Reduced Expression of Metallothionein-I/II in Renal Proximal Tubules Is Associated with Advanced Chronic Kidney Disease
Abstract
:1. Introduction
2. Results
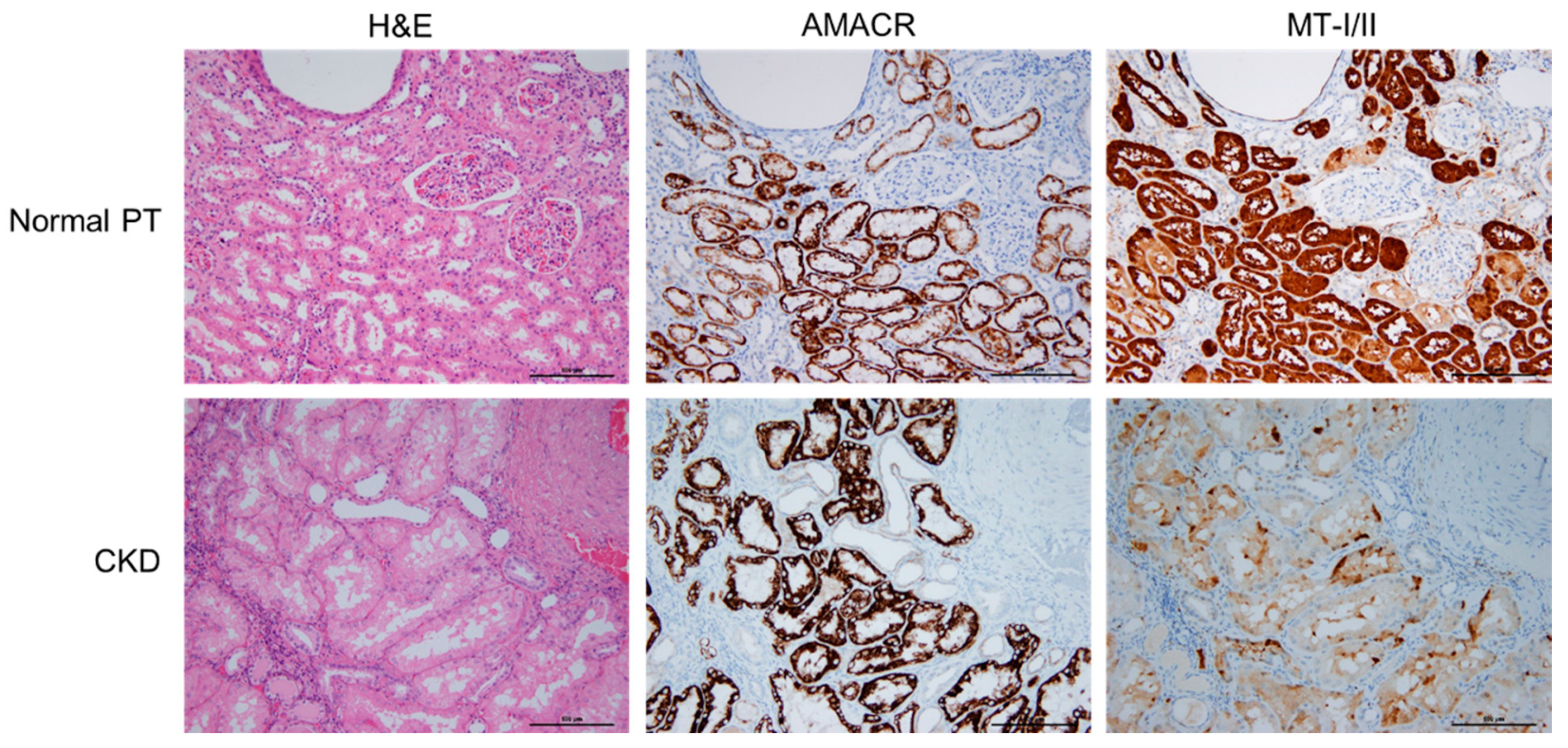
2.1. Expression of MT-I/II in Renal Tissues of Human CKD and Its Clinical Characteristics
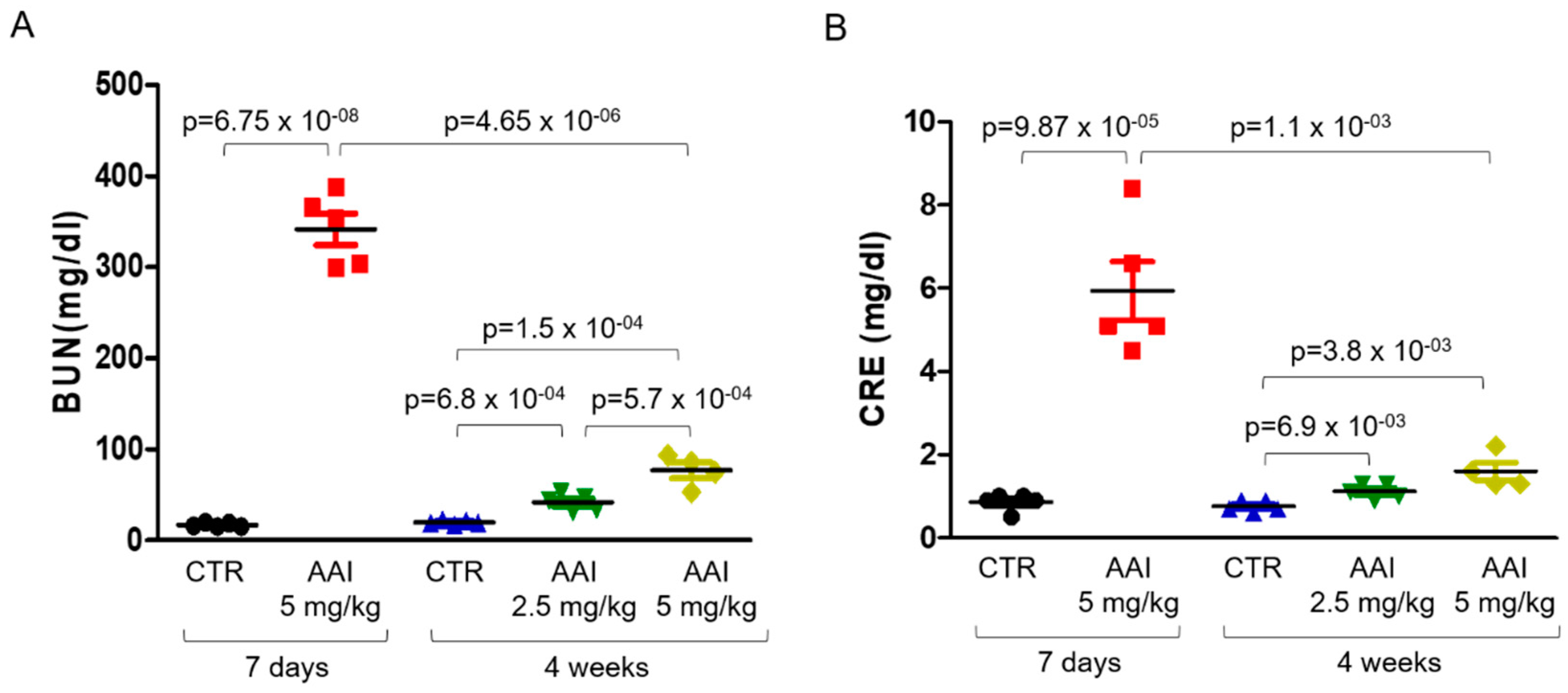
2.2. Expression of MT-I/II in AAI-Induced Nephropathy (AAN) Mouse Model
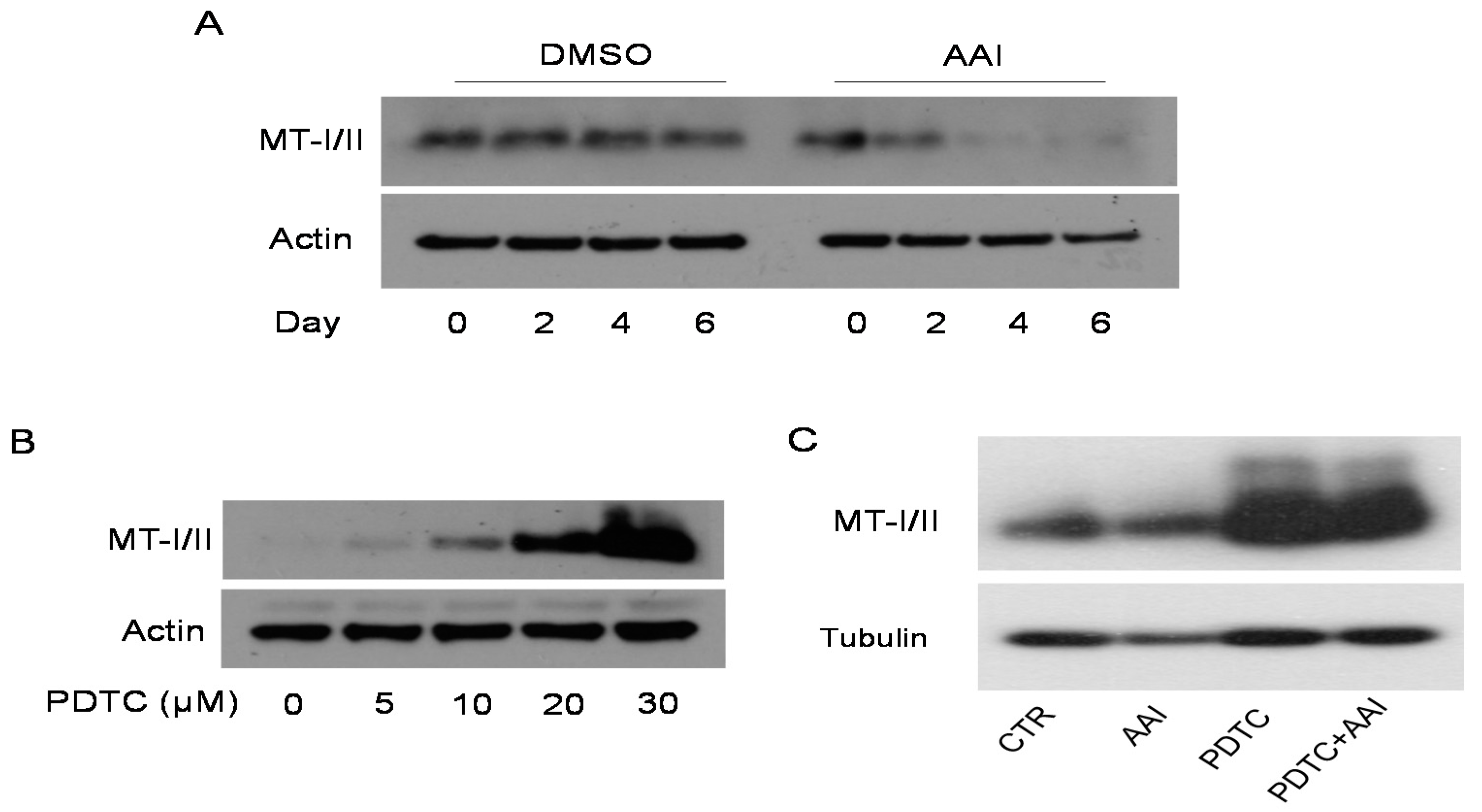
2.3. PDTC Restored AAI-Reduced MT-I/II Expression in HK2 Cells
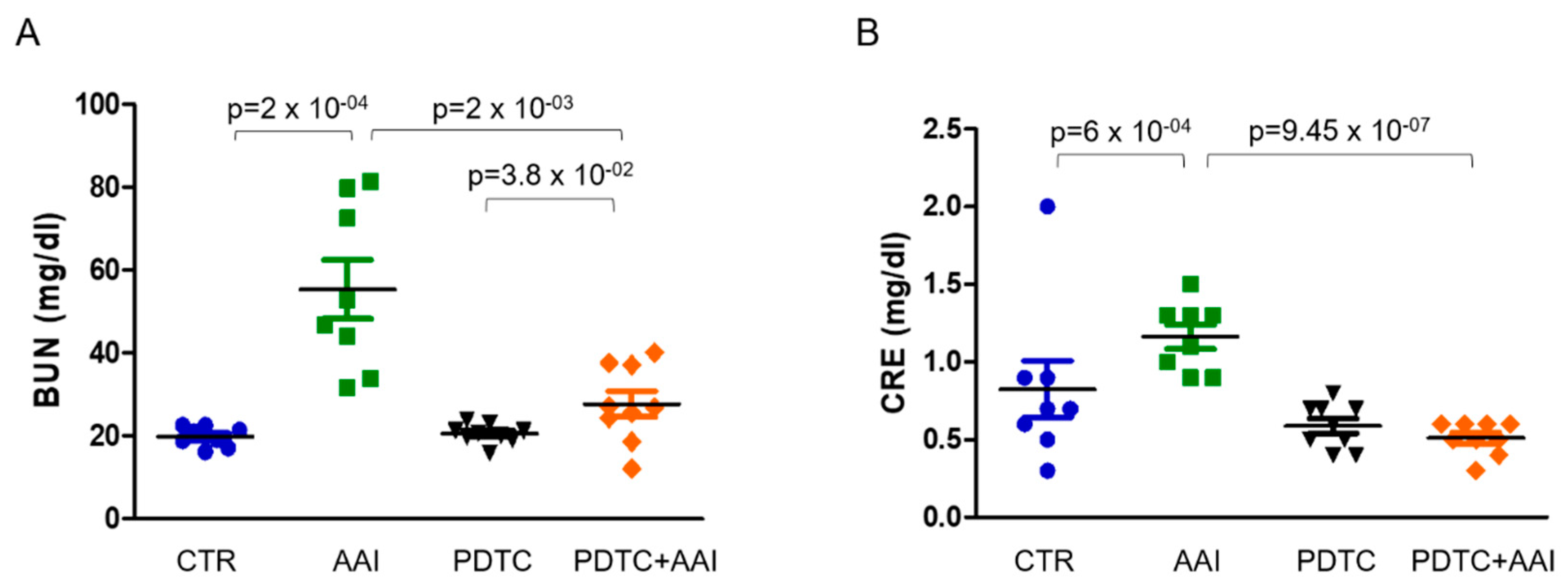
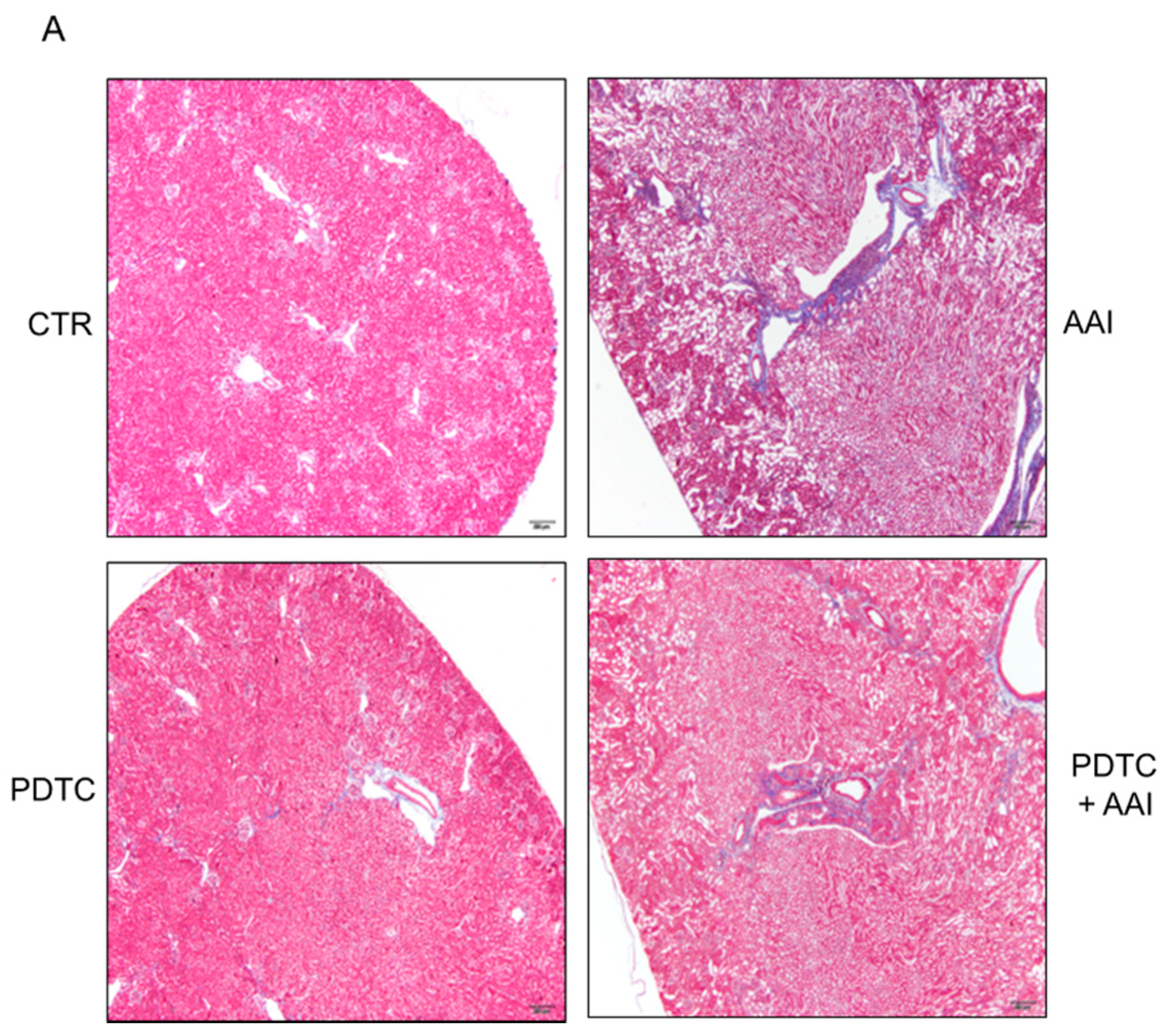
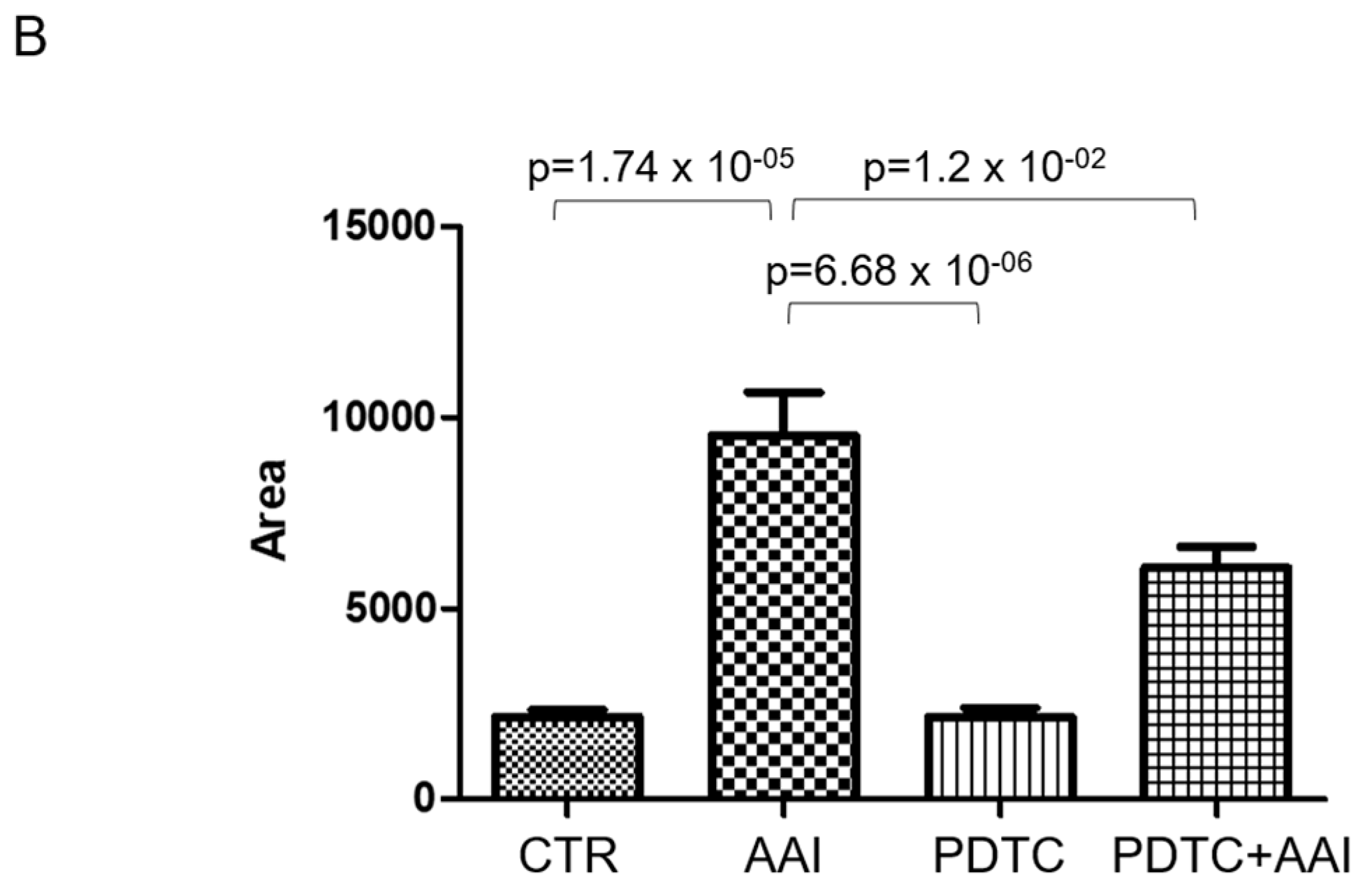
2.4. PDTC Attenuated Kidney Injury in AAN Mice
3. Discussion
4. Materials and Methods
4.1. Patients and Specimens
4.2. Immunohistochemical Stain of Human Kidney Tissues
4.3. Cell Culture and Reagents
4.4. Western Blot Analysis
4.5. Experimental Animals
4.6. Immunohistochemical Analysis and Measurement of Renal Fibrosis
4.7. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, L.; Scarpellini, A.; Funck, M.; Verderio, E.A.; Johnson, T.S. Development of a Chronic Kidney Disease Model in C57BL/6 Mice with Relevance to Human Pathology. Nephron Extra 2013, 3, 12–29. [Google Scholar] [CrossRef] [PubMed]
- Rabe, M.; Schaefer, F. Non-Transgenic Mouse Models of Kidney Disease. Nephron 2016, 133, 53–61. [Google Scholar] [CrossRef]
- Debelle, F.D.; Vanherweghem, J.-L.; Nortier, J.L. Aristolochic acid nephropathy: A worldwide problem. Kidney Int. 2008, 74, 158–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, B.; Xie, Y.; Guo, M.; Rosner, M.H.; Yang, H.; Ronco, C. Nephrotoxicity and Chinese herbal medicine. Clin. J. Am. Soc. Nephrol. 2018, 13, 1605–1611. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.-F.; Hsieh, C.-Y.; Lu, K.-C.; Chen, Y.-W.; Liang, S.-S.; Lin, C.