Genetic Aberration Analysis in Thai Colorectal Adenoma and Early-Stage Adenocarcinoma Patients by Whole-Exome Sequencing
Abstract
1. Introduction
2. Results
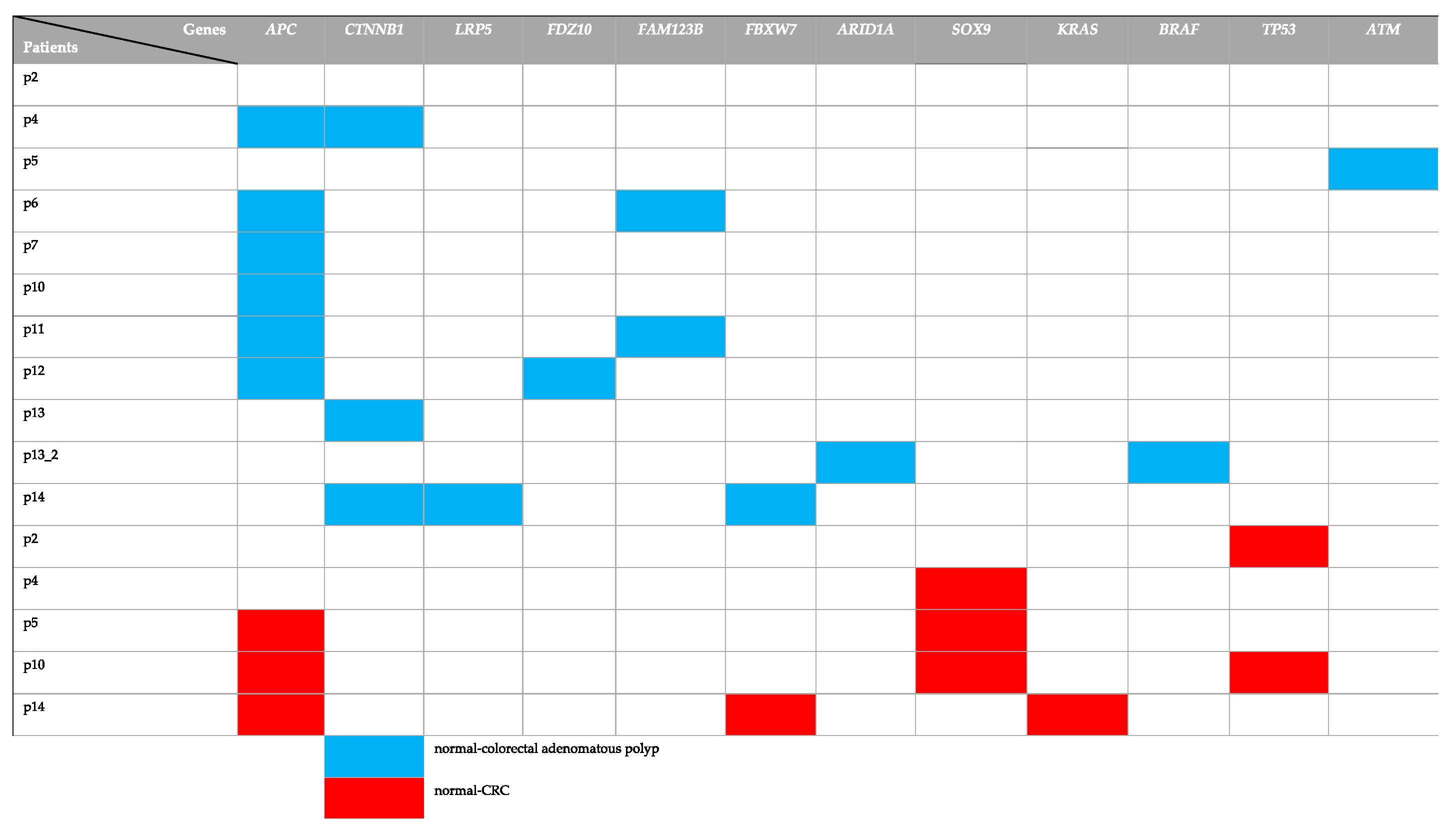
2.1. Identification of Gene with Somatic Mutations in Normal-Colorectal Adenoma and Normal-CRC in CRC Patients
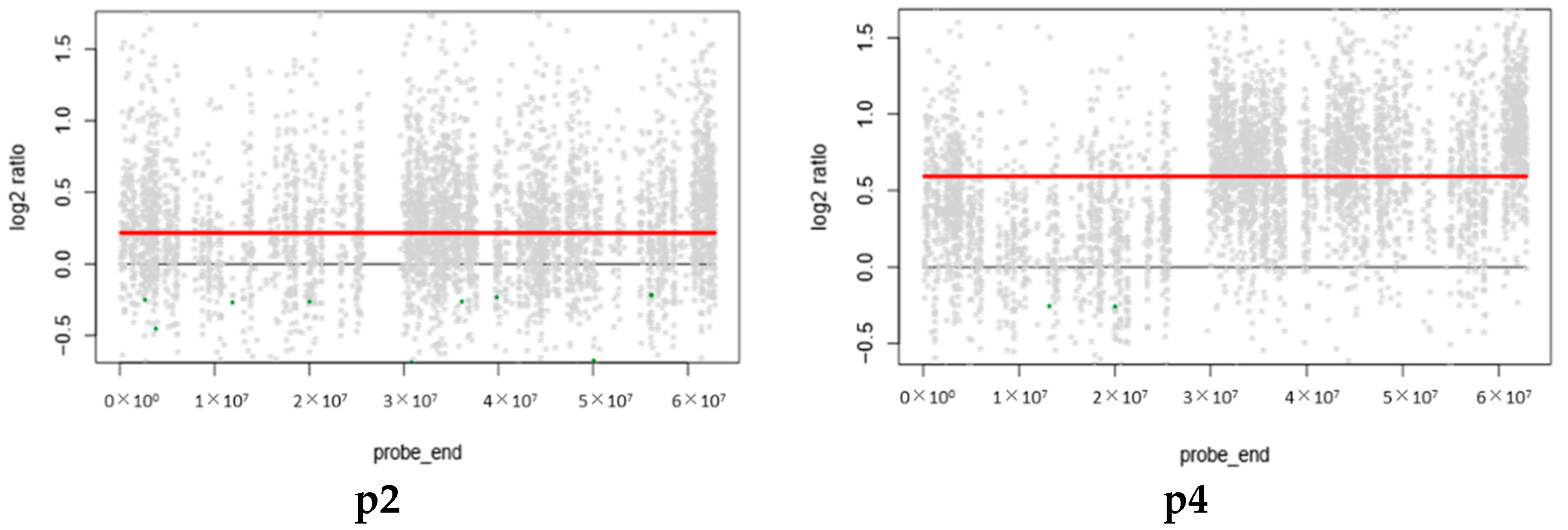
2.2. Copy Number Variation (CNVs)
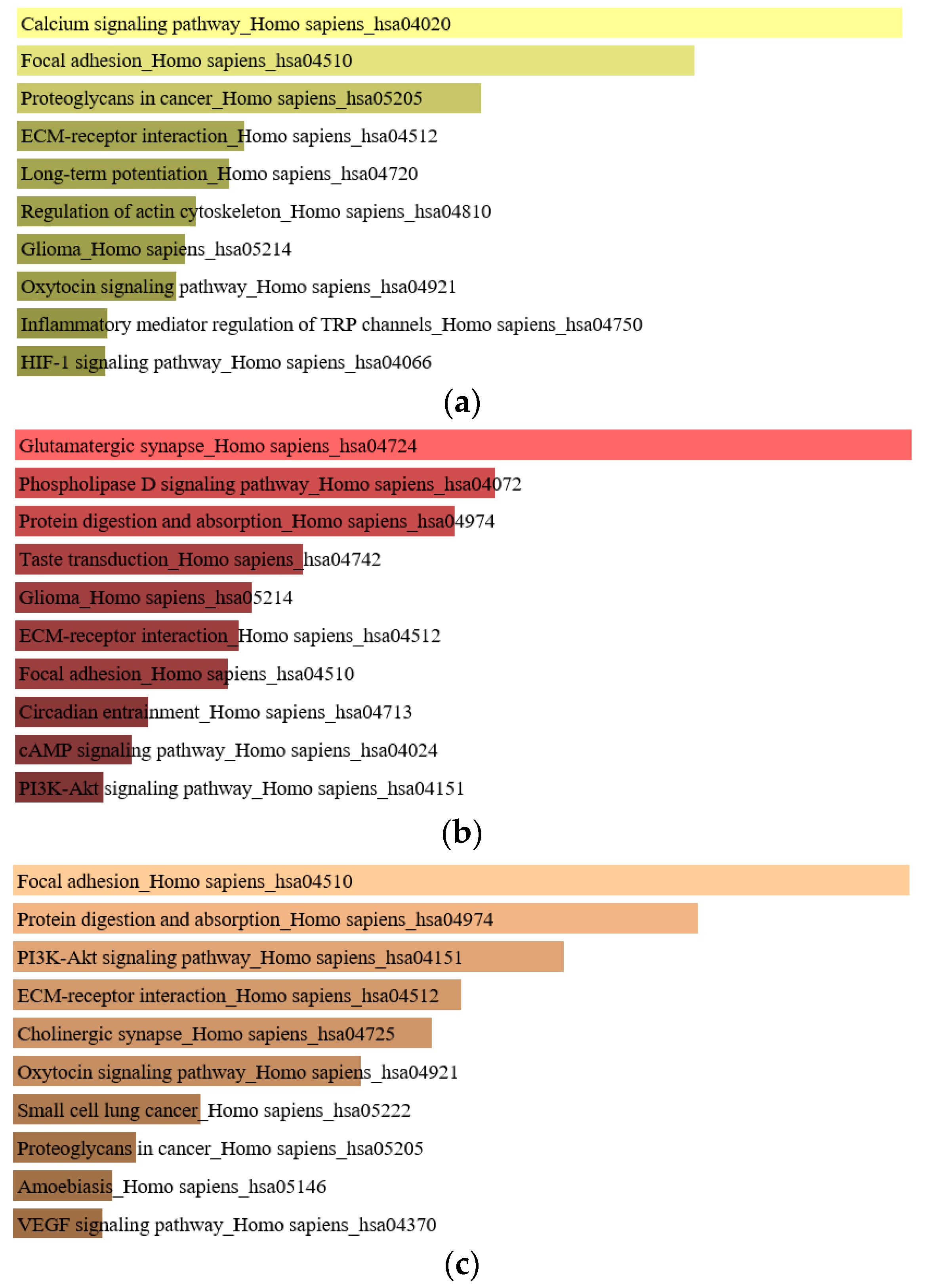
2.3. The Analysis of Enriched Genes in Normal-Colorectal Adenoma and Normal-CRC Groups
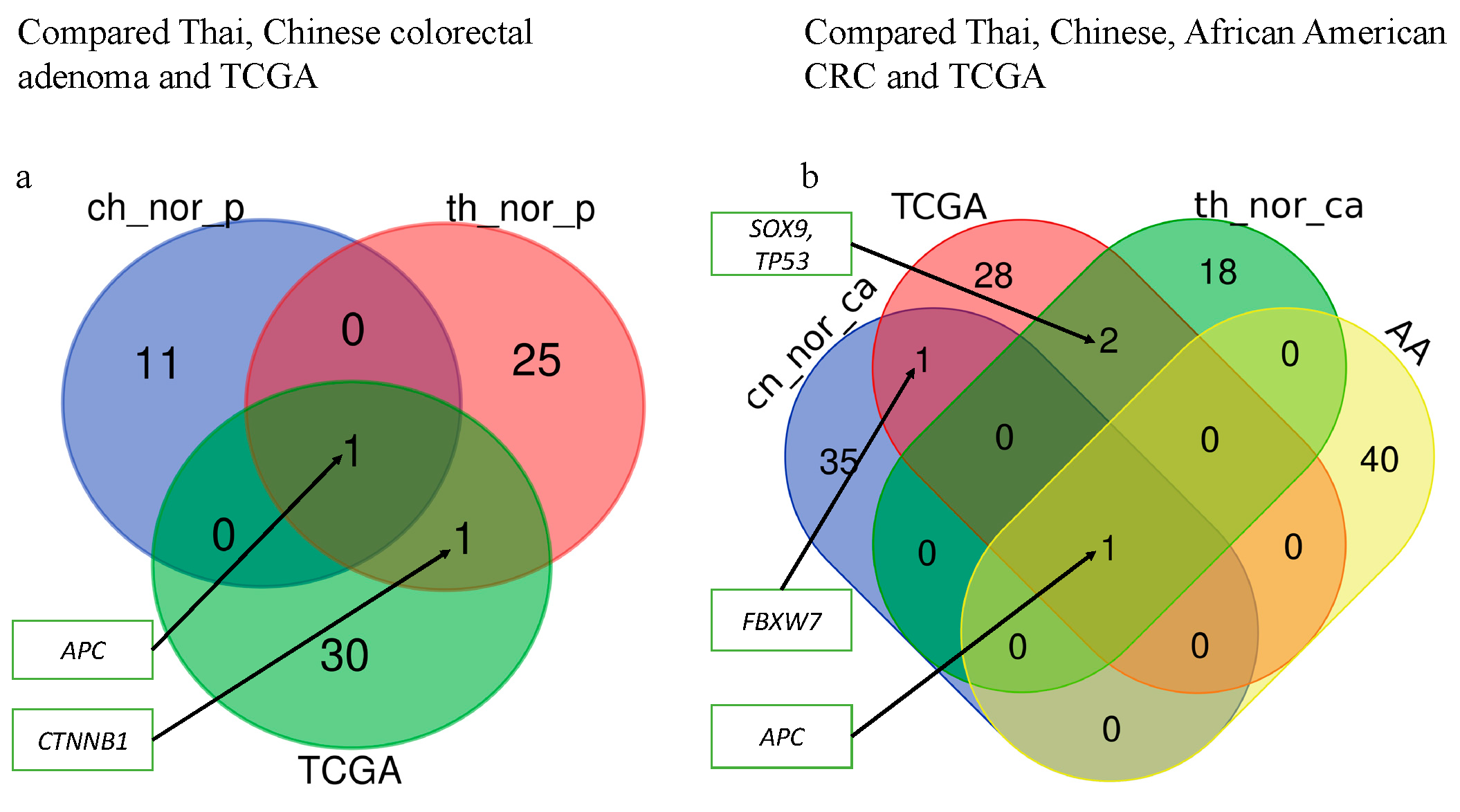
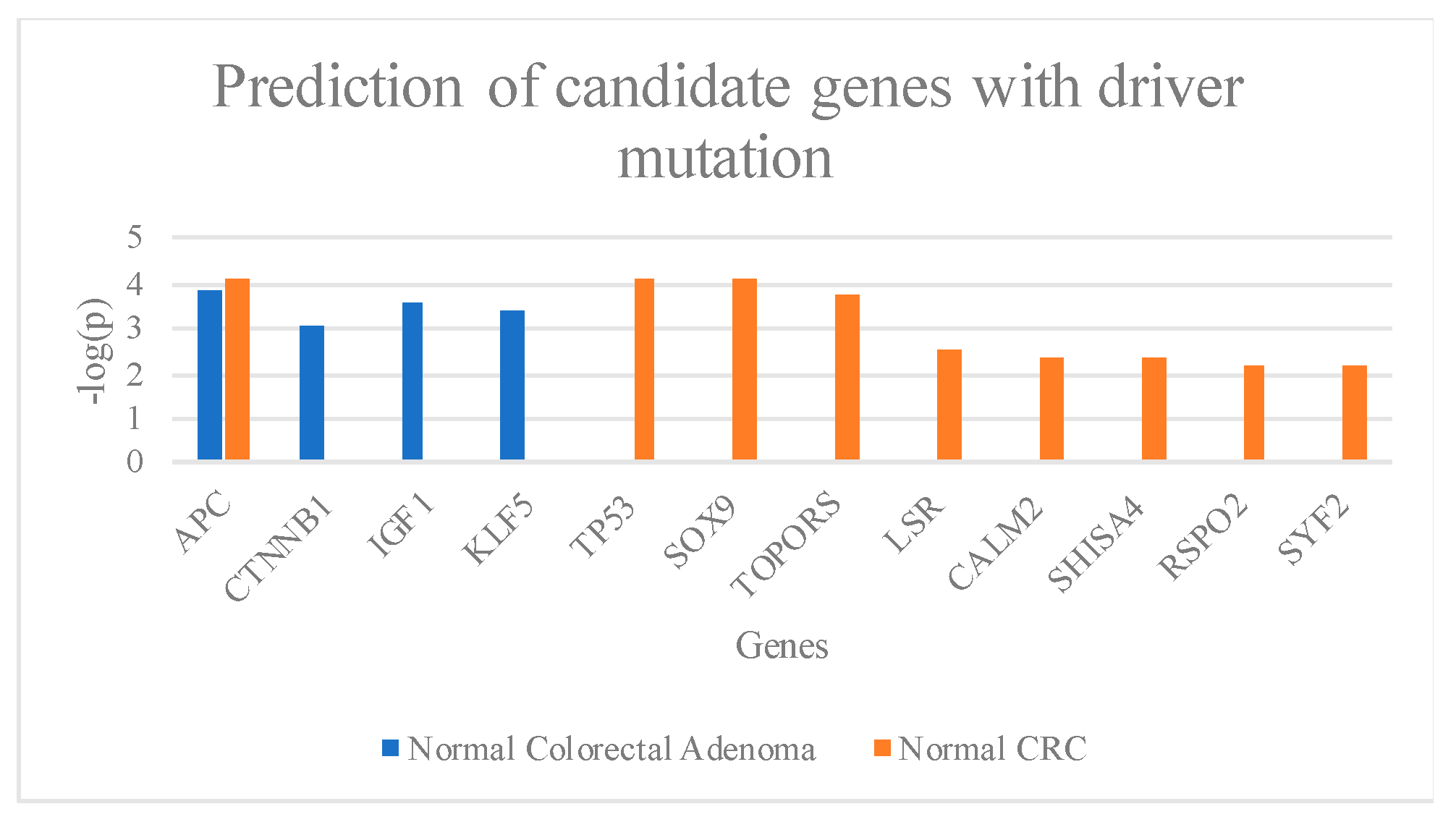
2.4. Candidate Genes with Driver Mutation in Normal-Colorectal Adenoma and Normal-CRC Groups
3. Discussion
4. Materials and Methods
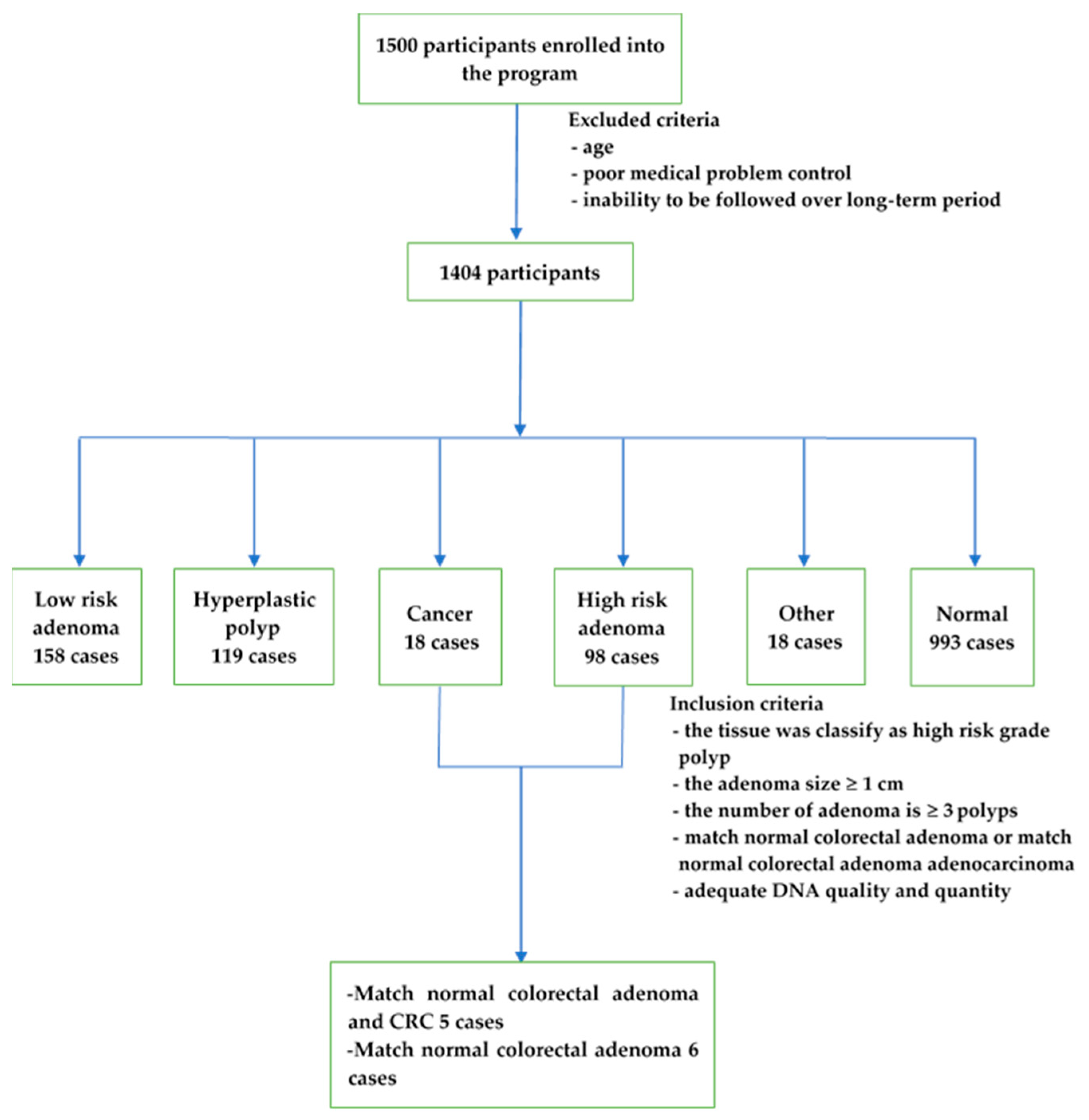
4.1. Samples
4.2. DNA Extraction and Library Preparation
4.3. Whole-Exome Analysis
4.4. CNV Analysis
4.5. The Analysis of Enriched Genes
4.6. The Genes with Driver Mutation Analysis
4.7. Availability of Data/Materials
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.D.; Siegel, R.L.; Lin, C.C.; Mariotto, A.B.; Kramer, J.L.; Rowland, J.H.; Stein, K.D.; Alteri, R.; Jemal, A. Cancer treatment and survivorship statistics, 2016. CA Cancer J. Clin. 2016, 66, 271–289. [Google Scholar] [CrossRef] [PubMed]
- US Census Bureau. U.S. and World Population Clock. Available online: https://www.census.gov/popclock/ (accessed on 14 April 2018).
- Phiphatpatthamaamphan, K.; Vilaichone, R. Colorectal Cancer in the Central Region of Thailand. Asian Pac. J. Cancer Prev. 2016, 17, 3647–3650. [Google Scholar]
- Information Technology Division, National Cancer Institute of Thailand. Hospital-Based Cancer Registry 2017; Pornsup Printing Co., Ltd.: Bangkok, Thailand, 2018. [Google Scholar]
- Information Technology Division, National Cancer Institute of Thailand. Hospital-Based Cancer Registry 2016; Pornsup Printing Co., Ltd.: Bangkok, Thailand, 2018. [Google Scholar]
- Khuhaprema, T.; Srivatanakul, P. Colon and rectum cancer in Thailand: An overview. Jpn. J. Clin. Oncol. 2008, 38, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Siripongpreeda, B.; Mahidol, C.; Dusitanond, N.; Sriprayoon, T.; Muyphuag, B.; Sricharunrat, T.; Teerayatanakul, N.; Chaiwong, W.; Worasawate, W.; Sattayarungsee, P.; et al. High prevalence of advanced colorectal neoplasia in the Thai population: A prospective screening colonoscopy of 1404 cases. BMC Gastroenterol. 2016, 16, 101. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fedewa, S.A.; Ahnen, D.J.; Meester, R.G.S.; Barzi, A.; Jemal, A. Colorectal cancer statistics, 2017. CA Cancer J. Clin. 2017, 67, 177–193. [Google Scholar] [CrossRef] [PubMed]
- Meester, R.G.; Doubeni, C.A.; Zauber, A.G.; Goede, S.L.; Levin, T.R.; Corley, D.A.; Jemal, A.; Lansdorp-Vogelaar, I. Public health impact of achieving 80% colorectal cancer screening rates in the United States by 2018. Cancer 2015, 121, 2281–2285. [Google Scholar] [CrossRef]
