Measuring Ocular Aberrations Sequentially Using a Digital Micromirror Device
Abstract
:1. Introduction
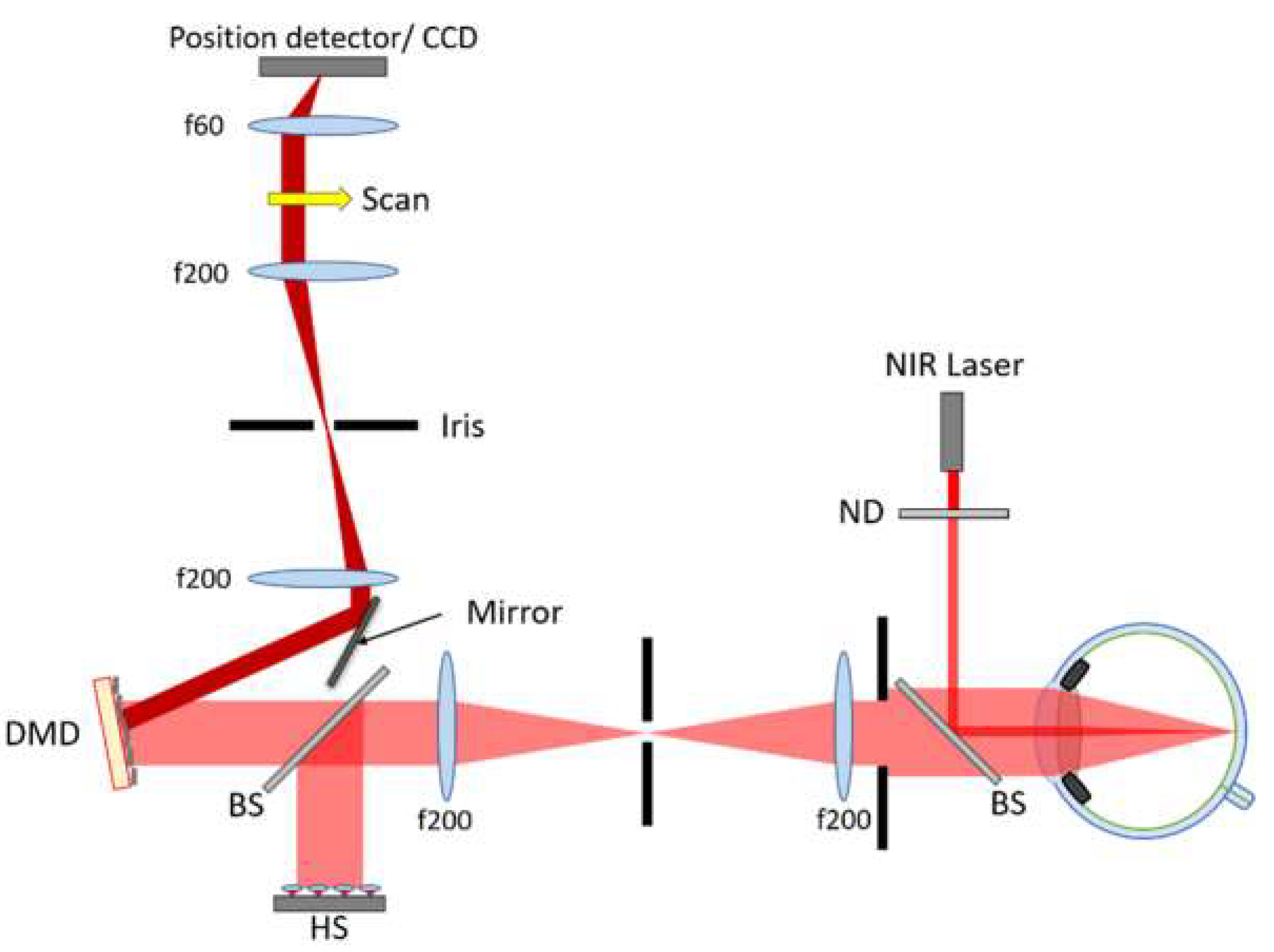
2. Materials and Methods
- (1)
- A 2D-lateral resistive position detector (PDP90A, ThorlabsTM, Newton, NJ, USA) of up to 0.75 μm spatial resolution, was used to register the central position of the PSF centroid (x,y) for each activated DMD cell. Although its angular resolution suffices, the limited sensitivity of this device prevents it from being used to determine ocular aberrations, but it is included here as a proof-of-principle in Section 3.1.1. Indeed, it may well find applications where power limitations are of less concern, such as in the characterization of laser beams.
