Effects of Aspirin or Clopidogrel on Colorectal Cancer Chemoprevention in Patients with Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Methods
2.1. Data Source
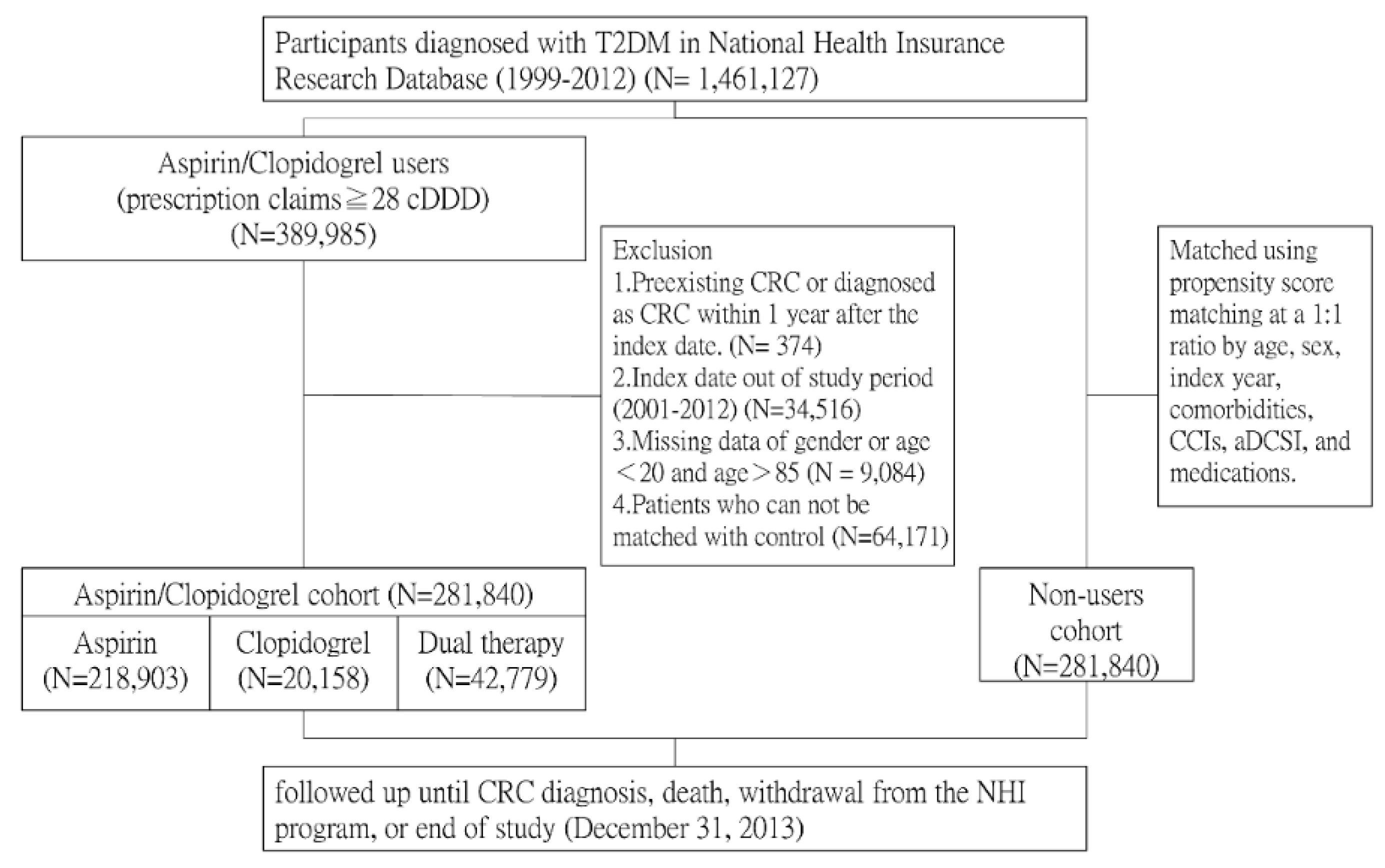
2.2. Study Population
2.3. Potential Confounders
2.4. Main Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics
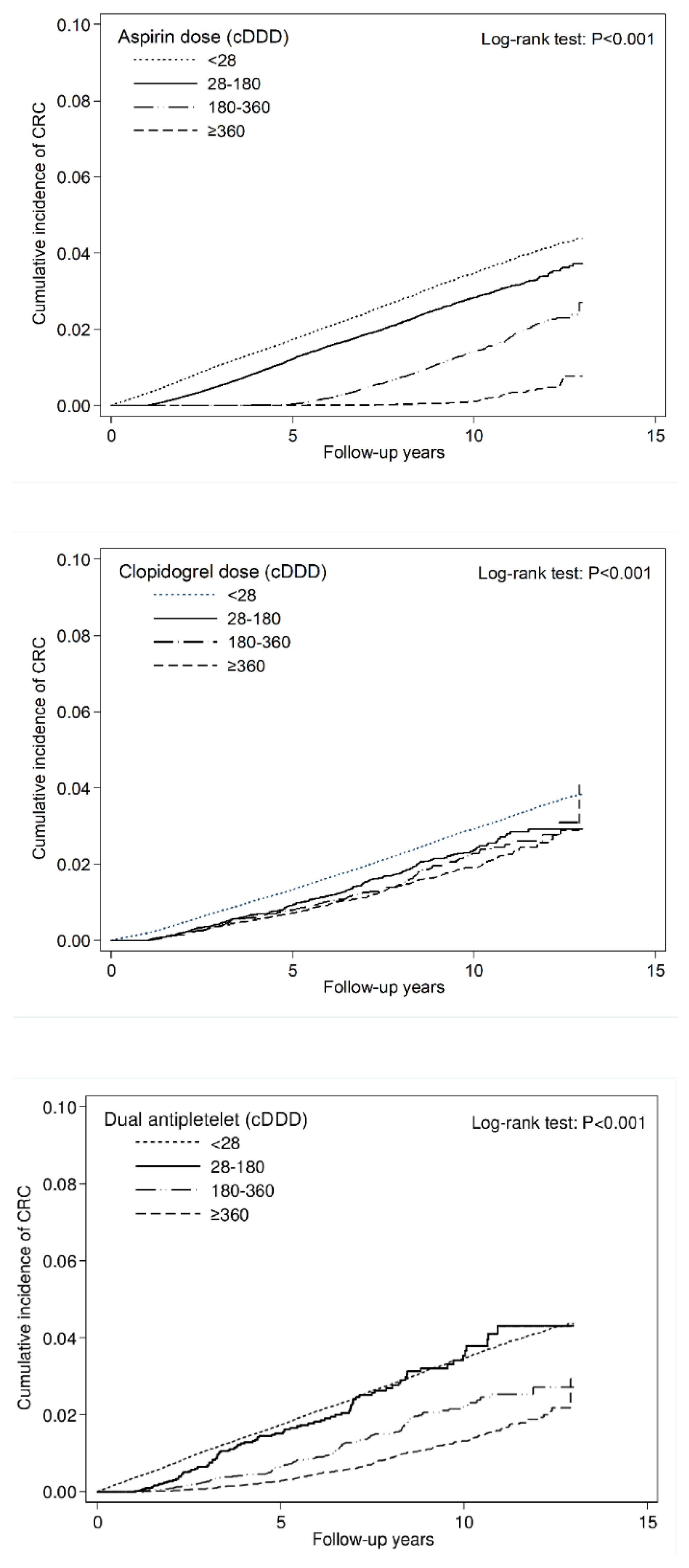
3.2. Overall Incidence and Estimated HR of CRC
3.3. Subgroup Analysis
3.4. Incidence and HR of CRC Stratified by Colon Cancer and Rectal Cancer
3.5. Sensitivity Analysis after Considering the Competing Risk of Death
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Yabroff, K.R.; Borowski, L.; Lipscomb, J. Economic studies in colorectal cancer: Challenges in measuring and comparing costs. J. Natl. Cancer Inst. Monogr. 2013, 2013, 62–78. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.E.; Sicree, R.A.; Zimmet, P.Z. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Suh, S.; Kim, K.W. Diabetes and cancer: Is diabetes causally related to cancer? Diabetes Metab. J. 2011, 35, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Wu, X.; Wu, B.; Pei, D.; Zhang, L.; Wei, L. The relationship between diabetes and colorectal cancer prognosis: A meta-analysis based on the cohort studies. PLoS ONE 2017, 12, e0176068. [Google Scholar] [CrossRef] [PubMed]
- Bardia, A.; Ebbert, J.O.; Vierkant, R.A.; Limburg, P.J.; Anderson, K.; Wang, A.H.; Olson, J.E.; Vachon, C.M.; Cerhan, J.R. Association of aspirin and nonaspirin nonsteroidal anti-inflammatory drugs with cancer incidence and mortality. J. Natl. Cancer Inst. 2007, 99, 881–889. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rothwell, P.M.; Wilson, M.; Elwin, C.E.; Norrving, B.; Algra, A.; Warlow, C.P.; Meade, T.W. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 2010, 376, 1741–1750. [Google Scholar] [CrossRef]
- Veettil, S.K.; Jinatongthai, P.; Nathisuwan, S.; Teerawattanapong, N.; Ching, S.M.; Lim, K.G.; Saokaew, S.; Phisalprapa, P.; Reid, C.M.; Chaiyakunapruk, N. Efficacy and safety of chemopreventive agents on colorectal cancer incidence and mortality: Systematic review and network meta-analysis. Clin. Epidemiol. 2018, 10, 1433–1445. [Google Scholar] [CrossRef]
- Peto, R.; Gray, R.; Collins, R.; Wheatley, K.; Hennekens, C.; Jamrozik, K.; Warlow, C.; Hafner, B.; Thompson, E.; Norton, S.; et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br. Med. J. (Clin. Res. Ed). 1988, 296, 313–316. [Google Scholar] [CrossRef]
- Farrell, B.; Godwin, J.; Richards, S.; Warlow, C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: Final results. J. Neurol. Neurosurg. Psychiatry 1991, 54, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Yang, T.; Gan, Y.; Li, W.; Wang, C.; Gong, Y.; Lu, Z. Associations between aspirin use and the risk of cancers: A meta-analysis of observational studies. BMC Cancer 2018, 18, 288. [Google Scholar] [CrossRef] [PubMed]
