Inflammasome Activation Induced by a Snake Venom Lys49-Phospholipase A2 Homologue
Abstract
1. Introduction
2. Results
2.1. BthTX-I Induced Inflammation and Myonecrosis in Mouse Gastrocnemius Muscle
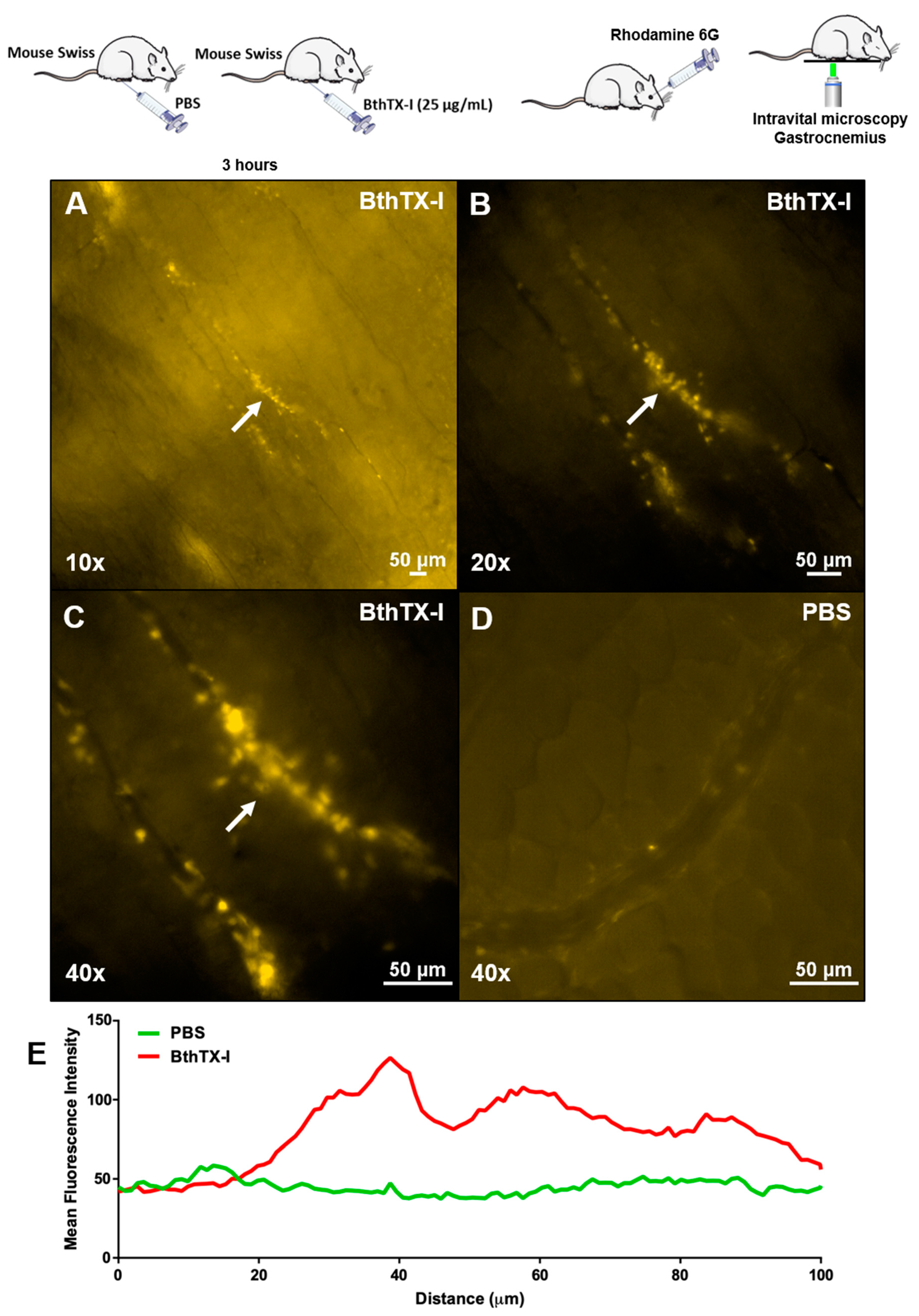
2.2. IL-1β Release by Injury in Muscle Gastrocnemius Induced by BthTX-I
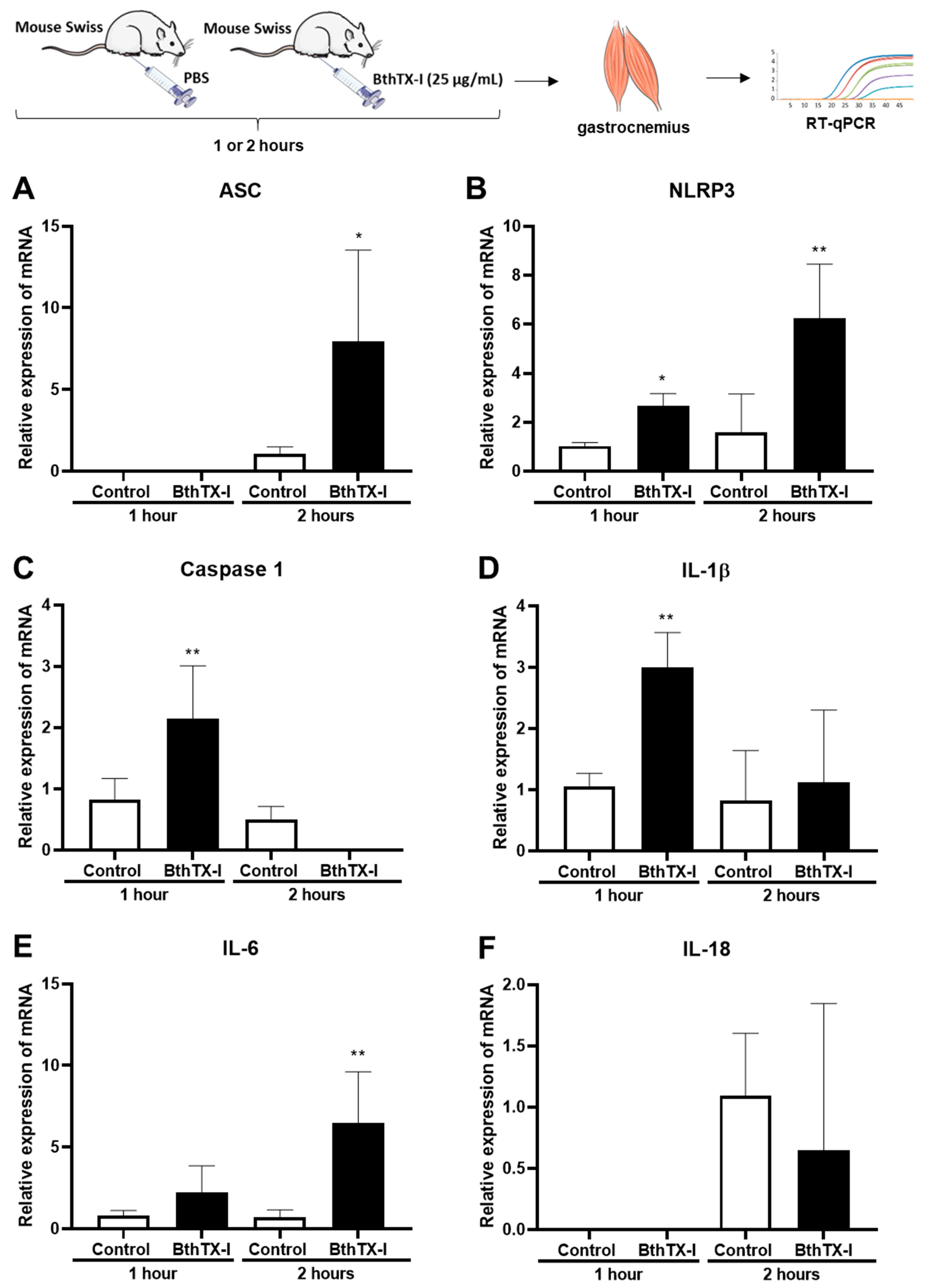
2.3. IL-1β Release by Injury in Muscle Gastrocnemius Induced by BthTX-I
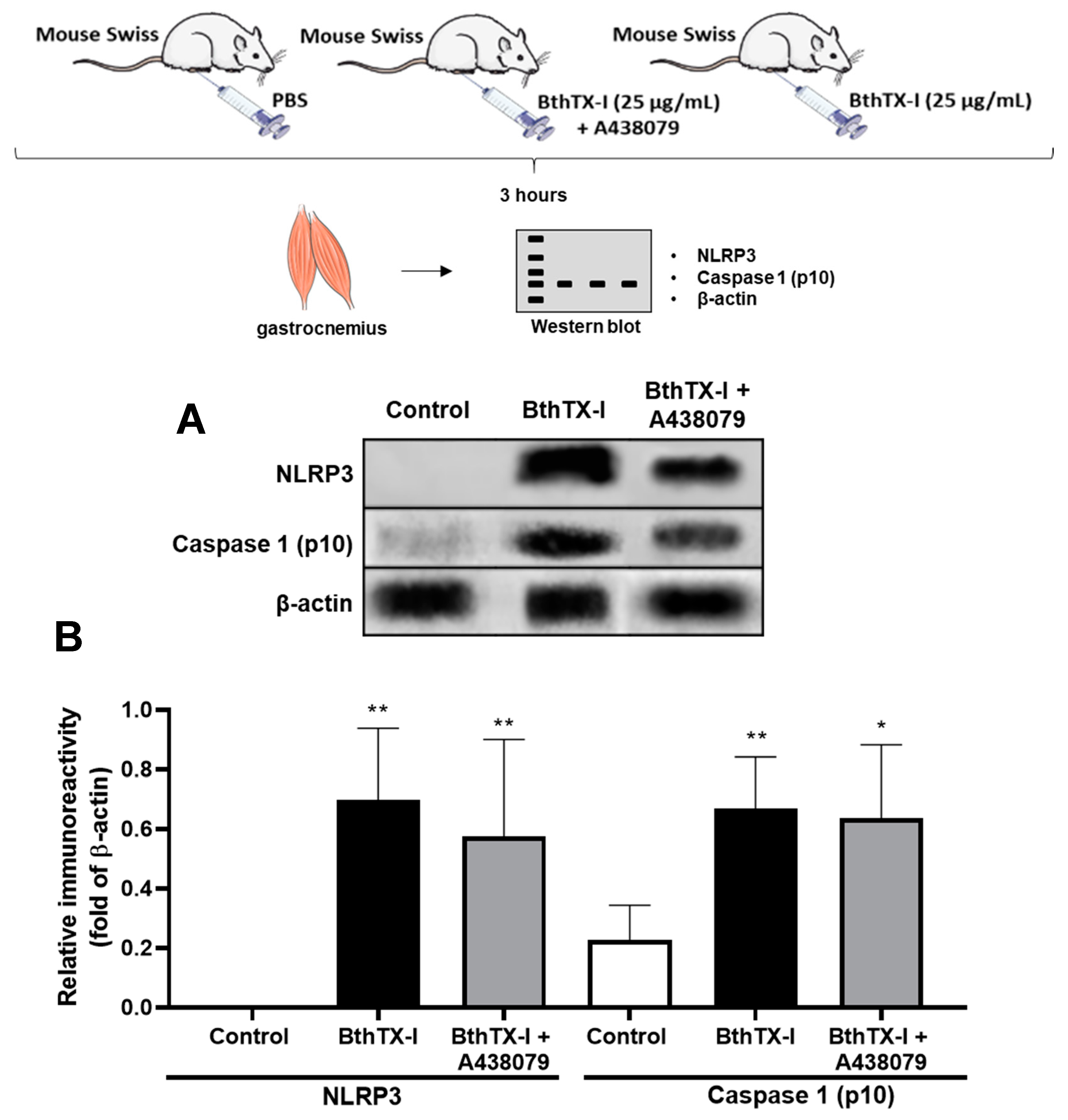
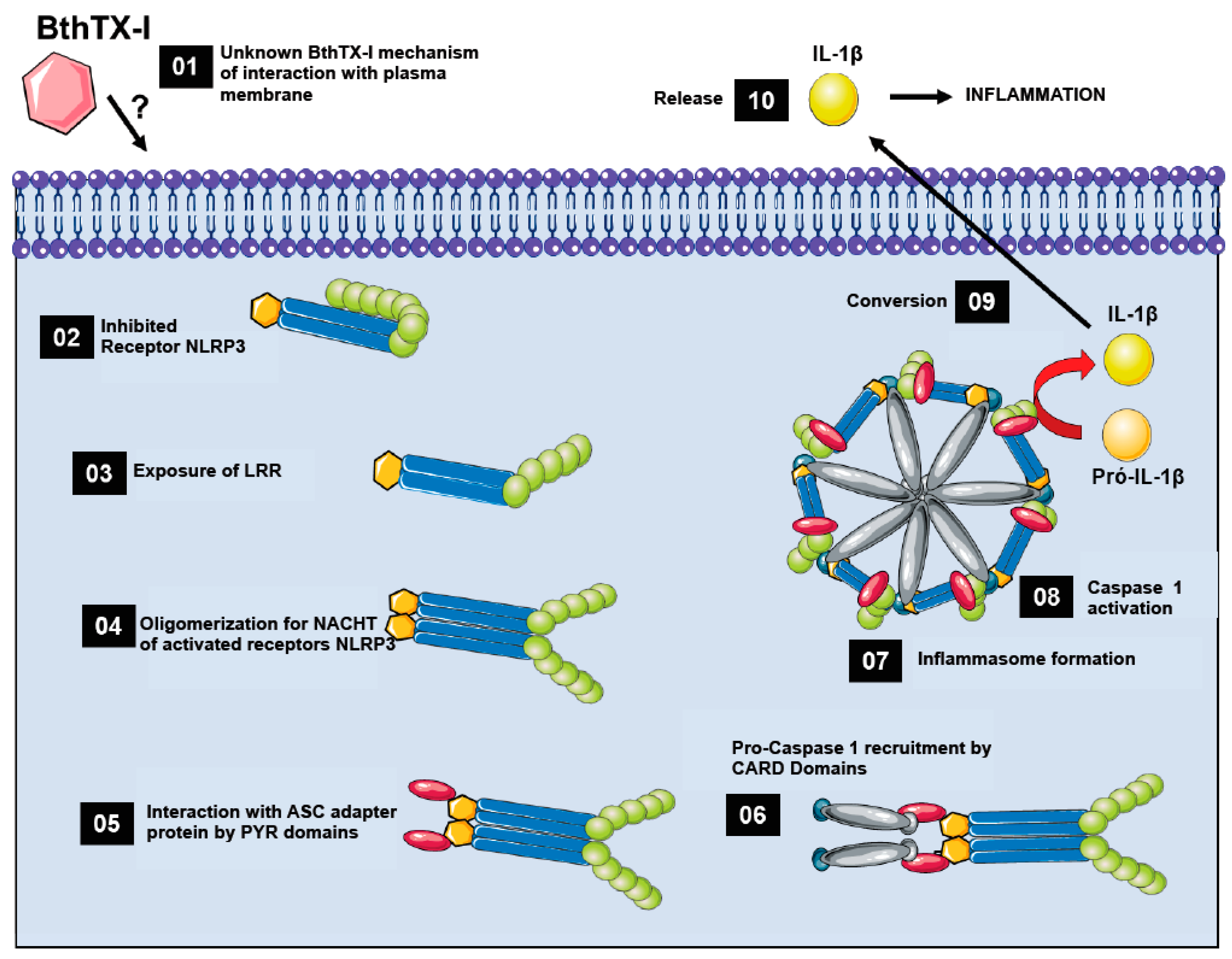
2.4. BthTX-I Induced Inflammasome Activation in Mouse Gastrocnemius Muscle
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Chemicals and Reagents
5.2. Animals
5.3. Phospholipases A2
5.4. Inflammatory and Myotoxic Reactions Induced in Gastrocnemius Muscle by BthTX-I
5.5. Intravital Microscopy of Gastrocnemius Muscle Inoculated with BthTX-I
5.6. Immunoblotting
5.7. Interleukin-1β (IL-1β) Quantification
Pharmacologic Modulation of P2X7 Receptor
5.8. Real-time qRT-PCR
5.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Latz, E.; Xiao, T.S.; Stutz, A. Activation and regulation of the inflammasomes. Nat. Rev. Immunol. 2013, 13, 397–411. [Google Scholar] [CrossRef]
- Pugin, J. How tissue injury alarms the immune system and causes a systemic inflammatory response syndrome. Ann. Intensive Care 2012, 2, 27. [Google Scholar] [CrossRef]
- Piccini, A.; Carta, S.; Tassi, S.; Lasiglié, D.; Fossati, G.; Rubartelli, A. ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1beta and IL-18 secretion in an autocrine way. Proc. Natl. Acad. Sci. USA 2008, 105, 8067–8072. [Google Scholar] [CrossRef] [PubMed]
- Csóka, B.; Németh, Z.H.; Törő, G.; Idzko, M.; Zech, A.; Koscsó, B.; Spolarics, Z.; Antonioli, L.; Cseri, K.; Erdélyi, K.; et al. Extracellular ATP protects against sepsis through macrophage P2X7 purinergic receptors by enhancing intracellular bacterial killing. FASEB J. 2015, 29, 3626–3637. [Google Scholar] [CrossRef] [PubMed]
