Revealing the Therapeutic Potential of Botulinum Neurotoxin Type A in Counteracting Paralysis and Neuropathic Pain in Spinally Injured Mice
Abstract
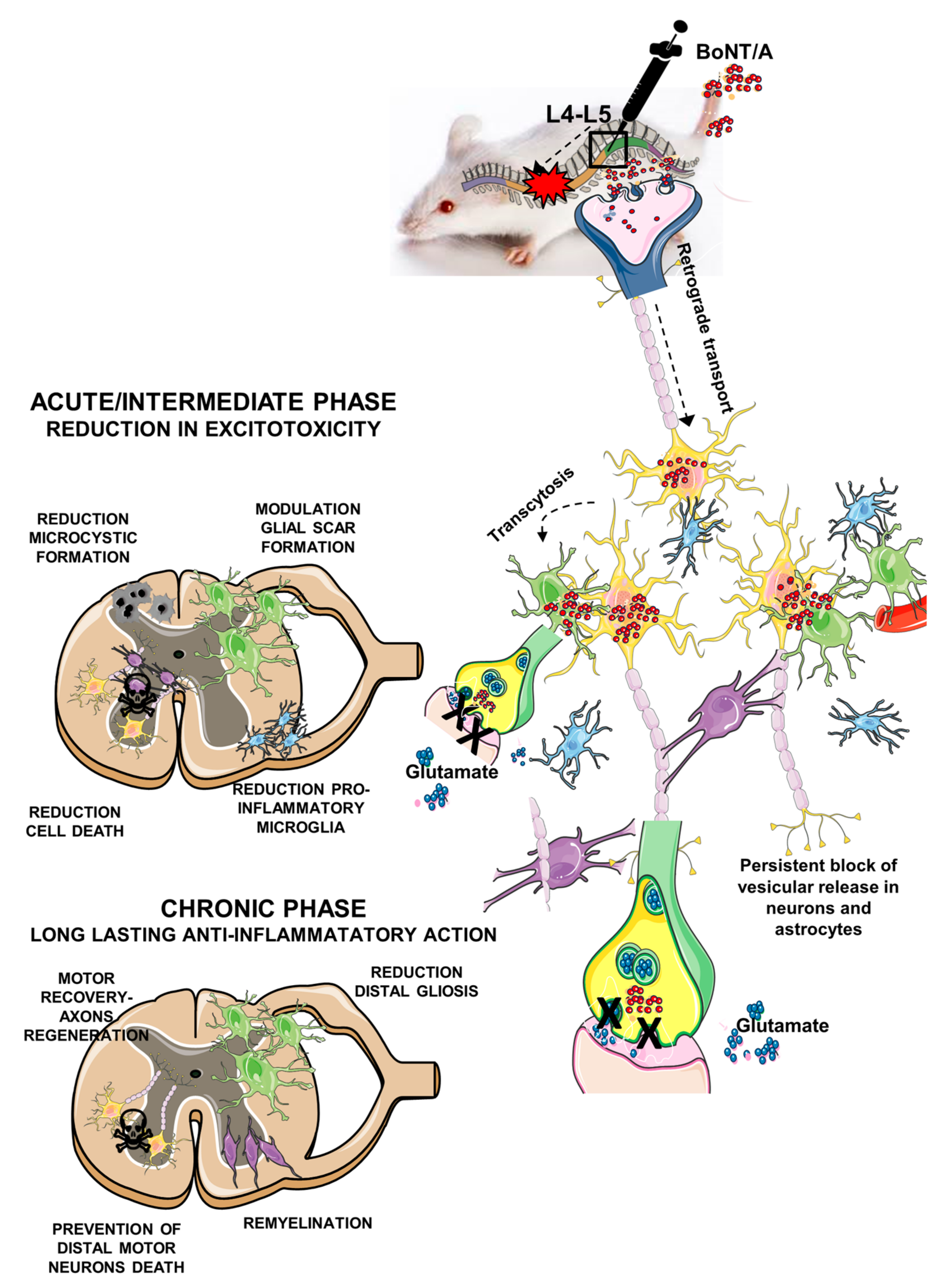
1. Introduction
2. Results
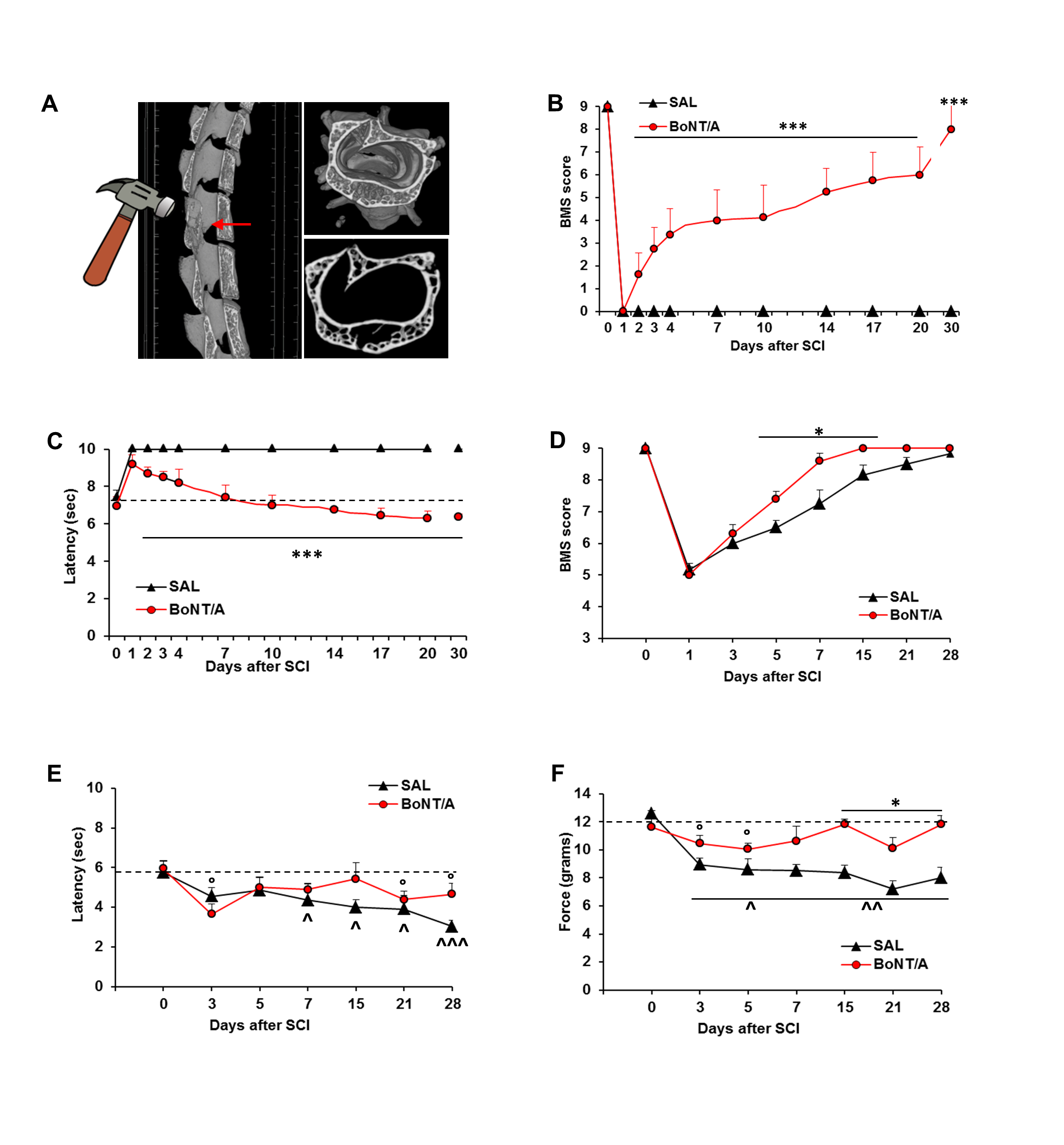
2.1. BoNT/A Improves Motor Control, Restores Thermal Sensitivity, and Counteracts NeP Onset in the Severe and Moderate SCI Mice
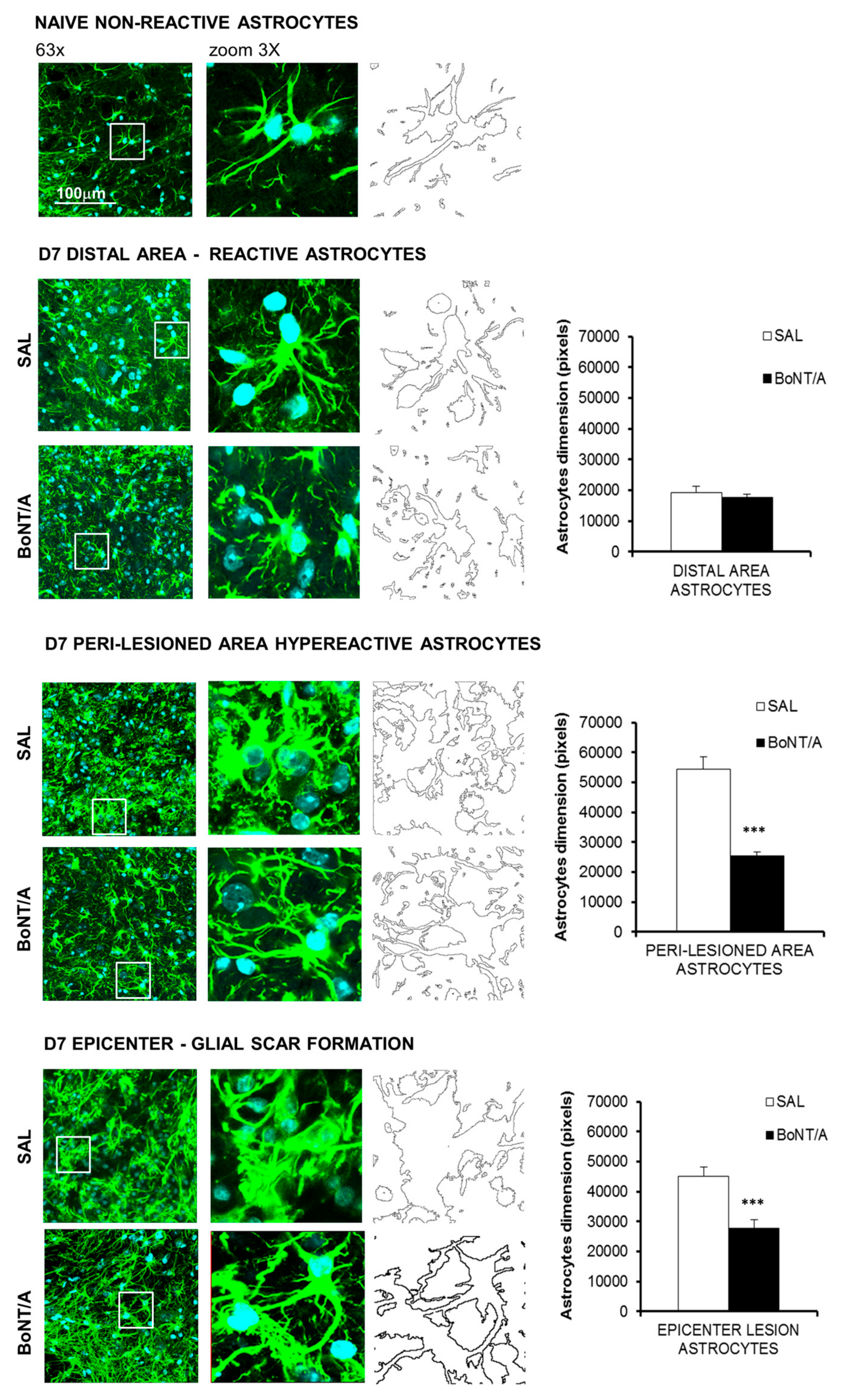
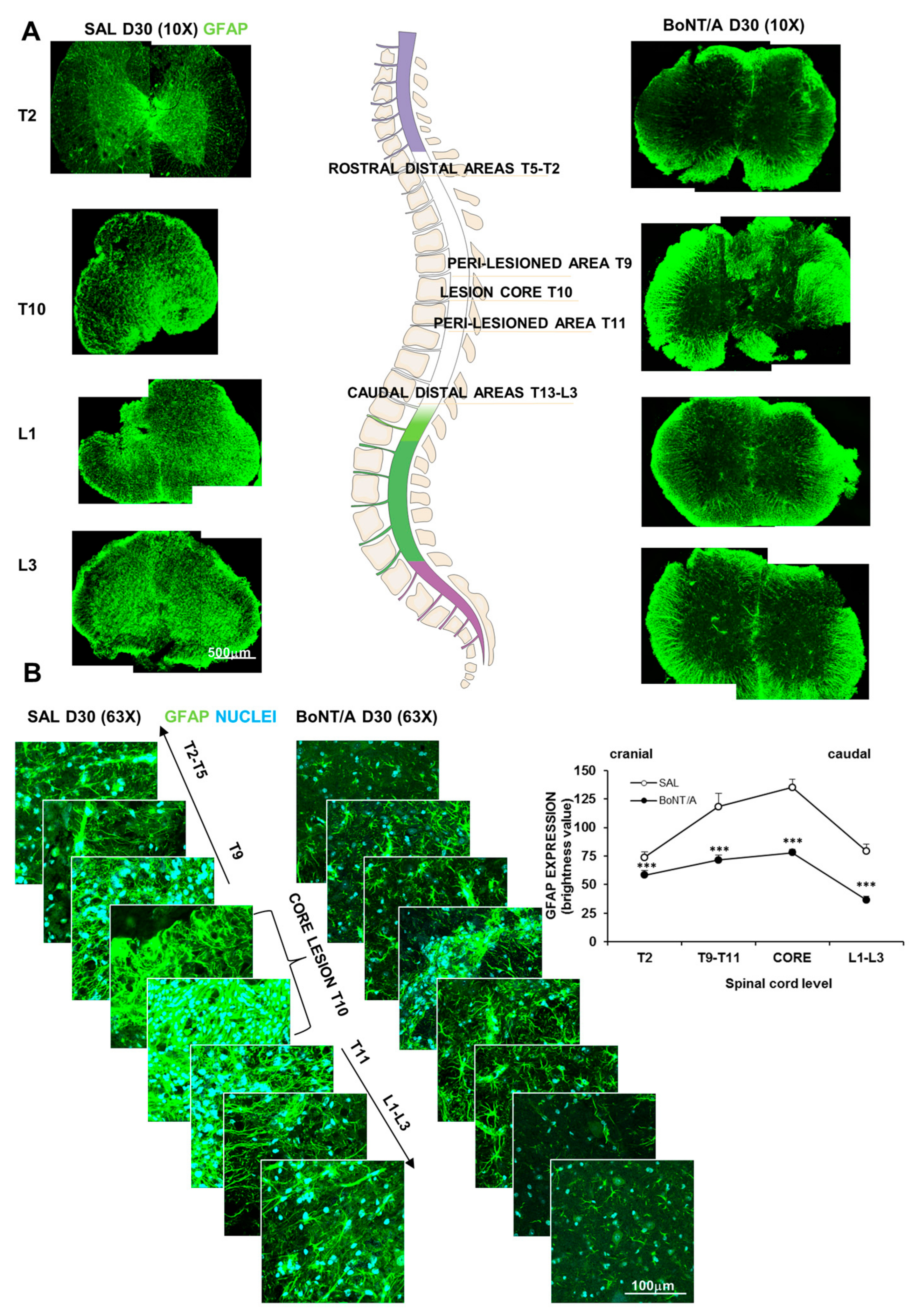
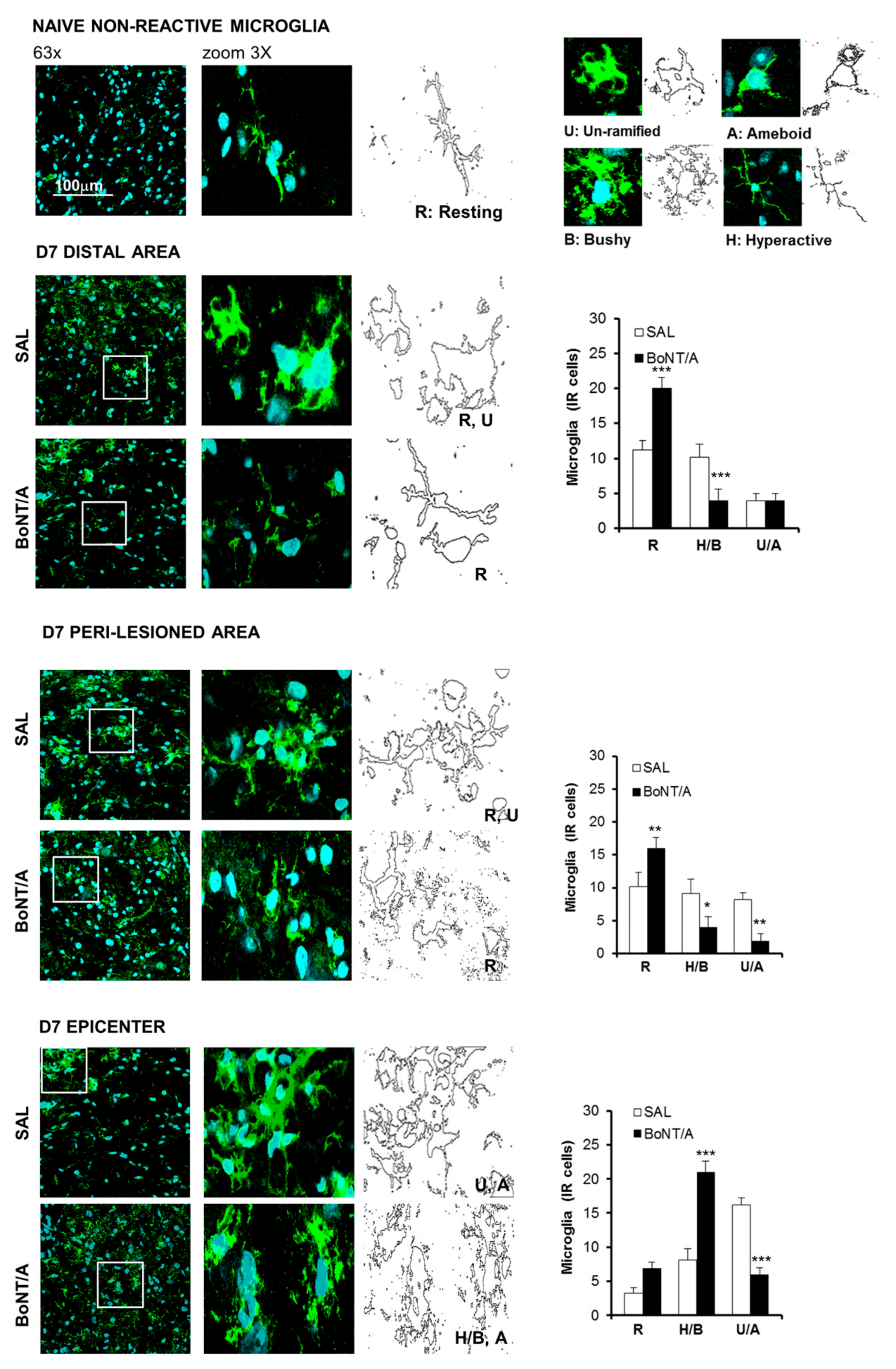
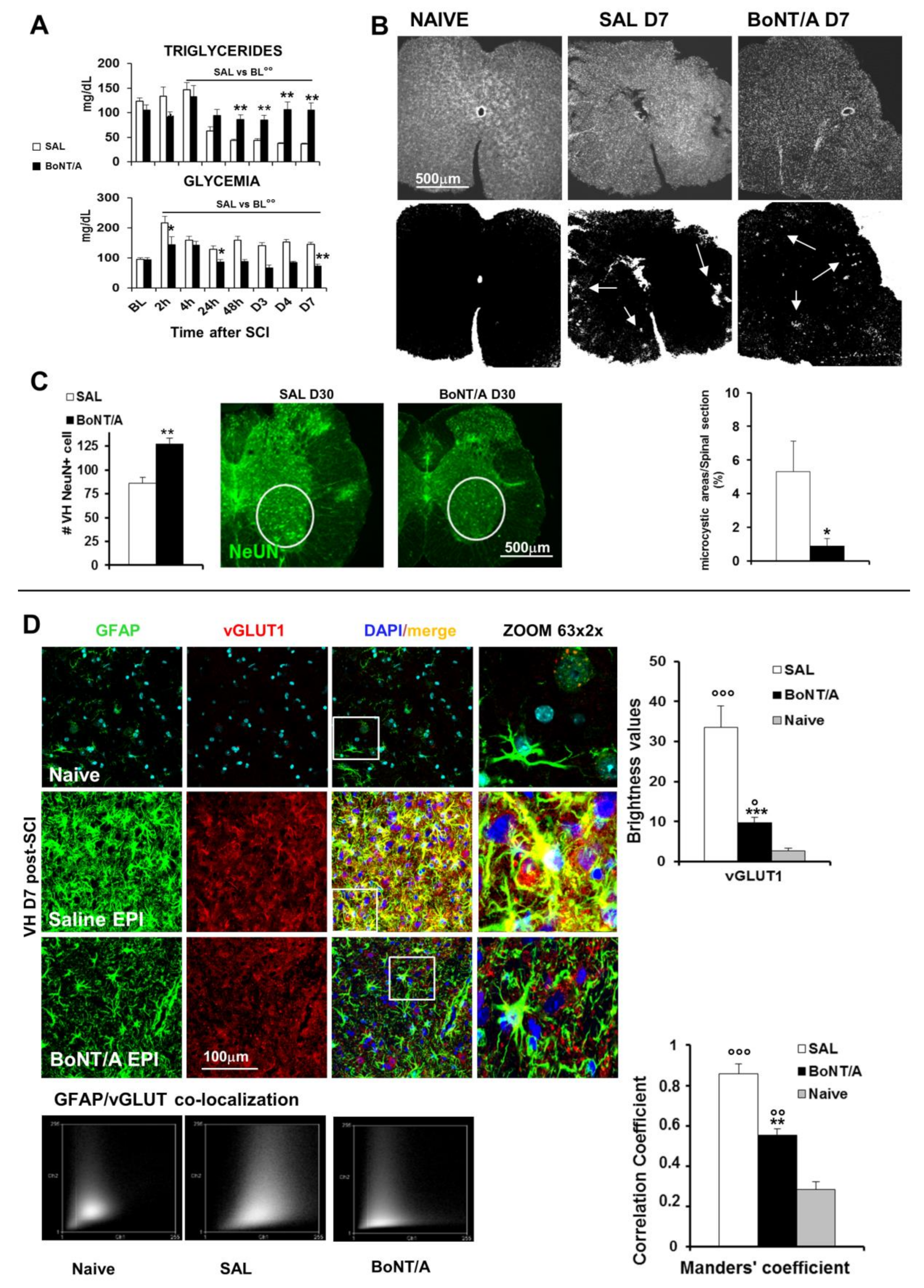
2.2. Modulatory Effects of BoNT/A on Glia Scarring and Microglia Reaction
2.3. Protective Effects of BoNT/A on Lipid and Glycemic Profiles, Cell Death, and Remyelination
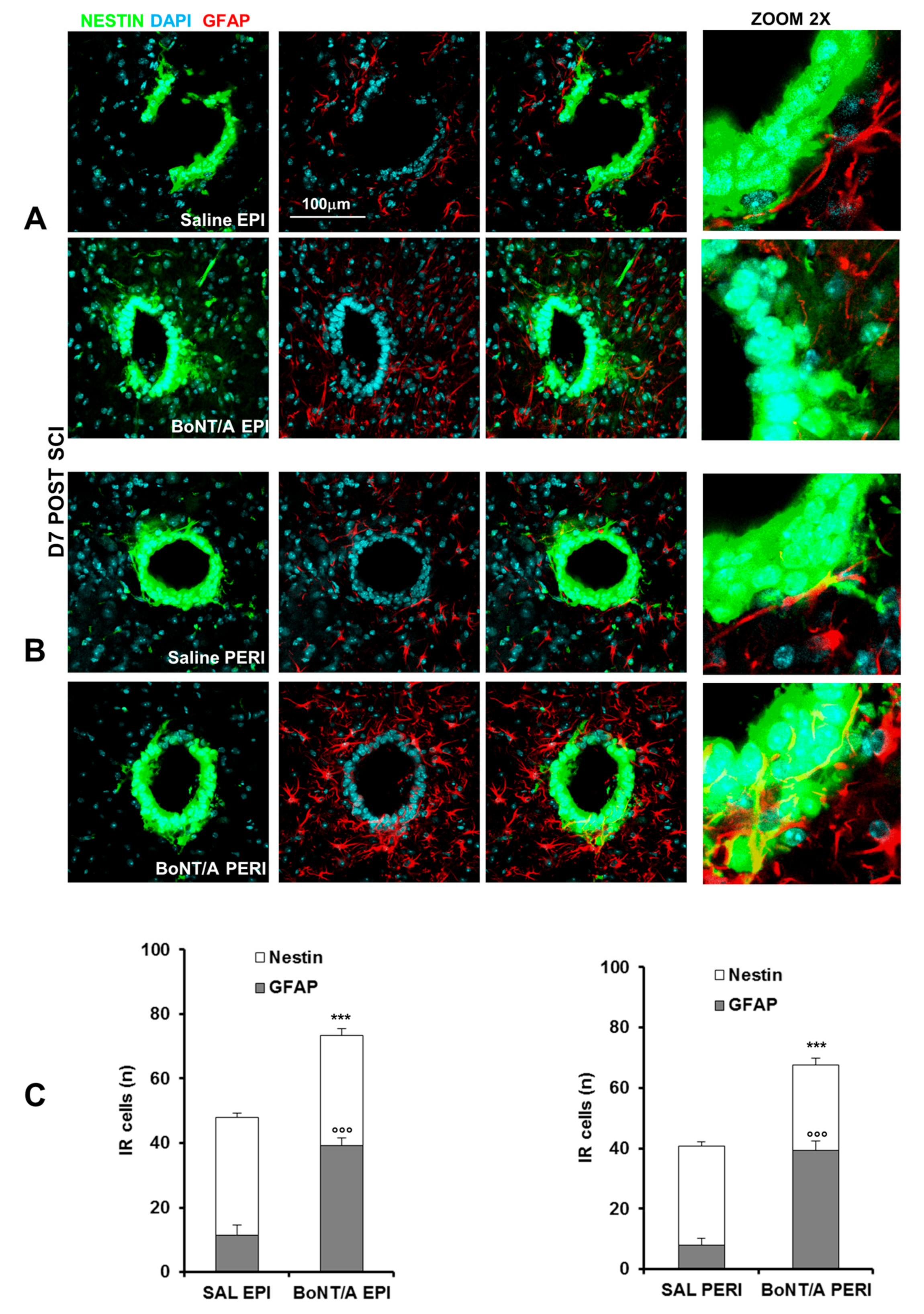
2.4. Effects of BoNT/A on Stem Cells Stimulation and 3D Spinal-Cord Reconstruction
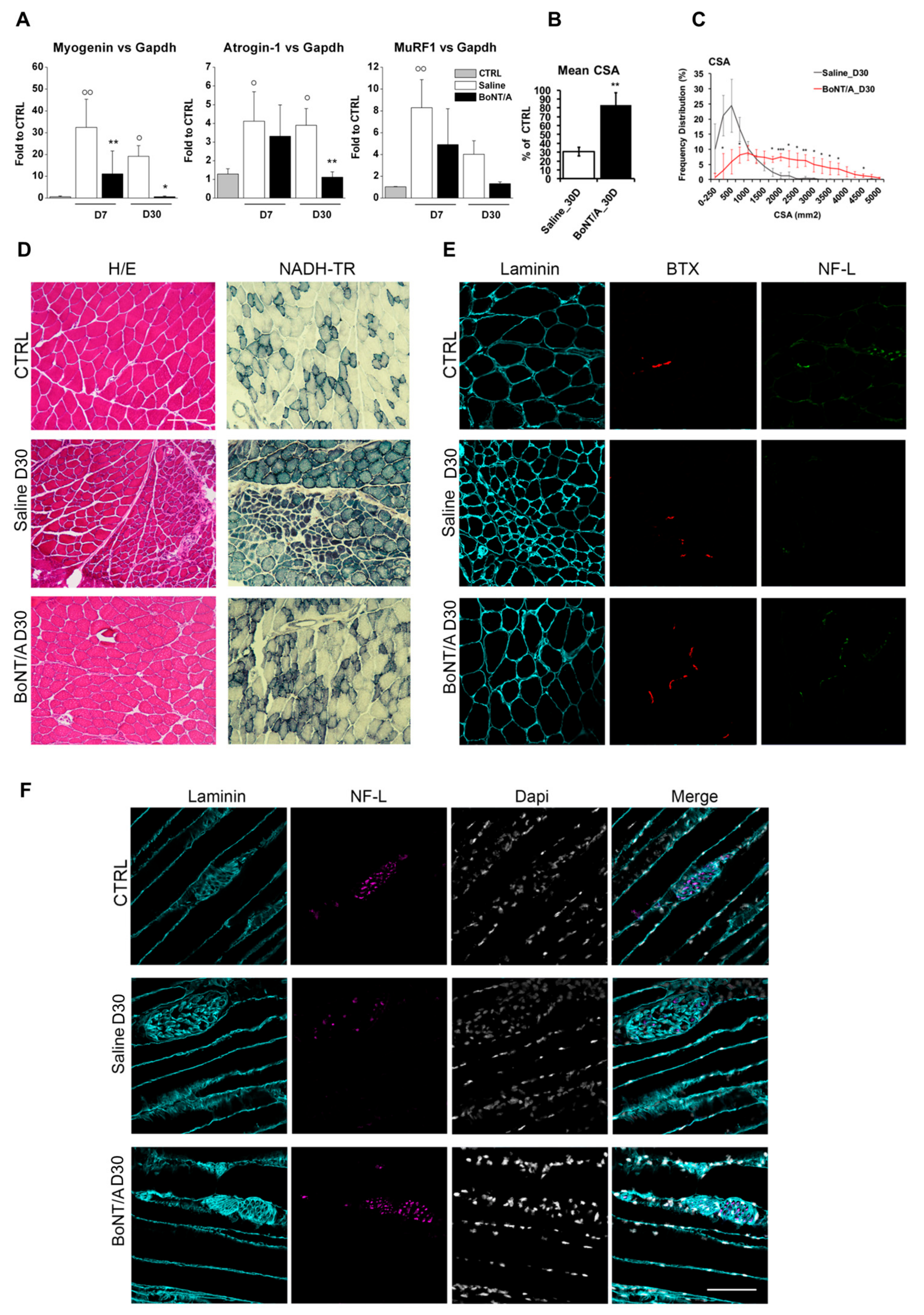
2.5. Muscle Atrophy Recovery after BoNT/A Treatment as Consequence of Motor Neurons Reconnection
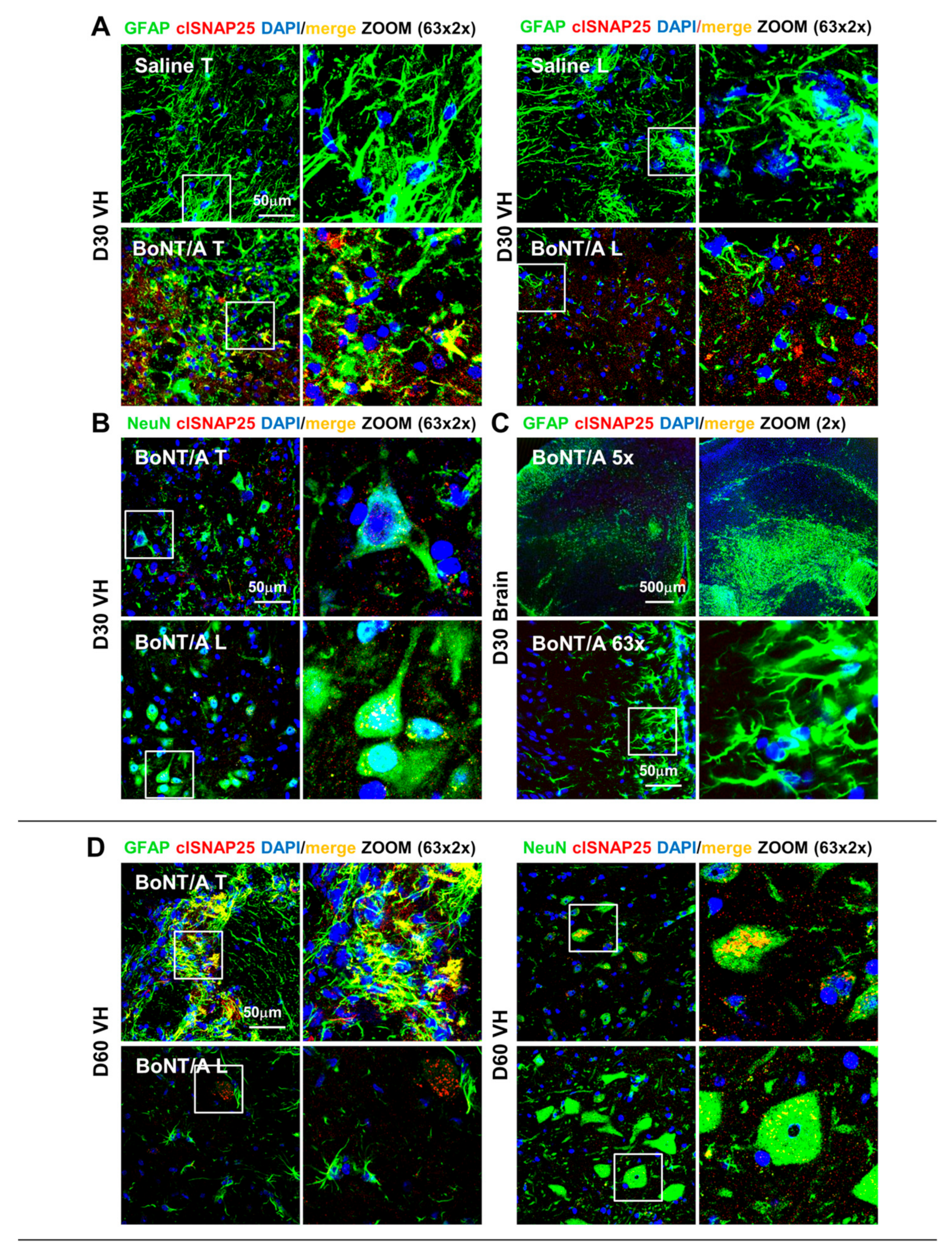
2.6. Long-Lasting Proteolytic Action of BoNT/A Affects Astrocytes and Neurons of Spinal Cord but Not Brain
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Surgery
4.2.1. Severe Trauma in CD1 Mice
4.2.2. Moderate Trauma
4.3. Drugs
4.4. Behavioral Test: Basso Mouse Scale (BMS)
4.5. Nociceptive Tests
4.5.1. Tail Flick Test
4.5.2. Mechanical Allodynia
4.6. Evaluation of Muscle Functionality
4.6.1. Histological Analysis of Skeletal Muscle
4.6.2. RT-PCR and qPCR
4.7. Immunohistochemistry
4.7.1. Histological Analysis of Spinal Cord Tissue
4.7.2. Lesion Size (Microcystic Degeneration and Neuronal Survival)
4.7.3. Morphometric Analysis
4.8. Western Blot
4.9. Micro Xray Computed Tomography (MicroCT)
4.10. Glycemia and Triglycerides Measurement
4.11. Experimental Design and Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Consortium for Spinal Cord Medicine. Early acute management in adults with spinal cord injury. J. Spinal Cord Med. 2008, 31, 403–479. [Google Scholar] [CrossRef]
