [CrossRef]
- Tiong, I.S.; Rodgers, S.E.; Lee, C.H.; McRae, S.J. Baseline and treatment-related changes in thrombin generation in patients with multiple myeloma. Leuk. Lymphoma 2017, 58, 941–949. [Google Scholar] [CrossRef]
- Legendre, P.; Verstraete, E.; Martin, M.; Poinsard, A.; Perrot, A.; Hulin, C.; Faure, G.; Latger-Cannard, V.; Perrin, J. Hypocoagulability as assessed by thrombin generation test in newly-diagnosed patients with multiple myeloma. Blood Cells Mol. Dis. 2017, 66, 47–49. [Google Scholar] [CrossRef]
- Fotiou, D.; Sergentanis, T.N.; Papageorgiou, L.; Stamatelopoulos, K.; Gavriatopoulou, M.; Kastritis, E.; Psaltopoulou, T.; Salta, S.; Van Dreden, P.; Sangare, R.; et al. Longer procoagulant phospholipid-dependent clotting time, lower endogenous thrombin potential and higher tissue factor pathway inhibitor concentrations are associated with increased VTE occurrence in patients with newly diagnosed multiple myeloma: Results of the prospective ROADMAP-MM-CAT study. Blood Cancer J. 2018, 8, 102. [Google Scholar] [CrossRef]
- Fouquet, G.; Tardy, S.; Demarquette, H.; Bonnet, S.; Gay, J.; Debarri, H.; Herbaux, C.; Guidez, S.; Michel, J.; Perrot, A.; et al. Efficacy and safety profile of long-term exposure to lenalidomide in patients with recurrent multiple myeloma. Cancer 2013, 119, 3680–3686. [Google Scholar] [CrossRef]
- Rajkumar, S.V.; Jacobus, S.; Callander, N.S.; Fonseca, R.; Vesole, D.H.; Williams, M.E.; Abonour, R.; Siegel, D.S.; Katz, M.; Greipp, P.R.; et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: An open-label randomised controlled trial. Lancet Oncol. 2010, 11, 29–37. [Google Scholar] [CrossRef]
- Rosovsky, R.; Hong, F.; Tocco, D.; Connell, B.; Mitsiades, C.; Schlossman, R.; Ghobrial, I.; Lockridge, L.; Warren, D.; Bradwin, G.; et al. Endothelial stress products and coagulation markers in patients with multiple myeloma treated with lenalidomide plus dexamethasone: An observational study. Br. J. Haematol. 2013, 160, 351–358. [Google Scholar] [CrossRef]
- Zonder, J.A.; Crowley, J.; Hussein, M.A.; Bolejack, V.; Moore, D.F., Sr.; Whittenberger, B.F.; Abidi, M.H.; Durie, B.G.; Barlogie, B. Lenalidomide and high-dose dexamethasone compared with dexamethasone as initial therapy for multiple myeloma: A randomized Southwest Oncology Group trial (S0232). Blood 2010, 116, 5838–5841. [Google Scholar] [CrossRef]
- Attal, M.; Lauwers-Cances, V.; Marit, G.; Caillot, D.; Moreau, P.; Facon, T.; Stoppa, A.M.; Hulin, C.; Benboubker, L.; Garderet, L.; et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N. Engl. J. Med. 2012, 366, 1782–1791. [Google Scholar] [CrossRef]
- Palumbo, A.; Hajek, R.; Delforge, M.; Kropff, M.; Petrucci, M.T.; Catalano, J.; Gisslinger, H.; Wiktor-Jedrzejczak, W.; Zodelava, M.; Weisel, K.; et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N. Engl. J. Med. 2012, 366, 1759–1769. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Swern, A.S.; Li, J.S.; Hussein, M.; Weiss, L.; Nagarwala, Y.; Baz, R. Efficacy and safety of long-term treatment with lenalidomide and dexamethasone in patients with relapsed/refractory multiple myeloma. Blood Cancer J. 2014, 4, e257. [Google Scholar] [CrossRef]
- Scott, L.J. Pomalidomide: A review of its use in patients with recurrent multiple myeloma. Drugs 2014, 74, 549–562. [Google Scholar] [CrossRef]
