Innovative Diagnostic Methods for Early Prostate Cancer Detection through Urine Analysis: A Review
Abstract
1. Introduction
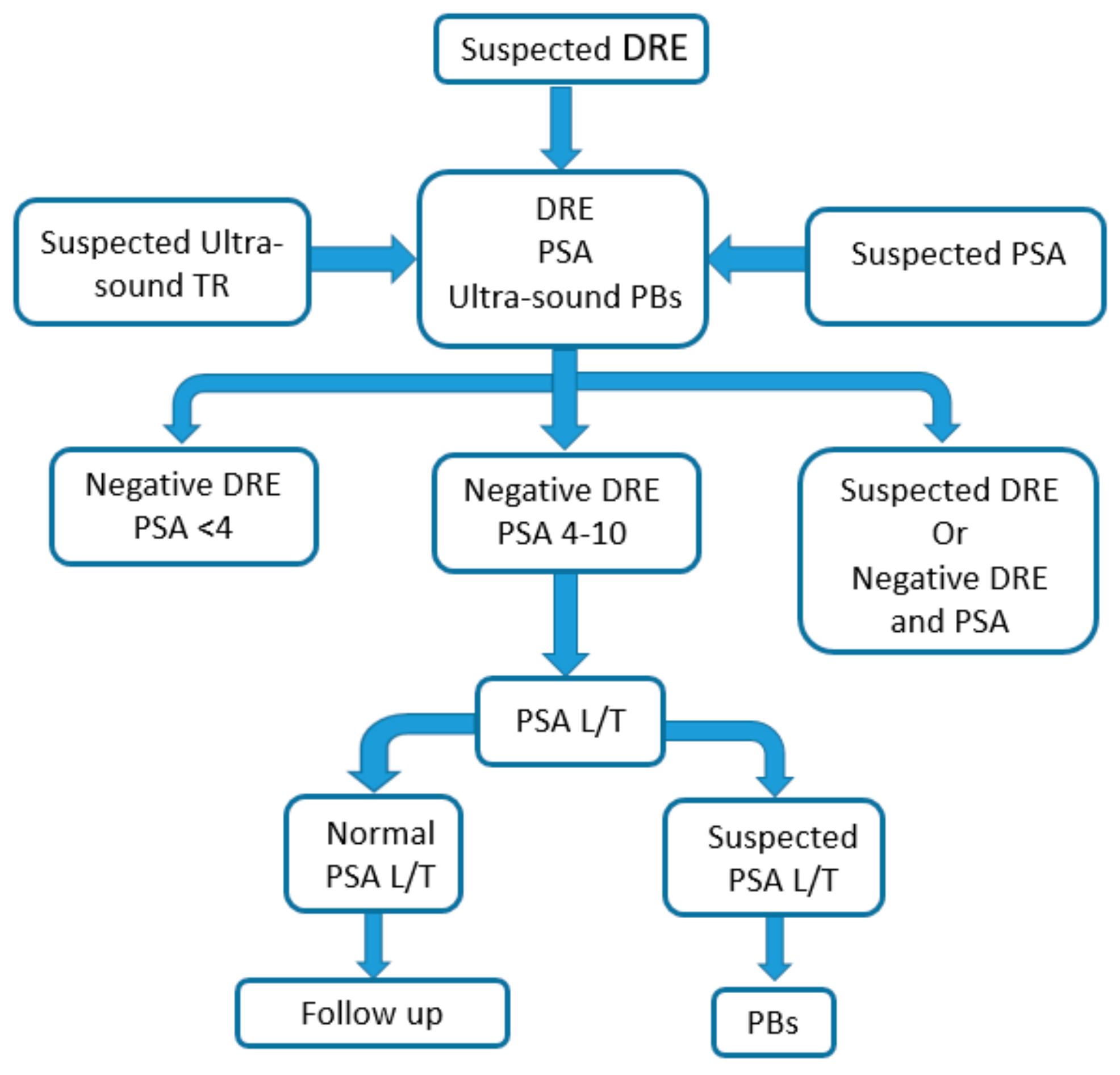
2. Overview of Traditional Diagnostic Methods
3. Innovative Techniques
- sensorial analysis, which relies on the mammalian sense of smell;
- senso-instrumental analysis, which tries to gather information about the olfactory properties of the analysed sample (urine) by means of specific instruments (i.e., electronic noses);
- chemical analysis, which relies on analytical techniques for the identification and quantification of chemical compounds (e.g., GC-MS).
3.1. Olfactory Fingerprint Investigation
3.1.1. Trained Dogs
3.1.2. Electronic Nose
3.2. Chemical Analysis
4. Discussion and Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| 10FoldCV | repeated 10-fold cross validation |
| ACN | acetonitrile |
| AUC | accuracy |
| BC | bladder cancer |
| BHP | benign prostate hypertrophy |
| CI | confidence interval |
| DDLLME | dispersive derivatisation liquid–liquid microextraction |
| DMF | dimethylformamide |
| DoubleCV | double cross validation |
| DRE | digital rectal examination |
| EN | electronic nose |
| ESI | electrospray ionisation |
| GC-MS | gas chromatography-mass spectrometry |
| GS | Gleason score |
| LC-MS | liquid chromatography-mass spectrometry |
| LDA | linear discriminant analysis |
| LOOCV | leave one out cross validation |
| MAD | microwave assisted derivatisation |
| MOS | metal oxide semiconductors |
| PBs | transrectal ultrasound-guided prostate biopsy |
| PCa | prostate cancer |
| PCA | principal component analysis |
| PLS-DA | partial least squares discriminant analysis |
| PSA | prostate specific antigen |
| Put | putrescine |
| RF | random forest |
| ROC | receiver operating characteristics |
| Spd | spermidine |
| Spm | spermine |
| SPME | solid phase microextraction |
| SVM | support vector machine |
| SVM-P | Support vector machine-polynomial |
| UPLC | ultra-high performance liquid chromatography |
| VOCs | volatile organic compounds |
References
- Society, A.C. 4 Essential Cancer Charts for 2016. Available online: https://www.cancer.org/latest-news/4-essential-cancer-charts-for-2016.html (accessed on 20 April 2017).
- National Cancer Institute—Surveillance, Epidemiology and End Result Program. Cancer Stat Facts: Prostate Cancer. Available online: https://seer.cancer.gov/statfacts/html/prost.html (accessed on 31 October 2017).
- Stenman, U.-H.; Leinonen, J.; Zhang, W.-M.; Finne, P. Prostate-specific antigen. Semin. Cancer Biol. 1999, 9, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Institute, N.C. About Cancer. Available online: https://www.cancer.gov/about-cancer/understanding/what-is-cancer (accessed on 6 March 2017).
