Mathematical Model for Skin Pain Sensation under Local Distributed Mechanical Compression for Electronic Skin Applications
Abstract
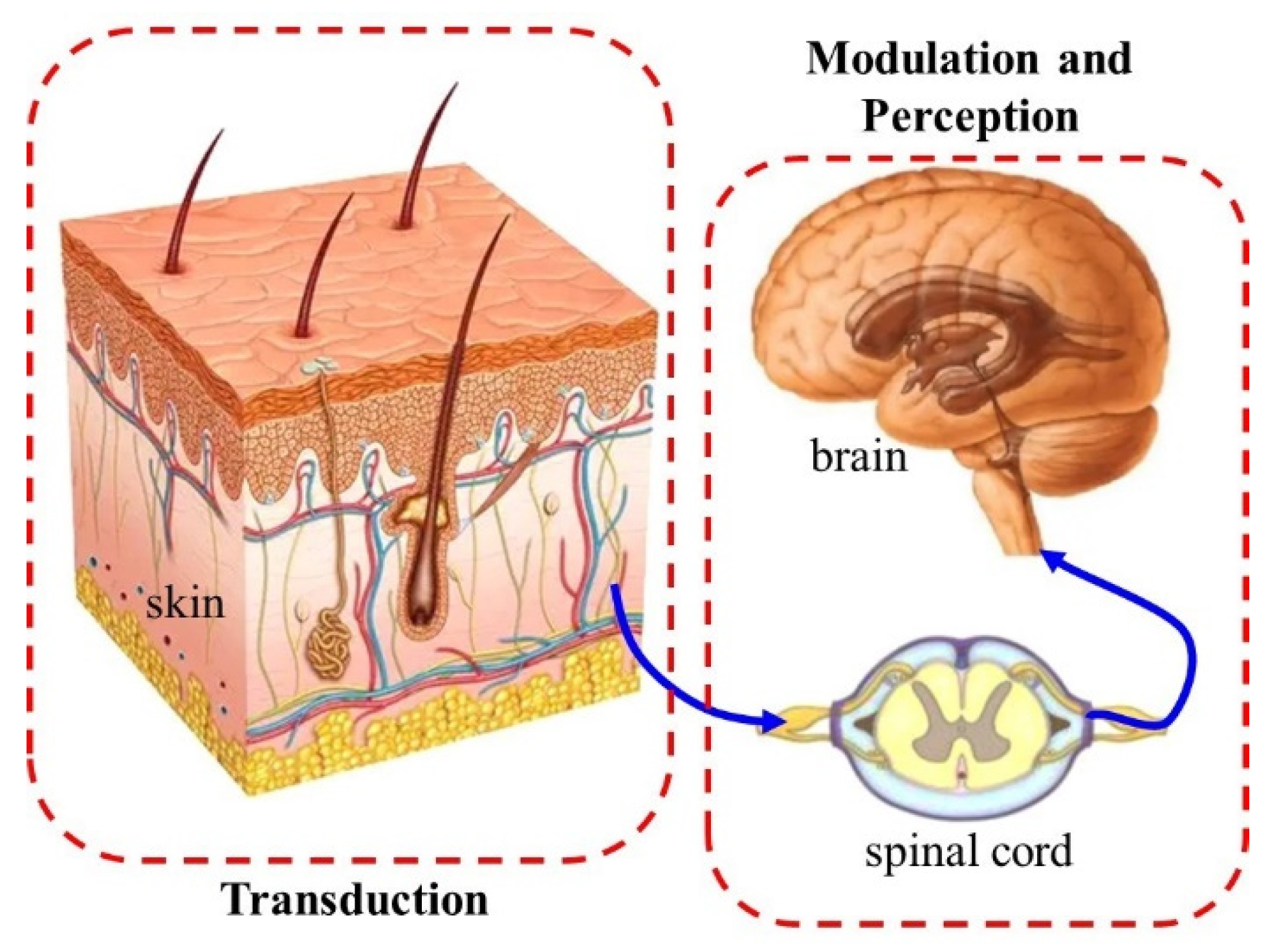
:1. Introduction
2. Modeling and Analysis
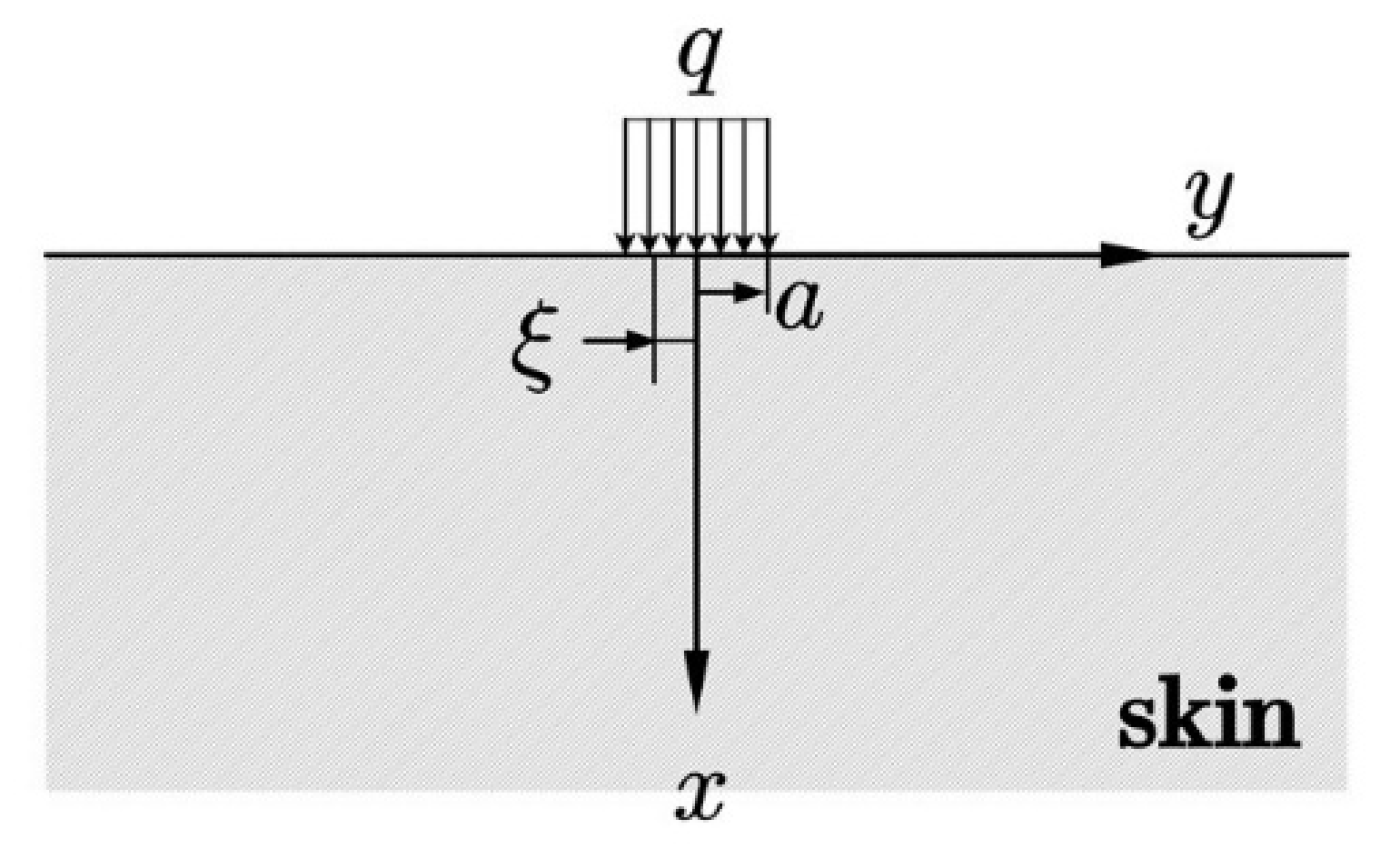
2.1. Mechanical Model of Skin Compression
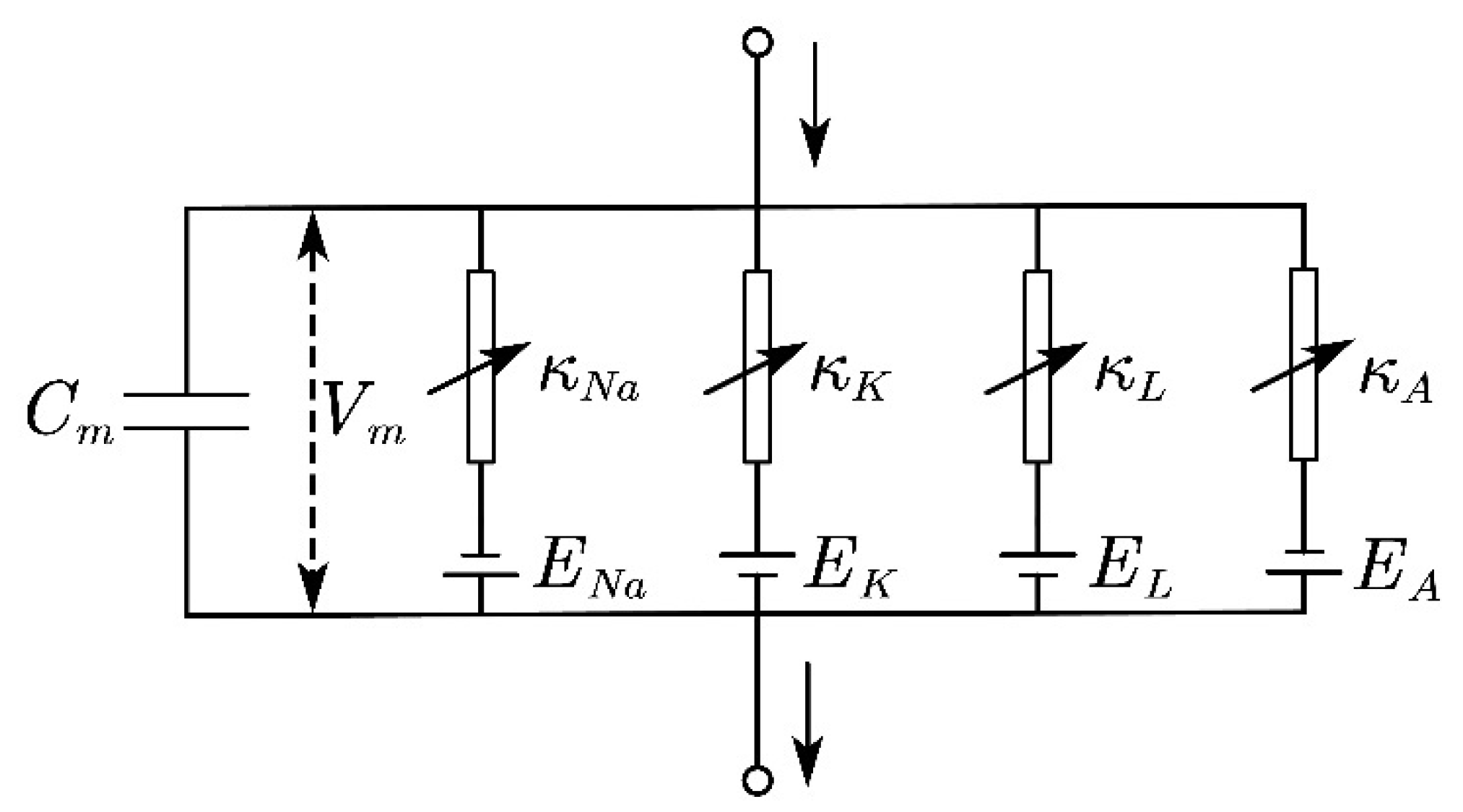
2.2. Model of Transduction
Current and Frequency Modulation
2.3. Model of Modulation and Perception
3. Results and Discussion
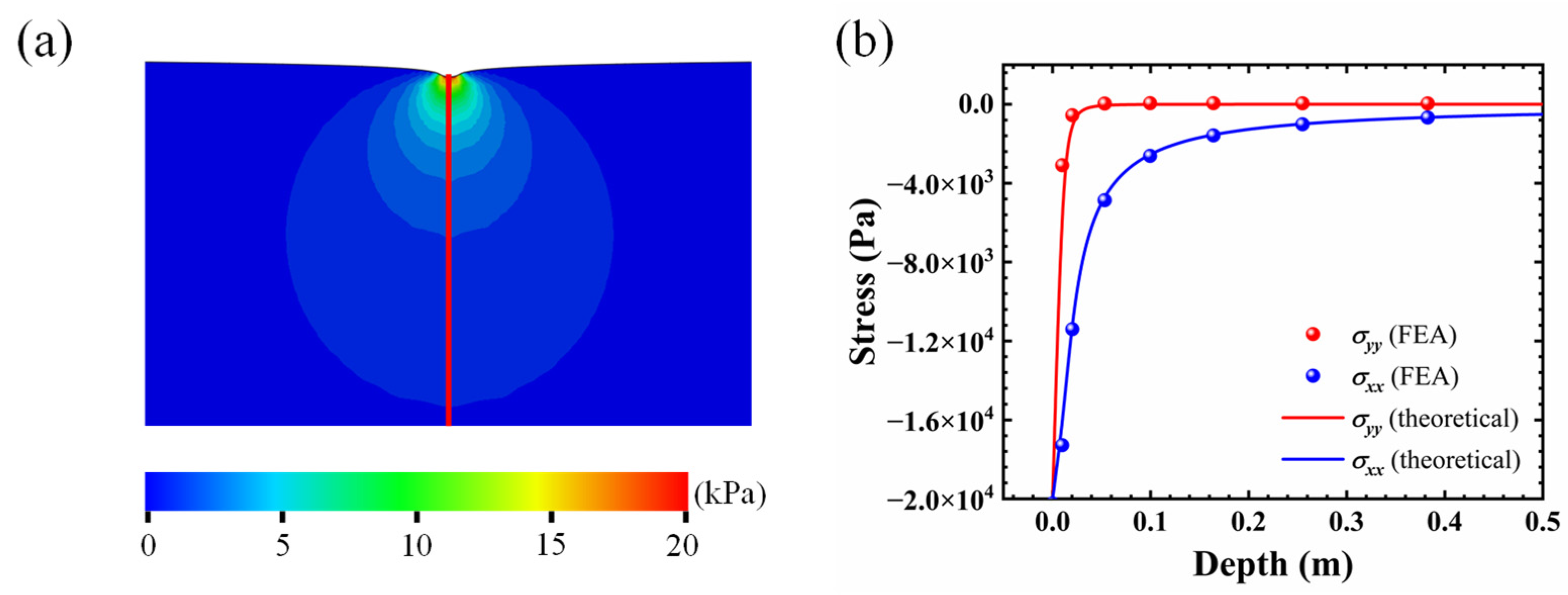
3.1. Stress Distributions in the Skin
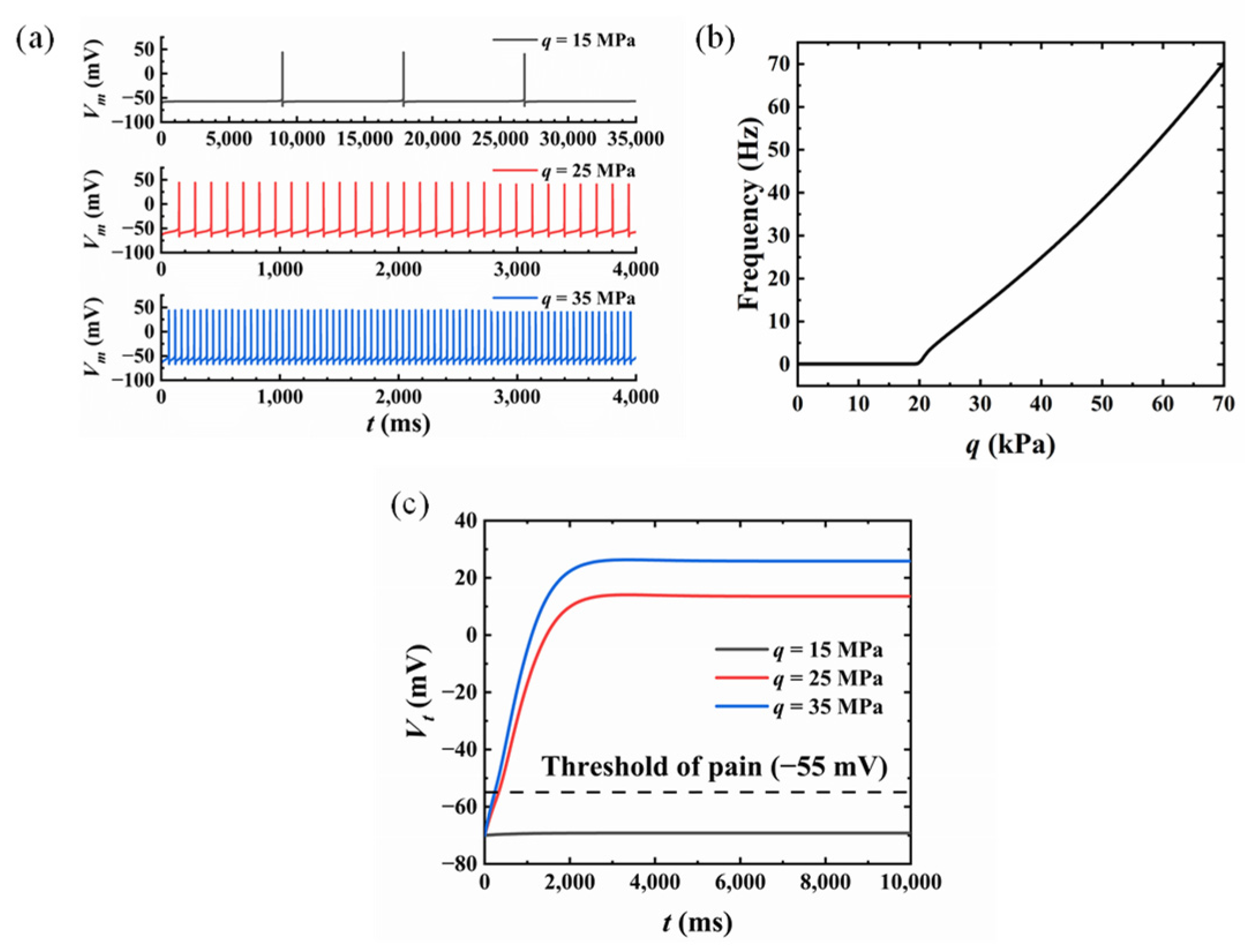
3.2. Influence of the Compression Amplitude
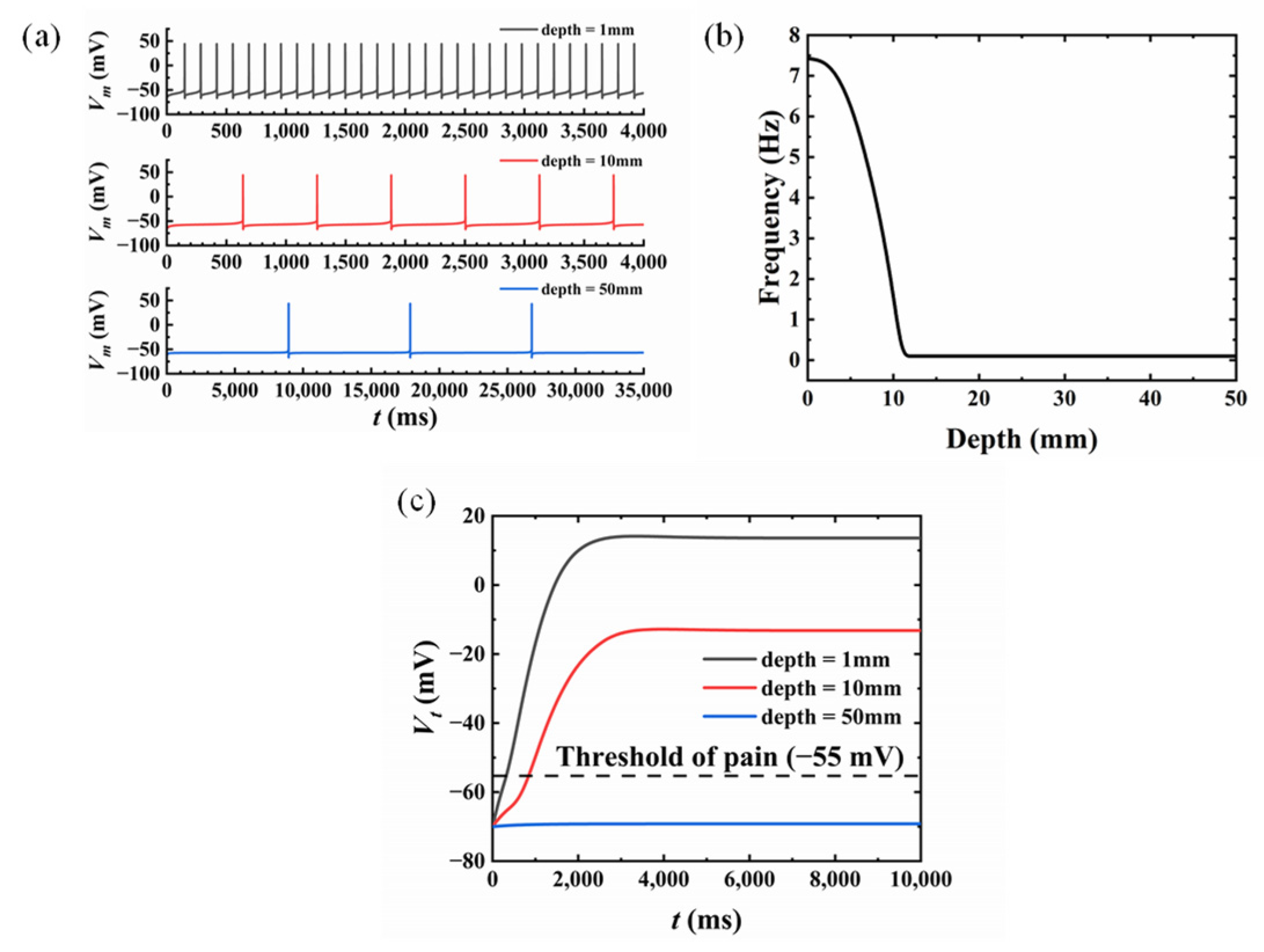
3.3. Influence of the Nociceptor Location
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Whitton, J.T.; Everall, J.D. The thickness of the epidermis. Br. J. Dermatol. 