- Richardson, P.G.; Siegel, D.S.; Vij, R.; Hofmeister, C.C.; Baz, R.; Jagannath, S.; Chen, C.; Lonial, S.; Jakubowiak, A.; Bahlis, N.; et al. Pomalidomide alone or in combination with low-dose dexamethasone in relapsed and refractory multiple myeloma: A randomized phase 2 study. Blood 2014, 123, 1826–1832. [Google Scholar] [CrossRef]
- Miguel, J.S.; Weisel, K.; Moreau, P.; Lacy, M.; Song, K.; Delforge, M.; Karlin, L.; Goldschmidt, H.; Banos, A.; Oriol, A.; et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): A randomised, open-label, phase 3 trial. Lancet Oncol. 2013, 14, 1055–1066. [Google Scholar] [CrossRef]
- Leleu, X.; Attal, M.; Arnulf, B.; Moreau, P.; Traulle, C.; Marit, G.; Mathiot, C.; Petillon, M.O.; Macro, M.; Roussel, M.; et al. Pomalidomide plus low-dose dexamethasone is active and well tolerated in bortezomib and lenalidomide-refractory multiple myeloma: Intergroupe Francophone du Myelome 2009-02. Blood 2013, 121, 1968–1975. [Google Scholar] [CrossRef]
- Zangari, M.; Fink, L.; Zhan, F.; Tricot, G. Low venous thromboembolic risk with bortezomib in multiple myeloma and potential protective effect with thalidomide/lenalidomide-based therapy: Review of data from phase 3 trials and studies of novel combination regimens. Clin. Lymphoma Myeloma Leuk. 2011, 11, 228–236. [Google Scholar] [CrossRef]
- Dimopoulos, M.; Wang, M.; Maisnar, V.; Minarik, J.; Bensinger, W.; Mateos, M.V.; Obreja, M.; Blaedel, J.; Moreau, P. Response and progression-free survival according to planned treatment duration in patients with relapsed multiple myeloma treated with carfilzomib, lenalidomide, and dexamethasone (KRd) versus lenalidomide and dexamethasone (Rd) in the phase III ASPIRE study. J. Hematol. Oncol. 2018, 11, 49. [Google Scholar] [CrossRef]
- Lonial, S.; Dimopoulos, M.; Palumbo, A.; White, D.; Grosicki, S.; Spicka, I.; Walter-Croneck, A.; Moreau, P.; Mateos, M.V.; Magen, H.; et al. Elotuzumab Therapy for Relapsed or Refractory Multiple Myeloma. N. Engl. J. Med. 2015, 373, 621–631. [Google Scholar] [CrossRef]
- Liu, Y.C.; Szmania, S.; van Rhee, F. Profile of elotuzumab and its potential in the treatment of multiple myeloma. Blood Lymphat. Cancer 2014, 2014, 15–27. [Google Scholar] [CrossRef][Green Version]
- Kumar, S.K.; Bensinger, W.I.; Zimmerman, T.M.; Reeder, C.B.; Berenson, J.R.; Berg, D.; Hui, A.M.; Gupta, N.; Di Bacco, A.; Yu, J.; et al. Phase 1 study of weekly dosing with the investigational oral proteasome inhibitor ixazomib in relapsed/refractory multiple myeloma. Blood 2014, 124, 1047–1055. [Google Scholar] [CrossRef]
- Kumar, S.K.; Berdeja, J.G.; Niesvizky, R.; Lonial, S.; Laubach, J.P.; Hamadani, M.; Stewart, A.K.; Hari, P.; Roy, V.; Vescio, R.; et al. Safety and tolerability of ixazomib, an oral proteasome inhibitor, in combination with lenalidomide and dexamethasone in patients with previously untreated multiple myeloma: An open-label phase 1/2 study. Lancet Oncol. 2014, 15, 1503–1512. [Google Scholar] [CrossRef]
- Mateos, M.V.; Dimopoulos, M.A.; Cavo, M.; Suzuki, K.; Jakubowiak, A.; Knop, S.; Doyen, C.; Lucio, P.; Nagy, Z.; Kaplan, P.; et al. Daratumumab plus Bortezomib, Melphalan, and Prednisone for Untreated Myeloma. N. Engl. J. Med. 2018, 378, 518–528. [Google Scholar] [CrossRef]