-C.; Hung, C.-F.; Liou, J.-C.; Wu, M.-S. Therapeutic Targeting of Aristolochic Acid Induced Uremic Toxin Retention, SMAD 2/3 and JNK/ERK Pathways in Tubulointerstitial Fibrosis: Nephroprotective Role of Propolis in Chronic Kidney Disease. Toxins 2020, 12, 364. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Leem, J.; Jeon, E.J. Protective Effects of Melatonin Against Aristolochic Acid-Induced Nephropathy in Mice. Bio-Molecules 2019, 10, 11. [Google Scholar] [CrossRef] [Green Version]
- Nortier, J.L.; Deschodt-Lanckman, M.M.; Simon, S.; Thielemans, N.O.; de Prez, E.G.; Depierreux, M.F.; Tielemans, C.L.; Richard, C.; Lauwerys, R.R.; Bernard, A.M.; et al. Proximal tubular injury in Chinese herbs nephropathy: Monitoring by neutral endopeptidase enzymuria. Kidney Int. 1997, 51, 288–293. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; Jiang, N.; Han, Y.; Yang, M.; Gao, P.; Xiong, X.; Xiong, S.; Zeng, L.; Xiao, Y.; Wei, L.; et al. Aristolochic acid induces renal fibrosis by arresting proximal tubular cells in G2/M phase mediated by HIF-1α. FASEB J. 2020, 34, 12599–12614. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Feng, J.; Dai, C.; Sun, L.; Jin, T.; Ma, J.; Wang, L. Role of Peritubular Capillary Loss and Hypoxia in Progressive Tubulointerstitial Fibrosis in a Rat Model of Aristolochic Acid Nephropathy. Am. J. Nephrol. 2006, 26, 363–371. [Google Scholar] [CrossRef]
- Guo, Y.; Hu, M.; Ma, J.; Chinnathambi, A.; Alharbi, S.A.; Shair, O.H.M.; Ge, P. Protective effect of panaxydol against repeated administration of aristolochic acid on renal function and lipid peroxidation products via activating Keap1-Nrf2/ARE pathway in rat kidney. J. Biochem. Mol. Toxicol. 2021, 35, e22619. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Li, X.; Wang, H. Possible mechanisms explaining the tendency towards interstitial fibrosis in aristolochic acid-induced acute tubular necrosis. Nephrol. Dial. Transplant. 2006, 22, 445–456. [Google Scholar] [CrossRef]
