Biological Mechanisms of Enterotoxigenic Bacteroides fragilis Toxin: Linking Inflammation, Colorectal Cancer, and Clinical Implications
Abstract
1. Introduction
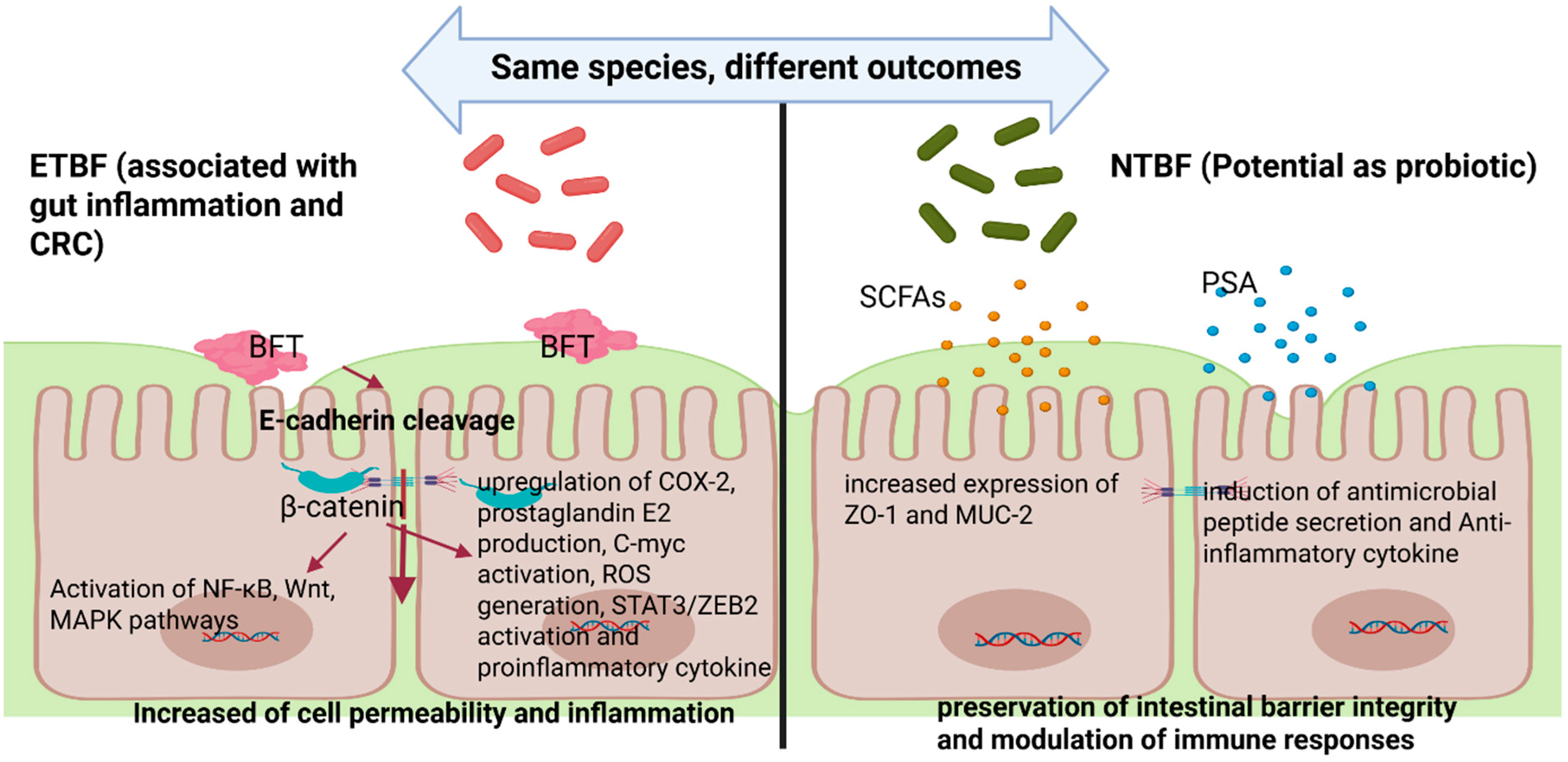
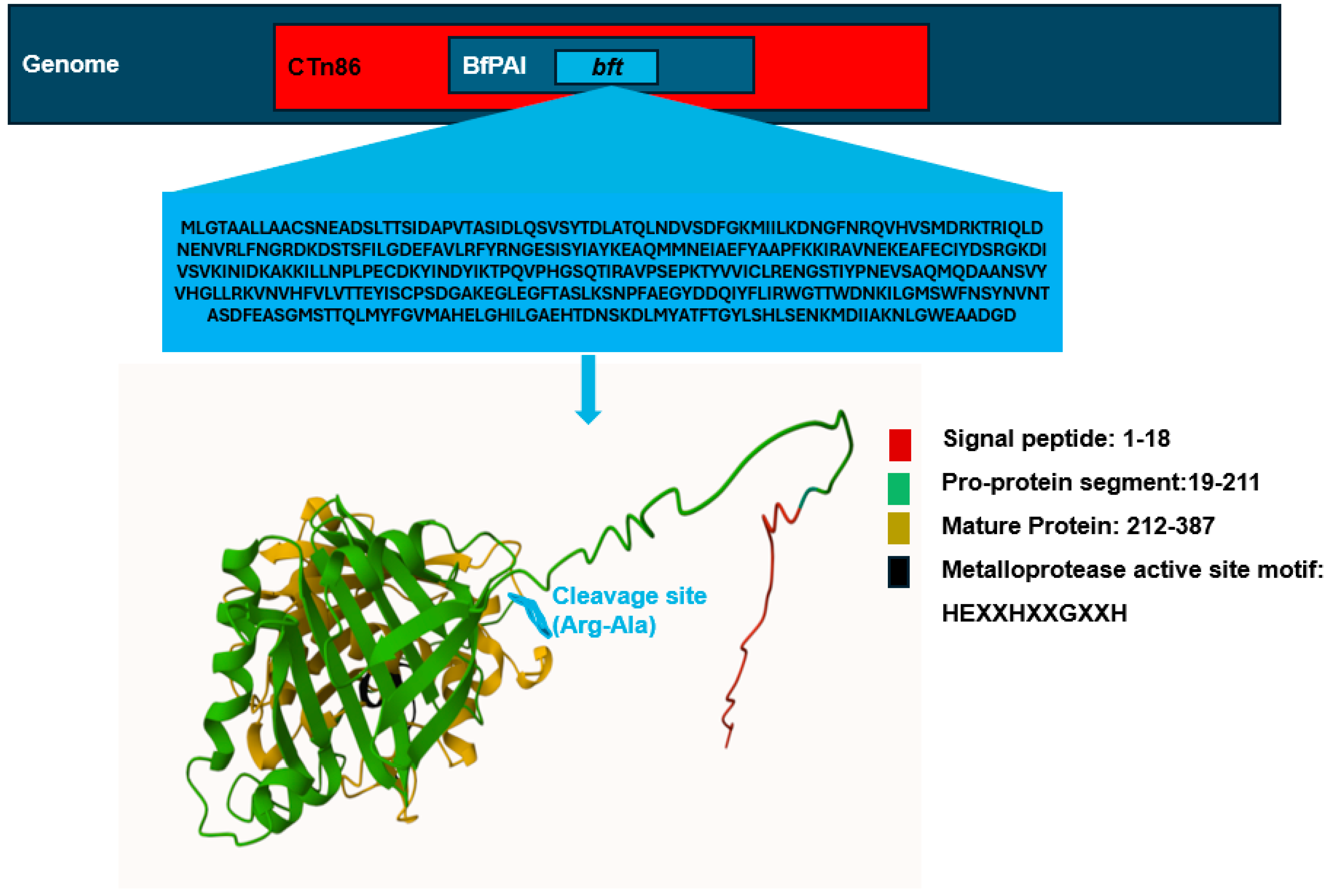
2. Molecular and Genetic Structure of Bacteroides fragilis Toxin (BFT)
3. ETBF-Associated Diseases and Underlying Mechanisms
4. Challenges in the Detection of Bacteroides fragilis and Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAD | Antibiotic-associated diarrhea |
| BfPAI | Bacteroides fragilis pathogenicity island |
| BFT | Bacteroides fragilis toxin |
| CRC | Colorectal cancer |
| CDI | Clostridioides difficile infection |
| CTn86 | Conjugative transposon 86 |
| DSS | Dextran sulfate sodium |
| ETBF | Enterotoxigenic Bacteroides fragilis |
| GI | Gastrointestinal |
| IL-10 | Interleukin-10 |
| IL-22 | Interleukin-22 |
| MUC-2 | Mucin 2 |
| NTBF | Non-toxigenic Bacteroides fragilis |
| OMVs | Outer membrane vesicles |
| PSA | Polysaccharide A |
| RprXY | Two-component regulatory system RprXY |
| STAT3 | Signal transducer and activator of transcription 3 |
| Treg | Regulatory T cell |
| ZEB2 | Zinc finger E-box binding homeobox 2 |
| ZO-1 | Zonula occludens-1 |
References
- Sender, R.; Fuchs, S.; Milo, R. Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol. 2016, 14, e1002533. [Google Scholar] [CrossRef] [PubMed]
- John, H.T.; Thomas, T.C.; Chukwuebuka, E.C.; Ali, A.B.; Anass, R.; Tefera, Y.Y.; Babu, B.; Negrut, N.; Ferician, A.; Marian, P. The Microbiota–Human Health Axis. Microorganisms 2025, 13, 948. [Google Scholar] [CrossRef] [PubMed]
- Shao, T.; Hsu, R.; Rafizadeh, D.L.; Wang, L.; Bowlus, C.L.; Kumar, N.; Mishra, J.; Timilsina, S.; Ridgway, W.M.; Gershwin, M.E.; et al. The Gut Ecosystem and Immune Tolerance. J. Autoimmun. 2023, 141, 103114. [Google Scholar] [CrossRef]
- Acevedo-Román, A.; Pagán-Zayas, N.; Velázquez-Rivera, L.I.; Torres-Ventura, A.C.; Godoy-Vitorino, F. Insights into Gut Dysbiosis: Inflammatory Diseases, Obesity, and Restoration Approaches. Int. J. Mol. Sci. 2024, 25, 971. [Google Scholar] [CrossRef]
- Zhou, W.; Cheng, Y.; Zhu, P.; Nasser, M.I.; Zhang, X.; Zhao, M. Implication of Gut Microbiota in Cardiovascular Diseases. Oxid. Med. Cell. Longev. 2020, 2020, 5394096. [Google Scholar] [CrossRef]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A Human Gut Microbial Gene Catalogue Established by Metagenomic Sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef]
- Townsend, G.E., 2nd; Han, W.; Schwalm, N.D.; Hong, X.; Bencivenga-Barry, N.A.; Goodman, A.L.; Groisman, E.A.; Ii, G.E.T.; Comstock, L.E. A Master Regulator of Bacteroides Thetaiotaomicron Gut Colonization Controls Carbohydrate Utilization and an Alternative Protein Synthesis Factor. mBio 2020, 11, e03221-19. [Google Scholar] [CrossRef] [PubMed]
- Sears, C.L.; Geis, A.L.; Housseau, F. Bacteroides fragilis Subverts Mucosal Biology: From Symbiont to Colon Carcinogenesis. J. Clin. Investig. 2014, 124, 4166–4172. [Google Scholar] [CrossRef]
- Cao, Y.; Wang, Z.; Yan, Y.; Ji, L.; He, J.; Xuan, B.; Shen, C.; Ma, Y.; Jiang, S.; Ma, D.; et al. Enterotoxigenic Bacteroides fragilis Promotes Intestinal Inflammation and Malignancy by Inhibiting Exosome-Packaged MiR-149-3p. Gastroenterology 2021, 161, 1552–1566.e12. [Google Scholar] [CrossRef]
