Plasma Metabolomics Identifies Lipid and Amino Acid Markers of Weight Loss in Patients with Upper Gastrointestinal Cancer
Abstract
1. Introduction
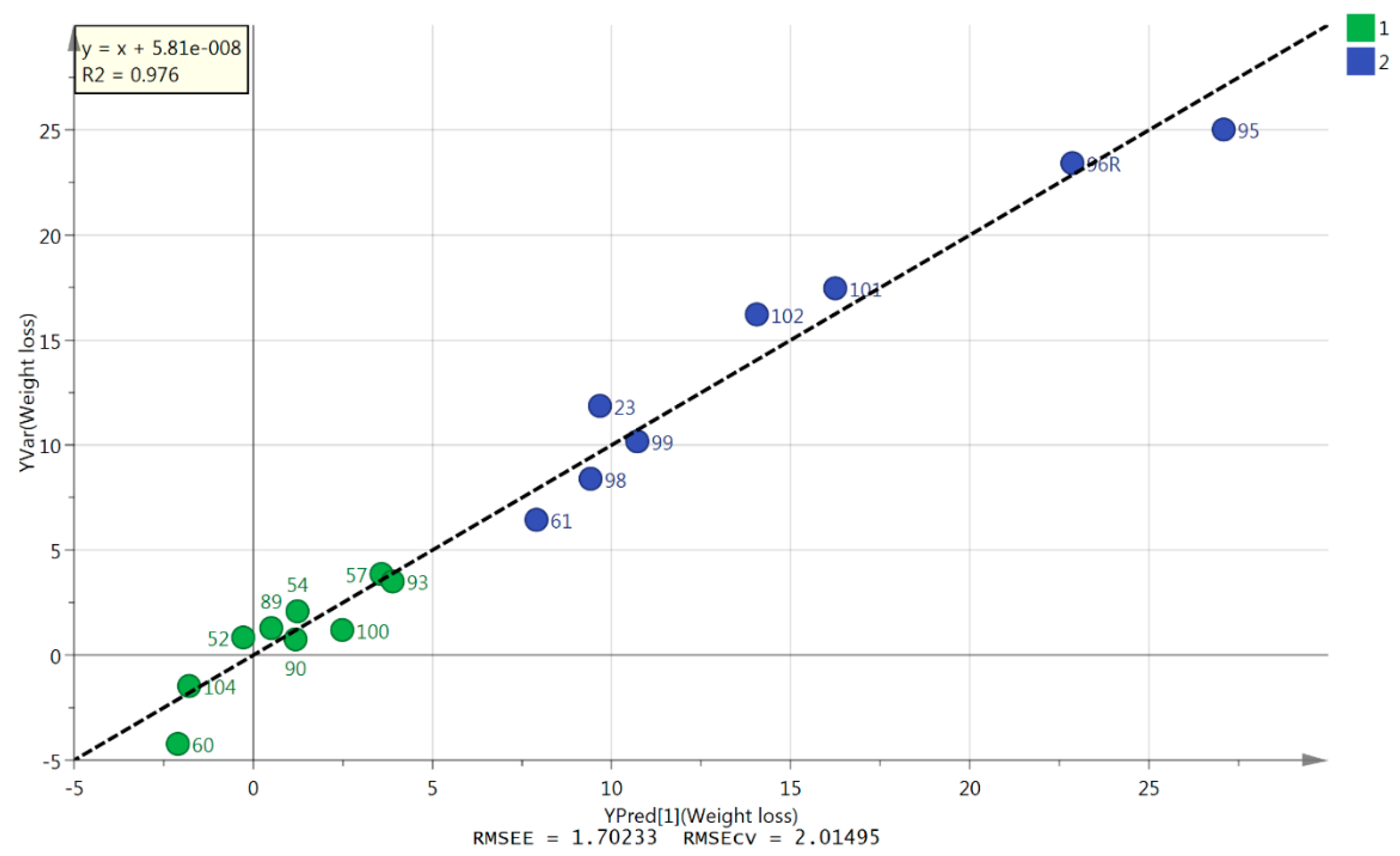
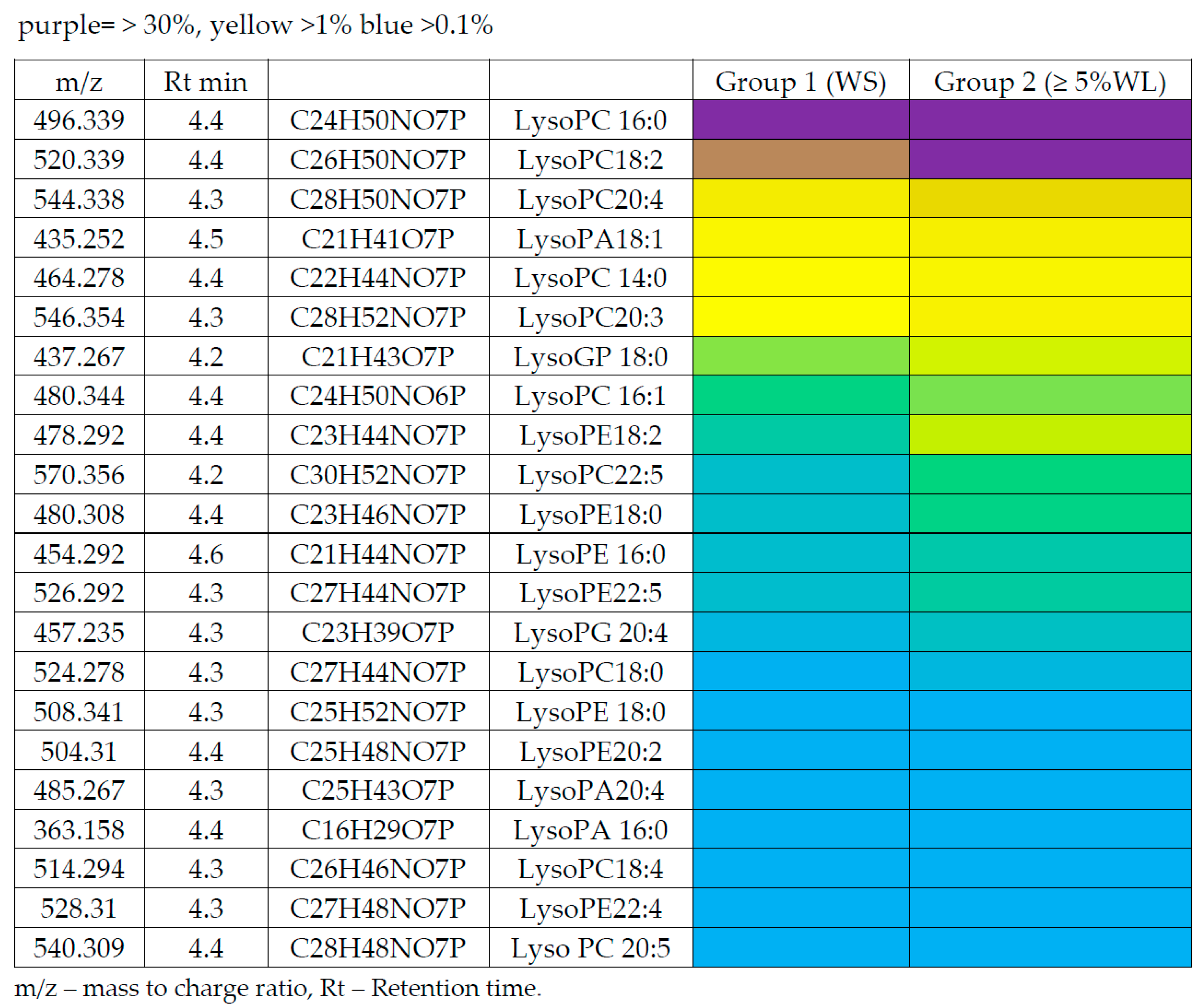
2. Results
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. CT Body Composition Analysis
4.3. Sample Collection and Storage
4.4. Chemicals and Solvents
4.5. Sample Preparation
4.6. LC-MS Conditions
4.7. Data Extraction and Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]
- Fearon, K.C.; Voss, A.C.; Hustead, D.S.; Cancer Cachexia Study Group. Definition of cancer cachexia: Effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis. Am. J. Clin. Nutr. 2006, 83, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.; Dinkel, C.; Mahajan, A.; Siddique, M.; Cook, G.J.R.; Goh, V. Imaging body composition in cancer patients: Visceral obesity, sarcopenia and sarcopenic obesity may impact on clinical outcome. Insights Imaging 2015, 6, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, A.; Armitage, E.; Garcia, A.; Barbas, C. Metabolomics as a tool for drug discovery and personalised medicine. Curr. Top. Med. Chem. 2014, 14, 2627–2636. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, T.; Ardeshirpour, F.; Asher, S.; Winnike, J.; Yin, X.; George, J.; Guttridge, D.C.; He, W.; Wysong, A.; Willis, M.S.; et al. Metabolomic analysis of cancer cachexia reveals distinct lipid and glucose alterations. Metabolomics 2008, 4, 216. [Google Scholar] [CrossRef]
- Eisner, R.; Stretch, C.; Eastman, T.; Xia, J.; Hau, D.; Damaraju, S.; Greiner, R.; Wishart, D.S.; Baracos, V.E. Learning to predict cancer-associated skeletal muscle wasting from 1H-NMR profiles of urinary metabolites. Metabolomics 2011, 7, 25–34. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Kobayashi, T.; Chavahara, N.; Inamura, Y.; Toyoda, M.; Kiyota, N.; Mukohara, T.; Nishiumi, S.; Azuma, T.; Yoshida, M.; et al. Metabolomics Evaluation of Serum Markers for Cachexia and Their Intra-Day Variation in Patients with Advanced Pancreatic Cancer. PLoS ONE 2014, 9, e113529. [Google Scholar] [CrossRef]
