Navigating the Complexities Involving the Identification of Botulinum Neurotoxins (BoNTs) and the Taxonomy of BoNT-Producing Clostridia
Abstract
1. History Involving Discovery of BoNTs and BoNT-Producing Clostridia
2. Complexities Involving Botulinum Neurotoxin Nomenclature
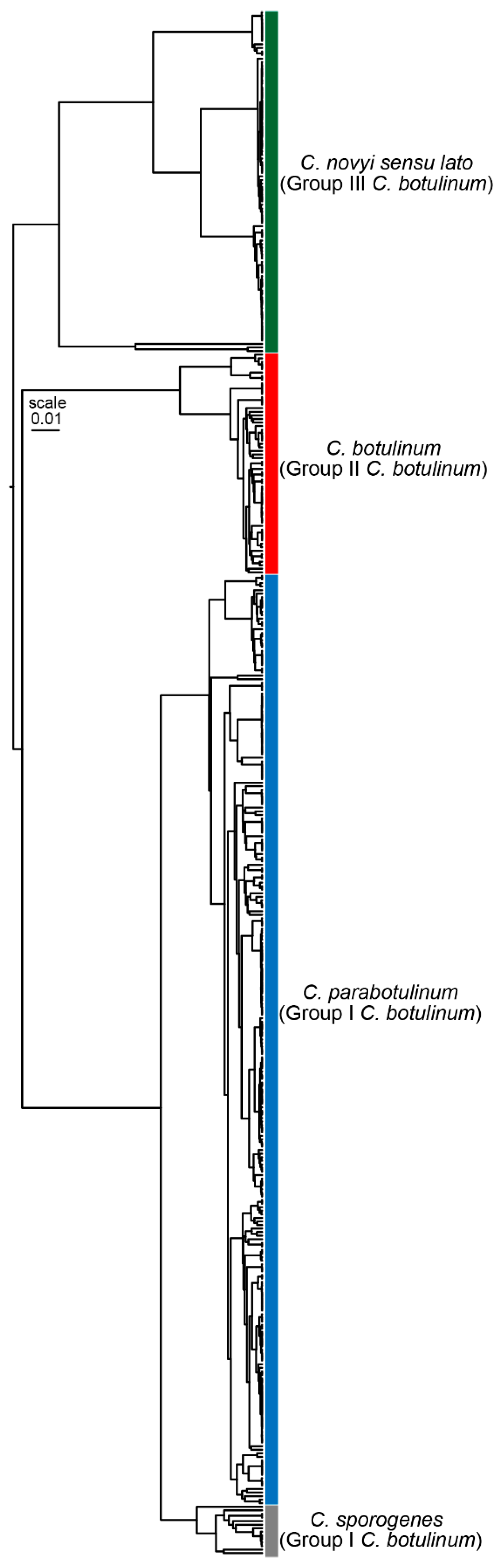
3. Nomenclature and Taxonomic Issues Surrounding BoNT-Producing Clostridium Species
4. Effective Communications Involving Botulism, Botulinum Neurotoxins, and BoNT-Producing Bacteria
4.1. Diagnosis/Treatment of Human Botulism
4.2. Animal Botulism
4.3. Epidemiology/Environmental Studies
4.4. Food Challenge Studies
4.5. Therapeutic BoNT Preparations
5. Summary
Author Contributions
Funding
Conflicts of Interest
References
- van Ermengem, E. Classics in infectious diseases. A new anaerobic bacillus and its relation to botulism. E. van Ermengem. Originally published as “Ueber einen neuen anaeroben Bacillus und seine Beziehungen zum Botulismus” in Zeitschrift fur Hygiene und Infektionskrankheiten 26: 1-56, 1897. Rev. Infect. Dis. 1979, 1, 701–719. [Google Scholar] [PubMed]
- Landmann, G. Ueber die ursache der Darmstadter bohnenvergiftung. Hyg. Rundschau 1904, 14, 449. [Google Scholar]
- Leuchs, J. Beitraege zur kenntnis des toxins und antitoxins des Bacillus botulinus. Z. Hyg. Infektionskr 1910, 76, 55–84. [Google Scholar] [CrossRef]
- Burke, G.S. Notes on Bacillus botulinus. J. Bacteriol. 1919, 4, 555–570. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Williamson, C.H.D.; Hill, K.K.; Johnson, S.L.; Xie, G.; Anniballi, F.; Auricchio, B.; Fernandez, R.A.; Caballero, P.A.; Keim, P.; et al. The Distinctive Evolution of orfX Clostridium parabotulinum Strains and Their Botulinum Neurotoxin Type A and F Gene Clusters Is Influenced by Environmental Factors and Gene Interactions via Mobile Genetic Elements. Front. Microbiol. 2021, 12, 566908. [Google Scholar] [CrossRef]
- Winslow, C.E.; Broadhurst, J.; Buchanan, R.E.; Krumwiede, C.; Rogers, L.A.; Smith, G.H. The Families and Genera of the Bacteria: Preliminary Report of the Committee of the Society of American Bacteriologists on Characterization and Classification of Bacterial Types. J. Bacteriol. 1917, 2, 505–566. [Google Scholar] [CrossRef]
- Seddon, H. Bulbar paralysis in cattle due to the action of a toxicogenic bacillus, with a discussion on the relationship of the condition to forage poisoning (botulism). J. Comp. Pathol. Therapeutics 1922, 35, 147–190. [Google Scholar] [CrossRef]
- Bengtson, I. A toxin-producing anaerobe isolated principally from fly larvae. Its relation to the organisms hitherto known to be causative factors in the production of botulism. Pub. Health Rpts. 1923, 38, 340–344. [Google Scholar] [CrossRef]
- Meyer, K.; Gunnison, J. South African cultures of Clostridium botulinum and parabotulinum, XXXVII with a description of Cl. botulinum type D, n.sp. J. Infect. Dis. 1929, 45, 106–118. [Google Scholar] [CrossRef]
- Gunnison, J.; Meyer, K. Cultural study of an international collection of Clostridium botulinum and parabotulinum XXXVIII. J. Infect. Dis. 1929, 45, 119–134. [Google Scholar] [CrossRef]
- Gunnison, J.; Cummings, J.; Meyer, K. Clostridium botulinum type E. Proc. Soc. Exp. Biol. 1936, 35, 278–280. [Google Scholar] [CrossRef]
- Prevot, A. Rapport d’introduction du president du sous-comite Clostridium pour l’unification de la nonmenclature des types toxigeniques de C. botulinum. (Introductory report from the chair of the Clostridium subcommittee for the unification of the nomenclature of toxigenic types of C. botulinum). Int. Bull. Bact. Nomencl. 1953, 3, 120–123. [Google Scholar]
- Moller, V.; Scheibel, I. Preliminary report on the isolation of an apparently new type of Cl. botulinum. Acta Pathol. Microbiol. Scand. 1960, 48, 80. [Google Scholar] [CrossRef]