- Cullen, S.P.; Kearney, C.J.; Clancy, D.M.; Martin, S.J. Diverse Activators of the NLRP3 Inflammasome Promote IL-1β Secretion by Triggering Necrosis. Cell Rep. 2015, 11, 1535–1548. [Google Scholar] [CrossRef] [PubMed]
- Fink, S.L.; Cookson, B.T. Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cell. Microbiol. 2006, 8, 1812–1825. [Google Scholar] [CrossRef]
- Franceschini, A.; Capece, M.; Chiozzi, P.; Falzoni, S.; Sanz, J.M.; Sarti, A.C.; Bonora, M.; Pinton, P.; Di Virgilio, F. The P2X7 receptor directly interacts with the NLRP3 inflammasome scaffold protein. FASEB J. 2015, 29, 2450–2461. [Google Scholar] [CrossRef]
- Idzko, M.; Ferrari, D.; Eltzschig, H.K. Nucleotide signalling during inflammation. Nature 2014, 509, 310–317. [Google Scholar] [CrossRef]
- Pelegrin, P.; Surprenant, A. Pannexin-1 mediates large pore formation and interleukin-1beta release by the ATP-gated P2X7 receptor. EMBO J. 2006, 25, 5071–5082. [Google Scholar] [CrossRef]
- Locovei, S.; Scemes, E.; Qiu, F.; Spray, D.C.; Dahl, G. Pannexin1 is part of the pore forming unit of the P2X(7) receptor death complex. FEBS Lett. 2007, 581, 483–488. [Google Scholar] [CrossRef]
- Yang, D.; He, Y.; Muñoz-Planillo, R.; Liu, Q.; Núñez, G. Caspase-11 Requires the Pannexin-1 Channel and the Purinergic P2X7 Pore to Mediate Pyroptosis and Endotoxic Shock. Immunity 2015, 43, 923–932. [Google Scholar] [CrossRef] [PubMed]
- Grant, R.W.; Dixit, V.D. Mechanisms of disease: Inflammasome activation and the development of type 2 diabetes. Front. Immunol. 2013, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Vandanmagsar, B.; Youm, Y.-H.; Ravussin, A.; Galgani, J.E.; Stadler, K.; Mynatt, R.L.; Ravussin, E.; Stephens, J.M.; Dixit, V.D. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat. Med. 2011, 17, 179–188. [Google Scholar] [CrossRef]