- Yang, Q.; Zhao, J.; Hao, J.; Li, B.; Huo, Y.; Han, Y.; Wan, L.L.; Li, J.; Huang, J.; Lu, J.; et al. Serum and urine metabolomics study reveals a distinct diagnostic model for cancer cachexia. J. Cachexia Sarcopenia Muscle 2018, 9, 71–85. [Google Scholar] [CrossRef]
- Cala, M.; Agullo-Ortuno, M.; Prieto-Garcia, E.; Gonzalez-Riano, C.; Parrilla-Rubio, L.; Barbas, C.; Díaz-García, C.V.; García, A.; Pernaut, C.; Adeva, J.; et al. Multiplatform plasma fingerprinting in cancer cachexia: A pilot observational and translational study. J. Cachexia Sarcopenia Muscle 2018, 9, 348–357. [Google Scholar] [CrossRef]
- Skipworth, R.J.E.; Stewart, G.D.; Bhana, M.; Christie, J.; Sturgeon, C.M.; Guttridge, D.C.; Cronshaw, A.D.; Fearon, K.C.; Ross, J.A. Mass spectrometric detection of candidate protein biomarkers of cancer cachexia in human urine. Int. J. Oncol. 2010, 36, 973–982. [Google Scholar]
- Argiles, J.; Busquets, S.; Stemmler, B.; Lopez-Soriano, F. Cancer cachexia: Understanding the molecular basis. Nat. Rev. Cancer 2014, 14, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Stephens, N.A.; Gallagher, I.J.; Rooyackers, O.; Skipworth, R.J.; Tan, B.H.; Marstrand, T.; Ross, J.A.; Guttridge, D.C.; Lundell, L.; Fearon, K.C.; et al. Using transcriptomics to identify and validate novel biomarkers of human skeletal muscle cancer cachexia. Genome Med. 2010, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, I.J.; Stephens, N.A.; MacDonald, A.J.; Skipworth, R.J.E.; Husi, H.; Greig, C.A.; Ross, J.A.; Timmons, J.A.; Fearon, K.C. Suppression of Skeletal Muscle Turnover in Cancer Cachexia: Evidence from the Transcriptome in Sequential Human Muscle Biopsies. Clin. Cancer Res. 2012, 18, 2817–2827. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, D.P.J.; Bakens, M.J.A.M.; Coolsen, M.M.E.; Rensen, S.S.; van Dam, R.M.; Bours, M.J.L.; Weijenberg, M.P.; Dejong, C.H.; Olde Damink, S.W. Low skeletal muscle radiation attenuation and visceral adiposity are associated with overall survival and surgical site infections in patients with pancreatic cancer. J. Cachexia Sarcopenia Muscle 2017, 8, 317–326. [Google Scholar] [CrossRef]