- Eklund, M.W.; Poysky, F.T.; Wieler, D.I. Characteristics of Clostridium botulinum type F isolated from the Pacific Coast of the United States. Appl. Microbiol. 1967, 15, 1316–1323. [Google Scholar] [CrossRef]
- Gimenez, D.F.; Ciccarelli, A.S. Another type of Clostridium botulinum. Zentralbl Bakteriol. Orig. 1970, 215, 221–224. [Google Scholar]
- Smith, L. Botulism: The Organism, its Toxins, the Disease; Charles C. Thomas: Springfield, IL, USA, 1977. [Google Scholar]
- Aureli, P.; Fenicia, L.; Pasolini, B.; Gianfranceschi, M.; McCroskey, L.M.; Hatheway, C.L. Two cases of type E infant botulism caused by neurotoxigenic Clostridium butyricum in Italy. J. Infect. Dis. 1986, 154, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Suen, J.C.; Hatheway, C.L.; Steigerwalt, A.G.; Brenner, D.J. Genetic confirmation of identities of neurotoxigenic Clostridium baratii and Clostridium butyricum implicated as agents of infant botulism. J. Clin. Microbiol. 1988, 26, 2191–2192. [Google Scholar] [CrossRef] [PubMed]
- Suen, J.C.; Hatheway, C.L.; Steigerwalt, A.G.; BJ, B. Clostridium argentinense sp. nov.: A genetically homogeneous group composed of all strains of Clostridium botulinum toxin type G. and some nontoxigenic strains previously identified as Clostridium subterminale or Clostridium hastiforme. Int. J. Syst. Bacteriol. 1988, 38, 375–381. [Google Scholar] [CrossRef]
- Hauser, D.; Eklund, M.W.; Kurazono, H.; Binz, T.; Niemann, H.; Gill, D.M.; Boquet, P.; Popoff, M.R. Nucleotide sequence of Clostridium botulinum C1 neurotoxin. Nucleic Acids Res. 1990, 18, 4924. [Google Scholar] [CrossRef]
- Cordoba, J.J.; Collins, M.D.; East, A.K. Studies on the genes encoding botulinum neurotoxin type A of Clostridium botulinum from a variety of sources. Syst. Appl. Microbiol. 1995, 18, 13–22. [Google Scholar]
- Moriishi, K.; Koura, M.; Fujii, N.; Fujinaga, Y.; Inoue, K.; Syuto, B.; Oguma, K. Molecular cloning of the gene encoding the mosaic neurotoxin, composed of parts of botulinum neurotoxin types C1 and D, and PCR detection of this gene from Clostridium botulinum type C organisms. Appl. Environ. Microbiol. 1996, 62, 662–667. [Google Scholar] [CrossRef]
- Skarin, H.; Hafstrom, T.; Westerberg, J.; Segerman, B. Clostridium botulinum group III: A group with dual identity shaped by plasmids, phages and mobile elements. BMC Genom. 2011, 12, 185. [Google Scholar] [CrossRef]
- Barash, J.R.; Arnon, S.S. A novel strain of Clostridium botulinum that produces type B and type H botulinum toxins. J. Infect. Dis. 2014, 209, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Dover, N.; Barash, J.R.; Hill, K.K.; Xie, G.; Arnon, S.S. Molecular characterization of a novel botulinum neurotoxin type H gene. J. Infect. Dis. 2014, 209, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Weigand, M.R.; Pena-Gonzalez, A.; Shirey, T.B.; Broeker, R.G.; Ishaq, M.K.; Konstantinidis, K.T.; Raphael, B.H. Implications of Genome-Based Discrimination between Clostridium botulinum Group I and Clostridium sporogenes Strains for Bacterial Taxonomy. Appl. Environ. Microbiol. 2015, 81, 5420–5429. [Google Scholar] [CrossRef]
- Williamson, C.H.; Sahl, J.W.; Smith, T.J.; Xie, G.; Foley, B.T.; Smith, L.A.; Fernandez, R.A.; Lindstrom, M.; Korkeala, H.; Keim, P.; et al. Comparative genomic analyses reveal broad diversity in botulinum-toxin-producing Clostridia. BMC Genom. 2016, 17, 180. [Google Scholar] [CrossRef]
- Mansfield, M.J.; Wentz, T.; Zhang, S.; Lee, E.; Dong, M.; Sharma, S.; Doxey, A. Newly identified relatives of botulinum neurotoxins shed light on their molecular evolution. bioRxiv 2017. [Google Scholar] [CrossRef]
