Potential of Venom-Derived Compounds for the Development of New Antimicrobial Agents
Abstract
1. Introduction
2. Venomous Animals as a Source of Antimicrobial Compounds
2.1. Antimicrobial Agents from Snakes
2.2. Antimicrobial Agents from Scorpions
2.3. Antimicrobial Agents from Spiders
2.4. Anti-Microbial Agents from Honeybees
2.5. Antimicrobial Agents from Wasps
2.6. Antimicrobial Agents from Ants
3. Mechanisms of Action of Venom-Based Anti-Microbial Agents
3.1. Antibacterial and Antifungal Mechanisms of the Action of Animal Venom
3.2. Antiviral Mechanisms of the Action of Animal Venom
3.3. Antiparasitic Mechanisms of the Action of Animal Venom
4. Synergistic Interactions and Combination Therapies
4.1. Css54 AMP
4.2. Macropin
4.3. Honeybee Venom and Its Melittin
5. Future Prospects and Challenges of Venom-Derived AMPs
5.1. Pharmacokinetic Barriers and Administration Challenges
5.2. Toxicity and Selectivity Issues
5.3. Production and Purity
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Staphylococcus aureus | S. aureus |
| Staphylococcus epidermidis | S. epidermidis |
| Pseudomonas aeruginosa | P. aeruginosa |
| Klebsiella pneumoniae | K. pneumoniae |
| Escherichia coli | E. coli |
| Bacillus cereus | B. cereus |
| Plasmodium berghei | P. berghei |
| Plasmodium falciparum | P. falciparum |
| Bacillus subtilis | B. subtilis |
| Bee Venom | BV |
| Helicobacter pylori | H. pylori |
| Candida auris | C. auris |
References
- Baker, R.E.; Mahmud, A.S.; Miller, I.F.; Rajeev, M.; Rasambainarivo, F.; Rice, B.L.; Takahashi, S.; Tatem, A.J.; Wagner, C.E.; Wang, L.-F.; et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 2022, 20, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Salam, M.A.; Al-Amin, M.Y.; Salam, M.T.; Pawar, J.S.; Akhter, N.; Rabaan, A.A.; Alqumber, M.A.A. Antimicrobial Resistance: A Growing Serious Threat for Global Public Health. Healthcare 2023, 11, 1946. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Gulumbe, B.H.; Sahal, M.R.; Abdulrahim, A.; Faggo, A.A.; Yusuf, Z.M.; Sambo, K.H.; Usman, N.I.; Bagwai, M.A.; Muhammad, W.N.; Adamu, A.; et al. Antibiotic resistance and the COVID-19 pandemic: A dual crisis with complex challenges in LMICs. Health Sci. Rep. 2023, 6, e1566. [Google Scholar] [CrossRef]
- Liu, B.; Pop, M. ARDB—Antibiotic Resistance Genes Database. Nucleic Acids Res. 2009, 37, D443–D447. [Google Scholar] [CrossRef]
- Woodman, M.E.; Worth, R.G.; Wooten, R.M. Capsule influences the deposition of critical complement C3 levels required for the killing of Burkholderia pseudomallei via NADPH-oxidase induction by human neutrophils. PLoS ONE 2012, 7, e52276. [Google Scholar] [CrossRef]
- Nelson, M.; Nunez, A.; Ngugi, S.A.; Sinclair, A.; Atkins, T.P. Characterization of lesion formation in marmosets following inhalational challenge with different strains of Burkholderia pseudomallei. Int. J. Exp. Pathol. 2015, 96, 414–426. [Google Scholar] [CrossRef]
- Lowy, F.D. Staphylococcus aureus infections. N. Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef]
- Guo, J.; Zhang, H.; Lin, W.; Lu, L.; Su, J.; Chen, X. Signaling pathways and targeted therapies for psoriasis. Signal Transduct. Target. Ther. 2023, 8, 437. [Google Scholar] [CrossRef]
- Ko, S.J.; Park, E.; Asandei, A.; Choi, J.Y.; Lee, S.C.; Seo, C.H.; Luchian, T.; Park, Y. Bee venom-derived antimicrobial peptide melectin has broad-spectrum potency, cell selectivity, and salt-resistant properties. Sci. Rep. 2020, 10, 10145. [Google Scholar] [CrossRef]
- Utkin, Y.N. Animal venom studies: Current benefits and future developments. World J. Biol. Chem. 2015, 6, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Bordon, K.d.C.F.; Cologna, C.T.; Fornari-Baldo, E.C.; Pinheiro-Júnior, E.L.; Cerni, F.A.; Amorim, F.G.; Anjolette, F.A.P.; Cordeiro, F.A.; Wiezel, G.A.; Cardoso, I.A.; et al. From Animal Poisons and Venoms to Medicines: Achievements, Challenges and Perspectives in Drug Discovery. Front. Pharmacol. 2020, 11, 1132. [Google Scholar] [CrossRef] [PubMed]
- Yacoub, T.; Rima, M.; Karam, M.; Fajloun, J. Antimicrobials from Venomous Animals: An Overview. Molecules 2020, 25, 2402. [Google Scholar] [CrossRef] [PubMed]
- Perumal Samy, R.; Stiles, B.G.; Franco, O.L.; Sethi, G.; Lim, L.H.K. Animal venoms as antimicrobial agents. Biochem. Pharmacol. 2017, 134, 127–138. [Google Scholar] [CrossRef]
- Costa Torres, A.F.; Dantas, R.T.; Toyama, M.H.; Diz Filho, E.; Zara, F.J.; Rodrigues de Queiroz, M.G.; Pinto Nogueira, N.A.; Rosa de Oliveira, M.; de Oliveira Toyama, D.; Monteiro, H.S.; et al. Antibacterial and antiparasitic effects of Bothrops marajoensis venom and its fractions: Phospholipase A2 and L-amino acid oxidase. Toxicon 2010, 55, 795–804. [Google Scholar] [CrossRef]
- de Oliveira, A.N.; Soares, A.M.; da Silva, S.L. Peptides from Animal Venom and Poisons. Int. J. Pept. Res. Ther. 2023, 29, 83. [Google Scholar] [CrossRef]
- A. Al-Shammery, K.; Hozzein, W.N. Antibacterial activities of two potential peptides extracted from Polistes wattii Cameron, 1900 (Vespidae: Polistinae) wasp venom collected at Eastern Province, Saudi Arabia. PLoS ONE 2022, 17, e0264035. [Google Scholar] [CrossRef]
- Benfield, A.H.; Henriques, S.T. Mode-of-Action of Antimicrobial Peptides: Membrane Disruption vs. Intracellular Mechanisms. Front. Med. Technol. 2020, 2, 610997. [Google Scholar] [CrossRef]
- Sabapathy, T.; Deplazes, E.; Mancera, R.L. Revisiting the Interaction of Melittin with Phospholipid Bilayers: The Effects of Concentration and Ionic Strength. Int. J. Mol. Sci. 2020, 21, 746. [Google Scholar] [CrossRef]
- Beschiaschvili, G.; Seelig, J. Melittin binding to mixed phosphatidylglycerol/phosphatidylcholine membranes. Biochemistry 1990, 29, 52–58. [Google Scholar] [CrossRef]
- Marte, F.; Sankar, P.; Patel, P.; Cassagnol, M. Captopril. In StatPearls; StatPearls Publishing Copyright © 2024; StatPearls Publishing LLC: Treasure Island, FL, USA, 2024. [Google Scholar]
- Kumar, A.; Herrmann, H.C. Tirofiban: An investigational platelet glycoprotein IIb/IIIa receptor antagonist. Expert. Opin. Investig. Drugs 1997, 6, 1257–1267. [Google Scholar] [CrossRef] [PubMed]
- Bansal, A.B.; Sattar, Y.; Patel, P.; Jamil, R.T. Eptifibatide. In StatPearls; StatPearls Publishing Copyright © 2024; StatPearls Publishing LLC: Treasure Island, FL, USA, 2024. [Google Scholar]
- Vu, T.T.; Stafford, A.R.; Leslie, B.A.; Kim, P.Y.; Fredenburgh, J.C.; Weitz, J.I. Batroxobin binds fibrin with higher affinity and promotes clot expansion to a greater extent than thrombin. J. Biol. Chem. 2013, 288, 16862–16871. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.M. Exenatide. Am. J. Health Syst. Pharm. 2006, 63, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Wie, C.S.; Derian, A. Ziconotide. In StatPearls; StatPearls Publishing Copyright © 2024; StatPearls Publishing LLC: Treasure Island, FL, USA, 2024. [Google Scholar]
- Ram, C.V. Captopril. Arch. Intern. Med. 1982, 142, 914–916. [Google Scholar] [CrossRef]
- USDA. Drug Approval Package: Integrilin (Eptifibatide) NDA #20-718. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/98/20718_Integrilin.cfm (accessed on 18 May 1998).
- USDA. Drug Approval Package: Aggrastat (Tirofiban Hydrochloride) NDA 20-912. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/99/20912S001_Aggrastat.cfm (accessed on 9 July 1999).
- USDA. Drug Approval Package: Prialt (Ziconotide Intrathecal Infusion) NDA 21-060. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2004/21-060_Prialt.cfm (accessed on 28 December 2004).
- USDA. Drug Approval Package: Byetta (Exenatide) NDA #021773. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/021773_byettatoc.cfm (accessed on 28 April 2005).
