Contribution of Mass Spectrometry to the Advances in Risk Characterization of Marine Biotoxins: Towards the Characterization of Metabolites Implied in Human Intoxications
Abstract
1. Introduction
2. Mass Spectrometry to Identify Marine Biotoxins Metabolites
2.1. Lipophilic Toxins Metabolites
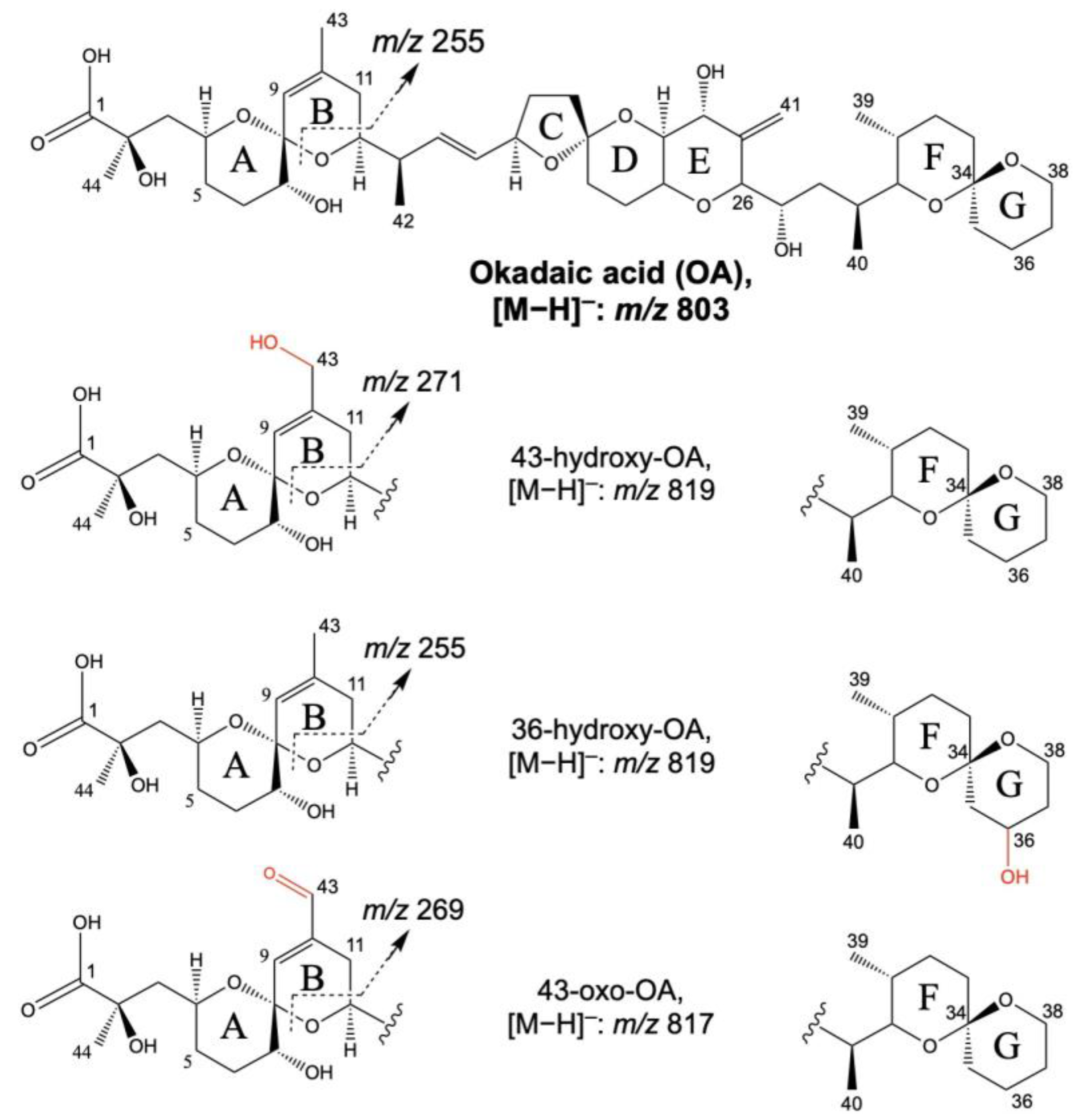
2.1.1. Diarrhetic Shellfish Poisoning Toxins and Azaspirazids Metabolites
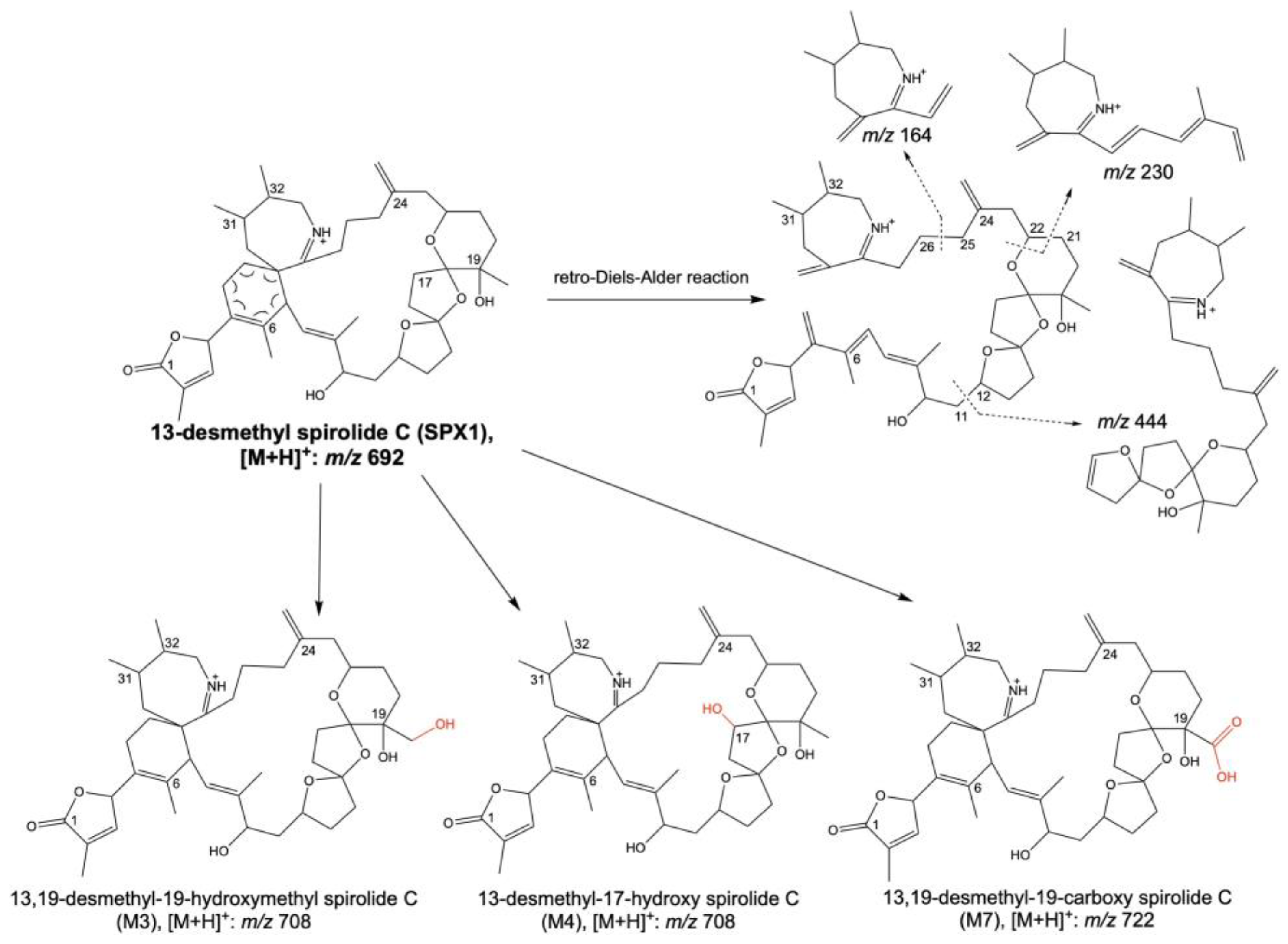
2.1.2. Spirolides Metabolites
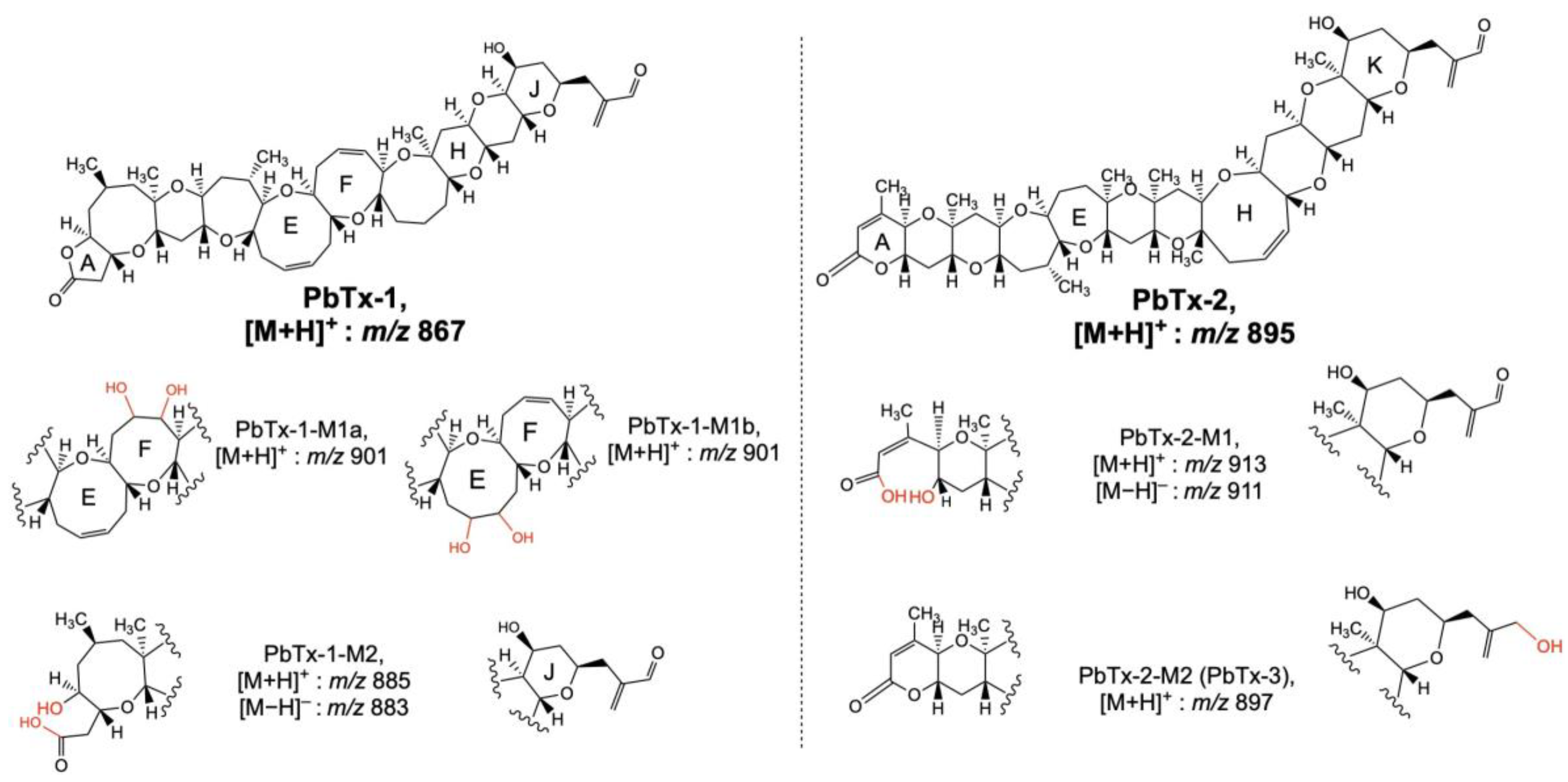
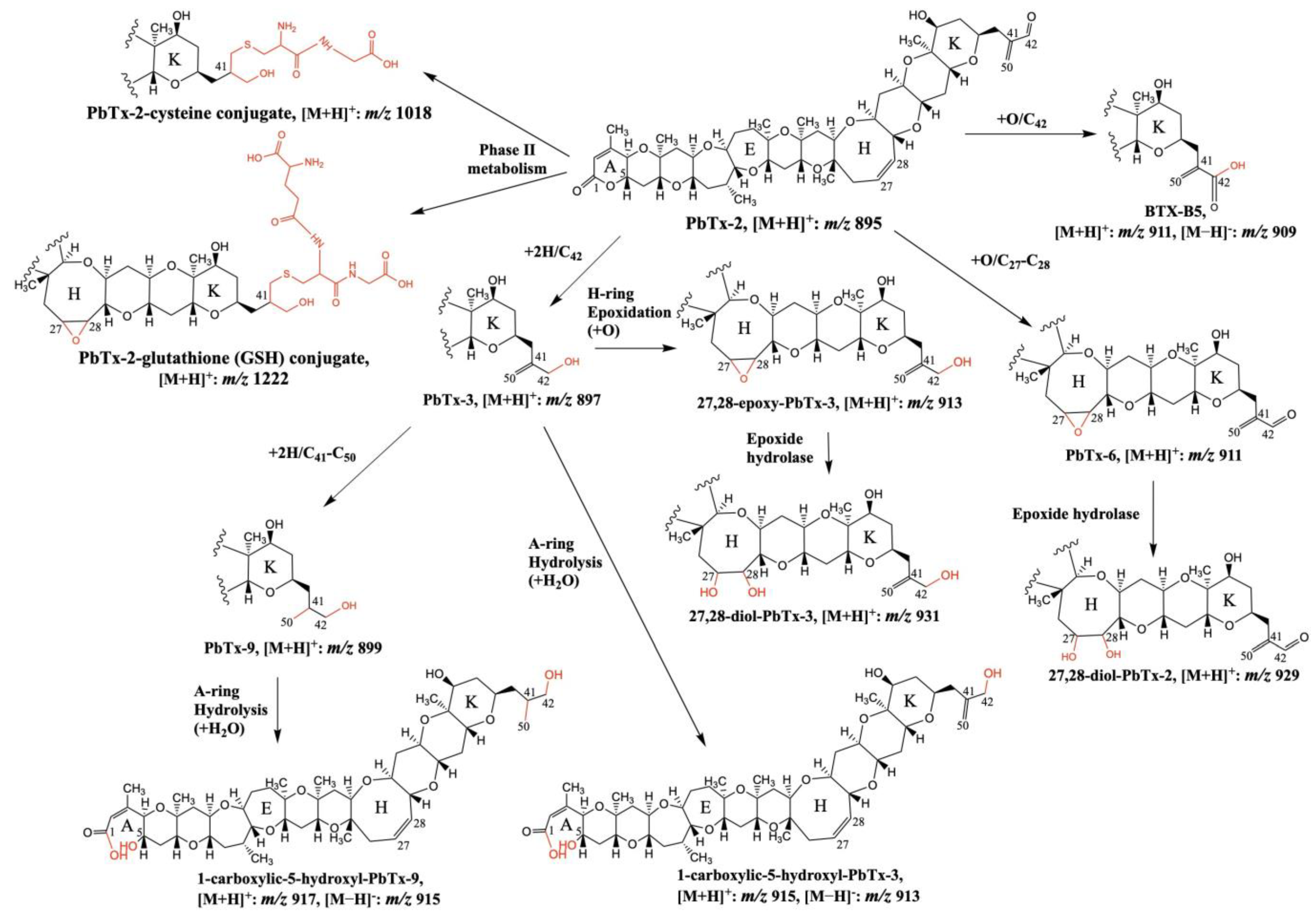
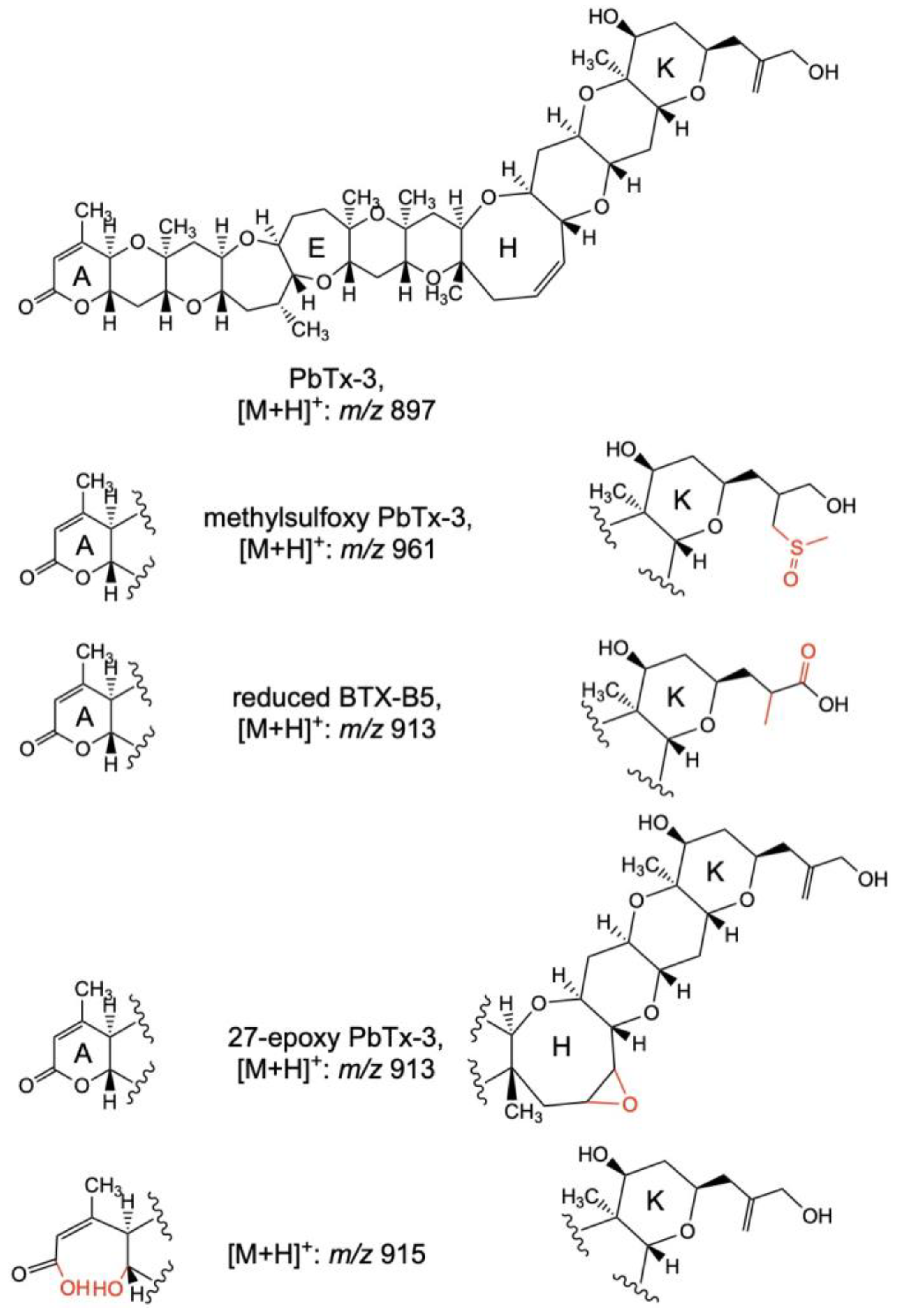
2.1.3. Brevetoxins Metabolites
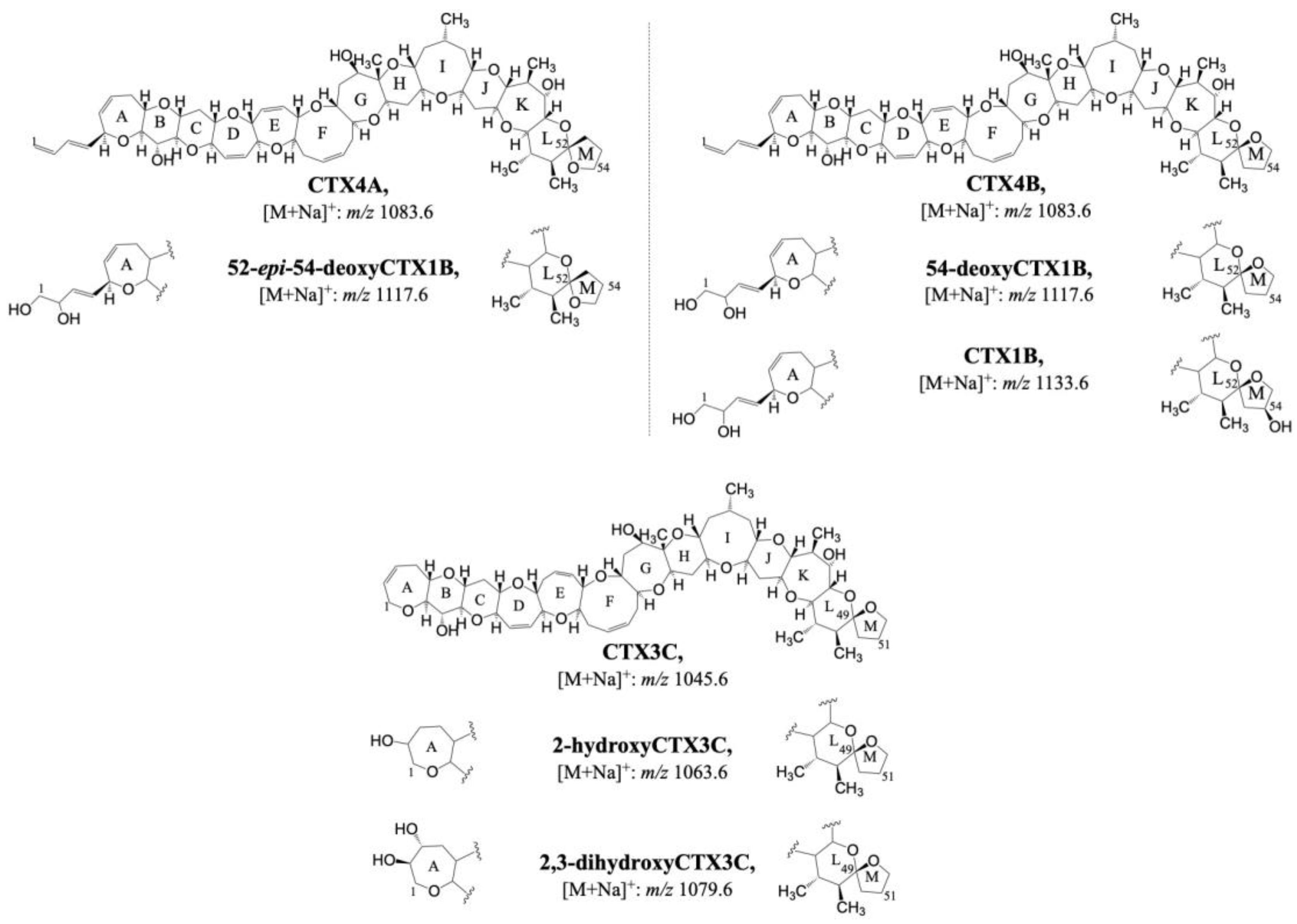
2.1.4. Ciguatoxins Metabolites
2.2. Hydrophilic Toxins Metabolites
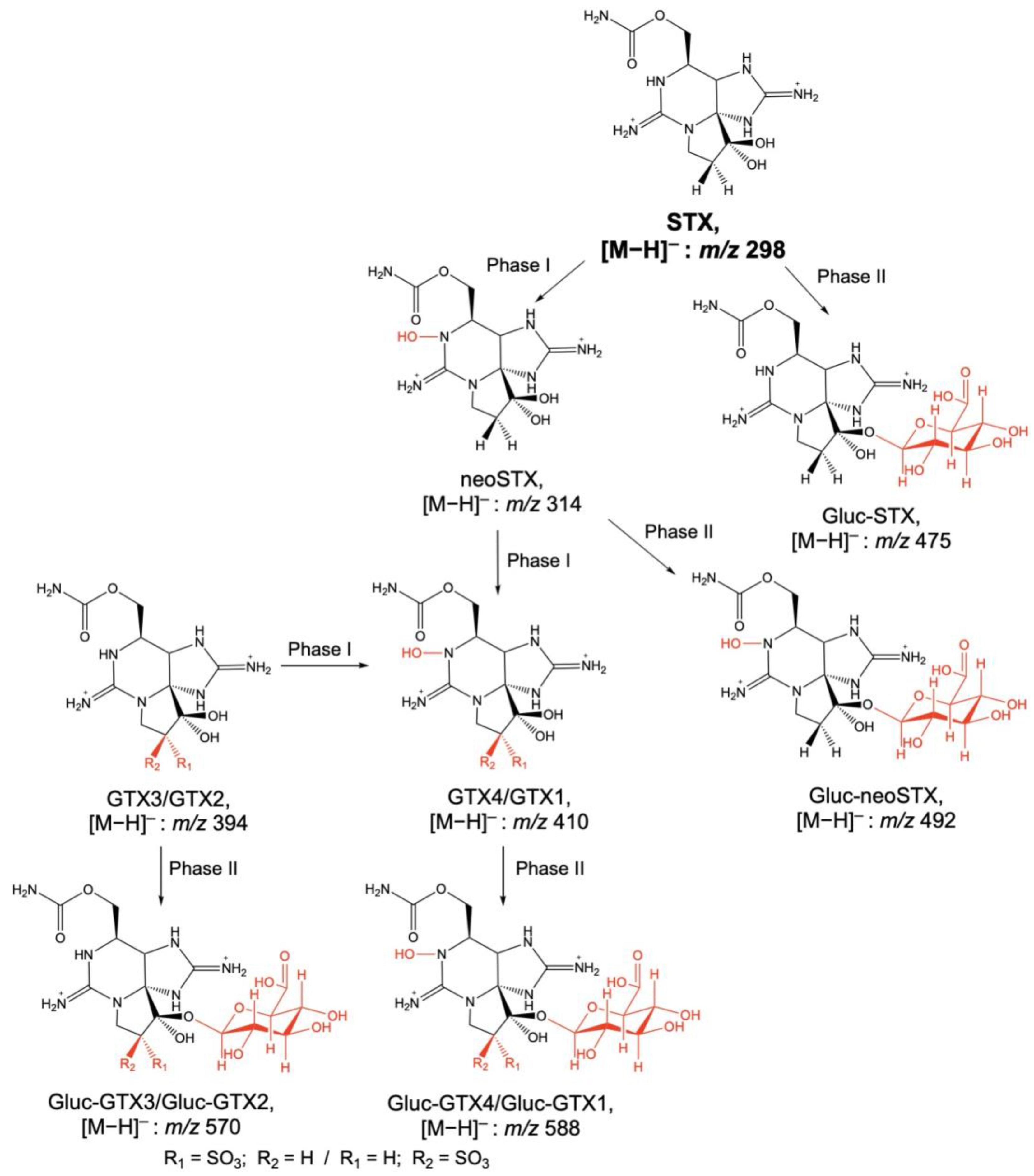
Paralytic Shellfish Toxins (PSTs) Metabolites
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Otero, P.; Silva, M. Emerging Marine Biotoxins in European Waters: Potential Risks and Analytical Challenges. Mar. Drugs 2022, 20, 199. [Google Scholar] [CrossRef] [PubMed]
- Louzao, M.C.; Vilariño, N.; Vale, C.; Costas, C.; Cao, A.; Raposo-garcia, S.; Vieytes, M.R.; Botana, L.M. Current Trends and New Challenges in Marine Phycotoxins. Mar. Drugs 2022, 20, 198. [Google Scholar] [CrossRef] [PubMed]
- Hallegraeff, G.M. OCEAN CLIMATE CHANGE, PHYTOPLANKTON COMMUNITY RESPONSES, AND HARMFUL ALGAL BLOOMS: A FORMIDABLE PREDICTIVE CHALLENGE. J. Phycol. 2010, 46, 220–235. [Google Scholar] [CrossRef]
- Visciano, P.; Schirone, M.; Berti, M.; Milandri, A.; Tofalo, R.; Suzzi, G. Marine Biotoxins: Occurrence, Toxicity, Regulatory Limits and Reference Methods. Front. Microbiol. 2016, 7, 1051. [Google Scholar] [CrossRef]
- Smith, V.H. Eutrophication of Freshwater and Coastal Marine Ecosystems a Global Problem. Environ. Sci. Pollut. Res. 2003, 10, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Pratheepa, V.K.; Botana, L.M.; Vasconcelos, V. Emergent Toxins in North Atlantic Temperate Waters: A Challenge for Monitoring Programs and Legislation. Toxins 2015, 7, 859–885. [Google Scholar] [CrossRef]
- Bagnis, R.; Berglund, F.; Elias, P.S.; van Esch, G.J.; Halstead, B.W.; Kojima, K. Problems of Toxicants in Marine Food Products. 1. Marine Biotoxins. Bull. World Health Organ. 1970, 42, 69–88. [Google Scholar]
- Landsberg, J.H. The Effects of Harmful Algal Blooms on Aquatic Organisms. Rev. Fish. Sci. 2002, 10, 113–390. [Google Scholar] [CrossRef]
- Ciminiello, P.; Fattorusso, E. Bivalve Molluscs as Vectors of Marine Biotoxins Involved in Seafood Poisoning. In Molluscs: From Chemo-Ecological Study to Biotechnological Application; Cimino, G., Gavagnin, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; pp. 53–82. ISBN 978-3-540-30880-5. [Google Scholar]
- James, K.J.; Carey, B.; O’Halloran, J.; van Pelt, F.N.A.M.; Škrabáková, Z. Shellfish Toxicity: Human Health Implications of Marine Algal Toxins. Epidemiol. Infect. 2010, 138, 927–940. [Google Scholar] [CrossRef]
- Hess, P. Requirements for Screening and Confirmatory Methods for the Detection and Quantification of Marine Biotoxins in End-Product and Official Control. Anal. Bioanal. Chem. 2010, 397, 1683–1694. [Google Scholar] [CrossRef]
