A Novel Microfluidic Device for Blood Plasma Filtration
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Sample Preparation
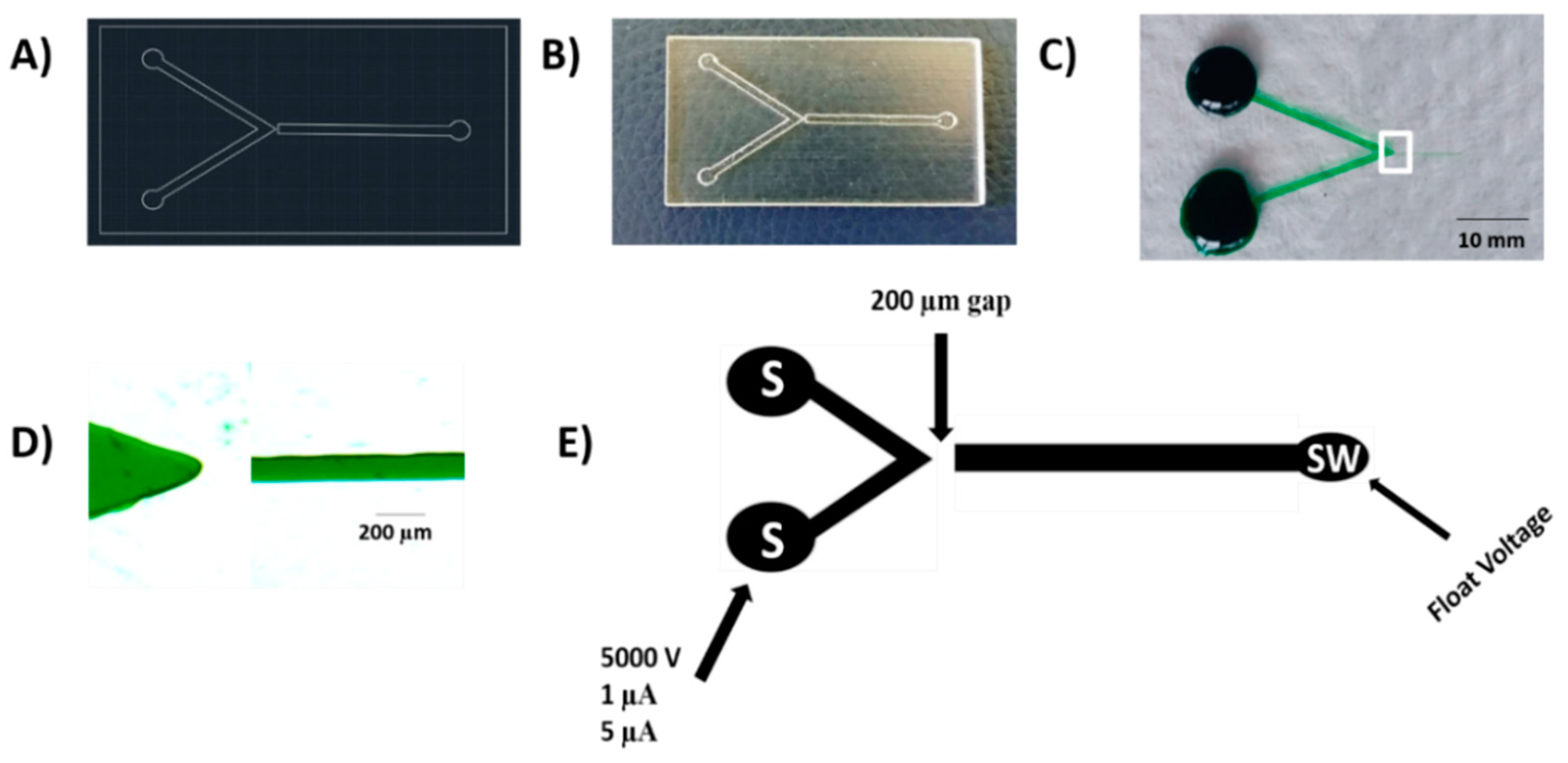
2.2. Device Fabrication
2.3. Creation of a Nano-Junction
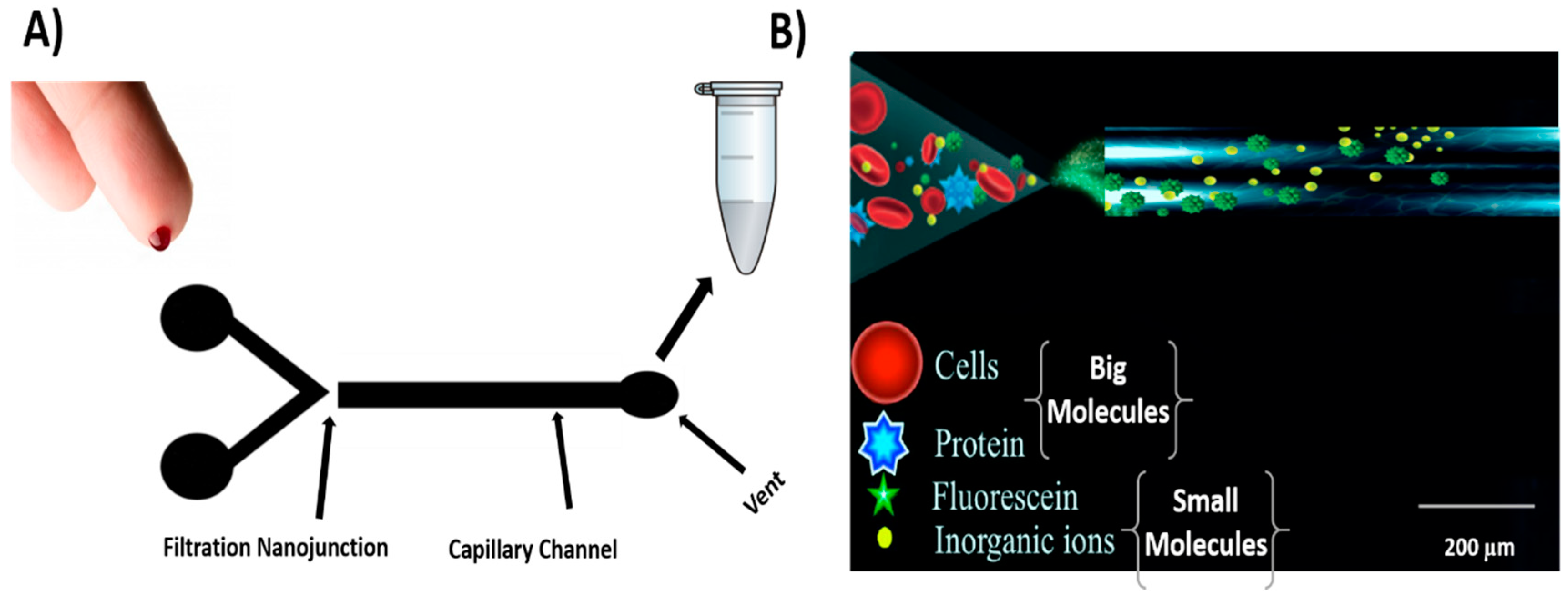
2.4. Device Operation and Experimental Practice
3. Results and Discussion
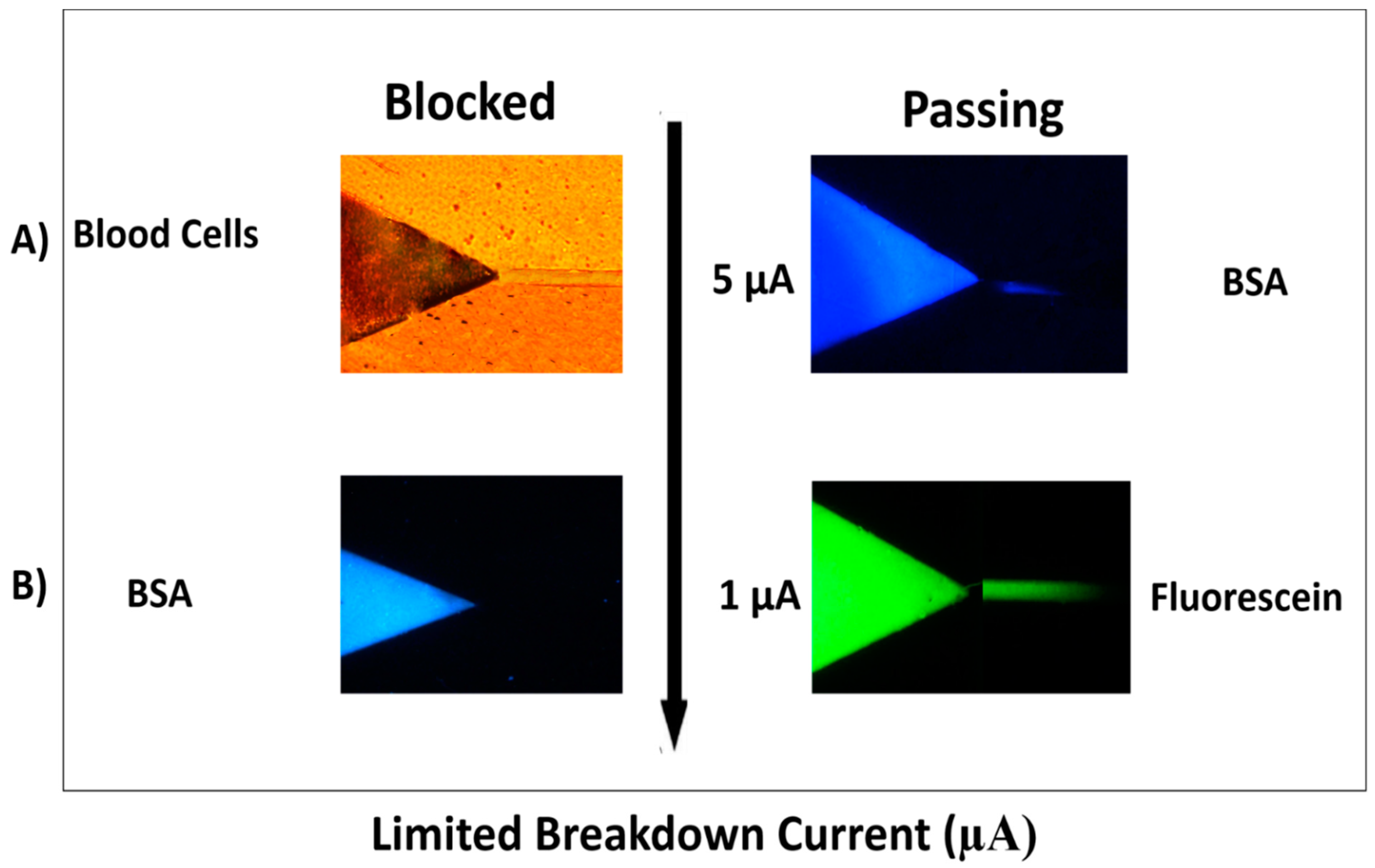
3.1. Filtration and Permeability Studies
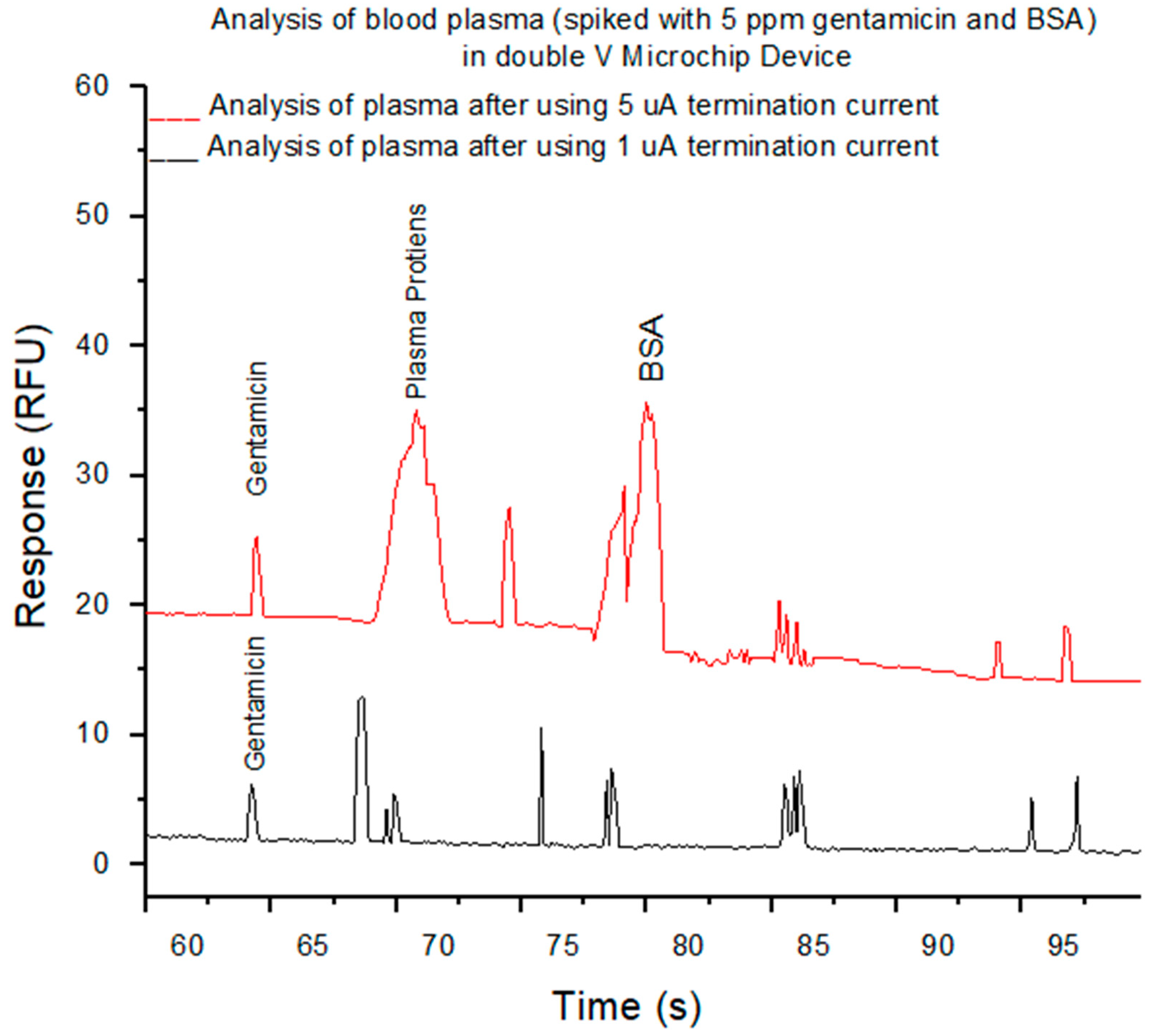
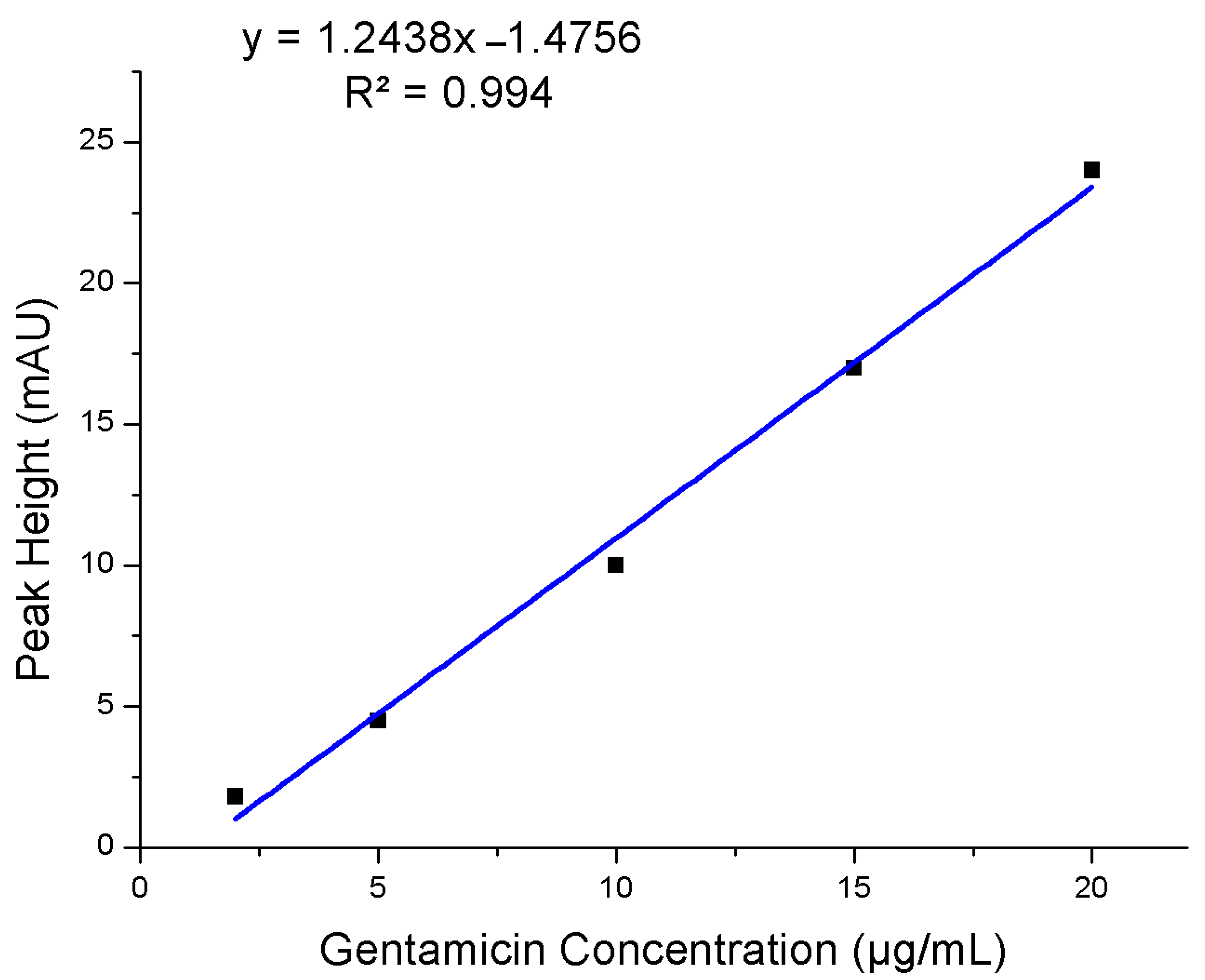
3.2. Analysis of Filtered Blood Plasma
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kersaudy-Kerhoas, M.; Sollier, E. Micro-scale blood plasma separation: From acoustophoresis to egg-beaters. Lab Chip 2013, 13, 3323–3346. [Google Scholar] [CrossRef]
- Mielczarek, W.S.; Obaje, E.; Bachmann, T.; Kersaudy-Kerhoas, M. Microfluidic blood plasma separation for medical diagnostics: Is it worth it? Lab Chip 2016, 16, 3441–3448. [Google Scholar] [CrossRef] [PubMed]
- Sturm, R.; Henion, J.; Abbott, R.; Wang, P. Novel membrane devices and their potential utility in blood sample collection prior to analysis of dried plasma spots. Bioanalysis 2015, 7, 1987–2002. [Google Scholar] [CrossRef]
- Emmons, G.; Rowland, M. Pharmacokinetic considerations as to when to use dried blood spot sampling. Bioanalysis 2010, 2, 1791–1796. [Google Scholar] [CrossRef]