- Spencer, A.; Lentzsch, S.; Weisel, K.; Avet-Loiseau, H.; Mark, T.M.; Spicka, I.; Masszi, T.; Lauri, B.; Levin, M.D.; Bosi, A.; et al. Daratumumab plus bortezomib and dexamethasone versus bortezomib and dexamethasone in relapsed or refractory multiple myeloma: Updated analysis of CASTOR. Haematologica 2018, 103, 2079–2087. [Google Scholar] [CrossRef]
- Rupa-Matysek, J.; Gil, L.; Wojtasinska, E.; Nowicki, A.; Dytfeld, D.; Kazmierczak, M.; Komarnicki, M. Inhibitory effects of bortezomib on platelet aggregation in patients with multiple myeloma. Thromb. Res. 2014, 134, 404–411. [Google Scholar] [CrossRef]
- Abdullah, W.Z.; Roshan, T.M.; Hussin, A.; Zain, W.S.; Abdullah, D. Increased PAC-1 expression among patients with multiple myeloma on concurrent thalidomide and warfarin. Blood Coagul. Fibrinolysis 2013, 24, 893–895. [Google Scholar] [CrossRef]
- Jilma, B.; Cvitko, T.; Winter-Fabry, A.; Petroczi, K.; Quehenberger, P.; Blann, A.D. High dose dexamethasone increases circulating P-selectin and von Willebrand factor levels in healthy men. Thromb. Haemost. 2005, 94, 797–801. [Google Scholar] [CrossRef]
- Swystun, L.L.; Shin, L.Y.; Beaudin, S.; Liaw, P.C. Chemotherapeutic agents doxorubicin and epirubicin induce a procoagulant phenotype on endothelial cells and blood monocytes. J. Thromb. Haemost. 2009, 7, 619–626. [Google Scholar] [CrossRef]
- Avcu, F.; Ural, A.U.; Cetin, T.; Nevruz, O. Effects of bortezomib on platelet aggregation and ATP release in human platelets, in vitro. Thromb. Res. 2008, 121, 567–571. [Google Scholar] [CrossRef]
- Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008, 111, 4902–4907. [Google Scholar] [CrossRef]
- Sanfilippo, K.M.; Wang, T.F.; Luo, S.; Thomas, T.S.; Carson, K.R.; Keller, J.W.; Kuderer, N.M.; Calverley, D.; Gage, B. Predictive ability of the khorana score for venous thromboembolism (VTE) in multiple myeloma (MM). J. Clin. Oncol. 2018, 36. [Google Scholar] [CrossRef]
- Syrigos, K.; Grapsa, D.; Sangare, R.; Evmorfiadis, I.; Larsen, A.K.; Van Dreden, P.; Boura, P.; Charpidou, A.; Kotteas, E.; Sergentanis, T.N.; et al. Prospective Assessment of Clinical Risk Factors and Biomarkers of Hypercoagulability for the Identification of Patients with Lung Adenocarcinoma at Risk for Cancer-associated Thrombosis. The Observational ROADMAP-CAT Study. Oncol. Press. 2018, 23, 1372–1381. [Google Scholar] [CrossRef]
- Sanfilippo, K.M.; Luo, S.; Wang, T.F.; Fiala, M.; Schoen, M.; Wildes, T.M.; Mikhael, J.; Kuderer, N.M.; Calverley, D.C.; Keller, J.; et al. Predicting venous thromboembolism in multiple myeloma: Development and validation of the IMPEDE VTE score. Am. J. Hematol. 2019. [Google Scholar] [CrossRef]
- Li, A.; Wu, Q.; Luo, S.; Warnick, G.S.; Zakai, N.A.; Libby, E.N.; Gage, B.F.; Garcia, D.A.; Lyman, G.H.; Sanfilippo, K.M. Derivation and Validation of a Risk Assessment Model for Immunomodulatory Drug-Associated Thrombosis Among Patients With Multiple Myeloma. J. Natl. Compr. Cancer Netw. 2019, 17, 840–847. [Google Scholar] [CrossRef]
- Al-Ani, F.; Bermejo, J.M.; Mateos, M.V.; Louzada, M. Thromboprophylaxis in multiple myeloma patients treated with lenalidomide—A systematic review. Thromb. Res. 2016, 141, 84–90. [Google Scholar] [CrossRef]
- Swan, D.; Rocci, A.; Bradbury, C.; Thachil, J. Venous thromboembolism in multiple myeloma—Choice of prophylaxis, role of direct oral anticoagulants and special considerations. Br. J. Haematol. 2018, 183, 538–556. [Google Scholar] [CrossRef]
