Liquid Crystals: A Novel Approach for Cancer Detection and Treatment
Abstract
1. Introduction
2. Liquid Crystal Based Detection of Cancer
2.1. Detection of the Cancer Biomarker CA125: Label-Free Immunodetection
2.2. Detection of Keratin Forming Cell Tumor Cell Line Type B (KB) Cancer Cells: Label-Free In Vitro Approach
2.3. Early Detection of Skin Cancer: By Using a Liquid Crystal Associated Device
3. Liquid Crystal Chemotherapeutic Drugs for the Treatment of Cancer (LCs as New Antitumor Drugs)
4. LC1 and LC2 Suppressive Effects on K562 Cell Growth
5. Apoptosis and Cell Cycle Arrest by LC1 and LC2
6. Toxic Properties of Liquid Crystals on the Growth of Cells
7. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
Abbreviations
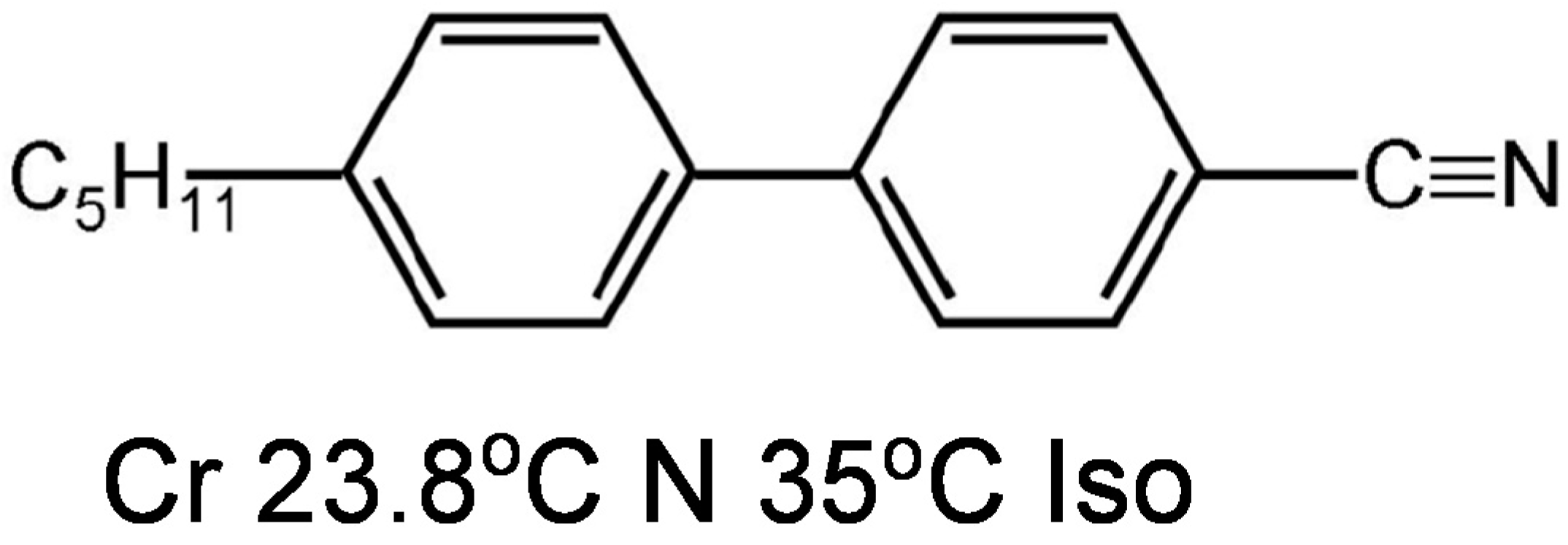
| 5CB | 4′-n-pentyl-4-cyanobiphenyl |
| ATM | Ataxia telangiectasia mutated |
| CML | Chronic myeloid leukemia |
| DI | Deionized |
| DMOAP | Dimethyloctadecyl[3-(trimethoxysilys)propyl]ammonium chloride |
| DOSI | Differential optical spectropolarimetric imaging system |
| HBsAg | Hepatitis B surface antigen |
| LC | Liquid crystal |
| LCTF | Liquid crystal tunable filter |
| LCRC | Liquid crystal related compound |
| MMS | Mohs micrographic surgery |
| NSCLC | Non-small cell lung cancer |
| OCT | Optical coherence tomography (OCT) |
| PBS | Phosphate-buffered saline |
| POM | Polarized optical microscope |
| ROS | Reactive oxygen species |
| SP | Spectropolarimetric imaging |
| UV | Ultraviolet |
| WILCPR | Wavelength independent liquid crystal polarization rotator |
References
- Golubnitschaja, O.; Flammer, J. What are the biomarkers for glaucoma? Surv. Ophthalmol. 2007, 52 (Suppl. 2), S155–S161. [Google Scholar] [CrossRef] [PubMed]
- Sawyers, C.L. The cancer biomarker problem. Nature 2008, 452, 548–552. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Du, G.; Wang, N.; Liu, C.; Hang, H.; Liang, W. Improving penetration in tumors with nanoassemblies of phospholipids and doxorubicin. J. Natl. Cancer Inst. 2007, 99, 1004–1015. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.H.; Hung, C.F.; Yang, S.C.; Wang, J.P.; Won, S.J.; Lin, C.N. Synthesis and cytotoxic, anti-inflammatory, and anti-oxidant activities of 2′,5′-dialkoxylchalcones as cancer chemopreventive agents. Bioorg. Med. Chem. 2008, 16, 7270–7276. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Prasad, A.K.; Parmar, V.S.; Ghosh, B.; Saini, N. 7,8-Dihydroxy-4-methylcoumarin induces apoptosis of human lung adenocarcinoma cells by ROS-independent mitochondrial pathway through partial inhibition of ERK/MAPK signaling. FEBS Lett. 2007, 581, 2447–2454. [Google Scholar] [CrossRef] [PubMed]
- Chou, T.C.; Zhang, X.; Zhong, Z.Y.; Li, Y.; Feng, L.; Eng, S.; Myles, D.R.; Johnson, R., Jr.; Wu, N.; Yin, Y.I.; et al. Therapeutic effect against human xenograft tumors in nude mice by the third generation microtubule stabilizing epothilones. Proc. Natl. Acad. Sci. USA 2008, 105, 13157–13162. [Google Scholar] [CrossRef] [PubMed]
- Chou, T.C.; Dong, H.; Zhang, X.; Tong, W.P.; Danishefsky, S.J. Therapeutic cure against human tumor xenografts in nude mice by a microtubule stabilization agent, fludelone, via parenteral or oral route. Cancer Res. 2005, 65, 9445–9454. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, Y.M.; Pyo, H. Gefitinib radiosensitizes non-small cell lung cancer cells through inhibition of ataxia telangiectasia mutated. Mol. Cancer 2010, 9, 222. [Google Scholar] [CrossRef] [PubMed]
- Santin, A.D.; Hermonat, P.L.; Ravaggi, A.; Bellone, S.; Roman, J.; Pecorelli, S.; Cannon, M.; Parham, G.P. Effects of concurrent cisplatinum administration during radiotherapy vs. radiotherapy alone on the immune function of patients with cancer of the uterine cervix. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 997–1006. [Google Scholar] [PubMed]
- Chandrasekhar, S. Liquid Crystals, 2nd ed.; Cambridge University Press: Cambridge, UK, 1992. [Google Scholar]
- Bahadur, B. Liquid Crystals—Applications and Uses; World Scientific: Toronto, ON, Canada, 1990. [Google Scholar]
- Castellano, J.A. Liquid crystal display applications: Past, Present & Future. Liq. Cryst. Today 1991, 1, 4–6. [Google Scholar]
- Iwabata, K.; Sugai, U.; Seki, Y.; Furue, H.; Sakaguchi, K. Applications of biomaterials to liquid crystals. Molecules 2013, 18, 4703–4717. [Google Scholar] [CrossRef] [PubMed]
- Sohn, J.I.; Hong, W.K.; Choi, S.S.; Coles, H.J.; Welland, M.E.; Cha, S.N.; Kim, J.M. Emerging Applications of Liquid Crystals Based on Nanotechnology. Materials 2014, 7, 2044–2061. [Google Scholar] [CrossRef] [PubMed]