- Zhang, W.; Zhu, B.; Xu, J.; Liu, Y.; Qiu, E.; Li, Z.; Li, Z.; He, Y.; Zhou, H.; Bai, Y.; et al. Bacteroides fragilis Protects against Antibiotic-Associated Diarrhea in Rats by Modulating Intestinal Defenses. Front. Immunol. 2018, 9, 1040. [Google Scholar] [CrossRef]
- Chung, L.; Thiele Orberg, E.; Geis, A.L.; Chan, J.L.; Fu, K.; DeStefano Shields, C.E.; Dejea, C.M.; Fathi, P.; Chen, J.; Finard, B.B.; et al. Bacteroides fragilis Toxin Coordinates a Pro-Carcinogenic Inflammatory Cascade via Targeting of Colonic Epithelial Cells. Cell Host Microbe 2018, 23, 203–214.e5. [Google Scholar] [CrossRef]
- He, Q.; Niu, M.; Bi, J.; Du, N.; Liu, S.; Yang, K.; Li, H.; Yao, J.; Du, Y.; Duan, Y. Protective Effects of a New Generation of Probiotic Bacteroides fragilis against Colitis In Vitro and In Vitro. Sci. Rep. 2023, 13, 1584. [Google Scholar] [CrossRef]
- Franco, A.A.; Cheng, R.K.; Goodman, A.; Sears, C.L. Modulation of Bft Expression by the Bacteroides fragilis Pathogenicity Island and Its Flanking Region. Mol. Microbiol. 2002, 45, 1067–1077. [Google Scholar] [CrossRef]
- Franco, A.A.; Mundy, L.M.; Trucksis, M.; Wu, S.; Kaper, J.B.; Sears, C.L. Cloning and Characterization of the Bacteroides fragilis Metalloprotease Toxin Gene. Infect. Immune 1997, 65, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, M.J.; Macfarlane, G.T. Nondigestible Oligosaccharides Enhance Bacterial Colonization Resistance against Clostridium Difficile in Vitro. Appl. Environ. Microbiol. 2003, 69, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.; Yang, S.; Zhang, Y.; Qian, K.; Zhang, Z.; Liu, Y.; Wang, Y.; Bai, Y.; Fan, H.; Zhao, X.; et al. Bacteroides fragilis Prevents Clostridium Difficile Infection in a Mouse Model by Restoring Gut Barrier and Microbiome Regulation. Front. Microbiol. 2018, 9, 2976. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.L.; Wu, S.; Geis, A.L.; Chan, G.V.; Gomes, T.A.M.; Beck, S.E.; Wu, X.; Fan, H.; Tam, A.J.; Chung, L.; et al. Non-Toxigenic Bacteroides fragilis (NTBF) Administration Reduces Bacteria-Driven Chronic Colitis and Tumor Development Independent of Polysaccharide A. Mucosal Immunol. 2019, 12, 164–177. [Google Scholar] [CrossRef]
- Zhang, W.; Zhou, Q.; Liu, H.; Xu, J.; Huang, R.; Shen, B.; Guo, Y.; Ai, X.; Xu, J.; Zhao, X.; et al. Bacteroides fragilis Strain ZY-312 Facilitates Colonic Mucosa Regeneration in Colitis via Motivating STAT3 Signaling Pathway Induced by IL-22 from ILC3 Secretion. Front. Immunol. 2023, 14, 1156762. [Google Scholar] [CrossRef]
- Kim, W.S.; Hwang, S.; Gwon, S.Y.; Jo, M.; Yoo, S.H.; Hong, J.; Jang, H.N.; Hong, J.E.; Kang, D.H.; Yun, M.; et al. Bacteroides fragilis Toxin Induces Sequential Proteolysis of E-Cadherin and Inflammatory Response in Mouse Intestinal Epithelial Cell Line. Microorganisms 2025, 13, 781. [Google Scholar] [CrossRef]
- Ramamurthy, D.; Pazhani, G.P.; Sarkar, A.; Nandy, R.K.; Rajendran, K.; Sur, D.; Manna, B.; Ramamurthy, T. Case-Control Study on the Role of Enterotoxigenic Bacteroides fragilis as a Cause of Diarrhea among Children in Kolkata, India. PLoS ONE 2013, 8, e6062. [Google Scholar] [CrossRef]