- Leader, A.; Zelikson-Saporta, R.; Pereg, D.; Spectre, G.; Rozovski, U.; Raanani, P.; Lishner, M. The Effect of Combined Aspirin and Clopidogrel Treatment on Cancer Incidence. Am. J. Med. 2017, 130, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Miguel, A.; Garcia-Rodriguez, L.A.; Gil, M.; Montoya, H.; Rodriguez-Martin, S.; de Abajo, F.J. Clopidogrel and Low-Dose Aspirin, Alone or Together, Reduce Risk of Colorectal Cancer. Clin. Gastroenterol. Hepatol. 2018, 17, 2024–2033.e2. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Grootendorst, P.; Anderson, G.M. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: A Monte Carlo study. Stat. Med. 2007, 26, 734–753. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.R.; Rubin, D.B. Constructing a Control Group Using Multivariate Matched Sampling Methods That Incorporate the Propensity Score. Am. Stat. 1985, 39, 33–38. [Google Scholar]
- Flossmann, E.; Rothwell, P.M. Effect of aspirin on long-term risk of colorectal cancer: Consistent evidence from randomised and observational studies. Lancet 2007, 369, 1603–1613. [Google Scholar] [CrossRef]
- Algra, A.M.; Rothwell, P.M. Effects of regular aspirin on long-term cancer incidence and metastasis: A systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol. 2012, 13, 518–527. [Google Scholar] [CrossRef]
- Okada, S.; Morimoto, T.; Ogawa, H.; Sakuma, M.; Matsumoto, C.; Soejima, H.; Nakayama, M.; Doi, N.; Jinnouchi, H.; Waki, M.; et al. Effect of Aspirin on Cancer Chemoprevention in Japanese Patients With Type 2 Diabetes: 10-Year Observational Follow-up of a Randomized Controlled Trial. Diabetes Care 2018, 41, 1757–1764. [Google Scholar] [CrossRef]
- Chan, A.T.; Giovannucci, E.L.; Meyerhardt, J.A.; Schernhammer, E.S.; Wu, K.; Fuchs, C.S. Aspirin dose and duration of use and risk of colorectal cancer in men. Gastroenterology 2008, 134, 21–28. [Google Scholar] [CrossRef]
- Chan, A.T.; Giovannucci, E.L.; Meyerhardt, J.A.; Schernhammer, E.S.; Curhan, G.C.; Fuchs, C.S. Long-term use of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA 2005, 294, 914–923. [Google Scholar] [CrossRef] [PubMed]
- Cole, B.F.; Logan, R.F.; Halabi, S.; Benamouzig, R.; Sandler, R.S.; Grainge, M.J.; Chaussade, S.; Baron, J.A. Aspirin for the chemoprevention of colorectal adenomas: Meta-analysis of the randomized trials. J. Natl. Cancer Inst. 2009, 101, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Cea Soriano, L.; Soriano-Gabarro, M.; Garcia Rodriguez, L.A. The Protective Effect of Low-Dose Aspirin against Colorectal Cancer Is Unlikely Explained by Selection Bias: Results from Three Different Study Designs in Clinical Practice. PLoS ONE. 2016, 11, e0159179. [Google Scholar] [CrossRef] [PubMed]
