Early Notice Pointer, an IoT-like Platform for Point-of-Care Feet and Body Balance Screening
Abstract
1. Introduction
2. Materials and Methods
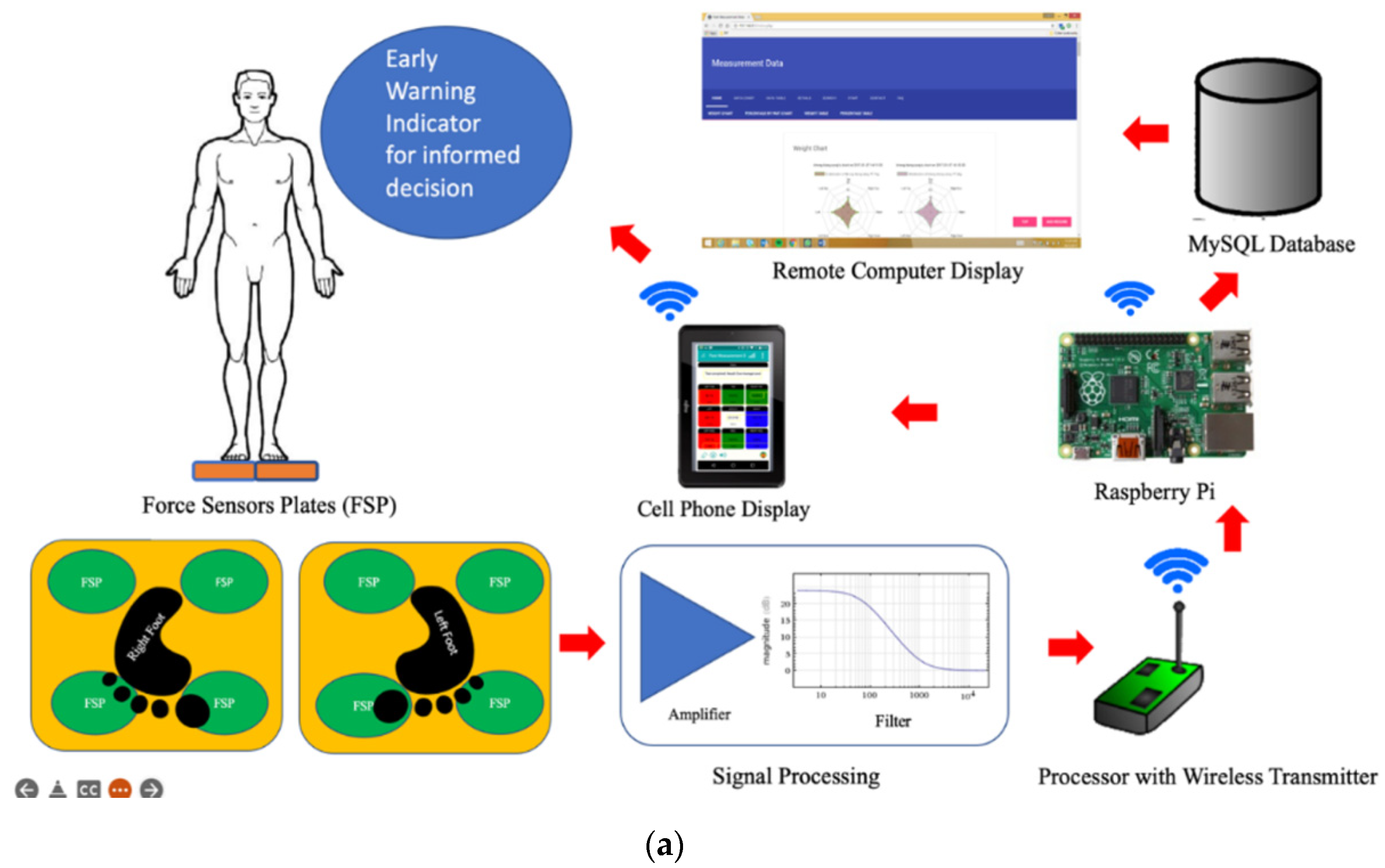
2.1. The Design of the Prototype
2.1.1. Materials Used to Design the Prototype
- Force Sensor Plates: Two identical force plates with compression load cells (ISVASIA SINGAPORE PTE LTD), used for measuring the left and right foot weight loads.
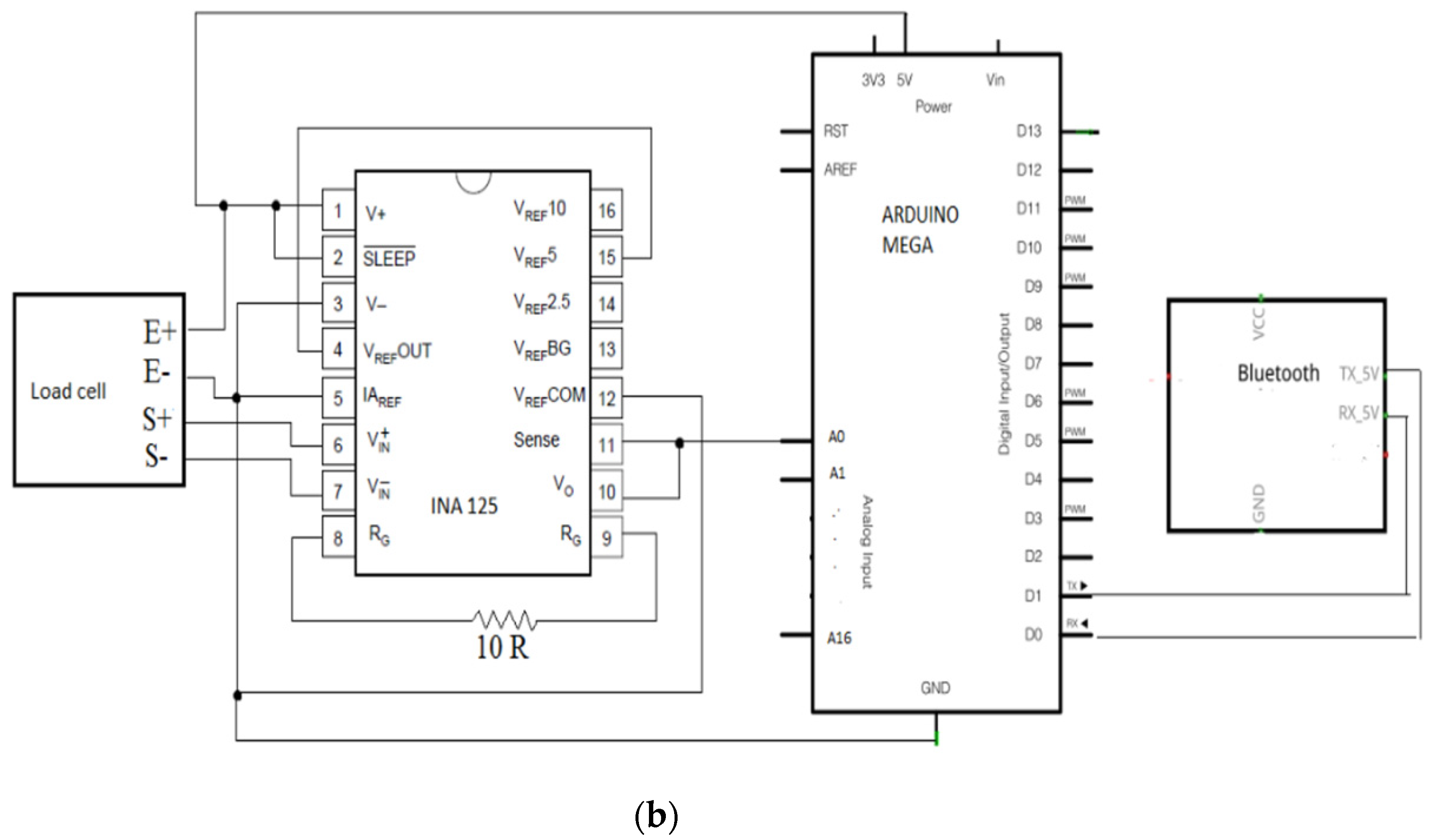
- Signal Processing: PCB with 8 INA125P (a 16-pin Instrumentation Amplifier) (Texas Instruments) to filter, amplify, and remove noise.
