Expression of TMBIM6 in Cancers: The Involvement of Sp1 and PKC
Abstract
1. Introduction
2. Results
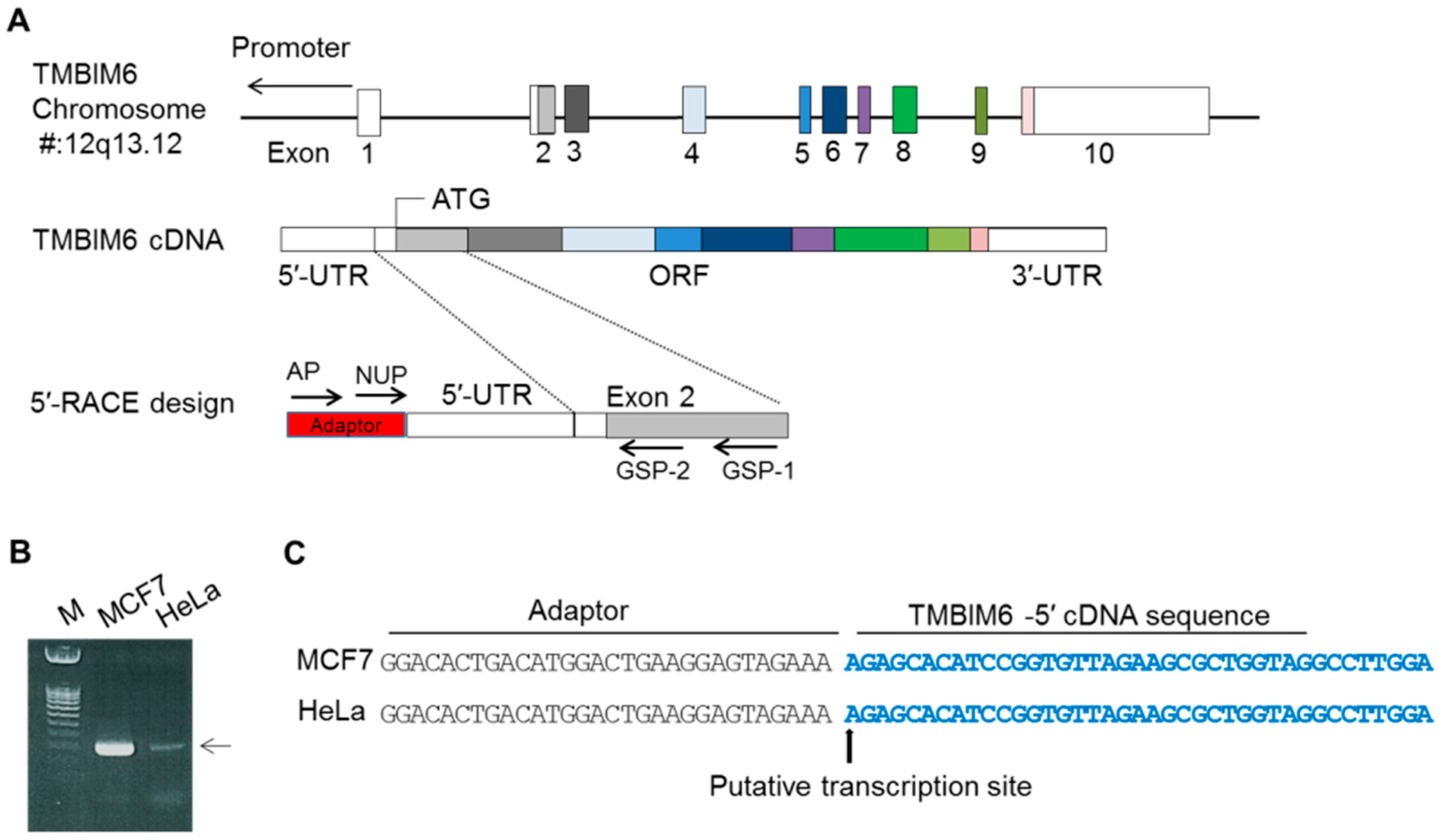
2.1. Mapping of Transcription Start Site (TSS) of Human TMBIM6 Gene
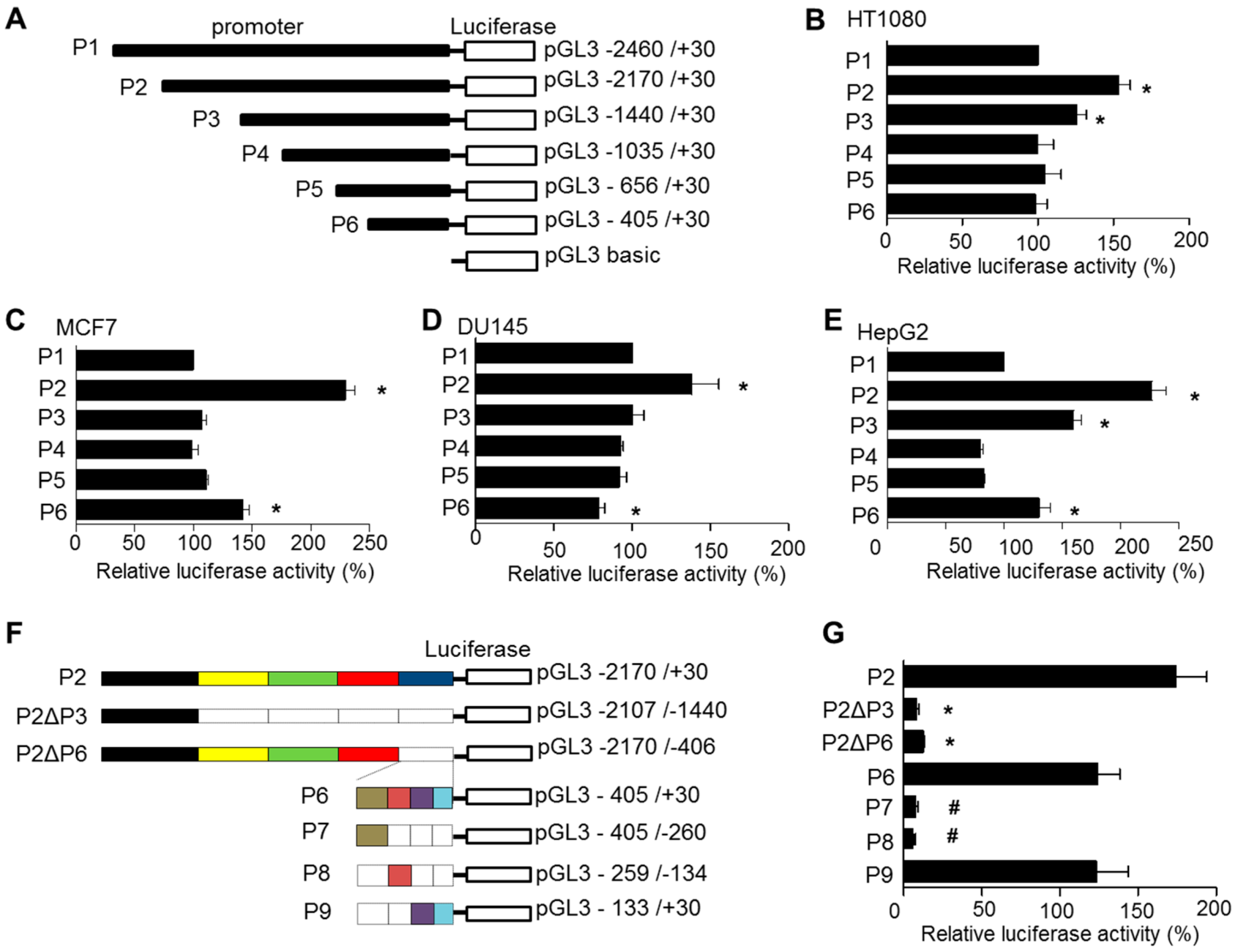
2.2. Identification of the Proximal Promoter Region of TMBIM6
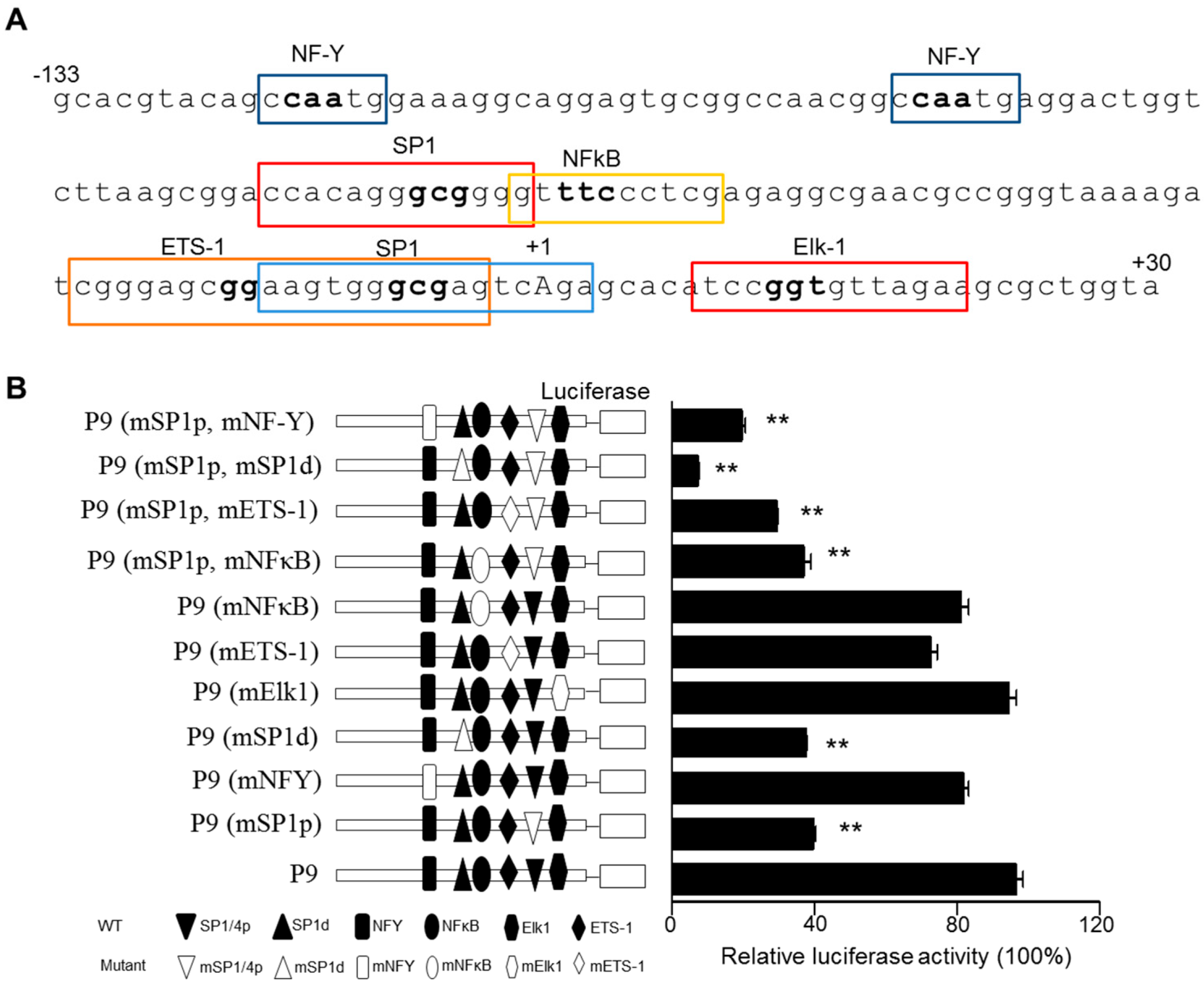
2.3. Analysis of the Proximal Promoter of the TMBIM6 Gene for Potential Interacting Factors
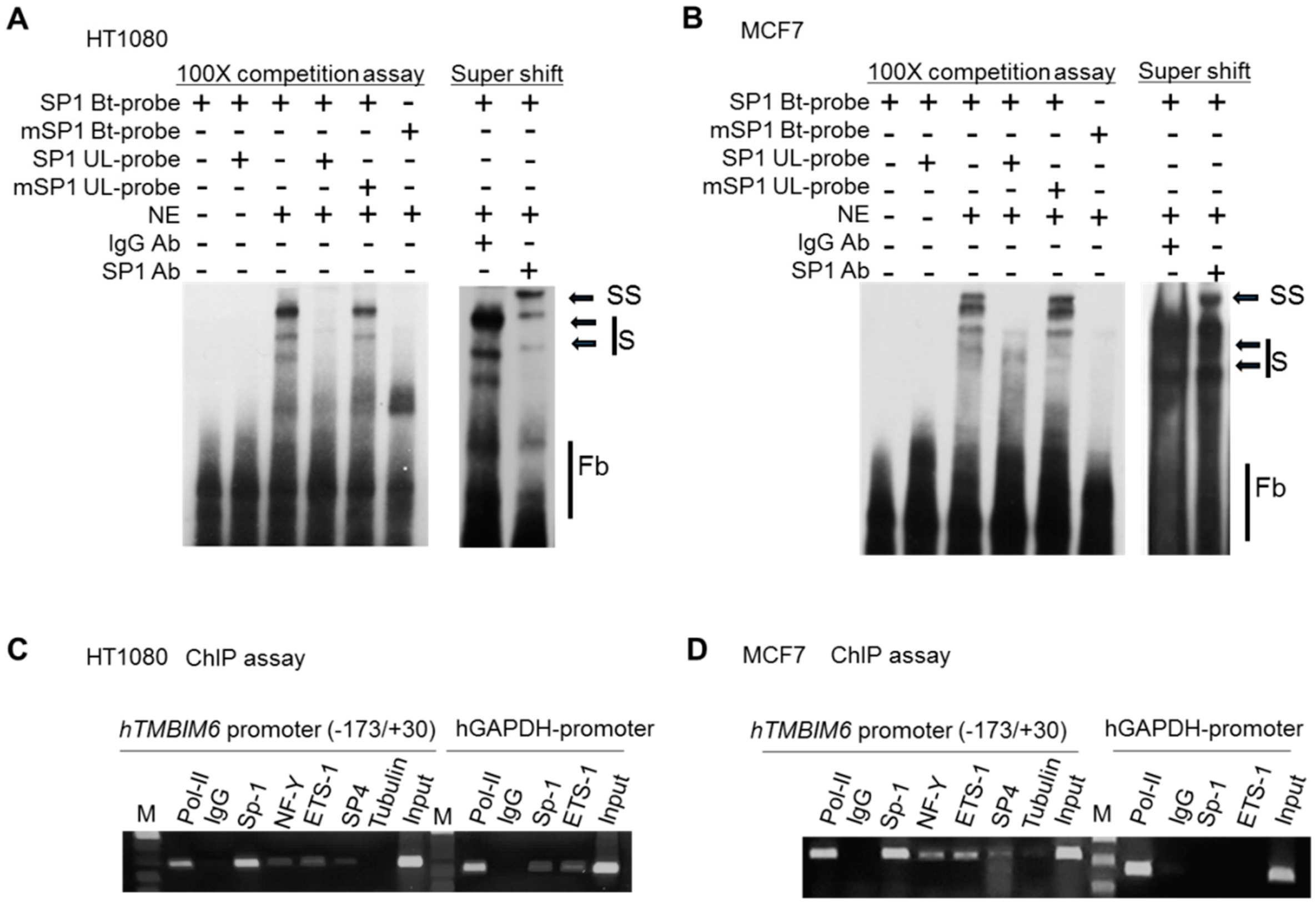
2.4. Sp1 Binds to the TMBIM6 Promoter: EMSA and ChIP Assay
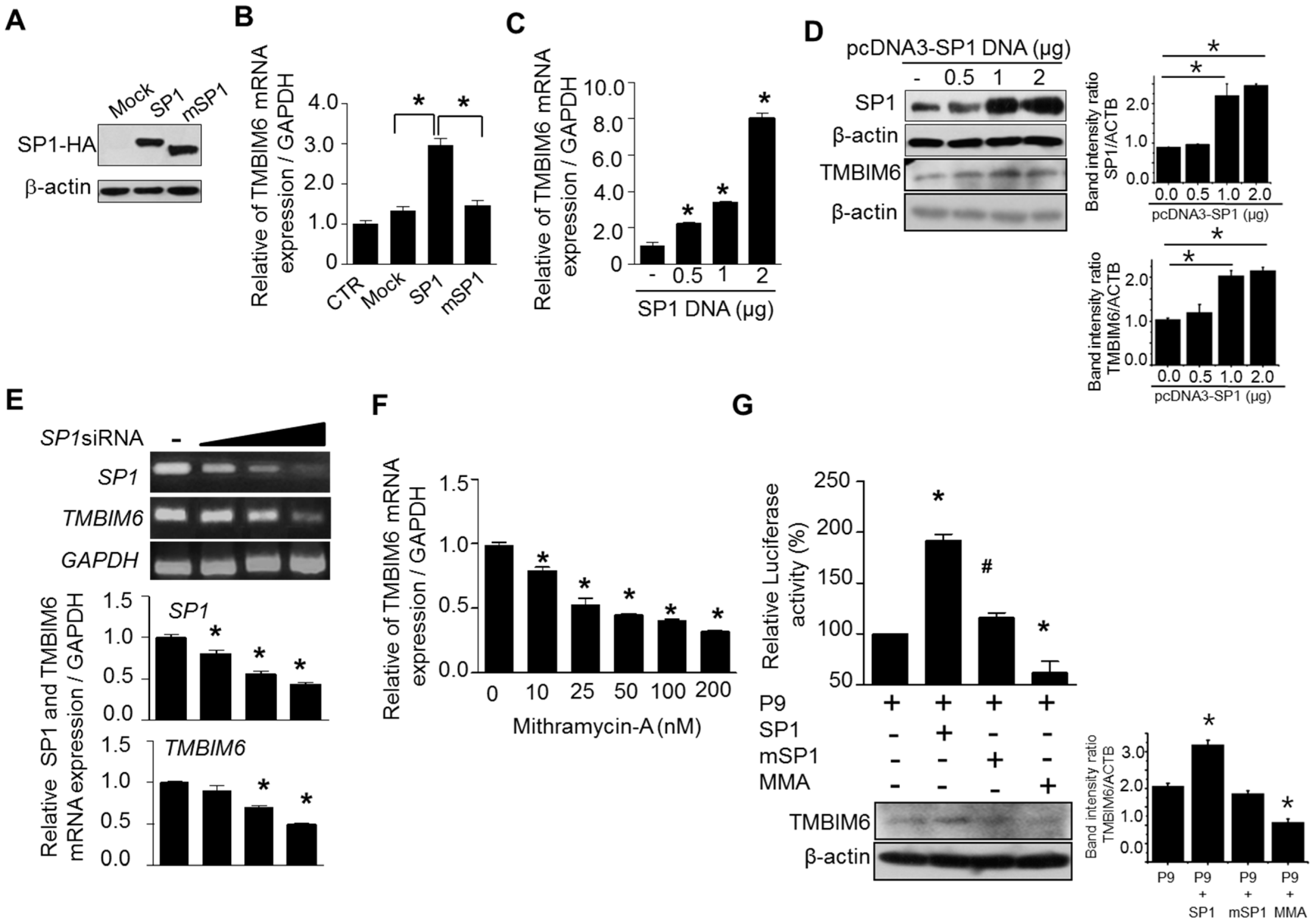
2.5. Regulation of Sp1 Controls TMBIM6 Promoter Activity and mRNA Expression
2.6. Sp1-Dependent TMBIM6 Expression Protects against Stress
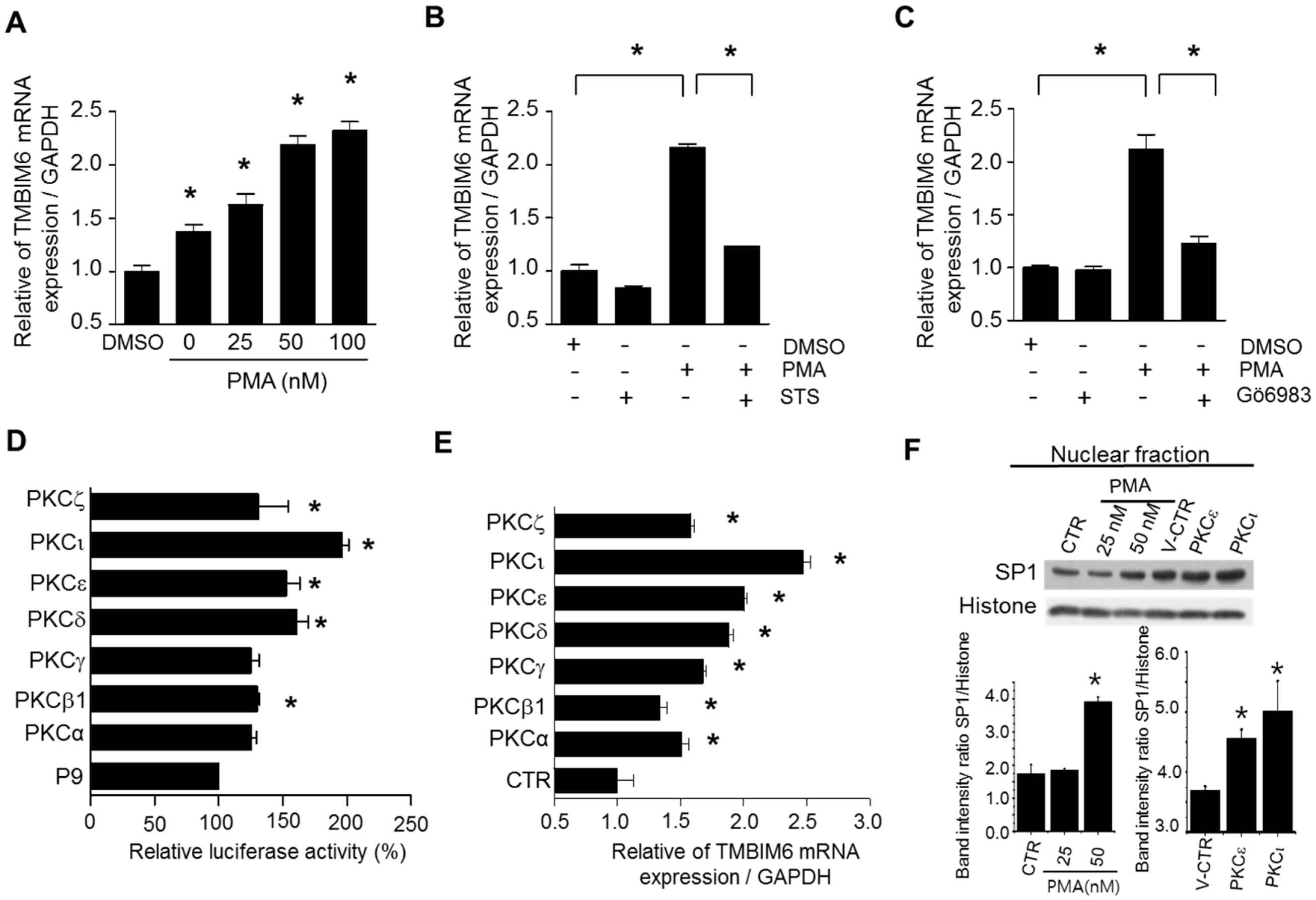
2.7. PMA Enhances Endogenous TMBIM6 mRNA Expression
2.8. PKCι, PKCε, and PKCδ Isoforms Enhance TMBIM6 Gene Expression
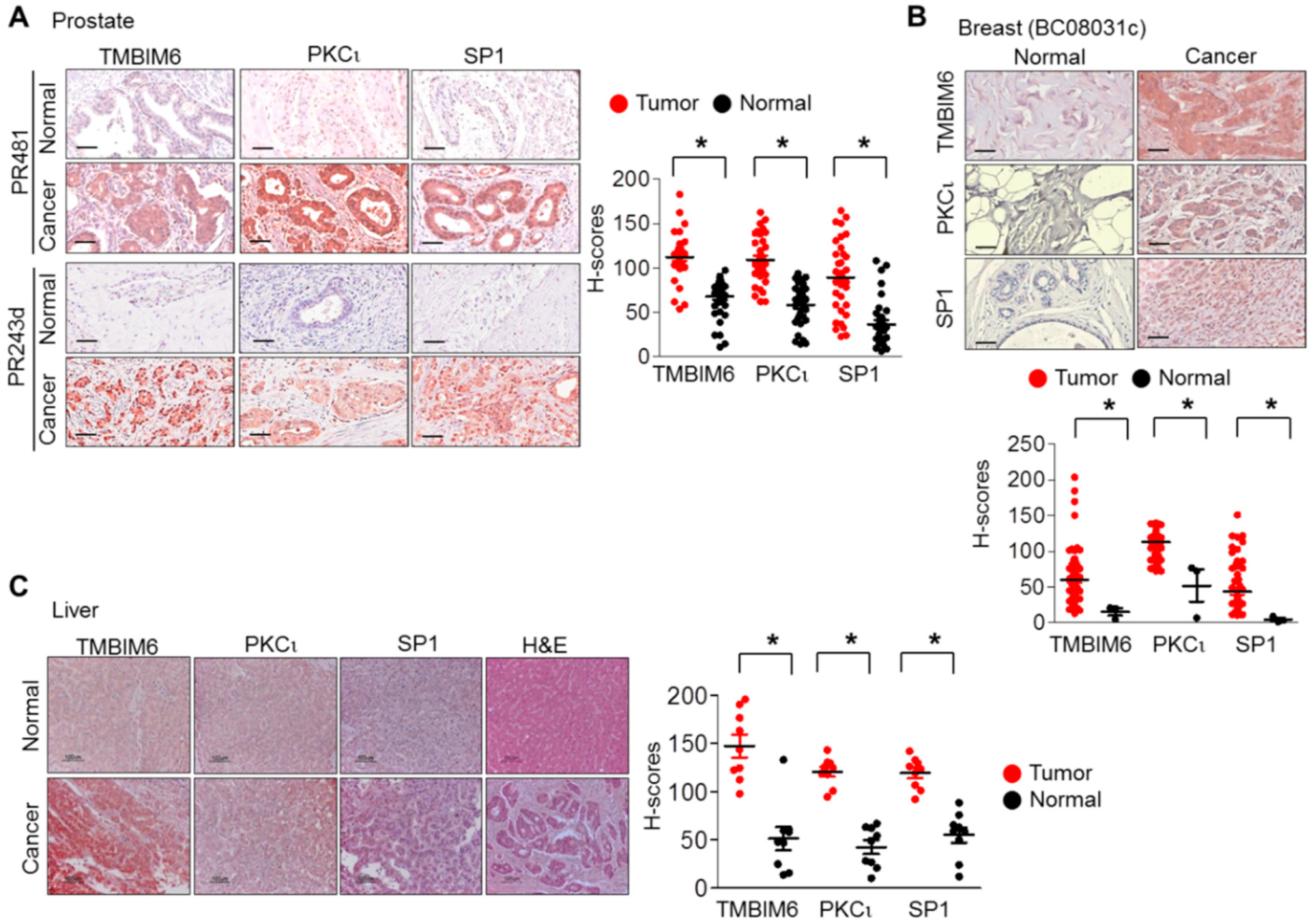
2.9. Expression Levels of PKCι, Sp1, and TMBIM6 in Human Breast, Prostate, and Liver Cancers
3. Discussion
4. Materials and Methods
4.1. Reagents and Expression Plasmids
4.2. Cell Culture
4.3. Quantitative Real-Time PCR (qRT-PCR)
4.4. Transcription Start Site Determination by 5′-RACE-PCR
4.5. Isolation of the 5′ Flanking Region/Promoter of the Human TMBIM6 Gene
4.6. Generation of TMBIM6 Promoter-Luciferase Reporter Plasmid Constructs
4.7. Luciferase Activity and TMBIM6 mRNA Induction
4.8. Site-Directed Mutagenesis Analysis
4.9. Chromatin Immunoprecipitation (ChIP) Assay
4.10. Electrophoretic Mobility Shift (EMSA) and Supershift Assays
4.11. DNA Sequence Alignment and Database Analysis of the 5′-Flanking Region of TMBIM6
4.12. Stimulation or Inhibition of Promoter Activity and Endogenous TMBIM6 mRNA Expression
4.13. Western Blotting
4.14. Immunohistochemistry
4.15. Cell Viability Assay
4.16. TCGA Data Acquisition and Analysis
4.17. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Ishikawa, T.; Watanabe, N.; Nagano, M.; Kawai-Yamada, M.; Lam, E. Bax inhibitor-1: A highly conserved endoplasmic reticulum-resident cell death suppressor. Cell Death Differ. 2011, 18, 1271–1278. [Google Scholar] [CrossRef] [PubMed]
- Walter, L.; Marynen, P.; Szpirer, J.; Levan, G.; Gunther, E. Identification of a novel conserved human gene, TEGT. Genomics 1995, 28, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Reed, J.C. Bax inhibitor-1, a mammalian apoptosis suppressor identified by functional screening in yeast. Mol. Cell 1998, 1, 337–346. [Google Scholar] [CrossRef]
- Chae, H.J.; Kim, H.R.; Xu, C.; Bailly-Maitre, B.; Krajewska, M.; Krajewski, S.; Banares, S.; Cui, J.; Digicaylioglu, M.; Ke, N.; et al. BI-1 regulates an apoptosis pathway linked to endoplasmic reticulum stress. Mol. Cell 2004, 15, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Lisak, D.A.; Schacht, T.; Enders, V.; Habicht, J.; Kiviluoto, S.; Schneider, J.; Henke, N.; Bultynck, G.; Methner, A. The transmembrane Bax inhibitor motif (TMBIM) containing protein family: Tissue expression, intracellular localization and effects on the ER CA(2)(+)-filling state. Biochim. Biophys. Acta 2015, 1853, 2104–2114. [Google Scholar] [CrossRef] [PubMed]
- Reimers, K.; Choi, C.Y.; Bucan, V.; Vogt, P.M. The Bax Inhibitor-1 (BI-1) family in apoptosis and tumorigenesis. Curr. Mol. Med. 2008, 8, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Li, X.Y.; Chen, Y.-C.; Zhou, K.-Y.; Zhang, M.-H.; Luo, H.-Q.; Kung, H.-F.; Zhou, X. Overexpression of Bax inhibitor-1 (BI-1) induces cell transformation in NIH3T3 cells. Cell Biol. Int. 2010, 34, 1099–1104. [Google Scholar] [CrossRef]