- Kumar, R.; Lim, J.; Mekary, R.A.; Rattani, A.; Dewan, M.C.; Sharif, S.Y.; Osorio-Fonseca, E.; Park, K.B. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurg. 2018, 113, e345–e363. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.B.; Cripps, R.A.; Fitzharris, M.; Wing, P.C. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord 2013, 52, 110–116. [Google Scholar] [CrossRef]
- Kim, Y.H.; Ha, K.Y.; Kim, S.-I. Spinal cord injury and related clinical trials. CIOS Clin. Orthop. Surg. 2017, 9, 1–9. [Google Scholar] [CrossRef]
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Myelin damage and repair in pathologic CNS: Challenges and prospects. Front. Mol. Neurosci. 2015, 8, 35. [Google Scholar] [CrossRef]
- Hutson, T.H.; Di Giovanni, S. The translational landscape in spinal cord injury: Focus on neuroplasticity and regeneration. Nat. Rev. Neurol. 2019, 15, 732–745. [Google Scholar] [CrossRef]
- Boccella, S.; Vacca, V.; Errico, F.; Marinelli, S.; Squillace, M.; Guida, F.; Di Maio, A.; Vitucci, D.; Palazzo, E.; De Novellis, V.; et al. D-aspartate modulates nociceptive-specific neuron activity and pain threshold in inflammatory and neuropathic pain condition in mice. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef]
- Marinelli, S.; Vacca, V.; De Angelis, F.; Pieroni, L.; Orsini, T.; Parisi, C.; Soligo, M.; Protto, V.; Manni, L.; Guerrieri, R.; et al. Innovative mouse model mimicking human-like features of spinal cord injury: Efficacy of Docosahexaenoic acid on acute and chronic phases. Sci. Rep. 2019, 9, 1–16. [Google Scholar] [CrossRef]
- Fonfria, E.; Maignel, J.; Lezmi, S.; Martin, V.; Splevins, A.; Shubber, S.; Kalinichev, M.; Foster, K.; Picaut, P.; Krupp, J. The expanding therapeutic utility of botulinum neurotoxins. Toxins 2018, 10, 208. [Google Scholar] [CrossRef]
- Antonucci, F.; Rossi, C.; Gianfranceschi, L.; Rossetto, O.; Caleo, M. Long-distance retrograde effects of botulinum neurotoxin A. J. Neurosci. 2008, 28, 3689–3696. [Google Scholar] [CrossRef]