- Contursi, A.; Grande, R.; Dovizio, M.; Bruno, A.; Fullone, R.; Patrignani, P. Platelets in cancer development and diagnosis. Biochem. Soc. Trans. 2018, 46, 1517–1527. [Google Scholar] [CrossRef] [PubMed]
- Jovani, M.; Chan, A.T. Do Aspirin and Clopidogrel Follow the Same Road Toward Prevention of Colorectal Cancer? Clin. Gastroenterol. Hepatol. 2019, 17, 1945–1947. [Google Scholar] [CrossRef]
- Drew, D.A.; Cao, Y.; Chan, A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer 2016, 16, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Amiri, L.; John, A.; Shafarin, J.; Adeghate, E.; Jayaprakash, P.; Yasin, J.; Howarth, F.C.; Raza, H. Enhanced Glucose Tolerance and Pancreatic Beta Cell Function by Low Dose Aspirin in Hyperglycemic Insulin-Resistant Type 2 Diabetic Goto-Kakizaki (GK) Rats. Cell Physiol. Biochem. 2015, 36, 1939–1950. [Google Scholar] [CrossRef]
- Abdin, A.A.; Baalash, A.A.; Hamooda, H.E. Effects of rosiglitazone and aspirin on experimental model of induced type 2 diabetes in rats: Focus on insulin resistance and inflammatory markers. J. Diabetes Complicat. 2010, 24, 168–178. [Google Scholar] [CrossRef]
- Komninou, D.; Ayonote, A.; Richie, J.P.; Jr Rigas, B. Insulin resistance and its contribution to colon carcinogenesis. Exp. Biol. Med. (Maywood) 2003, 228, 396–405. [Google Scholar] [CrossRef]
- Taher, M.A.; Nassir, E.S. Beneficial effects of clopidogrel on glycemic indices and oxidative stress in patients with type 2 diabetes. Saudi Pharm. J. 2011, 19, 107–113. [Google Scholar] [CrossRef]
- Nasir, A.; Kaiser, H.E.; Boulware, D.; Hakam, A.; Zhao, H.; Yeatman, T.; Barthel, J.; Coppola, D. Cyclooxygenase-2 expression in right- and left-sided colon cancer: A rationale for optimization of cyclooxygenase-2 inhibitor therapy. Clin. Colorectal Cancer 2004, 3, 243–247. [Google Scholar] [CrossRef] [PubMed]
| Variables | Nonusers N (%) | Users | Standardized Mean Difference § | ||
|---|---|---|---|---|---|
| Aspirin Monotherapy N (%) | Clopidogrel Monotherapy N (%) | Dual Antiplatelet N (%) | |||
| N = 281,840 | N = 218,903 | N = 20,158 | N = 42,779 | ||
| Sex | 0.016 | ||||
| Female | 131,113 (46.5) | 105,795 (48.3) | 8403 (41.7) | 14,719 (34.4) | |
| Male | 150,727 (53.5) | 113,108 (51.7) | 11,755 (58.3) | 28,060 (65.6) | |
| Age, Years | |||||
| <50 | 47,336 (16.8) | 37,300 (17.0) | 1725 (8.6) | 6196 (14.5) | 0.020 |
| 50–59 | 77,979 (27.7) | 66,656 (30.5) | 4163 (20.7) | 11,854 (27.7) | 0.037 |
| 60–69 | 76,223 (27.0) | 62,570 (28.6) | 5465 (27.1) | 12,880 (30.1) | 0.037 |