- Skipworth, R.J.E.; Moses, A.; Sangster, K.; Sturgeon, C.; Voss, A.; Fallon, M.; Anderson, R.A.; Ross, J.A.; Fearon, K.C. Interaction of gonadal status with systemic inflammation and opioid use in determining nutritional status and prognosis in advanced pancreatic cancer. Support. Care Cancer 2011, 19, 391–401. [Google Scholar] [CrossRef]
- Awad, S.; Tan, B.H.; Cui, H.; Bhalla, A.; Fearon, K.C.H.; Parsons, S.L.; Catton, J.A.; Lobo, D.N. Marked changes in body composition following neoadjuvant chemotherapy for oesophagogastric cancer. Clin Nutr. 2012, 31, 74–77. [Google Scholar] [CrossRef]
- Martin, L.; Birdsell, L.; MacDonald, N.; Reiman, T.; Clandinin, M.T.; McCargar, L.J.; Murphy, R.; Ghosh, S.; Sawyer, M.B.; Baracos, V.E. Cancer Cachexia in the Age of Obesity: Skeletal Muscle Depletion Is a Powerful Prognostic Factor, Independent of Body Mass Index. J. Clin. Oncol. 2013, 31, 1539–1547. [Google Scholar] [CrossRef]
- Raynal, P.; Montagner, A.; Dance, M.; Yart, A. Lysophospholipids and cancer: Current status and perpespectives. Pathol. Biol. 2005, 53, 57–62. [Google Scholar] [CrossRef]
- Fearon, K.C.H. Cancer cachexia and fat-muscle physiology. N. Engl. J. Med. 2011, 365, 565–567. [Google Scholar] [CrossRef]
- Shaw, J.; Wolfe, R. Fatty acid and glycerol kinetics in septic patients and in patients with gastrointestinal cancer. The response to glucose infusion and parenteral feeding. Ann. Surg. 1987, 205, 368–376. [Google Scholar] [CrossRef]
- Das, S.; Hoefler, G. The role of triglyceride lipases in cancer associated cachexia. Trends Mol. Med. 2013, 19, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, M.; Mazurak, V. Potential biomarkers of fat loss as a feature of cancer cachexia. Mediat. Inflamm. 2015, 820934. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Wolfe, R. Whole-body lipolysis and triglyceride-fatty acid cycling in cachectic patients with oesophageal cancer. J. Clin. Invest. 1990, 86, 1403–1408. [Google Scholar] [CrossRef] [PubMed]
- Gercel-Taylor, C.; Doering, D.; Kraemer, F.; Taylor, D. Abberations in normal systemic lipid metabolism in ovarian cancer patients. Gynecol. Oncol. 1996, 60, 35–41. [Google Scholar] [CrossRef]
- Dahlman, I.; Mejhert, N.; Linder, K.; Agustsson, T.; Mutch, D.; Kulyte, A.; Isaksson, B.; Permert, J.; Petrovic, N.; Nedergaard, J.; et al. Adipose tissue pathways involved in weight loss of cancer cachexia. Br. J. Cancer 2010, 102, 1541–1548. [Google Scholar] [CrossRef]