- Marinelli, S.; Vacca, V.; Ricordy, R.; Uggenti, C.; Tata, A.M.; Luvisetto, S.; Pavone, F. The analgesic effect on neuropathic pain of retrogradely transported botulinum neurotoxin A involves Schwann cells and Astrocytes. PLoS ONE 2012, 7, e47977. [Google Scholar] [CrossRef] [PubMed]
- Caleo, M.; Restani, L. Direct central nervous system effects of botulinum neurotoxin. Toxicon 2018, 147, 68–72. [Google Scholar] [CrossRef]
- Marinelli, S.; Luvisetto, S.; Cobianchi, S.; Makuch, W.; Obara, I.; Mezzaroma, E.; Caruso, M.; Straface, E.; Przewlocka, B.; Pavone, F. Botulinum neurotoxin type A counteracts neuropathic pain and facilitates functional recovery after peripheral nerve injury in animal models. Neuroscience 2010, 171, 316–328. [Google Scholar] [CrossRef]
- Pavone, F.; Luvisetto, S. Botulinum neurotoxin for pain management: Insights from animal models. Toxins 2010, 2, 2890–2913. [Google Scholar] [CrossRef]
- Cobianchi, S.; Jaramillo, J.; Luvisetto, S.; Pavone, F.; Navarro, X. Botulinum neurotoxin A promotes functional recovery after peripheral nerve injury by increasing regeneration of myelinated fibers. Neuroscience 2017, 359, 82–91. [Google Scholar] [CrossRef]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum neurotoxins: Biology, pharmacology, and toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef]
- Marinelli, S.; Pavone, F.; Luvisetto, S.; Vacca, V. A New Therapeutic Use of the Botulinum Neurotoxin Serotype A. International Patent Application No. PCT/IB2016/052280, 25 April 2015. [Google Scholar]
- Kundi, S.; Bicknell, R.; Ahmed, Z. Spinal cord injury: Current mammalian models. Am. J. Neurosci. 2013, 4, 1–12. [Google Scholar] [CrossRef]
- Cheriyan, J.; Ryan, D.J.; Weinreb, J.H.; Paul, J.C.; Lafage, V.; Kirsch, T.; Errico, T.J. Spinal cord injury models: A review. Spinal Cord 2014, 52, 588–595. [Google Scholar] [CrossRef]