| 70–85 | 80,302 (28.5) | 52,377 (23.9) | 8805 (43.7) | 11,849 (27.7) | 0.058 |
| Mean (SD) | 61.9 (12.0) | 61.0 (11.3) | 66.6 (11.3) | 62.3 (11.1) | 0.027 |
| Comorbidities | |||||
| Hypertension | 229,050 (81.3) | 171,934 (78.5) | 16,805 (83.4) | 33,324 (77.9) | 0.062 |
| Hyperlipidemia | 166,209 (59.0) | 127,098 (58.1) | 11,427 (56.7) | 24,046 (56.2) | 0.026 |
| CAD | 106,197 (37.7) | 79,578 (36.4) | 11,205 (55.6) | 20,904 (48.9) | 0.040 |
| Stroke | 40,658 (14.4) | 31,205 (14.3) | 7154 (35.5) | 6865 (16.1) | 0.045 |
| Arrhythmia | 47,949 (17.0) | 36,154 (16.5) | 5294 (26.3) | 7761 (18.1) | 0.012 |
| CKD | 14,252 (5.1) | 8464 (3.9) | 2896 (14.4) | 2643 (6.2) | 0.004 |
| COPD | 88,872 (31.5) | 65,698 (30.0) | 8359 (41.5) | 14,000 (32.7) | 0.006 |
| CCIs | |||||
| 0 | 176,684 (62.7) | 140,110 (64.0) | 4612 (22.9) | 18,781 (43.9) | 0.096 |
| 1 | 49,155 (17.4) | 41,522 (19.0) | 4537 (22.5) | 11,885 (27.8) | 0.080 |
| 2 | 25,954 (9.2) | 20,886 (9.5) | 4114 (20.4) | 6766 (15.8) | 0.068 |
| ≥3 | 30,047 (10.7) | 16,385 (7.5) | 6895 (34.2) | 5347 (12.5) | 0.017 |
| aDCSI | |||||
| 0 | 73,470 (26.1) | 53,935 (24.6) | 1289 (6.4) | 8056 (18.8) | 0.084 |
| 1 | 51,599 (18.3) | 42,006 (19.2) | 1527 (7.6) | 6707 (15.7) | 0.013 |
| ≥2 | 156,771 (55.6) | 122,962 (56.2) | 17,342 (86.0) | 28,016 (65.5) | 0.083 |
| Medications | |||||
| Anti-DM drugs | |||||
| Metformin | 130,138 (46.2) | 99,753 (45.6) | 8876 (44.0) | 17,812 (41.6) | 0.026 |
| Sulfonylureas | 134,766 (47.8) | 101,823 (46.5) | 9032 (44.8) | 20,271 (47.4) | 0.026 |
| AGI | 24,870 (8.8) | 17,103 (7.8) | 2506 (12.4) | 3200 (7.5) | 0.026 |
| Thiazolidinediones | 23,513 (8.3) | 15,933 (7.3) | 2238 (11.1) | 2953 (6.9) | 0.031 |
| Insulin | 41,127 (14.6) | 26,729 (12.2) | 6188 (30.7) | 6736 (15.8) | 0.015 |
| Anti-HTN drugs | |||||
| α-Blockers | 70,952 (25.2) | 51,343 (23.5) | 7832 (38.9) | 12,548 (29.3) | 0.006 |
| β-Blockers | 198,753 (70.5) | 149,804 (68.4) | 156,68 (77.7) | 30,142 (70.5) | 0.024 |
| PSD | 21,794 (7.7) | 14,969 (6.8) | 3324 (16.5) | 3553 (8.3) | 0.001 |
| Thiazides | 78,801 (28.0) | 60,352 (27.6) | 6964 (34.6) | 12,008 (28.1) | 0.004 |
| Loop diuretics | 95,472 (33.9) | 68,950 (31.5) | 10,658 (52.9) | 15,516 (36.3) | 0.003 |
| CCBs | 207,337 (73.6) | 155,461 (71.0) | 16,236 (80.5) | 30,879 (72.2) | 0.038 |
| ACEIs | 171,116 (60.7) | 128,789 (58.8) | 13,856 (68.7) | 26,076 (61.0) | 0.017 |
| ARBs | 88,480 (31.4) | 68,309 (31.2) | 9568 (47.5) | 14,261 (33.3) | 0.028 |
| Statins | 106,396 (37.8) | 79,589 (36.4) | 9453 (46.9) | 16,766 (39.2) | 0.004 |
| NSAIDs | 258,544 (91.7) | 201,541 (92.1) | 18,242 (90.5) | 38,551 (90.1) | 0.003 |