- Cauwels, A.; Rogge, E.; Vandendriessche, B.; Shiva, S.; Brouckaert, P. Extracellular ATP drives systemic inflammation, tissue damage and mortality. Cell Death Dis. 2014, 5, e1102. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, E.; Chiba, P.; Zaky, K. Phospholipases in biology and medicine. Clin. Biochem. 1990, 23, 349–370. [Google Scholar] [CrossRef]
- Kini, R.M.; Zhang, C.Y.; Tan, B.K. Pharmacological activity of the interdomain segment between metalloproteinase and disintegrin domains. Toxicon 1997, 35, 529–535. [Google Scholar] [CrossRef]
- Homsi-Brandeburgo, M.I.; Queiroz, L.S.; Santo-Neto, H.; Rodrigues-Simioni, L.; Giglio, J.R. Fractionation of Bothrops jararacussu snake venom: Partial chemical characterization and biological activity of bothropstoxin. Toxicon 1988, 26, 615–627. [Google Scholar] [CrossRef]
- Moura-da-Silva, A.M.; Cardoso, D.F.; Tanizaki, M.M. Differences in distribution of myotoxic proteins in venoms from different Bothrops species. Toxicon 1990, 28, 1293–1301. [Google Scholar] [CrossRef]
- Kashima, S.; Roberto, P.G.; Soares, A.M.; Astolfi-Filho, S.; Pereira, J.O.; Giuliati, S.; Faria, M.; Xavier, M.A.S.; Fontes, M.R.M.; Giglio, J.R.; et al. Analysis of Bothrops jararacussu venomous gland transcriptome focusing on structural and functional aspects: I—gene expression profile of highly expressed phospholipases A2. Biochimie 2004, 86, 211–219. [Google Scholar] [CrossRef]
- Francis, B.; Gutierrez, J.M.; Lomonte, B.; Kaiser, I.I. Myotoxin II from Bothrops asper (Terciopelo) venom is a lysine-49 phospholipase A2. Arch. Biochem. Biophys. 1991, 284, 352–359. [Google Scholar] [CrossRef]
- Ownby, C.L.; Selistre de Araujo, H.S.; White, S.P.; Fletcher, J.E. Lysine 49 phospholipase A2 proteins. Toxicon 1999, 37, 411–445. [Google Scholar] [CrossRef]
- Lomonte, B.; Angulo, Y.; Calderón, L. An overview of lysine-49 phospholipase A2 myotoxins from crotalid snake venoms and their structural determinants of myotoxic action. Toxicon 2003, 42, 885–901. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Lomonte, B. Phospholipases A2: Unveiling the secrets of a functionally versatile group of snake venom toxins. Toxicon 2013, 62, 27–39. [Google Scholar] [CrossRef]
