Ergonomic Recommendations in Ultrasound-Guided Botulinum Neurotoxin Chemodenervation for Spasticity: An International Expert Group Opinion
Abstract
1. Introduction
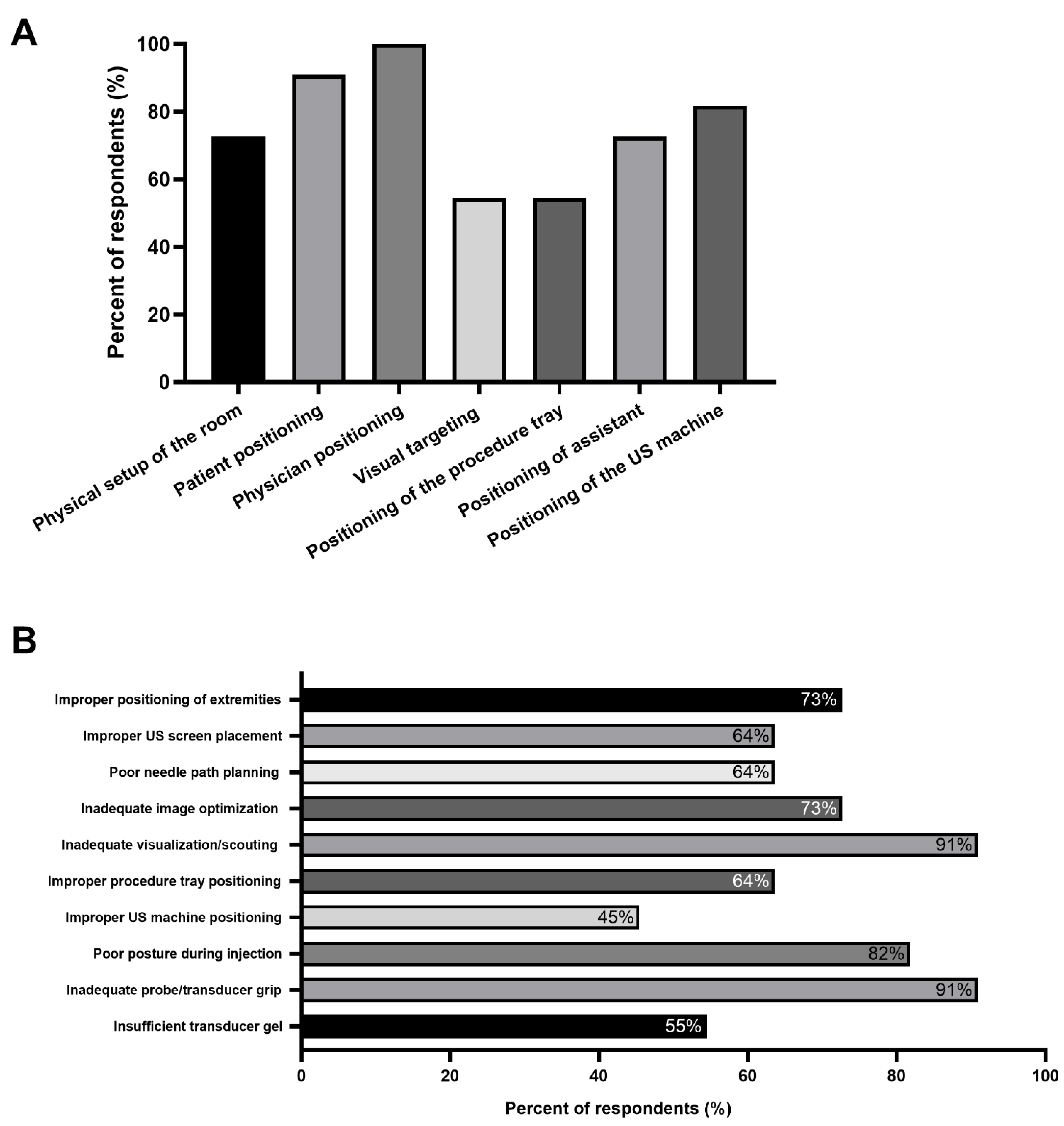
2. Ergonomics: The Reality
3. Results
4. Discussion
4.1. Overview
4.2. Workstation Ergonomics
4.2.1. Room Dimensions
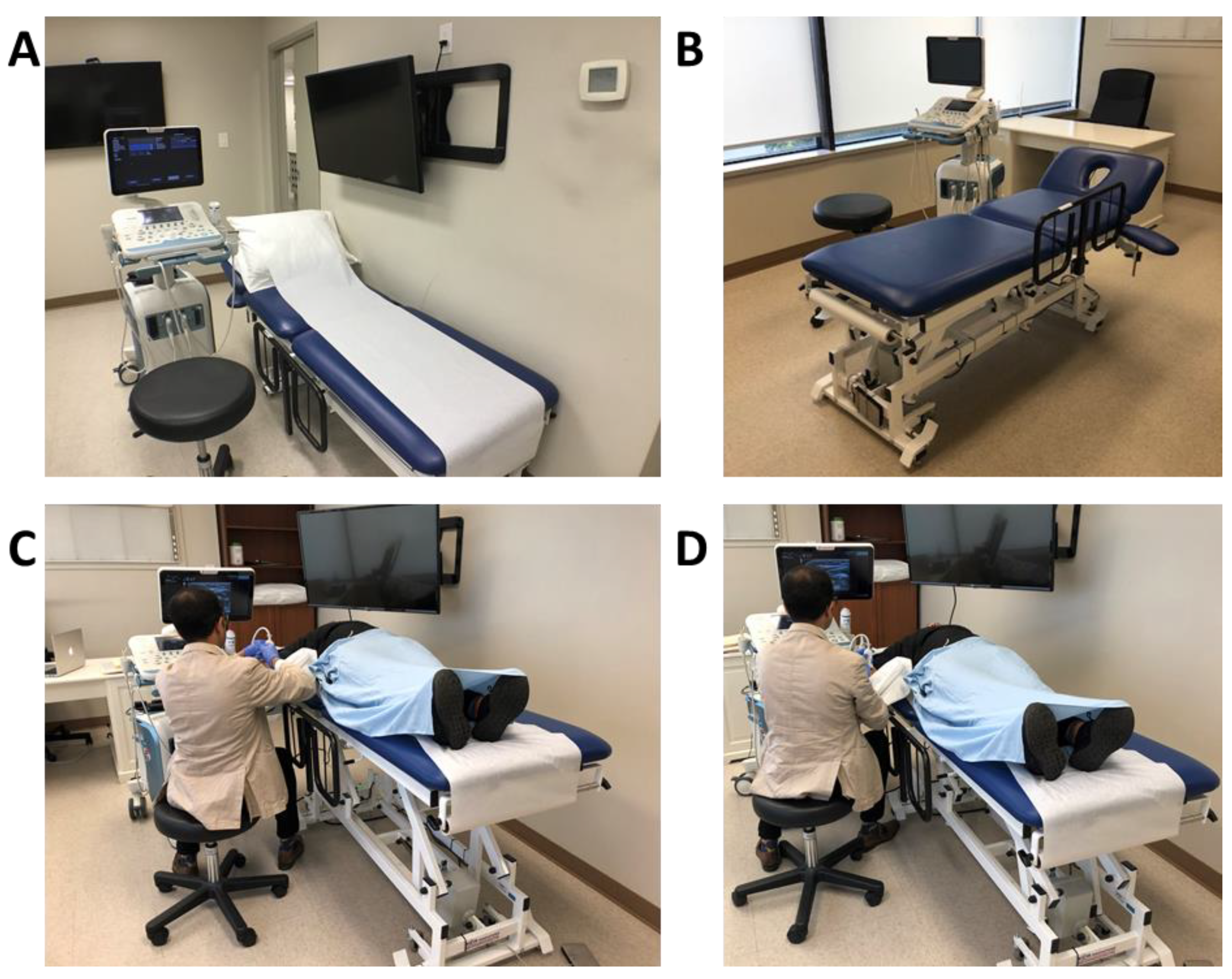