- Lu, B.; Li, Y.; Li, H.; Zhang, Y.; Xu, J.; Ren, L.; Fu, S.; Zhou, Y. Bax inhibitor-1 is overexpressed in non-small cell lung cancer and promotes its progression and metastasis. Int. J. Clin. Exp. Pathol. 2015, 8, 1411–1418. [Google Scholar]
- Grzmil, M.; Kaulfuss, S.; Thelen, P.; Hemmerlein, B.; Schweyer, S.; Obenauer, S.; Kang, T.W.; Burfeind, P. Expression and functional analysis of Bax inhibitor-1 in human breast cancer cells. J. Pathol. 2006, 208, 340–349. [Google Scholar] [CrossRef]
- Grzmil, M.; Thelen, P.; Hemmerlein, B.; Schweyer, S.; Voigt, S.; Mury, D.; Burfeind, P. Bax inhibitor-1 is overexpressed in prostate cancer and its specific down-regulation by RNA interference leads to cell death in human prostate carcinoma cells. Am. J. Pathol. 2003, 163, 543–552. [Google Scholar] [CrossRef]
- Tanaka, R.; Ishiyama, T.; Uchihara, T.; Inadome, Y.; Iijima, T.; Morishita, Y.; Kano, J.; Goya, T.; Noguchi, M. Expression of the Bax inhibitor-1 gene in pulmonary adenocarcinoma. Cancer 2006, 106, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wang, L.; Ye, Y.; Aakre, J.A.; Pu, X.; Chang, G.C.; Yang, P.C.; Roth, J.A.; Marks, R.S.; Lippman, S.M.; et al. Genome-wide association study of genetic predictors of overall survival for non-small cell lung cancer in never smokers. Cancer Res. 2013, 73, 4028–4038. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, M.; Li, J.; Feng, Z.; Su, J.; Li, J. Expression of BI-1 protein and its significance in breast cancer. Chin. -Ger. J. Clin. Oncol. 2009, 8, 160–163. [Google Scholar] [CrossRef]
- Zhang, M.; Li, X.; Zhang, Y.; Zhou, K. Bax inhibitor-1 mediates apoptosis-resistance in human nasopharyngeal carcinoma cells. Mol. Cell. Biochem. 2010, 333, 1. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.H.; Yan, C.; Shin, S.J.; Hong, S.C.; Ahn, T.; Moon, A.; Park, S.J.; Lee, Y.C.; Yoo, W.H.; Kim, H.T.; et al. BAX inhibitor-1 enhances cancer metastasis by altering glucose metabolism and activating the sodium-hydrogen exchanger: The alteration of mitochondrial function. Oncogene 2010, 29, 2130–2141. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.R.; Lee, G.H.; Cho, E.Y.; Chae, S.W.; Ahn, T.; Chae, H.J. Bax inhibitor 1 regulates ER-stress-induced ROS accumulation through the regulation of cytochrome P450 2E1. J. Cell Sci. 2009, 122, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q. TMBIM-mediated Ca2+ homeostasis and cell death. Biochim. Biophys. Acta Mol. Cell Res. 2017, 1864, 850–857. [Google Scholar] [CrossRef]
- Hossain, M.K.; Saha, S.K.; Abdal Dayem, A.; Kim, J.H.; Kim, K.; Yang, G.M.; Choi, H.Y.; Cho, S.G. Bax Inhibitor-1 Acts as an Anti-Influenza Factor by Inhibiting ROS Mediated Cell Death and Augmenting Heme-Oxygenase 1 Expression in Influenza Virus Infected Cells. Int. J. Mol. Sci. 2018, 19, 712. [Google Scholar] [CrossRef]
- Lisak, D.; Schacht, T.; Gawlitza, A.; Albrecht, P.; Aktas, O.; Koop, B.; Gliem, M.; Hofstetter, H.H.; Zanger, K.; Bultynck, G.; et al. BAX inhibitor-1 is a Ca2+ channel critically important for immune cell function and survival. Cell Death Differ. 2016, 23, 358–368. [Google Scholar] [CrossRef]