- Hanna, J. Towards a new horizon of optoelectronic devices with liquid crystals. Optoelectron. Rev. 2005, 13, 8. [Google Scholar]
- Mulet, X.; Boyd, B.J.; Drummond, C.J. Advances in drug delivery and medical imaging using colloidal lyotropic liquid crystalline dispersions. J. Colloid Interface Sci. 2013, 393, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Goodby, J.W.; Gortz, V.; Cowling, S.J.; Mackenzie, G.; Martin, P.; Plusquellec, D.; Benvegnu, T.; Boullanger, P.; Lafont, D.; Queneau, Y.; et al. Thermotropic liquid crystalline glycolipids. Chem. Soc. Rev. 2007, 36, 1971–2032. [Google Scholar] [CrossRef] [PubMed]
- Luk, Y.Y.; Campbell, S.F.; Abbott, N.L.; Murphy, C.J. Non-toxic thermotropic liquid crystals for use with mammalian cells. Liq. Cryst. 2004, 31, 10. [Google Scholar] [CrossRef]
- Binot, C.; Sadoc, J.-F.; Chouard, C.-H. Oncogenesis, lipids rafts and liquid crystals: A nanoscopic supplementary field for applied researches and a new hope of advances in cancer. Heliyon 2018, 4, e00687. [Google Scholar] [CrossRef] [PubMed]
- Garello, L.; Ribaldone, D. Isolated and silent congenital pulmonary valvular insufficiency. Cardiol. Prat. 1973, 24, 177–183. [Google Scholar] [PubMed]
- Woltman, J.; Jay, G.D.; Crawford, G.P. Liquid-crystal materials find a new order in biomedical applications. Nat. Mater. 2007, 6, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Pina, A.S.; Roque, A.C. Bio-recognition and detection using liquid crystals. Biosens. Bioelectron. 2009, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Brake, J.M.; Daschner, M.K.; Luk, Y.Y.; Abbott, N.L. Biomolecular interactions at phospholipid-decorated surfaces of liquid crystals. Science 2003, 302, 2094–2097. [Google Scholar] [CrossRef] [PubMed]
- Luk, Y.Y.; Tingey, M.L.; Dickson, K.A.; Raines, R.T.; Abbott, N.L. Imaging the binding ability of proteins immobilized on surfaces with different orientations by using liquid crystals. J. Am. Chem. Soc. 2004, 126, 9024–9032. [Google Scholar] [CrossRef] [PubMed]
- Tingey, M.L.; Wilyana, S.; Snodgrass, E.J.; Abbott, N.L. Imaging of affinity microcontact printed proteins by using liquid crystals. Langmuir 2004, 20, 6818–6826. [Google Scholar] [CrossRef] [PubMed]
- Clare, B.H.; Abbott, N.L. Orientations of nematic liquid crystals on surfaces presenting controlled densities of peptides: Amplification of protein-peptide binding events. Langmuir 2005, 21, 6451–6461. [Google Scholar] [CrossRef] [PubMed]
- Bi, X.; Lai, S.L.; Yang, K.L. Liquid crystal multiplexed protease assays reporting enzymatic activities as optical bar charts. Anal. Chem. 2009, 81, 5503–5509. [Google Scholar] [CrossRef] [PubMed]
- Hoogboom, J.; Velonia, K.; Rasing, T.; Rowan, A.E.; Nolte, R.J. LCD-based detection of enzymatic action. Chem. Commun. 2006, 4, 434–435. [Google Scholar] [CrossRef]
- Lockwood, N.A.; Mohr, J.C.; Ji, L.; Murphy, C.J.; Palecek, S.P.; de Pablo, J.J.; Abbott, N.L. Thermotropic Liquid Crystals as Substrates for Imaging the Reorganization of Matrigel by Human Embryonic Stem Cells. Adv. Funct. Mater. 2006, 16, 618–624. [Google Scholar] [CrossRef]
- Jang, C.H.; Cheng, L.L.; Olsen, C.W.; Abbott, N.L. Anchoring of nematic liquid crystals on viruses with different envelope structures. Nano Lett. 2006, 6, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- McCamley, M.K.; Artenstein, A.W.; Opal, S.M.; Crawford, G.P. Optical detection of sepsis markers using liquid crystal based biosensors. Proc. SPIE 2007, 6441. [Google Scholar] [CrossRef]
- Stern, E.; Vacic, A.; Rajan, N.K.; Criscione, J.M.; Park, J.; Ilic, B.R.; Mooney, D.J.; Reed, M.A.; Fahmy, T.M. Label-free biomarker detection from whole blood. Nat. Nanotechnol. 2010, 5, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Mitas, M.; Mikhitarian, K.; Walters, C.; Baron, P.L.; Elliott, B.M.; Brothers, T.E.; Robison, J.G.; Metcalf, J.S.; Palesch, Y.Y.; Zhang, Z.; et al. Quantitative real-time RT-PCR detection of breast cancer micrometastasis using a multigene marker panel. Int. J. Cancer 2001, 93, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Pauletti, G.; Dandekar, S.; Rong, H.; Ramos, L.; Peng, H.; Seshadri, R.; Slamon, D.J. Assessment of Methods for Tissue-Based Detection of the HER-2/neu Alteration in Human Breast Cancer: A Direct Comparison of Fluorescence In Situ Hybridization and Immunohistochemistry. J. Clin. Oncol. 2000, 18, 3651–3664. [Google Scholar] [CrossRef] [PubMed]