- Chaves, F.; León, G.; Alvarado, V.H.; Gutiérrez, J.M. Pharmacological modulation of edema induced by Lys-49 and Asp-49 myotoxic phospholipases A2 isolated from the venom of the snake Bothrops asper (terciopelo). Toxicon 1998, 36, 1861–1869. [Google Scholar] [CrossRef]
- Lomonte, B.; Gutiérrez, J.M.; Romero, M.; Núñez, J.; Tarkowski, A.; Hanson, L.A. An MTT-based method for the in vivo quantification of myotoxic activity of snake venoms and its neutralization by antibodies. J. Immunol. Methods 1993, 161, 231–237. [Google Scholar] [CrossRef]
- Zuliani, J.P.; Fernandes, C.M.; Zamuner, S.R.; Gutiérrez, J.M.; Teixeira, C.F.P. Inflammatory events induced by Lys-49 and Asp-49 phospholipases A2 isolated from Bothrops asper snake venom: Role of catalytic activity. Toxicon 2005, 45, 335–346. [Google Scholar] [CrossRef]
- Zuliani, J.P.; Gutiérrez, J.M.; Casais e Silva, L.L.; Coccuzzo Sampaio, S.; Lomonte, B.; de F. Pereira Teixeira, C. Activation of cellular functions in macrophages by venom secretory Asp-49 and Lys-49 phospholipases A(2). Toxicon 2005, 46, 523–532. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Ownby, C.L. Skeletal muscle degeneration induced by venom phospholipases A2: Insights into the mechanisms of local and systemic myotoxicity. Toxicon 2003, 42, 915–931. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Lomonte, B.; León, G.; Alape-Girón, A.; Flores-Díaz, M.; Sanz, L.; Angulo, Y.; Calvete, J.J. Snake venomics and antivenomics: Proteomic tools in the design and control of antivenoms for the treatment of snakebite envenoming. J. Proteom. 2009, 72, 165–182. [Google Scholar] [CrossRef]
- Lomonte, B.; Gutiérrez, J.M. Phospholipases A2 from viperidae snake venoms: How do they induce skeletal muscle damage? Acta Chim. Slov. 2011, 58, 647–659. [Google Scholar]