- Sanfilipo, K.; Carson, K.; BF, C. Aspirin May be Inadequate Thromboprophylaxis in Multiple Myeloma. Blood 2017, 130, 3419. [Google Scholar]
- Raskob, G.E.; van Es, N.; Verhamme, P.; Carrier, M.; Di Nisio, M.; Garcia, D.; Grosso, M.A.; Kakkar, A.K.; Kovacs, M.J.; Mercuri, M.F.; et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism. N. Engl. J. Med. 2018, 378, 615–624. [Google Scholar] [CrossRef]
- Man, L.; Morris, A.; Brown, J.; Palkimas, S.; Davidson, K. Use of direct oral anticoagulants in patients on immunomodulatory agents. J. Thromb. Thrombolysis 2017, 44, 298–302. [Google Scholar] [CrossRef]
- Storrar, N.P.F.; Mathur, A.; Johnson, P.R.E.; Roddie, P.H. Safety and efficacy of apixaban for routine thromboprophylaxis in myeloma patients treated with thalidomide- and lenalidomide-containing regimens. Br. J. Haematol. 2018. [Google Scholar] [CrossRef]
- Cornell, R.F.; Goldhaber, S.Z.; Engelhardt, B.G.; Moslehi, J.; Jagasia, M.; Patton, D.; Harrell, S.; Hall, R.; Wyatt, H.; Piazza, G. Apixaban for Primary Prevention of Venous Thromboembolism in Patients With Multiple Myeloma Receiving Immunomodulatory Therapy. Front. Oncol. 2019, 9, 45. [Google Scholar] [CrossRef]
- Pegourie, B.; Karlin, L.; Benboubker, L.; Orsini-Piocelle, F.; Tiab, M.; Auger-Quittet, S.; Rodon, P.; Royer, B.; Leleu, X.; Bareau, B.; et al. Apixaban for the prevention of thromboembolism in immunomodulatory-treated myeloma patients: Myelaxat, a phase 2 pilot study. Am. J. Hematol. 2019, 94, 635–640. [Google Scholar] [CrossRef]
- Riess, H.; Prandoni, P.; Harder, S.; Kreher, S.; Bauersachs, R. Direct oral anticoagulants for the treatment of venous thromboembolism in cancer patients: Potential for drug-drug interactions. Crit. Rev. Oncol. Hematol. 2018, 132, 169–179. [Google Scholar] [CrossRef]
- Short, N.J.; Connors, J.M. New oral anticoagulants and the cancer patient. Oncologist 2014, 19, 82–93. [Google Scholar] [CrossRef]
- Bellesoeur, A.; Thomas-Schoemann, A.; Allard, M.; Smadja, D.; Vidal, M.; Alexandre, J.; Goldwasser, F.; Blanchet, B. Pharmacokinetic variability of anticoagulants in patients with cancer-associated thrombosis: Clinical consequences. Crit. Rev. Oncol. Hematol. 2018, 129, 102–112. [Google Scholar] [CrossRef]
- Farge, D.; Bounameaux, H.; Brenner, B.; Cajfinger, F.; Debourdeau, P.; Khorana, A.A.; Pabinger, I.; Solymoss, S.; Douketis, J.; Kakkar, A. International clinical practice guidelines including guidance for direct oral anticoagulants in the treatment and prophylaxis of venous thromboembolism in patients with cancer. Lancet Oncol. 2016, 17, e452–e466. [Google Scholar] [CrossRef]
- Frere, C.; Benzidia, I.; Marjanovic, Z.; Farge, D. Recent Advances in the Management of Cancer-Associated Thrombosis: New Hopes but New Challenges. Cancers 2019, 11, 71. [Google Scholar] [CrossRef]
- Vedovati, M.C.; Giustozzi, M.; Becattini, C. Venous thromboembolism and cancer: Current and future role of direct-acting oral anticoagulants. Thromb. Res. 2019, 177, 33–41. [Google Scholar] [CrossRef]
- Lim, M.S.; Enjeti, A.K. Safety of anticoagulation in the treatment of venous thromboembolism in patients with haematological malignancies and thrombocytopenia: Report of 5 cases and literature review. Crit. Rev. Oncol. Hematol. 2016, 105, 92–99. [Google Scholar] [CrossRef][Green Version]