| Variables | No. non-CRC (%) | No. CRC (%) | Person-Years | IR# | Crude HR (95% CI) | p value | Adjusted HR (95% CI) † | p value |
|---|---|---|---|---|---|---|---|---|
| Aspirin or Clopidogrel | ||||||||
| Nonusers | 276082 (98.0) | 5758 (2.0) | 1635323 | 3.52 | Reference | Reference | ||
| Users | 278257 (98.7) | 3583 (1.3) | 1774199 | 2.02 | 0.57 (0.55–0.59) | <0.001 | 0.55 (0.53–0.58) | <0.001 |
| Aspirin or Clopidogrel | ||||||||
| Nonusers | 276082 (98.0) | 5758 (2.0) | 1635323 | 3.52 | Reference | Reference | ||
| Aspirin Monotherapy | 216058 (98.7) | 2845 (1.3) | 1393473 | 2.04 | 0.58 (0.55–0.60) | <0.001 | 0.59 (0.56–0.61) | <0.001 |
| Clopidogrel Monotherapy | 19888 (98.7) | 270 (1.3) | 78279.76 | 3.45 | 1.03 (0.91–1.17) | 0.609 | 0.77 (0.68–0.87) | <0.001 |
| Dual Antiplatelet Therapy | 42311 (98.9) | 468 (1.1) | 302446 | 1.55 | 0.43 (0.39–0.47) | <0.001 | 0.37 (0.33–0.40) | <0.001 |
| Dose of Aspirin Used | ||||||||
| <28 cDDDs | 295970 (98.0) | 6028 (2.0) | 1713603 | 3.52 | Reference | Reference | ||
| 28–179 cDDDs | 185267 (98.6) | 2661 (1.4) | 1053000 | 2.53 | 0.72 (0.69–0.76) | <0.001 | 0.73 (0.69–0.76) | <0.001 |
| 180–359 cDDDs | 64802 (99.1) | 621 (1.0) | 549969.8 | 1.13 | 0.31 (0.28–0.33) | <0.001 | 0.31 (0.28–0.33) | <0.001 |
| ≥360 cDDDs | 8300 (99.6) | 31 (0.4) | 92948.86 | 0.33 | 0.09 (0.06–0.12) | <0.001 | 0.08 (0.06–0.12) | <0.001 |
| p for Trend | <0.001 | <0.001 | ||||||
| Dose of Clopidogrel Used | ||||||||
| <28 cDDDs | 492140 (98.3) | 8603 (1.7) | 3028796 | 2.84 | Reference | Reference | ||
| 28–179 cDDDs | 22691 (98.8) | 280 (1.2) | 130777 | 2.14 | 0.75 (0.67–0.85) | <0.001 | 0.63 (0.56–0.71) | <0.001 |
| 180–359 cDDDs | 13075 (98.9) | 148 (1.1) | 76987.56 | 1.92 | 0.68 (0.58–0.80) | <0.001 | 0.58 (0.49–0.68) | <0.001 |
| ≥360 cDDDs | 26433 (98.8) | 310 (1.2) | 172961.2 | 1.79 | 0.63 (0.56–0.70) | <0.001 | 0.50 (0.44–0.56) | <0.001 |
| P for trend | <0.001 | <0.001 | ||||||
| Dose of Dual Antiplatelet Used | ||||||||
| <28 cDDDs | 276082 (98.0) | 5758 (2.0) | 1635323 | 3.52 | Reference | Reference | ||
| 28–179 cDDDs | 5294 (98.2) | 100 (1.9) | 30816.84 | 3.24 | 0.92 (0.76–1.12) | 0.421 | 0.78 (0.64–0.95) | 0.014 |
| 180–359 cDDDs | 11490 (98.9) | 133 (1.1) | 73431.77 | 1.81 | 0.51 (0.43–0.61) | <0.001 | 0.44 (0.37–0.53) | <0.001 |
| ≥360 cDDDs | 25527 (99.1) | 235 (0.9) | 198197.4 | 1.19 | 0.33 (0.29–0.38) | <0.001 | 0.28 (0.25–0.32) | <0.001 |
| P for trend | <0.001 | <0.001 | ||||||
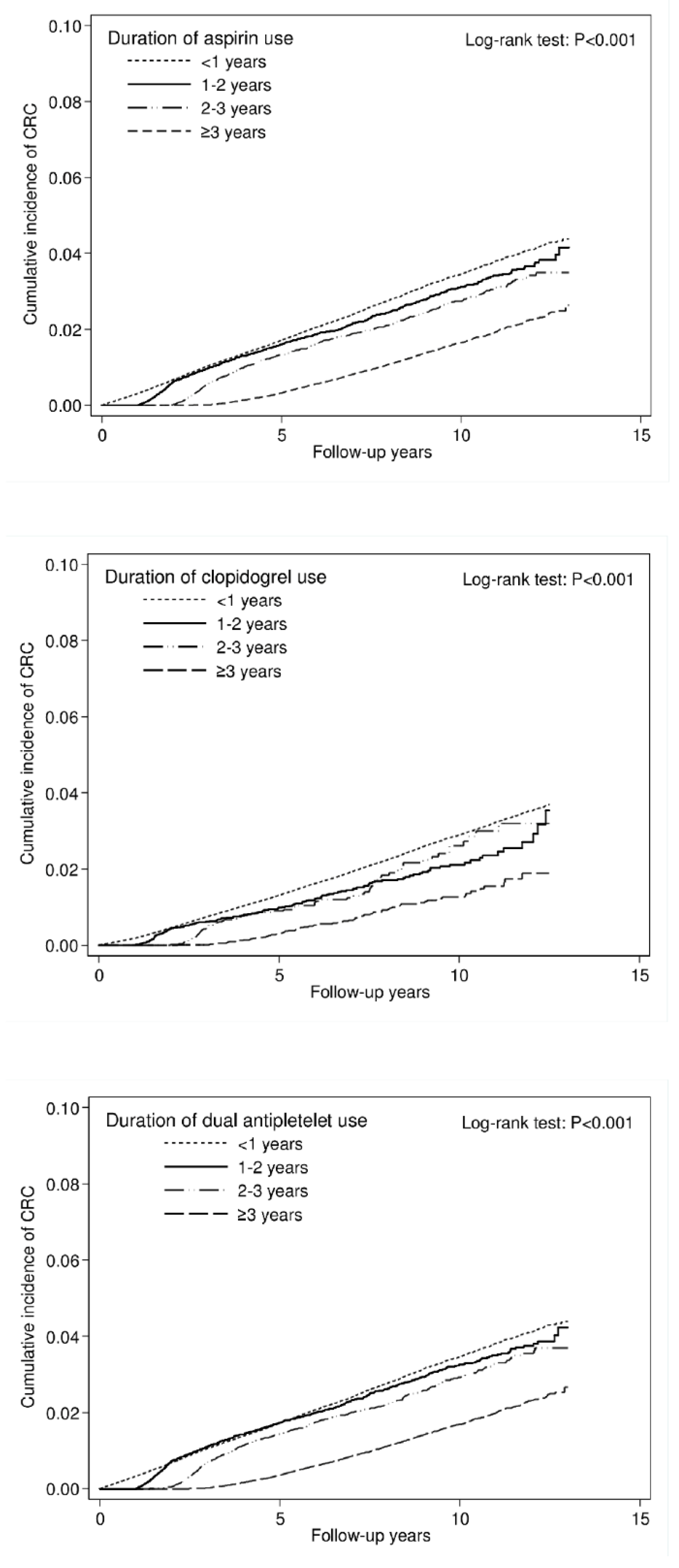
| Duration of Aspirin Use, Years | ||||||||
| <1 | 313173 (98.0) | 6305 (2.0) | 1807507 | 3.49 | Reference | Reference | ||
| 1–2 | 64177 (98.5) | 999 (1.5) | 326200.2 | 3.06 | 0.89 (0.83–0.95) | 0.001 | 0.90 (0.84–0.96) | 0.002 |