4.2.2. Height Adjustable Table and Comfortable Chair
4.2.3. Ability to Control Room Lighting, Adjusting Ultrasound Machine Parameters
4.2.4. Ultrasound Screen at Eye Level
4.2.5. Having an Assistant Available
4.2.6. Small Portable Surface
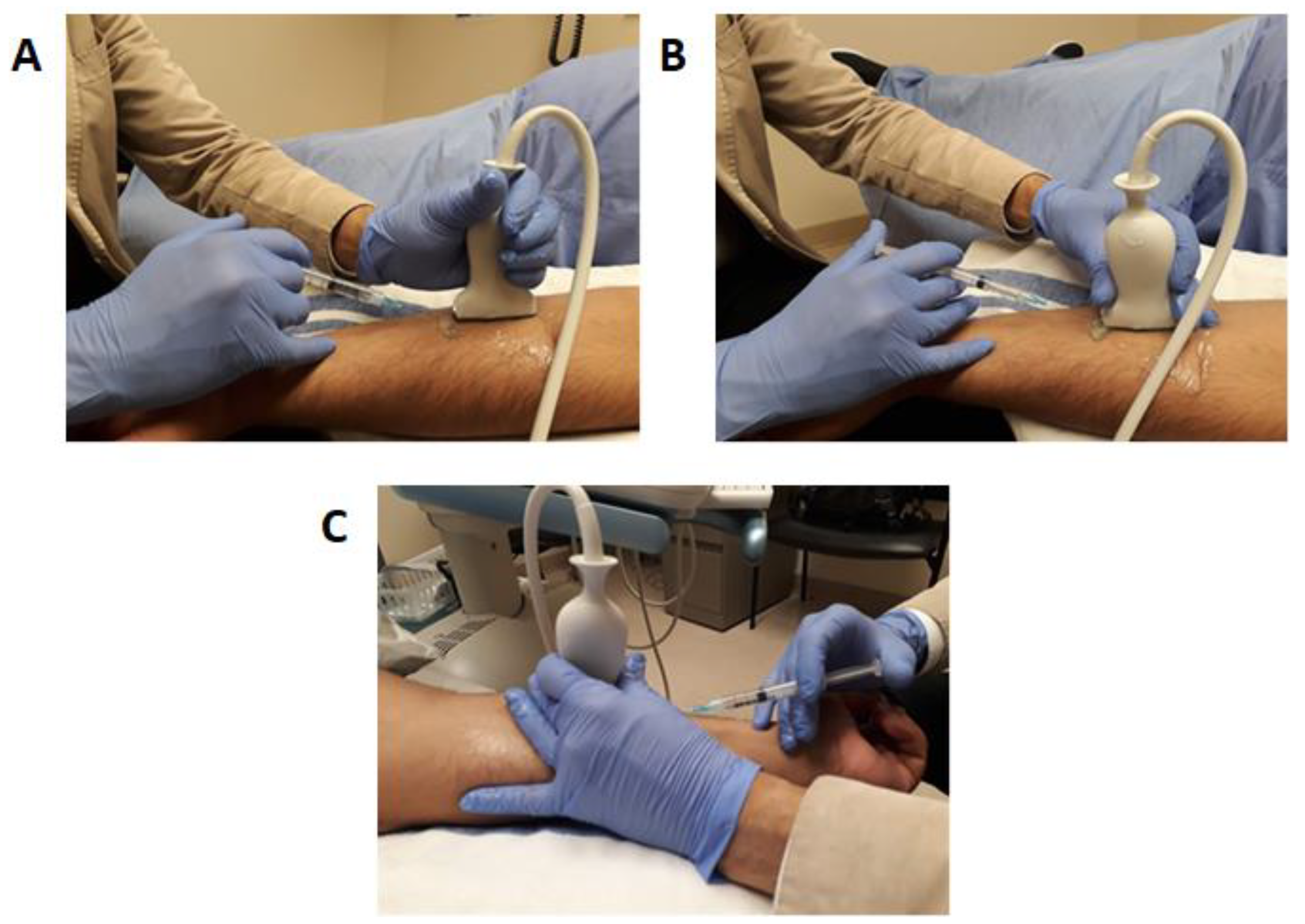
4.3. Physician Ergonomics
- (a)
- Neck should be flexed and not be extended.