- Schröder, F.H. PSA screening—A review of recent studies. Eur. J. Cancer 2009, 45, 402–404. [Google Scholar] [CrossRef]
- Velonas, V.M.; Woo, H.H.; dos Remedios, C.G.; Assinder, S.J. Current status of biomarkers for prostate cancer. Int. J. Mol. Sci. 2013, 14, 11034–11060. [Google Scholar] [CrossRef] [PubMed]
- Lima, A.R.; Bastos, M.D.L.; Carvalho, M.; Guedes de Pinho, P. Biomarker discovery in human prostate cancer: An update in metabolomics studies. Transl. Oncol. 2016, 9, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Nam, R.K.; Saskin, R.; Lee, Y.; Liu, Y.; Law, C.; Klotz, L.H.; Loblaw, D.A.; Trachtenberg, J.; Stanimirovic, A.; Simor, A.E.; et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J. Urol. 2010, 183, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, R.M.; Gilliland, F.D.; Adams-Cameron, M.; Hunt, W.C.; Key, C.R. Prostate-specific antigen testing accuracy in community practice. BMC Fam. Pract. 2002, 3, 19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fireman, B.H.; Quesenberry, C.P.; Somkin, C.P.; Jacobson, A.S.; Baer, D.; West, D.; Potosky, A.L.; Brown, M.L. Cost of care for cancer in a health maintenance organization. Health Care Financ. Rev. 1997, 18, 51–76. [Google Scholar] [PubMed]
- Diamandis, M.; White, N.M.; Yousef, G.M. Personalized medicine: Marking a new epoch in cancer patient management. Mol. Cancer Res. MCR 2010, 8, 1175–1187. [Google Scholar] [CrossRef] [PubMed]
- Olsen, O.; Gotzsche, P.C. Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 2001, CD001877. [Google Scholar] [CrossRef]
- Nyström, L.; Andersson, I.; Bjurstam, N.; Frisell, J.; Nordenskjöld, B.; Rutqvist, L.E. Long-term effects of mammography screening: Updated overview of the Swedish randomised trials. Lancet 2002, 359, 909–919. [Google Scholar] [CrossRef]
- Esserman, L.J.; Thompson, I.M., Jr.; Reid, B. Overdiagnosis and overtreatment in cancer: An opportunity for improvement. JAMA 2013, 310, 797–798. [Google Scholar] [CrossRef] [PubMed]
- Bjartell, A.S. Dogs sniffing urine: A future diagnostic tool or a way to identify new prostate cancer markers? Eur. Urol. 2011, 59, 202–203. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.T.; Schatz, C.B.; Myers, L.J.; Kosty, M.; Gonczy, C.; Kroener, J.; Tran, M.; Kurtzhals, P.; Heath, S.; Koziol, J.A.; et al. The use of canines in the detection of human cancers. J. Altern. Complement. Med. 2008, 14, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Cornu, J.N.; Cancel-Tassin, G.; Ondet, V.; Girardet, C.; Cussenot, O. Olfactory detection of prostate cancer by dogs sniffing urine: A step forward in early diagnosis. Eur. Urol. 2010, 59, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Elliker, K.R.; Sommerville, B.A.; Broom, D.M.; Neal, D.E.; Armstrong, S.; Williams, H.C. Key considerations for the experimental training and evaluation of cancer odour detection dogs: Lessons learnt from a double-blind, controlled trial of prostate cancer detection. BMC Urol. 2014, 14, 22. [Google Scholar] [CrossRef] [PubMed]
- Taverna, G.; Tidu, L.; Grizzi, F.; Torri, V.; Mandressi, A.; Sardella, P.; La Torre, G.; Cocciolone, G.; Seveso, M.; Giusti, G.; et al. Olfactory system of highly trained dogs detects prostate cancer in urine samples. J. Urol. 2015, 193, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Bernabei, M.; Pennazza, G.; Santonico, M.; Corsi, C.; Roscioni, C.; Paolesse, R.; Di Natale, C.; D’Amico, A. A preliminary study on the possibility to diagnose urinary tract cancers by an electronic nose. Sens. Actuators B Chem. 2008, 131, 1–4. [Google Scholar] [CrossRef]
- D’Amico, A.; Santonico, M.; Pennazza, G.; Capuano, R.; Vespasiani, G.; Del Fabbro, D.; Paolesse, R.; Di Natale, C.; Martinelli, E.; Agrò, E.F. A novel approach for prostate cancer diagnosis using a gas sensor array. Procedia Eng. 2012, 47, 1113–1116. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Del Fabbro, D.; Miano, R.; Santonico, M.; Capuano, R.; Pennazza, G.; D’Amico, A.; Finazzi-Agro, E. Prostate cancer diagnosis through electronic nose in the urine headspace setting: A pilot study. Prostate Cancer Prostatic Dis. 2014, 17, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Santonico, M.; Pennazza, G.; Asimakopoulos, A.D.; Del Fabbro, D.; Miano, R.; Capuano, R.; Finazzi-Agrò, E.; D’Amico, A. Chemical sensors for prostate cancer detection oriented to non-invasive approach. Procedia Eng. 2014, 87, 320–323. [Google Scholar] [CrossRef]
- Roine, A.; Veskimae, E.; Tuokko, A.; Kumpulainen, P.; Koskimaki, J.; Keinanen, T.A.; Hakkinen, M.R.; Vepsalainen, J.; Paavonen, T.; Lekkala, J.; et al. Detection of prostate cancer by an electronic nose: A proof of principle study. J. Urol. 2014, 192, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Sreekumar, A.; Poisson, L.M.; Rajendiran, T.M.; Khan, A.P.; Cao, Q.; Yu, J. Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature 2009, 457, 910–914. [Google Scholar] [CrossRef] [PubMed]
- Jentzmik, F.; Stephan, C.; Miller, K.; Schrader, M.; Erbersdobler, A.; Kristiansen, G. Sarcosine in urine after digital rectal examination fails as a marker in prostate cancer detection and identification of aggressive tumours. Eur. Urol. 2010, 58, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Cheng, X.; Wang, C.; Ma, Y. Quantitative determination of sarcosine and related compounds in urinary samples by liquid chromatography with tandem mass spectrometry. Anal. Chem. 2010, 82, 9022–9027. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Liu, T.; Ma, C.; Xue, R.; Deng, C.; Zeng, H. GC/Ms-based metabolomic approach to validate the role of urinary sarcosine and target biomarkers for human prostate cancer by microwave-assisted derivatization. Anal. Bioanal. Chem. 2011, 401, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Stabler, S.; Koyama, T.; Zhao, Z.; Martinez-Ferrer, M.; Allen, R.H.; Luka, Z.; Loukachevitch, L.V.; Clark, P.E.; Wagner, C.; Bhowmick, N.A. Serum methionine metabolites are risk factors for metastatic prostate cancer progression. PLoS ONE 2011, 6, e22486. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.; Dugheri, S.; Musci, M.; Bonacchi, A.; Salvadori, E.; Arcangeli, G.; Cupelli, V.; Lanciotti, M.; Masieri, L.; Serni, S.; et al. Fully automated solid-phase microextraction-fast gas chromatography-mass spectrometry method using a new ionic liquid column for high-throughput analysis of sarcosine and N-ethylglycine in human urine and urinary sediments. Anal. Chim. Acta 2011, 707, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Shamsipur, M.; Naseri, M.T.; Babri, M. Quantification of candidate prostate cancer metabolite biomarkers in urine using dispersive derivatization liquid-liquid microextraction followed by gas and liquid chromatography-mass spectrometry. J. Pharm. Biomed. Anal. 2013, 81–82, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Struck-Lewicka, W.; Kordalewska, M.; Bujak, R.; Yumba Mpanga, A.; Markuszewski, M.; Jacyna, J.; Matuszewski, M.; Kaliszan, R.; Markuszewski, M.J. Urine metabolic fingerprinting using LC-MS and GC-MS reveals metabolite changes in prostate cancer: A pilot study. J. Pharm. Biomed. Anal. 2015, 111, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Heger, Z.; Cernei, N.; Gumulec, J.; Masarik, M.; Eckschlager, T.; Hrabec, R.; Kizek, R. Determination of common urine substances as an assay for improving prostate carcinoma diagnostics. Oncol. Rep. 2014, 31, 1846–1854. [Google Scholar] [CrossRef] [PubMed]
- Khalid, T.; Aggio, R.; White, P.; De Lacy Costello, B.; Persad, R.; Al-Kateb, H.; Jones, P.; Probert, C.S.; Ratcliffe, N. Urinary volatile organic compounds for the detection of prostate cancer. PLoS ONE 2015, 10, e0143283. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, T.-H.; Chan, C.-F.; Chan, W.-L.; Chiu, K.-F.; Wong, W.-T.; Ng, C.-F.; Wong, K.-L. Urinary polyamines: A pilot study on their roles as prostate cancer detection biomarkers. PLoS ONE 2016, 11, e0162217. [Google Scholar] [CrossRef] [PubMed]
- Sroka, W.D.; Boughton, B.A.; Reddy, P.; Roessner, U.; Slupski, P.; Jarzemski, P.; Dabrowska, A.; Markuszewski, M.J.; Marszall, M.P. Determination of amino acids in urine of patients with prostate cancer and benign prostate growth. Eur. J. Cancer Prev. 2017, 26, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Peralbo, M.A.; Gómez-Gómez, E.; Calderón-Santiago, M.; Carrasco-Valiente, J.; Ruiz-García, J.; Requena-Tapia, M.J.; Luque de Castro, M.D.; Priego-Capote, F. Prostate cancer patients–negative biopsy controls discrimination by untargeted metabolomics analysis of urine by LC-QTOF: Upstream information on other omics. Sci. Rep. 2016, 6, 38243. [Google Scholar] [CrossRef] [PubMed]