| 2–3 | 44925 (98.6) | 620 (1.4) | 249687.8 | 2.48 | 0.72 (0.66–0.78) | <0.001 | 0.71 (0.65–0.77) | <0.001 |
| ≥3 | 132064 (98.9) | 1417 (1.1) | 1026127 | 1.38 | 0.38 (0.36–0.41) | <0.001 | 0.38 (0.36–0.40) | <0.001 |
| P for trend | <0.001 | <0.001 | ||||||
| Duration of Clopidogrel Use, Years | ||||||||
| <1 | 527837 (98.3) | 9039 (1.7) | 3236326 | 2.79 | Reference | Reference | ||
| 1–2 | 12145 (98.8) | 152 (1.2) | 71455.8 | 2.13 | 0.76 (0.65–0.90) | 0.001 | 0.64 (0.54–0.75) | <0.001 |
| 2v3 | 5409 (98.7) | 73 (1.3) | 33470.92 | 2.18 | 0.78 (0.62–0.98) | 0.036 | 0.63 (0.50–0.79) | <0.001 |
| ≥3 | 8948 (99.2) | 77 (0.9) | 68269.17 | 1.13 | 0.40 (0.32–0.50) | <0.001 | 0.31 (0.25–0.39) | <0.001 |
| p for trend | <0.001 | <0.001 | ||||||
| Duration of Dual Antiplatelet Use, Years | ||||||||
| <1 | 299519 (98.0) | 6114 (2.0) | 1744497 | 3.50 | Reference | Reference | ||
| 1–2 | 63439 (98.4) | 1009 (1.6) | 309113.5 | 3.26 | 0.95 (0.89–1.02) | 0.155 | 0.96 (0.89–1.02) | 0.194 |
| 2–3 | 46385 (98.6) | 651 (1.4) | 246389.1 | 2.64 | 0.77 (0.71–0.83) | <0.001 | 0.75 (0.69–0.81) | <0.001 |
| ≥3 | 144996 (98.9) | 1567 (1.1) | 1109523 | 1.41 | 0.39 (0.37–0.41) | <0.001 | 0.38 (0.36–0.40) | <0.001 |
| p for trend | <0.001 | <0.001 | ||||||
| Variables | Nonusers | Aspirin Monotherapy | Clopidogrel Monotherapy | Dual Antiplatelet Therapy | |||
|---|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) † | p value | Adjusted HR (95% CI) † | p value | Adjusted HR (95% CI) † | p value | ||
| Sex | |||||||
| Female | Reference | 0.57 (0.53–0.61) | <0.001 | 0.77 (0.63–0.94) | 0.01 | 0.39 (0.33–0.45) | <0.001 |
| Male | Reference | 0.60 (0.56–0.64) | <0.001 | 0.76 (0.65–0.90) | 0.001 | 0.36 (0.32–0.40) | <0.001 |
| Age | |||||||
| <50 | Reference | 0.58 (0.48–0.69) | <0.001 | 0.88 (0.45–1.73) | 0.714 | 0.47 (0.32–0.69) | <0.001 |
| 50–59 | Reference | 0.59 (0.54–0.65) | <0.001 | 0.58 (0.40–0.86) | 0.006 | 0.43 (0.35–0.52) | <0.001 |
| 60–69 | Reference | 0.54 (0.50–0.58) | <0.001 | 0.70 (0.55–0.88) | 0.002 | 0.32 (0.27–0.37) | <0.001 |
| 70–85 | Reference | 0.63 (0.59–0.68) | <0.001 | 0.85 (0.72–1.00) | 0.048 | 0.37 (0.31–0.42) | <0.001 |
| CCIs | |||||||
| 0 | Reference | 0.60 (0.57–0.64) | <0.001 | 0.90 (0.71–1.14) | 0.361 | 0.35 (0.31–0.41) | <0.001 |
| 1 | Reference | 0.56 (0.51–0.62) | <0.001 | 0.66 (0.51–0.86) | 0.002 | 0.39 (0.32–0.46) | <0.001 |
| 2 | Reference | 0.56 (0.49–0.64) | <0.001 | 0.69 (0.52–0.91) | 0.008 | 0.36 (0.28–0.45) | <0.001 |
| ≥3 | Reference | 0.60 (0.52–0.70) | <0.001 | 0.80 (0.64–1.01) | 0.057 | 0.34 (0.26–0.45) | <0.001 |
| aDCSI | |||||||
| 0 | Reference | 0.62 (0.57–0.68) | <0.001 | 0.97 (0.62–1.53) | 0.898 | 0.31 (0.24–0.40) | <0.001 |