- Tsoli, M.; Swarbrick, M.; Robertson, G. Lipolytic and thermogenic depletion of adipose tissue in cancer cachexia. Semin. Cell Dev. Biol. 2016, 54, 68–81. [Google Scholar] [CrossRef]
- Beloribi-Djefaflia, S.; Vasseur, S.; Guillaumond, F. Lipid metabolic reprogramming in cancer cells. Oncogenesis 2016, 5, e189. [Google Scholar] [CrossRef]
- Ackerman, D.; Simon, M. Hypoxia, lipids and cancer: Surviving the harsh tumor microenvironment. Trends Cell Biol. 2015, 24, 472–478. [Google Scholar] [CrossRef]
- Acharyya, S.; Butchbach, M.E.R.; Sahenk, Z.; Wang, H.; Saji, M.; Carathers, M.; Skipworth, R.J.; Fearon, K.C.; Hollingsworth, M.A.; Muscarella, P.; et al. Dystrophin glycoprotein complex dysfunction: A regulatory link between muscular dystrophy and cancer cachexia. Cancer Cell 2005, 8, 421–432. [Google Scholar] [CrossRef]
- Stretch, C.; Eastman, T.; Mandal, R.; Eisner, R.; Wishart, D.; Moutzakis, M.; Prado, C.M.; Damaraju, S.; Ball, R.O.; Greiner, R.; et al. Prediction of skeletal muscle and fat mass in patients with advanced cancer using a metabolomic approach. J. Nutr. 2011, 1, 14–21. [Google Scholar] [CrossRef]
- Tao, L.; Zhou, J.; Yuan, C.; Zhang, L.; Li, D.; Si, D.; Xiu, D.; Zhong, L. Metabolomics identifies serum and exosomes metabolite markers of pancreatic cancer. Metabolomics 2019, 15, 86. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Wang, K.; Liu, G.; Wang, Y.; Xu, J.; Liu, L.; Li, M.; Shi, J.; Aa, J.; Yu, L. Metabolic Perturbation and Potential Markers in Patients with Esophageal Cancer. Gastroenterol. Res. Pr. 2017, 2017, 5469597. [Google Scholar] [CrossRef] [PubMed]
| Demographics | Group 1 Weight Stable (n = 9) | Group 2 ≥5% Weight Loss (n = 9) | p Values |
|---|---|---|---|
| Male: Female | 8:1 | 5:4 | N/A |
| Age (years) | 61 (4.65) | 66 (10.53) | 0.167 |
| % Weight loss | 2.13 (1.35) | 14.39 (6.56) | 0.001 * |
| SMI | 47.17 (6.26) | 45.82 (7.72) | 0.536 |
| SATI | 46.25 (20.38) | 58.43 (33.86) | 0.379 |
| VATI | 57.57 (55.28) | 42.10 (33.48) | 0.506 |
| BMI (kg2/m2) | 24.93 (4.42) | 26.29 (4.64) | 0.534 |
| CRP (mg/L) | 17.88 (27.06) | 32.56 (50.44) | 0.453 |