- Kuipers, E.J.; Grady, W.M.; Lieberman, D.; Seufferlein, T.; Sung, J.J.; Boelens, P.G.; van de Velde, C.J.; Watanabe, T. Colorectal cancer. Nat. Rev. Dis. Primers 2015, 1, 15065. [Google Scholar] [CrossRef]
- Vogelstein, B.; Papadopoulos, N.; Velculescu, V.E.; Zhou, S.; Diaz, L.A., Jr.; Kinzler, K.W. Cancer genome landscapes. Science 2013, 339, 1546–1558. [Google Scholar] [CrossRef]
- Muzny, D.M.; Bainbridge, M.N.; Chang, K.; Dinh, H.H.; Drummond, J.A.; Fowler, G.; Kovar, C.L.; Lewis, L.R.; Morgan, M.B.; Newsham, I.F.; et al. Comprehensive molecular characterization of human colon and rectal cancer. Nature 2012, 487, 330–337. [Google Scholar] [CrossRef]
- Carethers, J.M.; Jung, B.H. Genetics and Genetic Biomarkers in Sporadic Colorectal Cancer. Gastroenterology 2015, 149, 1177–1190. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.D.; Parsons, D.W.; Jones, S.; Lin, J.; Sjoblom, T.; Leary, R.J.; Shen, D.; Boca, S.M.; Barber, T.; Ptak, J.; et al. The genomic landscapes of human breast and colorectal cancers. Science 2007, 318, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Guda, K.; Veigl, M.L.; Varadan, V.; Nosrati, A.; Ravi, L.; Lutterbaugh, J.; Beard, L.; Willson, J.K.V.; Sedwick, W.D.; Wang, Z.J.; et al. Novel recurrently mutated genes in African American colon cancers. Proc. Natl. Acad. Sci. USA 2015, 112, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, M.S.; Stojanov, P.; Polak, P.; Kryukov, G.V.; Cibulskis, K.; Sivachenko, A.; Carter, S.L.; Stewart, C.; Mermel, C.H.; Roberts, S.A.; et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 2013, 499, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Brim, H.; Ashktorab, H. Genomics of Colorectal Cancer in African Americans. Next Gener. Seq. Appl. 2016, 3. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.E.; Yang, L.; Zheng, L.T.; Ge, W.T.; Li, D.; Zhang, Y.; Hu, X.D.; Gao, Z.B.; Xu, J.H.; Huang, Y.Q.; et al. Exome Capture Sequencing of Adenoma Reveals Genetic Alterations in Multiple Cellular Pathways at the Early Stage of Colorectal Tumorigenesis. PLoS ONE 2013, 8, e53310. [Google Scholar] [CrossRef]
- Borras, E.; San Lucas, F.A.; Chang, K.; Zhou, R.; Masand, G.; Fowler, J.; Mork, M.E.; You, Y.N.; Taggart, M.W.; McAllister, F.; et al. Genomic Landscape of Colorectal Mucosa and Adenomas. Cancer Prev. Res. 2016, 9, 417–427. [Google Scholar] [CrossRef]
- Lin, S.H.; Raju, G.S.; Huff, C.; Ye, Y.; Gu, J.; Chen, J.S.; Hildebrandt, M.A.T.; Liang, H.; Menter, D.G.; Morris, J.; et al. The somatic mutation landscape of premalignant colorectal adenoma. Gut 2018, 67, 1299–1305. [Google Scholar] [CrossRef]
- Ashktorab, H.; Daremipouran, M.; Devaney, J.; Varma, S.; Rahi, H.; Lee, E.; Shokrani, B.; Schwartz, R.; Nickerson, M.L.; Brim, H. Identification of Novel Mutations by Exome Sequencing in African American Colorectal Cancer Patients. Cancer 2015, 121, 34–42. [Google Scholar] [CrossRef]