- Arduino Mega Development board with Wireless transmitter: uses 8 out of 16 analogue inputs (Arduino LLC).
- Cellphone/tablet Display: User interface for the measurement, analysis, and display of results.
- Remote Raspberry Pi for MySQL Databased: A pocket PC for hosting Database services for storage records for post-analysis (Adafruit Industry).
2.1.2. The Procedure to Design the Prototype
2.2. The Testing of the Prototype
2.2.1. Demographics
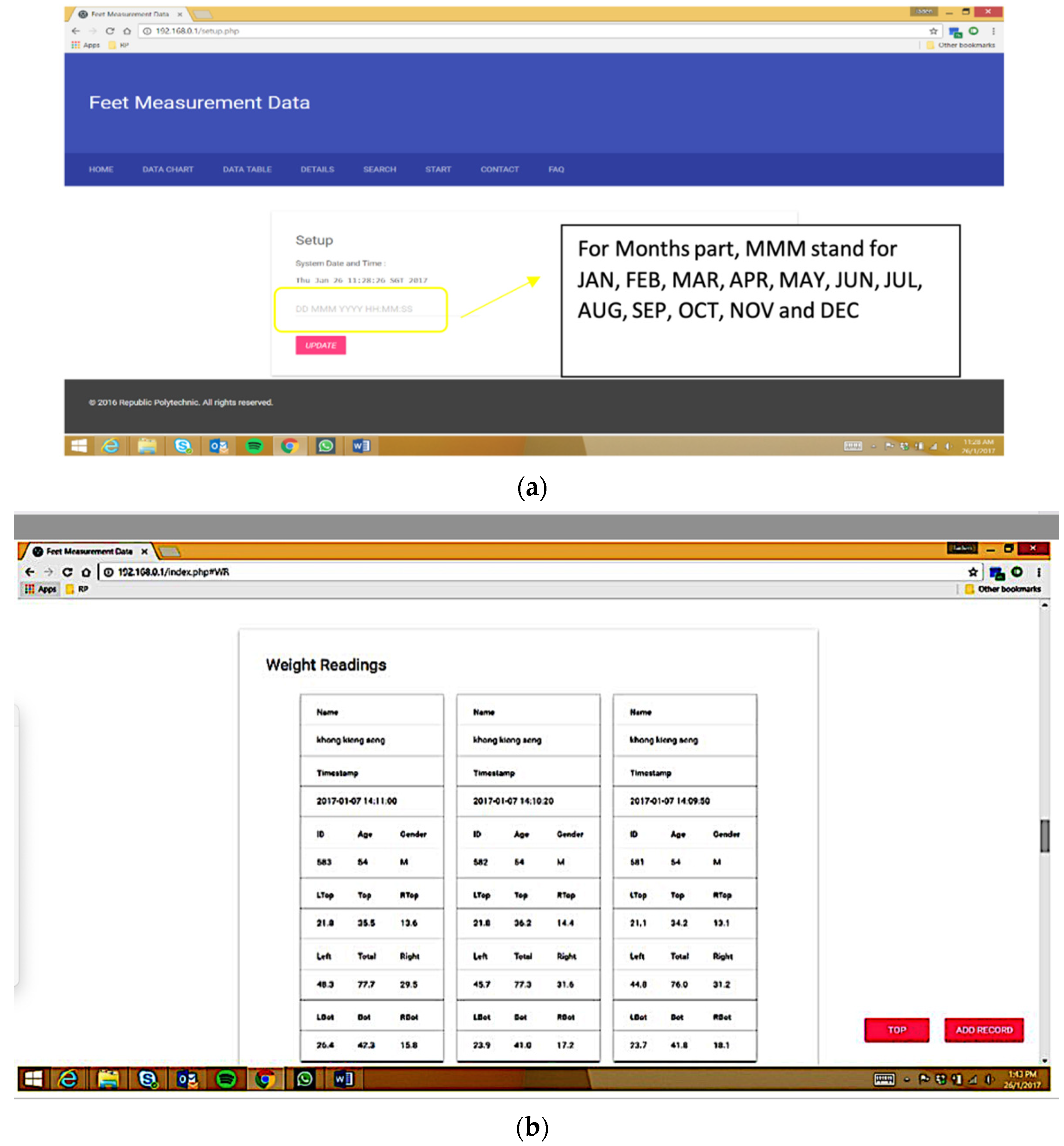
2.2.2. Data Acquisition
2.2.3. Data Analysis
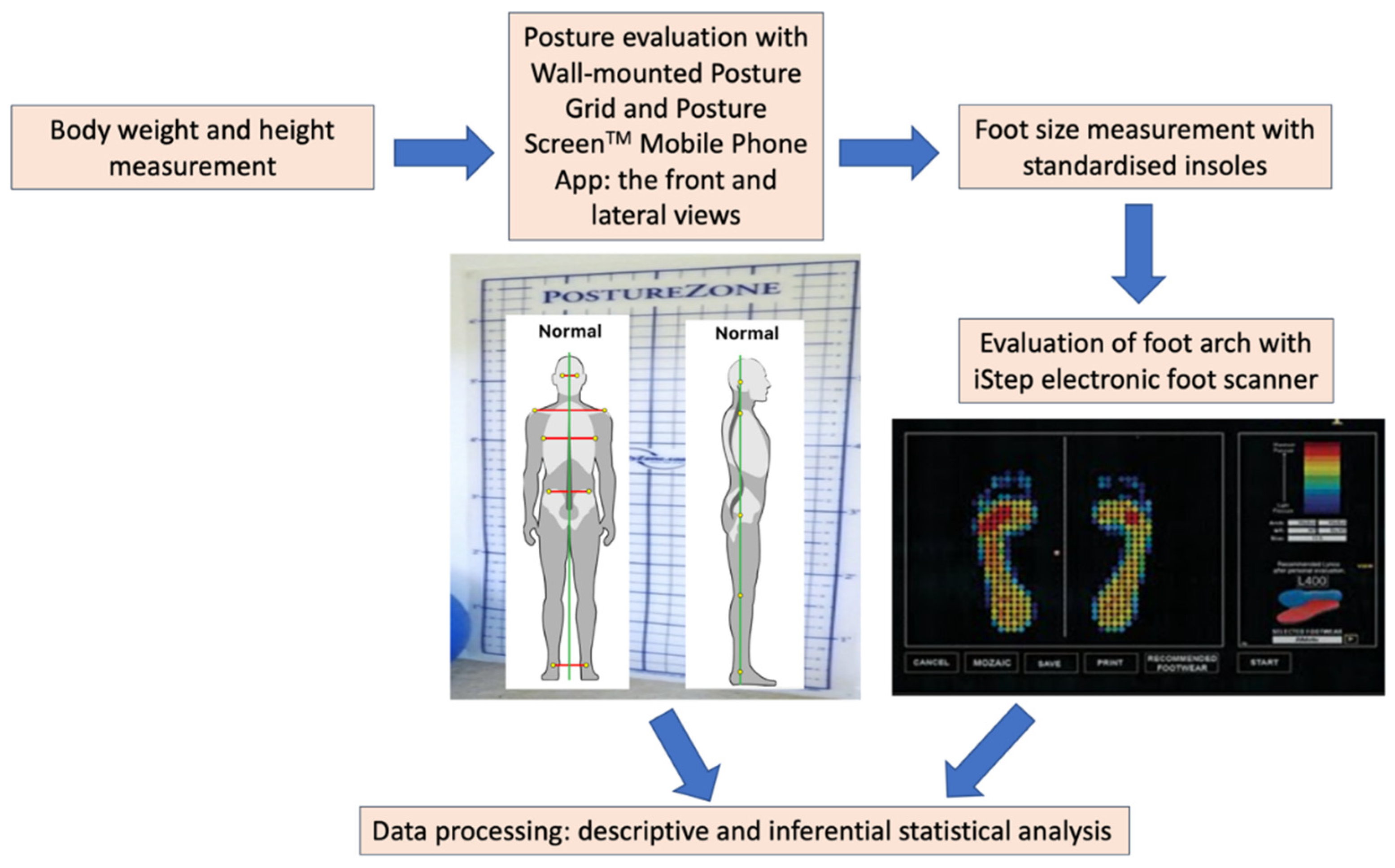
2.3. The Foot Arch and Balance Study
2.3.1. Demographics
2.3.2. Data Acquisition
2.3.3. Data Analysis
3. Results
- compares the load distribution between the two feet of a user,
- calculates the relative imbalance of the load distribution,
- issues an early warning if measurements exceed certain thresholds (the range of acceptable norms derived from the research data),
- ensures transmission of data in an IoT manner.
3.1. The Prototype
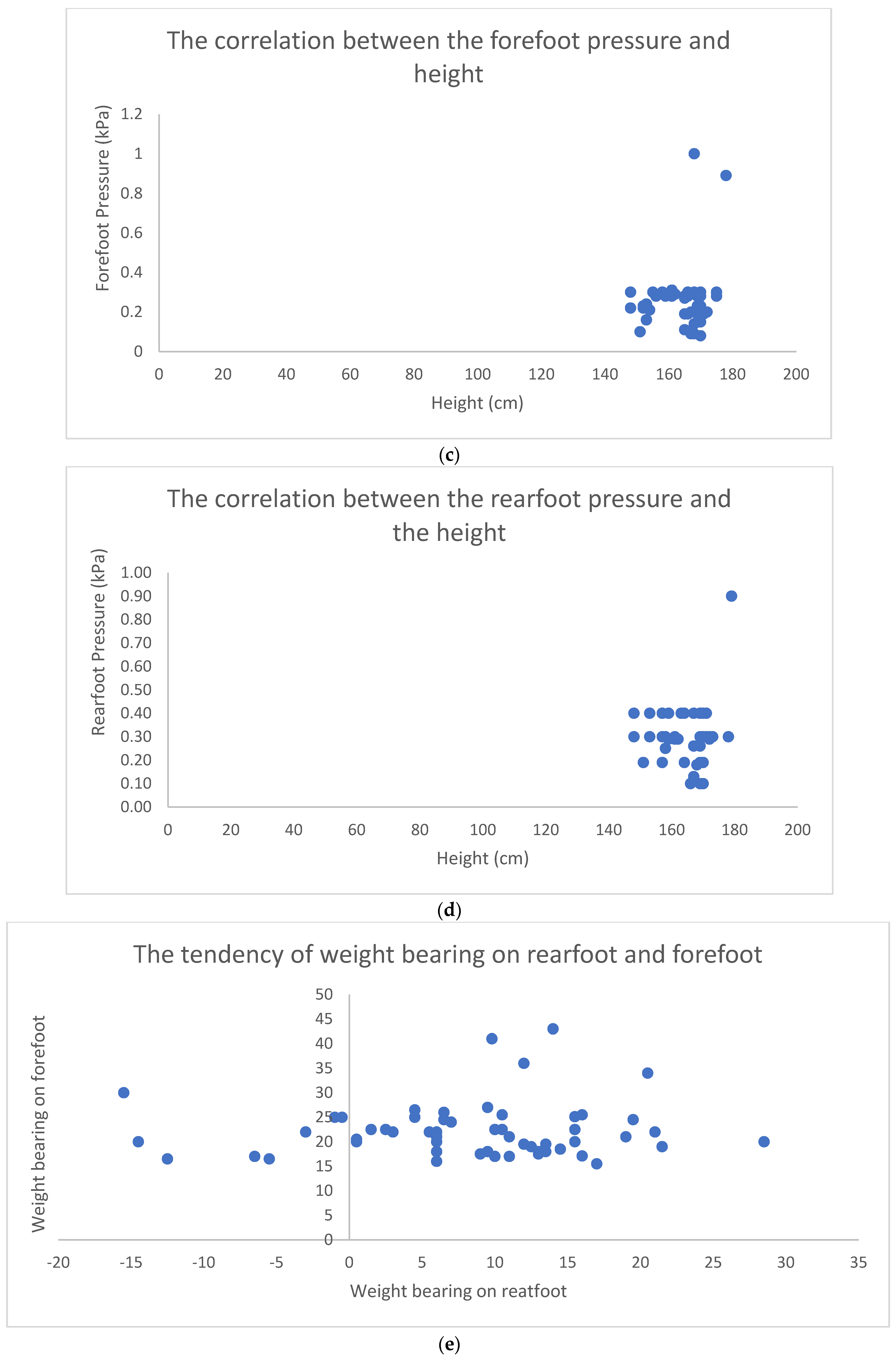
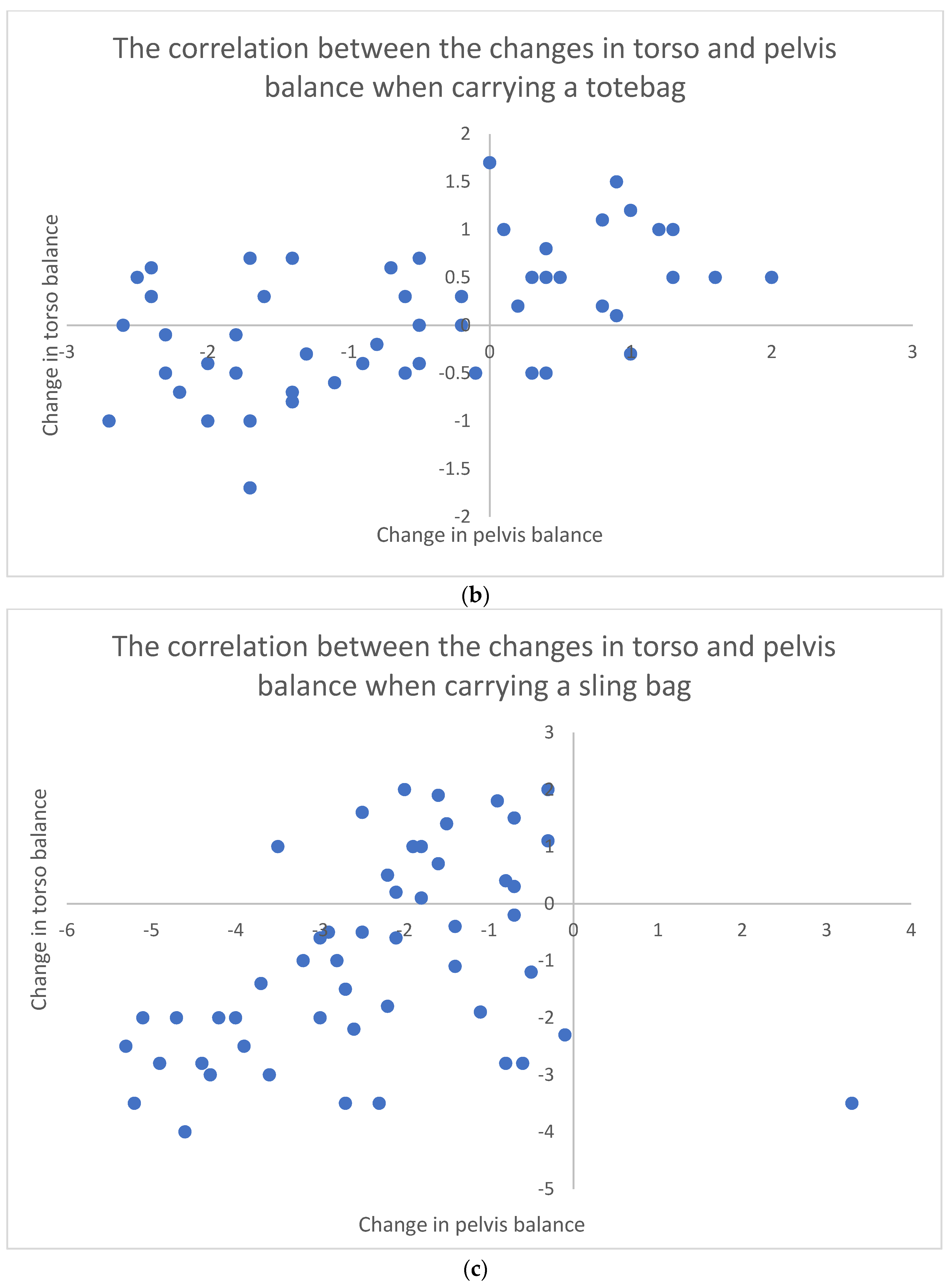
3.2. The Foot Arch and Balance Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Phillips, R.E. Foot. In The Physical Exam; Springer: Berlin/Heidelberg, Germany, 2018; pp. 237–244. [Google Scholar]
- López-López, D.; Vilar-Fernández, J.M.; Barros-García, G.; Losa-Iglesias, M.E.; Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R.; Calvo-Lobo, C. Foot arch height and quality of life in adults: A strobe observational study. Int. J. Environ. Res. Public Health 2018, 15, 1555. [Google Scholar] [CrossRef] [PubMed]
- Saito, I.; Okada, K.; Wakasa, M.; Abe, H.; Saito, A. Foot pressure pattern, hindfoot deformities, and their associations with foot pain in individuals with advanced medial knee osteoarthritis. Gait Posture 2018, 59, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, P.S.; Siddle, H.J. Pain in the Foot. ABC Rheumatol. 2018, 43, 50. [Google Scholar]
- Song, J.; Choe, K.; Neary, M.; Zifchock, R.A.; Cameron, K.L.; Trepa, M.; Hannan, M.T.; Hillstrom, H. Comprehensive biomechanical characterization of feet in USMA cadets: Comparison across race, gender, arch flexibility, and foot types. Gait Posture 2018, 60, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Gorter, K.J.; Kuyvenhoven, M.M.; de Melker, R.A. Nontraumatic foot complaints in older people. A population-based survey of risk factors, mobility, and well-being. J. Am. Podiatr. Med. Assoc. 2000, 90, 397–402. [Google Scholar] [CrossRef]