- Choma, D.; Daures, J.P.; Quantin, X.; Pujol, J.L. Aneuploidy and prognosis of non-small-cell lung cancer: A meta-analysis of published data. Br. J. Cancer 2001, 85, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Jiang, C.; Yu, C.; Zhang, S.; Liu, B.; Kong, J. Protein chips and nanomaterials for application in tumor marker immunoassays. Biosens. Bioelectron. 2009, 24, 3399–3411. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Fu, Z.; Yan, F.; Ju, H. Biomedical and clinical applications of immunoassays and immunosensors for tumor markers. Trends Anal. Chem. 2007, 26, 679–688. [Google Scholar] [CrossRef]
- Bast, R.C., Jr.; Feeney, M.; Lazarus, H.; Nadler, L.M.; Colvin, R.B.; Knapp, R.C. Reactivity of a monoclonal antibody with human ovarian carcinoma. J. Clin. Investig. 1981, 68, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Scholler, N.; Urban, N. CA125 in ovarian cancer. Biomark. Med. 2007, 1, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Berruti, A.; Tampellini, M.; Torta, M.; Buniva, T.; Gorzegno, G.; Dogliotti, L. Prognostic value in predicting overall survival of two mucinous markers: CA 15-3 and CA 125 in breast cancer patients at first relapse of disease. Eur. J. Cancer 1994, 30A, 2082–2084. [Google Scholar] [CrossRef]
- Norum, L.F.; Erikstein, B.; Nustad, K. Elevated CA125 in breast cancer—A sign of advanced disease. Tumour Biol. 2001, 22, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Baba, H.; Toh, Y.; Okamura, T.; Maehara, Y. Peritoneal lavage CEA/CA125 is a prognostic factor for gastric cancer patients. J. Cancer Res. Clin. Oncol. 2007, 133, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Cai, F.F.; Zhong, X.Y. An overview of biomarkers for the ovarian cancer diagnosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 158, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Das, J.; Kelley, S.O. Protein detection using arrayed microsensor chips: Tuning sensor footprint to achieve ultrasensitive readout of CA-125 in serum and whole blood. Anal. Chem. 2011, 83, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Guo, A.; Wu, D.; Ma, H.; Zhang, Y.; Li, H.; Du, B.; Wei, Q. An ultrasensitive enzyme-free electrochemical immunosensor for CA125 using Au@Pd core-shell nanoparticles as labels and platforms for signal amplification. J. Mater. Chem. B 2013, 1, 4052–4058. [Google Scholar] [CrossRef]
- Lin, J.; Ju, H. Electrochemical and chemiluminescent immunosensors for tumor markers. Biosens. Bioelectron. 2005, 20, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Sok, D.; Clarizia, L.J.; Farris, L.R.; McDonald, M.J. Novel fluoroimmunoassay for ovarian cancer biomarker CA-125. Anal. Bioanal. Chem. 2009, 393, 1521–1523. [Google Scholar] [CrossRef] [PubMed]
- Tang, D.; Yuan, R.; Chai, Y. Electrochemical immuno-bioanalysis for carcinoma antigen 125 based on thionine and gold nanoparticles-modified carbon paste interface. Anal. Chim. Acta 2006, 564, 158–165. [Google Scholar] [CrossRef]
- Yin, Y.; Cao, Y.; Xu, Y.; Li, G. Colorimetric immunoassay for detection of tumor markers. Int. J. Mol. Sci. 2010, 11, 5077–5094. [Google Scholar] [CrossRef] [PubMed]
- Scholler, N.; Crawford, M.; Sato, A.; Drescher, C.W.; O’Briant, K.C.; Kiviat, N.; Anderson, G.L.; Urban, N. Bead-based ELISA for validation of ovarian cancer early detection markers. Clin. Cancer Res. 2006, 12, 2117–2124. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.K.; Skaife, J.J.; Dubrovsky, T.B.; Abbott, N.L. Optical amplification of ligand-receptor binding using liquid crystals. Science 1998, 279, 2077–2080. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; Abbott, N.L. Rubbed Films of Functionalized Bovine Serum Albumin as Substrates for the Imaging of Protein–Receptor Interactions Using Liquid Crystals. Adv. Mater. 2001, 13, 1445–1449. [Google Scholar] [CrossRef]
- Xue, C.Y.; Yang, K.L. Dark-to-bright optical responses of liquid crystals supported on solid surfaces decorated with proteins. Langmuir 2008, 24, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Yang, K.L. Detection and quantification of DNA adsorbed on solid surfaces by using liquid crystals. Langmuir 2010, 26, 1427–1430. [Google Scholar] [CrossRef] [PubMed]