- Zornetta, I.; Azarnia Tehran, D.; Arrigoni, G.; Anniballi, F.; Bano, L.; Leka, O.; Zanotti, G.; Binz, T.; Montecucco, C. The first non Clostridial botulinum-like toxin cleaves VAMP within the juxtamembrane domain. Sci. Rep. 2016, 6, 30257. [Google Scholar] [CrossRef]
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Lundin, D.; Henriksson, L.; Miyashita, S.I.; Martinez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef]
- Popoff, M.R.; Bouvet, P. Genetic characteristics of toxigenic Clostridia and toxin gene evolution. Toxicon 2013, 75, 63–89. [Google Scholar] [CrossRef]
- Skarin, H.; Segerman, B. Plasmidome interchange between Clostridium botulinum, Clostridium novyi and Clostridium haemolyticum converts strains of independent lineages into distinctly different pathogens. PLoS ONE 2014, 9, e107777. [Google Scholar] [CrossRef]
- Hill, K.K.; Smith, T.J. Genetic diversity within Clostridium botulinum serotypes, botulinum neurotoxin gene clusters and toxin subtypes. Curr. Top. Microbiol. Immunol. 2013, 364, 1–20. [Google Scholar] [CrossRef]
- Peck, M.W.; Smith, T.J.; Anniballi, F.; Austin, J.W.; Bano, L.; Bradshaw, M.; Cuervo, P.; Cheng, L.W.; Derman, Y.; Dorner, B.G.; et al. Historical Perspectives and Guidelines for Botulinum Neurotoxin Subtype Nomenclature. Toxins 2017, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Fagan, R.P.; Neil, K.P.; Sasich, R.; Luquez, C.; Asaad, H.; Maslanka, S.; Khalil, W. Initial recovery and rebound of type F intestinal colonization botulism after administration of investigational heptavalent botulinum antitoxin. Clin. Infect. Dis. 2011, 53, e125–e128. [Google Scholar] [CrossRef]
- Smith, T.; Williamson, C.H.D.; Hill, K.; Sahl, J.; Keim, P. Botulinum Neurotoxin-Producing Bacteria. Isn’t It Time that We Called a Species a Species? mBio 2018, 9, e01469-18. [Google Scholar] [CrossRef] [PubMed]
- Schoenholz, P.; Meyer, K. Studies on the serologic classification of B. botulinus II. Agglutination. J. Immunol. 1924, 10, 1–53. [Google Scholar] [CrossRef]
- Starin, W.; Dack, G. Complement-fixation studies on Clostridium botulinum. J. Infect. Dis. 1923, 33, 137–147. [Google Scholar] [CrossRef]
- Hatheway, C. Botulism. In Laboratory Diagnosis of Infectious Diseases; Balows, A., Hausler, W.J., Ohashi, J., Turano, A., Eds.; Springer: New York, NY, USA, 1988; pp. 111–133. [Google Scholar]
- Kautter, D.; Lynt, R. Clostridium botulinum. In Bacteriological Analytical Manual, 5th ed.; Food and Drug Administration: Silver Spring, MD, USA, 1978; pp. 1–16. [Google Scholar]
- Hatheway, C.L.; McCroskey, L.M.; Lombard, G.L.; Dowell, V.R., Jr. Atypical toxin variant of Clostridium botulinum type B associated with infant botulism. J. Clin. Microbiol. 1981, 14, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Gimenez, D.F.; Gimenez, J.A. Identification of strain B 657 of Clostridium botulinum. Rev. Argent. Microbiol. 1983, 15, 51–55. [Google Scholar]
- Maslanka, S.E.; Luquez, C.; Dykes, J.K.; Tepp, W.H.; Pier, C.L.; Pellett, S.; Raphael, B.H.; Kalb, S.R.; Barr, J.R.; Rao, A.; et al. A Novel Botulinum Neurotoxin, Previously Reported as Serotype H, Has a Hybrid-Like Structure With Regions of Similarity to the Structures of Serotypes A and F and Is Neutralized With Serotype A Antitoxin. J. Infect. Dis. 2016, 213, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Centurioni, D.A.; Egan, C.T.; Perry, M.J. Current Developments in Diagnostic Assays for Laboratory Confirmation and Investigation of Botulism. J. Clin. Microbiol. 2022, 60, e0013920. [Google Scholar] [CrossRef]
- Gunnison, J.; Meyer, M.J. The occurrence of nontoxic strains of Cl. parabotulinum, XXXIV. J. Infect. Dis. 1929, 45, 79–86. [Google Scholar] [CrossRef]
- Eklund, M.W.; Poysky, M.J.; Boatman, E.S. Bacteriophages of Clostridium botulinum types A, B, E, and F and nontoxigenic strains resembling type E. J. Virol. 1969, 3, 270–274. [Google Scholar] [CrossRef]