- (b)
- Forearm horizontal to ground/examination table.
- (c)
- Arm abduction less than 30°.
- (d)
- Limited radial and ulnar deviation, less than 15° of wrist flexion and extension.
- (e)
- Arm should stay vertical at the side of the body with limited shoulder flexion and extension.
- (f)
- Attempt to have an ultrasound screen in the same line of sight as muscle to inject to minimize the degree of neck movement and facilitate a smooth transition of gaze from the screen to needle (“look down the barrel”).
- (g)
- Avoid excessive scapular protraction when injecting.
- (h)
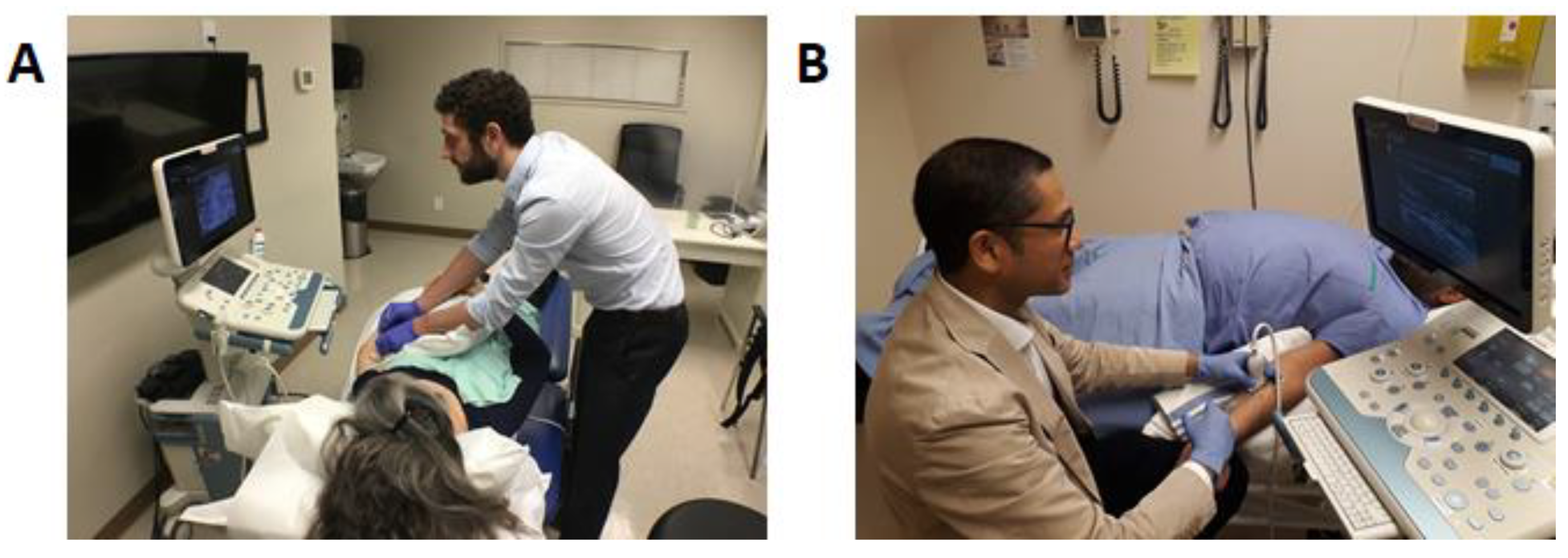
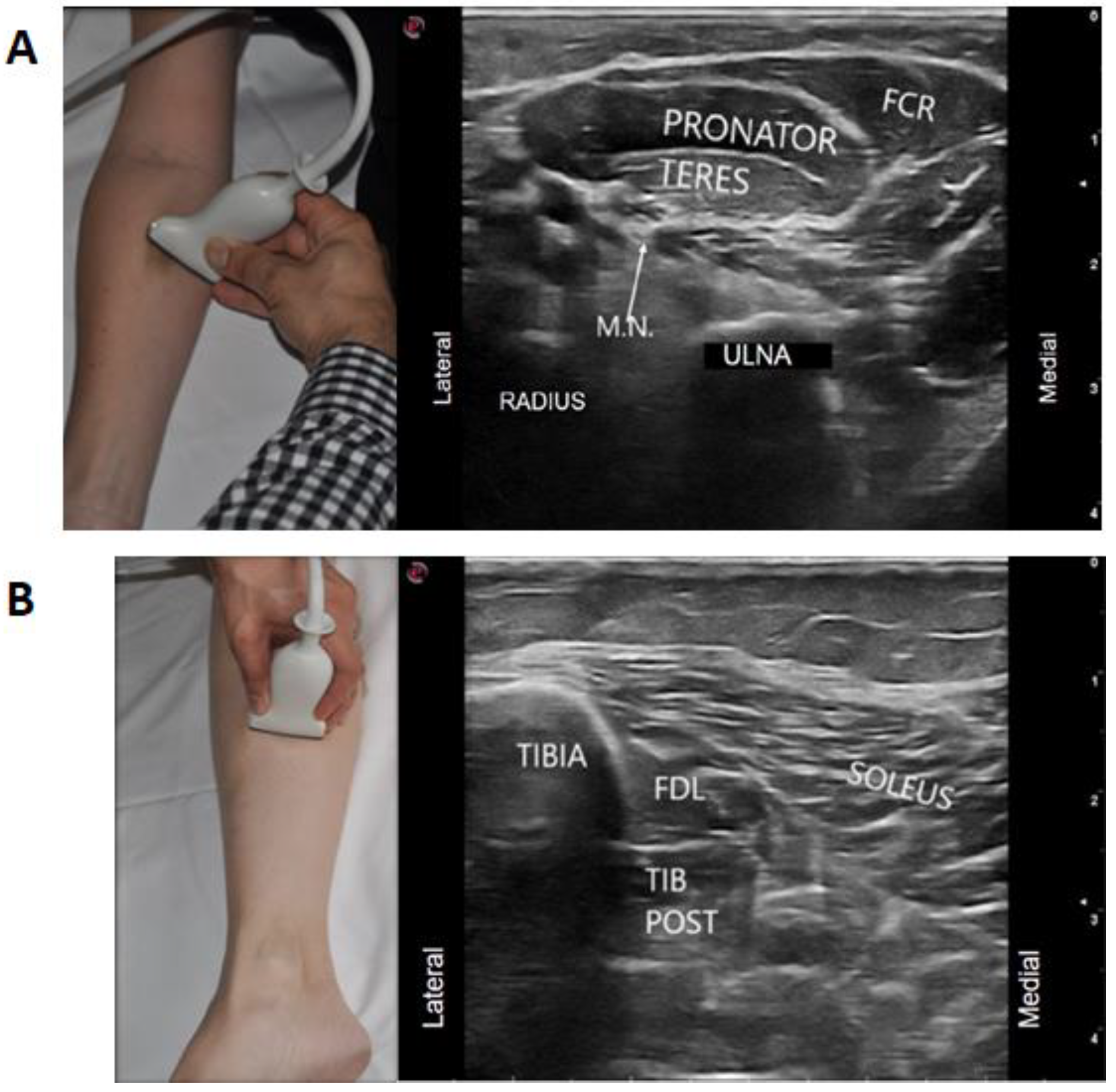
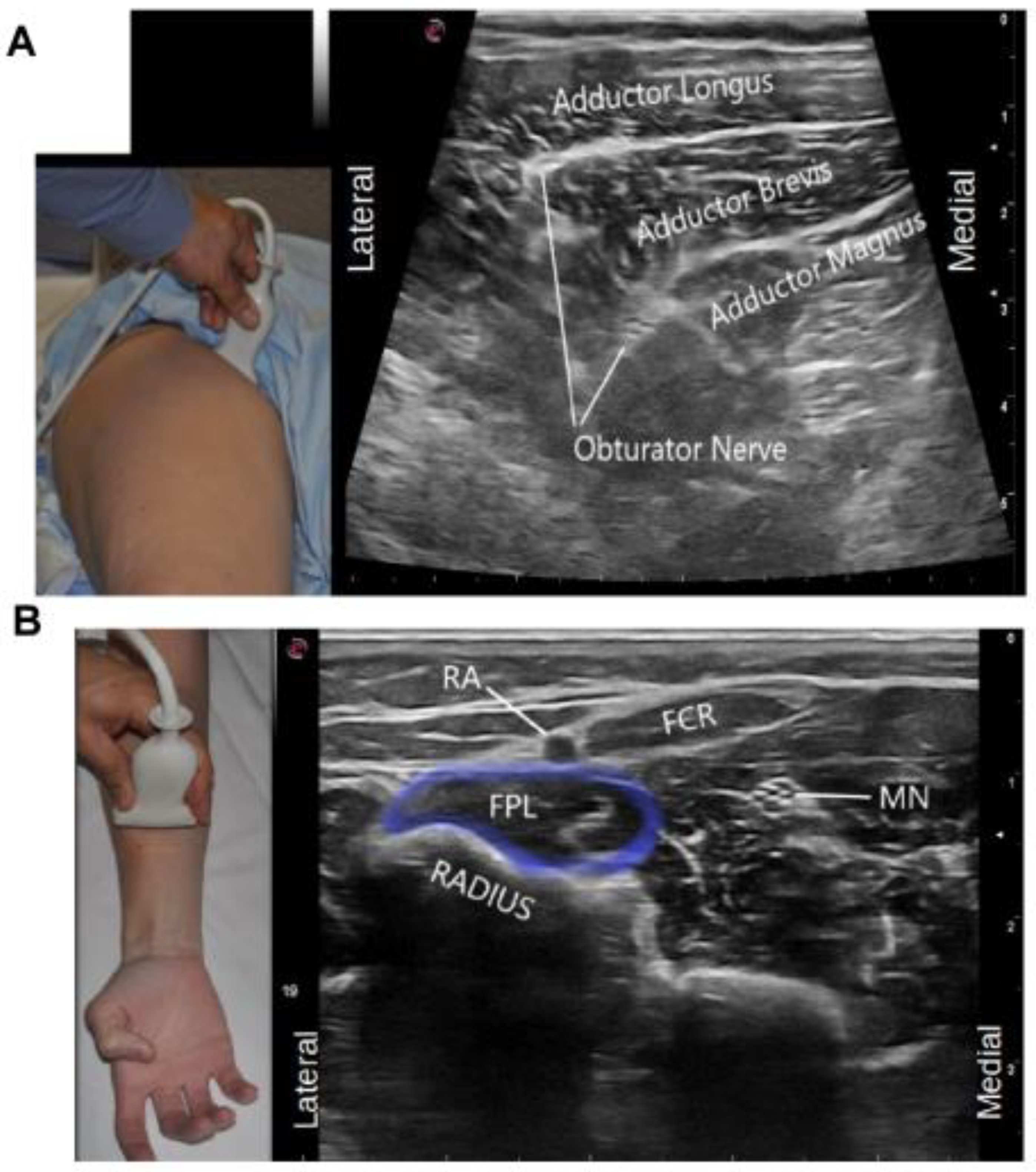
- Physicians should be on the same side as the injected limb to avoid reaching over the patient, as well as to avoid excessive scapular protraction from excessive reaching. Figure 3A shows incorrect physician positioning for injection of the upper limb and Figure 3B demonstrates the correct ergonomic position for an upper limb ultrasound guided chemodenervation for BoNT injection.