- Price, A.D.; Schwartz, D.K. DNA hybridization-induced reorientation of liquid crystal anchoring at the nematic liquid crystal/aqueous interface. J. Am. Chem. Soc. 2008, 130, 8188–8194. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.; Yang, S.; Shen, G.; Yu, R.; Wu, Z. Signal-enhanced liquid-crystal DNA biosensors based on enzymatic metal deposition. Angew. Chem. Int. Ed. Engl. 2010, 49, 8608–8611. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Liu, Y.; Tan, H.; Wu, C.; Wu, Z.; Shen, G.; Yu, R. Gold nanoparticle based signal enhancement liquid crystal biosensors for DNA hybridization assays. Chem. Commun. 2012, 48, 2861–2863. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Wu, C.; Tan, H.; Wu, Y.; Liao, S.; Wu, Z.; Shen, G.; Yu, R. Label-Free Liquid Crystal Biosensor Based on Specific Oligonucleotide Probes for Heavy Metal Ions. Anal. Chem. 2013, 85, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Nair, G.G.; Prasad, S.K.; Jayalakshmi, V.; Shanker, G.; Yelamaggad, C.V. Fast responding robust nematic liquid crystalline gels formed by a monodisperse dipeptide: Electro-optic and rheological studies. J. Phys. Chem. B. 2009, 113, 6647–6651. [Google Scholar] [CrossRef] [PubMed]
- Hartono, D.; Xue, C.-Y.; Yang, K.-L.; Yung, L.-Y.L. Decorating Liquid Crystal Surfaces with Proteins for Real-Time Detection of Specific Protein–Protein Binding. Adv. Funct. Mater. 2009, 19, 3574–3579. [Google Scholar] [CrossRef]
- Luk, Y.-Y.; Tingey, M.L.; Hall, D.J.; Israel, B.A.; Murphy, C.J.; Bertics, P.J.; Abbott, N.L. Using Liquid Crystals to Amplify Protein−Receptor Interactions: Design of Surfaces with Nanometer-Scale Topography that Present Histidine-Tagged Protein Receptors. Langmuir 2003, 19, 1671–1680. [Google Scholar] [CrossRef]
- Chen, C.H.; Yang, K.L. Liquid crystal-based immunoassays for detecting hepatitis B antibody. Anal. Biochem. 2012, 421, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; Shah, R.R.; Abbott, N.L. Orientations of liquid crystals on mechanically rubbed films of bovine serum albumin: A possible substrate for biomolecular assays based on liquid crystals. Anal. Chem. 2000, 72, 4646–4653. [Google Scholar] [CrossRef] [PubMed]
- Luk, Y.-Y.; Jang, C.-H.; Cheng, L.-L.; Israel, B.A.; Abbott, N.L. Influence of Lyotropic Liquid Crystals on the Ability of Antibodies To Bind to Surface-Immobilized Antigens. Chem. Mater. 2005, 17, 4774–4782. [Google Scholar] [CrossRef]
- Xue, C.-Y.; Khan, S.A.; Yang, K.-L. Exploring Optical Properties of Liquid Crystals for Developing Label-Free and High-Throughput Microfluidic Immunoassays. Adv. Mater. 2009, 21, 198–202. [Google Scholar] [CrossRef]
- Khan, M.; Park, S.Y. Liquid crystal-based proton sensitive glucose biosensor. Anal. Chem. 2014, 86, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.; Li, X.; Liao, S.; Yu, R.; Wu, Z. Highly-sensitive liquid crystal biosensor based on DNA dendrimers-mediated optical reorientation. Biosens. Bioelectron. 2014, 62, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Peula, J.M.; Hidalgo-Alvarez, R.F.J. De Las Nieves, Coadsorption of IgG and BSA onto sulfonated polystyrene latex: I. Sequential and competitive coadsorption isotherms. J. Biomater. Sci. Polym. Ed. 1996, 7, 231–240. [Google Scholar] [CrossRef]
- Mondiot, F.; Wang, X.; de Pablo, J.J.; Abbott, N.L. Liquid crystal-based emulsions for synthesis of spherical and non-spherical particles with chemical patches. J. Am. Chem. Soc. 2013, 135, 9972–9975. [Google Scholar] [CrossRef] [PubMed]
- Ong, L.H.; Ding, X.; Yang, K.L. Mechanistic study for immobilization of cysteine-labeled oligopeptides on UV-activated surfaces. Colloids Surf. B Biointerfaces 2014, 122, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Yang, K.L. Improving protein transfer efficiency and selectivity in affinity contact printing by using UV-modified surfaces. Langmuir 2011, 27, 5427–5432. [Google Scholar] [CrossRef] [PubMed]
- Herrwerth, S.; Eck, W.; Reinhardt, S.; Grunze, M. Factors that determine the protein resistance of oligoether self-assembled monolayers—Internal hydrophilicity, terminal hydrophilicity, and lateral packing density. J. Am. Chem. Soc. 2003, 125, 9359–9366. [Google Scholar] [CrossRef] [PubMed]
- Young-Jong, K.; Kyung-Hwang, L.; Hikaru, S.; Jiwon, H.; Takashi, I.; Kuniaki, M.; Hiroyuki, S. Surface Chemical Conversion of Organosilane Self-Assembled Monolayers with Active Oxygen Species Generated by Vacuum Ultraviolet Irradiation of Atmospheric Oxygen Molecules. Jpn. J. Appl. Phys. 2008, 47, 307. [Google Scholar]
- Moser, A.E.; Eckhardt, C.J. A method for reliable measurement of relative frictional properties of different self-assembled monolayers using frictional force microscopy. Thin Solid Films 2001, 382, 202–213. [Google Scholar] [CrossRef]
- Ye, T.; Wynn, D.; Dudek, R.; Borguet, E. Photoreactivity of Alkylsiloxane Self-Assembled Monolayers on Silicon Oxide Surfaces. Langmuir 2001, 17, 4497–4500. [Google Scholar] [CrossRef]