- Sung, P.S.; Zipple, J.T.; Andraka, J.M.; Danial, P. The kinetic and kinematic stability measures in healthy adult subjects with and without flat foot. Foot 2017, 30, 21–26. [Google Scholar] [CrossRef]
- Goldberg, D.S.; McGee, S.J. Pain as a global public health priority. BMC Public Health 2011, 11, 770. [Google Scholar] [CrossRef]
- Zemedikun, D.T.; Kigozi, J.; Wynne-Jones, G.; Guariglia, A.; Roberts, T. Methodological considerations in the assessment of direct and indirect costs of back pain: A systematic scoping review. PLoS ONE 2021, 16, e0251406. [Google Scholar] [CrossRef] [PubMed]
- Petty, N.J.; Ryder, D. Musculoskeletal Examination and Assessment E-Book: A Handbook for Therapists; Elsevier Health Sciences: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Hayes, K.W.; Johnson, M.E. Measures of adult general performance tests: The Berg Balance Scale, Dynamic Gait Index (DGI), Gait Velocity, Physical Performance Test (PPT), Timed Chair Stand Test, Timed Up and Go, and Tinetti Performance-Oriented Mobility Assessment (POMA). Arthritis Care Res. Off. J. Am. Coll. Rheumatol. 2003, 49, S28–S42. [Google Scholar] [CrossRef]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [PubMed]
- Wrisley, D.M.; Whitney, S.L. The effect of foot position on the modified clinical test of sensory interaction and balance. Arch. Phys. Med. Rehabil. 2004, 85, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Means, M.L.; Voss, J.F. Who reasons well? Two studies of informal reasoning among children of different grade, ability, and knowledge levels. Cogn. Instr. 1996, 14, 139–178. [Google Scholar] [CrossRef]
- Huxham, F.E.; Goldie, P.A.; Patla, A.E. Theoretical considerations in balance assessment. Aust. J. Physiother. 2001, 47, 89–100. [Google Scholar] [CrossRef]
- Chandler, J.M.; Duncan, P.W.; Studenski, S.A. Balance performance on the postural stress test: Comparison of young adults, healthy elderly, and fallers. Phys. Ther. 1990, 70, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Petró, B.; Papachatzopoulou, A.; Kiss, R.M. Devices and tasks involved in the objective assessment of standing dynamic balancing–A systematic literature review. PLoS ONE 2017, 12, e0185188. [Google Scholar] [CrossRef] [PubMed]
- Alahmari, K.A.; Marchetti, G.F.; Sparto, P.J.; Furman, J.M.; Whitney, S.L. Estimating postural control with the balance rehabilitation unit: Measurement consistency, accuracy, validity, and comparison with dynamic posturography. Arch. Phys. Med. Rehabil. 2014, 95, 65–73. [Google Scholar] [CrossRef]