4.4. Patient Ergonomics
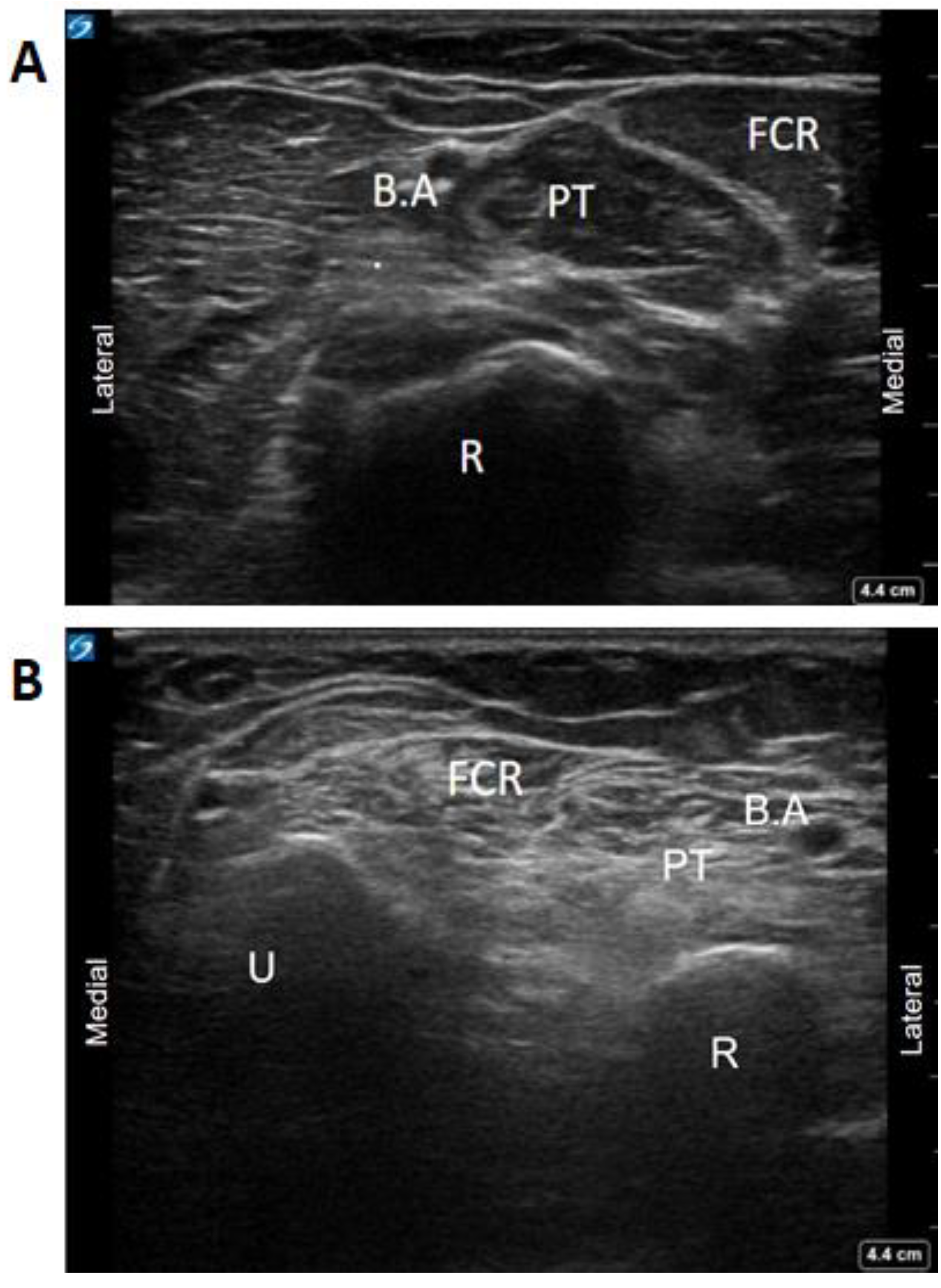
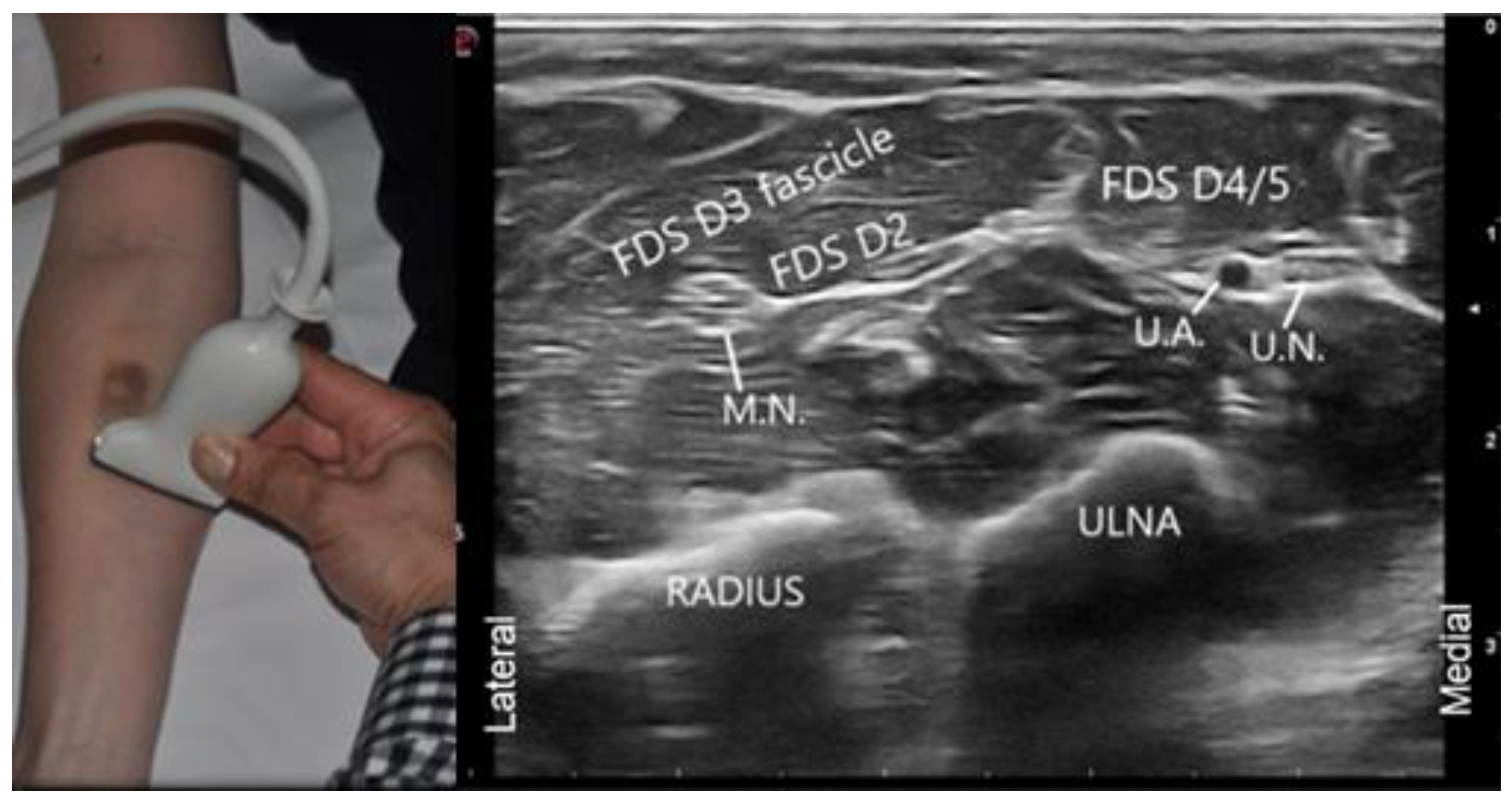
4.5. Visual Ergonomics Using Ultrasound
5. Conclusions
6. Methods
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Botulinum neurotoxin | BoNT |
| Ultrasound | US |
| Work-Related Musculoskeletal Disorders | WRMSDs |
| Musculoskeletal | MSK |
References
- Hignett, S.; Jones, E.L.; Miller, D.; Wolf, L.; Modi, C.; Shahzad, M.W.; Buckle, P.; Banerjee, J.; Catchpole, K. Human factors and ergonomics and quality improvement science: Integrating approaches for safety in healthcare. BMJ Qual. Saf. 2015, 24, 250–254. [Google Scholar] [CrossRef]
- Alter, K.E.; Karp, B.I. Ultrasound guidance for botulinum neurotoxin chemodenervation procedures. Toxins 2018, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Elovic, E.P.; Esquenazi, A.; Alter, K.E.; Lin, J.L.; Alfaro, A.; Kaelin, D.L. Chemodenervation and nerve blocks in the diagnosis and management of spasticity and muscle overactivity. PM&R 2009, 1, 842–851. [Google Scholar] [CrossRef]
- Kaymak, B.; Malas, F.Ü.; Kara, M.; On, A.Y.; Özçakar, L. Comment on Ultrasound Guidance for Botulinum Neurotoxin Chemodenervation Procedures. Toxins 2017, 10, 18-Quintessential Use of Ultrasound Guidance for Botulinum Toxin Injections-Muscle Innervation Zone Targeting Revisited. Toxins 2018, 10, 396. [Google Scholar] [CrossRef] [PubMed]
- Chiaramonte, R.; Bonfiglio, M.; Castorina, E.G.; Antoci, S.A.M. The primacy of ultrasound in the assessment of muscle architecture: Precision, accuracy, reliability of ultrasonography. Physiatrist, radiologist, general internist, and family practitioner’s experiences. Rev. Assoc. Med. Bras. 2019, 65, 165–170. [Google Scholar] [CrossRef]
- Mathevon, L.; Michel, F.; Aubry, S.; Testa, R.; Lapole, T.; Arnaudeau, L.F.; Fernandez, B.; Parratte, B.; Calmels, P. Two-dimensional and shear wave elastography ultrasound: A reliable method to analyse spastic muscles? Muscle Nerve 2018, 57, 222–228. [Google Scholar] [CrossRef]
- Gentile, D.; Floresta, G.; Patamia, V.; Chiaramonte, R.; Mauro, G.L.; Rescifina, A.; Vecchio, M. An Integrated Pharmacophore/Docking/3D-QSAR Approach to Screening a Large Library of Products in Search of Future Botulinum Neurotoxin a Inhibitors. Int. J. Mol. Sci. 2020, 21, 9470. [Google Scholar] [CrossRef] [PubMed]
- Gracies, J.M.; Jech, R.; Valkovic, P.; Marque, P.; Vecchio, M.; Denes, Z.; Vilain, C.; Delafont, B.; Picaut, P. When can maximal efficacy occur with repeat botulinum toxin injection in upper limb spastic paresis? Brain Commun. 2020, 3, fcaa201. [Google Scholar] [CrossRef]
- Santamato, A.; Ranieri, M.; Solfrizzi, V.; Lozupone, M.; Vecchio, M.; Daniele, A.; Greco, A.; Seripa, D.; Logroscino, G.; Panza, F. High doses of incobotulinumtoxinA for the treatment of post-stroke spasticity: Are they safe and effective? Expert Opin. Drug Metab. Toxicol. 2016, 12, 843–846. [Google Scholar] [CrossRef][Green Version]