- Olsen, I.; Johnson, J.; Moore, L.; Moore, E. Rejection of Clostridium putrificum and conservation of Clostridium botulinum and Clostridium sporogenes Request for an opinion. Int. J. Syst. Bacteriol. 1995, 45, 414. [Google Scholar] [CrossRef]
- Hoffman, R.E.; Pincomb, B.J.; Skeels, M.R. Type F infant botulism. Am. J. Dis. Child. 1982, 136, 270–271. [Google Scholar] [CrossRef]
- Hatheway, C.L. Laboratory procedures for cases of suspected infant botulism. Rev. Infect. Dis. 1979, 1, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.D.; McCroskey, L.M.; Pincomb, B.J.; Hatheway, C.L. Isolation of an organism resembling Clostridium barati which produces type F botulinal toxin from an infant with botulism. J. Clin. Microbiol. 1985, 21, 654–655. [Google Scholar] [CrossRef]
- Smith, L.; Holdeman, L. The Pathogenic Anaerobic Bacteria; Charles C. Thomas: Springfield, IL, USA, 1968. [Google Scholar]
- Collins, M.D.; East, A.K. Phylogeny and taxonomy of the food-borne pathogen Clostridium botulinum and its neurotoxins. J. Appl. Microbiol. 1998, 84, 5–17. [Google Scholar] [CrossRef]
- De Vos, P.; Garrity, G.; Jones, D.; Krieg, N.; Ludwig, W.; Rainey, F.; Schleifer, K.-H.; Whitman, W. The Firmicutes. In Bergey’s Manual of Systematic Bacteriology; Parte, A., Ed.; Springer: New York, NY, USA, 2009; pp. 739–816. [Google Scholar]
- Parker, C.; Tindall, B.; Garrity, G. International Code of Nomenclature of Prokaryotes. Int. J. Syst. Evol. Microbiol. 2008, 69, S1–S111. [Google Scholar]
- Prevot, A.; Fredette, V. Manual for the Classification and Determination of the Anaerobic Bacteria, 1st ed.; Lea & Febiger: Philadelphia, PA, USA, 1966. [Google Scholar]
- Hill, K.K.; Smith, T.J.; Helma, C.H.; Ticknor, L.O.; Foley, B.T.; Svensson, R.T.; Brown, J.L.; Johnson, E.A.; Smith, L.A.; Okinaka, R.T.; et al. Genetic diversity among Botulinum Neurotoxin-producing clostridial strains. J. Bacteriol. 2007, 189, 818–832. [Google Scholar] [CrossRef] [PubMed]
- Brunt, J.; van Vliet, A.H.M.; Carter, A.T.; Stringer, S.C.; Amar, C.; Grant, K.A.; Godbole, G.; Peck, M.W. Diversity of the Genomes and Neurotoxins of Strains of Clostridium botulinum Group I and Clostridium sporogenes Associated with Foodborne, Infant and Wound Botulism. Toxins 2020, 12, 586. [Google Scholar] [CrossRef]
- Pritchard, L.; Glover, R.; Humphris, S.; Elphinstone, J.; Toth, I. Genomics and taxonomy in diagnostics for food security: Soft-rotting enterobacterial plant pathogens. Anal. Methods 2016, 8, 12–24. [Google Scholar] [CrossRef]
- Delcher, A.L.; Salzberg, S.L.; Phillippy, A.M. Using MUMmer to identify similar regions in large sequence sets. Curr. Protoc. Bioinform. 2003, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Parks, D.H.; Chuvochina, M.; Waite, D.W.; Rinke, C.; Skarshewski, A.; Chaumeil, P.A.; Hugenholtz, P. A standardized bacterial taxonomy based on genome phylogeny substantially revises the tree of life. Nat. Biotechnol. 2018, 36, 996–1004. [Google Scholar] [CrossRef]
- Sanford, R.A.; Lloyd, K.G.; Konstantinidis, K.T.; Loffler, F.E. Microbial Taxonomy Run Amok. Trends Microbiol. 2021, 29, 394–404. [Google Scholar] [CrossRef]
- Hatheway, C.L.; McCroskey, L.M. Laboratory investigation of human and animal botulism. In Biomedical Aspects of Botulism; Lewis, G., Ed.; Academic Press: New York, NY, USA, 1981; pp. 165–180. [Google Scholar]
- Barker, D.; Gillum, K.T.; Niemuth, N.A.; Kodihalli, S. Therapeutic efficacy of equine botulism heptavalent antitoxin against all seven botulinum neurotoxins in symptomatic guinea pigs. PLoS ONE 2019, 14, e0222670. [Google Scholar] [CrossRef] [PubMed]