- EFSA Panel on Contaminants in the Food Chain (CONTAM); Knutsen, H.K.; Alexander, J.; Barregård, L.; Bignami, M.; Brüschweiler, B.; Ceccatelli, S.; Cottrill, B.; DiNovi, M.; Edler, L.; et al. Risks for Public Health Related to the Presence of Tetrodotoxin (TTX) and TTX Analogs in Marine Bivalves and Gastropods. EFSA J. 2017, 15, e04752. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Contaminants in the Food Chain (CONTAM). Scientific Opinion on Marine Biotoxins in Shellfish—Cyclic Imines (Spirolides, Gymnodimines, Pinnatoxins and Pteriatoxins). EFSA J. 2010, 8, 1628. [Google Scholar] [CrossRef]
- EFSA Panel on Contaminants in the Food Chain. Scientific Opinion on Marine Biotoxins in Shellfish—Emerging Toxins: Ciguatoxin Group. EFSA J. 2010, 8, 1627. [Google Scholar] [CrossRef]
- Alexander, J.; Benford, D.; Boobis, A.; Ceccatelli, S.; Cravedi, J.-P.; di Domenico, A.; Doerge, D.; Dogliotti, E.; Edler, L.; Farmer, P.; et al. Scientific Opinion on Marine Biotoxins in Shellfish—Emerging Toxins: Brevetoxin Group. EFSA J. 2010, 8, 1677. [Google Scholar] [CrossRef]
- Farabegoli, F.; Blanco, L.; Rodríguez, L.P.; Vieites, J.M.; Cabado, A.G. Phycotoxins in Marine Shellfish: Origin, Occurrence and Effects on Humans. Mar. Drugs 2018, 16, 188. [Google Scholar] [CrossRef]
- Vilariño, N.; Louzao, M.C.; Abal, P.; Cagide, E.; Carrera, C.; Vieytes, M.R.; Botana, L.M. Human Poisoning from Marine Toxins: Unknowns for Optimal Consumer Protection. Toxins 2018, 10, 324. [Google Scholar] [CrossRef] [PubMed]
- Vale, P.; Botelho, M.J.; Rodrigues, S.M.; Gomes, S.S.; Sampayo, M.A.d.M. Two Decades of Marine Biotoxin Monitoring in Bivalves from Portugal (1986–2006): A Review of Exposure Assessment. Harmful Algae 2008, 7, 11–25. [Google Scholar] [CrossRef]
- Nicolas, J.; Hoogenboom, R.L.A.P.; Hendriksen, P.J.M.; Bodero, M.; Bovee, T.F.H.; Rietjens, I.M.C.M.; Gerssen, A. Marine Biotoxins and Associated Outbreaks Following Seafood Consumption: Prevention and Surveillance in the 21st Century. Glob. Food Secur. 2017, 15, 11–21. [Google Scholar] [CrossRef]
- Gerssen, A.; Mulder, P.P.J.; McElhinney, M.A.; de Boer, J. Liquid Chromatography-Tandem Mass Spectrometry Method for the Detection of Marine Lipophilic Toxins under Alkaline Conditions. J. Chromatogr. A 2009, 1216, 1421–1430. [Google Scholar] [CrossRef]
- Dell’Aversano, C.; Hess, P.; Quilliam, M.A. Hydrophilic interaction liquid chromatography-mass spectrometry for the analysis of paralytic shellfish poisoning (PSP) toxins. J. Chromatogr. A 2005, 1081, 190–201. [Google Scholar] [CrossRef]
- Christian, B.; Luckas, B. Determination of Marine Biotoxins Relevant for Regulations: From the Mouse Bioassay to Coupled LC–MS Methods. Anal. Bioanal. Chem. 2008, 391, 117–134. [Google Scholar] [CrossRef]
- Zendong, Z.; McCarron, P.; Herrenknecht, C.; Sibat, M.; Amzil, Z.; Cole, R.B.; Hess, P. High Resolution Mass Spectrometry for Quantitative Analysis and Untargeted Screening of Algal Toxins in Mussels and Passive Samplers. J. Chromatogr. A 2015, 1416, 10–21. [Google Scholar] [CrossRef] [PubMed]