- Merino, V.R.C.; Nakano, V.; Liu, C.; Song, Y.; Finegold, S.M.; Avila-Campos, M.J. Quantitative Detection of Enterotoxigenic Bacteroides fragilis Subtypes Isolated from Children with and without Diarrhea. J. Clin. Microbiol. 2011, 49, 416–418. [Google Scholar] [CrossRef] [PubMed]
- Jo, M.; Hwang, S.; Lee, C.G.; Hong, J.E.; Kang, D.H.; Yoo, S.H.; Kim, W.S.; Yoo, J.Y.; Rhee, K.J. Promotion of Colitis in B Cell-Deficient C57BL/6 Mice Infected with Enterotoxigenic Bacteroides fragilis. Int. J. Mol. Sci. 2024, 25, 364. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Jiang, D.; Zhou, X.; Ye, X.; Yang, P.; He, Y. Recombinant Bacteroides fragilis Enterotoxin-1 (RBFT-1) Promotes Proliferation of Colorectal Cancer via CCL3-Related Molecular Pathways. Open Life Sci. 2021, 16, 408–418. [Google Scholar] [CrossRef]
- Wu, Z.; Yu, M.; Zeng, Y.; Huang, Y.; Zheng, W. LRP11-AS1 Mediates Enterotoxigenic Bacteroides fragilis-Related Carcinogenesis in Colorectal Cancer via the MiR-149-3p/CDK4 Pathway. Cancer Gene Ther. 2024, 32, 184–197. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, X.; Hu, T.; Huang, H.; Chen, G.; Jin, B.; Zeng, G.; Liu, J. Entero-Toxigenic Bacteroides fragilis Contributes to Intestinal Barrier Injury and Colorectal Cancer Progression by Mediating the BFT/STAT3/ZEB2 Pathway. Cell Cycle 2024, 23, 70–82. [Google Scholar] [CrossRef]
- Jasemi, S.; Emaneini, M.; Fazeli, M.S.; Ahmadinejad, Z.; Nomanpour, B.; Sadeghpour Heravi, F.; Sechi, L.A.; Feizabadi, M.M. Toxigenic and Non-Toxigenic Patterns I, II and III and Biofilm-Forming Ability in Bacteroides fragilis Strains Isolated from Patients Diagnosed with Colorectal Cancer. Gut Pathog. 2020, 12, 28. [Google Scholar] [CrossRef]
- Sárvári, K.P.; Sóki, J.; Iván, M.; Miszti, C.; Latkóczy, K.; Melegh, S.Z.; Urbán, E. Detection of Enterotoxin and Protease Genes among Hungarian Clinical Bacteroides fragilis Isolates. Anaerobe 2017, 48, 98–102. [Google Scholar] [CrossRef]
- Łuczak, M.; Obuch-Woszczatyński, P.; Pituch, H.; Leszczyński, P.; Martirosian, G.; Patrick, S.; Poxton, I.; Wintermans, R.G.F.; Dubreuil, L.; Meisel-Mikołajczyk, F. Search for Enterotoxin Gene in Bacteroides fragilis Strains Isolated from Clinical Specimens in Poland, Great Britain, the Netherlands and France. Med. Sci. Monit. 2001, 7, 222–225. [Google Scholar] [PubMed]
- Ulger, N.; Rajendram, D.; Yagci, A.; Gharbia, S.; Shah, H.N.; Gulluoglu, B.M.; Akin, L.M.; Demirkalem, P.; Celenk, T.; Soyletir, G. The Distribution of the Bft Alleles among Enterotoxigenic Bacteroides fragilis Strains from Stool Specimens and Extraintestinal Sites. Anaerobe 2006, 12, 71–74. [Google Scholar] [CrossRef]
- Cheng, W.T.; Kantilal, H.K.; Davamani, F. The Mechanism of Bacteroides fragilis Toxin Contributes to Colon Cancer Formation. Malays. J. Med. Sc. 2020, 27, 9–21. [Google Scholar] [CrossRef]
- Scott, N.; Whittle, E.; Jeraldo, P.; Chia, N. A Systemic Review of the Role of Enterotoxic Bacteroides fragilis in Colorectal Cancer. Neoplasia 2022, 29, 100797. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.A. The Bacteroides fragilis Pathogenicity Island Is Contained in a Putative Novel Conjugative Transposon. J. Bacteriol. 2004, 186, 6077–6092. [Google Scholar] [CrossRef]