- Neugebauer, S.; Giamarellos-Bourboulis, E.J.; Pelekanou, A.; Marioli, A.; Baziaka, F.; Tsangaris, I.; Bauer, M.; Kiehntopf, M. Metabolite profiles in sepsis: Developing prognostic tools based on the type of infection. Crit. Care Med. 2016, 44, 1649–1662. [Google Scholar] [CrossRef] [PubMed]
- Cheng, G. Circulating miRNAs: Roles in cancer diagnosis, prognosis and therapy. Adv. Drug Deliv. Rev. 2015, 81, 75–93. [Google Scholar] [CrossRef]
- Olsson, B.; Lautner, R.; Andreasson, U.; Öhrfelt, A.; Portelius, E.; Bjerke, M.; Hölttä, M.; Rosén, C.; Olsson, C.; Strobel, G. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: A systematic review and meta-analysis. Lancet Neurol. 2016, 15, 673–684. [Google Scholar] [CrossRef]
- Crowley, T.A.; Pizziconi, V. Isolation of plasma from whole blood using planar microfilters for lab-on-a-chip applications. Lab Chip 2005, 5, 922–929. [Google Scholar] [CrossRef]
- Kim, J.-H.; Woenker, T.; Adamec, J.; Regnier, F.E. Simple, miniaturized blood plasma extraction method. Anal. Chem. 2013, 85, 11501–11508. [Google Scholar] [CrossRef] [PubMed]
- Lei, B.U.; Prow, T.W. A review of microsampling techniques and their social impact. Biomed. Microdevices 2019, 21, 81. [Google Scholar] [CrossRef] [PubMed]
- Sollier, E.; Cubizolles, M.; Faivre, M.; Fouillet, Y.; Achard, J.L. A passive microfluidic device for plasma extraction from whole human blood. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2009, 2009, 7030–7033. [Google Scholar] [CrossRef] [PubMed]