- van den Top, H.J.; Gerssen, A.; McCarron, P.; van Egmond, H.P. Quantitative Determination of Marine Lipophilic Toxins in Mussels, Oysters and Cockles Using Liquid Chromatography-Mass Spectrometry: Inter-Laboratory Validation Study. Food Addit. Contam. Part A 2011, 28, 1745–1757. [Google Scholar] [CrossRef] [PubMed]
- Gerssen, A.; van Olst, E.H.W.; Mulder, P.P.J.; de Boer, J. In-House Validation of a Liquid Chromatography Tandem Mass Spectrometry Method for the Analysis of Lipophilic Marine Toxins in Shellfish Using Matrix-Matched Calibration. Anal. Bioanal. Chem. 2010, 397, 3079–3088. [Google Scholar] [CrossRef] [PubMed]
- Braña-Magdalena, A.; Leão-Martins, J.M.; Glauner, T.; Gago-Martínez, A. Intralaboratory Validation of a Fast and Sensitive UHPLC/MS/MS Method with Fast Polarity Switching for the Analysis of Lipophilic Shellfish Toxins. J. AOAC Int. 2014, 97, 285–292. [Google Scholar] [CrossRef]
- Turner, A.D.; McNabb, P.S.; Harwood, D.T.; Selwood, A.I.; Boundy, M.J. Single-Laboratory Validation of a Multitoxin Ultra-Performance LC–Hydrophilic Interaction LC–MS/MS Method for Quantitation of Paralytic Shellfish Toxins in Bivalve Shellfish. J. AOAC Int. 2015, 98, 609–621. [Google Scholar] [CrossRef] [PubMed]
- Boundy, M.J.; Selwood, A.I.; Harwood, D.T.; McNabb, P.S.; Turner, A.D. Development of a Sensitive and Selective Liquid Chromatography-Mass Spectrometry Method for High Throughput Analysis of Paralytic Shellfish Toxins Using Graphitised Carbon Solid Phase Extraction. J. Chromatogr. A 2015, 1387, 1–12. [Google Scholar] [CrossRef]
- Lawrence, J.F.; Niedzwiadek, B.; Menard, C.; de Rojas Astudillo, L.; Biré, R.; Burdaspal, P.A.; Ceredi, A.; Davis, B.; Dias, E.; Eaglesham, G.; et al. Quantitative Determination of Paralytic Shellfish Poisoning Toxins in Shellfish Using Prechromatographic Oxidation and Liquid Chromatography with Fluorescence Detection: Collaborative Study. J. AOAC Int. 2005, 88, 1714–1732. [Google Scholar] [CrossRef]
- Estevez, P.; Castro, D.; Leao, J.M.; Yasumoto, T.; Dickey, R.; Gago-Martinez, A. Implementation of Liquid Chromatography Tandem Mass Spectrometry for the Analysis of Ciguatera Fish Poisoning in Contaminated Fish Samples from Atlantic Coasts. Food Chem. 2019, 280, 8–14. [Google Scholar] [CrossRef]
- Klijnstra, M.D.; Faassen, E.J.; Gerssen, A. A Generic LC–HRMS Screening Method for Marine and Freshwater Phycotoxins in Fish, Shellfish, Water, and Supplements. Toxins 2021, 13, 823. [Google Scholar] [CrossRef]
- Estevez, P.; Castro, D.; Pequeño-Valtierra, A.; Giraldez, J.; Gago-Martinez, A. Emerging Marine Biotoxins in Seafood from European Coasts: Incidence and Analytical Challenges. Foods 2019, 8, 149. [Google Scholar] [CrossRef] [PubMed]
- Warth, B.; Sulyok, M.; Fruhmann, P.; Mikula, H.; Berthiller, F.; Schuhmacher, R.; Hametner, C.; Abia, W.A.; Adam, G.; Fröhlich, J.; et al. Development and Validation of a Rapid Multi-Biomarker Liquid Chromatography/Tandem Mass Spectrometry Method to Assess Human Exposure to Mycotoxins. Rapid Commun. Mass Spectrom. 2012, 26, 1533–1540. [Google Scholar] [CrossRef] [PubMed]