- Buckwold, S.L.; Shoemaker, N.B.; Sears, C.L.; Franco, A.A. Identification and Characterization of Conjugative Transposons CTn86 and CTn9343 in Bacteroides fragilis Strains. Appl. Environ. Microbiol. 2007, 73, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Kato, N.; Liu, C.-X.; Kato, H.; Watanabe, K.; Tanaka, Y.; Yamamoto, T.; Suzuki, K.; Ueno, K. A New Subtype of the Metalloprotease Toxin Gene and the Incidence of the Three Bft Subtypes among Bacteroides fragilis Isolates in Japan. FEMS Microbiol. Lett. 2000, 182, 171–176. [Google Scholar] [CrossRef][Green Version]
- Kling, J. Cloning and Characterization of the Gene for the Metalloprotease Enterotoxin of Bacteroides fragilis. FEMS Microbiol. Lett. 1997, 146, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Dreyfus, L.A.; Tzianabos, A.O.; Hayashi, C.; Sears, C.L. Diversity of the Metalloprotease Toxin Produced by Enterotoxigenic Bacteroides fragilis. Infect. Immun. 2002, 70, 2463–2471. [Google Scholar] [CrossRef]
- Chung, G.-T.; Franco, A.A.; Wu, S.; Rhie, G.-E.; Cheng, R.; Oh, H.-B.; Sears, C.L. Identification of a Third Metalloprotease Toxin Gene in Extraintestinal Isolates of Bacteroides fragilis. Infect Immun. 1999, 67, 4945–4949. [Google Scholar] [CrossRef]
- Moncrief, J.S.; Obiso, R.; Barroso, L.A.; Kling, J.J.; Wright, R.L.; Van Tassell, R.L.; Lyerly, D.M.; Wilkins, T.D. The Enterotoxin of Bacteroides fragilis Is a Metalloprotease. Infect. Immun. 1995, 63, 175–181. [Google Scholar] [CrossRef]
- Gomis-Rüth, F.X. Structural Aspects of the Metzincin Clan of Metalloendopeptidases. Mol. Biotechnol. 2003, 24, 157–202. [Google Scholar] [CrossRef]
- Sears, C.L. The Toxins of Bacteroides fragilis. Toxicon 2001, 39, 1737–1746. [Google Scholar] [CrossRef]
- Obiso, R.J.; Bevan, D.R.; Wilkins, T.D. Molecular Modeling and Analysis of Fragilysin, the Bacteroides fragilis Toxin. Clin. Infect. Dis. 1997, 2, S153–S155. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Remacle, A.G.; Shiryaev, S.A.; Strongin, A.Y. Distinct Interactions with Cellular E-Cadherin of the Two Virulent Metalloproteinases Encoded by a Bacteroides fragilis Pathogenicity Island. PLoS ONE 2014, 9, e113896. [Google Scholar] [CrossRef]
- Gomis-Rüth, F.X. Catalytic Domain Architecture of Metzincin Metalloproteases. J. Biol. Chem. 2009, 284, 15353–15357. [Google Scholar] [CrossRef]
- Franco, A.A.; Buckwold, S.L.; Shin, J.W.; Ascon, M.; Sears, C.L. Mutation of the Zinc-Binding Metalloprotease Motif Affects Bacteroides fragilis Toxin Activity but Does Not Affect Propeptide Processing. Infect. Immun. 2005, 73, 5273–5277. [Google Scholar] [CrossRef]
- Goulas, T.; Arolas, J.L.; Gomis-Rüth, F.X. Structure, Function and Latency Regulation of a Bacterial Enterotoxin Potentially Derived from a Mammalian Adamalysin/ADAM Xenolog. Proc. Natl. Acad. Sci. USA 2011, 108, 1856–1861. [Google Scholar] [CrossRef]
- Sears, C.L.; Buckwold, S.L.; Shin, J.W.; Franco, A.A. The C-Terminal Region of Bacteroides fragilis Toxin Is Essential to Its Biological Activity. Infect. Immun. 2006, 74, 5595–5601. [Google Scholar] [CrossRef] [PubMed]