| Cancer type | Pancreatic – 1 | Pancreatic – 6 | N/A |
| Oesophageal – 6 | Oesophageal – 2 | ||
| Gastric - 2 | Duodenal - 1 | ||
| Disease stage | 1 (n = 1) | 1 (n = 1) | |
| 2 (n = 0) | 2 (n = 5) | ||
| 3 (n = 6) | 3 (n = 1) | ||
| 4 (n = 1) | 4 (n = 2) | ||
| Unknown (n = 1) | - | ||
| Pre-operative chemotherapy | 4 | 2 | N/A |
| m/z | Rt Min. | Metabolite | VIP Value |
|---|---|---|---|
| 520.339 | 4.4 | Lyso-PC 18:2 | 1.82 |
| 116.071 | 13.0 | L-Proline | 1.43 |
| 255.233 | 4.3 | Hexadecanoic acid | 0.54 |
| 281.249 | 3.8 | Octadecenoic acid | 0.42 |
| 166.086 | 10.0 | Phenylalanine | 0.36 |
| 480.344 | 4.4 | Lyso-PC 16:1 | 0.20 |
| Polarity | m/z | Rt(min) | Metabolite | p Value | Ratio WL/WS |
|---|---|---|---|---|---|
| Amino acids | |||||
| P | 116.071 | 13.0 | L-Proline | 0.015 | 1.36 |
| P | 166.086 | 10.0 | L-Phenylalanine | 0.619 | 0.87 |
| Fatty acids | |||||
| N | 214.048 | 4.3 | sn-glycero-3-Phosphoethanolamine | 0.006 | 1.78 |
| N | 255.233 | 4.3 | Hexadecanoic acid | 0.049 | 1.21 |
| N | 277.217 | 3.9 | Octadecatrienoic acid | 0.010 | 1.60 |
| N | 279.233 | 4.2 | Linoleate | 0.002 | 1.36 |
| N | 281.249 | 3.8 | Octadecenoic acid | 0.023 | 1.22 |
| N | 293.249 | 4.2 | Nonadecadienoic acid | 0.019 | 1.24 |
| N | 303.233 | 4.1 | Eicosatetraenoic acid | 0.022 | 1.37 |
| N | 305.249 | 4.2 | Eicosatrienoic acid | 0.054 | 1.50 |
| N | 327.233 | 4.2 | Docosahexaenoic acid | 0.025 | 0.81 |
| N | 329.249 | 4.1 | Docosapentaenoic acid | 0.009 | 1.46 |
| N | 331.264 | 3.9 | Docosatetraenoic acid | 0.014 | 1.68 |
| P/N | 380.255 | 5.1 | Sphingenine phosphate | 0.033 | 1.28 |
| Lipids | |||||
| N | 214.048 | 4.3 | Glycerophosphoethanolamine | 0.006 | 1.78 |
| N | 381.205 | 4.6 | LPA 14:0 | 0.010 | 1.73 |
| N | 393.241 | 4.4 | LPA 16:0 ether | 0.048 | 1.37 |
| N | 433.236 | 4.4 | LPA 18:2 | 0.001 | 1.67 |
| N | 435.252 | 4.5 | LPA18:1 | 0.006 | 1.40 |
| N | 437.267 | 4.2 | LPA 18:0 | 0.028 | 1.23 |
| P/N | 454.292 | 4.6 | LPE 16:0 | 0.040 | 1.44 |
| N | 457.235 | 4.3 | LPA 20:4 | 0.001 | 1.62 |
| N | 464.278 | 4.4 | LPC 14:1 | 0.007 | 1.36 |
| P | 468.308 | 4.6 | LPC 14:0 | 0.026 | 1.58 |
| P/N | 476.278 | 4.4 | LPE 18:2 | 0.013 | 1.98 |
| P/N | 478.292 | 4.4 | LPE 18:1 | 0.013 | 2.02 |