- Chiaverini, N.; De Ley, M. Protective effect of metallothionein on oxidative stress-induced DNA damage. Free. Radic. Res. 2010, 44, 605–613. [Google Scholar] [CrossRef]
- Chmielewska, M.; Symonowicz, K.; Pula, B.; Owczarek, T.; Podhorska-Okolow, M.; Ugorski, M.; Dziegiel, P. Expression of metallothioneins I and II in kidney of doxorubicin-treated rats. Exp. Toxicol. Pathol. 2015, 67, 297–303. [Google Scholar] [CrossRef]
- Haq, F. Signaling events for metallothionein induction. Mutat. Res. Mol. Mech. Mutagen. 2003, 533, 211–226. [Google Scholar] [CrossRef] [PubMed]
- Thirumoorthy, N.; Sunder, A.S.; Kumar, K.M.; Kumar, M.S.; Ganesh, G.; Chatterjee, M. A Review of Metallothionein Isoforms and their Role in Pathophysiology. World J. Surg. Oncol. 2011, 9, 54. [Google Scholar] [CrossRef] [Green Version]
- Bauer, R. Metallothionein: A new soldier in the fight against chronic renal hypoxia? Kidney Int. 2009, 75, 257–259. [Google Scholar] [CrossRef] [Green Version]
- Ling, X.-B.; Wei, H.-W.; Wang, J.; Kong, Y.-Q.; Wu, Y.-Y.; Guo, J.-L.; Li, T.-F.; Li, J.-K. Mammalian Metallothionein-2A and Oxidative Stress. Int. J. Mol. Sci. 2016, 17, 1483. [Google Scholar] [CrossRef] [PubMed]
- Vašák, M. Advances in metallothionein structure and functions. J. Trace Elements Med. Biol. 2005, 19, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Alscher, D.M.; Biegger, D.; Mettang, T.; Dunst, R.; Wolken, D.; Kuhlmann, U.; Fritz, P. Peritoneal metallothionein content in patients with end-stage renal disease on or not on peritoneal dialysis. Perit. Dial. Int. 2001, 21, 92–94. [Google Scholar] [CrossRef]