- Chan, A.K.; Finlayson, H.; Mills, P.B. Does the method of botulinum neurotoxin injection for limb spasticity affect outcomes? A systematic review. Clin. Rehabil. 2017, 31, 713–721. [Google Scholar] [CrossRef]
- Py, A.G.; Zein Addeen, G.; Perrier, Y.; Carlier, R.Y.; Picard, A. Evaluation of the effectiveness of botulinum toxin injections in the lower limb muscles of children with cerebral palsy. Preliminary prospective study of the advantages of ultrasound guidance. Ann. Phys. Rehabil. Med. 2009, 52, 215–223. [Google Scholar] [CrossRef]
- Picelli, A.; Tamburin, S.; Bonetti, P.; Fontana, C.; Barausse, M.; Dambruoso, F.; Gajofatto, F.; Santilli, V.; Smania, N. Botulinum toxin type a injection into the Gastrocnemius muscle for spastic Equinus in adults with stroke. Am. J. Phys. Med. Rehabil. 2012, 91, 957–964. [Google Scholar] [CrossRef]
- Toxin Academy. Toxin Academy Courses: Web Page 2020. Available online: http://toxinacademy.com/courses.html (accessed on 12 September 2020).
- American Academy of Physical Medicine and Rehabilitation. AAPMR Annual Assembly Ultrasound-Guided Chemodenervation Skills Labs: Web Page 2020. Available online: https://www.aapmr.org/education/annual-assembly (accessed on 12 September 2020).
- American Academy of Physical Medicine and Rehabilitation. STEP Interventional Spasticity Certificate Program: Web Page 2020. Available online: https://www.aapmr.org/education/step-certificate-programs/step-interventional-spasticity-certificate-program (accessed on 12 September 2020).
- American Academy for Cerebral Palsy and Development Medicine A. American Academy for Cerebral Palsy and Developmental Medicine: Web Page 2020. Available online: https://www.aacpdm.org/education/ (accessed on 12 September 2020).
- Schroeder, A.S.; Berweck, S.; Fietzek, U.M.; Doberauer, J.; Wurzinger, L.; Reiter, K.; Wissel, J.; Heinen, F. MUC—Munich Ultrasound Course: Web Page 2020. Available online: http://munichultrasoundcourse.com/ (accessed on 12 September 2020).
- Baker, J.P.; Coffin, C.T. The importance of an ergonomic workstation to practicing sonographers. J. Ultrasound Med. 2013, 32, 1363–1375. [Google Scholar] [CrossRef]
- Wissel, J.; Ward, A.B.; Erztgaard, P.; Bensmail, D.; Hecht, M.J.; Lejeune, T.M.; Schnider, P. European consensus table on the use of botulinum toxin type a in adult spasticity. J. Rehabil. Med. 2009, 41, 13–25. [Google Scholar] [CrossRef]
- Euler, E.; Meadows, V. Elimination of Sonographer Musculoskeletal Injury in a Hospital-Based Cardiovascular Sonography Laboratory Following Implementation of Ergonomic Guidelines. J. Diagn. Med. Sonogr. 2012, 28, 325–328. [Google Scholar] [CrossRef]
- Pike, I.; Russo, A.; Berkowitz, J.; Baker, J.P.; Lessoway, V.A. The prevalence of musculoskeletal disorders among diagnostic medical sonographers. J. Diagn. Med. Sonogr. 1997, 13, 219–227. [Google Scholar] [CrossRef]