- Dickin, D.C. Obtaining reliable performance measures on the sensory organization test: Altered testing sequences in young adults. Clin. J. Sport Med. 2010, 20, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Ford-Smith, C.D.; Wyman, J.F.; Elswick Jr, R.; Fernandez, T.; Newton, R.A. Test-retest reliability of the sensory organization test in noninstitutionalized older adults. Arch. Phys. Med. Rehabil. 1995, 76, 77–81. [Google Scholar] [CrossRef]
- Hebert, J.R.; Manago, M.M. Reliability and validity of the computerized dynamic posturography sensory organization test in people with multiple sclerosis. Int. J. MS Care 2017, 19, 151–157. [Google Scholar] [CrossRef]
- Chien, C.-W.; Hu, M.-H.; Tang, P.-F.; Sheu, C.-F.; Hsieh, C.-L. A comparison of psychometric properties of the smart balance master system and the postural assessment scale for stroke in people who have had mild stroke. Arch. Phys. Med. Rehabil. 2007, 88, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Jayakaran, P.; Johnson, G.M.; Sullivan, S.J. Test-retest reliability of the Sensory Organization Test in older persons with a transtibial amputation. PMR 2011, 3, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Leitner, C.; Mair, P.; Paul, B.; Wick, F.; Mittermaier, C.; Sycha, T.; Ebenbichler, G. Reliability of posturographic measurements in the assessment of impaired sensorimotor function in chronic low back pain. J. Electromyogr. Kinesiol. 2009, 19, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Ruhe, A.; Fejer, R.; Walker, B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: A systematic review of the literature. Eur. Spine J. 2011, 20, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Lafond, D.; Duarte, M.; Prince, F. Comparison of three methods to estimate the center of mass during balance assessment. J. Biomech. 2004, 37, 1421–1426. [Google Scholar] [CrossRef]
- Maatar, D.; Fournier, R.; Naitali, A.; Lachiri, Z. Effect analysis of age and gender on postural stability using PCA decomposition. In Proceedings of the 2011 IEEE Workshop on Signal Processing Systems (SiPS), Beirut, Lebanon, 4–7 October 2011; pp. 349–354. [Google Scholar]
- Ferber-Viart, C.; Ionescu, E.; Morlet, T.; Froehlich, P.; Dubreuil, C. Balance in healthy individuals assessed with Equitest: Maturation and normative data for children and young adults. Int. J. Pediatric Otorhinolaryngol. 2007, 71, 1041–1046. [Google Scholar] [CrossRef]
- Petry, V.K.; Paletta, J.R.; El-Zayat, B.F.; Efe, T.; Michel, N.S.; Skwara, A. Influence of a training session on postural stability and foot loading patterns in soccer players. Orthop. Rev. 2016, 8, 6360. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lowe, B.D.; Weir, P.; Andrews, D. Observation-based posture assessment: Review of current practice and recommendations for improvement. 2014. Available online: http://www.cdc.gov/niosh (accessed on 26 April 2022).