- Subramanian Vignesh, K.; Deepe, G.S., Jr. Metallothioneins: Emerging Modulators in Immunity and Infection. Int. J. Mol. Sci. 2017, 18, 2197. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, S. Positive and negative regulators of the metallothionein gene (Review). Mol. Med. Rep. 2012, 12, 795–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kojima, I.; Tanaka, T.; Inagi, R.; Nishi, H.; Aburatani, H.; Kato, H.; Miyata, T.; Fujita, T.; Nangaku, M. Metallothionein is upregulated by hypoxia and stabilizes hypoxia-inducible factor in the kidney. Kidney Int. 2009, 75, 268–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, T.; Itano, Y.; Noji, S.; Matsumoto, K.; Taga, N.; Mizukawa, S.; Toda, N.; Matsumi, M.; Morita, K.; Hirakawa, M. Induction of renal metallothionein in rats with ischemic renal failure. Res. Commun. Mol. Pathol. Pharmacol. 2001, 110, 147–160. [Google Scholar] [PubMed]
- Wu, H.; Zhou, S.; Kong, L.; Chen, J.; Feng, W.; Cai, J.; Miao, L.; Tan, Y. Metallothionein deletion exacerbates intermittent hypoxia-induced renal injury in mice. Toxicol. Lett. 2015, 232, 340–348. [Google Scholar] [CrossRef]
- Wu, Y.-J.; Ko, B.-S.; Liang, S.-M.; Lu, Y.-J.; Jan, Y.-J.; Jiang, S.-S.; Shyue, S.-K.; Chen, L.; Liou, J.-Y. ZNF479 downregulates metallothionein-1 expression by regulating ASH2L and DNMT1 in hepatocellular carcinoma. Cell Death Dis. 2019, 10, 408. [Google Scholar] [CrossRef] [Green Version]
- Raudenska, M.; Dvorakova, V.; Pacal, L.; Chalasova, K.; Kratochvilova, M.; Gumulec, J.; Ruttkay-Nedecky, B.; Zitka, O.; Kankova, K.; Adam, V.; et al. Levels of heavy metals and their binding protein metallothionein in type 2 diabetics with kidney disease. J. Biochem. Mol. Toxicol. 2017, 31, e21891. [Google Scholar] [CrossRef]