- Khouri, J.M.; Motter, R.N.; Arnon, S.S. Safety and immunogenicity of investigational recombinant botulinum vaccine, rBV A/B, in volunteers with pre-existing botulinum toxoid immunity. Vaccine 2018, 36, 2041–2048. [Google Scholar] [CrossRef]
- McCarty, C.L.; Angelo, K.; Beer, K.D.; Cibulskas-White, K.; Quinn, K.; de Fijter, S.; Bokanyi, R.; St Germain, E.; Baransi, K.; Barlow, K.; et al. Large Outbreak of Botulism Associated with a Church Potluck Meal--Ohio, 2015. MMWR Morb. Mortal Wkly Rep. 2015, 64, 802–803. [Google Scholar] [CrossRef]
- Rosen, H.E.; Kimura, A.C.; Crandall, J.; Poe, A.; Nash, J.; Boetzer, J.; Tecle, S.; Mukhopadhyay, R.; McAuley, K.; Kasirye, O.; et al. Foodborne Botulism Outbreak Associated With Commercial Nacho Cheese Sauce From a Gas Station Market. Clin. Infect. Dis. 2020, 70, 1695–1700. [Google Scholar] [CrossRef]
- Marlow, M.; Edwards, L.; McCrickard, L.; Francois Watkins, L.K.; Anderson, J.; Hand, S.; Taylor, K.; Dykes, J.; Byers, P.; Chatham-Stephens, K. Mild Botulism From Illicitly Brewed Alcohol in a Large Prison Outbreak in Mississippi. Front. Public. Health 2021, 9, 716615. [Google Scholar] [CrossRef]
- Lindstrom, M.; Nevas, M.; Kurki, J.; Sauna-aho, R.; Latvala-Kiesila, A.; Polonen, I.; Korkeala, H. Type C botulism due to toxic feed affecting 52,000 farmed foxes and minks in Finland. J. Clin. Microbiol. 2004, 42, 4718–4725. [Google Scholar] [CrossRef]
- Nol, P.; Rocke, T.E.; Gross, K.; Yuill, T.M. Prevalence of neurotoxic Clostridium botulinum type C in the gastrointestinal tracts of tilapia (Oreochromis mossambicus) in the Salton Sea. J. Wildl. Dis. 2004, 40, 414–419. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Smith, L.; Sugiyama, H. Botulism in animals and fish. In Botulism, the Organism, its Toxins, the Disease; Smith, L., Sugiyama, H., Eds.; Charles C. Thomas: Springfield, IL, USA, 1988; pp. 135–146. [Google Scholar]
- Lamanna, C. The scope of the avian botulism problem. In Avian Botulism; Eklund, M., Dowell, V., Eds.; Charles C. Thomas: Springfield, IL, USA, 1987; pp. 5–11. [Google Scholar]
- Anniballi, F.; Fiore, A.; Lofstrom, C.; Skarin, H.; Auricchio, B.; Woudstra, C.; Bano, L.; Segerman, B.M.K.; Baverud, V.; Hansen, T. Management of animla botulism outbreaks: From clinical suspicion to prectical countermeasures to prevent or minimize outbreaks. Biosec. Bioterr. 2013, 11, S191–S198. [Google Scholar] [CrossRef]
- Critchley, E.M. A comparison of human and animal botulism: A review. J. R. Soc. Med. 1991, 84, 295–298. [Google Scholar] [CrossRef]
- Rossetto, O.; Pirazzini, M.; Montecucco, C. Botulinum neurotoxins: Genetic, structural and mechanistic insights. Nat. Rev. Microbiol. 2014, 12, 535–549. [Google Scholar] [CrossRef]
- Yule, A.M.; Barker, I.K.; Austin, J.W.; Moccia, R.D. Toxicity of Clostridium botulinum type E neurotoxin to Great Lakes fish: Implications for avian botulism. J. Wildl. Dis. 2006, 42, 479–493. [Google Scholar] [CrossRef]
- Stampfli, H.; Oliver-Espinosa, O. Botulism in animals. Available online: https://www.merckvetmanual.com/generalized-conditions/clostridial-diseases/botulism-in-animals?_gl=1*12fu0gv*_up*MQ..&gclid=Cj0KCQjwr82iBhCuARIsAO0EAZzYBDBgMeg1fJ-2Xmhebe6qmFqnlH67hxaKdVsc-z7EiKbk_ZAF3UwaArANEALw_wcB&gclsrc=aw.ds (accessed on 28 April 2023).
- Ortolani, E.L.; Brito, L.A.; Mori, C.S.; Schalch, U.; Pacheco, J.; Baldacci, L. Botulism outbreak associated with poultry litter consumption in three Brazilian cattle herds. Vet. Hum. Toxicol. 1997, 39, 89–92. [Google Scholar]
- McLoughlin, M.F.; McLlroy, S.G.; Neill, S.D. A major outbreak of botulism in cattle being fed ensiled poultry litter. Vet. Rec. 1988, 122, 579–581. [Google Scholar] [CrossRef]
- Stampfli, H. Botulism in horses. Available online: https://www.merckvetmanual.com/horse-owners/disorders-affecting-multiple-body-systems-of-horses/botulism-in-horses (accessed on 28 April 2023).