- Van Tassell, R.L.; Lyerly, D.M.; Wilkins, T.D. Purification and Characterization of an Enterotoxin from Bacteroides fragilis. Infect. Immun. 1992, 60, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Hecht, A.L.; Casterline, B.W.; Choi, V.M.; Bubeck Wardenburg, J. A Two-Component System Regulates Bacteroides fragilis Toxin to Maintain Intestinal Homeostasis and Prevent Lethal Disease. Cell Host Microbe 2017, 22, 443–448.e5. [Google Scholar] [CrossRef]
- Zakharzhevskaya, N.B.; Tsvetkov, V.B.; Vanyushkina, A.A.; Varizhuk, A.M.; Rakitina, D.V.; Podgorsky, V.V.; Vishnyakov, I.E.; Kharlampieva, D.D.; Manuvera, V.A.; Lisitsyn, F.V.; et al. Interaction of Bacteroides fragilis Toxin with Outer Membrane Vesicles Reveals New Mechanism of Its Secretion and Delivery. Front. Cell Infect. Microbiol. 2017, 7, 308. [Google Scholar] [CrossRef]
- Dornbusch, K.; Nord, C.-E.; Wadström, T. Biochemical Characterization and in Vitro Determination of Antibiotic Susceptibility of Clinical Isolates of Bacteroides fragilis. Scand. J. Infect. Dis. 1974, 6, 253–258. [Google Scholar] [CrossRef]
- Nielsen, M.L.; Justesen, T. Anaerobic and Aerobic Bacteriological Studies in Biliary Tract Disease. Scand. J. Gastroenterol. 1976, 11, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Kierzkowska, M.; Markowska, K.; Kownacki, J.; Podsiadły, E.; Majewska, A. Anaerobic Bacteraemia—Identification of Bacteroides and Phocaeicola in Blood Samples. Challenges in Antimicrobial Susceptibility Testing. Microbe 2025, 7, 100374. [Google Scholar] [CrossRef]
- Jasemi, S.; Emaneini, M.; Ahmadinejad, Z.; Fazeli, M.S.; Sechi, L.A.; Sadeghpour Heravi, F.; Feizabadi, M.M. Antibiotic Resistance Pattern of Bacteroides fragilis Isolated from Clinical and Colorectal Specimens. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 27. [Google Scholar] [CrossRef]
- Valguarnera, E.; Wardenburg, J.B. Good Gone Bad: One Toxin Away from Disease for Bacteroides fragilis. J. Mol. Biol. 2020, 432, 765–785. [Google Scholar] [CrossRef] [PubMed]
- Wexler, H.M. Bacteroides: The Good, the Bad, and the Nitty-Gritty. Clin. Microbiol. Rev. 2007, 20, 593–621. [Google Scholar] [CrossRef]
- Myers, L.L.; Firehammer, B.D.; Shoop, D.S.; Border, M.M. Bacteroides fragilis: A Possible Cause of Acute Diarrheal Disease in Newborn Lambs. Infect. Immune 1984, 44, 241–244. [Google Scholar] [CrossRef]
- Border, M.; Firehammer, B.D.; Shoop, D.S.; Myers, L.L. Isolation of Bacteroides fragilis from the Feces of Diarrheic Calves and Lambst. Clin. Microbiol. 1985, 21, 471–473. [Google Scholar] [CrossRef]
- Duimstra, J.R.; Myers, L.L.; Collins, J.E.; Benfield, D.A.; Shoop, D.S.; Bradbury, W.C. Enterovirulence of Enterotoxigenic Bacteroides fragilis in Gnotobiotic Pigs. Vet. Pathol. 1991, 28, 514–518. [Google Scholar] [CrossRef]
- Myers, L.L.; Shoop, D.S.; Stackhouse, L.L.; Newman, F.S.; Flaherty, R.J.; Letson, G.W.; Sack, A.R.B. Isolation of Enterotoxigenic Bacteroides fragilis from Humans with Diarrheat. J. Clin. Microbiol. 1987, 25, 2330–2333. [Google Scholar] [CrossRef]
- Ulger Toprak, N.; Yagci, A.; Gulluoglu, B.M.; Akin, M.L.; Demirkalem, P.; Celenk, T.; Soyletir, G. A Possible Role of Bacteroides fragilis Enterotoxin in the Aetiology of Colorectal Cancer. Clin. Microbiol. Infect. 2006, 12, 782–786. [Google Scholar] [CrossRef]
- Matsumiya, Y.; Suenaga, M.; Ishikawa, T.; Kudo, T.; Nakagawa, T.; Okamoto, K.; Tokunaga, M.; Hurtado, C.; Yamada, Y.; Oka, K.; et al. Clinical Significance of Bacteroides fragilis as a Potential Prognostic Factor in Colorectal Cancer. Anaerobe 2023, 84, 102784. [Google Scholar] [CrossRef] [PubMed]