- Rizzuto, M.A.; Sonne, M.W.; Vignais, N.; Keir, P.J. Evaluation of a virtual reality head mounted display as a tool for posture assessment in digital human modelling software. Appl. Ergon. 2019, 79, 1–8. [Google Scholar] [CrossRef]
- Corichi-Herrejón, J.; Santiago-Pineda, A.; Montes-Gómez, B.; Juárez-Cruz, A.S.; Reyes-Zárate, G.G.; Moreno-Moreno, J.; Pérez-Rojas, D. Ergonomics Assessment Based on IoT Wearable Device. In Proceedings of the International Conference on Human Interaction and Emerging Technologies, Strasbourg, France, 28–30 April 2021; pp. 508–515. [Google Scholar]
- Fera, M.; Greco, A.; Caterino, M.; Gerbino, S.; Caputo, F.; Macchiaroli, R.; D’Amato, E. Towards digital twin implementation for assessing production line performance and balancing. Sensors 2020, 20, 97. [Google Scholar] [CrossRef]
- Zhu, H.; Podesva, P.; Liu, X.; Zhang, H.; Teply, T.; Xu, Y.; Chang, H.; Qian, A.; Lei, Y.; Li, Y. IoT PCR for pandemic disease detection and its spread monitoring. Sens. Actuators B Chem. 2020, 303, 127098. [Google Scholar] [CrossRef] [PubMed]
- Matar, G.; Lina, J.-M.; Carrier, J.; Riley, A.; Kaddoum, G. Internet of Things in sleep monitoring: An application for posture recognition using supervised learning. In Proceedings of the 2016 IEEE 18th international conference on e-health networking, applications and services (Healthcom), Munich, Germany, 14–17 September 2016; pp. 1–6. [Google Scholar]
- Anwary, A.R.; Cetinkaya, D.; Vassallo, M.; Bouchachia, H. Smart-Cover: A real time sitting posture monitoring system. Sens. Actuators A Phys. 2021, 317, 112451. [Google Scholar] [CrossRef]
- Iliescu, F.S.; Ionescu, A.M.; Gogianu, L.; Simion, M.; Dediu, V.; Chifiriuc, M.C.; Pircalabioru, G.G.; Iliescu, C. Point-of-Care Testing-the Key in the Battle against SARS-CoV-2 Pandemic. Micromachines 2021, 12, 1464. [Google Scholar] [CrossRef]
- Beaugerie, L.; Kirchgesner, J. Balancing benefit vs risk of immunosuppressive therapy for individual patients with inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 2019, 17, 370–379. [Google Scholar] [CrossRef]
- Langaee, T.; Wagner, R.; Horne, L.P.; Lawson, L.A.; Becker, C.; Shahin, M.; Starostik, P.; Stacpoole, P.W. Personalized dosing of dichloroacetate using GSTZ1 clinical genotyping assay. Genet. Test. Mol. Biomark. 2018, 22, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm (accessed on 12 January 2022).