| 1 | Reference | 0.59 (0.53–0.66) | <0.001 | 0.94 (0.63–1.42) | 0.78 | 0.35 (0.28–0.45) | <0.001 |
| ≥2 | Reference | 0.57 (0.54–0.61) | <0.001 | 0.73 (0.64–0.84) | <0.001 | 0.38 (0.34–0.43) | <0.001 |
| Variables | No. non-CRC (%) | No. CRC (%) | Person-Years | IR# | Crude HR (95% CI) | p value | Adjusted HR (95% CI) † | p value |
|---|---|---|---|---|---|---|---|---|
| Colon Cancer (ICD-9-CM code: 153.x) Aspirin or Clopidogrel Use | ||||||||
| Nonusers | 277,711 (98.5) | 4129 (1.5) | 1,635,323 | 2.52 | Reference | Reference | ||
| Users | 279,244 (99.1) | 2596 (0.9) | 1,774,199 | 1.46 | 0.57 (0.55–0.60) | <0.001 | 0.56 (0.53–0.59) | <0.001 |
| Aspirin or Clopidogrel Use | ||||||||
| Nonusers | 277711 (98.5) | 4129 (1.5) | 1635323 | 2.52 | Reference | Reference | ||
| Aspirin Monotherapy | 216844 (99.1) | 2059 (0.9) | 1393473 | 1.48 | 0.58 (0.55–0.61) | <0.001 | 0.59 (0.56–0.63) | <0.001 |
| Clopidogrel Monotherapy | 19972 (99.1) | 186 (0.9) | 78279.76 | 2.38 | 1.00 (0.86–1.16) | 0.98 | 0.73 (0.63–0.85) | <0.001 |
| Dual Antiplatelet Therapy | 42428 (99.2) | 351 (0.8) | 302446 | 1.16 | 0.45 (0.40–0.50) | <0.001 | 0.38 (0.34–0.43) | <0.001 |
| Rectal Cancer (ICD-9-CM code: 154.x) Aspirin or Clopidogrel Use | ||||||||
| Nonusers | 280166 (99.4) | 1674 (0.6) | 1635323 | 1.02 | Reference | Reference | ||
| Users | 280829 (99.6) | 1011 (0.4) | 1774199 | 0.57 | 0.55 (0.51–0.60) | <0.001 | 0.54 (0.50–0.58) | <0.001 |
| Aspirin or Clopidogrel Use | ||||||||
| Nonusers | 280166 (99.4) | 1674 (0.6) | 1635323 | 1.02 | Reference | Reference | ||
| Aspirin Monotherapy | 218100 (99.6) | 803 (0.4) | 1393473 | 0.58 | 0.56 (0.51–0.61) | <0.001 | 0.57 (0.52–0.62) | <0.001 |
| Clopidogrel Monotherapy | 20072 (99.6) | 86 (0.4) | 78279.76 | 1.10 | 1.11 (0.90–1.39) | 0.326 | 0.86 (0.69–1.07) | 0.167 |
| Dual Antiplatelet Therapy | 42657 (99.7) | 122 (0.3) | 302446 | 0.40 | 0.39 (0.32–0.47) | <0.001 | 0.33 (0.27–0.40) | <0.001 |
| Variables | Crude SHR (95% CI) | p value | Adjusted SHR (95% CI) † | p value |
|---|---|---|---|---|
| Aspirin or Clopidogrel Use | ||||
| Nonusers | Reference | Reference | ||
| Users | 0.59 (0.56–0.61) | <0.001 | 0.58 (0.56–0.61) | <0.001 |
| Aspirin or Clopidogrel Use | ||||
| Nonusers | Reference | Reference | ||
| Aspirin Monotherapy | 0.60 (0.57–0.63) | <0.001 | 0.62 (0.59–0.65) | <0.001 |
| Clopidogrel Monotherapy | 0.87 (0.77–0.98) | 0.020 | 0.70 (0.62–0.79) | <0.001 |
| Dual Antiplatelet Therapy | 0.45 (0.41–0.49) | <0.001 | 0.40 (0.36–0.44) | <0.001 |
| Dose of Aspirin Used | ||||
| <28 cDDDs | Reference | Reference | ||
| 28–179 cDDDs | 0.74 (0.71–0.78) | <0.001 | 0.75 (0.72–0.79) | <0.001 |
| 180–359 cDDDs | 0.33 (0.31–0.36) | <0.001 | 0.34 (0.31–0.37) | <0.001 |