- Tarcha, E.J.; Olsen, C.M.; Probst, P.; Peckham, D.; Muñoz-Elías, E.J.; Kruger, J.G.; Iadonato, S.P. Safety and pharmacodynamics of dalazatide, a Kv1.3 channel inhibitor, in the treatment of plaque psoriasis: A randomized phase 1b trial. PLoS ONE 2017, 12, e0180762. [Google Scholar] [CrossRef]
- Chassagnon, I.R.; McCarthy, C.A.; Chin, Y.K.; Pineda, S.S.; Keramidas, A.; Mobli, M.; Pham, V.; De Silva, T.M.; Lynch, J.W.; Widdop, R.E.; et al. Potent neuroprotection after stroke afforded by a double-knot spider-venom peptide that inhibits acid-sensing ion channel 1a. Proc. Natl. Acad. Sci. USA 2017, 114, 3750–3755. [Google Scholar] [CrossRef]
- Dardevet, L.; Rani, D.; Aziz, T.A.; Bazin, I.; Sabatier, J.M.; Fadl, M.; Brambilla, E.; De Waard, M. Chlorotoxin: A helpful natural scorpion peptide to diagnose glioma and fight tumor invasion. Toxins 2015, 7, 1079–1101. [Google Scholar] [CrossRef]
- Lee, M.L.; Tan, N.H.; Fung, S.Y.; Sekaran, S.D. Antibacterial action of a heat-stable form of L-amino acid oxidase isolated from king cobra (Ophiophagus hannah) venom. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2011, 153, 237–242. [Google Scholar] [CrossRef]
- Yamane, E.S.; Bizerra, F.C.; Oliveira, E.B.; Moreira, J.T.; Rajabi, M.; Nunes, G.L.; de Souza, A.O.; da Silva, I.D.; Yamane, T.; Karpel, R.L.; et al. Unraveling the antifungal activity of a South American rattlesnake toxin crotamine. Biochimie 2013, 95, 231–240. [Google Scholar] [CrossRef]
- El Chamy Maluf, S.; Dal Mas, C.; Oliveira, E.B.; Melo, P.M.; Carmona, A.K.; Gazarini, M.L.; Hayashi, M.A. Inhibition of malaria parasite Plasmodium falciparum development by crotamine, a cell penetrating peptide from the snake venom. Peptides 2016, 78, 11–16. [Google Scholar] [CrossRef]
- Wei, L.; Gao, J.; Zhang, S.; Wu, S.; Xie, Z.; Ling, G.; Kuang, Y.-Q.; Yang, Y.; Yu, H.; Wang, Y. Identification and Characterization of the First Cathelicidin from Sea Snakes with Potent Antimicrobial and Anti-inflammatory Activity and Special Mechanism. J. Biol. Chem. 2015, 290, 16633–16652. [Google Scholar] [CrossRef] [PubMed]
- Carlile, S.R.; Shiels, J.; Kerrigan, L.; Delaney, R.; Megaw, J.; Gilmore, B.F.; Weldon, S.; Dalton, J.P.; Taggart, C.C. Sea snake cathelicidin (Hc-cath) exerts a protective effect in mouse models of lung inflammation and infection. Sci. Rep. 2019, 9, 6071. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hong, J.; Liu, X.; Yang, H.; Liu, R.; Wu, J.; Wang, A.; Lin, D.; Lai, R. Snake Cathelicidin from Bungarus fasciatus Is a Potent Peptide Antibiotics. PLoS ONE 2008, 3, e3217. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Z.; Chen, L.; Guang, H.; Li, Z.; Yang, H.; Li, J.; You, D.; Yu, H.; Lai, R. Cathelicidin-BF, a Snake Cathelicidin-Derived Antimicrobial Peptide, Could Be an Excellent Therapeutic Agent for Acne Vulgaris. PLoS ONE 2011, 6, e22120. [Google Scholar] [CrossRef]
- Sudarshan, S.; Dhananjaya, B.L. Antibacterial activity of an acidic phospholipase A2 (NN-XIb-PLA2) from the venom of Naja naja (Indian cobra). Springerplus 2016, 5, 112. [Google Scholar] [CrossRef]
- Nair, D.G.; Fry, B.G.; Alewood, P.; Kumar, P.P.; Kini, R.M. Antimicrobial activity of omwaprin, a new member of the waprin family of snake venom proteins. Biochem. J. 2007, 402, 93–104. [Google Scholar] [CrossRef]
- Samy, R.P.; Kandasamy, M.; Gopalakrishnakone, P.; Stiles, B.G.; Rowan, E.G.; Becker, D.; Shanmugam, M.K.; Sethi, G.; Chow, V.T. Wound healing activity and mechanisms of action of an antibacterial protein from the venom of the eastern diamondback rattlesnake (Crotalus adamanteus). PLoS ONE 2014, 9, e80199. [Google Scholar] [CrossRef]
- Dai, C.; Ma, Y.; Zhao, Z.; Zhao, R.; Wang, Q.; Wu, Y.; Cao, Z.; Li, W. Mucroporin, the first cationic host defense peptide from the venom of Lychas mucronatus. Antimicrob. Agents Chemother. 2008, 52, 3967–3972. [Google Scholar] [CrossRef]
- Li, Q.; Zhao, Z.; Zhou, D.; Chen, Y.; Hong, W.; Cao, L.; Yang, J.; Zhang, Y.; Shi, W.; Cao, Z.; et al. Virucidal activity of a scorpion venom peptide variant mucroporin-M1 against measles, SARS-CoV and influenza H5N1 viruses. Peptides 2011, 32, 1518–1525. [Google Scholar] [CrossRef]
- Zhao, Z.; Hong, W.; Zeng, Z.; Wu, Y.; Hu, K.; Tian, X.; Li, W.; Cao, Z. Mucroporin-M1 inhibits hepatitis B virus replication by activating the mitogen-activated protein kinase (MAPK) pathway and down-regulating HNF4α in vitro and in vivo. J. Biol. Chem. 2012, 287, 30181–30190. [Google Scholar] [CrossRef]
- Zeng, X.-C.; Zhou, L.; Shi, W.; Luo, X.; Zhang, L.; Nie, Y.; Wang, J.; Wu, S.; Cao, B.; Cao, H. Three new antimicrobial peptides from the scorpion Pandinus imperator. Peptides 2013, 45, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.C.; Wang, S.X.; Zhu, Y.; Zhu, S.Y.; Li, W.X. Identification and functional characterization of novel scorpion venom peptides with no disulfide bridge from Buthus martensii Karsch. Peptides 2004, 25, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Dai, C.; Li, Z.; Fan, Z.; Song, Y.; Wu, Y.; Cao, Z.; Li, W. Antibacterial activity and mechanism of a scorpion venom peptide derivative in vitro and in vivo. PLoS ONE 2012, 7, e40135. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Cao, L.; Zhong, M.; Zhang, Y.; Han, C.; Li, Q.; Yang, J.; Zhou, D.; Shi, W.; He, B.; et al. Anti-HIV-1 activity of a new scorpion venom peptide derivative Kn2-7. PLoS ONE 2012, 7, e34947. [Google Scholar] [CrossRef]
- Du, Q.; Hou, X.; Wang, L.; Zhang, Y.; Xi, X.; Wang, H.; Zhou, M.; Duan, J.; Wei, M.; Chen, T.; et al. AaeAP1 and AaeAP2: Novel Antimicrobial Peptides from the Venom of the Scorpion, Androctonus aeneas: Structural Characterisation, Molecular Cloning of Biosynthetic Precursor-Encoding cDNAs and Engineering of Analogues with Enhanced Antimicrobial and Anticancer Activities. Toxins 2015, 7, 219–237. [Google Scholar] [CrossRef]
- Zhao, Z.; Ma, Y.; Dai, C.; Zhao, R.; Li, S.; Wu, Y.; Cao, Z.; Li, W. Imcroporin, a new cationic antimicrobial peptide from the venom of the scorpion Isometrus maculates. Antimicrob. Agents Chemother. 2009, 53, 3472–3477. [Google Scholar] [CrossRef]
- Budnik, B.A.; Olsen, J.V.; Egorov, T.A.; Anisimova, V.E.; Galkina, T.G.; Musolyamov, A.K.; Grishin, E.V.; Zubarev, R.A. De novo sequencing of antimicrobial peptides isolated from the venom glands of the wolf spider Lycosa singoriensis. J. Mass. Spectrom. 2004, 39, 193–201. [Google Scholar] [CrossRef]
- Yan, S.; Wu, G. Detailed folding structures of M-lycotoxin-Hc1a and its mutageneses using 2D HP model. Mol. Simul. 2012, 38, 809–822. [Google Scholar] [CrossRef]