- Ljubojević, M.; Orct, T.; Micek, V.; Karaica, D.; Jurasović, J.; Breljak, D.; Madunić, I.V.; Rašić, D.; Jovanović, I.N.; Peraica, M.; et al. Sex-dependent expression of metallothioneins MT1 and MT2 and concentrations of trace elements in rat liver and kidney tissues: Effect of gonadectomy. J. Trace Elements Med. Biol. 2019, 53, 98–108. [Google Scholar] [CrossRef]
- Yang, C.-L.; Du, X.-H.; Zou, W.-Z.; Chen, W. Protective Effect of Zinc-Induced Metallothionein Synthesis on Gentamicin Nephrotoxicity in Rats. Ren. Fail. 1991, 13, 227–232. [Google Scholar] [CrossRef]
- Moon, S.-K.; Jung, S.-Y.; Choi, Y.-H.; Lee, Y.-C.; Patterson, C.; Kim, C.-H. PDTC, metal chelating compound, induces G1 phase cell cycle arrest in vascular smooth muscle cells through inducing p21Cip1 expression: Involvement of p38 mitogen activated protein kinase. J. Cell. Physiol. 2003, 198, 310–323. [Google Scholar] [CrossRef]
- Haddad, J.J.E.; Olver, R.E.; Land, S. Antioxidant/Pro-oxidant Equilibrium Regulates HIF-1α and NF-κB Redox Sensitivity. J. Biol. Chem. 2000, 275, 21130–21139. [Google Scholar] [CrossRef] [Green Version]
- Schmitt, A.; Brändle, A.-L.; Herzog, P.; Röchner, F.; Fragasso, A.; Munz, B. Effects of the anti-oxidant PDTC in combination with a single bout of treadmill running on murine skeletal muscle. Redox Rep. 2020, 25, 70–79. [Google Scholar] [CrossRef]
- Zhu, B.-Z.; Carr, A.C.; Frei, B. Pyrrolidine dithiocarbamate is a potent antioxidant against hypochlorous acid-induced protein damage. FEBS Lett. 2002, 532, 80–84. [Google Scholar] [CrossRef] [Green Version]
- Barnes, D.M.; Harris, W.H.; Smith, P.; Millis, R.R.; Rubens, R.D. Immunohistochemical determination of oestrogen receptor: Comparison of different methods of assessment of staining and correlation with clinical outcome of breast cancer patients. Br. J. Cancer 1996, 74, 1445–1451. [Google Scholar] [CrossRef]