- (2)
- A CCD camera (Scientific Camera 1501M-USB, ThorlabsTM, Newton, NJ, USA) with 6.45 μm pixel pitch and 14-bit digital output is used for the rest of the results in Section 3.1.2 and Section 3.2, allowing for high brightness variations and binning of pixels to increase acquisition speed when acquiring images of the PSF from which the centroid position can be determined.
3. Experimental Results
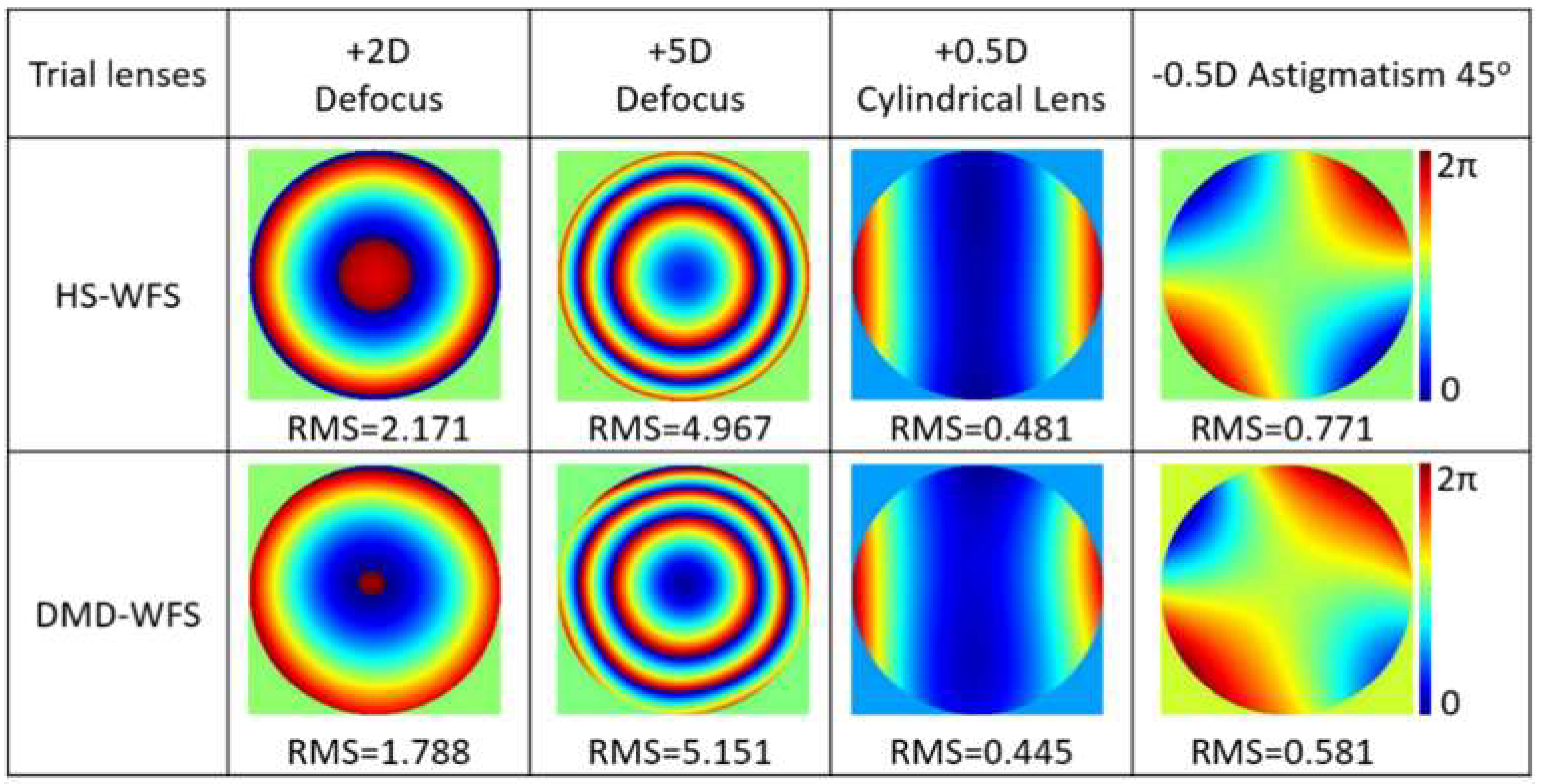
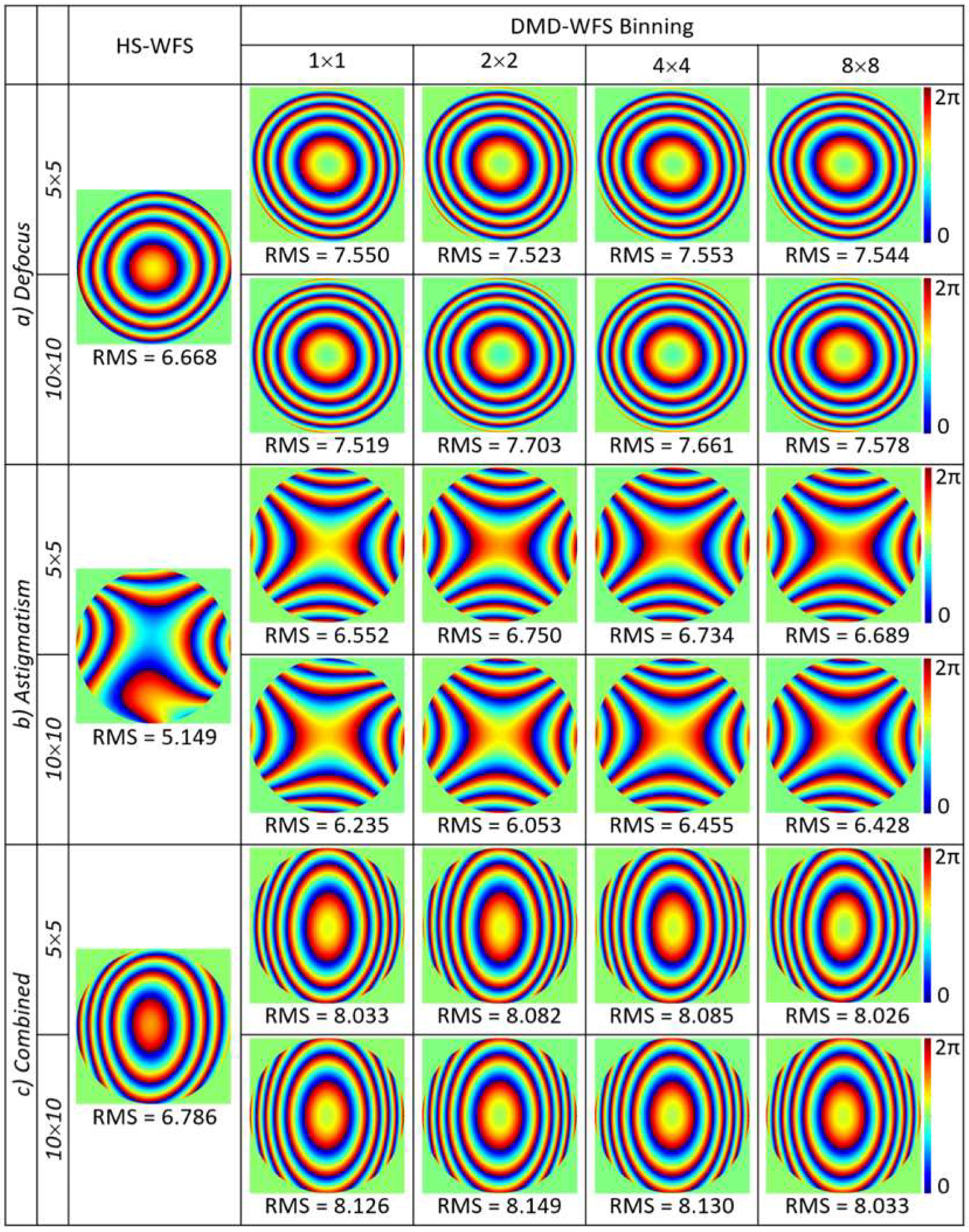
3.1. Wavefront Aberrations with an Artificial Eye
3.1.1. Lateral Position Detector
3.1.2. CCD Camera Detector
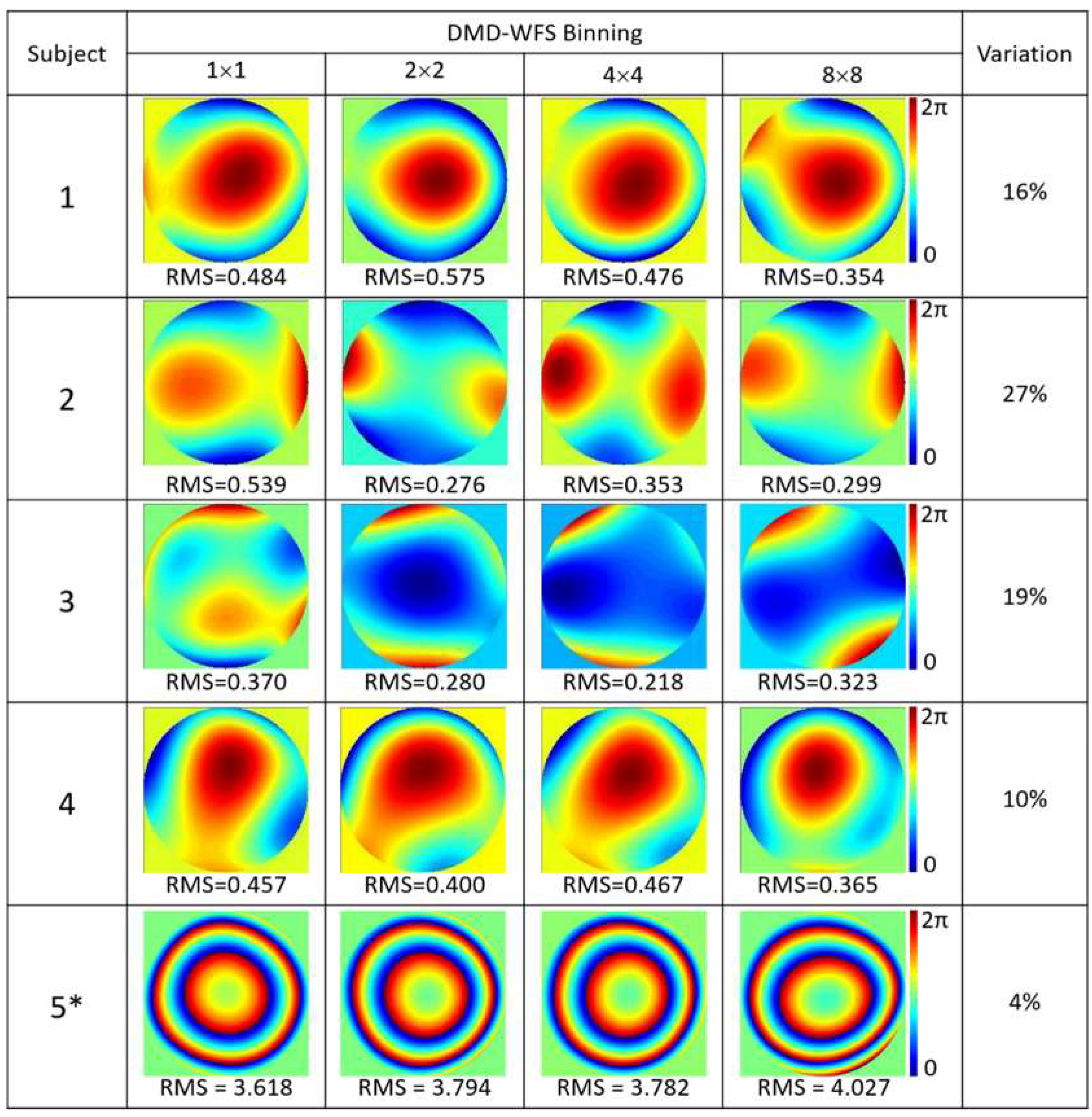
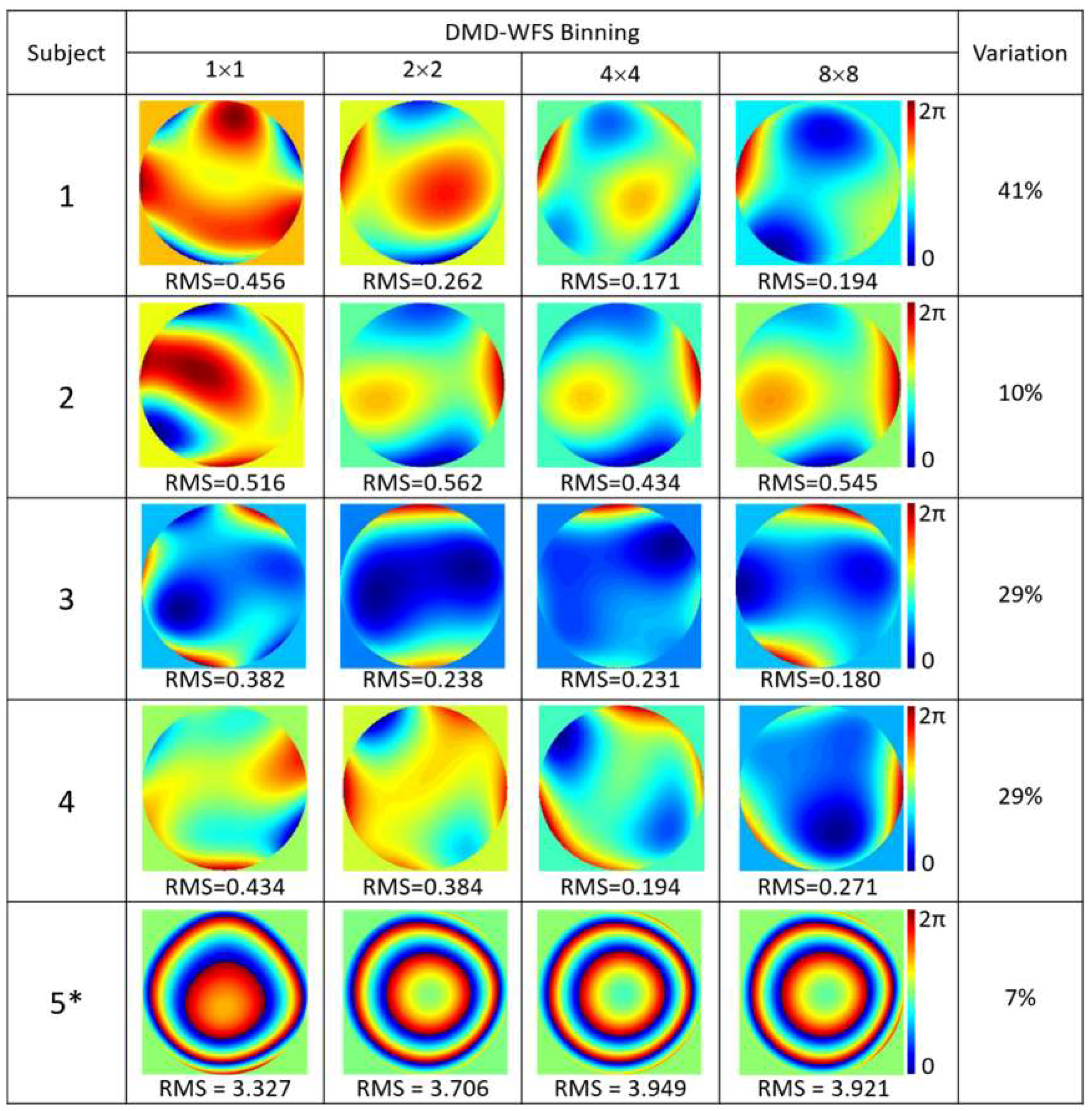
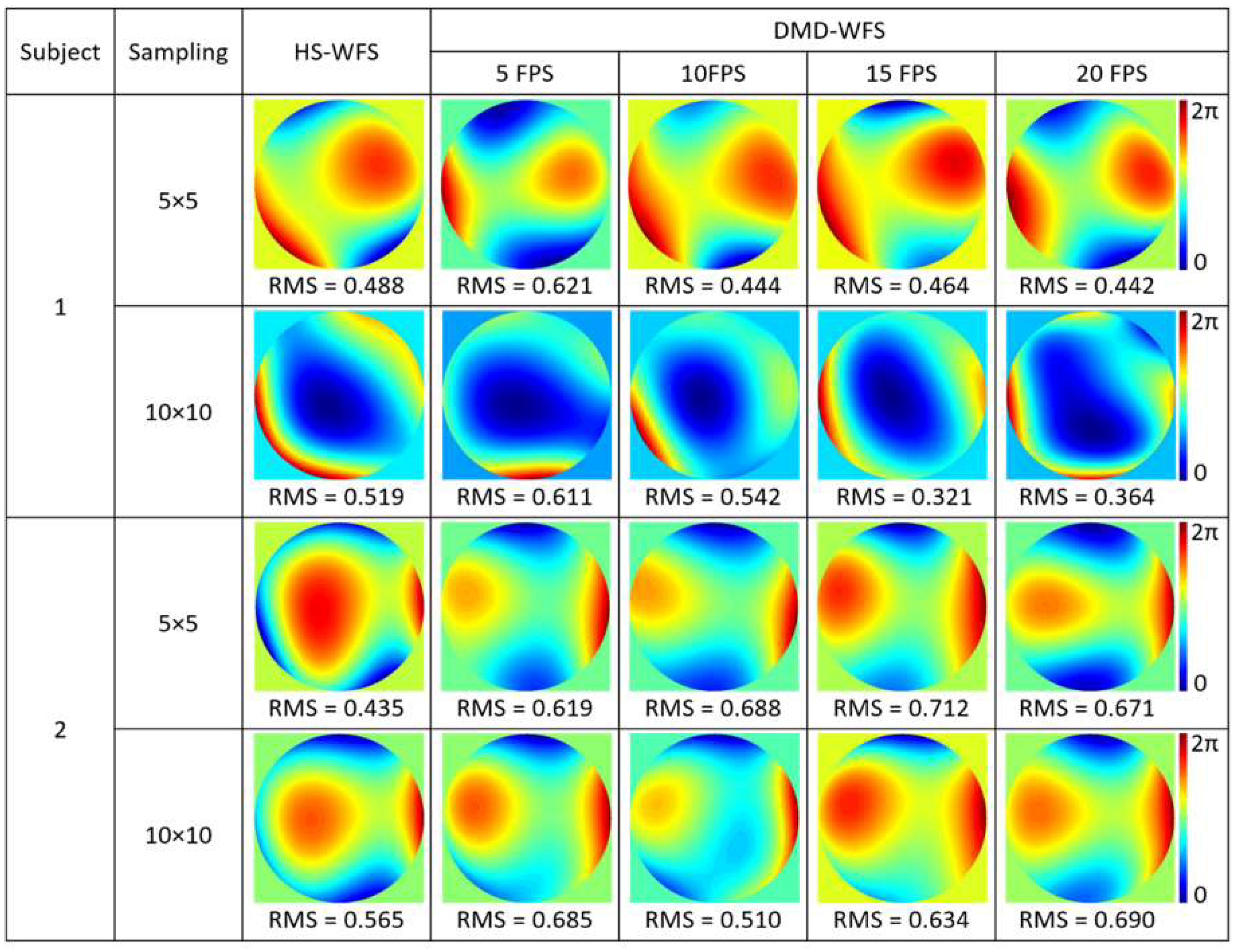
3.2. Wavefront Aberrations of the Real Eye
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Thibos, L.N.; Applegate, R.A.; Schwiegerling, J.T.; Webb, R. Standards for Reporting the Optical Aberrations of Eyes. J. Refract. Surg. 2002, 18, 652–660. [Google Scholar]