- Chapman, R.G.; Ostuni, E.; Takayama, S.; Holmlin, R.E.; Yan, L.; Whitesides, G.M. Surveying for Surfaces that Resist the Adsorption of Proteins. J. Am. Chem. Soc. 2000, 122, 8303–8304. [Google Scholar] [CrossRef]
- Hong, L.; Sugimura, H.; Furukawa, T.; Takai, O. Photoreactivity of Alkylsilane Self-Assembled Monolayers on Silicon Surfaces and Its Application to Preparing Micropatterned Ternary Monolayers. Langmuir 2003, 19, 1966–1969. [Google Scholar] [CrossRef]
- Zheng, J.; Li, L.; Chen, S.; Jiang, S. Molecular Simulation Study of Water Interactions with Oligo (Ethylene Glycol)-Terminated Alkanethiol Self-Assembled Monolayers. Langmuir 2004, 20, 8931–8938. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.-J.; Chang, C.-H.; Lee, W. Label-free protein sensing by employing blue phase liquid crystal. Biomed. Opt. Express 2017, 8, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Su, H.-W.; Lee, Y.-H.; Lee, M.-J.; Hsu, Y.-C.; Lee, W. Label-free immunodetection of the cancer biomarker CA125 using high-Δn liquid crystals. J. Biomed. Opt. 2014, 19, 077006. [Google Scholar] [CrossRef] [PubMed]
- Su, H.W.; Lee, M.J.; Lee, W. Surface modification of alignment layer by ultraviolet irradiation to dramatically improve the detection limit of liquid-crystal-based immunoassay for the cancer biomarker CA125. J. Biomed. Opt. 2015, 20, 57004. [Google Scholar] [CrossRef] [PubMed]
- Hartono, D.; Lai, S.L.; Yang, K.L.; Yung, L.Y. A liquid crystal-based sensor for real-time and label-free identification of phospholipase-like toxins and their inhibitors. Biosens. Bioelectron. 2009, 24, 2289–2293. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Gupta, J.K.; Kishimoto, K.; Shoji, Y.; Kato, T.; Abbott, N.L. Design of Biomolecular Interfaces using Liquid Crystals Containing Oligomeric Ethylene Glycol. Adv. Funct. Mater. 2010, 20, 2098–2106. [Google Scholar] [CrossRef] [PubMed]
- Vallamkondu Jayalakshmi, Gurumurthy Hegde, Geetha Gopinathan Nair, Subbarao Krishna Prasad, Photo-controlled conformation-assisted permanent optical storage device employing a polymer network liquid crystal. Phys. Chem. Chem. Phys. 2009, 11, 6450–6454. [CrossRef] [PubMed]
- Birchall, L.S.; Ulijn, R.V.; Webb, S.J. A combined SPS-LCD sensor for screening protease specificity. Chem. Commun. 2008, 25, 2861–2863. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Gupta, K.C.; Borah, J.S.; Park, S.Y.; Kim, Y.K.; Lee, J.H.; Kang, I.K. Folate ligand anchored liquid crystal microdroplets emulsion for in vitro detection of KB cancer cells. Langmuir 2014, 30, 10668–10677. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, S.; Wark, K.L.; Gupta, J.K.; Abbott, N.L.; Caruso, F. Liquid Crystal Emulsions as the Basis of Biological Sensors for the Optical Detection of Bacteria and Viruses. Adv. Funct. Mater. 2009, 19, 2260–2265. [Google Scholar] [CrossRef]
- Meli, M.V.; Lin, I.H.; Abbott, N.L. Preparation of microscopic and planar oil-water interfaces that are decorated with prescribed densities of insoluble amphiphiles. J. Am. Chem. Soc. 2008, 130, 4326–4333. [Google Scholar] [CrossRef] [PubMed]
- Price, A.D.; Schwartz, D.K. Fatty-acid monolayers at the nematic/water interface: Phases and liquid-crystal alignment. J. Phys. Chem. B 2007, 111, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, L.A.; Schumann, K.R.; Luk, Y.Y.; Israel, B.A.; Abbott, N.L. Orientational behavior of thermotropic liquid crystals on surfaces presenting electrostatically bound vesicular stomatitis virus. Langmuir 2004, 16, 2375–2385. [Google Scholar] [CrossRef]
- Piculell, L. Understanding and exploiting the phase behavior of mixtures of oppositely charged polymers and surfactants in water. Langmuir 2013, 29, 10313–10329. [Google Scholar] [CrossRef] [PubMed]
- Morton, C.A.; Mackie, R.M. Clinical accuracy of the diagnosis of cutaneous malignant melanoma. Br. J. Dermatol. 1998, 138, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Rajaram, N.; Aramil, T.J.; Lee, K.; Reichenberg, J.S.; Nguyen, T.H.; Tunnell, J.W. Design and validation of a clinical instrument for spectral diagnosis of cutaneous malignancy. Appl. Opt. 2010, 49, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Rajaram, N.; Nguyen, T.H.; Tunnell, J.W. Lookup table-based inverse model for determining optical properties of turbid media. J. Biomed. Opt. 2008, 13, 050501. [Google Scholar] [CrossRef] [PubMed]