- Rasetti-Escargueil, C.; Lemichez, E.; Popoff, M.R. Public Health Risk Associated with Botulism as Foodborne Zoonoses. Toxins 2019, 12, 17. [Google Scholar] [CrossRef] [PubMed]
- Hendrickx, D.; Varela Martinez, C.; Contzen, M.; Wagner-Wiening, C.; Janke, K.H.; Hernando Jimenez, P.; Massing, S.; Pichler, J.; Tichaczek-Dischinger, P.; Burckhardt, F.; et al. First cross-border outbreak of foodborne botulism in the European Union associated with the consumption of commercial dried roach (Rutilus rutilus). Front. Public. Health 2022, 10, 1039770. [Google Scholar] [CrossRef] [PubMed]
- Souillard, R.; Grosjean, D.; Le Gratiet, T.; Poezevara, T.; Rouxel, S.; Balaine, L.; Mace, S.; Martin, L.; Anniballi, F.; Chemaly, M.; et al. Asymptomatic Carriage of C. botulinum Type D/C in Broiler Flocks as the Source of Contamination of a Massive Botulism Outbreak on a Dairy Cattle Farm. Front. Microbiol. 2021, 12, 679377. [Google Scholar] [CrossRef] [PubMed]
- Palmateer, N.E.; Hope, V.D.; Roy, K.; Marongiu, A.; White, J.M.; Grant, K.A.; Ramsay, C.N.; Goldberg, D.J.; Ncube, F. Infections with spore-forming bacteria in persons who inject drugs, 2000–2009. Emerg. Infect. Dis. 2013, 19, 29–34. [Google Scholar] [CrossRef]
- Halpin, J.L.; Foltz, V.; Dykes, J.K.; Chatham-Stephens, K.; Luquez, C. Clostridium botulinum Type B Isolated From a Wound Botulism Case Due to Injection Drug Use Resembles Other Local Strains Originating From Hawaii. Front. Microbiol. 2021, 12, 678473. [Google Scholar] [CrossRef]
- Dabritz, H.A.; Hill, K.K.; Barash, J.R.; Ticknor, L.O.; Helma, C.H.; Dover, N.; Payne, J.R.; Arnon, S.S. Molecular epidemiology of infant botulism in California and elsewhere, 1976–2010. J. Infect. Dis. 2014, 210, 1711–1722. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Panditrao, M.V.; Chung, C.H.; Khouri, J.M.; Barash, J.R.; Motter, R.N.; Dover, N.; Arnon, S.S. Dual-Toxin (“Bivalent”) Infant Botulism in California, 1976–2020: Epidemiologic, Clinical, and Laboratory Aspects. J. Pediatr. 2023, 253, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Raphael, B.H.; Shirey, T.B.; Luquez, C.; Maslanka, S.E. Distinguishing highly-related outbreak-associated Clostridium botulinum type A(B) strains. BMC Microbiol. 2014, 14, 192. [Google Scholar] [CrossRef]
- Ma, X.; Li, K.; Li, F.; Su, J.; Meng, W.; Sun, Y.; Sun, H.; Sun, J.; Yuan, Y.; Lin, Y.; et al. Tracing Foodborne Botulism Events Caused by Clostridium botulinum in Xinjiang Province, China, Using a Core Genome Sequence Typing Scheme. Microbiol. Spectr. 2022, 10, e0116422. [Google Scholar] [CrossRef]
- Halpin, J.L.; Gomez, G.A.; Dykes, J.K.; Luquez, C. Draft Genome Sequences of 20 Clostridium botulinum Type A Isolates from Foodborne Botulism Outbreaks. Microbiol. Resour. Announc. 2023, 12, e0086822. [Google Scholar] [CrossRef]
- CDC. Botulism in the United States, 1899–1996 Handbook for Epidemiologists, Clinicians, and Laboratory Workers; CDC: Atlanta, GA, USA, 1998. [Google Scholar]
- Dolman, C.E. Botulism. Am. J. Nurs. 1964, 64, 119–124. [Google Scholar]
- Leclair, D.; Farber, J.M.; Doidge, B.; Blanchfield, B.; Suppa, S.; Pagotto, F.; Austin, J.W. Distribution of Clostridium botulinum type E strains in Nunavik, Northern Quebec, Canada. Appl. Environ. Microbiol. 2013, 79, 646–654. [Google Scholar] [CrossRef]
- Rebagliati, V.; Philippi, R.; Tornese, M.; Paiva, A.; Rossi, L.; Troncoso, A. Food-borne botulism in Argentina. J. Infect. Dev. Ctries. 2009, 3, 250–254. [Google Scholar] [CrossRef][Green Version]
- Long, S.S.; Gajewski, J.L.; Brown, L.W.; Gilligan, P.H. Clinical, laboratory, and environmental features of infant botulism in Southeastern Pennsylvania. Pediatrics 1985, 75, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Dolman, C.E.; Chang, H.; Kerr, D.E.; Shearer, A.R. Fish-borne and type E botulism: Two cases due to home-pickled herring. Can. J. Public. Health 1950, 41, 215–229. [Google Scholar]
- Eklund, M.W.; Wieler, D.I.; Poysky, F.T. Outgrowth and toxin production of nonproteolytic type B Clostridium botulinum at 3.3 to 5.6 C. J. Bacteriol. 1967, 93, 1461–1462. [Google Scholar] [CrossRef]
- Leclair, D.; Fung, J.; Isaac-Renton, J.L.; Proulx, J.F.; May-Hadford, J.; Ellis, A.; Ashton, E.; Bekal, S.; Farber, J.M.; Blanchfield, B.; et al. Foodborne botulism in Canada, 1985-2005. Emerg. Infect. Dis. 2013, 19, 961–968. [Google Scholar] [CrossRef]
- Dahlsten, E.; Korkeala, H.; Somervuo, P.; Lindstrom, M. PCR assay for differentiating between Group I (proteolytic) and Group II (nonproteolytic) strains of Clostridium botulinum. Int. J. Food Microbiol. 2008, 124, 108–111. [Google Scholar] [CrossRef]
- Sobel, J.; Tucker, N.; Sulka, A.; McLaughlin, J.; Maslanka, S. Foodborne botulism in the United States, 1990–2000. Emerg. Infect. Dis. 2004, 10, 1606–1611. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K. The protective measures of the state of California against botulism. J. Prev. Med. 1931, 5, 261–293. [Google Scholar]