- Segura-Ramírez, P.J.; Silva Júnior, P.I. Loxosceles gaucho Spider Venom: An Untapped Source of Antimicrobial Agents. Toxins 2018, 10, 522. [Google Scholar] [CrossRef]
- Choi, J.H.; Jang, A.Y.; Lin, S.; Lim, S.; Kim, D.; Park, K.; Han, S.M.; Yeo, J.H.; Seo, H.S. Melittin, a honeybee venom-derived antimicrobial peptide, may target methicillin-resistant Staphylococcus aureus. Mol. Med. Rep. 2015, 12, 6483–6490. [Google Scholar] [CrossRef]
- Zhang, H.-Q.; Sun, C.; Xu, N.; Liu, W. The current landscape of the antimicrobial peptide melittin and its therapeutic potential. Front. Immunol. 2024, 15, 1326033. [Google Scholar] [CrossRef] [PubMed]
- Baghian, A.; Jaynes, J.; Enright, F.; Kousoulas, K.G. An amphipathic alpha-helical synthetic peptide analogue of melittin inhibits herpes simplex virus-1 (HSV-1)-induced cell fusion and virus spread. Peptides 1997, 18, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Wachinger, M.; Kleinschmidt, A.; Winder, D.; von Pechmann, N.; Ludvigsen, A.; Neumann, M.; Holle, R.; Salmons, B.; Erfle, V.; Brack-Werner, R. Antimicrobial peptides melittin and cecropin inhibit replication of human immunodeficiency virus 1 by suppressing viral gene expression. J. Gen. Virol. 1998, 79 Pt 4, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Al-Rabia, M.W.; Alhakamy, N.A.; Ahmed, O.A.A.; Eljaaly, K.; Alaofi, A.L.; Mostafa, A.; Asfour, H.Z.; Aldarmahi, A.A.; Darwish, K.M.; Ibrahim, T.S.; et al. Repurposing of Sitagliptin- Melittin Optimized Nanoformula against SARS-CoV-2: Antiviral Screening and Molecular Docking Studies. Pharmaceutics 2021, 13, 307. [Google Scholar] [CrossRef]
- Askari, P.; Namaei, M.H.; Ghazvini, K.; Hosseini, M. In vitro and in vivo toxicity and antibacterial efficacy of melittin against clinical extensively drug-resistant bacteria. BMC Pharmacol. Toxicol. 2021, 22, 42. [Google Scholar] [CrossRef]
- Leandro, L.F.; Mendes, C.A.; Casemiro, L.A.; Vinholis, A.H.; Cunha, W.R.; de Almeida, R.; Martins, C.H. Antimicrobial activity of apitoxin, melittin and phospholipase A2 of honey bee (Apis mellifera) venom against oral pathogens. An. Acad. Bras. Cienc. 2015, 87, 147–155. [Google Scholar] [CrossRef]
- Indria Puti Mustika, K.L.M.S.B.W.G. Isolation and Antibacterial Activity of Honey Bee Venom Bioactive from Apis cerana. Int. J. Technol. 2022, 13, 291–319. [Google Scholar] [CrossRef]
- Farag, R.; Swaby, S. Antimicrobial effects of wasp (Vespa orientalis) venom. Egypt. Pharm. J. 2018, 17, 218–222. [Google Scholar]
- Park, N.G.; Yamato, Y.; Lee, S.; Sugihara, G. Interaction of mastoparan-B from venom of a hornet in Taiwan with phospholipid bilayers and its antimicrobial activity. Biopolymers 1995, 36, 793–801. [Google Scholar] [CrossRef]
- Souza, B.M.; Mendes, M.A.; Santos, L.D.; Marques, M.R.; César, L.M.; Almeida, R.N.; Pagnocca, F.C.; Konno, K.; Palma, M.S. Structural and functional characterization of two novel peptide toxins isolated from the venom of the social wasp Polybia paulista. Peptides 2005, 26, 2157–2164. [Google Scholar] [CrossRef]
- Wang, K.; Yan, J.; Chen, R.; Dang, W.; Zhang, B.; Zhang, W.; Song, J.; Wang, R. Membrane-active action mode of polybia-CP, a novel antimicrobial peptide isolated from the venom of Polybia paulista. Antimicrob. Agents Chemother. 2012, 56, 3318–3323. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, D.C.; Flowers, H.; Rockhold, R.; Herath, H.M.T.B.; Nanayakkara, N.P.D. Antibacterial Activity of Synthetic Fire Ant Venom: The Solenopsins and Isosolenopsins. Am. J. Med. Sci. 2009, 338, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Honorato, L.; Artunduaga Bonilla, J.J.; Ribeiro da Silva, L.; Kornetz, J.; Zamith-Miranda, D.; Valdez, A.F.; Nosanchuk, J.D.; Gonçalves Paterson Fox, E.; Nimrichter, L. Alkaloids solenopsins from fire ants display in vitro and in vivo activity against the yeast Candida auris. Virulence 2024, 15, 2413329. [Google Scholar] [CrossRef] [PubMed]
- Orivel, J.; Redeker, V.; Le Caer, J.-P.; Krier, F.; Revol-Junelles, A.-M.; Longeon, A.; Chaffotte, A.; Dejean, A.; Rossier, J. Ponericins, New Antibacterial and Insecticidal Peptides from the Venom of the Ant Pachycondyla goeldii. J. Biol. Chem. 2001, 276, 17823–17829. [Google Scholar] [CrossRef]
- Rifflet, A.; Gavalda, S.; Téné, N.; Orivel, J.; Leprince, J.; Guilhaudis, L.; Génin, E.; Vétillard, A.; Treilhou, M. Identification and characterization of a novel antimicrobial peptide from the venom of the ant Tetramorium bicarinatum. Peptides 2012, 38, 363–370. [Google Scholar] [CrossRef]
- Téné, N.; Bonnafé, E.; Berger, F.; Rifflet, A.; Guilhaudis, L.; Ségalas-Milazzo, I.; Pipy, B.; Coste, A.; Leprince, J.; Treilhou, M. Biochemical and biophysical combined study of bicarinalin, an ant venom antimicrobial peptide. Peptides 2016, 79, 103–113. [Google Scholar] [CrossRef]
- Munawar, A.; Ali, S.A.; Akrem, A.; Betzel, C. Snake Venom Peptides: Tools of Biodiscovery. Toxins 2018, 10, 474. [Google Scholar] [CrossRef]
- Perumal Samy, R.; Gopalakrishnakone, P.; Ho, B.; Chow, V.T. Purification, characterization and bactericidal activities of basic phospholipase A2 from the venom of Agkistrodon halys (Chinese pallas). Biochimie 2008, 90, 1372–1388. [Google Scholar] [CrossRef]
- Abdullahi, Z.U.; Musa, S.S.; Abu-Odah, H.; Ahmed, A.; Lawan, A.A.; Bello, U.M. Bactericidal Effects of Snake Venom Phospholipases A2: A Systematic Review and Analysis of Minimum Inhibitory Concentration. Physiologia 2023, 3, 30–42. [Google Scholar] [CrossRef]
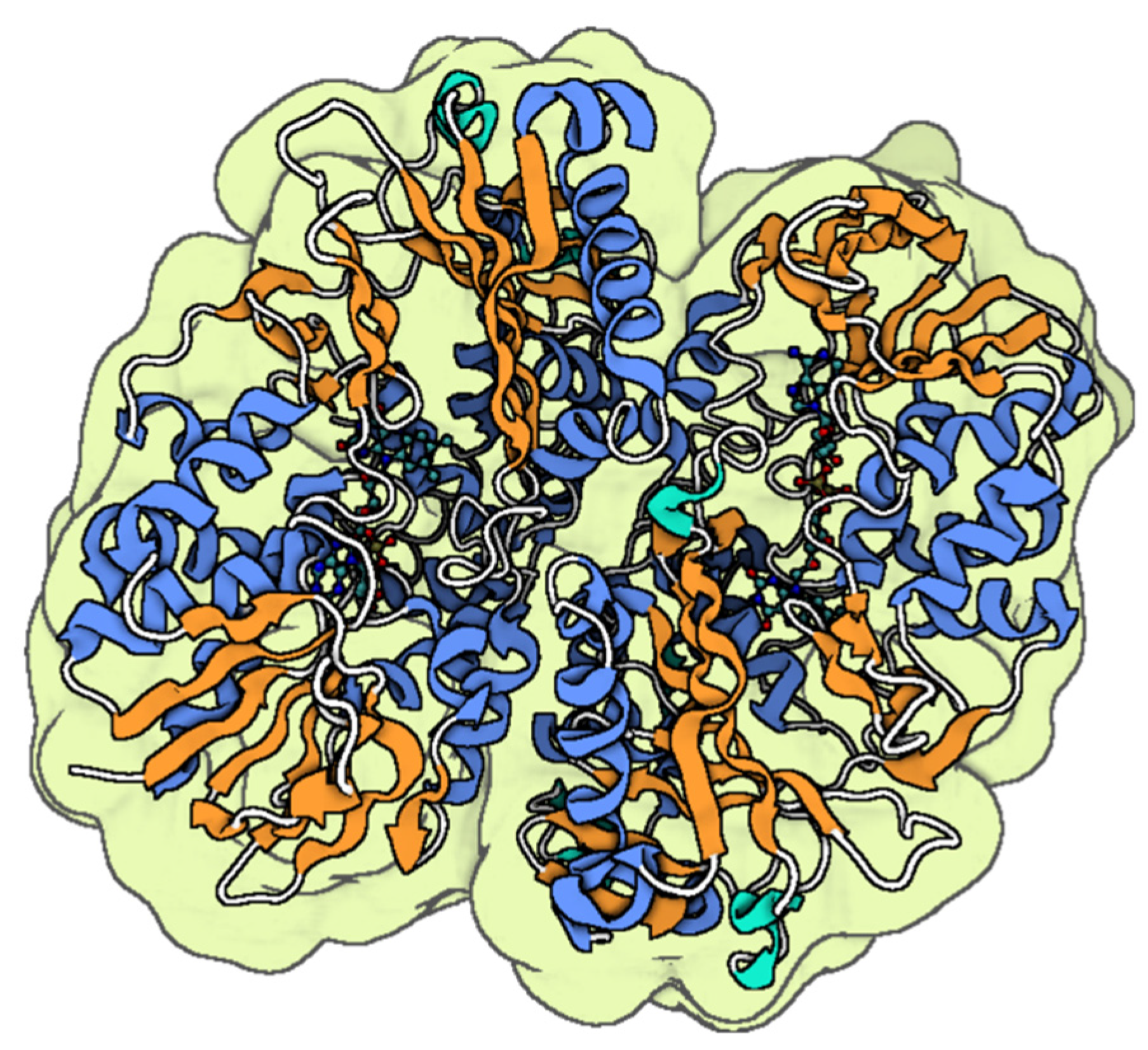
- Xu, S.; Gu, L.; Jiang, T.; Zhou, Y.; Lin, Z. Structures of cadmium-binding acidic phospholipase A2 from the venom of Agkistrodon halys Pallas at 1.9Å resolution. Biochem. Biophys. Res. Commun. 2003, 300, 271–277. [Google Scholar] [CrossRef]
- de Barros, E.; Gonçalves, R.M.; Cardoso, M.H.; Santos, N.C.; Franco, O.L.; Cândido, E.S. Snake Venom Cathelicidins as Natural Antimicrobial Peptides. Front. Pharmacol. 2019, 10, 1415. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; Samuel, R.L.; Massiah, M.A.; Gillmor, S.D. The structure and behavior of the NA-CATH antimicrobial peptide with liposomes. Biochim. Et Biophys. Acta (BBA)-Biomembr. 2015, 1848, 2394–2405. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhao, H.; Gan, T.-X.; Liu, X.-D.; Jin, Y.; Lee, W.-H.; Shen, J.-H.; Zhang, Y. Identification and characterization of novel reptile cathelicidins from elapid snakes. Peptides 2008, 29, 1685–1691. [Google Scholar] [CrossRef]