- Berlanda, S.F.; Breitfeld, M.; Dietsche, C.L.; Dittrich, P.S. Recent Advances in Microfluidic Technology for Bioanalysis and Diagnostics. Anal. Chem. 2021, 93, 311–331. [Google Scholar] [CrossRef]
- Thorslund, S.; Klett, O.; Nikolajeff, F.; Markides, K.; Bergquist, J. A hybrid poly (dimethylsiloxane) microsystem for on-chip whole blood filtration optimized for steroid screening. Biomed. Microdevices 2006, 8, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Kim, S.-H.; Kim, D.; Park, S.-J.; Park, J.-K. Plasma extraction in a capillary-driven microfluidic device using surfactant-added poly (dimethylsiloxane). Sens. Actuators B Chem. 2010, 145, 861–868. [Google Scholar] [CrossRef]
- Homsy, A.; van der Wal, P.D.; Doll, W.; Schaller, R.; Korsatko, S.; Ratzer, M.; Ellmerer, M.; Pieber, T.R.; Nicol, A.; De Rooij, N.F. Development and validation of a low cost blood filtration element separating plasma from undiluted whole blood. Biomicrofluidics 2012, 6, 012804. [Google Scholar] [CrossRef]
- Zhang, H.; Li, G.; Liao, L.; Mao, H.; Jin, Q.; Zhao, J. Direct detection of cancer biomarkers in blood using a “place n play” modular polydimethylsiloxane pump. Biomicrofluidics 2013, 7, 034105. [Google Scholar] [CrossRef] [PubMed]