- Lawler, M.; Alsina, D.; Adams, R.A.; Anderson, A.S.; Brown, G.; Fearnhead, N.S.; Fenwick, S.W.; Halloran, S.P.; Hochhauser, D.; Hull, M.A.; et al. Critical research gaps and recommendations to inform research prioritisation for more effective prevention and improved outcomes in colorectal cancer. Gut 2018, 67, 179–193. [Google Scholar] [CrossRef]
- Kovaleva, J.; Peters, F.T.M.; van der Mei, H.C.; Degener, J.E. Transmission of Infection by Flexible Gastrointestinal Endoscopy and Bronchoscopy. Clin. Microbiol. Rev. 2013, 26, 231–254. [Google Scholar] [CrossRef] [PubMed]
- Imperiale, T.F.; Ransohoff, D.F.; Itzkowitz, S.H. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 2014, 371, 187–188. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Feng, Q.; Wong, S.H.; Zhang, D.; Liang, Q.Y.; Qin, Y.W.; Tang, L.Q.; Zhao, H.; Stenvang, J.; Li, Y.L.; et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut 2017, 66, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Muguruma, N.; Tanaka, K.; Teramae, S.; Takayama, T. Colon capsule endoscopy: Toward the future. Clin. J. Gastroenterol. 2017, 10, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Mohelnikova-Duchonova, B.; Melichar, B.; Soucek, P. FOLFOX/FOLFIRI pharmacogenetics: The call for a personalized approach in colorectal cancer therapy. World J. Gastroenterol. 2014, 20, 10316–10330. [Google Scholar] [CrossRef]
- Pagano, E.; Borrelli, F.; Orlando, P.; Romano, B.; Monti, M.; Morbidelli, L.; Aviello, G.; Imperatore, R.; Capasso, R.; Piscitelli, F.; et al. Pharmacological inhibition of MAGL attenuates experimental colon carcinogenesis. Pharmacol. Res. 2017, 119, 227–236. [Google Scholar] [CrossRef]
- Giri, A.K.; Aittokallio, T. DNMT inhibitors increase methylation in the cancer genome. Front. Pharmacol. 2019, 10, 385. [Google Scholar] [CrossRef]
- Moon, J.R.; Oh, S.J.; Lee, C.K.; Chi, S.G.; Kim, H.J. TGF-β1 protects colon tumor cells from apoptosis through XAF1 suppression. Int. J. Oncol. 2019, 54, 2117–2126. [Google Scholar] [CrossRef]
- Cai, J.; Wang, H.; Jiao, X.; Huang, R.; Qin, Q.; Zhang, J.; Chen, H.; Feng, D.; Tian, X.; Wang, H. The RNA-binding protein HuR confers oxaliplatin resistance of colorectal cancer by upregulating CDC6. Mol. Cancer Ther. 2019. [Google Scholar] [CrossRef]
- Koustas, E.; Sarantis, P.; Kyriakopoulou, G.; Papavassiliou, A.G.; Karamouzis, M.V.J.C. The Interplay of Autophagy and Tumor Microenvironment in Colorectal Cancer—Ways of Enhancing Immunotherapy Action. Cancers 2019, 11, 533. [Google Scholar] [CrossRef]
- Rodríguez, J.P.; Guijas, C.; Astudillo, A.M.; Rubio, J.M.; Balboa, M.A.; Balsinde, J.J.C. Sequestration of 9-Hydroxystearic Acid in FAHFA (Fatty Acid Esters of Hydroxy Fatty Acids) as a Protective Mechanism for Colon Carcinoma Cells to Avoid Apoptotic Cell Death. Cancers 2019, 11, 524. [Google Scholar] [CrossRef] [PubMed]
- Faris, P.; Pellavio, G.; Ferulli, F.; Di Nezza, F.; Shekha, M.; Lim, D.; Maestri, M.; Guerra, G.; Ambrosone, L.; Pedrazzoli, P.J.C. Nicotinic Acid Adenine Dinucleotide Phosphate (NAADP) Induces Intracellular Ca2+ Release through the Two-Pore Channel TPC1 in Metastatic Colorectal Cancer Cells. Cancers 2019, 11, 542. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Watson, I.R.; Takahashi, K.; Futreal, P.A.; Chin, L. Emerging patterns of somatic mutations in cancer. Nat. Rev. Genet. 2013, 14, 703–718. [Google Scholar] [CrossRef] [PubMed]