- Li, S.A.; Lee, W.H.; Zhang, Y. Efficacy of OH-CATH30 and its analogs against drug-resistant bacteria in vitro and in mouse models. Antimicrob. Agents Chemother. 2012, 56, 3309–3317. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Zhang, F.; Guo, Z.; Chen, Y.; Zhang, M.; Yu, H.; Wang, Y. Characterization of a Cathelicidin from the Colubrinae Snake, Sinonatrix annularis. Zool. Sci. 2019, 36, 68–76. [Google Scholar] [CrossRef]
- Cai, S.; Qiao, X.; Feng, L.; Shi, N.; Wang, H.; Yang, H.; Guo, Z.; Wang, M.; Chen, Y.; Wang, Y.; et al. Python Cathelicidin CATHPb1 Protects against Multidrug-Resistant Staphylococcal Infections by Antimicrobial-Immunomodulatory Duality. J. Med. Chem. 2018, 61, 2075–2086. [Google Scholar] [CrossRef]
- Falcao, C.B.; de La Torre, B.G.; Pérez-Peinado, C.; Barron, A.E.; Andreu, D.; Rádis-Baptista, G. Vipericidins: A novel family of cathelicidin-related peptides from the venom gland of South American pit vipers. Amino Acids 2014, 46, 2561–2571. [Google Scholar] [CrossRef]
- Falcao, C.B.; Pérez-Peinado, C.; de la Torre, B.G.; Mayol, X.; Zamora-Carreras, H.; Jiménez, M.; Rádis-Baptista, G.; Andreu, D. Structural Dissection of Crotalicidin, a Rattlesnake Venom Cathelicidin, Retrieves a Fragment with Antimicrobial and Antitumor Activity. J. Med. Chem. 2015, 58, 8553–8563. [Google Scholar] [CrossRef]
- Quintana, J.C.; Chacón, A.M.; Vargas, L.; Segura, C.; Gutiérrez, J.M.; Alarcón, J.C. Antiplasmodial effect of the venom of Crotalus durissus cumanensis, crotoxin complex and Crotoxin B. Acta Trop. 2012, 124, 126–132. [Google Scholar] [CrossRef]
- Banigan, J.R.; Mandal, K.; Sawaya, M.R.; Thammavongsa, V.; Hendrickx, A.P.; Schneewind, O.; Yeates, T.O.; Kent, S.B. Determination of the X-ray structure of the snake venom protein omwaprin by total chemical synthesis and racemic protein crystallography. Protein Sci. 2010, 19, 1840–1849. [Google Scholar] [CrossRef]
- Rádis-Baptista, G.; Moreno, F.B.M.B.; Nogueira, L.d.L.; Martins, A.M.C.; Toyama, D.d.O.; Toyama, M.H.; Cavada, B.S.; de Azevedo, W.F.; Yamane, T. Crotacetin, a novel snake venom C-type lectin homolog of convulxin, exhibits an unpredictable antimicrobial activity. Cell Biochem. Biophys. 2006, 44, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Souza, T.A.; Abrego, J.R.; Betzel, C.; Murakami, M.T.; Arni, R.K. Structural insights into selectivity and cofactor binding in snake venom L-amino acid oxidases. Biochem. Biophys. Res. Commun. 2012, 421, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Sulca, M.A.; Remuzgo, C.; Cárdenas, J.; Kiyota, S.; Cheng, E.; Bemquerer, M.P.; Machini, M.T. Venom of the Peruvian snake Bothriopsis oligolepis: Detection of antibacterial activity and involvement of proteolytic enzymes and C-type lectins in growth inhibition of Staphylococcus aureus. Toxicon 2017, 134, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Okumu, M.O.; Eyaan, K.L.; Bett, L.K.; Gitahi, N. Antibacterial Activity of Venom from the Puff Adder (Bitis arietans), Egyptian Cobra (Naja haje), and Red Spitting Cobra (Naja pallida). Int. J. Microbiol. 2023, 2023, 7924853. [Google Scholar] [CrossRef]
- Ortiz, E.; Gurrola, G.B.; Schwartz, E.F.; Possani, L.D. Scorpion venom components as potential candidates for drug development. Toxicon 2015, 93, 125–135. [Google Scholar] [CrossRef]
- Rincón-Cortés, C.A.; Bayona-Rojas, M.A.; Reyes-Montaño, E.A.; Vega-Castro, N.A. Antimicrobial Activity Developed by Scorpion Venoms and Its Peptide Component. Toxins 2022, 14, 740. [Google Scholar] [CrossRef]
- Moerman, L.; Bosteels, S.; Noppe, W.; Willems, J.; Clynen, E.; Schoofs, L.; Thevissen, K.; Tytgat, J.; Van Eldere, J.; Van Der Walt, J.; et al. Antibacterial and antifungal properties of alpha-helical, cationic peptides in the venom of scorpions from southern Africa. Eur. J. Biochem. 2002, 269, 4799–4810. [Google Scholar] [CrossRef]
- Bao, A.; Zhong, J.; Zeng, X.-C.; Nie, Y.; Zhang, L.; Peng, Z.F. A novel cysteine-free venom peptide with strong antimicrobial activity against antibiotics-resistant pathogens from the scorpion Opistophthalmus glabrifrons. J. Pept. Sci. 2015, 21, 758–764. [Google Scholar] [CrossRef]
- Guilhelmelli, F.; Vilela, N.; Smidt, K.S.; de Oliveira, M.A.; da Cunha Morales Álvares, A.; Rigonatto, M.C.L.; da Silva Costa, P.H.; Tavares, A.H.; Freitas, S.M.d.; Nicola, A.M.; et al. Activity of Scorpion Venom-Derived Antifungal Peptides against Planktonic Cells of Candida spp. and Cryptococcus neoformans and Candida albicans Biofilms. Front. Microbiol. 2016, 7, 1844. [Google Scholar] [CrossRef]
- Harrison, P.L.; Abdel-Rahman, M.A.; Miller, K.; Strong, P.N. Antimicrobial peptides from scorpion venoms. Toxicon 2014, 88, 115–137. [Google Scholar] [CrossRef]
- Gao, B.; Xu, J.; Rodriguez Mdel, C.; Lanz-Mendoza, H.; Hernández-Rivas, R.; Du, W.; Zhu, S. Characterization of two linear cationic antimalarial peptides in the scorpion Mesobuthus eupeus. Biochimie 2010, 92, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, G. Insights into Antimicrobial Peptides from Spiders and Scorpions. Protein Pept. Lett. 2016, 23, 707–721. [Google Scholar] [CrossRef] [PubMed]
- Santos, D.M.; Reis, P.V.; Pimenta, A.M.C. Antimicrobial Peptides in Spider Venoms. In Spider Venoms; Gopalakrishnakone, P., Corzo, G.A., Diego-Garcia, E., de Lima, M.E., Eds.; Springer: Dordrecht, The Netherlands, 2015; pp. 1–15. [Google Scholar]
- Shin, M.K.; Hwang, I.-W.; Jang, B.-Y.; Bu, K.-B.; Han, D.-H.; Lee, S.-H.; Oh, J.W.; Yoo, J.S.; Sung, J.-S. The Identification of a Novel Spider Toxin Peptide, Lycotoxin-Pa2a, with Antibacterial and Anti-Inflammatory Activities. Antibiotics 2023, 12, 1708. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.K.; Hwang, I.-W.; Jang, B.-Y.; Bu, K.-B.; Yoo, J.S.; Sung, J.-S. In silico identification of novel antimicrobial peptides from the venom gland transcriptome of the spider Argiope bruennichi (Scopoli, 1772). Front. Microbiol. 2023, 14, 1249175. [Google Scholar] [CrossRef]
- Kim, W. Bee Venom and Its Sub-Components: Characterization, Pharmacology, and Therapeutics. Toxins 2021, 13, 191. [Google Scholar] [CrossRef]
- Wehbe, R.; Frangieh, J.; Rima, M.; El Obeid, D.; Sabatier, J.-M.; Fajloun, Z. Bee Venom: Overview of Main Compounds and Bioactivities for Therapeutic Interests. Molecules 2019, 24, 2997. [Google Scholar] [CrossRef]
- Yuva, B. Bee Venom: Its Potential Use in Alternative Medicine. Anti-Infect. Agents 2015, 13, 3–16. [Google Scholar] [CrossRef]
- Han, S.M.; Kim, J.M.; Hong, I.P.; Woo, S.O.; Kim, S.G.; Jang, H.R.; Pak, S.C. Antibacterial Activity and Antibiotic-Enhancing Effects of Honeybee Venom against Methicillin-Resistant Staphylococcus aureus. Molecules 2016, 21, 79. [Google Scholar] [CrossRef]