- Basso, D.M.; Fisher, L.C.; Anderson, A.J.; Jakeman, L.; McTigue, D.M.; Popovich, P.G. Basso mouse scale for locomotion detects differences in recovery after spinal cord injury in five common mouse strains. J. Neurotrauma 2006, 23, 635–659. [Google Scholar] [CrossRef]
- Yang, T.; Dai, Y.; Chen, G.; Cui, S. Dissecting the dual role of the glial scar and scar-forming astrocytes in spinal cord injury. Front. Cell Neurosci. 2020, 14, 78. [Google Scholar] [CrossRef]
- Yamamotová, A.; Sramkova, T.; Rokyta, R. Intensity of pain and biochemical changes in blood plasma in spinal cord trauma. Spinal Cord 2009, 48, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Kobayakawa, K.; Kumamaru, H.; Saiwai, H.; Kubota, K.; Ohkawa, Y.; Kishimoto, J.; Yokota, K.; Ideta, R.; Shiba, K.; Tozaki-Saitoh, H.; et al. Acute hyperglycemia impairs functional improvement after spinal cord injury in mice and humans. Sci. Transl. Med. 2014, 6, 256ra137. [Google Scholar] [CrossRef]
- Laclaustra, M.; van den Berg, E.L.M.; Hurtado-Roca, Y.; Castellote, J.M. Serum lipid profile in subjects with traumatic spinal cord injury. PLoS ONE 2015, 10, e0115522. [Google Scholar] [CrossRef]
- Mills, C.D.; Fullwood, S.D.; Hulsebosch, C.E. Changes in Metabotropic Glutamate receptor expression following spinal cord injury. Exp. Neurol. 2001, 170, 244–257. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Leung, G.K.K. Oligodendrocyte precursor cells in spinal cord injury: A review and update. BioMed Res. Int. 2015, 2015, 20. [Google Scholar] [CrossRef]
- Bartholdi, D.; Schwab, M.E. Oligodendroglial reaction following spinal cord injury in rat: Transient upregulation of MBP mRNA. Glia 1998, 23, 278–284. [Google Scholar] [CrossRef]
- Marichal, N.; Reali, C.; Trujillo-Cenóz, O.; Russo, R.E. Spinal Cord Stem Cells in Their Microenvironment: The Ependyma as a Stem Cell Niche. In Retinal Degenerative Diseases; Springer Science and Business Media LLC: New York, NY, USA, 2017; Volume 1041, pp. 55–79. [Google Scholar]