- Khanal, N.; Bociek, R.G.; Chen, B.; Vose, J.M.; Armitage, J.O.; Bierman, P.J.; Maness, L.J.; Lunning, M.A.; Gundabolu, K.; Bhatt, V.R. Venous thromboembolism in patients with hematologic malignancy and thrombocytopenia. Am. J. Hematol. 2016, 91, E468–E472. [Google Scholar] [CrossRef]
- Napolitano, M.; Saccullo, G.; Marietta, M.; Carpenedo, M.; Castaman, G.; Cerchiara, E.; Chistolini, A.; Contino, L.; De Stefano, V.; Falanga, A.; et al. Platelet cut-off for anticoagulant therapy in thrombocytopenic patients with blood cancer and venous thromboembolism: An expert consensus. Blood Transfus. 2018, 17, 171. [Google Scholar] [CrossRef]
- Carrier, M.; Abou-Nassar, K.; Mallick, R.; Tagalakis, V.; Shivakumar, S.; Schattner, A.; Kuruvilla, P.; Hill, D.; Spadafora, S.; Marquis, K.; et al. Apixaban to Prevent Venous Thromboembolism in Patients with Cancer. N. Engl. J. Med. 2018. [Google Scholar] [CrossRef]
- Park, D.Y.; Poudel, S.K.; Jia, X.; Wilks, M.L.; Pinkava, V.; O’Brien, M.; Tripp, B.; Song, J.-M.; McCrae, K.R.; Angelini, D.E.; et al. Clinical Outcomes with Direct Oral Anticoagulants Compared to Low Molecular Weight Heparins in the Treatment of Cancer-Associated Venous Thromboembolism. Blood 2018, 132, 1237. [Google Scholar] [CrossRef]
| Algorithm for MM Patient Risk Stratification | ||
|---|---|---|
| Patient-Related Risk Factors ASSIGN 1 Point for Each of the below: | Disease-Related Risk Factors: Assign 1 Point for Each of the below: | Treatment-Related Risk Factors: Assign Points as Seen below: |
| Body mass index >25, Age >75, Personal or family history of VTE, Central venous catheter, Acute infection or Hospitalization, Blood clotting disorders or Thrombophilia, Immobility with performance status of >1, Comorbidities (liver, renal impairment, chronic obstructive pulmonary disorder, diabetes mellitus, chronic inflammatory bowel disease), Race (Caucasian is a risk factor) |
|
|
| Risk stratification and recommended thromboprophylaxis: 0 points: Low risk None 1 point: Intermediate risk Aspirin at 100 mg >1 points: High risk Low molecular weight heparin at prophylactic dose or therapeutic dose of warfarin | ||
| Patient Related Risk Factors | |||||
|---|---|---|---|---|---|
| Age | Brown et al., 2016 [26] hazard of thrombosis for the 35–64 and 65–74 age groups compared to the 18–34 reference group, HR 2.8 for the 75 + age group (1.6–4.8 95% CI) | Baker et al. 2018 [22] Age not identified as risk factor for VTE (p = 0.56) | Bagratuni et al. 2013 [27] n = 200, VTEs were more frequent in patients >65 years (8.1% vs. 1.6%) | ||
| Body mass index ≥30 kg/m2 Family history Race | No specific studies in MM for these risk factors | ||||
| Personal history | Anaissie et al. 2012 [28] history of VTE was a strong predictor of VTE on univariate analysis (p < 0.000005) n = 604 | ||||
| Cardiac disease (e.g., symptomatic coronary artery disease, congestive heart failure, or history of stent placement/CABG) | Brown et al. [26] congestive cardiac failure associated with hazard HR = 1.7 (95% CI, 1.4–2.1), hypertension associated with hazard (HR = 1.2 (95% CI, 1.0–1.3)) | ||||
| Other comorbidity: | Diabetes mellitus, renal impairment, liver impairment, chronic inflammatory disease, COPD, immobilization, autoimmune disease, recent trauma or surgery, hospitalization, immobility, inherited thrombophilia, use of hormone replacement, acute infection No specific data on these risk factors in patients with MM available | ||||