- Stratton, M.R.; Campbell, P.J.; Futreal, P.A. The cancer genome. Nature 2009, 458, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Shlien, A.; Malkin, D. Copy number variations and cancer. Genome Med. 2009, 1, 62. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Wang, M.; Zhang, P.; Huang, T. Classification of cancers based on copy number variation landscapes. Biochim. Biophys. Acta 2016, 1860, 2750–2755. [Google Scholar] [CrossRef]
- Xu, J.F.; Kang, Q.; Ma, X.Y.; Pan, Y.M.; Yang, L.; Jin, P.; Wang, X.; Li, C.G.; Chen, X.C.; Wu, C.; et al. A Novel Method to Detect Early Colorectal Cancer Based on Chromosome Copy Number Variation in Plasma. Cell Physiol. Biochem. 2018, 45, 1444–1454. [Google Scholar] [CrossRef]
- Hassan, N.Z.A.; Mokhtar, N.M.; Sin, T.K.; Rose, I.M.; Sagap, I.; Harun, R.; Jamal, R. Integrated Analysis of Copy Number Variation and Genome-Wide Expression Profiling in Colorectal Cancer Tissues. PLoS ONE 2014, 9, e92553. [Google Scholar] [CrossRef]
- Ptashkin, R.N.; Pagan, C.; Yaeger, R.; Middha, S.; Shia, J.; O’Rourke, K.P.; Berger, M.F.; Wang, L.; Cimera, R.; Wang, J.J.; et al. Chromosome 20 q Amplification Defines a Subtype of Microsatellite Stable, Left-Sided Colon Cancers with Wild-type RAS/RAF and Better Overall Survival. Mol. Cancer Res. 2017, 15, 708–713. [Google Scholar] [CrossRef]
- Desgrosellier, J.S.; Cheresh, D.A. Integrins in cancer: Biological implications and therapeutic opportunities. Nat. Rev. Cancer 2010, 10, 890. [Google Scholar] [CrossRef]
- Maziveyi, M.; Alahari, S.K. Cell matrix adhesions in cancer: The proteins that form the glue. Oncotarget 2017, 8, 48471–48487. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Camma, C.; Giunta, M.; Fiorica, F.; Pagliaro, L.; Craxi, A.; Cottone, M. Preoperative radiotherapy for resectable rectal cancer: A meta-analysis. JAMA 2000, 284, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Renehan, A.G.; Egger, M.; Saunders, M.P.; O’Dwyer, S.T. Impact on survival of intensive follow up after curative resection for colorectal cancer: Systematic review and meta-analysis of randomised trials. BMJ 2002, 324, 813. [Google Scholar] [CrossRef]
- McGregor, S.E.; Hilsden, R.J.; Li, F.X.; Bryant, H.E.; Murray, A. Low uptake of colorectal cancer screening 3 yr after release of national recommendations for screening. Am. J. Gastroenterol. 2007, 102, 1727–1735. [Google Scholar] [CrossRef]
- Atkin, W.S.; Edwards, R.; Kralj-Hans, I.; Wooldrage, K.; Hart, A.R.; Northover, J.M.; Parkin, D.M.; Wardle, J.; Duffy, S.W.; Cuzick, J.; et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: A multicentre randomised controlled trial. Lancet 2010, 375, 1624–1633. [Google Scholar] [CrossRef]