- Albukhaty, S.; Al-Musawi, S.; Abdul Mahdi, S.; Sulaiman, G.M.; Alwahibi, M.S.; Dewir, Y.H.; Soliman, D.A.; Rizwana, H. Investigation of Dextran-Coated Superparamagnetic Nanoparticles for Targeted Vinblastine Controlled Release, Delivery, Apoptosis Induction, and Gene Expression in Pancreatic Cancer Cells. Molecules 2020, 25, 4721. [Google Scholar] [CrossRef]
- Li, X.; Chen, W.; Liu, G.; Lu, W.; Fu, J. Continuous-flow microfluidic blood cell sorting for unprocessed whole blood using surface-micromachined microfiltration membranes. Lab Chip 2014, 14, 2565–2575. [Google Scholar] [CrossRef] [PubMed]
- Beebe, D.J.; Mensing, G.A.; Walker, G.M. Physics and applications of microfluidics in biology. Annu. Rev. Biomed. Eng. 2002, 4, 261–286. [Google Scholar] [CrossRef]
- Blattert, C.; Jurischka, R.; Schoth, A.; Kerth, P.; Menz, W. Separation of Blood Cells and Plasma in Microchannel Bend Structures. In Proceedings of the International Society for Optical Engineering 5591, Lab-on-a-Chip: Platforms, Devices, and Applications, Philadelphia, PA, USA, 8 December 2004; pp. 143–151. [Google Scholar]
- Nilsson, A.; Petersson, F.; Jönsson, H.; Laurell, T. Acoustic control of suspended particles in micro fluidic chips. Lab Chip 2004, 4, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, C.C.; Li, H. Microfluidic chip for blood cell separation and collection based on crossflow filtration. Sens. Actuators B Chem. 2008, 130, 216–221. [Google Scholar] [CrossRef]