- Zamani, S.; Taslimi, R.; Sarabi, A.; Jasemi, S.; Sechi, L.A.; Feizabadi, M.M. Enterotoxigenic Bacteroides fragilis: A Possible Etiological Candidate for Bacterially-Induced Colorectal Precancerous and Cancerous Lesions. Front. Cell Infect. Microbiol. 2020, 9, 449. [Google Scholar] [CrossRef] [PubMed]
- Boleij, A.; Hechenbleikner, E.M.; Goodwin, A.C.; Badani, R.; Stein, E.M.; Lazarev, M.G.; Ellis, B.; Carroll, K.C.; Albesiano, E.; Wick, E.C.; et al. The Bacteroides fragilis Toxin Gene Is Prevalent in the Colon Mucosa of Colorectal Cancer Patients. Clin. Infect. Dis. 2015, 60, 208–215. [Google Scholar] [CrossRef]
- Viljoen, K.S.; Dakshinamurthy, A.; Goldberg, P.; Blackburn, J.M. Quantitative Profiling of Colorectal Cancer-Associated Bacteria Reveals Associations between Fusobacterium spp., Enterotoxigenic Bacteroides fragilis (ETBF) and Clinicopathological Features of Colorectal Cancer. PLoS ONE 2015, 10, e0119462. [Google Scholar] [CrossRef] [PubMed]
- Van, N.; Ahlberg, N.; Chul Jung, B.; Lee, M.H.; Ahn, S.J.; Lee, I.-S.; Kim, Y.S.; Rhee, K.-J. Evaluation of Enterotoxigenic Bacteroides fragilis from Colonic Washings from Patients Undergoing Colonoscopy. J. Exp. Biomed. 2012, 18, 362–368. [Google Scholar]
- Lennard, K.S.; Goosen, R.W.; Blackburn, J.M. Bacterially-Associated Transcriptional Remodelling in a Distinct Genomic Subtype of Colorectal Cancer Provides a Plausible Molecular Basis for Disease Development. PLoS ONE 2016, 11, e0166282. [Google Scholar] [CrossRef]
- Wu, S.; Shin, J.; Zhang, G.; Cohen, M.; Franco, A.; Sears, C.L. The Bacteroides fragilis Toxin Binds to a Specific Intestinal Epithelial Cell Receptor. Infect. Immun. 2006, 74, 5382–5390. [Google Scholar] [CrossRef]
- Wu, S.; Rhee, K.J.; Zhang, M.; Franco, A.; Sears, C.L. Erratum: Bacteroides fragilis Toxin Stimulates Intestinal Epithelial Cell Shedding and γ-Secretase-Dependent E-Cadherin Cleavage. J. Cell Sci. 2007, 120, 1944–1952. [Google Scholar] [CrossRef]
- Koshy, S.S.; Montrose, M.H.; Sears, C.L. Human Intestinal Epithelial Cells Swell and Demonstrate Actin Rearrangement in Response to the Metalloprotease Toxin of Bacteroides fragilis. Infect. Immun. 1996, 64, 5022–5028. [Google Scholar] [CrossRef]
- Donelli, G.; Fabbri, A.; Fiorentini, C. Bacteroides fragilis Enterotoxin Induces Cytoskeletal Changes and Surface Blebbing in HT-29 Cells. Infect. Immun. 1996, 64, 113–119. [Google Scholar] [CrossRef]
- Lee, C.G.; Hwang, S.; Gwon, S.Y.; Park, C.; Jo, M.; Hong, J.E.; Rhee, K.J. Bacteroides fragilis Toxin Induces Intestinal Epithelial Cell Secretion of Interleukin-8 by the E-Cadherin/β-Catenin/NF-ΚB Dependent Pathway. Biomedicines 2022, 10, 827. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Lee, J.Y.; Yoon, Y.M.; Oh, Y.K.; Kang, J.S.; Kim, Y.J.; Kim, K.H. Bacteroides fragilis Enterotoxin Induces Cyclooxygenase-2 and Fluid Secretion in Intestinal Epithelial Cells through NF-ΚB Activation. Eur. J. Immunol. 2006, 36, 2446–2456. [Google Scholar] [CrossRef]
- Allen, J.; Hao, S.; Sears, C.L.; Timp, W. Epigenetic Changes Induced by Bacteroides fragilis Toxin. Infect. Immun. 2019, 87, e00447-18. [Google Scholar] [CrossRef]