- Kuriki, K.; Tajima, K. The increasing incidence of colorectal cancer and the preventive strategy in Japan. Asian Pac. J. Cancer Prev. 2006, 7, 495–501. [Google Scholar]
- Levin, B.; Lieberman, D.A.; McFarland, B.; Andrews, K.S.; Brooks, D.; Bond, J.; Dash, C.; Giardiello, F.M.; Glick, S.; Johnson, D.; et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 2008, 134, 1570–1595. [Google Scholar] [CrossRef]
- Smith, R.A.; Andrews, K.S.; Brooks, D.; Fedewa, S.A.; Manassaram-Baptiste, D.; Saslow, D.; Brawley, O.W.; Wender, R.C. Cancer screening in the United States, 2017: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J. Clin. 2017, 67, 100–121. [Google Scholar] [CrossRef]
- Zhang, L.; Shay, J.W. Multiple Roles of APC and its Therapeutic Implications in Colorectal Cancer. J. Natl. Cancer Inst. 2017, 109. [Google Scholar] [CrossRef] [PubMed]
- Gao, C.; Wang, Y.; Broaddus, R.; Sun, L.; Xue, F.; Zhang, W. Exon 3 mutations of CTNNB1 drive tumorigenesis: A review. Oncotarget 2018, 9, 5492–5508. [Google Scholar] [CrossRef] [PubMed]
- Reaves, D.K.; Hoadley, K.A.; Fagan-Solis, K.D.; Jima, D.D.; Bereman, M.; Thorpe, L.; Hicks, J.; McDonald, D.; Troester, M.A.; Perou, C.M.; et al. Nuclear Localized LSR: A Novel Regulator of Breast Cancer Behavior and Tumorigenesis. Mol. Cancer Res. 2017, 15, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Marshall, H.; Bhaumik, M.; Aviv, H.; Moore, D.; Yao, M.; Dutta, J.; Rahim, H.; Gounder, M.; Ganesan, S.; Saleem, A.; et al. Deficiency of the dual ubiquitin/SUMO ligase Topors results in genetic instability and an increased rate of malignancy in mice. BMC Mol. Biol. 2010, 11, 31. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Choi, P.S.; Francis, J.M.; Gao, G.F.; Campbell, J.D.; Ramachandran, A.; Mitsuishi, Y.; Ha, G.; Shih, J.; Vazquez, F.; et al. Somatic Superenhancer Duplications and Hotspot Mutations Lead to Oncogenic Activation of the KLF5 Transcription Factor. Cancer Discov. 2018, 8, 108–125. [Google Scholar] [CrossRef] [PubMed]
- Vigneri, P.G.; Tirro, E.; Pennisi, M.S.; Massimino, M.; Stella, S.; Romano, C.; Manzella, L. The Insulin/IGF System in Colorectal Cancer Development and Resistance to Therapy. Front. Oncol. 2015, 5, 230. [Google Scholar] [CrossRef]
- Prevostel, C.; Rammah-Bouazza, C.; Trauchessec, H.; Canterel-Thouennon, L.; Busson, M.; Ychou, M.; Blache, P. SOX9 is an atypical intestinal tumor suppressor controlling the oncogenic Wnt/ss-catenin signaling. Oncotarget 2016, 7, 82228–82243. [Google Scholar] [CrossRef]
- Randon, G.; Fucà, G.; Rossini, D.; Raimondi, A.; Pagani, F.; Perrone, F.; Tamborini, E.; Busico, A.; Peverelli, G.; Morano, F. Prognostic impact of ATM mutations in patients with metastatic colorectal cancer. Sci. Rep. 2019, 9, 2858. [Google Scholar] [CrossRef]
- Wolff, R.K.; Hoffman, M.D.; Wolff, E.C.; Herrick, J.S.; Sakoda, L.C.; Samowitz, W.S.; Slattery, M.L. Mutation analysis of adenomas and carcinomas of the colon: Early and late drivers. Genes Chromosome Cancer 2018, 57, 366–376. [Google Scholar] [CrossRef]