- Shapiro, R.L.; Hatheway, C.; Swerdlow, D.L. Botulism in the United States: A clinical and epidemiologic review. Ann. Intern. Med. 1998, 129, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.A. Control of Clostridium botulinum in Foods. In New Weapons to Control Bacterial Growth; Villa, T., Vinas, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; pp. 83–93. [Google Scholar]
- National Advisory Committee on Microbiological Criteria for Foods. Parameters for determining inoculated pack/challenge study protocols. J. Food Protect. 2010, 74, 522. [Google Scholar]
- Poortmans, M.; Vanoirbeek, K.; Dorner, M.; Michiels, C. Selection and development of nontoxic nonproteolytic Clostridium botulinum surrogate strains for food challenge testing. Foods 2022, 11, 1577. [Google Scholar] [CrossRef]
- Brown, J.; Tran-Dinh, N.; Chapman, B. Clostridium sporogenes PA 3679 and its uses in the derivation of thermal processing schedules for low-acid shelf-stable foods and as a research model for proteolytic Clostridium botulinum. J. Food Protect. 2012, 75, 779–792. [Google Scholar]
- Schill, K.M.; Wang, Y.; Butler, R.R., 3rd; Pombert, J.F.; Reddy, N.R.; Skinner, G.E.; Larkin, J.W. Genetic Diversity of Clostridium sporogenes PA 3679 Isolates Obtained from Different Sources as Resolved by Pulsed-Field Gel Electrophoresis and High-Throughput Sequencing. Appl. Environ. Microbiol. 2016, 82, 384–393. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peck, M.W. Clostridium botulinum and the safety of minimally heated, chilled foods: An emerging issue? J. Appl. Microbiol. 2006, 101, 556–570. [Google Scholar] [CrossRef]
- Bowe, B.K.; Wentz, T.G.; Gregg, B.M.; Tepp, W.H.; Schill, K.M.; Sharma, S.; Pellett, S. Genomic diversity, competition, and toxin production by Group I and II Clostridium botulinum strains used in food challenge studies. Microorganisms 2022, 10, 1895. [Google Scholar] [CrossRef]
- Precedence Research. Botulinum Toxin Market (Product Type: Type A, Type B; Application: Therapeutic, Aesthetic, Glabellar Lines, Crow’s Feet, Forehead Lines, Others; End-Use, Hospitals, Dermatology Clinics, Spas & Cosmetic Centres) - Global Industry Analysis, Size, Share, Growth, Trends, Regional Outlook, and Forecast 2023-2032. Available online: https://www.precedenceresearch.com/botulinum-toxin-market (accessed on 14 June 2023).
- Chertow, D.S.; Tan, E.T.; Maslanka, S.E.; Schulte, J.; Bresnitz, E.A.; Weisman, R.S.; Bernstein, J.; Marcus, S.M.; Kumar, S.; Malecki, J.; et al. Botulism in 4 adults following cosmetic injections with an unlicensed, highly concentrated botulinum preparation. JAMA 2006, 296, 2476–2479. [Google Scholar] [CrossRef] [PubMed]
| Year | Bacterial Species Identifications | Identifications of Associated Toxins | References |
|---|---|---|---|
| 1897 | First BoNT-producing bacteria isolated (Bacillus botulinus) from a nonproteolytic organism | Botulinum toxin verified | [1] |
| 1904 | Second B. botulinus isolated; different characteristics (proteolytic) | Botulinum toxin verified | [2] |
| 1910, 1919 | B. botulinus | Discovery that Van Ermengem and Landmann toxins differ serologically, designated type A and type B | [3,4] |
| 1917 | B. botulinus nomenclature changed to Clostridium botulinum | [6] | |
| 1922 | Proteolytic C. botulinum name changed to C. parabotulinum | Type C toxin isolated from proteolytic C. botulinum, serologically confirmed | [7] |
| 1924 | C. botulinum name retained to reflect nonproteolytic status | Serologically distinct Type C toxin isolated from nonproteolytic C. botulinum | [8] |
| 1928 | C. parabotulinum | Type D toxin serologically confirmed | [9] |
| 1929 | C. parabotulinum/C. botulinum | The distinct type C toxins designated Cα, Cβ | [10] |
| 1937 | Type E-producing bacterium isolated from nonproteolytic C. botulinum | Type E toxin serologically confirmed | [11] |
| 1953 | Proposal that all BoNT-producing clostridia be named C. botulinum | [12] | |
| 1960 | Type F-producing bacterium isolated from proteolytic C. botulinum | Type F toxin serologically confirmed | [13] |
| 1967 | Type F-producing bacterium isolated from nonproteolytic C. botulinum | Type F toxin serologically confirmed | [14] |
| 1970 | C. botulinum | Type G toxin serologically confirmed | [15] |
| 1977 | Group system (C. botulinum Groups I–IV) instituted for improved detection of BoNT-producing bacteria | [16] | |
| 1986 | Type E-producing neuro-toxigenic Clostridium butyricum bacterium isolated (genetically confirmed) | Type E toxin serologically confirmed | [17] |
| 1988 | Type F-producing neuro-toxigenic Clostridium baratii bacterium isolated (genetically confirmed) | Type F toxin serologically confirmed | [18] |
| 1988 | BoNT/G-producing C. botulinum renamed Clostridium argentinense due to physiological/genetic differences with C. botulinum | [19] | |
| 1990 | C. botulinum | Cβ toxin renamed BoNT/C1 to distinguish from non-neurogenic C2 and C3 toxins that are also present in these strains | [20] |