- Chang, G.-C.; Liu, K.-J.; Hsieh, C.-L.; Hu, T.-S.; Charoenfuprasert, S.; Liu, H.-K.; Luh, K.-T.; Hsu, L.-H.; Wu, C.-W.; Ting, C.-C.; et al. Identification of α-Enolase as an Autoantigen in Lung Cancer: Its Overexpression Is Associated with Clinical Outcomes. Clin. Cancer Res. 2006, 12, 5746–5754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jan, Y.-J.; Ko, B.-S.; Hsu, C.; Chang, T.-C.; Chen, S.-C.; Wang, J.; Liou, J.-Y. Overexpressed focal adhesion kinase predicts a higher incidence of extrahepatic metastasis and worse survival in hepatocellular carcinoma. Hum. Pathol. 2009, 40, 1384–1390. [Google Scholar] [CrossRef] [PubMed]
- Ko, B.-S.; Chang, T.-C.; Hsu, C.; Chen, Y.-C.; Shen, T.-L.; Chen, S.-C.; Wang, J.; Wu, K.K.; Jan, Y.-J.; Liou, J.-Y. Overexpression of 14-3-3? predicts tumour metastasis and poor survival in hepatocellular carcinoma. Histopathology 2011, 58, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.-A.; Jan, Y.-J.; Ko, B.-S.; Chen, S.-C.; Liang, S.-M.; Hung, Y.-L.; Hsu, C.; Shen, T.-L.; Lee, Y.-M.; Chen, P.-F.; et al. Increased Expression of 14-3-3β Promotes Tumor Progression and Predicts Extrahepatic Metastasis and Worse Survival in Hepatocellular Carcinoma. Am. J. Pathol. 2011, 179, 2698–2708. [Google Scholar] [CrossRef]
- Liu, T.-A.; Jan, Y.-J.; Ko, B.-S.; Liang, S.-M.; Chen, S.-C.; Wang, J.; Hsu, C.; Wu, Y.-M.; Liou, J.-Y. 14-3-3ε Overexpression Contributes to Epithelial-Mesenchymal Transition of Hepatocellular Carcinoma. PLoS ONE 2013, 8, e57968. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.-J.; Jan, Y.-J.; Ko, B.-S.; Liang, S.-M.; Chen, L.; Wu, C.-C.; Chin, C.-H.; Kuo, C.-C.; Yet, S.-F.; Liou, J.-Y. Expression of Nik-related kinase in smooth muscle cells attenuates vascular inflammation and intimal hyperplasia. Aging 2020, 12, 7511–7533. [Google Scholar] [CrossRef]