- Gascoyne, P.R.; Vykoukal, J. Particle separation by dielectrophoresis. Electrophoresis 2002, 23, 1973–1983. [Google Scholar] [CrossRef]
- Nakashima, Y.; Hata, S.; Yasuda, T. Blood plasma separation and extraction from a minute amount of blood using dielectrophoretic and capillary forces. Sens. Actuators B Chem. 2010, 145, 561–569. [Google Scholar] [CrossRef]
- Cheng, S.J.; Hsieh, K.Y.; Chen, S.L.; Chen, C.Y.; Huang, C.Y.; Tsou, H.I.; Kumar, P.V.; Hsieh, J.C.; Chen, G.Y. Microfluidics and Nanomaterial-based Technologies for Circulating Tumor Cell Isolation and Detection. Sensors 2020, 20, 1875. [Google Scholar] [CrossRef] [PubMed]
- Jabir, M.; Sahib, U.I.; Taqi, Z.; Taha, A.; Sulaiman, G.; Albukhaty, S.; Al-Shammari, A.; Alwahibi, M.; Soliman, D.; Dewir, Y.H.; et al. Linalool-Loaded Glutathione-Modified Gold Nanoparticles Conjugated with CALNN Peptide as Apoptosis Inducer and NF-κB Translocation Inhibitor in SKOV-3 Cell Line. Int. J. Nanomed. 2020, 15, 9025–9047. [Google Scholar] [CrossRef]
- Albukhaty, S.; Naderi-Manesh, H.; Tiraihi, T.; Sakhi Jabir, M. Poly-l-lysine-coated superparamagnetic nanoparticles: A novel method for the transfection of pro-BDNF into neural stem cells. Artif. Cells Nanomed. Biotechnol. 2018, 46 (Suppl. S3), S125–S132. [Google Scholar] [CrossRef]