- Burton, I.W.; Quilliam, M.A.; Walter, J.A. Quantitative 1H NMR with External Standards: Use in Preparation of Calibration Solutions for Algal Toxins and Other Natural Products. Anal. Chem. 2005, 77, 3123–3131. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.J.; Beach, D.G.; McCarron, P. Non-Target Analysis and Stability Assessment of Reference Materials Using Liquid Chromatography–high-Resolution Mass Spectrometry. Anal. Chim. Acta 2022, 1201, 339622. [Google Scholar] [CrossRef] [PubMed]
- Castro, D.; Estévez, P.; Leao-Martins, J.M.; Dickey, R.W.; García-Álvarez, N.; Real, F.; Costa, P.R.; Gago-Martínez, A. Preparation of Ciguatoxin Reference Materials from Canary Islands (Spain) and Madeira Archipelago (Portugal) Fish. J. Mar. Sci. Eng. 2022, 10, 835. [Google Scholar] [CrossRef]
- Kittler, K.; Preiss-Weigert, A.; These, A. Identification Strategy Using Combined Mass Spectrometric Techniques for Elucidation of Phase I and Phase II in Vitro Metabolites of Lipophilic Marine Biotoxins. Anal. Chem. 2010, 82, 9329–9335. [Google Scholar] [CrossRef]
- Hui, J.P.M.; Grossert, J.S.; Cutler, M.J.; Melanson, J.E. Strategic Identification of in Vitro Metabolites of 13-Desmethyl Spirolide C Using Liquid Chromatography/High-Resolution Mass Spectrometry. Rapid Commun. Mass Spectrom. 2012, 26, 345–354. [Google Scholar] [CrossRef]
- Zanger, U.M.; Schwab, M. Cytochrome P450 Enzymes in Drug Metabolism: Regulation of Gene Expression, Enzyme Activities, and Impact of Genetic Variation. Pharmacol. Ther. 2013, 138, 103–141. [Google Scholar] [CrossRef]
- Testa, B.; Pedretti, A.; Vistoli, G. Reactions and Enzymes in the Metabolism of Drugs and Other Xenobiotics. Drug Discov. Today 2012, 17, 549–560. [Google Scholar] [CrossRef]
- Penner, N.; Woodward, C.; Prakash, C. Appendix: Drug Metabolizing Enzymes and Biotransformation Reactions. In ADME-Enabling Technologies in Drug Design and Development; Wiley Online Library: Hoboken, NJ, USA, 2012; pp. 545–565. [Google Scholar] [CrossRef]
- Jancova, P.; Anzenbacher, P.; Anzenbacherova, E. Phase II drug metabolizing enzymes. Biomed. Pap. 2010, 154, 103–116. [Google Scholar] [CrossRef]
- Turner, A.D.; Goya, A.B. Occurrence and Profiles of Lipophilic Toxins in Shellfish Harvested from Argentina. Toxicon 2015, 102, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, X.; Wang, S.; Chen, F.; Cao, W.; Sun, C.; Zheng, L.; Wang, X. Screening of Lipophilic Marine Toxins in Marine Aquaculture Environment Using Liquid Chromatography–Mass Spectrometry. Chemosphere 2017, 168, 32–40. [Google Scholar] [CrossRef] [PubMed]
- EN 32005R2074; COMMISSION REGULATION (EC) No 2074/2005 of 5 December 2005. European Union: Brussels, Belgium, 2005.
- EN 32011R0015; COMMISSION REGULATION (EU) No 15/2011 of 10 January 2011. European Union: Brussels, Belgium, 2011.
- Nagae, M.; Igarashi, T.; Mizukoshi, K.; Kuniyoshi, K.; Oshiro, N.; Yasumoto, T. Development and Validation of an LC–MS/MS Method for the Ultra-Trace Analysis of Pacific Ciguatoxins in Fish. J. AOAC Int. 2021, 104, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Amzil, Z.; Derrien, A.; Terrillon, A.T.; Duval, A.; Connes, C.; Marco-Miralles, F.; Nézan, E.; Mertens, K.N. Monitoring the Emergence of Algal Toxins in Shellfish: First Report on Detection of Brevetoxins in French Mediterranean Mussels. Mar. Drugs 2021, 19, 393. [Google Scholar] [CrossRef]