| ≥360 cDDDs | 0.10 (0.07–0.14) | <0.001 | 0.10 (0.07–0.14) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
| Dose of Clopidogrel Used | ||||
| <28 cDDDs | Reference | Reference | ||
| 28–179 cDDDs | 0.70 (0.63–0.79) | <0.001 | 0.61 (0.54–0.69) | <0.001 |
| 180–359 cDDDs | 0.66 (0.56–0.78) | <0.001 | 0.59 (0.50–0.69) | <0.001 |
| ≥360 cDDDs | 0.63 (0.56–0.71) | <0.001 | 0.53 (0.47–0.59) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
| Dose of Dual Antiplatelet Used | ||||
| <28 cDDDs | Reference | Reference | ||
| 28–179 cDDDs | 0.90 (0.74–1.09) | 0.272 | 0.79 (0.65–0.97) | 0.023 |
| 180–359 cDDDs | 0.52 (0.44–0.62) | <0.001 | 0.47 (0.40–0.56) | <0.001 |
| ≥360 cDDDs | 0.35 (0.31–0.40) | <0.001 | 0.31 (0.27–0.36) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
| Duration of Aspirin Use, Years | ||||
| <1 | ||||
| 1–2 | 0.89 (0.83–0.95) | <0.001 | 0.90 (0.85–0.97) | 0.0034 |
| 2–3 | 0.73 (0.68–0.80) | <0.001 | 0.74 (0.68–0.80) | <0.001 |
| ≥3 | 0.41 (0.39–0.44) | <0.001 | 0.42 (0.39–0.44) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
| Duration of Clopidogrel Use, Years | ||||
| <1 | ||||
| 1–2 | 0.75 (0.64–0.88) | <0.001 | 0.66 (0.56–0.77) | <0.001 |
| 2–3 | 0.77 (0.62–0.97) | 0.0292 | 0.66 (0.52–0.83) | <0.001 |
| ≥3 | 0.41 (0.33–0.51) | <0.001 | 0.34 (0.27–0.43) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
| Duration of Dual Antiplatelet Use, Years | ||||
| <1 | ||||
| 1–2 | 0.94 (0.88–1.00) | 0.0635 | 0.95 (0.88–1.01) | 0.1008 |
| 2–3 | 0.77 (0.71–0.84) | <0.001 | 0.77 (0.71–0.83) | <0.001 |
| ≥3 | 0.42 (0.40–0.44) | <0.001 | 0.41 (0.39–0.44) | <0.001 |
| p for trend | <0.001 | <0.001 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuan, Y.-C.; Huang, K.-W.; Lin, C.-L.; Luo, J.-C.; Kao, C.-H. Effects of Aspirin or Clopidogrel on Colorectal Cancer Chemoprevention in Patients with Type 2 Diabetes Mellitus. Cancers 2019, 11, 1468. https://doi.org/10.3390/cancers11101468
Kuan Y-C, Huang K-W, Lin C-L, Luo J-C, Kao C-H. Effects of Aspirin or Clopidogrel on Colorectal Cancer Chemoprevention in Patients with Type 2 Diabetes Mellitus. Cancers. 2019; 11(10):1468. https://doi.org/10.3390/cancers11101468
Chicago/Turabian StyleKuan, Yi-Chun, Kuang-Wei Huang, Cheng-Li Lin, Jiing-Chyuan Luo, and Chia-Hung Kao. 2019. "Effects of Aspirin or Clopidogrel on Colorectal Cancer Chemoprevention in Patients with Type 2 Diabetes Mellitus" Cancers 11, no. 10: 1468. https://doi.org/10.3390/cancers11101468
APA StyleKuan, Y.-C., Huang, K.-W., Lin, C.-L., Luo, J.-C., & Kao, C.-H. (2019). Effects of Aspirin or Clopidogrel on Colorectal Cancer Chemoprevention in Patients with Type 2 Diabetes Mellitus. Cancers, 11(10), 1468. https://doi.org/10.3390/cancers11101468