- Jeon, K.; Lim, H.; Kim, J.H.; Han, D.; Lee, E.R.; Yang, G.M.; Song, M.K.; Cho, S.G. Bax inhibitor-1 enhances survival and neuronal differentiation of embryonic stem cells via differential regulation of mitogen-activated protein kinases activities. Biochim. Biophys. Acta 2012, 1823, 2190–2200. [Google Scholar] [CrossRef]
- Jean, J.C.; Oakes, S.M.; Joyce-Brady, M. The Bax inhibitor-1 gene is differentially regulated in adult testis and developing lung by two alternative TATA-less promoters. Genomics 1999, 57, 201–208. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McKnight, S.L.; Kingsbury, R. Transcriptional control signals of a eukaryotic protein-coding gene. Science 1982, 217, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Soh, J.W.; Weinstein, I.B. Roles of specific isoforms of protein kinase C in the transcriptional control of cyclin D1 and related genes. J. Biol. Chem. 2003, 278, 34709–34716. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Wang, X.; Evers, B.M. Induction of cIAP-2 in human colon cancer cells through PKC delta/NF-kappa B. J. Biol. Chem. 2003, 278, 51091–51099. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, A.A.; Ma, X.; Wang, N.; Hombach-Klonisch, S.; Penner, C.; Ozturk, A.; Klonisch, T.; Pitz, M.; Murphy, L.; Leygue, E.; et al. Claudin 1 Is Highly Upregulated by PKC in MCF7 Human Breast Cancer Cells and Correlates Positively with PKCepsilon in Patient Biopsies. Transl. Oncol. 2019, 12, 561–575. [Google Scholar] [CrossRef]
- Coppola, C.J.; Ramaker, R.C.; Mendenhall, E.M. Identification and function of enhancers in the human genome. Hum. Mol. Genet. 2016, 25, R190–R197. [Google Scholar] [CrossRef]
- Sato, T.; Furukawa, K. Sequential action of Ets-1 and Sp1 in the activation of the human beta-1,4-galactosyltransferase V gene involved in abnormal glycosylation characteristic of cancer cells. J. Biol. Chem. 2007, 282, 27702–27712. [Google Scholar] [CrossRef]
- Clem, A.L.; Hamid, T.; Kakar, S.S. Characterization of the role of Sp1 and NF-Y in differential regulation of PTTG/securin expression in tumor cells. Gene 2003, 322, 113–121. [Google Scholar] [CrossRef]
- Chen, X.L.; Cai, Y.H.; Liu, Q.; Pan, L.L.; Shi, S.L.; Liu, X.L.; Chen, Y.; Li, J.G.; Wang, J.; Li, Y.; et al. ETS1 and SP1 drive DHX15 expression in acute lymphoblastic leukaemia. J. Cell. Mol. Med. 2018, 22, 2612–2621. [Google Scholar] [CrossRef]
- Rosmarin, A.G.; Luo, M.; Caprio, D.G.; Shang, J.; Simkevich, C.P. Sp1 cooperates with the ets transcription factor, GABP, to activate the CD18 (beta2 leukocyte integrin) promoter. J. Biol. Chem. 1998, 273, 13097–13103. [Google Scholar] [CrossRef]
- Singh, D.P.; Bhargavan, B.; Chhunchha, B.; Kubo, E.; Kumar, A.; Fatma, N. Transcriptional protein Sp1 regulates LEDGF transcription by directly interacting with its cis-elements in GC-rich region of TATA-less gene promoter. PLoS ONE 2012, 7, e37012. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.Y.; Jackson, N. Human CD1D gene has TATA boxless dual promoters: An SP1-binding element determines the function of the proximal promoter. J. Immunol. 2004, 172, 5512–5521. [Google Scholar] [CrossRef] [PubMed]
- Azizkhan, J.C.; Jensen, D.E.; Pierce, A.J.; Wade, M. Transcription from TATA-less promoters: Dihydrofolate reductase as a model. Crit. Rev. Eukaryot. Gene Expr. 1993, 3, 229–254. [Google Scholar] [PubMed]
- Xu, R.; Zhang, P.; Huang, J.; Ge, S.; Lu, J.; Qian, G. Sp1 and Sp3 regulate basal transcription of the survivin gene. Biochem. Biophys. Res. Commun. 2007, 356, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yang, Y.; Jiang, B.; Zhang, X.; Zou, Y.; Gong, Y. Sp1 and KLF15 regulate basal transcription of the human LRP5 gene. BMC Genet. 2010, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Gui, J.; Song, Y.; Han, N.L.; Zhou, S.F.; Sheu, F.S. Involvement of the GC-rich sequence and specific proteins (Sp1/Sp3) in the basal transcription activity of neurogranin gene. Biochem. Biophys. Res. Commun. 2006, 345, 124–132. [Google Scholar] [CrossRef]
- Xia, X.; Yan, C.; Wu, W.; Zhou, Y.; Hou, L.; Zuo, B.; Xu, D.; Ren, Z.; Xiong, Y. Characterization of the porcine peptidylarginine deiminase type VI gene (PADI6) promoter: Sp1 regulates basal transcription of the porcine PADI6. Gene 2016, 575, 551–558. [Google Scholar] [CrossRef]
- Hsu, C.F.; Sui, C.L.; Wu, W.C.; Wang, J.J.; Yang, D.H.; Chen, Y.C.; Yu, W.C.; Chang, H.S. Klf10 induces cell apoptosis through modulation of BI-1 expression and Ca2+ homeostasis in estrogen-responding adenocarcinoma cells. Int. J. Biochem. Cell Biol. 2011, 43, 666–673. [Google Scholar] [CrossRef]
- Memon, A.; Lee, W.K. KLF10 as a Tumor Suppressor Gene and Its TGF-beta Signaling. Cancers 2018, 10, 161. [Google Scholar] [CrossRef]
- Lomberk, G.; Urrutia, R. The family feud: Turning off Sp1 by Sp1-like KLF proteins. Biochem. J. 2005, 392, 1–11. [Google Scholar] [CrossRef]
- Choi, E.S.; Nam, J.S.; Jung, J.Y.; Cho, N.P.; Cho, S.D. Modulation of specificity protein 1 by mithramycin A as a novel therapeutic strategy for cervical cancer. Sci. Rep. 2014, 4, 7162. [Google Scholar] [CrossRef] [PubMed]
- Malek, A.; Nunez, L.E.; Magistri, M.; Brambilla, L.; Jovic, S.; Carbone, G.M.; Moris, F.; Catapano, C.V. Modulation of the activity of Sp transcription factors by mithramycin analogues as a new strategy for treatment of metastatic prostate cancer. PLoS ONE 2012, 7, e35130. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Guan, X.; Zhang, J.; Jia, Z.; Wei, D.; Li, Q.; Yao, J.; Xie, K. Targeted inhibition of Sp1-mediated transcription for antiangiogenic therapy of metastatic human gastric cancer in orthotopic nude mouse models. Int. J. Oncol. 2008, 33, 161–167. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McGrath, E.P.; Logue, S.E.; Mnich, K.; Deegan, S.; Jager, R.; Gorman, A.M.; Samali, A. The Unfolded Protein Response in Breast Cancer. Cancers 2018, 10, 344. [Google Scholar] [CrossRef] [PubMed]
- Avril, T.; Vauleon, E.; Chevet, E. Endoplasmic reticulum stress signaling and chemotherapy resistance in solid cancers. Oncogenesis 2017, 6, e373. [Google Scholar] [CrossRef] [PubMed]
- Tanimukai, H.; Kanayama, D.; Omi, T.; Takeda, M.; Kudo, T. Paclitaxel induces neurotoxicity through endoplasmic reticulum stress. Biochem. Biophys. Res. Commun. 2013, 437, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Maddalena, F.; Sisinni, L.; Lettini, G.; Condelli, V.; Matassa, D.S.; Piscazzi, A.; Amoroso, M.R.; La Torre, G.; Esposito, F.; Landriscina, M. Resistance to paclitxel in breast carcinoma cells requires a quality control of mitochondrial antiapoptotic proteins by TRAP1. Mol. Oncol. 2013, 7, 895–906. [Google Scholar] [CrossRef]
- Emadi, A.; Jones, R.J.; Brodsky, R.A. Cyclophosphamide and cancer: Golden anniversary. Nat. Rev. Clin. Oncol. 2009, 6, 638–647. [Google Scholar] [CrossRef]
- Caino, M.C.; von Burstin, V.A.; Lopez-Haber, C.; Kazanietz, M.G. Differential regulation of gene expression by protein kinase C isozymes as determined by genome-wide expression analysis. J. Biol. Chem. 2011, 286, 11254–11264. [Google Scholar] [CrossRef]
- Cooke, M.; Magimaidas, A.; Casado-Medrano, V.; Kazanietz, M.G. Protein kinase C in cancer: The top five unanswered questions. Mol. Carcinog. 2017, 56, 1531–1542. [Google Scholar] [CrossRef]
- Smirnova, I.S.; Chang, S.; Forsthuber, T.G. Prosurvival and proapoptotic functions of ERK1/2 activation in murine thymocytes in vitro. Cell. Immunol. 2010, 261, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Moulding, D.A.; Giles, R.V.; Spiller, D.G.; White, M.R.; Tidd, D.M.; Edwards, S.W. Apoptosis is rapidly triggered by antisense depletion of MCL-1 in differentiating U937 cells. Blood 2000, 96, 1756–1763. [Google Scholar] [PubMed]
- Zeng, C.; Wang, W.; Yu, X.; Yang, L.; Chen, S.; Li, Y. Pathways related to PMA-differentiated THP1 human monocytic leukemia cells revealed by RNA-Seq. Sci. China Life Sci. 2015, 58, 1282–1287. [Google Scholar] [CrossRef] [PubMed]
- Angel, P.; Imagawa, M.; Chiu, R.; Stein, B.; Imbra, R.J.; Rahmsdorf, H.J.; Jonat, C.; Herrlich, P.; Karin, M. Phorbol ester-inducible genes contain a common cis element recognized by a TPA-modulated trans-acting factor. Cell 1987, 49, 729–739. [Google Scholar] [CrossRef]
- Edbrooke, M.R.; Burt, D.W.; Cheshire, J.K.; Woo, P. Identification of cis-acting sequences responsible for phorbol ester induction of human serum amyloid A gene expression via a nuclear factor kappaB-like transcription factor. Mol. Cell. Biol. 1989, 9, 1908–1916. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Yoon, S.H.; Choe, E.Y.; Cho, S.H.; Woo, C.H.; Rho, J.Y.; Kim, J.H. PMA-induced up-regulation of MMP-9 is regulated by a PKCalpha-NF-kappaB cascade in human lung epithelial cells. Exp. Mol. Med. 2007, 39, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Mitkiewicz, M.; Bac, B.; Kuropatwa, M.; Kurowska, E.; Matuszyk, J.; Siednienko, J. Sp1 mediates phorbol ester (PMA)-induced expression of membrane-bound guanylyl cyclase GC-A in human monocytic THP-1 cells. Acta Biochim. Pol. 2018, 65, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.Y.; Wu, R.; Chen, Y.; Tarasova, N.; Chang, M.M. PMA stimulates MUC5B gene expression through an Sp1-based mechanism in airway epithelial cells. Am. J. Respir. Cell Mol. Biol. 2007, 37, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.; Cockrell, C.A.; Ferro, T.J. Expression of alpha-ENaC2 is dependent on an upstream Sp1 binding motif and is modulated by protein phosphatase 1 in lung epithelial cells. Biochem. Biophys. Res. Commun. 2003, 303, 1159–1168. [Google Scholar] [CrossRef]
- Reyland, M.E.; Jones, D.N. Multifunctional roles of PKCdelta: Opportunities for targeted therapy in human disease. Pharmacol. Ther. 2016, 165, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Garg, R.; Caino, M.C.; Kazanietz, M.G. Regulation of Transcriptional Networks by PKC Isozymes: Identification of c-Rel as a Key Transcription Factor for PKC-Regulated Genes. PLoS ONE 2013, 8, e67319. [Google Scholar] [CrossRef] [PubMed]
- McKiernan, E.; O’Brien, K.; Grebenchtchikov, N.; Geurts-Moespot, A.; Sieuwerts, A.M.; Martens, J.W.; Magdolen, V.; Evoy, D.; McDermott, E.; Crown, J.; et al. Protein kinase Cdelta expression in breast cancer as measured by real-time PCR, western blotting and ELISA. Br. J. Cancer 2008, 99, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Fukase, N.; Kawamoto, T.; Kishimoto, K.; Hara, H.; Okada, Y.; Onishi, Y.; Toda, M.; Kurosaka, M.; Akisue, T. Protein kinase Cdelta in tumorigenesis of human malignant fibrous histiocytoma. Oncol. Rep. 2011, 26, 1221–1226. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, Z.; Forman, L.W.; Williams, R.M.; Faller, D.V. Protein kinase C-delta inactivation inhibits the proliferation and survival of cancer stem cells in culture and in vivo. BMC Cancer 2014, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Lonne, G.K.; Masoumi, K.C.; Lennartsson, J.; Larsson, C. Protein kinase Cdelta supports survival of MDA-MB-231 breast cancer cells by suppressing the ERK1/2 pathway. J. Biol. Chem. 2009, 284, 33456–33465. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.S.; West, K.A.; Blumberg, P.M.; Dennis, P.A. Altered protein kinase C (PKC) isoforms in non-small cell lung cancer cells: PKCdelta promotes cellular survival and chemotherapeutic resistance. Cancer Res. 2003, 63, 780–786. [Google Scholar] [PubMed]
- Garg, R.; Blando, J.M.; Perez, C.J.; Abba, M.C.; Benavides, F.; Kazanietz, M.G. Protein Kinase C Epsilon Cooperates with PTEN Loss for Prostate Tumorigenesis through the CXCL13-CXCR5 Pathway. Cell Rep. 2017, 19, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Jain, K.; Basu, A. The Multifunctional Protein Kinase C-epsilon in Cancer Development and Progression. Cancers 2014, 6, 860–878. [Google Scholar] [CrossRef]
- Hong, D.H.; Petrovics, G.; Anderson, W.B.; Forstner, J.; Forstner, G. Induction of mucin gene expression in human colonic cell lines by PMA is dependent on PKC-epsilon. Am. J. Physiol. 1999, 277, G1041–G1047. [Google Scholar] [CrossRef]
- Awadelkarim, K.D.; Callens, C.; Rosse, C.; Susini, A.; Vacher, S.; Rouleau, E.; Lidereau, R.; Bieche, I. Quantification of PKC family genes in sporadic breast cancer by qRT-PCR: Evidence that PKCiota/lambda overexpression is an independent prognostic factor. Int. J. Cancer 2012, 131, 2852–2862. [Google Scholar] [CrossRef]
- Kojima, Y.; Akimoto, K.; Nagashima, Y.; Ishiguro, H.; Shirai, S.; Chishima, T.; Ichikawa, Y.; Ishikawa, T.; Sasaki, T.; Kubota, Y.; et al. The overexpression and altered localization of the atypical protein kinase C lambda/iota in breast cancer correlates with the pathologic type of these tumors. Hum. Pathol. 2008, 39, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Tan, N.Y.; Khachigian, L.M. Sp1 phosphorylation and its regulation of gene transcription. Mol. Cell. Biol. 2009, 29, 2483–2488. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.K.; Choi, Y.H.; Kim, C.H.; Choi, W.S. p38MAPK mediates benzyl isothiocyanate-induced p21WAF1 expression in vascular smooth muscle cells via the regulation of Sp1. Biochem. Biophys. Res. Commun. 2006, 350, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.T.; Yang, W.B.; Chang, W.C.; Hung, J.J. Interplay of posttranslational modifications in Sp1 mediates Sp1 stability during cell cycle progression. J. Mol. Biol. 2011, 414, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, G.; Harrington, A.; Hungerford, J.; Martinez-Hernandez, A.; Gerling, I.C.; Raghow, R.; Solomon, S. Insulin dynamically regulates calmodulin gene expression by sequential o-glycosylation and phosphorylation of sp1 and its subcellular compartmentalization in liver cells. J. Biol. Chem. 2006, 281, 3642–3650. [Google Scholar] [CrossRef] [PubMed]
- Rafty, L.A.; Khachigian, L.M. Sp1 phosphorylation regulates inducible expression of platelet-derived growth factor B-chain gene via atypical protein kinase C-zeta. Nucleic Acids Res. 2001, 29, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Pal, S.; Claffey, K.P.; Cohen, H.T.; Mukhopadhyay, D. Activation of Sp1-mediated vascular permeability factor/vascular endothelial growth factor transcription requires specific interaction with protein kinase C zeta. J. Biol. Chem. 1998, 273, 26277–26280. [Google Scholar] [CrossRef]
- Galvez, A.S.; Brunskill, E.W.; Marreez, Y.; Benner, B.J.; Regula, K.M.; Kirschenbaum, L.A.; Dorn, G.W., 2nd. Distinct pathways regulate proapoptotic Nix and BNip3 in cardiac stress. J. Biol. Chem. 2006, 281, 1442–1448. [Google Scholar] [CrossRef]
- Cadoret, A.; Baron-Delage, S.; Bertrand, F.; Kornprost, M.; Groyer, A.; Gespach, C.; Capeau, J.; Cherqui, G. Oncogene-induced up-regulation of Caco-2 cell proliferation involves IGF-II gene activation through a protein kinase C-mediated pathway. Oncogene 1998, 17, 877–887. [Google Scholar] [CrossRef][Green Version]
- Qian, Y.; Yao, W.; Yang, T.; Yang, Y.; Liu, Y.; Shen, Q.; Zhang, J.; Qi, W.; Wang, J. aPKC-iota/P-Sp1/Snail signaling induces epithelial-mesenchymal transition and immunosuppression in cholangiocarcinoma. Hepatology 2017, 66, 1165–1182. [Google Scholar] [CrossRef]
- Carrara, G.; Saraiva, N.; Parsons, M.; Byrne, B.; Prole, D.L.; Taylor, C.W.; Smith, G.L. Golgi anti-apoptotic proteins are highly conserved ion channels that affect apoptosis and cell migration. J. Biol. Chem. 2015, 290, 11785–11801. [Google Scholar] [CrossRef] [PubMed]
- Saraiva, N.; Prole, D.L.; Carrara, G.; Johnson, B.F.; Taylor, C.W.; Parsons, M.; Smith, G.L. hGAAP promotes cell adhesion and migration via the stimulation of store-operated Ca2+ entry and calpain 2. J. Cell Biol. 2013, 202, 699–713. [Google Scholar] [CrossRef] [PubMed]
- Carrara, G.; Parsons, M.; Saraiva, N.; Smith, G.L. Golgi anti-apoptotic protein: A tale of camels, calcium, channels and cancer. Open Biol. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Reimers, K.; Choi, C.Y.; Bucan, V.; Vogt, P.M. The growth-hormone inducible transmembrane protein (Ghitm) belongs to the Bax inhibitory protein-like family. Int. J. Biol. Sci. 2007, 3, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.H.; Li, Q.; Hu, H.; Ni, B.; Liu, X.; Huang, C.; Zhang, Z.Z.; Zhao, G. Transmembrane protein GRINA modulates aerobic glycolysis and promotes tumor progression in gastric cancer. J. Exp. Clin. Cancer Res. 2018, 37, 308. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Yerges-Armstrong, L.M.; Chu, Y.; Zmuda, J.M.; Zhang, Y. Transcriptional Regulation of Frizzled-1 in Human Osteoblasts by Sp1. PLoS ONE 2016, 11, e0163277. [Google Scholar] [CrossRef]
- Park, S.J.; Lee, K.S.; Kim, S.R.; Min, K.H.; Moon, H.; Lee, M.H.; Chung, C.R.; Han, H.J.; Puri, K.D.; Lee, Y.C. Phosphoinositide 3-kinase delta inhibitor suppresses interleukin-17 expression in a murine asthma model. Eur. Respir. J. 2010, 36, 1448–1459. [Google Scholar] [CrossRef]
- Ciriello, G.; Gatza, M.L.; Beck, A.H.; Wilkerson, M.D.; Rhie, S.K.; Pastore, A.; Zhang, H.; McLellan, M.; Yau, C.; Kandoth, C.; et al. Comprehensive Molecular Portraits of Invasive Lobular Breast Cancer. Cell 2015, 163, 506–519. [Google Scholar] [CrossRef]
- Anaya, J. OncoLnc: Linking TCGA survival data to mRNAs, miRNAs, and lncRNAs. PeerJ Comput. Sci. 2016, 2, e67. [Google Scholar] [CrossRef]