- Hess, P.; Abadie, E.; Hervé, F.; Berteaux, T.; Séchet, V.; Aráoz, R.; Molgó, J.; Zakarian, A.; Sibat, M.; Rundberget, T.; et al. Pinnatoxin G Is Responsible for Atypical Toxicity in Mussels (Mytilus Galloprovincialis) and Clams (Venerupis Decussata) from Ingril, a French Mediterranean Lagoon. Toxicon 2013, 75, 16–26. [Google Scholar] [CrossRef]
- Lee, J.S.; Igarashi, T.; Fraga, S.; Dahl, E.; Hovgaard, P.; Yasumoto, T. Determination of Diarrhetic Shellfish Toxins in Various Dinoflagellate Species. J. Appl. Phycol. 1989, 1, 147–152. [Google Scholar] [CrossRef]
- Tillmann, U.; Elbrächter, M.; Krock, B.; John, U.; Cembella, A. Azadinium Spinosum Gen. et Sp. Nov. (Dinophyceae) Identified as a Primary Producer of Azaspiracid Toxins. Eur. J. Phycol. 2009, 44, 63–79. [Google Scholar] [CrossRef]
- Twiner, M.J.; Rehmann, N.; Hess, P.; Doucette, G.J. Azaspiracid Shellfish Poisoning: A Review on the Chemistry, Ecology, and Toxicology with an Emphasis on Human Health Impacts. Mar. Drugs 2008, 6, 39–72. [Google Scholar] [CrossRef]
- García, C.; Truan, D.; Lagos, M.; Santelices, J.P.; Díaz, J.C.; Lagos, N. Metabolic Transformation of Dinophysistoxin-3 into Dinophysistoxin-1 Causes Human Intoxication by Consumption of O-Acyl-Derivatives Dinophysistoxins Contaminated Shellfish. J. Toxicol. Sci. 2005, 30, 287–296. [Google Scholar] [CrossRef]
- James, K.J.; Sáez, M.J.F.; Furey, A.; Lehane, M. Azaspiracid Poisoning, the Food-Borne Illness Associated with Shellfish Consumption. Food Addit. Contam. 2004, 21, 879–892. [Google Scholar] [CrossRef]
- James, K.J.; Lehane, M.; Moroney, C.; Fernandez-Puente, P.; Satake, M.; Yasumoto, T.; Furey, A. Azaspiracid Shellfish Poisoning: Unusual Toxin Dynamics in Shellfish and the Increased Risk of Acute Human Intoxications. Food Addit. Contam. 2002, 19, 555–561. [Google Scholar] [CrossRef]
- McCarron, P.; Emteborg, H.; Nulty, C.; Rundberget, T.; Loader, J.I.; Teipel, K.; Miles, C.O.; Quilliam, M.A.; Hess, P. A Mussel Tissue Certified Reference Material for Multiple Phycotoxins. Part 1: Design and Preparation. Anal. Bioanal. Chem. 2011, 400, 821–833. [Google Scholar] [CrossRef] [PubMed]
- McCarron, P.; Giddings, S.D.; Reeves, K.L.; Hess, P.; Quilliam, M.A. A Mussel (Mytilus Edulis) Tissue Certified Reference Material for the Marine Biotoxins Azaspiracids. Anal. Bioanal. Chem. 2015, 407, 2985–2996. [Google Scholar] [CrossRef] [PubMed]
- Beach, D.G.; Crain, S.; Lewis, N.; le Blanc, P.; Hardstaff, W.R.; Perez, R.A.; Giddings, S.D.; Martinez-Farina, C.F.; Stefanova, R.; Burton, I.W.; et al. Development of Certified Reference Materials for Diarrhetic Shellfish Poisoning Toxins, Part 1: Calibration Solutions. J. AOAC Int. 2016, 99, 1151–1162. [Google Scholar] [CrossRef] [PubMed]
- EURLMB. EU-Harmonised Standard Operating Procedure for Determination of Lipophilic Marine Biotoxins in Molluscs by LC–MS/MS, 5th ed.; EURLMB: Vigo, Spain, 2015.