- Li, S.; Liu, J.; Zheng, X.; Ren, L.; Yang, Y.; Li, W.; Fu, W.; Wang, J.; Du, G. Tumorigenic Bacteria in Colorectal Cancer: Mechanisms and Treatments. Cancer Biol. Med. 2021, 18, 147–162. [Google Scholar] [CrossRef]
- Goodwin, A.C.; Destefano Shields, C.E.; Wu, S.; Huso, D.L.; Wu, X.Q.; Murray-Stewart, T.R.; Hacker-Prietz, A.; Rabizadeh, S.; Woster, P.M.; Sears, C.L.; et al. Polyamine Catabolism Contributes to Enterotoxigenic Bacteroides fragilis-Induced Colon Tumorigenesis. Proc. Natl. Acad. Sci. USA 2011, 108, 15354–15359. [Google Scholar] [CrossRef] [PubMed]
- Sears, C.L. Enterotoxigenic Bacteroides fragilis: A Rogue among Symbiotes. Clin. Microbiol. Rev. 2009, 22, 349–369. [Google Scholar] [CrossRef]
- Wu, S.; Rhee, K.J.; Albesiano, E.; Rabizadeh, S.; Wu, X.; Yen, H.R.; Huso, D.L.; Brancati, F.L.; Wick, E.; McAllister, F.; et al. A Human Colonic Commensal Promotes Colon Tumorigenesis via Activation of T Helper Type 17 T Cell Responses. Nat. Med. 2009, 15, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Patrick, S. A Tale of Two Habitats: Bacteroides fragilis, a Lethal Pathogen and Resident in the Human Gastrointestinal Microbiome. Microbiology 2022, 168, 4. [Google Scholar] [CrossRef]
- Ho, P.L.; Ho, L.Y.; Yau, C.Y.; Tong, M.K.; Chow, K.H. A Novel Selective Medium for Isolation of Bacteroides fragilis from Clinical Specimens. J. Clin. Microbiol. 2017, 55, 384–390. [Google Scholar] [CrossRef]
- Liu, C.; Song, Y.; McTeague, M.; Vu, A.W.; Wexler, H.; Finegold, S.M. Rapid Identification of the Species of the Bacteroides fragilis Group by Multiplex PCR Assays Using Group- and Species-Specific Primers. FEMS Microbiol. Lett. 2003, 222, 9–16. [Google Scholar] [CrossRef]
- Nagy, E. Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry: A New Possibility for the Identification and Typing of Anaerobic Bacteria. Future Microbiol. 2014, 9, 217–233. [Google Scholar] [CrossRef] [PubMed]
- Nagy, E.; Maier, T.; Urban, E.; Terhes, G.; Kostrzewa, M.; Nord, C.E.; Hedberg, M.; Könönen, E.; Dubreuil, L.; Dosa, E.; et al. Species Identification of Clinical Isolates of Bacteroides by Matrix-Assisted Laser-Desorption/Ionization Time-of-Flight Mass Spectrometry. Clin. Microbiol. Infect. 2009, 15, 796–802. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, M.; Ohkuma, M. Identification and Classification of the Genus Bacteroides by Multilocus Sequence Analysis. Microbiology 2011, 157, 3388–3397. [Google Scholar] [CrossRef]
- Weikel, C.S.; Grieco, F.D.; Reuben, J.; Myers, L.L.; Bradley Sack, A.R. Human Colonic Epithelial Cells, HT29/C1, Treated with Crude Bacteroides fragilis Enterotoxin Dramatically Alter Their Morphology. Infect. Immun. 1992, 60, 321–327. [Google Scholar] [CrossRef]
- Lee, C.S.; Marion, J.W.; Lee, J. A Novel Genetic Marker for the Rapid Detection of Bacteroides fragilis in Recreational Water as a Human-Specific Faecal Indicator. J. Water Health 2011, 9, 253–264. [Google Scholar] [CrossRef]
- Jotwani, R.; Kato, N.; Kato, H.; Watanabe, K.; Ueno, K. Detection of Bacteroides fragilis in Clinical Specimens by Polymerase Chain Reaction Amplification of the Neuraminidase Gene. Curr. Microbiol. 1995, 31, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Lee, J. Evaluation of New GyrB-Based Real-Time PCR System for the Detection of B. Fragilis as an Indicator of Human-Specific Fecal Contamination. J. Microbiol. Methods 2010, 82, 311–318. [Google Scholar] [CrossRef]