- Sandri, M. Protein breakdown in muscle wasting: Role of autophagy-lysosome and ubiquitin-proteasome. Int. J. Biochem. Cell Boil. 2013, 45, 2121–2129. [Google Scholar] [CrossRef]
- Moresi, V.; Williams, A.H.; Meadows, E.; Flynn, J.M.; Potthoff, M.J.; McAnally, J.; Shelton, J.M.; Backs, J.; Klein, W.H.; Richardson, J.A.; et al. Myogenin and class II HDACs control neurogenic muscle atrophy by inducing E3 Ubiquitin Ligases. Cell 2010, 143, 35–45. [Google Scholar] [CrossRef]
- Rhéaume, C.; Cai, B.B.; Wang, J.; Fernandez-Salas, E.; Aoki, K.R.; Francis, J.; Broide, R.S. A highly specific Monoclonal antibody for botulinum neurotoxin Type A-Cleaved SNAP25. Toxins 2015, 7, 2354–2370. [Google Scholar] [CrossRef]
- Vogelaar, C.F. Extrinsic and intrinsic mechanisms of axon regeneration: The need for spinal cord injury treatment strategies to address both. Neural Regen. Res. 2016, 11, 572–574. [Google Scholar] [CrossRef]
- Yiu, G.; He, Z. Glial inhibition of CNS axon regeneration. Nat. Rev. Neurosci. 2006, 7, 617–627. [Google Scholar] [CrossRef]
- Karimi-Abdolrezaee, S.; Billakanti, R. Reactive Astrogliosis after spinal cord injury—Beneficial and detrimental effects. Mol. Neurobiol. 2012, 46, 251–264. [Google Scholar] [CrossRef]
- Hausmann, O.N. Post-traumatic inflammation following spinal cord injury. Spinal Cord 2003, 41, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Ju, G.; Wang, J.; Wang, Y.; Zhao, X. Spinal cord contusion. Neural Regen. Res. 2014, 9, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Walters, E.T. Neuroinflammatory contributions to pain after SCI: Roles for central glial mechanisms and nociceptor-mediated host defense. Exp. Neurol. 2014, 258, 48–61. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Dong, B.; Mao, Y.; Guan, W.; Cao, J.; Zhu, R.; Wang, S. Review: Traumatic brain injury and hyperglycemia, a potentially modifiable risk factor. Oncotarget 2016, 7, 71052–71061. [Google Scholar] [CrossRef]