- Liu, L.; Guo, F.; Crain, S.; Quilliam, M.A.; Wang, X.; Rein, K.S. The Structures of Three Metabolites of the Algal Hepatotoxin Okadaic Acid Produced by Oxidation with Human Cytochrome P450. Bioorg. Med. Chem. 2012, 20, 3742–3745. [Google Scholar] [CrossRef]
- Guo, F.; An, T.; Rein, K.S. The Algal Hepatoxoxin Okadaic Acid Is a Substrate for Human Cytochromes CYP3A4 and CYP3A5. Toxicon 2010, 55, 325–332. [Google Scholar] [CrossRef]
- Kolrep, F.; Hessel, S.; These, A.; Ehlers, A.; Rein, K.; Lampen, A. Differences in Metabolism of the Marine Biotoxin Okadaic Acid by Human and Rat Cytochrome P450 Monooxygenases. Arch. Toxicol. 2016, 90, 2025–2036. [Google Scholar] [CrossRef]
- Kolrep, F.; Rein, K.; Lampen, A.; Hessel-Pras, S. Metabolism of Okadaic Acid by NADPH-Dependent Enzymes Present in Human or Rat Liver S9 Fractions Results in Different Toxic Effects. Toxicol. Vitr. 2017, 42, 161–170. [Google Scholar] [CrossRef]
- Cembella, A.D.; Lewis, N.I.; Quilliam, M.A. The Marine Dinoflagellate Alexandrium Ostenfeldii (Dinophyceae) as the Causative Organism of Spirolide Shellfish Toxins. Phycologia 2000, 39, 67–74. [Google Scholar] [CrossRef]
- Hu, T.; Burton, I.W.; Cembella, A.D.; Curtis, J.M.; Quilliam, M.A.; Walter, J.A.; Wright, J.L.C. Characterization of Spirolides A, C, and 13-Desmethyl C, New Marine Toxins Isolated from Toxic Plankton and Contaminated Shellfish. J. Nat. Prod. 2001, 64, 308–312. [Google Scholar] [CrossRef]
- Aasen, J.; MacKinnon, S.L.; LeBlanc, P.; Walter, J.A.; Hovgaard, P.; Aune, T.; Quilliam, M.A. Detection and Identification of Spirolides in Norwegian Shellfish and Plankton. Chem. Res. Toxicol. 2005, 18, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Sleno, L.; Windust, A.J.; Volmer, D.A. Structural Study of Spirolide Marine Toxins by Mass Spectrometry. Part I. Fragmentation Pathways of 13-Desmethyl Spirolide C by Collision-Induced Dissociation and Infrared Multiphoton Dissociation Mass Spectrometry. Anal. Bioanal. Chem. 2004, 378, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Sleno, L.; Chalmers, M.J.; Volmer, D.A. Structural Study of Spirolide Marine Toxins by Mass Spectrometry. Part II. Mass Spectrometric Characterization of Unknown Spirolides and Related Compounds in a Cultured Phytoplankton Extract. Anal. Bioanal. Chem. 2004, 378, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Munday, R. Toxicology of Cyclic Imines: Gymnodimine, Spirolides, Pinnatoxins, Pteriatoxins, Prorocentrolide, Spiro-Prorocentrimine, and Symbioimines; CRC Press: Boca Raton, FL, USA, 2008. [Google Scholar]
- Hu, T.; Curtis, J.M.; Walter, J.A.; Wright, J.L.C. Characterization of Biologically Inactive Spirolides E and F: Identification of the Spirolide Pharmacophore. Tetrahedron Lett. 1996, 37, 7671–7674. [Google Scholar] [CrossRef]
- Munday, R.; Quilliam, M.A.; LeBlanc, P.; Lewis, N.; Gallant, P.; Sperker, S.A.; Ewart, H.S.; MacKinnon, S.L. Investigations into the Toxicology of Spirolides, a Group of Marine Phycotoxins. Toxins 2012, 4, 1–14. [Google Scholar] [CrossRef]
- Nieva, J.A.; Tebben, J.; Tillmann, U.; Wohlrab, S.; Krock, B. Mass Spectrometry-Based Characterization of New Spirolides from Alexandrium Ostenfeldii (Dinophyceae). Mar. Drugs 2020, 18, 505. [Google Scholar] [CrossRef]
- Yasumoto, T.; Murata, M. Marine Toxins. Chem. Rev. 1993, 93, 1897–1909. [Google Scholar] [CrossRef]
- Watkins, S.M.; Reich, A.; Fleming, L.E.; Hammond, R. Neurotoxic Shellfish Poisoning. Mar. Drugs 2008, 6, 431–455. [Google Scholar] [CrossRef]
- Heil, D.C. Karenia Brevis Monitoring, Management, and Mitigation for Florida Molluscan Shellfish Harvesting Areas. Harmful Algae 2009, 8, 608–610. [Google Scholar] [CrossRef]
- Ishida, H.; Nozawa, A.; Nukaya, H.; Tsuji, K. Comparative Concentrations of Brevetoxins PbTx-2, PbTx-3, BTX-B1 and BTX-B5 in Cockle, Austrovenus Stutchburyi, Greenshell Mussel, Perna Canaliculus, and Pacific Oyster, Crassostrea Gigas, Involved Neurotoxic Shellfish Poisoning in New Zealand. Toxicon 2004, 43, 779–789. [Google Scholar] [CrossRef]
- Wang, W.; Hua, Y.; Wang, G.; Cole, R.B. Characterization of Rat Liver Microsomal and Hepatocytal Metabolites of Brevetoxins by Liquid Chromatography-Electrospray Tandem Mass Spectrometry. Anal. Bioanal. Chem. 2005, 383, 67–75. [Google Scholar] [CrossRef]
- Radwan, F.F.Y.; Ramsdell, J.S. Characterization of in Vitro Oxidative and Conjugative Metabolic Pathways for Brevetoxin (PbTx-2). Toxicol. Sci. 2006, 89, 57–65. [Google Scholar] [CrossRef]
- Guo, F.; An, T.; Rein, K.S. Human Metabolites of Brevetoxin PbTx-2: Identification and Confirmation of Structure. Toxicon 2010, 56, 648. [Google Scholar] [CrossRef] [PubMed]
- Abraham, A.; Plakas, S.M.; Flewelling, L.J.; el Said, K.R.; Jester, E.L.E.; Granade, H.R.; White, K.D.; Dickey, R.W. Biomarkers of Neurotoxic Shellfish Poisoning. Toxicon 2008, 52, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Abraham, A.; Flewelling, L.J.; el Said, K.R.; Odom, W.; Geiger, S.P.; Granholm, A.A.; Jackson, J.T.; Bodager, D. An Occurrence of Neurotoxic Shellfish Poisoning by Consumption of Gastropods Contaminated with Brevetoxins. Toxicon 2021, 191, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Adachi, R.; Nakajima, I. Finding of a Dinoflagellate as a Likely Culprit of Ciguatera. NIPPON SUISAN GAKKAISHI 1977, 43, 1021–1026. [Google Scholar] [CrossRef]
- Litaker, R.W.; Vandersea, M.W.; Faust, M.A.; Kibler, S.R.; Nau, A.W.; Holland, W.C.; Chinain, M.; Holmes, M.J.; Tester, P.A. Global Distribution of Ciguatera Causing Dinoflagellates in the Genus Gambierdiscus. Toxicon 2010, 56, 711–730. [Google Scholar] [CrossRef]
- Murata, M.; Legrand, A.M.; Ishibashi, Y.; Yasumoto, T. Structures of Ciguatoxin and Its Congener. J. Am. Chem. Soc. 1989, 111, 8929–8931. [Google Scholar] [CrossRef]