1973, 89, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.C.; Mun, J.; Kwon, S.Y.; Park, S.; Bao, Z.N.; Park, S. Electronic Skin: Recent Progress and Future Prospects for Skin-Attachable Devices for Health Monitoring, Robotics, and Prosthetics. Adv. Mater. 2019, 31, 1904765. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.A. Surface deflection of primate fingertip under line load. J. Biomech. 1989, 22, 343–349. [Google Scholar] [CrossRef]
- Dandekar, K.; Raju, B.I.; Srinivasan, M.A. 3-D finite-element models of human and monkey fingertips to investigate the mechanics of tactile sense. J. Biomech. Eng. Trans. Asme 2003, 125, 682–691. [Google Scholar] [CrossRef]
- Xu, F.; Lu, T.J.; Seffen, K.A. Biothermomechanics of skin tissues. J. Mech. Phys. Solids 2008, 56, 1852–1884. [Google Scholar] [CrossRef]
- Li, Y.H.; Zhang, J.P.; Xing, Y.F.; Song, J.Z. Thermomechanical Analysis of Epidermal Electronic Devices Integrated With Human Skin. J. Appl. Mech. Trans. Asme 2017, 84, 111004. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, Y.H.; Dong, S.J.; Cui, Y.; Dai, Z. An analytic model for transient heat conduction in bi-layered structures with flexible serpentine heaters. Appl. Math. Mech.-Engl. Ed. 2021, 42, 1279–1296. [Google Scholar] [CrossRef]
- Xu, F.; Lu, T.J.; Seffen, K.A. Skin thermal pain modeling—A holistic method. J. Therm. Biol. 2008, 33, 223–237. [Google Scholar] [CrossRef]
- Yin, Y.F.; Li, M.; Li, Y.H.; Song, J.Z. Skin pain sensation of epidermal electronic device/skin system considering non-Fourier heat conduction. J. Mech. Phys. Solids 2020, 138, 103927. [Google Scholar] [CrossRef]
- Yang, W.; Sherman, V.R.; Gludovatz, B.; Schaible, E.; Stewart, P.; Ritchie, R.O.; Meyers, M.A. On the tear resistance of skin. Nat. Commun. 2015, 6, 6649. [Google Scholar] [CrossRef] [Green Version]
- Britton, N.F.; Skevington, S.M. On the mathematical modelling of pain. Neurochem. Res. 1996, 21, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.J.; Lu, T.J. A multi-scale view of skin thermal pain: From nociception to pain sensation. Philos. Trans. R. Soc. A-Math. Phys. Eng. Sci. 2010, 368, 521–559. [Google Scholar] [CrossRef]