| Use of erythropoietin (EPO) | Anaissie et al. 2012 [28] n = 604 prophylactic EPO (p = 0.002; OR, 2.488; 95% CI, 1.432–4.324) | Chalayer et al. 2018 [29] OR 0.49 (95% CI 0.18–3.83) | Knight et al. 2015 [30] n plus lenalidomide: OR 3.21 (1.72–6.01 95% CI, p < 0.001) | Galli et al. 2004 [31] n = 199, 8.1% prevalence with EPO vs. 9.3% without, p > 0.5) | Leleu et al. 2013 [5] Relative RIsk of VTE 3.46 (0.45–3.7 95% CI, p = 0.04) |
| Central venous catheter or pacemaker | Cortelezzi et al. 2005 [32] 12% VTE events in 416 patients with hematologic malignancies and CVC insertion (MM diagnosis seen in 18.8% of pts) | ||||
| Disease-specific risk factors | |||||
| New diagnosis of MM | Zangari et al. 2003 [33] (n = 535) newly diagnosed disease (OR, 2.5; p = 0.001) | ||||
| Chromosome 11 abnormalities | Zangari et al. 2003 [33] (n = 535) (OR, 1.8; p = 0.048) | ||||
| Microparticle (MP)-associated tissue factor and tissue factor (TF) | Auwerda et al. 2011 [34]: (n = 122) NDMM; MP-TF levels prior to treatment initiation did not predict VTE, but MP-TF remained elevated in patients who developed VTE 15.1 [10.3–25.2], in contrast to patients not developing VTE (11.4 [7.0–25.2], p < 0.001 | ||||
| Thrombin lag phase(s) | Undas et al. 2015 [35] 60 [52–60.5] vs. 50 [36,37,38,39,40,41,42,43,44,45], p = 0.01 in patients with VTE | ||||
| Thrombin peak concentration (nmol/L) | Undas et al. 2015 [35] higher peak concentration associated with VTE; 503.5 (418–550) vs. 344.8 (269–411) in patients without VTE, p < 0.001 | Leiba et al. 2017 [45] higher peak height values (620 vs. 400 nM, p < 0.001) associated with higher VTE risk | Chalayer et al. 2018 [29] 186 nmol/L for patient with VTE vs. 149 nmol/L for not VTE, p = 0.22 in univariate analysis | Ay et al. 2011 [25] associated with VTE risk | |
| Thrombin peak time (min) | Chalayer et al. 2018 [29] at baseline; 10.8 min for patients with VTE vs. 9 min for no VTE, p = 0.82 in univariate analysis, no significant association with VTE | Ay et al. 2011 [25] associated with VTE risk | |||
| Endogenous thrombin potential (ETP) (Mxmin) | Dargaud et al. 2019; ETP higher in MM patients versus controls [46] | Ay et al. 2011 [25] not associated with VTE risk | Leiba et al. 2017 [45] higher EPT (2896 vs. 2028 nMxmin, p < 0.001) associated with higher VTE risk | Chalayer et al. 2018 [29] increase in ETP between baseline and cycle 4—no association with VTE | |
| Thrombin-activatable fibrinolysis inhibitor (TAFI) (mg/mL) | Undas et al. 2015 [35] higher levels associated with VTE 45.3 (44.6–47.4) vs. 38.9 (33.5–42.3) <0.001 | ||||
| Plasminogen activator inhibitory (PAI-1) (IU/mL) | Undas et al. 2015; [35] higher PAI-1 levels associated with VTE risk 11 (9.9–12.8) vs. 8.3 (6.4–10.5), p = 0.004 | ||||
| Lower clot permeability and clot lysis | Undas et al. 2015; [35] in patients with lower clot permeability Ks (10−9 cm2) and lower D-Drate, (maximum rate of increase in D-dimer levels in the lysis assay) associated with higher VTE risk | ||||