- Lewis, R.J.; Holmes, M.J. Origin and Transfer of Toxins Involved in Ciguatera. Comp. Biochem. Physiol. Part C Comp. 1993, 106, 615–628. [Google Scholar] [CrossRef]
- Pearn, J. Neurology of Ciguatera. J. Neurol. Neurosurg. Psychiatry 2001, 70, 4–8. [Google Scholar] [CrossRef]
- Kato, T.; Yasumoto, T. Quantification of Representative Ciguatoxins in the Pacific Using Quantitative Nuclear Magnetic Resonance Spectroscopy. Mar. Drugs 2017, 15, 309. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.J.; Vernoux, J.-P.; Brereton, I.M. Structure of Caribbean Ciguatoxin Isolated from Caranx Latus. J. Am. Chem. Soc. 1998, 120, 5914–5920. [Google Scholar] [CrossRef]
- Hamilton, B.; Hurbungs, M.; Vernoux, J.P.; Jones, A.; Lewis, R.J. Isolation and Characterisation of Indian Ocean Ciguatoxin. Toxicon 2002, 40, 685–693. [Google Scholar] [CrossRef]
- Ikehara, T.; Kuniyoshi, K.; Oshiro, N.; Yasumoto, T. Biooxidation of Ciguatoxins Leads to Species-Specific Toxin Profiles. Toxins 2017, 9, 205. [Google Scholar] [CrossRef] [PubMed]
- Yogi, K.; Oshiro, N.; Inafuku, Y.; Hirama, M.; Yasumoto, T. Detailed LC–MS/MS Analysis of Ciguatoxins Revealing Distinct Regional and Species Characteristics in Fish and Causative Alga from the Pacific. Anal. Chem. 2011, 83, 8886–8891. [Google Scholar] [CrossRef]
- Gwinn, J.K.; Uhlig, S.; Ivanova, L.; Fæste, C.K.; Kryuchkov, F.; Robertson, A. In Vitro Glucuronidation of Caribbean Ciguatoxins in Fish: First Report of Conjugative Ciguatoxin Metabolites. Chem. Res. Toxicol. 2021, 34, 1910–1925. [Google Scholar] [CrossRef]
- Lefebvre, K.A.; Bill, B.D.; Erickson, A.; Baugh, K.A.; O’Rourke, L.; Costa, P.R.; Nance, S.; Trainer, V.L. Characterization of Intracellular and Extracellular Saxitoxin Levels in Both Field and Cultured Alexandrium Spp. Samples from Sequim Bay, Washington. Mar. Drugs 2008, 6, 103–116. [Google Scholar] [CrossRef]
- Oshima, Y.; Blackburn, S.I.; Hallegraeff, G.M. Comparative Study on Paralytic Shellfish Toxin Profiles of the Dinoflagellate Gymnodinium Catenatum from Three Different Countries. Mar. Biol. 1993, 116, 471–476. [Google Scholar] [CrossRef]
- Usup, G.; Kulis, D.M.; Anderson, D.M. Growth and Toxin Production of the Toxic Dinoflagellate Pyrodinium bahamense Var. Compressum in Laboratory Cultures. Nat. Toxins 1994, 2, 254–262. [Google Scholar] [CrossRef]
- Alexander, J.; Benford, D.; Cockburn, A.; Cravedi, J.-P.; Dogliotti, E.; di Domenico, A.; Luisa Fernández-Cruz, M.; Fink-Gremmels, J.; Fürst, P.; Galli, C.; et al. Marine Biotoxins in Shellfish—Saxitoxin Group. EFSA J. 2009, 7, 1019. [Google Scholar] [CrossRef]
- de Carvalho, M.; Jacinto, J.; Ramos, N.; de Oliveira, V.; Pinho e Melo, T.; de Sá, J. Paralytic Shellfish Poisoning: Clinical and Electrophysiological Observations. J. Neurol. 1998, 245, 551–554. [Google Scholar] [CrossRef]
- Dell’Aversano, C.; Walter, J.A.; Burton, I.W.; Stirling, D.J.; Fattorusso, E.; Quilliam, M.A. Isolation and Structure Elucidation of New and Unusual Saxitoxin Analogs from Mussels. J. Nat. Prod. 2008, 71, 1518–1523. [Google Scholar] [CrossRef] [PubMed]
- García, C.; Rodriguez-Navarro, A.; Díaz, J.C.; Torres, R.; Lagos, N. Evidence of in Vitro Glucuronidation and Enzymatic Transformation of Paralytic Shellfish Toxins by Healthy Human Liver Microsomes Fraction. Toxicon 2009, 53, 206–213. [Google Scholar] [CrossRef] [PubMed]
- García, C.; Barriga, A.; Díaz, J.C.; Lagos, M.; Lagos, N. Route of Metabolization and Detoxication of Paralytic Shellfish Toxins in Humans. Toxicon 2010, 55, 135–144. [Google Scholar] [CrossRef] [PubMed]
| Toxins | Syndrome | Parent Compound |
|---|---|---|
| Lipophilic | Diarrhetic Shellfish Poisoning (DSP) | Okadaic acid (OA) |
| - | Yessotoxins (YTXs) | |
| Azaspiracid Poisoning (AZP) | Azaspiracids (AZAs) | |
| - | Cyclic Imines (CIs) | |
| Ciguatera Poisoning (CP) | Ciguatoxins (CTXs) | |
| Neurotoxic Shellfish Poisoning (NSP) | Brevetoxins (PbTxs) | |
| Hydrophilic | Amnesic Shellfish Poisoning (ASP) | Domoic acid (DA) |
| Paralytic Shellfish Poisoning (PSP) | Saxitoxin (STX) | |
| Pufferfish Poisoning (PFP) | Tetrodotoxin (TTX) |
| Toxin Molecular Formula | Q1/Q3 (m/z) | In Vitro Incubation | Metabolite | Q1/Q3 (m/z) | Reference | |
|---|---|---|---|---|---|---|
| OA C44H68O13 | [M−H]− 803/255 | Human | CYP3A4 and CYP3A5 | +16 uma (+O): 36-hydroxy-OA, | [M−H]− 819/255 | [61] |
| +16 uma (+O): 43-hydroxy-OA | [M−H]− 819/271 | |||||
| +14 uma (+O/−H2): 43-oxo-OA | [M−H]− 817/269 | |||||
| CYP3A4 and CYP3A5 | +16 uma (+O): C44H68O14; M1, M2 and M3 | [M−H]− 819/255 [M−H]− 819/255 [M−H]− 819/271 | [62] | |||
| +14 uma (+O/–H2): C44H66O14; M4, M6 | [M−H]− 817/269 [M−H]− 817/255 | |||||
| CYP3A5 | +14 uma (+O/−H2): C44H66O14; M5 | [M−H]− 817/255 | ||||
| +32 uma (+2×O): C44H68O15; M7 | [M−H]− 835/255 | |||||
| S9 mix | +16 uma (+O): C44H68O14; M1, M2, M3 | [M−H]− 819/255 [M−H]− 819/255 [M−H]− 819/271 | [63] | |||
| +14 uma (+O/−H2): C44H66O14; M4 | [M−H]− 817/269 | |||||
| Rat | Cyp3a1 | +16 uma (+O): C44H68O14; M1, M2 and M3 | [M−H]– 819/255 [M−H]– 819/255 [M−H]– 819/271 | [62] | ||
| CYP3A2 | +16 uma (+O): C44H68O14; M3 | [M−H]– 819/271 | ||||
| S9 mix | +16 uma (+O): C44H68O14; M1, M2, M3 | [M−H]− 819/255 [M−H]− 819/255 [M−H]− 819/271 | [63] | |||
| +14 uma (+O/−H2): C44H66O14; M4 | [M−H]− 817/269 | |||||
| +16 uma (+O): C44H68O14 | [M−H]− 819/271 [M−H]− 819/255 | [37] | ||||
| +14 uma (+O/−H2): C44H66O14 | [M−H]− 817/269 | |||||
| DTX1 C45H70O13 | [M−H]− 817/255 | Rat | S9 mix | +16 uma (+O): C45H70O14 | [M−H]− 833/271 [M−H]− 833/255 | [37] |
| +14 uma (+O/−H2): C45H68O14 | [M−H]− 831/269 | |||||
| DTX2 C44H68O13 | [M−H]− 803/255 | +16 uma (+O): C44H68O14 | [M−H]− 819/271 [M−H]− 819/255 | [37] | ||
| YTX C55H82O21S2 | [M−H]− 1141/106 | +16 uma (+O): C55H82O22S2 | [M−H]− 1157/1077 | [37] | ||
| AZA1 C47H71NO12 | [M+H]+ 842/824 | +176 uma (+C6H8O6): C53H79NO18 | [M+H]+ 1018/848 | [37] | ||