- Gkotsos, G.; Virgiliou, C.; Lagoudaki, I.; Sardeli, C.; Raikos, N.; Theodoridis, G.; Dimitriadis, G. The role of sarcosine, uracil, and kynurenic acid metabolism in urine for diagnosis and progression monitoring of prostate cancer. Metabolites 2017, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Dereziński, P.; Klupczynska, A.; Sawicki, W.; Pałka, J.A.; Kokot, Z.J. Amino acid profiles of serum and urine in search for prostate cancer biomarkers: A pilot study. Int. J. Med. Sci. 2017, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Aggio, R.B.; de Lacy Costello, B.; White, P.; Khalid, T.; Ratcliffe, N.M.; Persad, R.; Probert, C.S. The use of a gas chromatography-sensor system combined with advanced statistical methods, towards the diagnosis of urological malignancies. J. Breath Res. 2016, 10, 017106. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.C.; Yates, J.R., III. The application of mass spectrometry to membrane proteomics. Nat. Biotechnol. 2003, 21, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Capelli, L.; Taverna, G.; Bellini, A.; Eusebio, L.; Buffi, N.; Lazzeri, M.; Guazzoni, G.; Bozzini, G.; Seveso, M.; Mandressi, A.; et al. Application and uses of electronic noses for clinical diagnosis on urine samples: A review. Sensors 2016, 16, 1708. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, J.J.; London, A.N.; Luo, J.; Kharasch, E.D. Urinary biomarkers for the early diagnosis of kidney cancer. Mayo Clin. Proc. 2010, 85, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Xylinas, E.; Kluth, L.A.; Rieken, M.; Karakiewicz, P.I.; Lotan, Y.; Shariat, S.F. Urine markers for detection and surveillance of bladder cancer. Urol. Oncol. 2014, 32, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Anton Amann, D.S. Volatile Biomarkers: Non-Invasive Diagnosis in Physiology and Medicine; Elsevier: New York, NY, USA, 2013. [Google Scholar]
- Smith, S.; Burden, H.; Persad, R.; Whittington, K.; Costello, B.D.L.; Ratcliffe, N.M.; Probert, C.S. A comparative study of the analysis of human urine headspace using gas chromatography–Mass spectrometry. J. Breath Res. 2008, 2, 037022. [Google Scholar] [CrossRef] [PubMed]
- Mills, G.A.; Walker, V. Headspace solid-phase microextraction profiling of volatile compounds in urine: Application to metabolic investigations. J. Chromatogr. B 2001, 753, 259–268. [Google Scholar] [CrossRef]
- De Lacy Costello, B.M.; Ratcliffe, N. Volatile Organic Compounds (VOCS) Found in Urine and Stool; Elsevier: New York, NY, USA, 2013; pp. 405–462. [Google Scholar]
- Rigau, M.; Olivan, M.; Garcia, M.; Sequeiros, T.; Montes, M.; Colás, E.; Llauradó, M.; Planas, J.; de Torres, I.; Morote, J.; et al. The present and future of prostate cancer urine biomarkers. Int. J. Mol. Sci. 2013, 14, 12620–12649. [Google Scholar] [CrossRef] [PubMed]
- Zlatkis, A.; Bertsch, W.; Lichtenstein, H.A.; Tishbee, A.; Shunbo, F.; Liebich, H.M.; Coscia, A.M.; Fleischer, N. Profile of volatile metabolites in urine by gas chromatography-mass spectrometry. Anal. Chem. 1973, 45, 763–767. [Google Scholar] [CrossRef] [PubMed]
- Liebich, H.M. Specific detection of volatile metabolites in urines of normal subjects and patients with diabetes mellitus using computerized mass fragmentography. J. Chromatogr. 1975, 112, 551–557. [Google Scholar] [CrossRef]
- Kwak, J.; Grigsby, C.C.; Smith, B.R.; Rizki, M.M.; Preti, G. Changes in volatile compounds of human urine as it ages: Their interaction with water. J. Chromatogr. B 2013, 941, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Samudrala, D.; Geurts, B.; Brown, P.A.; Szymańska, E.; Mandon, J.; Jansen, J.; Buydens, L.; Harren, F.J.M.; Cristescu, S.M. Changes in urine headspace composition as an effect of strenuous walking. Metabolomics 2015, 11, 1656–1666. [Google Scholar] [CrossRef] [PubMed]
- Trock, B.J. Application of metabolomics to prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2011, 29, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Jordan, K.W.; Cheng, L.L. NMR-based metabolomics approach to target biomarkers for human prostate cancer. Expert Rev. Proteom. 2007, 4, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Dwivedi, D.K.; Jagannathan, N.R. High-resolution nmr spectroscopy of human body fluids and tissues in relation to prostate cancer. NMR Biomed. 2014, 27, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.S.; Heiden, M.V.; Giovannucci, E.L.; Mucci, L.A. Metabolomic biomarkers of prostate cancer: Prediction, diagnosis, progression, prognosis and recurrence. Cancer Epidemiol. Biomark. Prev. 2016, 25, 887–906. [Google Scholar] [CrossRef] [PubMed]
- Ohori, M.; Wheeler, T.M.; Dunn, J.K.; Stamey, T.A.; Scardino, P.T. The pathological features and prognosis of prostate cancer detectable with current diagnostic tests. J. Urol. 1994, 152, 1714–1720. [Google Scholar] [CrossRef]
- Eichler, K.; Hempel, S.; Wilby, J.; Myers, L.; Bachmann, L.M.; Kleijnen, J. Diagnostic value of systematic biopsy methods in the investigation of prostate cancer: A systematic review. J. Urol. 2006, 175, 1605–1612. [Google Scholar] [CrossRef]
- Cooner, W.H.; Mosley, B.R.; Rutherford, C.L.; Beard, J.H.; Pond, H.S.; Terry, W.J.; Igel, T.C.; Kidd, D.D. Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J. Urol. 1990, 143, 1146–1152. [Google Scholar] [CrossRef]
- Hoffman, R.M. Screening for prostate cancer. N. Engl. J. Med. 2011, 365, 2013–2019. [Google Scholar] [CrossRef] [PubMed]
- Schröder, F.H.; Kruger, A.B.; Rietbergen, J.; Kranse, R.; Maas, P.V.D.; Beemsterboer, P.; Hoedemaeker, R. Evaluation of the digital rectal examination as a screening test for prostate cancer. JNCI J. Natl. Cancer Inst. 1998, 90, 1817–1823. [Google Scholar] [CrossRef] [PubMed]
- Oesterling, J.E. Prostate specific antigen: A critical assessment of the most useful tumor marker for adenocarcinoma of the prostate. J. Urol. 1991, 145, 907–923. [Google Scholar] [CrossRef]
- Carter, H.B.; Pearson, J.D.; Metter, E.J.; Brant, L.J.; Chan, D.W.; Andres, R.; Fozard, J.L.; Walsh, P.C. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. JAMA 1992, 267, 2215–2220. [Google Scholar] [CrossRef] [PubMed]
- Schmid, H.P.; McNeal, J.E.; Stamey, T.A. Observations on the doubling time of prostate cancer. The use of serial prostate-specific antigen in patients with untreated disease as a measure of increasing cancer volume. Cancer 1993, 71, 2031–2040. [Google Scholar] [CrossRef]
- Sangar, V.K.; Ragavan, N.; Matanhelia, S.S.; Watson, M.W.; Blades, R.A. The economic consequences of prostate and bladder cancer in the UK. BJU Int. 2005, 95, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Skolarus, T.A.; Miller, D.C.; Wei, J.T.; Hollenbeck, B.K. Understanding prostate cancer spending growth among medicare beneficiaries. Urology 2011, 77, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Wilt, T.J.; Brawer, M.K.; Jones, K.M.; Barry, M.J.; Aronson, W.J.; Fox, S.; Gingrich, J.R.; Wei, J.T.; Gilhooly, P.; Grob, B.M.; et al. Radical prostatectomy versus observation for localized prostate cancer. N. Engl. J. Med. 2012, 367, 203–213. [Google Scholar] [CrossRef] [PubMed]
- You, J.; Cozzi, P.; Walsh, B.; Willcox, M.; Kearsley, J.; Russell, P.; Li, Y. Innovative biomarkers for prostate cancer early diagnosis and progression. Crit. Rev. Oncol. Hematol. 2010, 73, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Adhyam, M.; Gupta, A.K. A review on the clinical utility of PSA in cancer prostate. Indian J. Surg. Oncol. 2012, 3, 120–129. [Google Scholar] [CrossRef] [PubMed]
- McJimpsey, E.L. Molecular form differences between prostate-specific antigen (PSA) standards create quantitative discordances in PSA elisa measurements. Sci. Rep. 2016, 6, 22050. [Google Scholar] [CrossRef] [PubMed]
- Jansen, F.H.; van Schaik, R.H.N.; Kurstjens, J.; Horninger, W.; Klocker, H.; Bektic, J.; Wildhagen, M.F.; Roobol, M.J.; Bangma, C.H.; Bartsch, G. Prostate-specific antigen (PSA) isoform p2PSA in combination with total PSA and free PSA improves diagnostic accuracy in prostate cancer detection. Eur. Urol. 2010, 57, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Faria, E.F.; Carvalhal, G.F.; dos Reis, R.B.; Tobias-Machado, M.; Vieira, R.A.; Reis, L.O.; Nogueira, L.; Machado, R.D.; Freitas, C.H., Jr.; Magnabosco, W.J.; et al. Use of low free to total PSA ratio in prostate cancer screening: Detection rates, clinical and pathological findings in brazilian men with serum PSA levels <4.0 ng/mL. BJU Int. 2012, 110, E653–E657. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, Z.Z.; Huang, Y.L.; Song, H.J.; Wang, Y.J. Value of free/total prostate-specific antigen (F/T PSA) ratios for prostate cancer detection in patients with total serum prostate-specific antigen between 4 and 10 ng/mL: A meta-analysis. Medicine 2018, 97, e0249. [Google Scholar] [CrossRef] [PubMed]
- Digital Rectal Examination. 2017. Available online: https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/tests-and-procedures/digital-rectal-exam-dre2017 (accessed on 14 February 2018).