- Available online: https://www.breastcancer.org/symptoms/testing/types/mammaprint (accessed on 12 January 2022).
- Zasowski, E.J.; Lodise, T.P. The importance of individualized vancomycin dosing to ensure optimal exposure early in therapy. J. Clin. Pharmacol. 2018, 58, 1131–1133. [Google Scholar] [CrossRef] [PubMed]
- Bredenberg, S.; Nyholm, D.; Aquilonius, S.-M.; Nyström, C. An automatic dose dispenser for microtablets—a new concept for individual dosage of drugs in tablet form. Int. J. Pharm. 2003, 261, 137–146. [Google Scholar] [CrossRef]
- Guo, H.; Lan, C.; Zhou, Z.; Sun, P.; Wei, D.; Li, C. Transparent, flexible, and stretchable WS 2 based humidity sensors for electronic skin. Nanoscale 2017, 9, 6246–6253. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.-K.; Myoung, J.-M. Wearable and Semitransparent Pressure-Sensitive Light-Emitting Sensor Based on Electrochemiluminescence. ACS Nano 2020, 14, 8716–8723. [Google Scholar] [CrossRef]
- Dahiya, R. E-skin: From humanoids to humans [point of view]. Proc. IEEE 2019, 107, 247–252. [Google Scholar] [CrossRef]
- Cai, G.; Wang, J.; Lin, M.-F.; Chen, J.; Cui, M.; Qian, K.; Li, S.; Cui, P.; Lee, P.S. A semitransparent snake-like tactile and olfactory bionic sensor with reversibly stretchable properties. NPG Asia Mater. 2017, 9, e437. [Google Scholar] [CrossRef]
- Chen, X.; Luo, F.; Yuan, M.; Xie, D.; Shen, L.; Zheng, K.; Wang, Z.; Li, X.; Tao, L.Q. A dual-functional graphene-based self-alarm health-monitoring E-skin. Adv. Funct. Mater. 2019, 29, 1904706. [Google Scholar] [CrossRef]
- Niu, S.; Matsuhisa, N.; Beker, L.; Li, J.; Wang, S.; Wang, J.; Jiang, Y.; Yan, X.; Yun, Y.; Burnett, W.; et al. A wireless body area sensor network based on stretchable passive tags. Nat. Electron. 2019, 2, 361–368. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Yang, T.; Li, X.; Zang, X.; Zhu, M.; Wang, K.; Wu, D.; Zhu, H. Wearable and highly sensitive graphene strain sensors for human motion monitoring. Adv. Funct. Mater. 2014, 24, 4666–4670. [Google Scholar] [CrossRef]
- Dagdeviren, C.; Su, Y.; Joe, P.; Yona, R.; Liu, Y.; Kim, Y.-S.; Huang, Y.; Damadoran, A.R.; Xia, J.; Martin, L.W. Conformable amplified lead zirconate titanate sensors with enhanced piezoelectric response for cutaneous pressure monitoring. Nat. Commun. 2014, 5, 4496. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.; Tee, B.C.-K.; Mei, J.; Appleton, A.L.; Kim, D.H.; Wang, H.; Bao, Z. Flexible polymer transistors with high pressure sensitivity for application in electronic skin and health monitoring. Nat. Commun. 2013, 4, 1859. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Haghighi, P.D.; Burstein, F.; Yap, L.W.; Cheng, W.; Yao, L.; Cicuttini, F. Electronic skin wearable sensors for detecting Lumbar–Pelvic movements. Sensors 2020, 20, 1510. [Google Scholar] [CrossRef]
- Zaltieri, M.; Massaroni, C.; Lo Presti, D.; Bravi, M.; Sabbadini, R.; Miccinilli, S.; Sterzi, S.; Formica, D.; Schena, E. A Wearable Device Based on a Fiber Bragg Grating Sensor for Low Back Movements Monitoring. Sensors 2020, 20, 3825. [Google Scholar] [CrossRef]
- Frediani, G.; Botondi, B.; Quartini, L.; Zonfrillo, G.; Bocchi, L.; Carpi, F. Wearable kinematic monitoring system based on piezocapacitive sensors. In pHealth 2019; IOS Press: Amsterdam, The Netherlands, 2019; pp. 103–108. [Google Scholar]
- Ezeukwu, A.; Orji, E.; Okezue, O.; Ezugwu, U. Foot Anthropometric Measurement of Primary School Children With and Without Flatfoot: A Comparative Study. Online J. Health Allied Sci. 2018, 17, 10. [Google Scholar]
- Allum, J.H.; Carpenter, M.G. A speedy solution for balance and gait analysis: Angular velocity measured at the centre of body mass. Curr. Opin. Neurol. 2005, 18, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, N.; Warabi, T.; Kato, M.; Kiriyama, K.; Yoshida, T.; Chiba, S. Posterior-anterior body weight shift during stance period studied by measuring sole-floor reaction forces during healthy and hemiplegic human walking. Neurosci. Lett. 2006, 399, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Darekar, A.; McFadyen, B.J.; Lamontagne, A.; Fung, J. Efficacy of virtual reality-based intervention on balance and mobility disorders post-stroke: A scoping review. J. Neuroeng. Rehabil. 2015, 12, 46. [Google Scholar] [CrossRef] [PubMed]