- Melo, P.A.; Homsi-Brandeburgo, M.I.; Giglio, J.R.; Suarez-Kurtz, G. Antagonism of the myotoxic effects of Bothrops jararacussu venom and bothropstoxin by polyanions. Toxicon 1993, 31, 285–291. [Google Scholar] [CrossRef]
- Veronese, E.L.G.; Esmeraldino, L.E.; Trombone, A.P.F.; Santana, A.E.; Bechara, G.H.; Kettelhut, I.; Cintra, A.C.O.; Giglio, J.R.; Sampaio, S. V Inhibition of the myotoxic activity of Bothrops jararacussu venom and its two major myotoxins, BthTX-I and BthTX-II, by the aqueous extract of Tabernaemontana catharinensis A. DC. (Apocynaceae). Phytomedicine 2005, 12, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.M.; Chaves, F.; Cerdas, L. Inflammatory infiltrate in skeletal muscle injected with Bothrops asper venom. Rev. Biol. Trop. 1986, 34, 209–214. [Google Scholar] [PubMed]
- Teixeira, C.F.P.; Landucci, E.C.T.; Antunes, E.; Chacur, M.; Cury, Y. Inflammatory effects of snake venom myotoxic phospholipases A2. Toxicon 2003, 42, 947–962. [Google Scholar] [CrossRef]
- Kharraz, Y.; Guerra, J.; Mann, C.J.; Serrano, A.L.; Muñoz-Cánoves, P. Macrophage plasticity and the role of inflammation in skeletal muscle repair. Mediat. Inflamm. 2013, 2013, 491497. [Google Scholar] [CrossRef]
- Joosten, L.A.B.; Netea, M.G.; Dinarello, C.A. Interleukin-1β in innate inflammation, autophagy and immunity. Semin. Immunol. 2013, 25, 416–424. [Google Scholar] [CrossRef]
- Barberà-Cremades, M.; Baroja-Mazo, A.; Gomez, A.I.; Machado, F.; Di Virgilio, F.; Pelegrín, P. P2X7 receptor-stimulation causes fever via PGE2 and IL-1β release. FASEB J. 2012, 26, 2951–2962. [Google Scholar] [CrossRef]
- Kurashima, Y.; Kiyono, H.; Kunisawa, J. Pathophysiological role of extracellular purinergic mediators in the control of intestinal inflammation. Mediat. Inflamm. 2015, 2015, 427125. [Google Scholar] [CrossRef]
- Rawat, R.; Cohen, T.V.; Ampong, B.; Francia, D.; Henriques-Pons, A.; Hoffman, E.P.; Nagaraju, K. Inflammasome up-regulation and activation in dysferlin-deficient skeletal muscle. Am. J. Pathol. 2010, 176, 2891–2900. [Google Scholar] [CrossRef]