- Baudoux, T.E.; Pozdzik, A.A.; Arlt, V.M.; De Prez, E.G.; Antoine, M.-H.; Quellard, N.; Goujon, J.-M.; Nortier, J.L. Probenecid prevents acute tubular necrosis in a mouse model of aristolochic acid nephropathy. Kidney Int. 2012, 82, 1105–1113. [Google Scholar] [CrossRef] [Green Version]

| Characters | Number (%) |
|---|---|
| Total | 120 (100%) |
| Age (y/o) | |
| Median ± SD | 65.0 ± 15.1 |
| 20–29 | 1 (0.8%) |
| 30–39 | 12 (9.9%) |
| 40–49 | 11 (9.1%) |
| 50–59 | 18 (14.9%) |
| 60–69 | 32 (26.4%) |
| 70–79 | 30 (24.8%) |
| ≥80 | 16 (13.2%) |
| Gender | |
| Male | 62 (51.2%) |
| Female | 58 (47.9%) |
| Diagnosis | |
| RCC | 53 (43.8%) |
| UC | 42 (34.7%) |
| AML | 6 (5.0%) |
| ESRD | 11 (9.1%) |
| Other | 8 (6.6%) |
| CKD stage | |
| 1 | 10 (8.3%) |
| 2 | 41 (33.9%) |
| 3 | 29 (24.0%) |
| 4 | 5 (4.1%) |
| 5 | 35 (28.9%) |
| Functional grade | |
| I | 51 (42.1%) |
| II | 34 (28.1%) |
| III | 35 (28.9%) |
| eGFR (excluding dialysis) | |
| Mean ± SD | 66.8 ± 27.6 |
| Histology Grade | |
| 1 | 37 (30.6%) |
| 2 | 30 (24.8%) |
| 3 | 17 (14.0%) |
| 4A | 14 (11.6%) |
| 4B | 22 (18.2%) |
| Characters | Non-Tumor Part Q-Score | p-Value |
|---|---|---|
| (Mean ± SD) | ||
| Age | ||
| <65 y/o | 5.16 ± 1.14 | 0.184 |
| ≥65 y/o | 4.81 ± 1.45 | |
| Gender | ||
| Male | 4.82 ± 1.41 | 0.230 |
| Female | 5.14 ± 1.46 | |
| Diagnosis | ||
| RCC | 5.43 ± 1.08 | <0.001 |
| UC | 4.36 ± 1.43 | |
| AML | 6.50 ± 1.23 | |
| ESRD | 3.55 ± 0.69 | |
| Others | 6.00 ± 1.51 | |
| Functional grade | ||
| I | 5.86 ± 1.18 | <0.001 |
| II | 5.15 ± 1.13 | |
| III | 3.51 ± 0.72 | |
| Histology Grade | ||
| 1 | 6.76 ± 0.44 | <0.001 |
| 2 | 4.77 ± 0.79 | |
| 3 | 4.29 ± 0.92 | |
| 4A | 3.86 ± 0.77 | |
| 4B | 3.50 ± 0.74 |
| Parameters | Estimated | 95% Confident Intervals | p-Value |