- Elena, S.; Georgeta, N.; Cecilia, G.; Elena, L. Identification of the Balance Capability–A Perceptual-motor Component-in Teenagers. Procedia-Soc. Behav. Sci. 2014, 127, 260–264. [Google Scholar] [CrossRef]
- Verma, S.; Kumar, D.; Kumawat, A.; Dutta, A.; Lahiri, U. A low-cost adaptive balance training platform for stroke patients: A usability study. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 935–944. [Google Scholar] [CrossRef]
- Periyasamy, R.; Anand, S. The effect of foot arch on plantar pressure distribution during standing. J. Med. Eng. Technol. 2013, 37, 342–347. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Whitney, S.; Hudak, M.; Marchetti, G. The dynamic gait index relates to self-reported fall history in individuals with vestibular dysfunction. J. Vestib. Res. 2000, 10, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kendall, J.C.; Bird, A.R.; Azari, M.F. Foot posture, leg length discrepancy and low back pain–Their relationship and clinical management using foot orthoses–An overview. Foot 2014, 24, 75–80. [Google Scholar] [CrossRef]
- Raeissadat, S.A.; Sedighipour, L.; Pournajaf, S.; Vahab Kashani, R.; Sadeghi, S. Effect of posture training with weighted kypho-orthosis (WKO) on improving balance in women with osteoporosis. J. Aging Res. 2014, 2014, 427903. [Google Scholar] [CrossRef][Green Version]
- Buchbinder, R. Plantar fasciitis. N. Engl. J. Med. 2004, 350, 2159–2166. [Google Scholar] [CrossRef]
- Drew, T.; Prentice, S.; Schepens, B. Cortical and brainstem control of locomotion. Prog. Brain Res. 2004, 143, 251–261. [Google Scholar] [PubMed]
- Aboutorabi, A.; Arazpour, M.; Bahramizadeh, M.; Hutchins, S.W.; Fadayevatan, R. The effect of aging on gait parameters in able-bodied older subjects: A literature review. Aging Clin. Exp. Res. 2016, 28, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; Schlueter, H.; El-Gohary, M.; Mattek, N.; Duncan, C.; Kaye, J.; Horak, F.B. Continuous monitoring of turning mobility and its association to falls and cognitive function: A pilot study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2016, 71, 1102–1108. [Google Scholar] [CrossRef]
- Fuller, G.F. Falls in the elderly. Am. Fam. Physician 2000, 61, 2159. [Google Scholar]
- Muir, S.W.; Gopaul, K.; Montero Odasso, M.M. The role of cognitive impairment in fall risk among older adults: A systematic review and meta-analysis. Age Ageing 2012, 41, 299–308. [Google Scholar] [CrossRef]
- Robinovitch, S.N.; Feldman, F.; Yang, Y.; Schonnop, R.; Leung, P.M.; Sarraf, T.; Sims-Gould, J.; Loughin, M. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet 2013, 381, 47–54. [Google Scholar] [CrossRef]
- Aggarwal, N.; Anand, T.; Kishore, J.; Ingle, G.K. Low back pain and associated risk factors among undergraduate students of a medical college in Delhi. Educ. Health 2013, 26, 103. [Google Scholar]
- Lowe, T.G.; Line, B.G. Evidence based medicine: Analysis of Scheuermann kyphosis. Spine 2007, 32, S115–S119. [Google Scholar] [CrossRef]
- Szczygieł, E.; Zielonka, K.; Mętel, S.; Golec, J. Musculo-skeletal and pulmonary effects of sitting position–a systematic review. Ann. Agric. Environ. Med. 2017, 24, 8–12. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Stoltenberg, B.E.; Collinsworth, K.M.; Giesel, C.L.; Williams, D.G.; Kardouni, C.H.; Molloy, J.M.; Goffar, S.L.; Christie, D.S.; McPoil, T. Dynamic plantar pressure parameters associated with static arch height index during gait. Clin. Biomech. 2009, 24, 391–396. [Google Scholar] [CrossRef]
- Walker, M.; Fan, H.-J. Relationship between foot pressure pattern and foot type. Foot Ankle Int. 1998, 19, 379–383. [Google Scholar] [CrossRef]
- Xiong, S.; Goonetilleke, R.S.; Witana, C.P.; Weerasinghe, T.W.; Au, E.Y.L. Foot arch characterization: A review, a new metric, and a comparison. J. Am. Podiatr. Med. Assoc. 2010, 100, 14–24. [Google Scholar]
- Benvenuti, F.; Ferrucci, L.; Guralnik, J.M.; Gangemi, S.; Baroni, A. Foot pain and disability in older persons: An epidemiologic survey. J. Am. Geriatr. Soc. 1995, 43, 479–484. [Google Scholar] [CrossRef]
- Cho, K.; Lee, K.; Lee, B.; Lee, H.; Lee, W. Relationship between postural sway and dynamic balance in stroke patients. J. Phys. Ther. Sci. 2014, 26, 1989–1992. [Google Scholar] [CrossRef] [PubMed]