- Ming, G.-L.; Song, H. Adult neurogenesis in the mammalian brain: Significant answers and significant questions. Neuron 2011, 70, 687–702. [Google Scholar] [CrossRef]
- Ke, Y.; Chi, L.; Xu, R.; Luo, C.; Gozal, D.; Liu, R. Early response of endogenous adult neural progenitor cells to acute spinal cord injury in mice. Stem Cells 2005, 24, 1011–1019. [Google Scholar] [CrossRef]
- Xu, R.; Wu, C.; Tao, Y.; Yi, J.; Yang, Y.; Zhang, X.; Liu, R. Nestin-positive cells in the spinal cord: A potential source of neural stem cells. Int. J. Dev. Neurosci. 2008, 26, 813–820. [Google Scholar] [CrossRef]
- Qin, Y.; Zhang, W.; Yang, P. Current states of endogenous stem cells in adult spinal cord. J. Neurosci. Res. 2014, 93, 391–398. [Google Scholar] [CrossRef]
- Martino, G.; Pluchino, S. The therapeutic potential of neural stem cells. Nat. Rev. Neurosci. 2006, 7, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Dooley, D.; Vidal, P.; Hendrix, S. Immunopharmacological intervention for successful neural stem cell therapy: New perspectives in CNS neurogenesis and repair. Pharmacol. Ther. 2014, 141, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Finnerup, N.B. Neuropathic pain and spasticity: Iintricate consequences of spinal cord injury. Spinal Cord 2017, 55, 1046–1050. [Google Scholar] [CrossRef]
- Giangregorio, L.; McCartney, N. Bone loss and muscle atrophy in spinal cord injury: Epidemiology, fracture prediction, and rehabilitation strategies. J. Spinal Cord Med. 2006, 29, 489–500. [Google Scholar] [CrossRef]
- Mignone, J.L.; Kukekov, V.; Chiang, A.-S.; Steindler, D.; Yenikolopov, G. Neural stem and progenitor cells in nestin-GFP transgenic mice. J. Comp. Neurol. 2004, 469, 311–324. [Google Scholar] [CrossRef]
- Zimmermann, M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983, 16, 109–110. [Google Scholar] [CrossRef]