- Li, T.; Yi, L.; Hai, L.; Ma, H.W.; Tao, Z.N.; Zhang, C.; Abeysekera, I.R.; Zhao, K.; Yang, Y.H.; Wang, W.; et al. The interactome and spatial redistribution feature of Ca2+ receptor protein calmodulin reveals a novel role in invadopodia-mediated invasion. Cell Death Dis. 2018, 9, 292. [Google Scholar] [CrossRef]
- Cruciat, C.M.; Niehrs, C. Secreted and Transmembrane Wnt Inhibitors and Activators. Cold Spring Harb. Perspect. Biol. 2013, 3, a015081. [Google Scholar] [CrossRef] [PubMed]
- Furushima, K.; Yamamoto, A.; Nagano, T.; Shibata, M.; Miyachi, H.; Abe, T.; Ohshima, N.; Kiyonari, H.; Aizawa, S. Mouse homologues of Shisa antagonistic to Wnt and Fgf signalings. Dev. Biol. 2007, 306, 480–492. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Liao, W.; Zhang, L.; Tu, X.; Hu, J.; Chen, T.; Dai, X.; Xiong, Y.; Liang, W.; Ding, C.; et al. RSPO2 suppresses colorectal cancer metastasis by counteracting the Wnt5a/Fzd7-driven noncanonical Wnt pathway. Cancer Lett. 2017, 402, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Shi, F.; Cai, F.F.; Cai, L.; Lin, X.Y.; Zhang, W.; Wang, Q.Q.; Zhao, Y.J.; Ni, Q.C.; Wang, H.; He, Z.X. Overexpression of SYF2 promotes cell proliferation and correlates with poor prognosis in human breast cancer. Oncotarget 2017, 8, 88453–88463. [Google Scholar] [CrossRef] [PubMed]
- Abdelmaksoud-Damak, R.; Miladi-Abdennadher, I.; Triki, M.; Khabir, A.; Charfi, S.; Ayadi, L.; Frikha, M.; Sellami-Boudawara, T.; Mokdad-Gargouri, R. Expression and mutation pattern of beta-catenin and adenomatous polyposis coli in colorectal cancer patients. Arch. Med. Res. 2015, 46, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Hasanpour, M.; Galehdari, H.; Masjedizadeh, A.; Ajami, N. A unique profile of adenomatous polyposis coli gene mutations in Iranian patients suffering sporadic colorectal cancer. Cell J. 2014, 16, 17–24. [Google Scholar] [PubMed]
- Voorham, Q.J.; Carvalho, B.; Spiertz, A.J.; Claes, B.; Mongera, S.; van Grieken, N.C.; Grabsch, H.; Kliment, M.; Rembacken, B.; van de Wiel, M.A.; et al. Comprehensive mutation analysis in colorectal flat adenomas. PLoS ONE 2012, 7, e41963. [Google Scholar] [CrossRef]
- Giovannucci, E. Insulin, insulin-like growth factors and colon cancer: A review of the evidence. J. Nutr. 2001, 131, 3109S–3120S. [Google Scholar] [CrossRef]
- Fukuda, R.; Hirota, K.; Fan, F.; Do Jung, Y.; Ellis, L.M.; Semenza, G.L. Insulin-like growth factor 1 induces hypoxia-inducible factor 1-mediated vascular endothelial growth factor expression, which is dependent on MAP kinase and phosphatidylinositol 3-kinase signaling in colon cancer cells. J. Biol. Chem. 2002, 277, 38205–38211. [Google Scholar] [CrossRef]
- McConnell, B.B.; Bialkowska, A.B.; Nandan, M.O.; Ghaleb, A.M.; Gordon, F.J.; Yang, V.W. Haploinsufficiency of Kruppel-like factor 5 rescues the tumor-initiating effect of the Apc(Min) mutation in the intestine. Cancer Res. 2009, 69, 4125–4133. [Google Scholar] [CrossRef]