- Golightly, Y.M.; Hannan, M.T.; Dufour, A.B.; Hillstrom, H.J.; Jordan, J.M. Foot disorders associated with overpronated and oversupinated foot function: The Johnston County osteoarthritis project. Foot Ankle Int. 2014, 35, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Dawe, R.J.; Leurgans, S.E.; Yang, J.; Bennett, J.M.; Hausdorff, J.M.; Lim, A.S.; Gaiteri, C.; Bennett, D.A.; Buchman, A.S. Association between quantitative gait and balance measures and total daily physical activity in community-dwelling older adults. J. Gerontol. Ser. A 2018, 73, 636–642. [Google Scholar] [CrossRef]
- Fjeldstad, C.; Pardo, G.; Bemben, D.; Bemben, M. Decreased postural balance in multiple sclerosis patients with low disability. Int. J. Rehabil. Res. 2011, 34, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Lin, X.; Li, C.; Zhao, Y.; Yu, Z.; Han, X. Sagittal imbalance of the spine is associated with poor sitting posture among primary and secondary school students in China: A cross-sectional study. BMC Musculoskelet. Disord. 2022, 23, 98. [Google Scholar] [CrossRef]
- Pokorska-Bocci, A.; Kroese, M.; Sagoo, G.S.; Hall, A.; Burton, H. Personalised medicine in the UK: Challenges of implementation and impact on healthcare system. Genome Med. 2014, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Pircalabioru, G.G.; Iliescu, F.S.; Mihaescu, G.; Cucu, A.I.; Ionescu, O.N.; Popescu, M.; Simion, M.; Burlibasa, L.; Tica, M.; Chifiriuc, M.C.; et al. Advances in the Rapid Diagnostic of Viral Respiratory Tract Infections. Front. Cell. Infect. Microbiol. 2022, 12, 807253. [Google Scholar] [CrossRef] [PubMed]
- Bunea, A.-C.; Dediu, V.; Laszlo, E.A.; Pistriţu, F.; Carp, M.; Iliescu, F.S.; Ionescu, O.N.; Iliescu, C. E-Skin: The Dawn of a New Era of On-Body Monitoring Systems. Micromachines 2021, 12, 1091. [Google Scholar] [CrossRef] [PubMed]
- Boutry, C.M.; Beker, L.; Kaizawa, Y.; Vassos, C.; Tran, H.; Hinckley, A.C.; Pfattner, R.; Niu, S.; Li, J.; Claverie, J. Biodegradable and flexible arterial-pulse sensor for the wireless monitoring of blood flow. Nat. Biomed. Eng. 2019, 3, 47–57. [Google Scholar] [CrossRef]
- Liu, X.; Wei, Y.; Qiu, Y. Advanced Flexible Skin-Like Pressure and Strain Sensors for Human Health Monitoring. Micromachines 2021, 12, 695. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.S.; Lee, C.H.; Kim, N.K.; An, T.; Kim, G.H. Sensors for Biosignal/Health Monitoring in Electronic Skin. Polymers 2021, 13, 2478. [Google Scholar] [CrossRef]



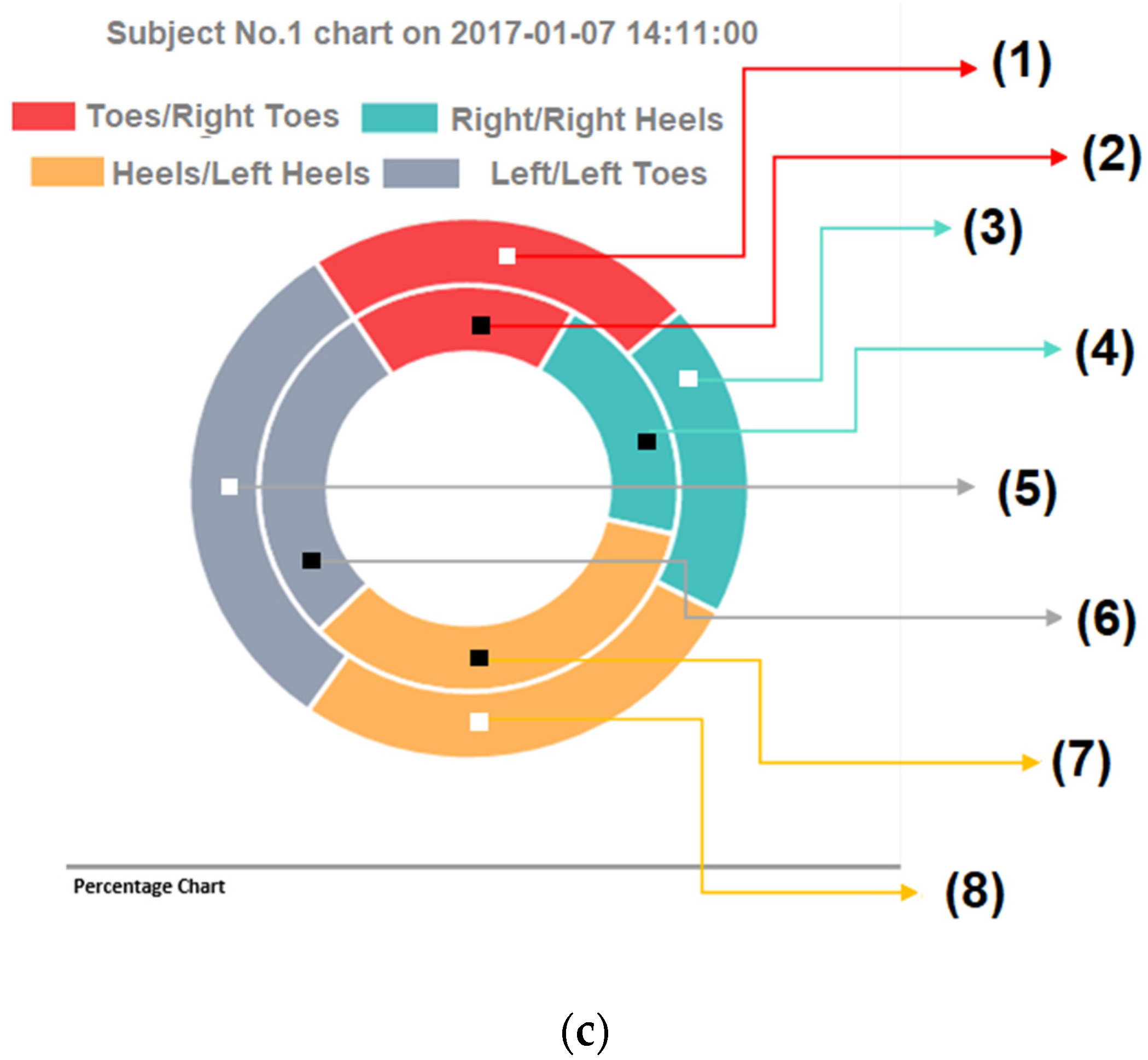



| Red Point >= 2: Above Average Level | ||
|---|---|---|
| Blue Point > 2: Below Average Level | ||
| Red Point < 2 or Blue <= 2: Average Level | ||
| >=7.9% | >=16.1% | >=7.9% |
| <=4.9% | <=10.1% | <=4.9% |
| Best = 6.4%, <7.9% And >4.9% | Best = 13.1%, <16.1% and >10.1% | Best = 6.4%, Not < 7.9% and >4.9% |
| Any correct colour value will be given 1 point | Any correct colour value will be given 2 points | Any correct colour value will be given 1 point |
| >=19.8% | Weight Value | >=19.5% |
| <=13.8% | <=13.5% | |
| Best = 16.8%, <19.8% And >13.80% | Best = 16.5%, <19.5% and >13.5% | |
| Any correct colour value will be given 2 points | Any correct colour value will be given 2 points | |
| >=11.6% | >=23.2% | >=11.3% |
| <=8.6% | <=17.2% | <=8.3% |
| Best = 10.1%, <11.6 And >8.6% | Best = 20.2%, <23.2% and > 17.2% | Best = 9.8%, <11.3% and >8.3% |
| Any correct colour value will be given 1 point | Any correct colour value will be given 2 points | Any correct colour value will be given 1 point |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iliescu, F.S.; Hong, L.T.; Toh, J.M.J.; Suchea, M.P.; Ionescu, O.N.; Iliescu, C. Early Notice Pointer, an IoT-like Platform for Point-of-Care Feet and Body Balance Screening. Micromachines 2022, 13, 682. https://doi.org/10.3390/mi13050682
Iliescu FS, Hong LT, Toh JMJ, Suchea MP, Ionescu ON, Iliescu C. Early Notice Pointer, an IoT-like Platform for Point-of-Care Feet and Body Balance Screening. Micromachines. 2022; 13(5):682. https://doi.org/10.3390/mi13050682
Chicago/Turabian StyleIliescu, Florina Silvia, Ling Tim Hong, Jin Ming Jaden Toh, Mirela Petruta Suchea, Octavian Narcis Ionescu, and Ciprian Iliescu. 2022. "Early Notice Pointer, an IoT-like Platform for Point-of-Care Feet and Body Balance Screening" Micromachines 13, no. 5: 682. https://doi.org/10.3390/mi13050682
APA StyleIliescu, F. S., Hong, L. T., Toh, J. M. J., Suchea, M. P., Ionescu, O. N., & Iliescu, C. (2022). Early Notice Pointer, an IoT-like Platform for Point-of-Care Feet and Body Balance Screening. Micromachines, 13(5), 682. https://doi.org/10.3390/mi13050682