- Daukantas, P. Using Optics to Detect Skin Cancer. Opt. Photonics News 2007, 18, 28–33. [Google Scholar] [CrossRef]
- Liew, Y.M.; McLaughlin, R.A.; Wood, F.M.; Sampson, D.D. Motion correction of in vivo three-dimensional optical coherence tomography of human skin using a fiducial marker. Biomed. Opt. Express 2012, 3, 1774–1786. [Google Scholar] [CrossRef] [PubMed]
- Welzel, J.; Lankenau, E.; Birngruber, R.; Engelhardt, R. Optical coherence tomography of the human skin. J. Am. Acad. Dermatol. 1997, 37, 958–963. [Google Scholar] [CrossRef]
- Gambichler, T.; Orlikov, A.; Vasa, R.; Moussa, G.; Hoffmann, K.; Stucker, M.; Altmeyer, P.; Bechara, F.G. In vivo optical coherence tomography of basal cell carcinoma. J. Dermatol. Sci. 2007, 45, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.T.; Li, M.L.; Zhang, H.F.; Maslov, K.; Stoica, G.; Wang, L.V. Three-dimensional imaging of skin melanoma in vivo by dual-wavelength photoacoustic microscopy. J. Biomed. Opt. 2006, 11, 34032. [Google Scholar] [CrossRef] [PubMed]
- Baba, J.S.; Chung, J.R.; DeLaughter, A.H.; Cameron, B.D.; Cote, G.L. Development and calibration of an automated Mueller matrix polarization imaging system. J. Biomed. Opt. 2002, 7, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Jacques, S.L.; Ramella-Roman, J.C.; Lee, K. Imaging skin pathology with polarized light. J. Biomed. Opt. 2002, 7, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Ramella-Roman, J.C.; Lee, K.; Prahl, S.A.; Jacques, S.L. Jacques, Design, testing, and clinical studies of a handheld polarized light camera. J. Biomed. Opt. 2004, 9, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Yaroslavsky, A.N.; Neel, V.; Anderson, R.R. Demarcation of nonmelanoma skin cancer margins in thick excisions using multispectral polarized light imaging. J. Investig. Dermatol. 2003, 121, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Demos, S.G.; Alfano, R.R. Optical polarization imaging. Appl. Opt. 1997, 36, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Demos, S.G.; Radousky, H.B.; Alfano, R.R. Deep subsurface imaging in tissues using spectral and polarization filtering. Opt. Express 2000, 7, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.M.; Reisfeld, R.A.; Cheresh, D.A. Integrin alpha v beta 3 rescues melanoma cells from apoptosis in three-dimensional dermal collagen. Proc. Natl. Acad. Sci. USA 1994, 91, 8856–8860. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.R.; Parrish, J.A. The optics of human skin. J. Investig. Dermatol. 1981, 77, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Backman, V.; Gurjar, R.; Badizadegan, K.; Itzkan, I.; Dasari, R.R.; Perelman, L.T.; Feld, M.S. Polarized light scattering spectroscopy for quantitative measurement of epithelial cellular structures in situ. IEEE J. Sel. Top. Quantum Electron. 1999, 5, 1019–1026. [Google Scholar] [CrossRef]
- Gurjar, R.S.; Backman, V.; Perelman, L.T.; Georgakoudi, I.; Badizadegan, K.; Itzkan, I.; Dasari, R.R.; Feld, M.S. Imaging human epithelial properties with polarized light-scattering spectroscopy. Nat. Med. 2001, 7, 1245–1248. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.E.; Kent, D.E. Surgical margins in the treatment of nonmelanoma skin cancer and mohs micrographic surgery. Curr. Surg. 2005, 62, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Philp, J.; Carter, N.J.; Lenn, C.P. Improved optical discrimination of skin with polarized light. J. Soc. Cosmet. Chem. 1988, 39, 11. [Google Scholar]
- Anderson, R. Polarized light examination and photography of the skin. Arch. Dermatol. 1991, 127, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Al-Arashi, M.Y.; Salomatina, E.; Yaroslavsky, A.N. Multimodal confocal microscopy for diagnosing nonmelanoma skin cancers. Lasers Surg. Med. 2007, 39, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Laude-Boulesteix, B.; De Martino, A.; Drevillon, B.; Schwartz, L. Mueller polarimetric imaging system with liquid crystals. Appl. Opt. 2004, 43, 2824–2832. [Google Scholar] [CrossRef] [PubMed]
- Weber, A.; Cheney, M.; Smithwick, Q.; Elsner, A. Polarimetric imaging and blood vessel quantification. Opt. Express 2004, 12, 5178–5190. [Google Scholar] [CrossRef] [PubMed]
- Bock, W.J.; Gannot, I.; Tanev, S. Optical Waveguide Sensing and Imaging; Springer: Dordrecht, The Netherlands, 2008. [Google Scholar]
- Aharon, O.; Abdulhalim, I.; Arnon, O.; Rosenberg, L.; Dyomin, V.; Silberstein, E. Differential optical spectropolarimetric imaging system assisted by liquid crystal devices for skin imaging. J. Biomed. Opt. 2011, 16, 086008. [Google Scholar] [CrossRef] [PubMed]