- López-Gil, N.; Howland, H.C. Measurement of the Eye’s Near Infrared Wave-Front Aberration Using the Objective Crossed-Cylinder Aberroscope Technique. Vision Res. 1999, 39, 2031–2037. [Google Scholar] [CrossRef]
- Walsh, G.; Howland, H.C.; Charman, W.N. Objective Technique for the Determination of Monochromatic Aberrations of the Human Eye. J. Opt. Soc. Am. A 1984, 1, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Marcos, S.; Diaz-Santana, L.; Llorente, L.; Dainty, C. Ocular Aberrations with Ray Tracing and Shack–Hartmann Wave-Front Sensors: Does Polarization Play a Role? J. Opt. Soc. Am. A 2002, 19, 1063–1072. [Google Scholar] [CrossRef]
- Artal, P. Understanding Aberrations by Using Double-pass Techniques. J. Refract. Surg. 2000, 16, 560–562. [Google Scholar]
- Liang, J.; Grimm, B.; Goelz, S.; Bille, J.F. Objective Measurement of Wave Aberrations of the Human Eye with the Use of a Hartmann–Shack Wave-Front Sensor. J. Opt. Soc. Am. A 1994, 11, 1949–1957. [Google Scholar] [CrossRef]
- Hongbin, Y.; Guangya, Z.; Siong, C.F.; Feiwen, L.; Shouhua, W.A. Tunable Shack–Hartmann Wavefront Sensor Based on a Liquid-Filled Microlens Array. J. Micromech. Microeng. 2008, 18, 105017. [Google Scholar] [CrossRef]
- Seifert, L.; Liesener, J.; Tiziani, H.J. The Adaptive Shack–Hartmann Sensor. Opt. Commun. 2003, 216, 313–319. [Google Scholar] [CrossRef]
- Akondi, V.; Falldorf, C.; Marcos, S.; Vohnsen, B. Phase Unwrapping with a Virtual Hartmann–Shack Wavefront Sensor. Opt. Express 2015, 23, 25425–25439. [Google Scholar] [CrossRef]
- Maeda, N. Wavefront Technology in Ophthalmology. Curr. Opin. Ophthalmol. 2001, 12, 294–299. [Google Scholar] [CrossRef]
- Gobbe, M.; Guillon, M. Corneal Wavefront Aberration Measurements to Detect Keratoconus Patients. Cont. Lens Anterior Eye 2005, 28, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Dolgin, E. The Myopia Boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Vohnsen, B.; Carmichael, M.A.; Qaysi, S.; Sharmin, N. Hartmann–Shack Wavefront Sensing without a Lenslet Array Using a Digital Micromirror Device. Appl. Opt. 2018, 57, E199–E204. [Google Scholar] [CrossRef] [PubMed]
- Lochocki, B.; Gambín, A.; Manzanera, S.; Irles, E.; Tajahuerce, E.; Lancis, J.; Artal, P. Single Pixel Camera Ophthalmoscope. Optica 2016, 3, 1056–1059. [Google Scholar] [CrossRef]
- Carmichael, M.A.; Vohnsen, B. Analysing the Impact of Myopia on the Stiles-Crawford Effect of the First Kind Using a Digital Micromirror Device. Ophthal. Physl. Opt. 2018, 38, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Navarro, R.; Moreno-Barriuso, E. Laser Ray-Tracing Method for Optical Testing. Opt. Lett. 1999, 24, 951. [Google Scholar] [CrossRef] [PubMed]
- Akondi, V.; Vohnsen, B. Myopic Aberrations: Impact of Centroiding Noise in Hartmann Shack Wavefront Sensing. Ophthal. Physl. Opt. 2013, 33, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Thibos, L.N.; Hong, X.; Bradley, A.; Cheng, X. Statistical Variation of Aberration Structure and Image Quality in a Normal Population of Healthy Eyes. J. Opt. Soc. Am. A 2002, 19, 2329–2348. [Google Scholar] [CrossRef]
- Ryle, J.P.; Vohnsen, B.; Sheridan, J.T. Simultaneous Drift, Microsaccades, and Ocular Microtremor Measurement from a Single Noncontact Far-Field Optical Sensor. J. Biomed. Opt. 2015, 20, 027004. [Google Scholar] [CrossRef]
- Rayner, K. Eye Movements in Reading and Information Processing: 20 Years of Research. Psychol. Bull. 1998, 124, 372–422. [Google Scholar] [CrossRef]
- Otero-Millan, J.; Troncoso, X.G.; Macknik, S.L.; Serrano-Pedraza, I.; Martinez-Conde, S. Saccades and Microsaccades during Visual Fixation, Exploration, and Search: Foundations for a Common