- Evans, K.; Roll, S.; Baker, J. Work-related musculoskeletal disorders (WRMSD) among registered diagnostic medical sonographers and vascular technologists: A representative sample. J. Diagn. Med. Sonogr. 2009, 25, 287–299. [Google Scholar] [CrossRef]
- Scholl, C.; Salisbury, H. Barriers to Performing Ergonomic Scanning Techniques for Sonographers. J. Diagn. Med. Sonogr. 2017, 33, 406–411. [Google Scholar] [CrossRef]
- Murphey, S.; Evans, K.; Merton, D. Industry Standards for the Prevention of Work Related Musculoskeletal Disorders in Sonography. J. Diagn. Med. Sonogr. 2017, 33, 371–391. [Google Scholar] [CrossRef]
- Smith, J. AIUM Practice Parameter for the Performance of Selected Ultrasound-Guided Procedures. J. Ultrasound Med. 2016, 35, 1–40. [Google Scholar] [CrossRef]
- Aguirre-Ospina, O.D.; González-Maldonado, J.F.; Ríos-Medina, Á.M. Ergonomía en los bloqueos nerviosos guiados por ultrasonografía. Revista Colombiana de Anestesiología 2015, 43, 331–339. [Google Scholar] [CrossRef]
- Sites, B.D.; Spence, B.C.; Gallagher, J.D.; Wiley, C.W.; Bertrand, M.L.; Blike, G.T. Characterizing Novice Behavior Associated with Learning Ultrasound-Guided Peripheral Regional Anesthesia. Reg. Anesth. Pain Med. 2007, 32, 107–115. [Google Scholar] [CrossRef]
- Baker, J. The “Price” We All Pay for Ignoring Ergonomics in Sonography. SRU Newsl. 2011, 21, 3–4. [Google Scholar]
- Harrison, G.; Harris, A. Work-related musculoskeletal disorders in ultrasound: Can you reduce risk? Ultrasound 2015, 23, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Bevilacqua, L.; Mirk, P.; Fileni, A.; Castellino, N. Work-Related Musculoskeletal Complaints in Sonologists. J. Occup. Environ. Med. 1999, 41, 981–988. [Google Scholar] [CrossRef]
- Alter, K.E.; Hallett, M.; Karp, B.; Lungu, C. Ultrasound-Guided Chemodenervation Procedures: Text and Atlas Hardcover; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Chapman, G.A.; Johnson, D.; Bodenham, A.R. Visualisation of needle position using ultrasonography. Anaesthesia 2006, 61, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Fietzek, U.M.; Schroeder, A.S.; Wissel, J.; Heinen, F.; Berweck, S. Split-screen video demonstration of sonography-guided muscle identification and injection of botulinum toxin. Mov. Disord. 2010, 25, 2225–2228. [Google Scholar] [CrossRef]
- Hill, J.J.; Slade, M.D.; Russi, M.B. Anthropometric measurements, job strain, and prevalence of musculoskeletal symptoms in female medical sonographers. Work 2009, 33, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Seto, E.; Biclar, L. Ambidextrous sonographic scanning to reduce sonographer repetitive strain injury. J. Diagn. Med. Sonogr. 2008, 24, 127–135. [Google Scholar] [CrossRef]
- Moreta, M.C.; Fleet, A.; Reebye, R.; McKernan, G.; Berger, M.; Farag, J.; Munin, M.C. Reliability and Validity of the Modified Heckmatt Scale in Evaluating Muscle Changes with Ultrasound in Spasticity. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100071. [Google Scholar] [CrossRef]