- Ermakova, O.V.; Orsini, T.; Gambadoro, A.; Chiani, F.; Tocchini-Valentini, G.P. Three-dimensional microCT imaging of murine embryonic development from immediate post-implantation to organogenesis: Application for phenotyping analysis of early embryonic lethality in mutant animals. Mamm. Genome 2017, 29, 245–259. [Google Scholar] [CrossRef]
- Schiavo, G.; Montecucco, C. Tetanus and botulism neurotoxins: Isolation and assay. Methods Enzymol. 1995, 248, 643–652. [Google Scholar] [CrossRef]
- Luvisetto, S.; Rossetto, O.; Montecucco, C.; Pavone, F. Toxicity of botulinum neurotoxins in central nervous system of mice. Toxicon 2003, 41, 475–481. [Google Scholar] [CrossRef]
- Luvisetto, S.; Marinelli, S.; Lucchetti, F.; Marchi, F.; Cobianchi, S.; Rossetto, O.; Montecucco, C.; Pavone, F. Botulinum neurotoxins and formalin-induced pain: Central vs. peripheral effects in mice. Brain Res. 2006, 1082, 124–131. [Google Scholar] [CrossRef]
- Luvisetto, S.; Marinelli, S.; Cobianchi, S.; Pavone, F. Anti-allodynic efficacy of botulinum neurotoxin A in a model of neuropathic pain. Neuroscience 2007, 145, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Fiacco, E.; Castagnetti, F.; Bianconi, V.; Madaro, L.; De Bardi, M.; Nazio, F.; D’Amico, A.; Bertini, E.; Cecconi, F.; Puri, P.L.; et al. Autophagy regulates satellite cell ability to regenerate normal and dystrophic muscles. Cell Death Differ. 2016, 23, 1839–1849. [Google Scholar] [CrossRef] [PubMed]
- Madaro, L.; Marrocco, V.; Carnio, S.; Sandri, M.; Bouchè, M. Intracellular signaling in ER stress-induced autophagy in skeletal muscle cells. FASEB J. 2013, 27, 1990–2000. [Google Scholar] [CrossRef]
- Manders, E.M.; Stap, J.; Brakenhoff, G.J.; Van Driel, R.; Aten, J.A. Dynamics of three-dimensional replication patterns during the S-phase, analysed by double labelling of DNA and confocal microscopy. J. Cell Sci. 1992, 103, 857–862. [Google Scholar]


| Acute Phase (Initial Physical Insult) | Intermediate Phase (Cascade of Detrimental Events) | Chronic Phase (Irreversible Damage) |
|---|---|---|