- Han, S.; Yeo, J.; Baek, H.; Lin, S.M.; Meyer, S.; Molan, P. Postantibiotic effect of purified melittin from honeybee (Apis mellifera) venom against Escherichia coli and Staphylococcus aureus. J. Asian Nat. Prod. Res. 2009, 11, 796–804. [Google Scholar] [CrossRef]
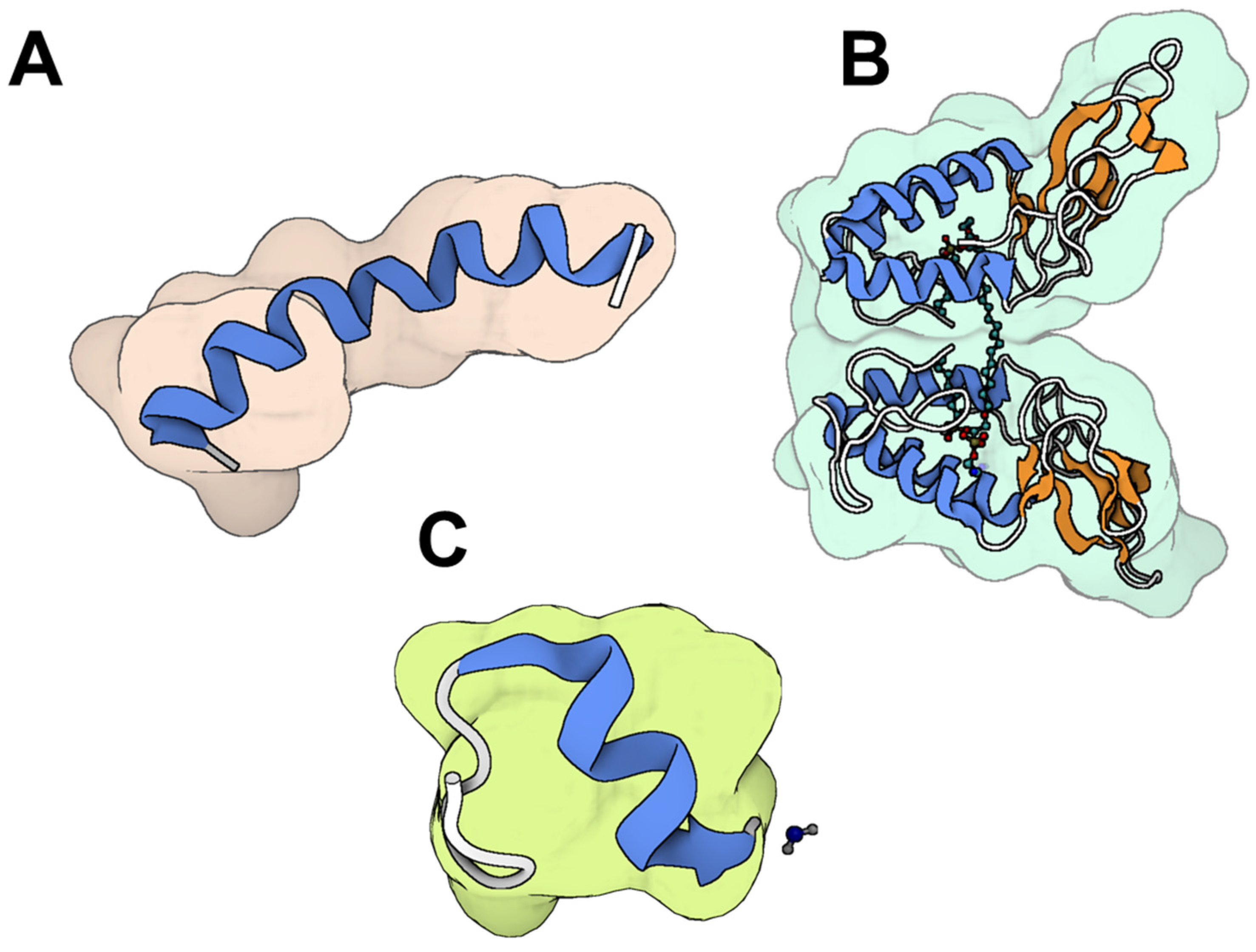
- Ramirez, L.S.; Pande, J.; Shekhtman, A. Helical Structure of Recombinant Melittin. J. Phys. Chem. B 2019, 123, 356–368. [Google Scholar] [CrossRef]
- Scott, D.L.; Otwinowski, Z.; Gelb, M.H.; Sigler, P.B. Crystal structure of bee-venom phospholipase A2 in a complex with a transition-state analogue. Science 1990, 250, 1563–1566. [Google Scholar] [CrossRef] [PubMed]
- Kuzmenkov, A.I.; Peigneur, S.; Nasburg, J.A.; Mineev, K.S.; Nikolaev, M.V.; Pinheiro-Junior, E.L.; Arseniev, A.S.; Wulff, H.; Tytgat, J.; Vassilevski, A.A. Apamin structure and pharmacology revisited. Front. Pharmacol. 2022, 13, 977440. [Google Scholar] [CrossRef] [PubMed]
- Socarras, K.M.; Theophilus, P.A.S.; Torres, J.P.; Gupta, K.; Sapi, E. Antimicrobial Activity of Bee Venom and Melittin against Borrelia burgdorferi. Antibiotics 2017, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.B.; Lee, B.-H.; Nikapitiya, C.; Kim, J.-H.; Kim, T.-H.; Lee, H.-C.; Kim, C.G.; Lee, J.-S.; Kim, C.-J. Inhibitory effects of bee venom and its components against viruses in vitro and in vivo. J. Microbiol. 2016, 54, 853–866. [Google Scholar] [CrossRef]
- Yu, A.-R.; Kim, J.-J.; Park, G.-S.; Oh, S.-M.; Han, C.-S.; Lee, M.-Y. The antifungal activity of bee venom against dermatophytes. J. Appl. Biol. Chem. 2012, 55, 7–11. [Google Scholar] [CrossRef]
- Lee, S.B. Antifungal Activity of Bee Venom and Sweet Bee Venom against Clinically Isolated Candida albicans. J. Pharmacopunct. 2016, 19, 45–50. [Google Scholar] [CrossRef]
- Al-Ani, I.; Zimmermann, S.; Reichling, J.; Wink, M. Pharmacological synergism of bee venom and melittin with antibiotics and plant secondary metabolites against multi-drug resistant microbial pathogens. Phytomedicine 2015, 22, 245–255. [Google Scholar] [CrossRef]
- Luo, L.; Kamau, P.M.; Lai, R. Bioactive Peptides and Proteins from Wasp Venoms. Biomolecules 2022, 12, 527. [Google Scholar] [CrossRef]
- Bulet, P.; Stöcklin, R.; Menin, L. Anti-microbial peptides: From invertebrates to vertebrates. Immunol. Rev. 2004, 198, 169–184. [Google Scholar] [CrossRef]
- Reddy, K.V.; Yedery, R.D.; Aranha, C. Antimicrobial peptides: Premises and promises. Int. J. Antimicrob. Agents 2004, 24, 536–547. [Google Scholar] [CrossRef]
- Jalaei, J.; Fazeli, M.; Rajaian, H.; Shekarforoush, S.S. In vitro antibacterial effect of wasp (Vespa orientalis) venom. J. Venom. Anim. Toxins Incl. Trop. Dis. 2014, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Katsu, T.; Kuroko, M.; Morikawa, T.; Sanchika, K.; Yamanaka, H.; Shinoda, S.; Fujita, Y. Interaction of wasp venom mastoparan with biomembranes. Biochim. Et Biophys. Acta (BBA)-Biomembr. 1990, 1027, 185–190. [Google Scholar] [CrossRef]
- Lin, C.H.; Tzen, J.T.; Shyu, C.L.; Yang, M.J.; Tu, W.C. Structural and biological characterization of mastoparans in the venom of Vespa species in Taiwan. Peptides 2011, 32, 2027–2036. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Wang, Y.; Lee, W.H.; Zhang, Y. Antimicrobial peptides from the venom gland of the social wasp Vespa tropica. Toxicon 2013, 74, 151–157. [Google Scholar] [CrossRef]
- Boaro, A.; Ageitos, L.; Torres, M.D.T.; Blasco, E.B.; Oztekin, S.; de la Fuente-Nunez, C. Structure-function-guided design of synthetic peptides with anti-infective activity derived from wasp venom. Cell Rep. Phys. Sci. 2023, 4, 101459. [Google Scholar] [CrossRef]
- Torres, M.D.T.; Silva, A.F.; Andrade, G.P.; Pedron, C.N.; Cerchiaro, G.; Ribeiro, A.O.; Oliveira, V.X., Jr.; de la Fuente-Nunez, C. The wasp venom antimicrobial peptide polybia-CP and its synthetic derivatives display antiplasmodial and anticancer properties. Bioeng. Transl. Med. 2020, 5, e10167. [Google Scholar] [CrossRef]
- Blum, M.S. Ant Venoms: Chemical and Pharmacological Properties. J. Toxicol. Toxin Rev. 1992, 11, 115–164. [Google Scholar] [CrossRef]
- Xu, G.; Chen, L. Biological Activities and Ecological Significance of Fire Ant Venom Alkaloids. Toxins 2023, 15, 439. [Google Scholar] [CrossRef]
- Chen, L.; Fadamiro, H.Y. Re-investigation of venom chemistry of Solenopsis fire ants. II. Identification of novel alkaloids in S. invicta. Toxicon 2009, 53, 479–486. [Google Scholar] [CrossRef]
- Menk, J.J.; Matuhara, Y.E.; Sebestyen-França, H.; Henrique-Silva, F.; Ferro, M.; Rodrigues, R.S.; Santos-Júnior, C.D. Antimicrobial Peptide Arsenal Predicted from the Venom Gland Transcriptome of the Tropical Trap-Jaw Ant Odontomachus chelifer. Toxins 2023, 15, 345. [Google Scholar] [CrossRef]
- Guzman, J.; Téné, N.; Touchard, A.; Castillo, D.; Belkhelfa, H.; Haddioui-Hbabi, L.; Treilhou, M.; Sauvain, M. Anti-Helicobacter pylori Properties of the Ant-Venom Peptide Bicarinalin. Toxins 2017, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Perumal Samy, R.; Gopalakrishnakone, P.; Thwin, M.M.; Chow, T.K.; Bow, H.; Yap, E.H.; Thong, T.W. Antibacterial activity of snake, scorpion and bee venoms: A comparison with purified venom phospholipase A2 enzymes. J. Appl. Microbiol. 2007, 102, 650–659. [Google Scholar] [CrossRef] [PubMed]
- Lima, W.G.; de Lima, M.E. Therapeutic Prospection of Animal Venoms-Derived Antimicrobial Peptides against Infections by Multidrug-Resistant Acinetobacter baumannii: A Systematic Review of Pre-Clinical Studies. Toxins 2023, 15, 268. [Google Scholar] [CrossRef] [PubMed]
- Amorim-Carmo, B.; Parente, A.M.S.; Souza, E.S.; Silva-Junior, A.A.; Araújo, R.M.; Fernandes-Pedrosa, M.F. Antimicrobial Peptide Analogs From Scorpions: Modifications and Structure-Activity. Front. Mol. Biosci. 2022, 9, 887763. [Google Scholar] [CrossRef]
- Graf, M.; Wilson, D.N. Intracellular Antimicrobial Peptides Targeting the Protein Synthesis Machinery. Adv. Exp. Med. Biol. 2019, 1117, 73–89. [Google Scholar] [CrossRef]
- Moravej, H.; Moravej, Z.; Yazdanparast, M.; Heiat, M.; Mirhosseini, A.; Moosazadeh Moghaddam, M.; Mirnejad, R. Antimicrobial Peptides: Features, Action, and Their Resistance Mechanisms in Bacteria. Microb. Drug Resist. 2018, 24, 747–767. [Google Scholar] [CrossRef]
- Aisenbrey, C.; Marquette, A.; Bechinger, B. The Mechanisms of Action of Cationic Antimicrobial Peptides Refined by Novel Concepts from Biophysical Investigations. Adv. Exp. Med. Biol. 2019, 1117, 33–64. [Google Scholar] [CrossRef]