- Kwong, L.N.; Dove, W.F. APC and Its Modifiers in Colon Cancer. Adv. Exp. Med. Biol. 2009, 656, 85–106. [Google Scholar] [CrossRef] [PubMed]
- Nandan, M.O.; Ghaleb, A.M.; McConnell, B.B.; Patel, N.V.; Robine, S.; Yang, V.W. Kruppel-like factor 5 is a crucial mediator of intestinal tumorigenesis in mice harboring combined ApcMin and KRASV12 mutations. Mol. Cancer 2010, 9, 63. [Google Scholar] [CrossRef] [PubMed]
- Sjoblom, T.; Jones, S.; Wood, L.D.; Parsons, D.W.; Lin, J.; Barber, T.D.; Mandelker, D.; Leary, R.J.; Ptak, J.; Silliman, N.; et al. The consensus coding sequences of human breast and colorectal cancers. Science 2006, 314, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Bruun, J.; Kolberg, M.; Nesland, J.M.; Svindland, A.; Nesbakken, A.; Lothe, R.A. Prognostic Significance of beta-Catenin, E-Cadherin, and SOX9 in Colorectal Cancer: Results from a Large Population-Representative Series. Front. Oncol. 2014, 4, 118. [Google Scholar] [CrossRef] [PubMed]
- Seshagiri, S.; Stawiski, E.W.; Durinck, S.; Modrusan, Z.; Storm, E.E.; Conboy, C.B.; Chaudhuri, S.; Guan, Y.H.; Janakiraman, V.; Jaiswal, B.S.; et al. Recurrent R-spondin fusions in colon cancer. Nature 2012, 488, 660. [Google Scholar] [CrossRef]
- Lu, B.; Fang, Y.; Xu, J.; Wang, L.; Xu, F.; Xu, E.; Huang, Q.; Lai, M. Analysis of SOX9 expression in colorectal cancer. Am. J. Clin. Pathol. 2008, 130, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Matheu, A.; Collado, M.; Wise, C.; Manterola, L.; Cekaite, L.; Tye, A.J.; Canamero, M.; Bujanda, L.; Schedl, A.; Cheah, K.S.E.; et al. Oncogenicity of the Developmental Transcription Factor Sox9. Cancer Res. 2012, 72, 1301–1315. [Google Scholar] [CrossRef]
- Zhan, T.; Rindtorff, N.; Boutros, M. Wnt signaling in cancer. Oncogene 2017, 36, 1461–1473. [Google Scholar] [CrossRef]
- Suleiman, S.H.; Koko, M.E.; Nasir, W.H.; Elfateh, O.; Elgizouli, U.K.; Abdallah, M.O.E.; Alfarouk, K.O.; Hussain, A.; Faisal, S.; Ibrahim, F.M.A.; et al. Exome sequencing of a colorectal cancer family reveals shared mutation pattern and predisposition circuitry along tumor pathways. Front. Genet. 2015, 6. [Google Scholar] [CrossRef]
- Fearnhead, N.S.; Wilding, J.L.; Bodmer, W.F. Genetics of colorectal cancer: Hereditary aspects and overview of colorectal tumorigenesis. Br. Med. Bull. 2002, 64, 27–43. [Google Scholar] [CrossRef]
- Rusan, N.M.; Peifer, M. Original CIN: Reviewing roles for APC in chromosome instability. J. Cell Biol. 2008, 181, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Druliner, B.R.; Wang, P.W.; Bae, T.; Baheti, S.; Slettedahl, S.; Mahoney, D.; Vasmatzis, N.; Xu, H.; Kim, M.; Bockol, M.; et al. Molecular characterization of colorectal adenomas with and without malignancy reveals distinguishing genome, transcriptome and methylome alterations. Sci. Rep. 2018, 8, 3161. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009, 25, 1754–1760. [Google Scholar] [CrossRef] [PubMed]
- Boardinstitute. Picard Tools by Broad Institute. Available online: www.broadinstitute.github.io/picard (accessed on 6 May 2016).