- Al-Musawi, S.; Albukhaty, S.; Al-Karagoly, H.; Sulaiman, G.M.; Alwahibi, M.S.; Dewir, Y.H.; Soliman, D.A.; Rizwana, H. Antibacterial Activity of Honey/Chitosan Nanofibers Loaded with Capsaicin and Gold Nanoparticles for Wound Dressing. Molecules 2020, 25, 4770. [Google Scholar] [CrossRef]
- Albukhaty, S.; Al-Bayati, L.; Al-Karagoly, H.; Al-Musawi, S. Preparation and characterization of titanium dioxide nanoparticles and in vitro investigation of their cytotoxicity and antibacterial activity against Staphylococcus aureus and Escherichia coli. Anim. Biotechnol. 2020, 28, 1–7. [Google Scholar] [CrossRef]
- Al-aqbi, Z.T.; Yap, Y.C.; Li, F.; Breadmore, M.C. Integrated Microfluidic Devices Fabricated in Poly (Methyl Methacrylate)(PMMA) for On-site Therapeutic Drug Monitoring of Aminoglycosides in Whole Blood. Biosensors 2019, 9, 19. [Google Scholar] [CrossRef]
- Macdonald, N.P.; Currivan, S.A.; Tedone, L.; Paull, B. Direct production of microstructured surfaces for planar chromatography using 3D printing. Anal. Chem. 2017, 89, 2457–2463. [Google Scholar] [CrossRef] [PubMed]
- Shallan, A.I.; Gaudry, A.J.; Guijt, R.M.; Breadmore, M.C. Tuneable nanochannel formation for sample-in/answer-out devices. Chem. Commun. 2013, 49, 2816–2818. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Guijt, R.M.; Breadmore, M.C. Nanoporous membranes for microfluidic concentration prior to electrophoretic separation of proteins in urine. Anal. Chem. 2016, 88, 8257–8263. [Google Scholar] [CrossRef] [PubMed]