- Helfand, B.T.; Glaser, A.P.; Rimar, K.; Zargaroff, S.; Hedges, J.; McGuire, B.B.; Catalona, W.J.; McVary, K.T. Prostate cancer diagnosis is associated with an increased risk of erectile dysfunction after prostate biopsy. BJU Int. 2013, 111, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Loeb, S.; van den Heuvel, S.; Zhu, X.; Bangma, C.H.; Schröder, F.H.; Roobol, M.J. Infectious complications and hospital admissions after prostate biopsy in a European randomized trial. Eur. Urol. 2012, 61, 1110–1114. [Google Scholar] [CrossRef] [PubMed]
- Carroll, P. Md Transrectal Ultrasound Guided Prostate Biopsy. 2017. Available online: http://urology2008-2012.ucsf.edu/patientguides/pdf/uroonc/prostate_biopsy.pdf (accessed on 14 February 2018).
- Djavan, B.; Ravery, V.; Zlotta, A.; Dobronski, P.; Dobrovits, M.; Fakhari, M.; Seitz, C.; Susani, M.; Borkowski, A.; Boccon-Gibod, L.; et al. Prospective evaluation of prostate cancer detected on biopsies 1, 2, 3 and 4: When should we stop? J. Urol. 2001, 166, 1679–1683. [Google Scholar] [CrossRef]
- Muller, S.; Lilleaasen, G.; Sand, T.E.; Lofsgaard, L.; Estop-Garanto, M.; Helgo, D.; Sund, P.; Mygland, V. Poor reproducibility of pirads score in two multiparametric mris before biopsy in men with elevated PSA. World J. Urol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Qiu, S.; Zhang, A.H. High-throughput metabolomics to identify metabolites to serve as diagnostic biomarkers of prostate cancer. Anal. Methods 2016, 8, 3284–3290. [Google Scholar] [CrossRef]
- Wilson, A.; Baietto, M. Applications and advances in electronic-nose technologies. Sensors 2009, 9, 5099–5148. [Google Scholar] [CrossRef] [PubMed]
- Gebicki, J. Application of electrochemical sensors and sensor matrixes for measurement of odorous chemical compounds. TrAC Trends Anal. Chem. 2016, 77, 1–13. [Google Scholar] [CrossRef]
- Munoz, R.; Sivret, E.C.; Parcsi, G.; Lebrero, R.; Wang, X.; Suffet, I.H.; Stuetz, R.M. Monitoring techniques for odour abatement assessment. Water Res. 2010, 44, 5129–5149. [Google Scholar] [CrossRef] [PubMed]
- Röck, F.; Barsan, N.; Weimar, U. Electronic nose: Current status and future trends. Chem. Rev. 2008, 108, 705–725. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.W.; Moore, D.R.; Marzouk, E.B.; Glenn, F.R.; Hallock, R.M. Canine olfaction and electronic nose detection of volatile organic compounds in the detection of cancer: A review. Cancer Investig. 2015, 33, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Ampuero, S.; Bosset, J.O. The electronic nose applied to dairy products: A review. Sens. Actuators B Chem. 2003, 94, 1–12. [Google Scholar] [CrossRef]
- Adamsen, F. Hippocratic Writings: Aphorism, 5th ed.; Atomics, W., Ed.; Elsevier: New York, NY, USA, 1994. [Google Scholar]
- Van de Goor, R.M.; Leunis, N.; van Hooren, M.R.; Francisca, E.; Masclee, A.; Kremer, B.; Kross, K.W. Feasibility of electronic nose technology for discriminating between head and neck, bladder, and colon carcinomas. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Peng, G.; Hakim, M.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Tisch, U.; Haick, H. Detection of lung, breast, colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. Br. J. Cancer 2010, 103, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Gazit, I.; Goldblatt, A.; Terkel, J. The role of context specificity in learning: The effects of training context on explosives detection in dogs. Anim. Cognit. 2005, 8, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Nolan, R.G.D. Mine Detecting K-9′s: Summary Report 1975–1976; US Army Techical Report; Army Mobility Equipment Research and Development Command: Fort Belvoir, VA, USA, 1977. [Google Scholar]
- Quignon, P.; Rimbault, M.; Robin, S.; Galibert, F. Genetics of canine olfaction and receptor diversity. Mamm. Genome 2012, 23, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Smith, T. Can Dogs Smell Cancers? Available online: http://companiontraining.com.com/can-dogs-smell-cancer (accessed on 18 January 2018).
- Fens, N.; van der Schee, M.P.; Brinkman, P.; Sterk, P.J. Exhaled breath analysis by electronic nose in airways disease. Established issues and key questions. Clin. Exp. Allergy 2013, 43, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Wojnowski, W.; Partyka, A.; Dymerski, T.; Gebicki, J.; Namiesnik, J. Electronic noses in medical diagnostics. Curr. Med. Chem. 2017. [Google Scholar] [CrossRef]
- Oh, E.H.; Song, H.S.; Park, T.H. Recent advances in electronic and bioelectronic noses and their biomedical applications. Enzyme Microb. Technol. 2011, 48, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Dragonieri, S.; Schot, R.; Mertens, B.J.; Le Cessie, S.; Gauw, S.A.; Spanevello, A.; Resta, O.; Willard, N.P.; Vink, T.J.; Rabe, K.F.; et al. An electronic nose in the discrimination of patients with asthma and controls. J. Allergy Clin. Immunol. 2007, 120, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, E.A.; Bai, J.; Plotto, A.; Dea, S. Electronic noses and tongues: Applications for the food and pharmaceutical industries. Sensors 2011, 11, 4744–4766. [Google Scholar] [CrossRef] [PubMed]
- Peris, M.; Escuder-Gilabert, L. A 21st century technique for food control: Electronic noses. Anal. Chim. Acta 2009, 638, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Capelli, L.; Sironi, S.; Del Rosso, R. Electronic noses for environmental monitoring applications. Sensors 2014, 14, 19979–20007. [Google Scholar] [CrossRef] [PubMed]
- Selena Sironi, L.E.; Capelli, L.; Remondini, M.; del Rosso, R. Use of an electronic nose for indoor air quality monitoring. Chem. Eng. Trans. 2014, 40. [Google Scholar] [CrossRef]
- Pavlou, A.; Turner, A.P.F.; Magan, N. Recognition of anaerobic bacterial isolates in vitro using electronic nose technology. Lett. Appl. Microbiol. 2002, 35, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Yates, J.W.T.; Chappell, M.J.; Gardner, J.W.; Dow, C.S.; Dowson, C.; Hamood, A.; Bolt, F.; Beeby, L. Data reduction in headspace analysis of blood and urine samples for robust bacterial identification. Comput. Methods Programs Biomed. 2005, 79, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Pavlou, A.K.; Magan, N.; McNulty, C.; Jones, J.M.; Sharp, D.; Brown, J.; Turner, A.P.F. Use of an electronic nose system for diagnoses of urinary tract infections. Biosens. Bioelectron. 2002, 17, 893–899. [Google Scholar] [CrossRef]
- Kodogiannis, V.S.; Lygouras, J.N.; Tarczynski, A.; Chowdrey, H.S. Artificial odor discrimination system using electronic nose and neural networks for the identification of urinary tract infection. IEEE Trans. Inf. Technol. Biomed. 2008, 12, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Roine, A.; Saviauk, T.; Kumpulainen, P.; Karjalainen, M.; Tuokko, A.; Aittoniemi, J.; Vuento, R.; Lekkala, J.; Lehtimäki, T.; Tammela, T.L.; et al. Rapid and accurate detection of urinary pathogens by mobile IMS-based electronic nose: A proof-of-principle study. PLoS ONE 2014, 9, e114279. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Tan, Y.; Xie, H.; Shen, F. A novel method for diabetes diagnosis based on electronic nose. Biosens. Bioelectron. 1997, 12, 1031–1036. [Google Scholar] [PubMed]
- Corrado Di Natale, A.M.; Macagnano, A.; Antuzzi, D.; Paolesse, R.; D’Amico, A. Electronic nose analysis of urine samples containing blood. Physiol. Meas. 1999, 20, 377. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Guo, H.-R.; Chang, Y.-H.; Kao, M.-T.; Wang, H.-H.; Hong, R.-I. Application of the electronic nose for uremia diagnosis. Sens. Actuators B Chem. 2001, 76, 177–180. [Google Scholar] [CrossRef]
- Arasaradnam, R.P.; Ouaret, N.; Thomas, M.G.; Gold, P.; Quraishi, M.N.; Nwokolo, C.U.; Bardhan, K.D.; Covington, J.A. Evaluation of gut bacterial populations using an electronic e-nose and field asymmetric ion mobility spectrometry: Further insights into ‘fermentonomics’. J. Med. Eng. Technol. 2012, 36, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Covington, J.; Westenbrink, E.; Ouaret, N.; Harbord, R.; Bailey, C.; Connell, N.; Cullis, J.; Williams, N.; Nwokolo, C.; Bardhan, K.D.; et al. Application of a novel tool for diagnosing bile acid diarrhoea. Sensors 2013, 13, 11899–11912. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.; Pennazza, G.; Santonico, M.; Martinelli, E.; Roscioni, C.; Galluccio, G.; Paolesse, R.; Di Natale, C. An investigation on electronic nose diagnosis of lung cancer. Lung Cancer 2010, 68, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Ali, S.; Philip, P.; Sarkar, F. Clinical advances in molecular biomarkers for cancer diagnosis and therapy. Int. J. Mol. Sci. 2013, 14, 14771. [Google Scholar] [CrossRef] [PubMed]
- Institute, National Cancer. Biomarker Definition. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=45618 (accessed on 6 March 2017).