| Spinal shock and hemorrhage | Microcystic formation | Mature cystic formation |
| Ischemia and cell death | Apoptosis | Extending apoptosis out of injury site |
| Edema, thrombosis and inflammation | Edema, immune cells invasion, microglia response, cytokines release | Demyelination |
| Glutamatergic excitotoxicity | Astrocytes hypertrophy and glia scar formation | Scarring |
| Demyelination | ||
| Electrolytes and metabolic alterations | Electrolytes and metabolic alterations | Regeneration/sprouting |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vacca, V.; Madaro, L.; De Angelis, F.; Proietti, D.; Cobianchi, S.; Orsini, T.; Puri, P.L.; Luvisetto, S.; Pavone, F.; Marinelli, S. Revealing the Therapeutic Potential of Botulinum Neurotoxin Type A in Counteracting Paralysis and Neuropathic Pain in Spinally Injured Mice. Toxins 2020, 12, 491. https://doi.org/10.3390/toxins12080491
Vacca V, Madaro L, De Angelis F, Proietti D, Cobianchi S, Orsini T, Puri PL, Luvisetto S, Pavone F, Marinelli S. Revealing the Therapeutic Potential of Botulinum Neurotoxin Type A in Counteracting Paralysis and Neuropathic Pain in Spinally Injured Mice. Toxins. 2020; 12(8):491. https://doi.org/10.3390/toxins12080491
Chicago/Turabian StyleVacca, Valentina, Luca Madaro, Federica De Angelis, Daisy Proietti, Stefano Cobianchi, Tiziana Orsini, Pier Lorenzo Puri, Siro Luvisetto, Flaminia Pavone, and Sara Marinelli. 2020. "Revealing the Therapeutic Potential of Botulinum Neurotoxin Type A in Counteracting Paralysis and Neuropathic Pain in Spinally Injured Mice" Toxins 12, no. 8: 491. https://doi.org/10.3390/toxins12080491
APA StyleVacca, V., Madaro, L., De Angelis, F., Proietti, D., Cobianchi, S., Orsini, T., Puri, P. L., Luvisetto, S., Pavone, F., & Marinelli, S. (2020). Revealing the Therapeutic Potential of Botulinum Neurotoxin Type A in Counteracting Paralysis and Neuropathic Pain in Spinally Injured Mice. Toxins, 12(8), 491. https://doi.org/10.3390/toxins12080491