- Aitchison, A.; Frizelle, F.A.; Keenan, J.I. PCR Detection of the Bacteroides fragilis Enterotoxin Gene Relies on Robust Primer Design. J. Clin. Microbiol. 2016, 54, 239–240. [Google Scholar] [CrossRef]
- Purcell, R.V.; Pearson, J.; Frizelle, F.A.; Keenan, J.I. Comparison of Standard, Quantitative and Digital PCR in the Detection of Enterotoxigenic Bacteroides fragilis. Sci. Rep. 2016, 6, 34554. [Google Scholar] [CrossRef]
- Guo, Y.; Ouyang, Z.; He, W.; Zhang, J.; Qin, Q.; Jiao, M.; Muyldermans, S.; Zheng, F.; Wen, Y. Screening and Epitope Characterization of Diagnostic Nanobody against Total and Activated Bacteroides fragilis Toxin. Front. Immunol. 2023, 14, 1065274. [Google Scholar] [CrossRef]
- Mootien, S.; Kaplan, P.M. Monoclonal Antibodies Specific for Bacteroides fragilis Enterotoxins BFT1 and BFT2 and Their Use in Immunoassays. PLoS ONE 2017, 12, e0173128. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Alesanco, A.; Eckhard, U.; Asencio del Rio, M.; Vega, S.; Guevara, T.; Velazquez-Campoy, A.; Gomis-Rüth, F.X.; Abian, O. Repositioning Small Molecule Drugs as Allosteric Inhibitors of the BFT-3 Toxin from Enterotoxigenic Bacteroides fragilis. Protein Sci. 2022, 31, e4427. [Google Scholar] [CrossRef] [PubMed]
- Mathipa, M.G.; Thantsha, M.S. Probiotic Engineering: Towards Development of Robust Probiotic Strains with Enhanced Functional Properties and for Targeted Control of Enteric Pathogens. Gut Pathog. 2017, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Odamaki, T.; Sugahara, H.; Yonezawa, S.; Yaeshima, T.; Iwatsuki, K.; Tanabe, S.; Tominaga, T.; Togashi, H.; Benno, Y.; Xiao, J. Effect of the Oral Intake of Yogurt Containing Bifidobacterium Longum BB536 on the Cell Numbers of Enterotoxigenic Bacteroides fragilis in Microbiota. Anaerobe 2012, 18, 14–18. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jasemi, S.; Molicotti, P.; Fais, M.; Cossu, I.; Simula, E.R.; Sechi, L.A. Biological Mechanisms of Enterotoxigenic Bacteroides fragilis Toxin: Linking Inflammation, Colorectal Cancer, and Clinical Implications. Toxins 2025, 17, 305. https://doi.org/10.3390/toxins17060305
Jasemi S, Molicotti P, Fais M, Cossu I, Simula ER, Sechi LA. Biological Mechanisms of Enterotoxigenic Bacteroides fragilis Toxin: Linking Inflammation, Colorectal Cancer, and Clinical Implications. Toxins. 2025; 17(6):305. https://doi.org/10.3390/toxins17060305
Chicago/Turabian StyleJasemi, Seyedesomaye, Paola Molicotti, Milena Fais, Ilaria Cossu, Elena Rita Simula, and Leonardo A. Sechi. 2025. "Biological Mechanisms of Enterotoxigenic Bacteroides fragilis Toxin: Linking Inflammation, Colorectal Cancer, and Clinical Implications" Toxins 17, no. 6: 305. https://doi.org/10.3390/toxins17060305
APA StyleJasemi, S., Molicotti, P., Fais, M., Cossu, I., Simula, E. R., & Sechi, L. A. (2025). Biological Mechanisms of Enterotoxigenic Bacteroides fragilis Toxin: Linking Inflammation, Colorectal Cancer, and Clinical Implications. Toxins, 17(6), 305. https://doi.org/10.3390/toxins17060305