| P/N | 480.308 | 4.4 | LPE 18:0 | 0.012 | 2.07 |
| P/N | 480.344 | 4.4 | LPC16:1 | 0.089 | 1.32 |
| N | 485.267 | 4.3 | LPA 22:4 | 0.007 | 1.96 |
| P/N | 496.339 | 4.4 | LPC 16:0 | 0.040 | 1.34 |
| N | 498.262 | 4.3 | LPE 20:5 | 0.053 | 2.13 |
| P/N | 500.278 | 4.4 | LPE 20:4 | 0.002 | 2.36 |
| N | 504.31 | 4.4 | LPE 20:2 | 0.002 | 1.65 |
| N | 514.294 | 4.3 | LPC 18:4 | 0.005 | 2.28 |
| P/N | 520.339 | 4.4 | LPC 18:2 | 0.001 | 1.75 |
| P/N | 524.278 | 4.3 | LPE 22:6 | 0.032 | 1.45 |
| N | 526.294 | 4.3 | LPE 22:5 | 0.004 | 2.51 |
| N | 528.31 | 4.3 | LPE22:4 | 0.004 | 2.01 |
| P/N | 544.338 | 4.3 | LPC 20:4 | 0.014 | 1.81 |
| P/N | 546.354 | 4.3 | LPC 20:3 | 0.026 | 1.91 |
| P | 570.356 | 4.2 | LPC 22:5 | 0.009 | 1.89 |
| P | 731.605 | 4.2 | SMd18:0/18:1 | 0.052 | 1.29 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, J.; Alshehri, A.; Ramage, M.I.; Stephens, N.A.; Mullen, A.B.; Boyd, M.; Ross, J.A.; Wigmore, S.J.; Watson, D.G.; Skipworth, R.J.E. Plasma Metabolomics Identifies Lipid and Amino Acid Markers of Weight Loss in Patients with Upper Gastrointestinal Cancer. Cancers 2019, 11, 1594. https://doi.org/10.3390/cancers11101594
Miller J, Alshehri A, Ramage MI, Stephens NA, Mullen AB, Boyd M, Ross JA, Wigmore SJ, Watson DG, Skipworth RJE. Plasma Metabolomics Identifies Lipid and Amino Acid Markers of Weight Loss in Patients with Upper Gastrointestinal Cancer. Cancers. 2019; 11(10):1594. https://doi.org/10.3390/cancers11101594
Chicago/Turabian StyleMiller, Janice, Ahmed Alshehri, Michael I. Ramage, Nathan A. Stephens, Alexander B. Mullen, Marie Boyd, James A. Ross, Stephen J. Wigmore, David G. Watson, and Richard J.E. Skipworth. 2019. "Plasma Metabolomics Identifies Lipid and Amino Acid Markers of Weight Loss in Patients with Upper Gastrointestinal Cancer" Cancers 11, no. 10: 1594. https://doi.org/10.3390/cancers11101594
APA StyleMiller, J., Alshehri, A., Ramage, M. I., Stephens, N. A., Mullen, A. B., Boyd, M., Ross, J. A., Wigmore, S. J., Watson, D. G., & Skipworth, R. J. E. (2019). Plasma Metabolomics Identifies Lipid and Amino Acid Markers of Weight Loss in Patients with Upper Gastrointestinal Cancer. Cancers, 11(10), 1594. https://doi.org/10.3390/cancers11101594