| Acquired activated protein C resistance (aAPC-R) | Zangari et al. 2002 [47] higher proportion of patients with APC resistance developed DVT (5/14 versus 7/38; p = 0.04)–41.7% prevalence of APC-R in the group of NDMM who developed VTE | Cini et al. 2010 [48] no difference in VTE occurrence between patients with APCR (6.7% vs. 10.3%, p = 1.0) | Elice et al. 2006 [49] higher incidence of VTE with aAPC-R; 1178 patients; 31% versus 12%; p < 0.001) | ||
| NFκB1 gene single nucleotide polymorphism | Bagratuni et al. 2013 [27] NFκB1 and VTE risk: OR 3.76, 95%CI 1–16, p = 0.051 | ||||
| Factor v. Leiden (R506Q) or G20210A prothrombin mutation | Cini et al. [48] patients with polymorphisms had not increased VTE rate (10% vs. 9.4%, p = 0.27) | Bagratuni et al. 2013 [27] FVLeiden and FIIG20210A not associated with higher VTE rates | |||
| P-selectin (ng/mL) | Ay et al. 2008 [50] Elevated P-selectin (>53.1 ng/mL) risk factor for VTE (HR = 2.6, 95% CI, 1.4–4.9, p = 003) | ||||
| vonWillenbrand (VWF) increased levels | Minnema et al. 2003 [51] N = 19 patients on thalidomide VWF-Ag in patients with VTE was 375 ± 121% vs. 235 ± 116% in patients without VTE (p = 0.03) | Van Marion et al. 2008 [52] higher levels of VWF not associated with VTE OR 2.69 95% CI 0.71–10.26, p = 0.147 | |||
| FVIII (factor VIII) | Minnema et al. 2003 [51] N = 19 patients on thalidomide FVIII:C was 352 ± 67% vs. 283 ± 114% in patients without VTE (p = 0.17) | Cini et al. 2010: [48] elevated FVIII activity not associated with higher VTE rate (10% vs. 7.4% p = 0.76) | Van Marion et al. 2008 [52] higher levels of FVIII not associated with VTE occurrence | ||
| Other biomarkers | Increased D-dimer levels, prothrombin 1 and 2 increased levels, hyperviscosity, antiphospholipid antibodies, lupus anticoagulant—resistance to protein C pathway No data on these biomarkers and VTE risk | ||||
| Myeloma Therapy Related [53] | |||||
Multi-agent chemotherapy Doxorubicin
| |||||
| CLINICAL RAMs for VTE in MM | |
|---|---|
| IMPEDE VTE Score | SAVED Score* |
| Immunomodulatory drug (+4) BMI ≥ 25 kg/m2 (+1) Pathologic fracture pelvis/femur (+4) Erythropoiesis-stimulating agent (+1) Dexamethasone (High-dose) (+4) Dexamethasone Low-Dose (+2) Doxorubicin (+3) Ethnicity/Race = Asian (−3) VTE history (+5) Tunneled line/CVC (+2) Existing use of therapeutic warfarin or low molecular weight heparin (LWMH) (−5) Existing use of prophylactic LMWH or aspirin (−3) | Surgery (within last 90 days) (+2) Asian Race (−3) VTE history (+3) Eight (age >=80 years) (+1) Dexamethasone dose
|
| Stratified risk groups based on weighted scoring system | |
|
|
| Missing: recommendation on thromboprophylaxis based on risk groups | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fotiou, D.; Gavriatopoulou, M.; Terpos, E. Multiple Myeloma and Thrombosis: Prophylaxis and Risk Prediction Tools. Cancers 2020, 12, 191. https://doi.org/10.3390/cancers12010191
Fotiou D, Gavriatopoulou M, Terpos E. Multiple Myeloma and Thrombosis: Prophylaxis and Risk Prediction Tools. Cancers. 2020; 12(1):191. https://doi.org/10.3390/cancers12010191
Chicago/Turabian StyleFotiou, Despina, Maria Gavriatopoulou, and Evangelos Terpos. 2020. "Multiple Myeloma and Thrombosis: Prophylaxis and Risk Prediction Tools" Cancers 12, no. 1: 191. https://doi.org/10.3390/cancers12010191
APA StyleFotiou, D., Gavriatopoulou, M., & Terpos, E. (2020). Multiple Myeloma and Thrombosis: Prophylaxis and Risk Prediction Tools. Cancers, 12(1), 191. https://doi.org/10.3390/cancers12010191