- Guryanova, S.V.; Ovchinnikova, T.V. Immunomodulatory and Allergenic Properties of Antimicrobial Peptides. Int. J. Mol. Sci. 2022, 23, 2499. [Google Scholar] [CrossRef]
- Bocian, A.; Hus, K.K. Antibacterial properties of snake venom components. Chem. Pap. 2020, 74, 407–419. [Google Scholar] [CrossRef]
- Oguiura, N.; Boni-Mitake, M.; Affonso, R.; Zhang, G. In vitro antibacterial and hemolytic activities of crotamine, a small basic myotoxin from rattlesnake Crotalus durissus. J. Antibiot. 2011, 64, 327–331. [Google Scholar] [CrossRef]
- Santamaría, C.; Larios, S.; Angulo, Y.; Pizarro-Cerda, J.; Gorvel, J.P.; Moreno, E.; Lomonte, B. Antimicrobial activity of myotoxic phospholipases A2 from crotalid snake venoms and synthetic peptide variants derived from their C-terminal region. Toxicon 2005, 45, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Páramo, L.; Lomonte, B.; Pizarro-Cerdá, J.; Bengoechea, J.-A.; Gorvel, J.-P.; Moreno, E. Bactericidal activity of Lys49 and Asp49 myotoxic phospholipases A2 from Bothrops asper snake venom. Eur. J. Biochem. 1998, 253, 452–461. [Google Scholar] [CrossRef] [PubMed]
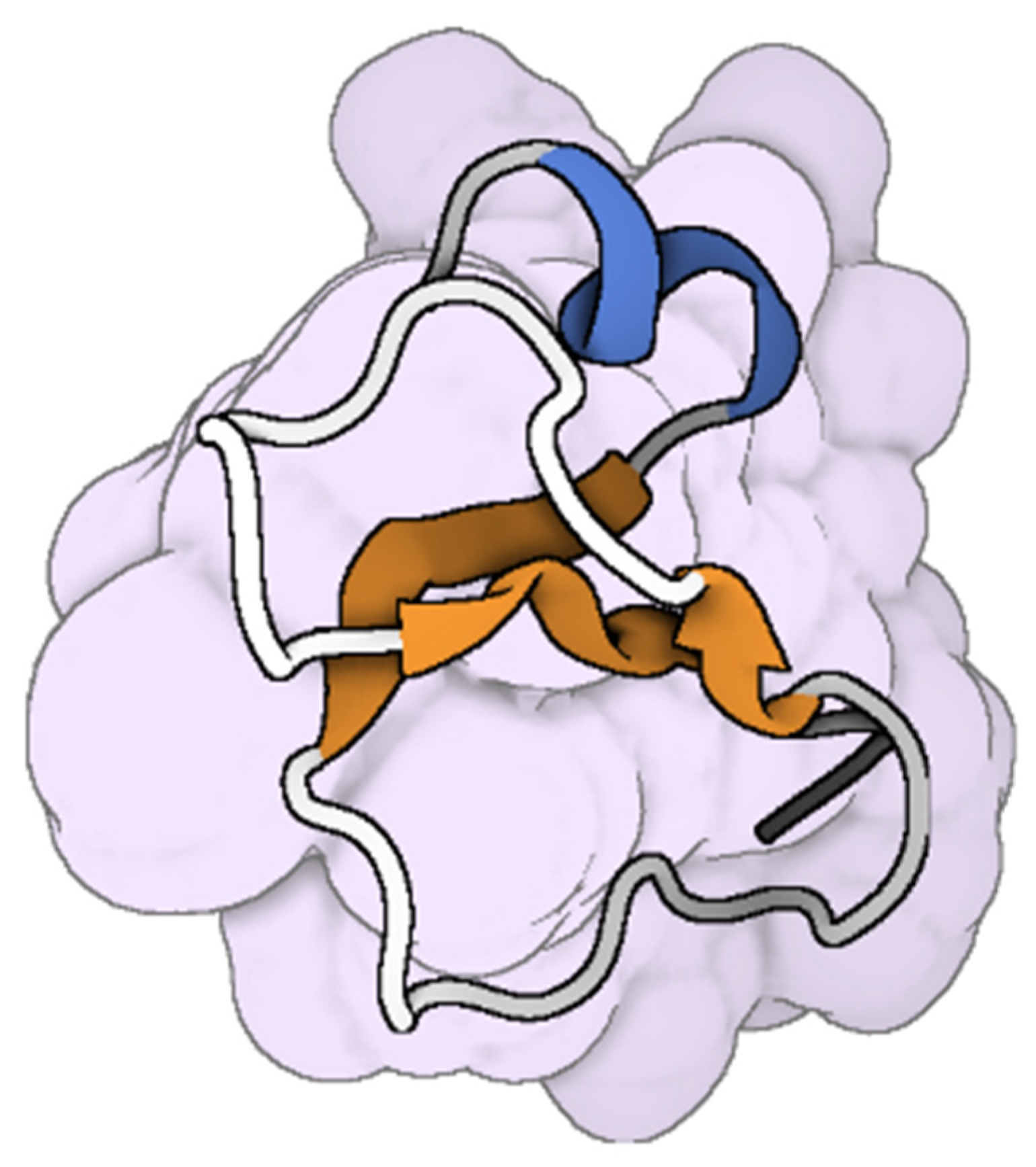
- Costa, B.A.; Sanches, L.; Gomide, A.B.; Bizerra, F.; Dal Mas, C.; Oliveira, E.B.; Perez, K.R.; Itri, R.; Oguiura, N.; Hayashi, M.A. Interaction of the rattlesnake toxin crotamine with model membranes. J. Phys. Chem. B 2014, 118, 5471–5479. [Google Scholar] [CrossRef] [PubMed]
- Coorens, M.; van Dijk, A.; Bikker, F.; Veldhuizen, E.J.; Haagsman, H.P. Importance of Endosomal Cathelicidin Degradation To Enhance DNA-Induced Chicken Macrophage Activation. J. Immunol. 2015, 195, 3970–3977. [Google Scholar] [CrossRef]
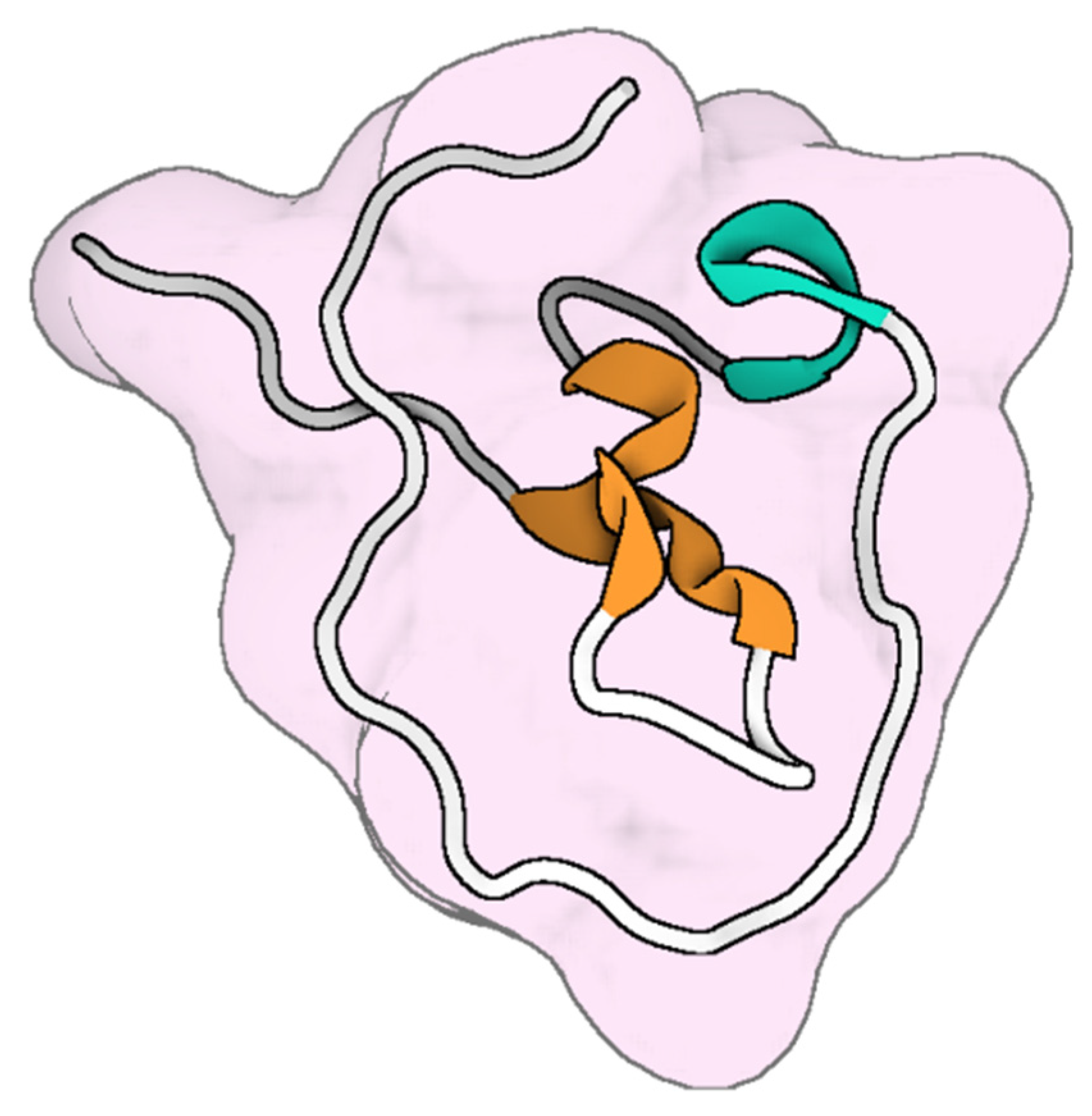
- Nicastro, G.; Franzoni, L.; de Chiara, C.; Mancin, A.C.; Giglio, J.R.; Spisni, A. Solution structure of crotamine, a Na+ channel affecting toxin from Crotalus durissus terrificus venom. Eur. J. Biochem. 2003, 270, 1969–1979. [Google Scholar] [CrossRef]
- Torres-Larios, A.; Gurrola, G.B.; Zamudio, F.Z.; Possani, L.D. Hadrurin, a new antimicrobial peptide from the venom of the scorpion Hadrurus aztecus. Eur. J. Biochem. 2000, 267, 5023–5031. [Google Scholar] [CrossRef]
- Mandard, N.; Sy, D.; Maufrais, C.; Bonmatin, J.M.; Bulet, P.; Hetru, C.; Vovelle, F. Androctonin, a novel antimicrobial peptide from scorpion Androctonus australis: Solution structure and molecular dynamics simulations in the presence of a lipid monolayer. J. Biomol. Struct. Dyn. 1999, 17, 367–380. [Google Scholar] [CrossRef]
- Yan, L.; Adams, M.E. Lycotoxins, Antimicrobial Peptides from Venom of the Wolf SpiderLycosa carolinensis *. J. Biol. Chem. 1998, 273, 2059–2066. [Google Scholar] [CrossRef]
- Habermann, E. Bee and wasp venoms. Science 1972, 177, 314–322. [Google Scholar] [CrossRef]
- Steiner, H.; Hultmark, D.; Engström, A.; Bennich, H.; Boman, H.G. Sequence and specificity of two antibacterial proteins involved in insect immunity. Nature 1981, 292, 246–248. [Google Scholar] [CrossRef]
- Giacometti, A.; Cirioni, O.; Kamysz, W.; D’Amato, G.; Silvestri, C.; Del Prete, M.S.; Łukasiak, J.; Scalise, G. Comparative activities of cecropin A, melittin, and cecropin A-melittin peptide CA(1-7)M(2-9)NH2 against multidrug-resistant nosocomial isolates of Acinetobacter baumannii. Peptides 2003, 24, 1315–1318. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.T.; Sun, T.L.; Hung, W.C.; Huang, H.W. Process of inducing pores in membranes by melittin. Proc. Natl. Acad. Sci. USA 2013, 110, 14243–14248. [Google Scholar] [CrossRef] [PubMed]
- Lima, W.G.; de Brito, J.C.M.; Cardoso, V.N.; Fernandes, S.O.A. In-depth characterization of antibacterial activity of melittin against Staphylococcus aureus and use in a model of non-surgical MRSA-infected skin wounds. Eur. J. Pharm. Sci. 2021, 156, 105592. [Google Scholar] [CrossRef] [PubMed]
- Brogden, K.A. Antimicrobial peptides: Pore formers or metabolic inhibitors in bacteria? Nat. Rev. Microbiol. 2005, 3, 238–250. [Google Scholar] [CrossRef]
- Benmoussa, K.; Authier, H.; Prat, M.; AlaEddine, M.; Lefèvre, L.; Rahabi, M.C.; Bernad, J.; Aubouy, A.; Bonnafé, E.; Leprince, J.; et al. P17, an Original Host Defense Peptide from Ant Venom, Promotes Antifungal Activities of Macrophages through the Induction of C-Type Lectin Receptors Dependent on LTB4-Mediated PPARγ Activation. Front. Immunol. 2017, 8, 1650. [Google Scholar] [CrossRef]
- Cecilio, A.B.; Caldas, S.; Oliveira, R.A.; Santos, A.S.; Richardson, M.; Naumann, G.B.; Schneider, F.S.; Alvarenga, V.G.; Estevão-Costa, M.I.; Fuly, A.L.; et al. Molecular characterization of Lys49 and Asp49 phospholipases A2 from snake venom and their antiviral activities against Dengue virus. Toxins 2013, 5, 1780–1798. [Google Scholar] [CrossRef]
- Fenard, D.; Lambeau, G.; Valentin, E.; Lefebvre, J.C.; Lazdunski, M.; Doglio, A. Secreted phospholipases A(2), a new class of HIV inhibitors that block virus entry into host cells. J. Clin. Invest. 1999, 104, 611–618. [Google Scholar] [CrossRef]
- El-Bitar, A.M.H.; Sarhan, M.; Abdel-Rahman, M.A.; Quintero-Hernandez, V.; Aoki-Utsubo, C.; Moustafa, M.A.; Possani, L.D.; Hotta, H. Smp76, a Scorpine-Like Peptide Isolated from the Venom of the Scorpion Scorpio maurus palmatus, with a Potent Antiviral Activity Against Hepatitis C Virus and Dengue Virus. Int. J. Pept. Res. Ther. 2020, 26, 811–821. [Google Scholar] [CrossRef]
- Ji, M.; Zhu, T.; Xing, M.; Luan, N.; Mwangi, J.; Yan, X.; Mo, G.; Rong, M.; Li, B.; Lai, R.; et al. An Antiviral Peptide from Alopecosa nagpag Spider Targets NS2B-NS3 Protease of Flaviviruses. Toxins 2019, 11, 584. [Google Scholar] [CrossRef]
- Jalalifar, S.; Razavi, S.; Mirzaei, R.; Irajian, G.; Pooshang Bagheri, K. A hope for ineffective antibiotics to return to treatment: Investigating the anti-biofilm potential of melittin alone and in combination with penicillin and oxacillin against multidrug resistant-MRSA and -VRSA. Front. Microbiol. 2024, 14, 1269392. [Google Scholar] [CrossRef]
- Humphries, R.; Bobenchik, A.; Hindler, J.; Schuetz, A. Overview of Changes to the Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing, M100, 31 st Edition. J. Clin. Microbiol. 2021, 59, e0021321. [Google Scholar] [CrossRef] [PubMed]
- Giske, C.; Turnidge, J.; Canton, R.; Kahlmeter, G. Update from the European Committee on Antimicrobial Susceptibility Testing (EUCAST). J. Clin. Microbiol. 2022, 60, e00276-21. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.; Chaturvedi, V.; Espinel-Ingroff, A.; Ghannoum, M.; Gosey, L.L.; Odds, F.C. Reference method for broth dilution antifungal susceptibility testing of yeasts: Approved standard-second edition. CLSI document M27-A2 (ISBN 1-56238-469-4). Clin. Lab. Stand. Inst. 2008, 22, 1–51. [Google Scholar]