|---|---|---|---|
| Age | |||
| <65 y/o | 1 | ||
| ≥65 y/o | 0.989 | 0.757–1.292 | 0.934 |
| Gender | |||
| Male | 1 | ||
| Female | 1.326 | 1.037–1.697 | 0.025 |
| Diagnosis | |||
| RCC | 1 | ||
| UC | 0.813 | 0.578–1.144 | 0.232 |
| ESRD | 0.894 | 0.534–1.496 | 0.666 |
| AML + Others | 0.892 | 0.591–1.347 | 0.583 |
| Histology Grade | |||
| 1 | 1 | ||
| 2 + 3 | 0.130 | 0.097–0.175 | <0.001 |
| 4A + 4B | 0.089 | 0.287–0.718 | <0.001 |
| Functional grade | |||
| I | 1 | ||
| II | 1.113 | 0.781–1.585 | 0.550 |
| III | 0.454 | 0.287–0.718 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, Y.-J.; Wu, Y.-J.; Chen, L.-J.; Ko, B.-S.; Chang, T.-C.; Wu, Y.-J.; Liang, S.-M.; Jan, Y.-J.; Liou, J.-Y. Reduced Expression of Metallothionein-I/II in Renal Proximal Tubules Is Associated with Advanced Chronic Kidney Disease. Toxins 2021, 13, 568. https://doi.org/10.3390/toxins13080568
Lu Y-J, Wu Y-J, Chen L-J, Ko B-S, Chang T-C, Wu Y-J, Liang S-M, Jan Y-J, Liou J-Y. Reduced Expression of Metallothionein-I/II in Renal Proximal Tubules Is Associated with Advanced Chronic Kidney Disease. Toxins. 2021; 13(8):568. https://doi.org/10.3390/toxins13080568
Chicago/Turabian StyleLu, Yi-Jhu, Ya-Ju Wu, Lu-Jen Chen, Bor-Sheng Ko, Tzu-Ching Chang, Yi-Ju Wu, Shu-Man Liang, Yee-Jee Jan, and Jun-Yang Liou. 2021. "Reduced Expression of Metallothionein-I/II in Renal Proximal Tubules Is Associated with Advanced Chronic Kidney Disease" Toxins 13, no. 8: 568. https://doi.org/10.3390/toxins13080568
APA StyleLu, Y.-J., Wu, Y.-J., Chen, L.-J., Ko, B.-S., Chang, T.-C., Wu, Y.-J., Liang, S.-M., Jan, Y.-J., & Liou, J.-Y. (2021). Reduced Expression of Metallothionein-I/II in Renal Proximal Tubules Is Associated with Advanced Chronic Kidney Disease. Toxins, 13(8), 568. https://doi.org/10.3390/toxins13080568