| Construct | Forward (5′→3′) | Reverse (5′→3′) |
| pGL3-TMBIM6-P1 | atctggtaccgggactctaaaaag (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P2 | atcggtaccaaaatgaatgtggatactggtct (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P3 | atcggtacctcatattgtcttatgcccaatttc (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P4 | atcggtacctcctgctacactacagcaaaaa (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P5 | atcggtaccgcctactgagaatcataccctg (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P6 | atcggtaccttttaatgtgttctctgaatcg (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| pGL3-TMBIM6-P2ΔP3 | atcggtaccaaaatgaatgtggatactggtct (KpnI) | atcaagcttggggtggtctcctcccttatt (HindIII) |
| pGL3-TMBIM6-P2ΔP6 | atcggtaccaaaatgaatgtggatactggtct (KpnI) | atcagatctaaaaaaaaaaagcgccctcgcaag (BglII) |
| pGL3-TMBIM6-P7 | atcggtaccttttaatgtgttctctgaatcg (KpnI) | atcagatctctctagtggagaaagtgaaaatg (BglII) |
| pGL3-TMBIM6-P8 | atcggtaccgcagcagcgcaccgtgac (KpnI) | atcagatctataaacagcggctgcttag (BglII) |
| pGL3-TMBIM6-P9 | atcggtaccgcacgtacagccaatgg (KpnI) | atcagatcttaccagcgcttctaacacc (BglII) |
| qRT-PCR | ||
| hTMBIM6-v1 | gagcacatccggtgttagaa | gtgttgccatcagccaaatc |
| GAPDH | ctcagacaccatggggaaggtg | ctcagccttgacggtgccatg |
| Primers Used for Site-Directed Mutations | |
| Name | Sequence 5′→3′ |
| mSp1-d-S | aagcggaccacaggTATgggtttccctcgagaggc |
| mSp1-d-AS | gcctctcgagggaaacccATAcctgtggtccgctt |
| mSp1-p-S | tcgggagcggaagtggTTAagtcagagcacatcc |
| mSp1-p-AS | ggatgtgctctgactTAAccacttccgctcccga |
| mNFY-p-S | gtgcggccaacggcTTTtgaggactggtcttaag |
| mNFY-p-AS | cttaagaccagtcctcaAAAgccgttggccgcac |
| mNFkB-S | accacagggcggggtCATcctcgagaggcgaacg |
| mNFkB-AS | cgttcgcctctcgaggATGaccccgccctgtggt |
| mElk-1-S | cgagtcagagcacatAAgTtgttagaagcgctggt |
| mElk-1-AS | accagcgcttctaacaAcTTatgtgctctgactcg |
| mETS1-S | gtaaaagatcgggagcTAaagtgggcgagtcagag |
| mETS1-AS | ctctgactcgcccacttTAgctcccgatcttttac |
| Probes Used in EMSA | |
| Name | Sequence 5′ to 3′ |
| Sp1-1-S | gcggaccacagggcggggtttccctcgagaggc |
| Sp1-1-AS | gcctctcgagggaaaccccgccctgtggtccgc |
| Sp1-2-S | cgggagcggaagtgggcgagtcagagcacatccg |
| Sp1-2-AS | cggatgtgctctgactcgcccacttccgctcccg |
| Note: Mutant primers mentioned above are used as probes for respective sites | |
| ChIP Assay Primers | |
| G-TMBIM6 S | cgacaagctcaggcctctgaac |
| G-TMBIM6 AS | taccagcgcttctaacaccgga |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Junjappa, R.P.; Kim, H.-K.; Park, S.Y.; Bhattarai, K.R.; Kim, K.-W.; Soh, J.-W.; Kim, H.-R.; Chae, H.-J. Expression of TMBIM6 in Cancers: The Involvement of Sp1 and PKC. Cancers 2019, 11, 974. https://doi.org/10.3390/cancers11070974
Junjappa RP, Kim H-K, Park SY, Bhattarai KR, Kim K-W, Soh J-W, Kim H-R, Chae H-J. Expression of TMBIM6 in Cancers: The Involvement of Sp1 and PKC. Cancers. 2019; 11(7):974. https://doi.org/10.3390/cancers11070974
Chicago/Turabian StyleJunjappa, Raghu Patil, Hyun-Kyoung Kim, Seong Yeol Park, Kashi Raj Bhattarai, Kyung-Woon Kim, Jae-Won Soh, Hyung-Ryong Kim, and Han-Jung Chae. 2019. "Expression of TMBIM6 in Cancers: The Involvement of Sp1 and PKC" Cancers 11, no. 7: 974. https://doi.org/10.3390/cancers11070974
APA StyleJunjappa, R. P., Kim, H.-K., Park, S. Y., Bhattarai, K. R., Kim, K.-W., Soh, J.-W., Kim, H.-R., & Chae, H.-J. (2019). Expression of TMBIM6 in Cancers: The Involvement of Sp1 and PKC. Cancers, 11(7), 974. https://doi.org/10.3390/cancers11070974