- Di Carlo, S.F.M. Drift correction methods for gas chemical sensors in artificial olfaction systems: Techniques and challenges. In Advances in Chemical Sensors/Wang; Intech: Rijeka, Croatia, 2012; pp. 305–326. [Google Scholar]
- Brereton, G.R. Applied Chemometrics for Scientists; Wiley: Hoboken, NJ, USA, 2007. [Google Scholar]
- Boeker, P. On ‘electronic nose’ methodology. Sens. Actuators B Chem. 2014, 204, 2–17. [Google Scholar] [CrossRef]
| Reference | Authors | Population Involved Controls/Sick | Trained Dogs | Samples Collection and Treatments | Training Method | Results | |
|---|---|---|---|---|---|---|---|
| [16] | Gordon et al. (2008) | 186 | 57 PCa | 4 | Storage temperature: −20 °C; Sample preparation: thawed, placed in a screw-top vial; Sample somministration: screw-top vials were put into mason jars | Training site: trainer’s home Trainer: Owner Duration: 12–14 months Frequency: 2–7 d/w | Specificity: 1: 36%; 2: 36%; 3: 63%; 4: 81% Sensitivity: 1: <10%; 2: <20%; 3: 20%; 4: 25% |
| [17] | Cornu et al. (2010) | training phase: 16; double blind phase: 33 | training phase: 26; double blind phase: 33 | 1 | Storage temperature: −4 °C; Sample preparation: slowly heating to 37 °C; Sample somministration: samples placed in perforated boxes | Trainer: Professional Duration: 16 months Frequency: 5 d/w | Specificity: 91%; Sensitivity: 91% |
| [18] | Elliker et al. (2014) | 67 | 50 PCa | 2 | Storage temperature: −20 °C; Sample preparation: defrosting in a 37 °C water bath; Sample somministration: samples were put in open top propylene test tubes | Stage 1: dogs had to find and indicate PCa urine samples; Stage 2: dogs had to discriminate PCa samples from controls; No information about duration and frequency of training | Specificity: 1: 71%; 2: 75%; Sensitivity: 1: 13%; 2: 25% |
| [19] | Taverna et al. (2015) | 540 | 362 PCa | 2 | Storage temperature: −20 °C; Sample preparation: defrosting to 37 °C; Sample somministration: samples were put into circular perforated metal containers placed in thermally sealed plastic containers | Training Site: central Trainer: professional No information about duration and frequency of training | Specificity: 1: 98.7%; 2: 97.6%; Sensitivity: 1: 100%; 2: 98.6% |
| Reference | Authors | Participants Controls/Sick | Samples Collection and Treatments | Instrument (Sensor Type) | Statistical Methods | Results | |
|---|---|---|---|---|---|---|---|
| [20] | Bernabei et al. (2007) | 29 BPH; 33 other urological pathologies; 18 controls | 25 BC 12 PCa | Urine collection: in the morning before any food intake; Storage temperature: no info; Headspace creation: urine was put at 25 °C for the necessary time to obtain a steady headspace, then 10 mL of headspace were injected into a 2 L sterile bag pre-filled with N2; EN analysis: no info | ENQBE (Conducting polymers) | PLS-DA; PCA; LOOCV | qualitative plot; discrimination between PCa and BC samples and controls 100%; differentiation between different classes, not complete discrimination |
| [21] | D’Amico et al. (2012) | 15 | 6 PCa | Urine collection: before PBs; Storage temperature: no info; Headspace creation: a dynamic headspace was obtained putting urine in sterile urine boxes with a dedicated top; EN analysis: no info | EN: University of Rome “Tor Vergata” (Conducting polymers) | PLS-DA | qualitative plot |
| [22] | Asimakopoulos et al. (2014) | 27 | 14 PCa | Urine collection: before PBs; Storage temperature: no info; Headspace creation: a dynamic headspace was obtained putting urine in sterile urine boxes with a dedicated top; EN analysis: no info | EN: University of Rome “Tor Vergata” (Conducting polymers) | PLS-DA; LOOCV | Sensitivity: 71.4%, specificity: 92.6% |
| [23] | Santonico et al. (2014) | 27 | 14 PCa | Urine collection: before PBs; Storage temperature: no info; Headspace creation: a dynamic headspace was obtained putting urine in sterile urine boxes with a dedicated top; EN analysis: 200 s for the measurement phase, 600 s for the cleaning phase | EN: University of Rome “Tor Vergata” (Conducting polymers) | PLS-DA; LOOCV | qualitative plot |
| [24] | Roine et al. (2014) | 24 (15 BPH and 9 post radical prostatectomy) | 50 PCa | Urine collection: in the morning; Storage temperature: −70 °C; Headspace creation: urine was defrosted and pipetted to a plate heated and maintained at 37 °C; EN analysis: 15 min for the measurement phase, 10 min for recovery | EN: ChemPRO 100-eNose (Electrode strips and MOS sensors) | LOOCV; LDA | LOOCV: sensitivity 78%, specificity 67%, accuracy 77% LDA: sensitivity 82%, specificity 88% |
| Reference | Authors | Population Controls/Sick | Sample Preparation Method | Analytical Method | Statistical Methods | Biomarkers | Results |
|---|---|---|---|---|---|---|---|
| [25] | Sreekumar et al. (2009) | 51/59 | Urine collection: After DRE for PCa patients; Storage and pre-treatments: Samples were stored at −80 °C until analysis; Sample preparation: Samples underwent organic and aqueous extractions. The extracted was equally divided into LC and GC fractions, which were dried on a TurboVapR. Prior to injection, all samples were resuspended in identical volume and injection standards were added. | LC-MS: The vacuum dried sample was re-solubilised in 100 µL of injection solvent. The system was operated using a gradient of acetonitrile. The columns were maintained in temperature-controlled chambers during use and were exchanged and washed after every 50 injections. GC-MS: The column used was 5% phenyl-methyl polysiloxane, the temperature from 40 °C to 300 °C in 16 min. ID GC-MS: For analysing sarcosine and alanine, residual water was removed by forming an azeotrope with 100 uL of DMF and drying the suspension under vacuum. An Agilent 6890N GC equipped with a 15 m DB-5capillary column interfaced with an Agilent 5975 MSD mass detector. | Wilcoxon rank-sum test; t-test; Kruskal–Wallis test; Pearson’s correlation; NOVA; Z-score plot; heat maps | Sarcosine; Uracil; Kynurenine; Glycerol-3-phosphate; Leucine; Proline | Sarcosine was significantly higher in urine sediments (AUC 71%) and supernatants (AUC 67%) of PCa patients; Uracil, Kynurenine, Glycerol-3-phosphate, Leucine, Proline were elevated upon disease progression. |
| [26] | Jentzmik et al. (2010) | 45/107 | Urine collection: after DRE for PCa patients; Second morning void urine for healthy participants; Storage and pre-treatments: Samples were centrifuged (1500× g, 10 min, 4 °C) and stored at −80 °C; Sample preparation: no info | Ez:fast amino acid analysis: SPME followed on a L-LE with the subsequent GC-MS on a 5973 MS and 6890 GC system. Recovery was checked with samples spiked with known amounts of sarcosine. | Mann–Whitney U test; Wilcoxon matched-pairs test; Spearman rank correlation; Fischer’s exact test; ROC analysis | Sarcosine | Median Sarcosine/creatinine was 13% lower in PCa patients than in controls |
| [27] | Jiang et al. (2010) | 5/5 | Urine collection: no info; Storage and pre-treatments: Samples were frozen at −80 °C; Sample preparation: Samples were thawed at room T and diluted 3 times using water; 10 µL of diluted urine were mixed with 10 µL of the internal standard solution and 1480 µL of 0.1% formic acid in water; those samples were diluted 450 times and injected for HPLC/MS/MS analysis | HPLC: An LC system working at 25 °C under a flow rate of 250 μL/min using a gradient system with the mobile phase consisting of (A) 0.1% formic acid in water and (B) 0.1% formic acid in acetonitrile (100%) was used for metabolite separation. The gradient program was initial 98% A and 2% B, linear gradient to 60% A and 40% B in 5 min, and return to initial conditions in 0.1 min at a flow rate of 250 μL/min, followed by equilibration for 10 min. MS/MS: An API 4000Q trap MS/MS system operated in multiple-reaction monitoring mode with ESI-positive ionisation was used. Turbo Spray was used as the ion source. The capillary voltage was set at 5.5 kV. Nitrogen gas was used as the curtain gas and cone gas. The cone gas flow was 50 L/h, and the desolvaation gas flow was 800 L/h. Optimal detection conditions were determined by direct infusion of each standard solution (20 ppb) in solvent A using a syringe pump. Parent-ion and daughter-ion scans were performed using nitrogen as the collision gas at a pressure of 3.8 × 103 millibar and a flow of 0.2 mL/min. | Multivariate statistics | Sarcosine; Proline; Kynurenine; Uracil; Glycerol-3-phosphate; Creatinine | nMmetabolites/µMcreatinine: PCa patients: Sarcosine 120; Proline 40; Kynurenine 15; Uracil 10; Glycerol-3-phosphate 85; Controls: Sarcosine 30; Proline 5; Kynurenine 8; Uracil 5; Glycerol-3-phosphate 30 |
| [28] | Wu et al. (2010) | 8 BHP; 20 healthy male/20 | Urine collection: first morning urine; Storage and pre-treatments: Samples were centrifuged within 1 h at 3000 rpm for 10 min at 25 °C; aliquoted in 1 mL and stored at −80 °C; Sample preparation: Samples were thawed by incubation at 37 °C for 3 min and vortex-mixed for 15 s. 800 µL methanol, 100 µL ribitol and 100 µ were added into each sample and vortex-mixed for 5 min and ultrasonicated at room T for 5 min. pH was adjusted to 9–10 with NaOH and solution was filtered by 0.45 µm membrane. 100 µL of filtrate were transferred to a screw vial and evaporated under N2 | ID GC-MS: 1 µL of derivatised sample was injected splittless into an Agilent 6980 GC equipped with a 30 m × 0.25 nm i.d. fused-silica capillary column with 0.25 µm HP-5MS stationary phase. Injector T was set at 250 °C, column T was initially kept at 80 °C for 3 min and increased to 280 °C at 10 °C/min, where it was held for 2 min. Column effluent was introduced into Agilent 5973 mass selective detector: quadrupole T 150 °C, ion source T 230 °C, solvent delay 180 s. | Two-sample t test; PCA; ROC analysis | Sarcosine; Propenoic acid; Pyrimidine; Dihyroxybutanoic acid; Creatinine; Purine; Glucopyranoside; Ribofuranoside; Xylonic acid; Xylopyranose | PCa patients average sarcosine value were 13% higher than healthy controls and 19% higher than BPH controls. Also propenoic acid, dihyroxybutanoic acid, creatinine, and xylonic acid, dihyroxybutanoic acid and xylonic acid, concentrations were higher in PCa patients. |
| [29] | Stabler et al. (2011) | 29 recurrent free; 25 PCa recurrence | Urine collection: before prostatectomy; Storage and pre-treatments: Samples were stored at −80 °C; Sample preparation: no info | GC-MS: A Durabond DB.1 fused silica capillary column (30 m × 0.25 mm) from J&W Scientific, Inc. and a Hewlett-Packard Co. 5992B gas chromatograph-mass spectrometer equipped with a falling needle injector were used. | Wilcoxon rank sum test; Fisher exact test; Spearman’s rank correlation | Cysteine; Homocysteine; Dimethylglycine; Sarcosine | Higher serum homocysteine, cystathionine, and cysteine levels independently predicted risk of early biochemical recurrence and PCa aggressiveness. The methionine further supplemented known clinical variables to increase sensitivity and specificity. |
| [30] | Bianchi et al. (2011) | 13 healthy; 10 BHP/33 | Urine collection: after DRE; Storage and pre-treatments: no info; Sample preparation: no info | SPME: A Gerstel MultiPurpose Sampler DualRail WorkStation MPS autosampler equipped with two sample trays, two-heated incubator shakers, a 100 µL syringe and a 3-position trays MFX was used. Hexyl chloroformate (10 μL), 10 μL of pyridine and 10 μL of hexanol were added, under continuous agitation at 500 rpm, in 0.9 mL clear crimp vials with sleeve for 10 × 32 vial containing 400 μL of urine. Norvaline was used as internal standard. After 5 min, 20 μL were diluted in 0.9 mL clear crimp vials previously filled with 800 μL of water. Simultaneously, the SPME fibres were transported between the 3-position tray and the vial. Urine sediments were washed with water under sonication and filtered. The filter was then broken up adding 500 µL of HCl and 1 mL of acetone into a 10 mL vial placed in an ultrasound bath for 10 min. Extraction was performed using PDMS/DBV fibre that was immersed in vial for 15 min at 35 °C. A constant magnetic stirring was applied. The desorption was carried out at 260 °C for 1 min. GC-MS: Oven setting was as follows: 80 °C for 0.3 min, 80 °C min−1 up to 200 °C, 200 °C for 0.3 min, 50 °C min−1 up to 290 °C. Inlet pressure, column flow and average linear velocity were 623.1 kPa, 0.97 mL min−1 and 51.3 cm s−1. The QP 2010 series MS detector (Shimadzu) equipped with the acquisition system GC Solution software was operated under the selected ion monitoring mode by applying a delay time of 2.9 min | Mann–Whitney U; Kruskal–Wallis tests; ROC analysis | Sarcosine; N-ethylglycine | µgSarcosine/gCreatinine discriminates between healthy, BHP and PCa patients Cut-off 179 µg/g: sensitivity 79%; specificity 87% |
| [31] | Shamsipur et al. (2012) | 20/12 | Urine collection: no info; Storage and pre-treatments: sample were frozen at −22 °C; Sample preparation: urine was thawed at room T and shaken vigorously for 1 min | DDLLME: 4 mL of water spiked with standard solution were treated with 12 M NaOH to obtain the desired pH. Standard amino acids were spiked into the solution at a level of 200 µg/L for initial screening and 50 µg/L for final optimisation. 150 µL acetonitrile, 200 µL pyridine and 25 µL carbon tetrachloride were added and the solution was mixed vigorously for 15 s. i-BuCF (250 µL) were added and shaken for 30 s. The solution was left to stand for 1 min and then centrifuged at 2260× g for 4 min for phase separation. 10 µL of the sediment phase was injected into the GC-MS for analysis. GC-MS: Processed samples were analysed using an Agilent 6890 GC coupled to an Agilent 5973 inert EI/CI mass selective detector. He was maintained at a constant flow of 1.8 mL min−1. The injection port was set to splitless and maintained at an optimised temperature of 280 °C. The oven temperature program was as follows: 80 °C (initial temperature), ramped to 155 °C at 10 °C min−1, holding at 155 °C for 5 min, then ramped to 172 °C at 2 °C min−1 holding for 2 min, finally ramped to 280 °C at 40 °C min−1 and holding for 6 min. T settings for the transfer-line heater, ion source, and quadrupole of the MS were 280, 150, and 150 °C, respectively. The dwell time for each scan was 150 ms ion−1, and the solvent delay was 7 min. The electron impact ionisation energy was 70 eV. | Bland-Altman | Sarcosine; Alanine; Proline; Leucine | Sarcosine mean concentrations were higher in PCa patients; Leucine mean concentration was lower in PCa patients |
| [32] | Struck-Lewicka et al. (2014) | 32/32 | Urine collection: no info; Storage and pre-treatments: Samples were stored at −80 °C; Sample preparation: no info | LC-TOF/MS: Urine samples after thawing at room temperature were vortex-mixed for 1 min and centrifuged at 4000× g for 10 min. Subsequently the supernatant was diluted in deionised water and then centrifuged at 4000× g for 15 min. After centrifugation, the samples were filtered directly to HPLC vials using 0.2 μm nylon filters. GC-MS: samples were thawed at room temperature for 1 h. The first step was addition of 50 μL of urease to 200 μL of urine. Next, the sample incubation in 37 °C for 30 min was applied (to decompose and remove excess amount of urea). Next, 800 μL of cold methanol (kept for 30 min in −80 °C) and 10 μL of pentadecanoic acid were added to urine samples. Then the samples were vortex-mixed for 5 min and centrifuged at 4000 g for 15 min. 200 μL of supernatants were transferred into glass inserts in GC vials and evaporated to dryness in 30 °C for 1 h 30 min. Next, 30 μL of methoxyamine in pyridine in concentration of 15 mg/mL was added to urine samples. The next step was vortex-mixing of each sample for 10 min and then incubation of all samples for 16 h in room temperature in dark place. The silylation process was performed with addition of 30 μL of BSTFA with 1% TMCS, vortex-mixing of each sample for 5 min and incubation for 1 h in 70 °C. Before GC-MS analysis, addition of 70 μL of hexane and vortex-mixing for 10 min were performed | MFE algorithm; PCA; PLS-DA; 7-fold cross validation | 35 metabolites | LC-TOF/MS: Positive ionisation mode R2 0.756, G2 0.579; Negative ionisation mode R2 0.763, G2 0.508 GC-MS: R2 0.788, G2 0.711 |
| [33] | Heger et al. (2014) | 32/32 | Urine collection: no info; Storage and pre-treatments: 500 µL of urine were mixed with 500 µL of 35% HCl and mineralised using the microwave equipment MW 3000. 100 µL of mineralised sample were diluted with 900 µL of dilution buffer and centrifuged using Centrifuge 5417R. 500 µL of the sample were diluted in 500 µL of 0.6 M NaOH; Sample preparation: no info | IELC: A glass column with an inner diameter of 3.7 and length of 350 mm was filled manually with strong cation exchanger in sodium cycle with ~12 μm particles and 8% porosity. The column was thermostated at 60 °C. Double channel VIS detector with an inner cell of 5 μL was set to two wavelengths: 440 and 570 nm. Elution of amino acids was carried out by buffer containing 10.0 g of citric acid, 5.6 g of sodium citrate, and 8.36 g of natrium chloride per litre of solution (pH 3.0). The flow rate was 0.25 mL·min−1. The reactor temperature was set to 120 °C. IEMA: The immunoenzymometric assay was used for analysis of PSA and fPSA | Shapiro–Wilk test; t test; hierarchical clustering | aspartic acid, threonine, methionine, isoleucine, leucine, tyrosine, arginine; sarcosine; proline; concentrations of K+, Na+, Cl−, uric acid, urea, PSA, glucose, total proteins, fPSA, creatinine and pH | All amino acids were increased in PCa patients, except for phenylalanine amounts. In controls, higher levels of K+ and uric acid and lower levels of urea and creatine were detected. PSA and free PSA were below the detection limit in controls. |
| [34] | Khalid et al. (2015) | 43/59 | Urine collection: no info; Storage and pre-treatments: Samples were stored at −20 °C; Sample preparation: Each sample was defrosted by immersing the vial in a water bath at 60 °C for 30 s. One single aliquot of urine sample per patient was used for VOC analysis. Thereafter, each sample was treated with an equal volume (0.75 mL) of sodium hydroxide 1 M. The mixture was equilibrated at 60 °C in a water bath for 30 min prior to SPME. | SPME: The SPME fibre was 85 μm thick and consisted of carboxen/polydimethylsiloxane. It was exposed to the headspace above the urine mixture for 20 min. GC-MS: VOCs were thermally desorbed from the fibre at 220 °C in the injection port of the GC/MS for 5 min. Injection was made in splitless mode and a split of 50 mL/min was turned on two minutes into the run. It was used helium as carrier gas (99.996% purity). Capillary column consisted of 94% dimethyl polysiloxane and 6% cyanopropyl-phenyl. The GC/MS T program of the run was as follows: initial oven T was held at 40 °C for 2 min then T was ramped up at a rate of 5 °C/min to 220 °C, with a 4 min hold at this T to give a total run time of 42 min. The mass spectrometer was run in electron impact (EI) ionisation mode, scanning the mass ion range 10–300 at 0.05 scan/s. A 4 min solvent delay was used at the start of the run. | Random Forest; LDA; 10-fold cross validation; double cross validation | 2,6-dimethyl-7-octen-2-ol; Pentanal; 3-octanone; 2-octanone | Except for pentanal, all of these compounds were down-regulated and/or less frequently present in the urine samples from PCa patients. Model AUC based on 4 biomarkers discovered was 63–65%, while it was 74% (RF) and 65% (LDA) if combined with PSA level. |
| [35] | Tsoi et al. (2016) | 88 BHP; 11 healthy/66 | Urine collection: after lunch prior PBs; Storage and pre-treatments: −20 °C; Sample preparation: Firstly, urine samples were thawed and centrifuged for 5 min at 13,000 rpm at room T. Urine sample supernatant (120 μL) and 60 μL of internal standard working solution were mixed with 420 μL of water. Of this well-mixed solution, 550 μL was passed through SPE, which had been conditioned and equilibrated with 1 mL of methanol and water respectively. Water (450 μL) was passed through the cartridge afterwards to elute out all polyamines. Of these SPE-treated samples, 400 μL were then mixed with 100 μL of 10% HFBA, and the final mixture was ready for instrumental analysis | UPLC-MS/MS: The column used was an Agilent EclipsePlus C18 RRHD (2.1 × 50 mm, 1.8 μm) protected with an Agilent SB-C18 guard column (2.1 × 5 mm, 1.8 μm). The LC elution profiles were optimised as follows: Eluent A was water with 0.1% HFBA while eluent B was acetonitrile with 0.1% HFBA. Eluent A was decreased from 95% to 60% in 10 min, and from 60% to 10% in 1 min. Afterwards the gradient was held constant for 5 min. The gradient was then increased from 10% to 95% in 1 min, and held constant for 8 additional minutes. The autosampler and column temperatures were set at 4 and 35 °C respectively. Injection was achieved by 5-s needle wash in Flush Port mode for 3 times with eluent B. Ten microlitres was injected each time. For the source parameter, drying gas (N2) temperature was set as 300 °C with 5 L/min flow rate. Nebuliser pressure was 45 psi. Sheath gas temperature was set as 250 °C with 11 L/min flow rate. Capillary voltage was set as 3500 V. | Student’s t-test; ROC analysis | putrescine (Put), spermidine (Spd) and spermine (Spm) | Normalised Spd was significantly lower in PCa than in BHP patients and controls The AUC for normalised Put, Spd and Spm were found to be 0.63 ± 0.05, 0.65 ± 0.05 and 0.83 ± 0.03 respectively |
| [36] | Sroka et al. (2016) | 25 BHP/25 | Urine collection: prior and after prostate massage; Storage and pre-treatments: Sodium azide solution was added. Samples were stored at −80 °C; Sample preparation: 10 µL aliquot of each urine sample or standard solution was added to 70 µL of 200 mM borate buffer containing 25 µM 2-Aminobutyric acid, 1 mM ascorbic acid and 10 mM TCEP. The solution was vortexed, centrifuged. 20 µL of 10 mM Aqc reagent dissolved in 100%ACN was added. The solution was vortexed, centrifuged, heated with shaking at 55 °C for 10 min. | LC-ESI-QqQ-MS: Mobile phase consisted of (A) 0.1% formic acid in water (v/v) and (B) 0.1% formic acid in ACN (v/v). Flow rate was set to 300 µL min−1. Separation was performed at 30 °C with monitored pressure below 400 bar. Analysis time was 19 min. The gradient was run from 0–2 min using 1% solvent B, then linearly raised over 7 min from 1% to 15% solvent B. then raised to 30% solvent B over 5 min and dropped to 1% for re-equilibration which lasted 5 min. Concentrations were quantified using Agilent 1200 LC-system coupled to an Agilent 6410 ESI-QqQ-MS. Injection volumes of 2 µL of samples or standards were used. Ions were monitored in the positive ion mode. Source conditions were set to sheath gas temperature 315 °C. Gas flow 10 L min−1. nebuliser pressure 45 psi and capillary voltage 3800 V. | t-test; U Mann-Whitney analysis; ROC curves | Arginine; Homoserine; Proline; Tyramine | In PCa samples, higher concentrations of arginine both before (p = 0.018) and after (p = 0.009) prostate massage and higher levels of proline only after prostate massage (p = 0.032) were detected. Higher levels of proline and homoserine and tyramine correlate with GS7 with respect to GS 6 and GS 5. |
| [37] | Fernandez-Peralbo et al. (2016) | 42/62 | Urine collection: prior PBs Storage and pre-treatments: Samples were stored at −80 °C Sample preparation: After thawing at room T, urine samples were vortex-mixed for 1 min and centrifuged at 21,000× g for 5 min. Then, 50 μL of the supernatant were 1:2 (v/v) diluted with 5 mM ammonium formate in water (pH 5.5–7.5) | LC-QTOF: A Mediterranea Sea C18 analytical column thermostated at 25 °C was used. The initial mobile phase was a mixture of 98% phase A (0.1% formic acid in water) and 2% phase B (0.1% formic acid in ACN). After injection, the initial mobile phase was kept under isocratic conditions for 1 min; then, a linear gradient of phase B from 2% to 100% was applied within 16 min. The flow rate was 0.6 mL/min. The total analysis time was 17 min, and 5 min were required to re-establish the initial conditions. The injected volume was 5 μL. The autosampler was kept at 4 °C to increase sample stability. | unpaired t-test (p-value < 0.05); PLS-DA | 28 metabolites | Almost all metabolites were present at lower concentrations in PCa patients than in controls, Training: Specificity 92.9%; Sensibility 88.4% Validation: Specificity 78.6%; Sensibility 63.2% |
| [38] | Gkotsos et al. (2017) | 49/52 | Urine collection: second morning void midstream; Storage and pre-treatments: −80 °C after post-centrifugation (each sample centrifuged at 1500× g, for 10 min, at 4 °C); Sample preparation: 100 μL of sample was diluted with 100 μL of MeOH. The samples were vortex-mixed (1 min) and centrifuged for 10 min (7000 g) to remove particulate matter and macromolecules. 50 μL of supernatant was diluted with 100 μL of MeCN and transferred to LC/MS vial, which was maintained at 10 °C. | UPLC-MS/MS: Separation was performed on a ACQUITY UPLC™ BEH AMIDE column 1.7 μm, 2.1 mm × 150 mm suitable for polar metabolites. Sarcosine, uracil, and kynurenic acid were detected using Multiple Reaction Monitoring (MRM) mode in a single injection of 15.5 min. The MRM transitions for the three metabolites were set as follows: sarcosine m/z 90–44, CV = 20 V, CE = 8 V; uracil m/z 113–70, CV = 40 V, CE = 15 V; and kynurenic acid m/z 190–172, CV = 32 V, CE = 12 V. For chromatographic separation the mobile phase was a mixture of (A) ACN/H2O, 95:5 v/v and (B) H2O/ACN, 70:30 v/v both with final ammonium formate buffer concentration of 10 Mm and elution was performed with a gradient program started with 100% A, then rising to 15% B linearly over the next 2 min, finally reaching 40% B over 2 min and returning to initial conditions over 5 min. The column was equilibrated for 6 min in the initial conditions. Flow rate was 0.5 mL/min | Kruskal–Wallis test; ROC analysis; Pearson correlation; Orthogonal Projections to Latent Structures Discriminant Analysis (OPLS-DA) | Sarcosine; Uracil; Kynurenic acid | Decreased median sarcosine and kynurenic acid and increased uracil concentrations were observed for patients with prostate cancer compared to participants without malignancy. |
| [39] | Derezinski et al. (2017) | 40/49 | Urine collection: second morning void midstream; Storage and pre-treatments: −80 °C after post-centrifugation (each sample centrifuged at 1500× g, for 10 min, at 4 °C); Sample preparation: 100 μL of sample was diluted with 100 μL of MeOH. The samples were vortex-mixed (1 min) and centrifuged for 10 min (7000 g) to remove particulate matter and macromolecules. 50 μL of supernatant was diluted with 100 μL of MeCN and transferred to LC/MS vial, which was maintained at 10 °C. | LC-ESI-MS/MS combined with aTRAQ: HPLC instrument 1260 Infinity combined with a 4000 QTRAP mass spectrometer with an EI source. The column was maintained at 50 °C with a flow rate of 800 μL/min. A mobile phase gradient of eluent A (0.1% formic acid and 0.01% heptafluorobutyric acid in water) and eluent B (0.1% formic acid and 0.01% heptafluorobutyric acid in methanol) was applied. The gradient profile was the following: from 2% to 40% of B from 0 till 6 min, maintained at 40% of B for 4 min, then increased to 90% of B till 11 min and held at 90% of B for 1 min. After 12 min the gradient decreased to 2% of B. From 13 to 18 min the mobile phase composition was unaltered. The injection volume was set at 2 µL. The mass spectrometer operated in positive ionisation mode with the following parameters: entrance potential, 10 V; declustering potential, 30 V and collision cell exit potential, 5 V. Collision energy of 30 eV was applied with the exception of cystathionine, cysteine, homocysteine, argininosuccinic acid, hydroxylysine, lysine, and ornithine (50 V). Scheduled multiple reaction monitoring mode was used with nitrogen as a collision gas. Data acquisition and processing were performed using the Analyst 1.5 software. | Mann-Whitney U test, Student’s t-test, Welch’s F test, ROC curve analysis, PLS-DA, Shapiro-Wilk test | 1-methylhistidine, 3-methylhistidine, Alanine, arginine, argininosuccinic acid, asparagine, aspartic acid, citrulline, carnosine, 39 metabolites | In PCa samples, taurine was present at significant higher level, while γ-amino- The PLS-DA model built on selected metabolites achieved sensitivity and specificity of 89.47% and 73.33%, respectively, whereas the total group membership classification value was 82.35%. |
| [40] | Aggio et al. (2015) | 73 with haematuria and poor stream without cancer/58 PCa; 24 BC | Urine collection: before PBs Storage temperature: −20 °C Headspace creation: samples were defrosted in water bath at 60 °C for 30 s, mixed with 0.75 mL of 1 M sodium hydroxide, reimmersed in water bath at 60 °C for 50 min EN analysis: 2 cm3 of headspace were extracted and analysed | Hybrid GC-MOS sensor system: It is composed of a gas chromatography (GC) oven fitted with a commercially available capillary column interfaced to a heated (450 °C) metal oxide sensor (MOS chemresistor composite of tin oxide and zinc oxide 50:50 by wt). The injection port of the GC was fitted with a 1 mm quartz linear and heated to 150 °C. Cylinder air at 35 psi was used as carrier gas. The temperature program was: 30 °C held for 6 min, up to 100 °C at 5 °C/min, hold 100 °C for 22 min. Volatile organic compounds (VOCs) exiting the GC column reach the MOS sensor, which resistance was recorded. | LOOCV; DoubleCV; SVM-P; Monte Carlo permutation | none | LOOCV: sensitivity 95%, specificity 96%; DoubleCV: sensitivity 87%, specificity 99%; SVM-P: sensitivity with respect to BC 78%; Monte Carlo permutation: chance-like accuracy 50% |
| Biomarkers Proposed | Concentrations in PCa Samples with Respect Controls | |
|---|---|---|
| Increasing Trend | Decreasing Trend | |
| Sarcosine | [25,28,29,30,31] | [36,38] |
| Isoleucine | [33] | [32,39] |
| Threonine | [33] | [32,39] |
| Proline | [31,33,36,37,38] | - |
| Citrulline | [31,33,36,37,38] | - |
| Homocitrulline | [31,33,36,37,38] | - |
| Histidine | - | [37,39] |
| Methylhistidine | - | [37,39] |
| Serine | - | [32,39] |
| Methionine | [33] | [39] |
| Tyrosine | [33] | [32,37,39] |
| Arginine | [36] | [39] |
| kynurenic acid | [27] | [38] |
| Uracil | [27,38] | - |
| Glutamine | - | [32,39] |
| Approaches Considered | Pros | Cons |
|---|---|---|
| Trained dogs | Highest diagnostic accuracy achieved | Influence of the discriminative ability on experimental protocol adopted; expensive and time-intensive dog training |
| Electronic noses | Rapid and relative inexpensive analysis | No uniformity concerning sample preparation, analysis and data processing techniques |
| Chemical analysis | Identification and quantification of possible PCa biomarker | Divergent opinions upon the concentrations of same metabolites in PCa samples with respect to controls; time-intensive analysis |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bax, C.; Taverna, G.; Eusebio, L.; Sironi, S.; Grizzi, F.; Guazzoni, G.; Capelli, L. Innovative Diagnostic Methods for Early Prostate Cancer Detection through Urine Analysis: A Review. Cancers 2018, 10, 123. https://doi.org/10.3390/cancers10040123
Bax C, Taverna G, Eusebio L, Sironi S, Grizzi F, Guazzoni G, Capelli L. Innovative Diagnostic Methods for Early Prostate Cancer Detection through Urine Analysis: A Review. Cancers. 2018; 10(4):123. https://doi.org/10.3390/cancers10040123
Chicago/Turabian StyleBax, Carmen, Gianluigi Taverna, Lidia Eusebio, Selena Sironi, Fabio Grizzi, Giorgio Guazzoni, and Laura Capelli. 2018. "Innovative Diagnostic Methods for Early Prostate Cancer Detection through Urine Analysis: A Review" Cancers 10, no. 4: 123. https://doi.org/10.3390/cancers10040123
APA StyleBax, C., Taverna, G., Eusebio, L., Sironi, S., Grizzi, F., Guazzoni, G., & Capelli, L. (2018). Innovative Diagnostic Methods for Early Prostate Cancer Detection through Urine Analysis: A Review. Cancers, 10(4), 123. https://doi.org/10.3390/cancers10040123