- Cintra-Francischinelli, M.; Pizzo, P.; Angulo, Y.; Gutiérrez, J.M.; Montecucco, C.; Lomonte, B. The C-terminal region of a Lys49 myotoxin mediates Ca2+ influx in C2C12 myotubes. Toxicon 2010, 55, 590–596. [Google Scholar] [CrossRef]
- Fernandes, C.A.H.; Borges, R.J.; Lomonte, B.; Fontes, M.R.M. A structure-based proposal for a comprehensive myotoxic mechanism of phospholipase A2-like proteins from viperid snake venoms. Biochim. Biophys. Acta 2014, 1844, 2265–2276. [Google Scholar] [CrossRef]
- Montecucco, C.; Gutiérrez, J.M.; Lomonte, B. Cellular pathology induced by snake venom phospholipase A2 myotoxins and neurotoxins: Common aspects of their mechanisms of action. Cell. Mol. Life Sci. 2008, 65, 2897–2912. [Google Scholar] [CrossRef]
- Zhang, C.; Medzihradszky, K.F.; Sánchez, E.E.; Basbaum, A.I.; Julius, D. Lys49 myotoxin from the Brazilian lancehead pit viper elicits pain through regulated ATP release. Proc. Natl. Acad. Sci. USA 2017, 114, E2524–E2532. [Google Scholar] [CrossRef] [PubMed]
- Landucci, E.C.; Castro, R.C.; Pereira, M.F.; Cintra, A.C.; Giglio, J.R.; Marangoni, S.; Oliveira, B.; Cirino, G.; Antunes, E.; De Nucci, G. Mast cell degranulation induced by two phospholipase A2 homologues: Dissociation between enzymatic and biological activities. Eur. J. Pharmacol. 1998, 343, 257–263. [Google Scholar] [CrossRef]
- De Castro, R.C.; Landucci, E.C.; Toyama, M.H.; Giglio, J.R.; Marangoni, S.; De Nucci, G.; Antunes, E. Leucocyte recruitment induced by type II phospholipases A(2) into the rat pleural cavity. Toxicon 2000, 38, 1773–1785. [Google Scholar] [CrossRef]
- Gambero, A.; Landucci, E.C.T.; Toyama, M.H.; Marangoni, S.; Giglio, J.R.; Nader, H.B.; Dietrich, C.P.; De Nucci, G.; Antunes, E. Human neutrophil migration in vitro induced by secretory phospholipases A2: A role for cell surface glycosaminoglycans. Biochem. Pharmacol. 2002, 63, 65–72. [Google Scholar] [CrossRef]