- Picelli, A.; Bonetti, P.; Fontana, C.; Barausse, M.; Dambruoso, F.; Gajofatto, F.; Girardi, P.; Manca, M.; Gimigliano, R.; Smania, N. Is spastic muscle echo intensity related to the response to botulinum toxin type A in patients with stroke? A cohort study. Arch. Phys. Med. Rehabil. 2012, 93, 1253–1258. [Google Scholar] [CrossRef] [PubMed]
- Henzel, M.K.; Munin, M.C.; Niyonkuru, C.; Skidmore, E.R.; Weber, D.J.; Zafonte, R.D. Comparison of Surface and Ultrasound Localization to Identify Forearm Flexor Muscles for Botulinum Toxin Injections. PM&R 2010, 2, 642–646. [Google Scholar] [CrossRef]
| Question | Mean (Range) |
|---|---|
| How many years of experience do you have regarding the use of ultrasound-guided chemodenervation for spasticity management? | 12.2 years (3–22) |
| How many years of teaching do you have with regards to training medical students, residents and other junior staff physicians in the area of ultrasound-guided chemodenervation? | 10.5 years (2–20) |
| In the courses you have attended for ultrasound-guided injection, what percentage formally addressed the proper ergonomics of ultrasound-guided injections? | 17.3% (0–50) |
| Question & Responses | Responses (%) |
| When you perform ultrasound-guided chemodenervation do you operate alone or with another person assisting? | |
| Alone | 0 (0%) |
| Assisted | 4 (36.4%) |
| Both | 7 (63.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lagnau, P.; Lo, A.; Sandarage, R.; Alter, K.; Picelli, A.; Wissel, J.; Verduzco-Gutierrez, M.; Suputtitada, A.; Munin, M.C.; Carda, S.; et al. Ergonomic Recommendations in Ultrasound-Guided Botulinum Neurotoxin Chemodenervation for Spasticity: An International Expert Group Opinion. Toxins 2021, 13, 249. https://doi.org/10.3390/toxins13040249
Lagnau P, Lo A, Sandarage R, Alter K, Picelli A, Wissel J, Verduzco-Gutierrez M, Suputtitada A, Munin MC, Carda S, et al. Ergonomic Recommendations in Ultrasound-Guided Botulinum Neurotoxin Chemodenervation for Spasticity: An International Expert Group Opinion. Toxins. 2021; 13(4):249. https://doi.org/10.3390/toxins13040249
Chicago/Turabian StyleLagnau, Philippe, Alto Lo, Ryan Sandarage, Katharine Alter, Alessandro Picelli, Jorg Wissel, Monica Verduzco-Gutierrez, Areerat Suputtitada, Michael C. Munin, Stefano Carda, and et al. 2021. "Ergonomic Recommendations in Ultrasound-Guided Botulinum Neurotoxin Chemodenervation for Spasticity: An International Expert Group Opinion" Toxins 13, no. 4: 249. https://doi.org/10.3390/toxins13040249
APA StyleLagnau, P., Lo, A., Sandarage, R., Alter, K., Picelli, A., Wissel, J., Verduzco-Gutierrez, M., Suputtitada, A., Munin, M. C., Carda, S., Khan, O., Koçer, S., & Reebye, R. (2021). Ergonomic Recommendations in Ultrasound-Guided Botulinum Neurotoxin Chemodenervation for Spasticity: An International Expert Group Opinion. Toxins, 13(4), 249. https://doi.org/10.3390/toxins13040249