- Sala, A.; Cabassi, C.S.; Santospirito, D.; Polverini, E.; Flisi, S.; Cavirani, S.; Taddei, S. Novel Naja atra cardiotoxin 1 (CTX-1) derived antimicrobial peptides with broad spectrum activity. PLoS ONE 2018, 13, e0190778. [Google Scholar] [CrossRef]
- Garcia, F.; Villegas, E.; Espino-Solis, G.P.; Rodriguez, A.; Paniagua-Solis, J.F.; Sandoval-Lopez, G.; Possani, L.D.; Corzo, G. Antimicrobial peptides from arachnid venoms and their microbicidal activity in the presence of commercial antibiotics. J. Antibiot. 2013, 66, 3–10. [Google Scholar] [CrossRef]
- Ko, S.J.; Kim, M.K.; Bang, J.K.; Seo, C.H.; Luchian, T.; Park, Y. Macropis fulvipes Venom component Macropin Exerts its Antibacterial and Anti-Biofilm Properties by Damaging the Plasma Membranes of Drug Resistant Bacteria. Sci. Rep. 2017, 7, 16580. [Google Scholar] [CrossRef]
- Obiang-Obounou, B.W.; Kang, O.H.; Choi, J.G.; Keum, J.H.; Kim, S.B.; Mun, S.H.; Shin, D.W.; Kim, K.W.; Park, C.B.; Kim, Y.G.; et al. The mechanism of action of sanguinarine against methicillin-resistant Staphylococcus aureus. J. Toxicol. Sci. 2011, 36, 277–283. [Google Scholar] [CrossRef]
- Bevalian, P.; Pashaei, F.; Akbari, R.; Pooshang Bagheri, K. Eradication of vancomycin-resistant Staphylococcus aureus on a mouse model of third-degree burn infection by melittin: An antimicrobial peptide from bee venom. Toxicon 2021, 199, 49–59. [Google Scholar] [CrossRef]
- El-Seedi, H.; Abd El-Wahed, A.; Yosri, N.; Musharraf, S.G.; Chen, L.; Moustafa, M.; Zou, X.; Al-Mousawi, S.; Guo, Z.; Khatib, A.; et al. Antimicrobial Properties of Apis mellifera’s Bee Venom. Toxins 2020, 12, 451. [Google Scholar] [CrossRef]
- Hakimi Alni, R.; Tavasoli, F.; Barati, A.; Shahrokhi Badarbani, S.; Salimi, Z.; Babaeekhou, L. Synergistic activity of melittin with mupirocin: A study against methicillin-resistant S. Aureus (MRSA) and methicillin-susceptible S. Aureus (MSSA) isolates. Saudi J. Biol. Sci. 2020, 27, 2580–2585. [Google Scholar] [CrossRef]
- Wang, A.; Zheng, Y.; Zhu, W.; Yang, L.; Yang, Y.; Peng, J. Melittin-Based Nano-Delivery Systems for Cancer Therapy. Biomolecules 2022, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Hancock, R.E.W.; Sahl, H.-G. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat. Biotechnol. 2006, 24, 1551–1557. [Google Scholar] [CrossRef] [PubMed]
- Reis, P.V.M.; Boff, D.; Verly, R.M.; Melo-Braga, M.N.; Cortés, M.E.; Santos, D.M.; Pimenta, A.M.C.; Amaral, F.A.; Resende, J.M.; de Lima, M.E. LyeTxI-b, a Synthetic Peptide Derived From Lycosa erythrognatha Spider Venom, Shows Potent Antibiotic Activity in Vitro and in Vivo. Front. Microbiol. 2018, 9, 667. [Google Scholar] [CrossRef] [PubMed]
- Thankappan, B.; Angayarkanni, J. Biological characterization of omw1 and omw2: Antimicrobial peptides derived from omwaprin. 3 Biotech. 2019, 9, 295. [Google Scholar] [CrossRef]
- Fadaka, A.O.; Sibuyi, N.R.S.; Madiehe, A.M.; Meyer, M. Nanotechnology-Based Delivery Systems for Antimicrobial Peptides. Pharmaceutics 2021, 13, 1795. [Google Scholar] [CrossRef]
- Gagandeep, K.R.; Balenahalli Narasingappa, R.; Vishnu Vyas, G. Unveiling mechanisms of antimicrobial peptide: Actions beyond the membranes disruption. Heliyon 2024, 10, e38079. [Google Scholar] [CrossRef]
- Aburayan, W.S.; Alajmi, A.M.; Alfahad, A.J.; Alsharif, W.K.; Alshehri, A.A.; Booq, R.Y.; Alsudir, S.A.; Alsulaihem, F.M.; Bukhary, H.A.; Badr, M.Y.; et al. Melittin from Bee Venom Encapsulating Electrospun Fibers as a Potential Antimicrobial Wound Dressing Patches for Skin Infections. Pharmaceutics 2022, 14, 725. [Google Scholar] [CrossRef]
- Calvete, J.J.; Juárez, P.; Sanz, L. Snake venomics. Strategy and applications. J. Mass. Spectrom. 2007, 42, 1405–1414. [Google Scholar] [CrossRef]
- Abd El-Aziz, T.M.; Soares, A.G.; Stockand, J.D. Advances in venomics: Modern separation techniques and mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2020, 1160, 122352. [Google Scholar] [CrossRef]
- Klint, J.K.; Senff, S.; Saez, N.J.; Seshadri, R.; Lau, H.Y.; Bende, N.S.; Undheim, E.A.B.; Rash, L.D.; Mobli, M.; King, G.F. Production of Recombinant Disulfide-Rich Venom Peptides for Structural and Functional Analysis via Expression in the Periplasm of E. coli. PLoS ONE 2013, 8, e63865. [Google Scholar] [CrossRef]
- Oliveira, A.L.; Viegas, M.F.; da Silva, S.L.; Soares, A.M.; Ramos, M.J.; Fernandes, P.A. The chemistry of snake venom and its medicinal potential. Nat. Rev. Chem. 2022, 6, 451–469. [Google Scholar] [CrossRef]



| Drug Name | Venom Source | Medical Use | Biological Target | FDA Approval Year | Ref. |
|---|---|---|---|---|---|
| Captopril | Bothrops jararaca (Brazilian pit viper) | Hypertension | Inhibition of angiotensin-converting enzyme (ACE) | 1981 | [27] |
| Eptifibatide | Sistrurus miliarius (Pygmy rattlesnake) | Acute coronary syndrome | Antagonist of the platelet receptor glycoprotein IIb/IIIa receptor | 1998 | [28] |
| Tirofiban | Echis carinatus (Saw-scaled viper) | Acute coronary syndrome | Reversible antagonist of the platelet glycoprotein IIb/IIIa receptor | 1998 | [29] |
| Ziconotide | Conus magus (Cone snail) | Severe chronic pain | Block N-type calcium channels | 2004 | [30] |
| Exenatide | Heloderma suspectum (Gila monster) | Type 2 diabetes mellitus | Binding and activation of GLP-1 receptor to reduce plasma glucose and lower HbA1c | 2005 | [31] |
| Dalazatide (ShK-186) | Stichodactyla helianthus (Sea anemone) | Autoimmune diseases (psoriasis, MS) | Kv1.3 potassium channel | In clinical trials | [32] |
| Hi1a | Hadronyche infensa (Australian funnel-web spider) | Cardioprotection during heart attack and stroke | Acid-sensing ion channel 1a (ASIC1a) | In clinical trials | [33] |
| Chlorotoxin | Leiurus quinquestriatus (Deathstalker scorpion) | Tumor imaging, glioma targeting | Matrix metalloproteinase-2 (MMP-2), annexin A2, and chloride channels | In clinical trials | [34] |
| Animal Source | Species | Active Component | Activity Type | Target Pathogens | Ref. |
|---|---|---|---|---|---|
| Snake | Ophiophagus hannah | L-amino acid oxidase (L-AAO) | Antibacterial, antifungal | Staphylococcus aureus, Staphylococcus epidermidis | [35] |
| Crotalus durissus terrificus | Crotamine | Antibacterial, antifungal, antiparasitic | Escherichia coli, Bacillus subtilis, Candida spp., Plasmodium falciparum | [36,37] | |
| Hydrophis cyanocinctus | Cathelicidin (Hc-CATH) | Antibacterial | Staphylococcus aureus, Escherichia coli, Vibrio cholerae | [38,39] | |