- Cervera, J.; Ramírez, P.; Manzanares, J.A.; Mafé, S. Incorporating ionic size in the transport equations for charged nanopores. Microfluid. Nanofluid. 2010, 9, 41–53. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-aqbi, Z.T.; Albukhaty, S.; Zarzoor, A.M.; Sulaiman, G.M.; Khalil, K.A.A.; Belali, T.; Soliman, M.T.A. A Novel Microfluidic Device for Blood Plasma Filtration. Micromachines 2021, 12, 336. https://doi.org/10.3390/mi12030336
Al-aqbi ZT, Albukhaty S, Zarzoor AM, Sulaiman GM, Khalil KAA, Belali T, Soliman MTA. A Novel Microfluidic Device for Blood Plasma Filtration. Micromachines. 2021; 12(3):336. https://doi.org/10.3390/mi12030336
Chicago/Turabian StyleAl-aqbi, Zaidon T., Salim Albukhaty, Ameerah M. Zarzoor, Ghassan M. Sulaiman, Khalil A. A. Khalil, Tareg Belali, and Mohamed T. A. Soliman. 2021. "A Novel Microfluidic Device for Blood Plasma Filtration" Micromachines 12, no. 3: 336. https://doi.org/10.3390/mi12030336
APA StyleAl-aqbi, Z. T., Albukhaty, S., Zarzoor, A. M., Sulaiman, G. M., Khalil, K. A. A., Belali, T., & Soliman, M. T. A. (2021). A Novel Microfluidic Device for Blood Plasma Filtration. Micromachines, 12(3), 336. https://doi.org/10.3390/mi12030336