- Gambero, A.; Thomazzi, S.M.; Cintra, A.C.O.; Landucci, E.C.T.; De Nucci, G.; Antunes, E. Signalling pathways regulating human neutrophil migration induced by secretory phospholipases A2. Toxicon 2004, 44, 473–481. [Google Scholar] [CrossRef]
- Reis, P.V.; Tavares, M.N.M.; Rego, A.M.C.; Ferreira e Ferreira, A.A.; Setubal, S.S.; Soares, A.M.; Zamuner, S.R.; Zuliani, J.P. Light emitting diode (LED) photobiomodulation therapy on murine macrophage exposed to Bothropstoxin-I and Bothrostoxin-II myotoxins. Toxicon 2019, 172, 45–52. [Google Scholar] [CrossRef]
- Lamkanfi, M.; Dixit, V.M. Inflammasomes and their roles in health and disease. Annu. Rev. Cell Dev. Biol. 2012, 28, 137–161. [Google Scholar] [CrossRef]
- Lamkanfi, M.; Dixit, V.M. Mechanisms and functions of inflammasomes. Cell 2014, 157, 1013–1022. [Google Scholar] [CrossRef]
- Wen, H.; Miao, E.A.; Ting, J.P.-Y. Mechanisms of NOD-like receptor-associated inflammasome activation. Immunity 2013, 39, 432–441. [Google Scholar] [CrossRef]
- Andrião-Escarso, S.H.; Soares, A.M.; Rodrigues, V.M.; Angulo, Y.; Díaz, C.; Lomonte, B.; Gutiérrez, J.M.; Giglio, J.R. Myotoxic phospholipases A(2) in bothrops snake venoms: Effect of chemical modifications on the enzymatic and pharmacological properties of bothropstoxins from Bothrops jararacussu. Biochimie 2000, 82, 755–763. [Google Scholar] [CrossRef]
- Laemmli, U.K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 1970, 227, 680–685. [Google Scholar] [CrossRef] [PubMed]
- De Souza, C.A.; Kayano, A.M.; Setúbal, S.S.; Pontes, A.S.; Furtado, J.L.; Kwasniewski, F.H.; Zaqueo, K.D.; Soares, A.M.; Stábeli, R.G.; Zuliani, J.P. Local and systemic biochemical alterations induced by Bothrops atrox snake venom in mice. J. Venom Res. 2012, 3, 28–34. [Google Scholar] [PubMed]