- Goldscheider, A. Ueber den Schmerz in Physiologischer und Klinischer Hinsicht; Hirschwald: Berlin, Germany, 1894. [Google Scholar]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory: A gate control system modulates sensory input from the skin before it evokes pain perception and response. Pain Forum 1996, 5, 3–11. [Google Scholar] [CrossRef]
- Xu, F.; Wen, T.; Seffen, K.; Lu, T.J. Modeling of skin thermal pain: A preliminary study. Appl. Math. Comput. 2008, 205, 37–46. [Google Scholar] [CrossRef]
- Lang, V.A.; Lundh, T.; Ortiz-Catalan, M. Mathematical and Computational Models for Pain: A Systematic Review. Pain Med. 2021, 22, 2806–2817. [Google Scholar] [CrossRef]
- Hodgkin, A.L.; Huxley, A.F. A quantitative description of membrane current and its application to conduction and excitation in nerve. J. Physiol. 1952, 117, 500–544. [Google Scholar] [CrossRef]
- Hodgkin, A.L.; Huxley, A.F. Currents carried by sodium and potassium ions through the membrane of the giant axon of Loligo. J. Physiol. 1952, 116, 449–472. [Google Scholar] [CrossRef]
- Britton, N.F.; Skevington, S.M. A mathematical model of the gate control theory of pain. J. Theor. Biol. 1989, 137, 91–105. [Google Scholar] [CrossRef]
- Minamitani, H.; Hagita, N. A Neural Network Model of Pain Mechanisms: Computer Simulation of the Central Neural Activities Essential for the Pain and Touch Sensations. Syst. Man Cybern. IEEE Trans. 1981, 11, 481–493. [Google Scholar] [CrossRef]
- Haeri, M.; Asemani, D.; Gharibzadeh, S. Modeling of pain using artificial neural networks. J. Theor. Biol. 2003, 220, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Timoshenko, S.P.; Goodier, J.N. Theory of Elasticity, 3rd ed.; McGraw-Hill: New York, NY, USA, 1970. [Google Scholar]