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.; Daly, M.; et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef] [PubMed]
- Cibulskis, K.; Lawrence, M.S.; Carter, S.L.; Sivachenko, A.; Jaffe, D.; Sougnez, C.; Gabriel, S.; Meyerson, M.; Lander, E.S.; Getz, G. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 2013, 31, 213–219. [Google Scholar] [CrossRef]
- McLaren, W.; Gil, L.; Hunt, S.E.; Riat, H.S.; Ritchie, G.R.; Thormann, A.; Flicek, P.; Cunningham, F. The Ensembl Variant Effect Predictor. Genome Biol. 2016, 17, 122. [Google Scholar] [CrossRef]
- Sathirapongsasuti, J.F.; Lee, H.; Horst, B.A.; Brunner, G.; Cochran, A.J.; Binder, S.; Quackenbush, J.; Nelson, S.F. Exome sequencing-based copy-number variation and loss of heterozygosity detection: ExomeCNV. Bioinformatics 2011, 27, 2648–2654. [Google Scholar] [CrossRef]
- Ivakhno, S.; Tavare, S. CNAnova: A new approach for finding recurrent copy number abnormalities in cancer SNP microarray data. Bioinformatics 2010, 26, 1395–1402. [Google Scholar] [CrossRef]
- Kuleshov, M.V.; Jones, M.R.; Rouillard, A.D.; Fernandez, N.F.; Duan, Q.; Wang, Z.; Koplev, S.; Jenkins, S.L.; Jagodnik, K.M.; Lachmann, A.; et al. Enrichr: A comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016, 44, W90–W97. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.Y.; Tan, C.M.; Kou, Y.; Duan, Q.; Wang, Z.; Meirelles, G.V.; Clark, N.R.; Ma’ayan, A. Enrichr: Interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinform. 2013, 14, 128. [Google Scholar] [CrossRef] [PubMed]

| Patient | Chr | Start | Stop | Reference | Alternative | Gene | Mutation | Exonic Function | Protein Change | Known |
|---|---|---|---|---|---|---|---|---|---|---|
| p5t | 5 | 112174631 | 112174631 | C | T | APC | SNV | Stop gain | p.Arg1114Ter | rs121913331, COSM13125 |
| p10t | 5 | 112151185 | 112151185 | T | G | APC | SNV | Splice Region variant | - | |
| p14t | 5 | 112155021 | 112155022 | TG | - | APC | deletion | Frame shift variant | p.Met431ArgfsTer12 | |
| p4low | 5 | 112175639 | 112175639 | C | T | APC | SNV | Stop gain | p.Arg1450Ter | rs121913332, COSM13127 |
| p6low | 5 | 112174249 | 112174249 | T | A | APC | SNV | Stop gain | p.Tyr986Ter | |
| p7low | 5 | 112174129 | 112174129 | A | - | APC | deletion | Frame shift variant | p.Cys947ValfsTer8 | |
| p7low | 5 | 112175255 | 112175255 | G | T | APC | SNV | Stop gain | p.Glu1322Ter | |
| p10low | 5 | 112175390 | 112175391 | - | A | APC | Insertion | Frame shift variant | p.Thr1368AspfsTer7 | |
| p11low | 5 | 112175639 | 112175639 | C | T | APC | SNV | Stop gain | p.Arg1450Ter | rs121913332, COSM13127 |
| p12low | 5 | 112155031 | 112155032 | - | A | APC | Insertion | Frame shift variant | p.Asn436LysfsTer8 | |
| p2t | 17 | 7578510 | 7578510 | G | - | TP53 | Deletion | Frame shift variant | p.C141Afs*29 | COSM69019 |
| p10t | 17 | 7576889 | 7576890 | - | T | TP53 | Insertion | Frame shift variant | p.K320Efs*17 | |
| p4t | 17 | 70119862 | 70119863 | - | TTCGA | SOX9 | Insertion | Missense mutation | p.V291Sfs*94 | |
| p5t | 17 | 70119855 | 70119856 | - | CGAGA | SOX9 | Insertion | Frame shift variant | p.F289Rfs*96 | |
| p10t | 17 | 70118889 | 70118889 | A | A | SOX9 | SNV | Frame shift variant | p.F154Y | |
| p4low | 3 | 41274898 | 41274898 | G | C | CTNNB1 | SNV | Missense mutation | p.Trp383Ser | |
| p13low | 3 | 41266124 | 41266124 | A | G | CTNNB1 | SNV | Missense mutation | p.Thr41Ala | rs121913412 |
| p14low | 3 | 41266097 | 41266097 | G | A | CTNNB1 | SNV | Missense mutation | p.Asp32Asn | rs28931588 |
| p14low | 4 | 153258983 | 153258983 | G | A | FBXW7 | SNV | Stop gain | p.Arg278Ter | |
| p14t | 4 | 153268102 | 153268102 | C | - | FBXW7 | Deletion | Frame shift variant | p.Glu236AsnfsTer3 |
| Patient | Gender/Age | Adenoma | Adenocarcinoma | Stage/TNM | LVI | Location |
|---|---|---|---|---|---|---|
| p2 | M/65 | TA | A | I/pT2N0M0 | Y | L |
| p4 | M/55 | TA | A | IIA/pT3N0M0 | N | L |
| p5 | F/58 | SA | A | IIA/pT3N0M0 | Y | L |
| p6 | M/64 | TA | - | - | N | L |
| p7 | M/58 | TA | - | - | N | L |
| p10 | F/56 | TA | A | IIA/pT3N0M0 | Y | R |
| p11 | M/58 | TA | - | - | N | L |
| p12 | M/60 | TA | - | - | N | L |
| p13 | M/61 | TA | - | - | N | L |
| p13_2 | M/61 | SA | - | - | N | L |
| p14 | M/66 | TA | A | IIA/pT3N0M0 | N | L |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Intarajak, T.; Udomchaiprasertkul, W.; Bunyoo, C.; Yimnoon, J.; Soonklang, K.; Wiriyaukaradecha, K.; Lamlertthon, W.; Sricharunrat, T.; Chaiwiriyawong, W.; Siriphongpreeda, B.; et al. Genetic Aberration Analysis in Thai Colorectal Adenoma and Early-Stage Adenocarcinoma Patients by Whole-Exome Sequencing. Cancers 2019, 11, 977. https://doi.org/10.3390/cancers11070977
Intarajak T, Udomchaiprasertkul W, Bunyoo C, Yimnoon J, Soonklang K, Wiriyaukaradecha K, Lamlertthon W, Sricharunrat T, Chaiwiriyawong W, Siriphongpreeda B, et al. Genetic Aberration Analysis in Thai Colorectal Adenoma and Early-Stage Adenocarcinoma Patients by Whole-Exome Sequencing. Cancers. 2019; 11(7):977. https://doi.org/10.3390/cancers11070977
Chicago/Turabian StyleIntarajak, Thoranin, Wandee Udomchaiprasertkul, Chakrit Bunyoo, Jutamas Yimnoon, Kamonwan Soonklang, Kriangpol Wiriyaukaradecha, Wisut Lamlertthon, Thaniya Sricharunrat, Worawit Chaiwiriyawong, Bunchorn Siriphongpreeda, and et al. 2019. "Genetic Aberration Analysis in Thai Colorectal Adenoma and Early-Stage Adenocarcinoma Patients by Whole-Exome Sequencing" Cancers 11, no. 7: 977. https://doi.org/10.3390/cancers11070977
APA StyleIntarajak, T., Udomchaiprasertkul, W., Bunyoo, C., Yimnoon, J., Soonklang, K., Wiriyaukaradecha, K., Lamlertthon, W., Sricharunrat, T., Chaiwiriyawong, W., Siriphongpreeda, B., Sutheeworapong, S., Kusonmano, K., Kittichotirat, W., Thammarongtham, C., Jenjaroenpun, P., Wongsurawat, T., Nookaew, I., Auewarakul, C., & Cheevadhanarak, S. (2019). Genetic Aberration Analysis in Thai Colorectal Adenoma and Early-Stage Adenocarcinoma Patients by Whole-Exome Sequencing. Cancers, 11(7), 977. https://doi.org/10.3390/cancers11070977