| Bungarus fasciatus | Cathelicidin-BF | Antibacterial | Propionibacterium acnes, Klebsiella pneumoniae, Salmonella typhimurium | [40,41] | |
| Bothrops marajoensis | L-amino acid oxidase (L-AAO) | Antibacterial, antifungal, anti-parasitic | Staphylococcus aureus, Pseudomonas aeruginosa, Candida albicans, Leishmania chagasi, Leishmania amazonensis | [15] | |
| Naja naja | PLA2 (NN-XIb-PLA2) | Antibacterial | Staphylococcus aureus, Bacillus subtilis | [42] | |
| Oxyuranus microlepidotus | Omwaprin | Antibacterial | Bacillus megaterium, Staphylococcus warneri | [43] | |
| Crotalus adamanteus | PLA2 (CaTx-II) | Antibacterial | Burkholderia pseudomallei, Staphylococcus aureus, Enterobacter aerogenes | [44] | |
| Scorpion | Lychas mucronatus | Mucroporin-M1 | Antibacterial, antiviral | Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, measles, severe acute respiratory syndrome coronavirus (SARS-CoV), hepatitis B virus (HBV), and influenza H5N1 | [45,46,47] |
| Pandinus imperator | Pandinin peptides | Antifungal | Candida albicans | [48] | |
| Mesobuthus martensii | BmKn2, BmKn2-7 | Antibacterial, antiviral | Staphylococcus aureus, Micrococcus luteus, Escherichia coli, Pseudomonas aeruginosa, Neisseria gonorrhoeae, HIV-1 | [49,50,51] | |
| Androctonus aeneas | AaeAP1, AaeAP2 | Antibacterial, antifungal | Staphylococcus aureus, Candida albicans | [52] | |
| Isometrus scorpion | Imcroporin | Antibacterial | Methicillin-resistant Staphylococcus aureus | [53] | |
| Spider | Lycosa singoriensis | M-lycotoxin-Ls3a | Antibacterial, antifungal | Staphylococcus aureus, Bacillus subtilis, Escherichia coli, Pseudomonas aeruginosa, Candida albicans | [54] |
| Hogna carolinensis | M-lycotoxin-Hc1a | Antibacterial, antifungal | Staphylococcus aureus, Bacillus subtilis, Candida albicans | [55] | |
| Loxosceles gaucho | U1-SCRTX-Lg1a | Antibacterial | Escherichia coli, Pseudomonas aeruginosa, Enterobacter cloacae | [56] | |
| Honeybee | Apis mellifera | Melittin and PLA2 | Antibacterial, antifungal, antiviral | Methicillin-resistant Staphylococcus aureus, Escherichia coli, Acinetobacter baumannii, Candida albicans, Herpes simplex virus (HSV), Human immunodeficiency virus (HIV), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), | [57,58,59,60,61,62,63] |
| Apis cerana | PLA2 | Antibacterial | Escherichia coli | [64] | |
| Wasp | Vespa orientalis | Whole venom | Antibacterial | Bacillus cereus, Staphylococcus aureus | [65] |
| Vespa basalis | Mastoparan B | Antibacterial | Enterococcus faecalis, Bacillus subtilis, Shigella flexneri | [66] | |
| Polybia paulista | Polybia-CP | Antibacterial | Staphylococcus aureus, Bacillus subtilis, Escherichia coli, Pseudomonas aeruginosa, Staphylococcus epidermidis | [67,68] | |
| Ant | Solenopsis invicta | Solenopsins | Antibacterial, antifungal | Streptococcus pneumoniae, Staphylococcus aureus, Enterococcus faecalis, Stenotrophomonas maltophilia, Candida auris | [69,70] |
| Pachycondyla goeldii | Ponericins | Antibacterial | Geobacillus stearothermophilus, Bacillus subtilis, Bacillus megaterium, Lactococcus lactis, Pseudomonas aeruginosa | [71] | |
| Tetramorium bicarinatum | Bicarinalin | Antibacterial, antifungal, antiparasitic | Cronobacter sakazakii, Helicobacter pylori, Candida albicans, Aspergillus niger, Leishmania infantum | [72,73] |
| Cathelicidin Name | Snake Species | Active Peptide Sequence | Number of Residues (aa) | Ref. |
|---|---|---|---|---|
| NA-CATH | Naja atra | KRFKKFFKKLKNSVKKRAKKFFKKPKVIGVTFPF | 34 | [79] |
| OH-CATH | Ophiophagus hannah | KRFKKFFKKLKNSVKKRAKKFFKKPRVIGVSIPF | 34 | [80] |
| Cathelicidin-BF | Bungarus fasciatus | KFFRKLKKSVKKRAKEFFKKPRVIGVSIPF | 30 | [40] |
| OH-CATH30 | Ophiophagus hannah | KFFKKLKNSVKKRAKKFFKKPRVIGVSIPF | 30 | [81] |
| Hc-CATH | Hydrophis cyanocinctus | KFFKRLLKSVRRAVKKFRKKPRLIGLSTLL | 30 | [38] |
| SA-CATH | Sinonatrix annularis | KFFKKLKKSVKKHVKKFFKKPKVIGVSIPF | 30 | [82] |
| CATHPb1 | Python bivittatus | KRFKKFFRKIKKGFRKIFKKTKIFIGGTIPI | 31 | [83] |
| Batroxicidin (BatxC) | Bothrops atrox | KRFKKFFKKLKNSVKKRVKKFFRKPRVIGVTFPF | 34 | [84] |
| Crotalicidin (Ctn) | Crotalus durissus terrificus | KRFKKFFKKVKKSVKKRLKKIFKKPMVIGVTIPF | 34 | [85] |
| Pt_CRAMP1 | Pseudonaja textilis | KRFKKFFMKLKKSVKKRVMKFFKKPMVIGVTFPF | 34 | [84] |
| Pt_CRAMP2 | Pseudonaja textilis | KRFKKFFRKLKKSVKKRVKKFFKKPRVIGVTIPF | 34 | [84] |
| Venom-Derived Peptide | Source | Target Microbe | MIC (μg/mL) | Conventional Antibiotic | MIC (μg/mL) | Notes | Ref. |
|---|---|---|---|---|---|---|---|
| Melittin | Honeybee (Apis mellifera) | Staphylococcus aureus | 2–10 | Vancomycin | 1–2 | Disrupts bacterial membranes vs. cell wall synthesis inhibition. | [158,159] |
| Cathelicidin-BF | Banded krait (Bungarus fasciatus) | Escherichia coli | 5–20 | Ciprofloxacin | 0.1–1 | Membrane permeabilization vs. DNA gyrase inhibition. | [41,160] |
| Hadrurin | Scorpion (Hadrurus aztecus) | Pseudomonas aeruginosa | 10–50 | Ceftazidime | 2–8 | Pore formation vs. cell wall synthesis inhibition. | [144,159] |
| Cardiotoxin 1 | Chinese cobra (Naja atra) | Candida albicans | 6–50 | Fluconazole | 1–4 | Generates ROS vs. ergosterol synthesis inhibition. | [161,162] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabea, E.Y.; Mahmoud, E.D.; Mohamed, N.K.; Ansary, E.R.; Alrouby, M.R.; Shehata, R.R.; Mokhtar, Y.Y.; Arullampalam, P.; Hegazy, A.M.; Al-Sabi, A.; et al. Potential of Venom-Derived Compounds for the Development of New Antimicrobial Agents. Toxins 2025, 17, 238. https://doi.org/10.3390/toxins17050238
Rabea EY, Mahmoud ED, Mohamed NK, Ansary ER, Alrouby MR, Shehata RR, Mokhtar YY, Arullampalam P, Hegazy AM, Al-Sabi A, et al. Potential of Venom-Derived Compounds for the Development of New Antimicrobial Agents. Toxins. 2025; 17(5):238. https://doi.org/10.3390/toxins17050238
Chicago/Turabian StyleRabea, Esraa Yasser, Esraa Dakrory Mahmoud, Nada Khaled Mohamed, Erada Rabea Ansary, Mahmoud Roushdy Alrouby, Rabab Reda Shehata, Youssef Yasser Mokhtar, Prakash Arullampalam, Ahmed M. Hegazy, Ahmed Al-Sabi, and et al. 2025. "Potential of Venom-Derived Compounds for the Development of New Antimicrobial Agents" Toxins 17, no. 5: 238. https://doi.org/10.3390/toxins17050238
APA StyleRabea, E. Y., Mahmoud, E. D., Mohamed, N. K., Ansary, E. R., Alrouby, M. R., Shehata, R. R., Mokhtar, Y. Y., Arullampalam, P., Hegazy, A. M., Al-Sabi, A., & Abd El-Aziz, T. M. (2025). Potential of Venom-Derived Compounds for the Development of New Antimicrobial Agents. Toxins, 17(5), 238. https://doi.org/10.3390/toxins17050238