| 1995 | C. botulinum | Beginnings of toxin subtype enumerations (A1, A2, etc.) | [21] |
| 1996 | C. botulinum | Discovery of BoNT/CD (Cα) and BoNT/DC mosaic toxins | [22] |
| 2011 | Proposal to rename C. botulinum Group III to genospecies C. novyi sensu lato due to genomic similarities with C. novyi | Produce BoNT/C and BoNT/D toxin subtypes | [23] |
| 2013 | C. botulinum | Novel toxin identified from an infant botulism case, designated H/FA/HA | [24,25] |
| 2016 | Discovery of type B-producing neuro-toxigenic Clostridium sporogenes | Produce multiple BoNT/B subtypes | [26,27] |
| 2017 | C. botulinum, Weisella spp., Chryseobacterium spp. | BoNT-like neurotoxins (including BoNT/X) discovered through genomic mining | [28,29,30] |
| Toxin Subtypes | Bacterial Metabolic Type | Species/Groups/Lineages |
|---|---|---|
| A1–A8, HA | proteolytic | C. parabotulinum (C. botulinum Group I) |
| B1–B3, B5–B8 | proteolytic | C. parabotulinum (C. botulinum Group I) |
| B1, B2, B5, B6 | proteolytic | C. sporogenes (C. botulinum Group I) |
| B4 | nonproteolytic | C. botulinum (Group II BEF) |
| C, CD, D, DC | proteolytic | C. novyi sensu lato (C. botulinum Group III) |
| E1–E3, E6–E8, E10–12 | nonproteolytic | C. botulinum (Group II E) |
| E4, E5 | nonproteolytic | C. butyricum |
| E9 | nonproteolytic | C. botulinum (Group II BEF) |
| F1–F5, F8 | proteolytic | C. parabotulinum (C. botulinum Group I) |
| F6 | nonproteolytic | C. botulinum (Group II BEF) |
| F7 | nonproteolytic | C. baratii |
| G | proteolytic | C. argentinense |
| Group I (C. botulinum) | Group I (C. sporogenes) | Group II (C. botulinum) | Group III (C. botulinum) | Group IV (C. argentinense) | Group V (C. baratii) | Group VI (C. butyricum) | |
|---|---|---|---|---|---|---|---|
| Lipase produced | + | + | + | + | - | - | - |
| Lecithinase produced | - | - | - | −/+ | - | + | - |
| Esculin hydrolyzed | + | + | - | - | - | + | + |
| Starch hydrolyzed | - | - | +/− | - | - | +/− | + |
| Proteolytic? | yes | yes | no | weak/variable | yes | no | no |
| Saccharolytic? | no | no | yes | weak/variable | no | yes | yes |
| Heat resistance of spores | high | low | intermediate | ||||
| Optimal growth temperature | 35–40 °C | 35–40 °C | 18–35 °C | 40 °C | 37 °C | 30–45 °C | 30–37 °C |
| Minimal growth temperature | 10+ °C | 4 °C | 15 °C | 10 °C |
| Laboratory animals | Susceptible to toxin types: |
|---|---|
| Mice | Susceptible to all toxin types |
| Guinea pigs | Susceptible to all toxin types |
| Rats | Resistant to all toxin types except BoNT/A |
| Domestic animals | Susceptible to toxin types: |
| Cattle | C, D, D/C, (A, B, C/D) |
| Horses | B, C, (A) |
| Sheep/goats | C, D |
| Poultry | C/D |
| Pigs | Appear to be resistant to all toxin types |
| Minks/foxes/ferrets | C, (A, E) |
| Wild animals | Susceptible to toxin types: |
| Migratory birds | C/D |
| Waterfowl/fish-eating raptors | C, E |
| Bighorn sheep | C |
| Fish | E |
| Turtles | C |
| Vultures, flamingos | Appear to be resistant to all toxin types |
| Generic Name | Brand Name(s) | Company | Toxin State |
|---|---|---|---|
| onabotulinumtoxinA | Botox/Botox Cosmetic/Vistabel/Vistabex | Abbvie. Inc. (Allergan), Irving, CA | BoNT/A complex |
| abobotulinumtoxinA | Dysport/Azzalure | Ipsen (Galderma) Cambridge, MA | BoNT/A complex |
| incobotulinumtoxinA | Xeomin | Merz Pharmaceuticals Frankfort, Germany | BoNT/A |
| letibotulinumtoxinA | Botulax/Letybo | Hugel, Inc. South Korea | BoNT/A unknown |
| nivobotulinumtoxinA | Meditoxin/Botulift | Medytox, Inc South Korea | BoNT/A complex |
| prabotulinumtoxinA | Jeuveau/Nabota | Daewoong Pharmaceutical South Korea | BoNT/A complex |
| daxibotulinumtoxinA-lanm | Daxxify | Revance Therapeutics Nashville, TN | BoNT/A |
| rimabotulinumtoxinB | MyoBloc/Neurobloc | Solstice Neurosciences, LLC South San Francisco, CA | BoNT/B complex |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, T.J.; Schill, K.M.; Williamson, C.H.D. Navigating the Complexities Involving the Identification of Botulinum Neurotoxins (BoNTs) and the Taxonomy of BoNT-Producing Clostridia. Toxins 2023, 15, 545. https://doi.org/10.3390/toxins15090545
Smith TJ, Schill KM, Williamson CHD. Navigating the Complexities Involving the Identification of Botulinum Neurotoxins (BoNTs) and the Taxonomy of BoNT-Producing Clostridia. Toxins. 2023; 15(9):545. https://doi.org/10.3390/toxins15090545
Chicago/Turabian StyleSmith, Theresa J., Kristin M. Schill, and Charles H. D. Williamson. 2023. "Navigating the Complexities Involving the Identification of Botulinum Neurotoxins (BoNTs) and the Taxonomy of BoNT-Producing Clostridia" Toxins 15, no. 9: 545. https://doi.org/10.3390/toxins15090545
APA StyleSmith, T. J., Schill, K. M., & Williamson, C. H. D. (2023). Navigating the Complexities Involving the Identification of Botulinum Neurotoxins (BoNTs) and the Taxonomy of BoNT-Producing Clostridia. Toxins, 15(9), 545. https://doi.org/10.3390/toxins15090545