Saccadic Generator. J. Vis. 2008, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Wong, Y.L.; Saw, S.M. Epidemiology of Pathologic Myopia in Asia and Worldwide. Asia Pac. J. Ophthalmol. 2016, 5, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, T.; Yamamoto, T.; Okamoto, F.; Oshika, T. Time Course of Changes in Ocular Wavefront Aberration after Administration of Eye Ointment. Eye 2012, 26, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Cox, M.A.; Toninelli, E.; Cheng, L.; Padgett, M.; Forbes, A. A High-Speed, Wavelength Invariant, Single-Pixel Wavefront Sensor with a Digital Micromirror Device. Opt. Express 2019, in press. [Google Scholar]

| HS-WFS | DMD-WFS | |||||||
|---|---|---|---|---|---|---|---|---|
| c2,0[μm] | c2,2[μm] | Sphere[D] | Cyl.[D] | c2,0[μm] | c2,2[μm] | Sphere[D] | Cyl.[D] | |
| a) | 6.638 | 0.308 | 11.50 | 0.75 | 7.519 | −0.024 | 13.02 | 0.00 |
| b) | 0.627 | −4.867 | 1.08 | −11.90 | 0.561 | −6.511 | 0.97 | −15.95 |
| c) | 6.270 | −2.472 | 10.85 | −6.05 | 7.084 | −3.769 | 12.27 | −9.23 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carmichael Martins, A.; Vohnsen, B. Measuring Ocular Aberrations Sequentially Using a Digital Micromirror Device. Micromachines 2019, 10, 117. https://doi.org/10.3390/mi10020117
Carmichael Martins A, Vohnsen B. Measuring Ocular Aberrations Sequentially Using a Digital Micromirror Device. Micromachines. 2019; 10(2):117. https://doi.org/10.3390/mi10020117
Chicago/Turabian StyleCarmichael Martins, Alessandra, and Brian Vohnsen. 2019. "Measuring Ocular Aberrations Sequentially Using a Digital Micromirror Device" Micromachines 10, no. 2: 117. https://doi.org/10.3390/mi10020117
APA StyleCarmichael Martins, A., & Vohnsen, B. (2019). Measuring Ocular Aberrations Sequentially Using a Digital Micromirror Device. Micromachines, 10(2), 117. https://doi.org/10.3390/mi10020117