| +16 uma (+O): C47H71NO13 | [M+H]+ 858/824 | |||||
| +32 uma (2×O): C47H71NO14 | [M+H]+ 874/856 | |||||
| +48 uma (3×O): C47H71NO15 | [M+H]+ 890/872 | |||||
| −2 uma (−H2): C47H69NO12 | [M+H]+ 840/822 | |||||
| PTX2 C47H70O14 | [M+NH4]+ 876/823 | +16 uma (+O): C47H70O15 | [M+NH4]+ 892/839 | [37] | ||
| +32 uma (2×O): C47H70O16 | [M+NH4]+ 908/855 | |||||
| +48 uma (3×O): C47H70O17 | [M+NH4]+ 924/871 | |||||
| Toxin Molecular Formula | m/z [M+H]+ | Metabolite | m/z [M+H]+ |
|---|---|---|---|
| SPX1 C42H61NO7 | 692.4521 | +14 uma (+O/−H2): C42H59NO8; M1 | 706.4313 |
| +14 uma (+O/−H2): C42H59NO8; M2 | 706.4313 | ||
| +16 uma (+O): C42H61NO8; 13,19-desmethyl-19-hydroxymethyl spirolide C; M3 | 708.4470 | ||
| +16 uma (+O): C42H61NO8; 13-desmethyl-17-hydroxy spirolide C; M4 | 708.4470 | ||
| +18 uma (−CH2 + 2 × O): C41H59NO9; M5 | 710.4263 | ||
| +18 uma (−CH2 + 2 × O): C41H59NO9; M6 | 710.4263 | ||
| +30 uma (−2 × H + 2 × O): C42H59NO9; 13,19-desmethyl-19-carboxy spirolide C; M7 | 722.4263 | ||
| +32 uma (+2 × O): C42H61NO9; M8 | 724.4419 | ||
| +32 uma (+2 × O): C42H61NO9; M9 | 724.4419 |
| Toxin Molecular Formula | m/z | In Vitro Incubation | Metabolite | m/z | Reference |
|---|---|---|---|---|---|
| PbTx-1 C49H70O13 | [M+H]+ 867 | Rat liver hepatocytes | +34 uma; C49H72O15; PbTx-1-M1a/M1b | [M+H]+ 901 | [77] |
| +18 uma; C49H72O14; PbTx-1-M2 | [M+H]+ 885 [M–H]− 883 | ||||
| PbTx-2 C50H70O14 | [M+H]+ 895 | Rat liver microsomes | +18 uma; C50H72O15; PbTx-2-M1 | [M+H]+ 913 [M−H]– 911 | |
| +2 uma; C50H72O14; PbTx-2-M2 (PbTx-3) | [M+H]+ 897 | ||||
| Rat CYP1A2 and CYP3A1 | +2 uma; C50H72O14; PbTx-3 | [M+H]+ 897 | [78] | ||
| +4 uma; C50H74O14; PbTX-9 | [M+H]+ 899 | ||||
| +34 uma; C50H72O16; 27,28-diol-PbTx-2 | [M+H]+ 929 | ||||
| +16 uma; C50H70O15; BTX-B5 | [M+H]+ 911 [M−H]− 909 | ||||
| Rat hepatocytes | +16 uma; C50H70O15; PbTx-6 | [M+H]+ 911 | |||
| +18 uma; C50H72O15; 27,28-epoxy-PbTx3 | [M+H]+ 913 | ||||
| +20 uma; C50H74O15; 1-carboxylic-5-hydroxyl-PbTx-3 | [M+H]+ 915 [M–H]− 913 | ||||
| +22 uma; C50H76O15; 1-carboxylic-5-hydroxyl-PbTx-9 | [M+H]+ 917 [M−H]− 915 | ||||
| +36 uma; C50H74O16; 27,28-diol-PbTx-3 | [M+H]+ 931 | ||||
| Human liver microsomes | +16 uma; C50H70O15; BTX-B5 | [M+H]+ 911 [M–H]− 909 | [79] | ||
| +4 uma; C50H74O14; PbTX-9 | [M+H]+ 899 | ||||
| +18 uma; C50H72O15; 41,43-dihydro-BTX-B5 | [M+H]+ 913 | ||||
| +2 uma; C50H72O14; 41,43-dihydro-PbTx-2 | [M+H]+ 897 |
| Urine PbTxs Metabolite | m/z | References | |
|---|---|---|---|
| Major metabolites | PbTx-3, C50H72O14 | [M+H]+: m/z 897 | [80,81] |
| methylsulfoxy PbTx-3, C51H76O15S | [M+H]+: m/z 961 | [80] | |
| reduced BTX-B5, C50H72O15 | [M+H]+: m/z 913 | [80,81] | |
| 27-epoxy PbTx-3, C50H72O15 | [M+H]+: m/z 913 | [80,81] | |
| Minor metabolites | opened A-ring derivative of PbTx-3, C50H74O15 | [M+H]+: m/z 915 | [80,81] |
| C49H72O15 | [M+H]+: m/z 901 | [80] | |
| C49H74O14 | [M+H]+: m/z 887 | [80] | |
| Toxin Molecular Formula | Q1/Q3 (m/z) | Metabolite | Q1/Q3 (m/z) |
|---|---|---|---|
| CTX4A C60H84O16 | [M+Na]+ 1083.6/1083.6 | 52-epi-54-deoxyCTX1B | [M+Na]+ 1117.6/1117.6 |
| CTX4B C60H84O16 | [M+Na]+ 1083.6/1083.6 | 54-deoxyCTX1B | [M+Na]+ 1117.6/1117.6 |
| CTX1B | [M+Na]+ 1133.6/1133.6 | ||
| CTX3C C57H82O16 | [M+Na]+ 1045.6/1045.6 | 2-hydroxyCTX3C | [M+Na]+ 1063.6/1063.6 |
| 2,3-dihydroxyCTX3C | [M+Na]+ 1079.6/1079.6 |
| Toxin Molecular Formula | Q1/Q3 (m/z) | Metabolite | Q1/Q3 (m/z) |
|---|---|---|---|
| STX C10H17N7O4 | [M−H]− 298/99 [M−H]− 298/137 [M−H]− 298/160 | neoSTX | [M−H]− 314/99 [M−H]− 314/175 [M−H]− 314/603 [M−H]− 314/619 [M−H]− 314/625 |
| Gluc-STX | [M−H]− 475/163 [M−H]− 475/288 [M−H]− 475/316 [M−H]− 475/388 [M−H]− 475/410 [M−H]− 475/418 | ||
| neoSTX C10H17N7O5 | [M−H]− 314/99 [M−H]− 314/175 [M−H]− 314/603 [M−H]− 314/619 [M−H]− 314/625 | GTX4/GTX1 | [M−H]− 410/210 [M−H]− 410/254 [M−H]− 410/323 |
| Gluc-neoSTX | [M−H]− 492/226 [M−H]− 492/342 [M−H]− 492/379 [M−H]− 492/418 [M−H]− 492/438 | ||
| GTX1 C10H17N7O9S | [M−H]− 410/210 [M−H]− 410/254 [M−H]− 410/323 | Gluc-GTX1 | [M−H]− 588/255 [M−H]− 588/323 [M−H]− 588/403 |
| GTX2 C10H17N7O8S | [M−H]− 394/297 [M−H]− 394/311 [M−H]− 394/365 | GTX4/GTX1 | [M−H]− 410/210 [M−H]− 410/254 [M−H]− 410/323 |
| Gluc-GTX2 | [M−H]− 570/194 [M−H]− 570/322 [M−H]− 570/395 | ||
| GTX3 C10H17N7O8S | [M−H]− 394/297 [M−H]− 394/311 [M−H]− 394/365 | GTX4/GTX1 | [M−H]− 410/210 [M−H]− 410/254 [M−H]− 410/323 |
| Gluc-GTX3 | [M−H]− 570/194 [M−H]− 570/322 [M−H]− 570/395 | ||
| GTX4 C10H17N7O9S | [M−H]− 410/210 [M−H]− 410/254 [M−H]− 410/323 | Gluc-GTX4 | [M−H]− 588/255 [M−H]− 588/323 [M−H]− 588/403 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Estevez, P.; Gago-Martinez, A. Contribution of Mass Spectrometry to the Advances in Risk Characterization of Marine Biotoxins: Towards the Characterization of Metabolites Implied in Human Intoxications. Toxins 2023, 15, 103. https://doi.org/10.3390/toxins15020103
Estevez P, Gago-Martinez A. Contribution of Mass Spectrometry to the Advances in Risk Characterization of Marine Biotoxins: Towards the Characterization of Metabolites Implied in Human Intoxications. Toxins. 2023; 15(2):103. https://doi.org/10.3390/toxins15020103
Chicago/Turabian StyleEstevez, Pablo, and Ana Gago-Martinez. 2023. "Contribution of Mass Spectrometry to the Advances in Risk Characterization of Marine Biotoxins: Towards the Characterization of Metabolites Implied in Human Intoxications" Toxins 15, no. 2: 103. https://doi.org/10.3390/toxins15020103
APA StyleEstevez, P., & Gago-Martinez, A. (2023). Contribution of Mass Spectrometry to the Advances in Risk Characterization of Marine Biotoxins: Towards the Characterization of Metabolites Implied in Human Intoxications. Toxins, 15(2), 103. https://doi.org/10.3390/toxins15020103