- Connor, J.A.; Stevens, C.F. Voltage clamp studies of a transient outward membrane current in gastropod neural somata. J. Physiol. 1971, 213, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.A.; Walter, D.; McKown, R. Neural repetitive firing: Modifications of the Hodgkin-Huxley axon suggested by experimental results from crustacean axons. Biophys. J. 1977, 18, 81–102. [Google Scholar] [CrossRef]
- James, N.C.; Richard, A.M. Cutaneous nociceptors. In Neurobiology of Nociceptors (edsC. Belmonte & F. Cervero); Oxford University Press: Oxford, UK, 1996; pp. 117–145. [Google Scholar]
- Xu, F.; Wen, T.; Lu, T.J.; Seffen, K.A. Modeling of nociceptor transduction in skin thermal pain sensation. J. Biomech. Eng. Trans. Asme 2008, 130, 041013. [Google Scholar] [CrossRef]
- Zhang, J.P.; Li, Y.H.; Xing, Y.F.; Song, J.Z. Three-dimensional thermomechanical analysis of epidermal electronic devices on human skin. Int. J. Solids Struct. 2019, 167, 48–57. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ji, D.; Shi, Y.; Chen, J.; Zhao, Z.; Zhao, G. Mathematical Model for Skin Pain Sensation under Local Distributed Mechanical Compression for Electronic Skin Applications. Micromachines 2022, 13, 1402. https://doi.org/10.3390/mi13091402
Ji D, Shi Y, Chen J, Zhao Z, Zhao G. Mathematical Model for Skin Pain Sensation under Local Distributed Mechanical Compression for Electronic Skin Applications. Micromachines. 2022; 13(9):1402. https://doi.org/10.3390/mi13091402
Chicago/Turabian StyleJi, Dongcan, Yingli Shi, Jiayun Chen, Zhao Zhao, and Guozhong Zhao. 2022. "Mathematical Model for Skin Pain Sensation under Local Distributed Mechanical Compression for Electronic Skin Applications" Micromachines 13, no. 9: 1402. https://doi.org/10.3390/mi13091402
APA StyleJi, D., Shi, Y., Chen, J., Zhao, Z., & Zhao, G. (2022). Mathematical Model for Skin Pain Sensation under Local Distributed Mechanical Compression for Electronic Skin Applications. Micromachines, 13(9), 1402. https://doi.org/10.3390/mi13091402