- Aharon, O.; Abdulhalim, I. Liquid crystal Lyot tunable filter with extended free spectral range. Opt. Express 2009, 17, 11426–11433. [Google Scholar] [CrossRef] [PubMed]
- Aharon, O.; Abdulhalim, I.S. Liquid crystal wavelength-independent continuous polarization rotator. Opt. Eng. 2010, 49, 034002. [Google Scholar] [CrossRef]
- Ye, C. Construction of an optical rotator using quarter-wave plates and an optical retarder. Opt. Eng. 1995, 34, 3031–3036. [Google Scholar] [CrossRef]
- Kuo, P.L.; Hsu, Y.L.; Lin, T.C.; Chang, J.K.; Lin, C.C. Induction of cell cycle arrest and apoptosis in human non-small cell lung cancer A549 cells by casuarinin from the bark of Terminalia arjuna Linn. Anticancer Drugs 2005, 16, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Abe, A.; Yamane, M.; Tomoda, A. Prevention of growth of human lung carcinoma cells and induction of apoptosis by a novel phenoxazinone, 2-amino-4,4alpha-dihydro-4alpha,7-dimethyl-3H-phenoxazine-3-one. Anticancer Drugs 2001, 12, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Pairam, E.; Vallamkondu, J.; Koning, V.; van Zuiden, B.C.; Ellis, P.W.; Bates, M.A.; Vitelli, V.; Fernandez-Nieves, A. Stable nematic droplets with handles. Proc. Natl. Acad. Sci. USA 2013, 110, 9295–9300. [Google Scholar] [CrossRef] [PubMed]
- Zaki, Y.H.; Al-Gendey, M.S.; Abdelhamid, A.O. A facile synthesis, and antimicrobial and anticancer activities of some pyridines, thioamides, thiazole, urea, quinazoline, β-naphthyl carbamate, and pyrano[2,3-d]thiazole derivatives. Chem. Cent. J. 2018, 12, s13065. [Google Scholar] [CrossRef] [PubMed]
- Geetha, G.N.; Krishna Prasad, S.; Bhargavi, R.; Jayalakshmi, V.; Shanker, G.; Yelamaggad, C.V. Soft glass rheology in liquid crystalline gels formed by a monodisperse dipeptide. J. Phys. Chem. B 2009, 114, 697–704. [Google Scholar]
- Zhang, J.H.; Fan, C.D.; Zhao, B.X.; Shin, D.S.; Dong, W.L.; Xie, Y.S.; Miao, J.Y. Synthesis and preliminary biological evaluation of novel pyrazolo[1,5-a]pyrazin-4(5H)-one derivatives as potential agents against A549 lung cancer cells. Bioorg. Med. Chem. 2008, 16, 10165–10171. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhuang, L.; Chen, Y. Effection and mechanism of radiosensitivity of non-small cell lung cancer cell line H358 following gefitinib treatment. Zhongguo Fei Ai Za Zhi 2011, 14, 841–847. (In Chinese) [Google Scholar] [PubMed]
- Prasad, S.K.; Nair, G.G.; Hegde, G.; Jayalakshmi, V. Evidence of wormlike micellar behavior in chromonic liquid crystals: Rheological, X-ray, and dielectric studies. J. Phys. Chem. B 2007, 111, 9741–9746. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, C.L.; Bennett, D.B.; Lechuga-Ballesteros, D. Pharmaceutical Liquid Crystals: The Relevance of Partially Ordered Systems. J. Pharm. Sci. 2005, 94, 1861–1880. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.H.; Chien, C.M.; Lu, M.C.; Lin, Y.H.; Hu, X.W.; Lin, S.R. Up-regulation of Bax and endonuclease G, and down-modulation of Bcl-XL involved in cardiotoxin III-induced apoptosis in K562 cells. Exp. Mol. Med. 2006, 38, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Fukushi, Y.; Yoshino, Y.; Ishikawa, J.; Sagisaka, M.; Kashiwakura, I.; Yoshizawa, A.; Hazawa, M.; Takahashi, K.; Nishizawa, A.; Yoshizawa, A. Synthesis and anticancer properties of phenyl benzoate derivatives possessing a terminal hydroxyl group. J. Mater. Chem. B 2014, 2, 1335–1343. [Google Scholar] [CrossRef]
- Wakasaya, T.; Yoshino, H.; Fukushi, Y.; Yoshizawa, A.; Kashiwakura, I. A liquid crystal-related compound induces cell cycle arrest at the G2/M phase and apoptosis in the A549 human non-small cell lung cancer cell line. Int. J. Oncol. 2013, 42, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Fukushi, Y.; Hazawa, M.; Takahashi, K.; Yoshizawa, A.; Kashiwakura, I. Liquid crystal-related compound-induced cell growth suppression and apoptosis in the chronic myelogenous leukemia K562 cell line. Investig. New Drugs 2011, 29, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Hazawa, M.; Takahashi, K.; Nishizawa, A.; Yoshizawa, A.; Kashiwakura, I. Suppressive effects of liquid crystal compounds on the growth of the A549 human lung cancer cell line. Investig. New Drugs 2011, 29, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Puil, L.; Liu, J.; Gish, G.; Mbamalu, G.; Bowtell, D.; Pelicci, P.G.; Arlinghaus, R.; Pawson, T. Bcr-Abl oncoproteins bind directly to activators of the Ras signalling pathway. EMBO J. 1994, 13, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Skorski, T.; Bellacosa, A.; Nieborowska-Skorska, M.; Majewski, M.; Martinez, R.; Choi, J.K.; Trotta, R.; Wlodarski, P.; Perrotti, D.; Chan, T.O.; et al. Transformation of hematopoietic cells by BCR/ABL requires activation of a PI-3k/Akt-dependent pathway. EMBO J. 1997, 16, 6151–6161. [Google Scholar] [CrossRef] [PubMed]
- Druker, B.J.; Sawyers, C.L.; Kantarjian, H.; Resta, D.J.; Reese, S.F.; Ford, J.M.; Capdeville, R.; Talpaz, M. Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N. Engl. J. Med. 2001, 344, 1038–1042. [Google Scholar] [CrossRef] [PubMed]
- McCubrey, J.A.; Steelman, L.S.; Chappell, W.H.; Abrams, S.L.; Wong, E.W.; Chang, F.; Lehmann, B.; Terrian, D.M.; Milella, M.; Tafuri, A.; et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance. Biochim. Biophys. Acta 2007, 1773, 1263–1284. [Google Scholar] [CrossRef] [PubMed]
- Fava, C.; Kantarjian, H.; Cortes, J.; Jabbour, E. Development and targeted use of nilotinib in chronic myeloid leukemia. Drug Des. Dev. Ther. 2009, 2, 233–243. [Google Scholar]
- Hanna, T.P.; Kangolle, A.C. Cancer control in developing countries: Using health data and health services research to measure and improve access, quality and efficiency. BMC Int. Health Hum. Rights 2010, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.D.; Li, G.; Hu, H.; Jiang, C.; Kang, K.S.; Lee, Y.S.; Kim, S.H.; Lu, J. Involvement of c-Jun N-terminal kinase in G2/M arrest and caspase-mediated apoptosis induced by sulforaphane in DU145 prostate cancer cells. Nutr. Cancer 2005, 52, 213–224. [Google Scholar] [CrossRef] [PubMed]
- McCubrey, J.A.; Steelman, L.S.; Abrams, S.L.; Lee, J.T.; Chang, F.; Bertrand, F.E.; Navolanic, P.M.; Terrian, D.M.; Franklin, R.A.; D’Assoro, A.B.; et al. Roles of the RAF/MEK/ERK and PI3K/PTEN/AKT pathways in malignant transformation and drug resistance. Adv. Enzyme Regul. 2006, 46, 249–279. [Google Scholar] [CrossRef] [PubMed]
- Xia, Z.; Dickens, M.; Raingeaud, J.; Davis, R.J.; Greenberg, M.E. Opposing effects of ERK and JNK-p38 MAP kinases on apoptosis. Science 1995, 270, 1326–1331. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Fu, Y. Antiproliferative effect of indomethacin on CML cells is related to the suppression of STATs/Bcl-XL signal pathway. Ann. Hematol. 2006, 85, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Li, Y.; Li, J.; Li, H.; Fu, J.; Liu, Y.; Liu, H.; Chen, X. (-)Gossypol and its combination with imatinib induce apoptosis in human chronic myeloid leukemic cells. Leuk. Lymphoma 2007, 48, 2204–2212. [Google Scholar] [CrossRef] [PubMed]
- Bourougaa, K.; Naski, N.; Boularan, C.; Mlynarczyk, C.; Candeias, M.M.; Marullo, S.; Fahraeus, R. Endoplasmic reticulum stress induces G2 cell-cycle arrest via mRNA translation of the p53 isoform p53/47. Mol. Cell 2010, 38, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, J.; Takahashi, Y.; Hazawa, M.; Fukushi, Y.; Yoshizawa, A.; Kashiwakura, I. Suppressive effects of liquid crystal compounds on the growth of U937 human leukemic monocyte lymphoma cells. Cancer Cell Int. 2012, 12, 3. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Fan, X.; Xu, X.; Yang, X.; Wang, X.; Liang, H.P. Evodiamine induces caspase-dependent apoptosis and S phase arrest in human colon lovo cells. Anticancer Drugs 2010, 21, 766–776. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M. Involvement of DNA-PK and ATM in radiation- and heat-induced DNA damage recognition and apoptotic cell death. J. Radiat. Res. 2010, 51, 493–501. [Google Scholar] [CrossRef] [PubMed]






© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vallamkondu, J.; Corgiat, E.B.; Buchaiah, G.; Kandimalla, R.; Reddy, P.H. Liquid Crystals: A Novel Approach for Cancer Detection and Treatment. Cancers 2018, 10, 462. https://doi.org/10.3390/cancers10110462
Vallamkondu J, Corgiat EB, Buchaiah G, Kandimalla R, Reddy PH. Liquid Crystals: A Novel Approach for Cancer Detection and Treatment. Cancers. 2018; 10(11):462. https://doi.org/10.3390/cancers10110462
Chicago/Turabian StyleVallamkondu, Jayalakshmi, Edwin Bernard Corgiat, Gollapelli Buchaiah, Ramesh Kandimalla, and P. Hemachandra Reddy. 2018. "Liquid Crystals: A Novel Approach for Cancer Detection and Treatment" Cancers 10, no. 11: 462. https://doi.org/10.3390/cancers10110462
APA StyleVallamkondu, J., Corgiat, E. B., Buchaiah, G., Kandimalla, R., & Reddy, P. H. (2018). Liquid Crystals: A Novel Approach for Cancer Detection and Treatment. Cancers, 10(11), 462. https://doi.org/10.3390/cancers10110462