- Zanin, R.F.; da Silva, G.L.; Erig, T.; Sperotto, N.D.M.; Leite, C.E.; Coutinho-Silva, R.; Batastini, A.M.O.; Morrone, F.B. Decrease of serum adenine nucleotide hydrolysis in an irritant contact dermatitis mice model: Potential P2X7R involvement. Mol. Cell. Biochem. 2015, 404, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Pontes, A.S.; da, S.; Setúbal, S.; Xavier, C.V.; Lacouth-Silva, F.; Kayano, A.M.; Pires, W.L.; Nery, N.M.; Boeri de Castro, O.; da Silva, S.D.; et al. Effect of l-amino acid oxidase from Calloselasma rhodosthoma snake venom on human neutrophils. Toxicon 2014, 80, 27–37. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative CT method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]

| Gene | Sequence | GenBank | Primer Bank |
|---|---|---|---|
| β-actin | F: GGCTGTATTCCCCTCCATCG R: CCAGTTGGTAACAATGCCATGT | NM_007393 | 6671509a1 |
| ASC | F: CTTGTCAGGGGATGAACTCAAAA R: GCCATACGACTCCAGATAGTAGC | NM_023258 | 31560222a1 |
| Caspase 1 | F: ACAAGGCACGGGACCTATG R: TCCCAGTCAGTCCTGGAAATG | NM_009807 | 6753282a1 |
| IL-1β | F: GCAACTGTTCCTGAACTCAACT R: ATCTTTTGGGGTCCGTCAACT | NM_008361 | 6680415a1 |
| IL-6 | F: TAGTCCTTCCTACCCCAATTTCC R: TTGGTCCTTAGCCACTCCTTC | NM_031168 | 13624311a1 |
| IL-18 | F: GACTCTTGCGTCAACTTCAAGG R: CAGGCTGTCTTTTGTCAACGA | NM_008360 | 6680413a1 |
| NLRP3 | F: ATTACCCGCCCGAGAAAGG R: TCGCAGCAAAGATCCACACAG | NM_145827 | 22003870a1 |
| P2X7R | F: GACAAACAAAGTCACCCGGAT R: CGCTCACCAAAGCAAAGCTAAT | NM_001038845 | 6754964a1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boeno, C.N.; Paloschi, M.V.; Lopes, J.A.; Pires, W.L.; Setúbal, S.d.S.; Evangelista, J.R.; Soares, A.M.; Zuliani, J.P. Inflammasome Activation Induced by a Snake Venom Lys49-Phospholipase A2 Homologue. Toxins 2020, 12, 22. https://doi.org/10.3390/toxins12010022
Boeno CN, Paloschi MV, Lopes JA, Pires WL, Setúbal SdS, Evangelista JR, Soares AM, Zuliani JP. Inflammasome Activation Induced by a Snake Venom Lys49-Phospholipase A2 Homologue. Toxins. 2020; 12(1):22. https://doi.org/10.3390/toxins12010022
Chicago/Turabian StyleBoeno, Charles Nunes, Mauro Valentino Paloschi, