Swallowing Safety and Efficiency after Open Partial Horizontal Laryngectomy: A Videofluoroscopic Study
Abstract
1. Introduction
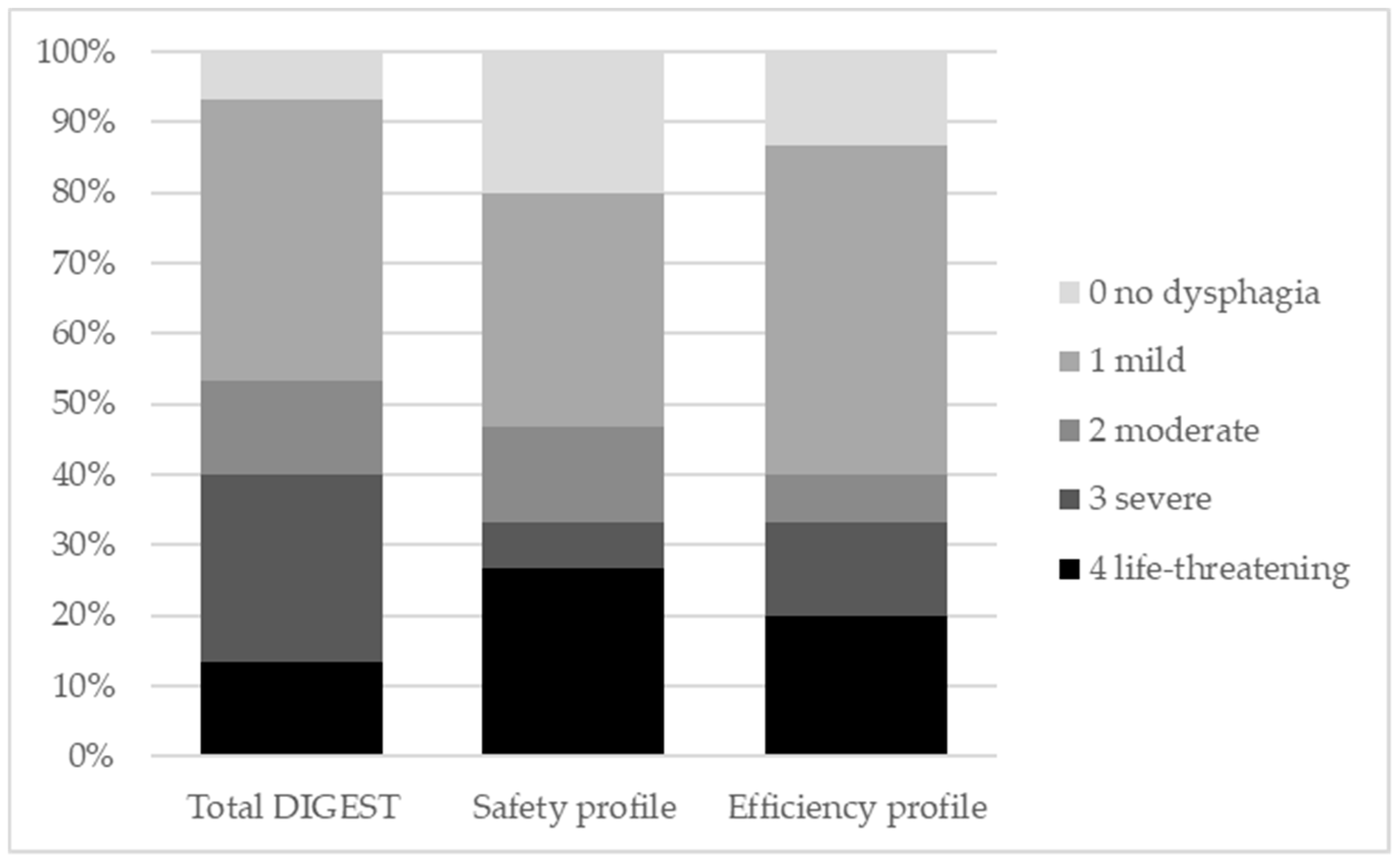
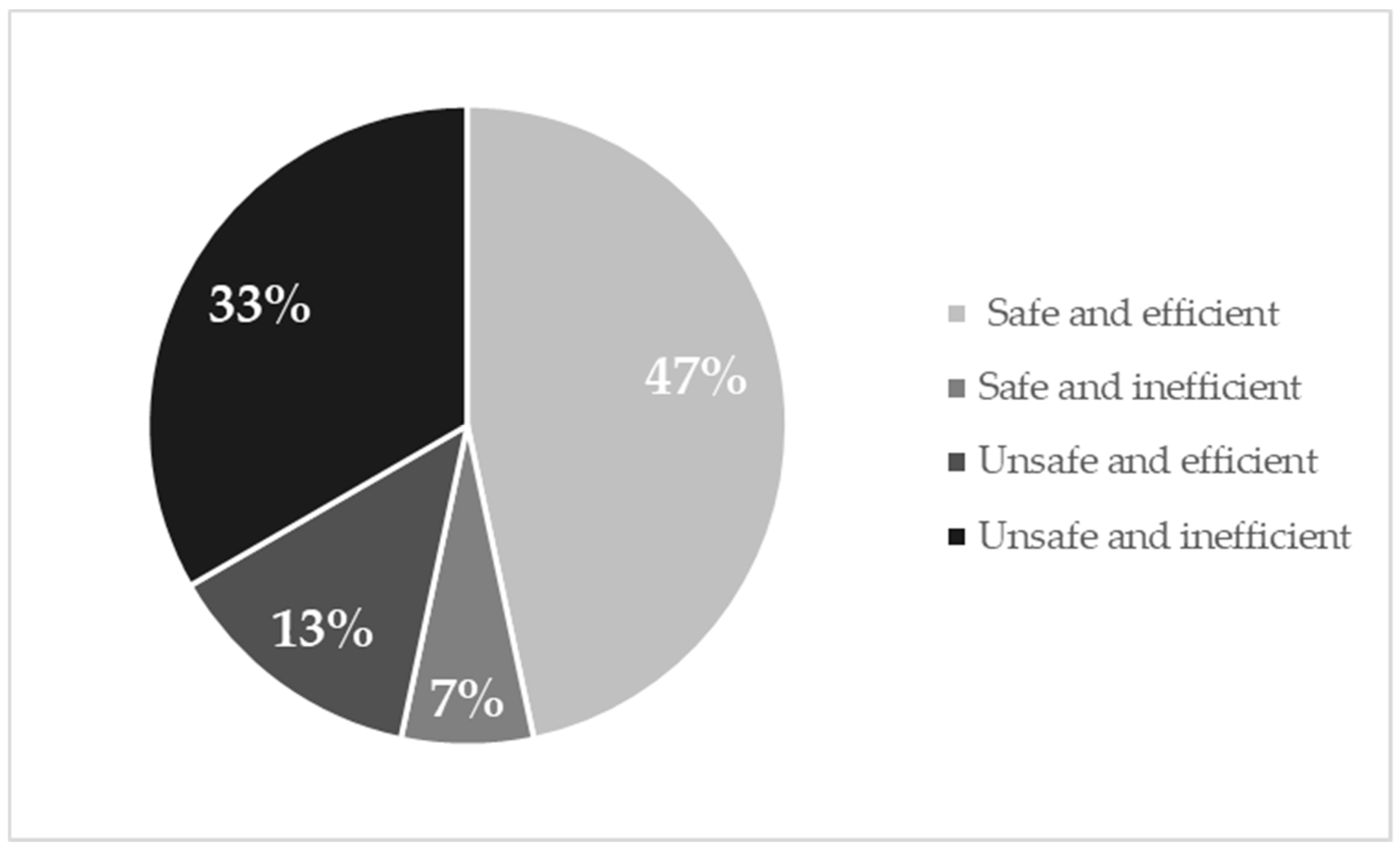
2. Results
2.1. Swallowing Safety: Comparison of Videofluoroscopic Variables
2.2. Swallowing Efficiency: Comparison of Videofluoroscopic Variables
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Videofluoroscopic Study of Swallowing
4.3. Dynamic Imaging Grade of Swallowing Toxicity (DIGEST)
4.4. Videofluoroscopic Measures
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Succo, G.; Peretti, G.; Piazza, C.; Remacle, M.; Eckel, H.E.; Chevalier, D.; Simo, R.; Hantzakos, A.G.; Rizzotto, G.; Lucioni, M.; et al. Open partial horizontal laryngectomies: A proposal for classification by the working committee on nomenclature of the European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2014, 271, 2489–2496. [Google Scholar]
- Ertekin, C.; Aydogdu, I. Neurophysiology of swallowing. Clin. Neurophysiol. 2003, 114, 2226–2244. [Google Scholar] [PubMed]
- Rofes, L.; Arreola, V.; Almirall, J.; Cabré, M.; Campins, L.; García-Peris, P.; Speyer, R.; Clavé, P. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol. Res. Pract. 2011, 2011, 818979. [Google Scholar] [PubMed]
- Ekberg, O.; Hamdy, S.; Woisard, V.; Wuttge-Hannig, A.; Ortega, P. Social and psychological burden of dysphagia: Its impact on diagnosis and treatment. Dysphagia 2002, 17, 139–146. [Google Scholar] [PubMed]
- Lips, M.; Speyer, R.; Zumach, A.; Kross, K.W.; Kremer, B. Supracricoid laryngectomy and dysphagia: A systematic literature review. Laryngoscope 2015, 125, 2143–2156. [Google Scholar]
- Schindler, A.; Pizzorni, N.; Mozzanica, F.; Fantini, M.; Ginocchio, D.; Bertolin, A.; Crosetti, E.; Succo, G. Functional outcomes after supracricoid laryngectomy: What do we not know and what do we need to know? Eur. Arch. Otorhinolaryngol. 2016, 273, 3459–3475. [Google Scholar]
- Gallo, O.; Deganello, A.; Gitti, G.; Santoro, R.; Senesi, M.; Scala, J.; Boddi, V.; De Campora, E. Prognostic role of pneumonia in supracricoid and supraglottic laryngectomies. Oral Oncol. 2009, 45, 30–38. [Google Scholar]
- Woisard, V.; Puech, M.; Yardeni, E.; Serrano, E.; Pessey, J.J. Deglutition after supracricoid laryngectomy: Compensatory mechanisms and sequelae. Dysphagia 1996, 11, 265–269. [Google Scholar]
- Yücetürk, A.V.; Tarhan, S.; Günhan, K.; Yüksel, P. Videofluoroscopic evaluation of the swallowing function after supracricoid laryngectomy. Eur. Arch. Otorhinolaryngol. 2005, 262, 198–203. [Google Scholar]
- Lewin, J.S.; Hutcheson, K.A.; Barringer, D.A.; May, A.H.; Roberts, D.B.; Holsinger, F.C.; Diaz, E.M. Functional analysis of swallowing outcomes after supracricoid partial laryngectomy. Head Neck 2008, 30, 559–566. [Google Scholar]
- Hutcheson, K.A.; Barrow, M.P.; Barringer, D.A.; Knott, J.K.; Lin, H.Y.; Weber, R.S.; Fuller, C.D.; Lai, S.Y.; Alvarez, C.; Raut, J.; et al. Dynamic Imaging Grade of Swallowing Toxiciy (DIGEST): Scale development and validation. Cancer 2017, 123, 62–70. [Google Scholar]
- Laccourreye, O.; Brasnu, D.; Périé, S.; Muscatello, L.; Ménard, M.; Weinstein, G. Supracricoid partial laryngectomies in the elderly: Mortality, complications, and functional outcome. Laryngoscope 1998, 108, 237–242. [Google Scholar]
- Schindler, A.; Favero, E.; Capaccio, P.; Albera, R.; Cavalot, A.L.; Ottaviani, F. Supracricoid laryngectomy: Age influence on long-term functional results. Laryngoscope 2009, 119, 1218–1225. [Google Scholar]
- Benito, J.; Holsinger, F.C.; Pérez-Martín, A.; Garcia, D.; Weinstein, G.S.; Laccoureye, O. Aspiration after supracricoid partial laryngectomy: Incidence, risk factors, management, and outcomes. Head Neck 2011, 33, 679–685. [Google Scholar]
- Naudo, P.; Laccourreye, O.; Weinstein, G.; Jouffre, V.; Laccourreye, H.; Brasnu, D. Complications and functional outcome after supracricoid partial laryngectomy with cricohyoidoepiglottopexy. Otolaryngol. Head Neck Surg. 1998, 118, 124–129. [Google Scholar]
- Ekberg, O. Closure of the laryngeal vestibule during deglutition. Acta Otolaryngol. 1982, 93, 123–129. [Google Scholar]
- Logemann, J.A.; Kahrilas, P.J.; Cheng, J.; Pauloski, B.R.; Gibbons, P.J.; Rademaker, A.W.; Lin, S. Closure mechanisms of laryngeal vestibule during swallow. Am. J. Physiol. 1992, 262, G338–G344. [Google Scholar]
- Pearson, W.G., Jr.; Taylor, B.K.; Blair, J.; Martin-Harris, B. Computational analysis of swallowing mechanics underlying impaired epiglottic inversion. Laryngoscope 2016, 126, 1854–1858. [Google Scholar]
- Alicandri-Ciufelli, M.; Piccinini, A.; Bergamini, G.; Ruberto, M.; Ghidini, A.; Marchioni, D.; Presutti, L. Atypical neoglottis after supracricoid laryngectomy: A morphological and functional analysis. Eur. Arch. Otorhinolaryngol. 2011, 268, 1029–1234. [Google Scholar]
- Logemann, J.A.; Gibbons, P.; Rademaker, A.W.; Pauloski, B.R.; Kahrilas, P.J.; Bacon, M.; Bowman, J.; McCracken, E. Mechanisms of recovery of swallow after supraglottic laryngectomy. J. Speech Hear. Res. 1994, 37, 965–974. [Google Scholar]
- Ohmae, Y.; Logemann, J.A.; Kaiser, P.; Hanson, D.G.; Kahrilas, P.J. Effects of two breath-holding maneuvers on oropharyngeal swallow. Ann. Otol. Rhinol. Laryngol. 1996, 105, 123–131. [Google Scholar]
- Logemann, J.A.; Pauloski, B.R.; Rademaker, A.W.; Colangelo, L.A. Super-supraglottic swallow in irradiated head and neck cancer patients. Head Neck 1997, 19, 535–540. [Google Scholar] [PubMed]
- Ricci Maccarini, A.; Stacchini, M.; Salsi, D.; Padovani, D.; Pieri, F.; Casolino, D. Surgical rehabilitation of dysphagia after partial laryngectomy. Acta Otorhionalygol. Ital. 2007, 27, 294–298. [Google Scholar]
- Shaw, S.M.; Martino, R. The Normal Swallow Muscular and Neurophysiological Control. Otolaryngol. Clin. N. Am. 2013, 46, 937–956. [Google Scholar]
- Belafsky, P.C.; Kuhn, M.A. The Clinician’s Guide to Swallowing Fluoroscopy; Springer: New York, NY, USA, 2014; pp. 51–68. [Google Scholar]
- McConnel, F.M. Analysis of pressure generation and bolus transit during pharyngeal swallowing. Laryngoscope 1988, 98, 71–78. [Google Scholar] [PubMed]
- Omari, T.; Schar, M. High-resolution manometry: What about the pharynx? Curr. Opin. Otolaryngol. Head Neck Surg. 2018, 26, 382–391. [Google Scholar] [PubMed]
- Rademaker, A.W.; Pauloski, B.R.; Logemann, J.A.; Shanahan, T.K. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J. Speech Hear. Res. 1994, 37, 314–325. [Google Scholar]
- Pauloski, B.R.; Logemann, J.A. Impact of tongue base and posterior pharyngeal wall biomechanics on pharyngeal clearance in irradiated postsurgical oral and oropharyngeal cancer patients. Head Neck 2000, 22, 120–131. [Google Scholar]
- Knigge, M.A.; Thibeault, S. Relationship between tongue base region pressures and vallecular clearance. Dysphagia 2016, 31, 391–397. [Google Scholar]
- Pouderoux, P.; Kahrilas, P.J. Deglutitive tongue force modulation by volition, volume and viscosity in humans. Gastroenterology 1995, 108, 1418–1426. [Google Scholar]
- Shaker, R.; Kern, M.; Bardan, E.; Taylor, A.; Stewart, E.T.; Hoffman, R.G.; Arndorfer, R.C.; Hofmann, C.; Bonnevier, J. Augmentation of deglutitive upper esophageal sphincter opening in the elderly by exercise. Am. J. Physiol. 1997, 272, G1518–G1522. [Google Scholar] [PubMed]
- McCullough, G.H.; Kim, Y. Effects of the Mendelsohn Maneuver on extent of hyoid movement and UES opening post-stroke. Dysphagia 2013, 28, 511–519. [Google Scholar] [PubMed]
- Lazarus, C.; Logemann, J.A.; Song, C.W.; Rademaker, A.W.; Kahrillas, P.J. Effects of voluntary maneuvers on tongue base function for swallowing. Folia. Phonaitr. Logop. 2002, 54, 171–176. [Google Scholar]
- Fuju, M.; Logemann, J.A. Effect of a tongue-holding maneuver on posterior pharyngeal wall movement during deglutition. Am. J. Speech Lang. Pathol. 1996, 5, 23–30. [Google Scholar]
- Martin-Harris, B.; McFarland, D.; Hill, E.G.; Strange, C.B.; Focht, K.L.; Wan, Z.; Blair, J.; McGrattan, K. Respiratory-swallow training in patients with head and neck cancer. Arch. Phys. Med. Rehabil. 2015, 96, 885–893. [Google Scholar]
- Kraaijenga, S.A.C.; Lapid, O.; van der Molen, L.; Hilgers, F.J.M.; Smeele, L.E.; van den Brekel, M.W.M. Feasibility and potential value of lipofilling in post-treatment oropharyngeal dysfunction. Laryngoscope 2016, 126, 2672–2678. [Google Scholar] [PubMed]
- Ottaviani, F.; Schindler, A.; Klinger, F.; Scarponi, L.; Succo, G.; Mozzanica, F. Functional fat injection under local anesthesia to treat severe postsurgical dysphagia, case report. Head Neck 2019, 41, E16–E20. [Google Scholar]
- Molfenter, S.M.; Steele, C.M. Temporal variability in the deglutition literature. Dysphagia 2012, 27, 162–177. [Google Scholar] [PubMed]
- Rizzotto, G.; Succo, G.; Lucioni, M.; Pazzaia, T. Subtotal laryngectomy with tracheohyoidopexy: A possible alternative to total laryngectomy. Laryngoscope 2006, 116, 1907–1917. [Google Scholar] [PubMed]
- Brady, S.; Donizelli, J. The modified barium swallow and the functional endoscopic evaluation of swallowing. Otolaryngol. Clin. No. Am. 2013, 46, 1009–1022. [Google Scholar]
- Italian Association of Medical Oncology (AIOM). [Linee Guida. Tumori Della Testa e del Tronco]. 2018. Available online: www.aiom.it (accessed on 22 March 2018).
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [PubMed]
- Martin-Harris, B.; Brodsky, M.B.; Michel, Y.; Castell, D.O.; Schleicher, M.; Sandidge, J.; Maxwell, R.; Blair, J. MBS Measurement Tool for Swallow Impairment-MBSImp: Establishing a standard. Dysphagia 2008, 23, 392–405. [Google Scholar]
- Tabor, L.C.; Plowman, E.K.; Romero-Clark, C.; Youssof, S. Oropharyngeal dysphagia profiles in individuals with oculopharyngeal muscular dystrophy. Neurogastroenterol. Motil. 2018, 30, e13251. [Google Scholar] [PubMed]
- Brodsky, M.B.; McFarland, D.H.; Dozier, T.S.; Blair, J.A.; Ayers, C.; Gillespie, M.B.; Day, T.A.; Martin-Harris, B. Respiratory-swallow phase patterns and their relationship to swallowing impairment in treated oropharyngeal cancer. Head Neck 2010, 32, 481–489. [Google Scholar] [PubMed]
| Measure | Consistency | Safe | Unsafe | p | ||
|---|---|---|---|---|---|---|
| Median | IQ Range | Median | IQ Range | |||
| TPT (s) | solid | 0.36 | 0.10 | 0.32 | 0.40 | 0.867 |
| semisolid | 0.32 | 0.10 | 0.36 | 0.20 | 0.336 | |
| liquid | 0.42 | 0.11 | 0.36 | 0.04 | 0.536 | |
| POD (s) | solid | 0.26 | 0.10 | 0.24 | 0.08 | 0.397 |
| semisolid | 0.24 | 0.07 | 0.28 | 0.04 | 1 | |
| liquid | 0.28 | 0.07 | 0.24 | 0.08 | 0.867 | |
| POL (mm) | solid | 8.5 | 3.5 | 8 | 3 | 0.867 |
| semisolid | 12 | 5.5 | 11 | 5 | 0.152 | |
| liquid | 10 | 3 | 12 | 4 | 0.232 | |
| HMS (mm) | solid | 5 | 10.8 | 2 | 14 | 0.955 |
| semisolid | 1 | 3.5 | 6 | 14 | 0.232 | |
| liquid | 0 | 3.5 | 4 | 6 | 0.397 | |
| HMR (mm) | solid | 29 | 7.5 | 26 | 12 | 0.867 |
| semisolid | 27 | 14.5 | 32 | 1 | 0.694 | |
| liquid | 27 | 11.3 | 22 | 16 | 0.536 | |
| HVS (mm) | solid | 60.5 | 13.5 | 62 | 4 | 0.867 |
| semisolid | 60 | 15.5 | 64 | 1 | 0.613 | |
| liquid | 58 | 15 | 60 | 2 | 0.779 | |
| LC | solid | 1 | 1.75 | 3 | 1 | 0.021 * |
| semisolid | 1 | 0.75 | 3 | 3 | 0.152 | |
| liquid | 2 | 2 | 4 | 1 | 0.021 * | |
| EM | solid | 1 | 1 | 2 | 0 | 0.121 |
| semisolid | 1 | 0.75 | 2 | 1 | 0.152 | |
| liquid | 1 | 0.75 | 2 | 0 | 0.054 | |
| IPS | solid | 0 | 1 | 0 | 1 | 0.955 |
| semisolid | 0 | 0 | 0 | 0 | 1 | |
| liquid | 0.5 | 1 | 0 | 0 | 0.336 | |
| TBR | solid | 1 | 0.75 | 2 | 1 | 0.336 |
| semisolid | 1 | 0.75 | 2 | 1 | 0.152 | |
| liquid | 1.5 | 1 | 2 | 1 | 0.536 | |
| Measure | Consistency | Efficient | Inefficient | p | ||
|---|---|---|---|---|---|---|
| Median | IQ Range | Median | IQ Range | |||
| TPT (s) | solid | 0.36 | 0.08 | 0.36 | 0.37 | 0.328 |
| semisolid | 0.32 | 0.06 | 0.40 | 0.19 | 0.008 * | |
| liquid | 0.40 | 0.14 | 0.36 | 0.06 | 0.776 | |
| POD (s) | solid | 0.24 | 0.12 | 0.24 | 0.1 | 0.776 |
| semisolid | 0.24 | 0.02 | 0.28 | 0.05 | 0.066 | |
| liquid | 0.28 | 0.10 | 0.28 | 0.07 | 1 | |
| POL (mm) | solid | 9 | 4.5 | 8 | 3 | 0.607 |
| semisolid | 12 | 4 | 9.5 | 4 | 0.008 * | |
| liquid | 12 | 3.5 | 10.5 | 3.5 | 0.689 | |
| HMS (mm) | solid | 6 | 10.5 | 2 | 12.5 | 0.689 |
| semisolid | 2 | 5 | 6 | 12.5 | 0.456 | |
| liquid | 0 | 3 | 6 | 1 | 0.088 | |
| HMR (mm) | solid | 28 | 8.5 | 26 | 14.25 | 0.776 |
| semisolid | 28 | 11 | 33 | 13 | 0.328 | |
| liquid | 24 | 15 | 29 | 13.5 | 0.388 | |
| HVS (mm) | solid | 64 | 13 | 60 | 0.75 | 0.328 |
| semisolid | 66 | 16 | 63 | 1.05 | 0.607 | |
| liquid | 60 | 16 | 61 | 0.7 | 0.689 | |
| LC | solid | 2 | 2 | 3 | 3 | 0.456 |
| semisolid | 1 | 0.5 | 3.5 | 3 | 0.066 | |
| liquid | 3 | 3 | 3.5 | 2 | 0.388 | |
| EM | solid | 2 | 1 | 2 | 1 | 0.776 |
| semisolid | 1 | 1 | 2 | 1 | 0.328 | |
| liquid | 1 | 1 | 2 | 1 | 0.529 | |
| IPS | solid | 0 | 0.5 | 0.5 | 1.25 | 0.328 |
| semisolid | 0 | 0 | 0 | 0.25 | 0.864 | |
| liquid | 0 | 1 | 0 | 1.5 | 1 | |
| TBR | solid | 1 | 0 | 2 | 0.25 | 0.018 * |
| semisolid | 1 | 0.5 | 2 | 0.25 | 0.049 * | |
| liquid | 1 | 1 | 2 | 0.25 | 0.224 | |
| Measure | Abbreviation | Unit of Measurement | Definition |
|---|---|---|---|
| Total pharyngeal transit time | TPT | s | Time from when bolus head first passes posterior nasal spine to time when bolus tale exits PES |
| PES opening duration | POD | s | Time from when PES first opens for bolus entry to when it first closes behind the bolus |
| PES opening (lateral) | POL | mm | Distance at the narrowest point of opening between C3 and C6 (upper esophageal sphincter) on lateral fluoroscopic view |
| Hyoidomandibular distance during swallowing | HMS | mm | Distance between the upper margin of the hyoid bone and lower margin of the mandible during swallowing |
| Hyoidomandibular distance at rest | HMR | mm | Distance between the upper margin of the hyoid bone and lower margin of the mandible at the standing point immediately prior to swallowing |
| Hyoidovertebral distance during swallowing | HVS | mm | Distance between the anterior border of vertebral spine and hyoid bone during swallowing |
| Ordinal Variable | Abbreviation | Operational Definitions |
|---|---|---|
| Laryngeal closure | LC | Ability to close the laryngeal vestibule during swallowing, assessed based on the presence or absence of air in the vestibule. Ratings:
|
| Epiglottic movement | EM | Tilting of the epiglottis during swallowing, assessed based on the contact between the epiglottis and the CAU. Ratings:
|
| Initiation of pharyngeal swallowing | IPS | Site of onset of the swallowing reflex. Ratings:
|
| Tongue base retraction | TBR | Backward movement of the tongue during swallowing, assessed based on the contact between the tongue base and the posterior pharyngeal wall. Ratings:
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pizzorni, N.; Schindler, A.; Castellari, M.; Fantini, M.; Crosetti, E.; Succo, G. Swallowing Safety and Efficiency after Open Partial Horizontal Laryngectomy: A Videofluoroscopic Study. Cancers 2019, 11, 549. https://doi.org/10.3390/cancers11040549
Pizzorni N, Schindler A, Castellari M, Fantini M, Crosetti E, Succo G. Swallowing Safety and Efficiency after Open Partial Horizontal Laryngectomy: A Videofluoroscopic Study. Cancers. 2019; 11(4):549. https://doi.org/10.3390/cancers11040549
Chicago/Turabian StylePizzorni, Nicole, Antonio Schindler, Micol Castellari, Marco Fantini, Erika Crosetti, and Giovanni Succo. 2019. "Swallowing Safety and Efficiency after Open Partial Horizontal Laryngectomy: A Videofluoroscopic Study" Cancers 11, no. 4: 549. https://doi.org/10.3390/cancers11040549
APA StylePizzorni, N., Schindler, A., Castellari, M., Fantini, M., Crosetti, E., & Succo, G. (2019). Swallowing Safety and Efficiency after Open Partial Horizontal Laryngectomy: A Videofluoroscopic Study. Cancers, 11(4), 549. https://doi.org/10.3390/cancers11040549





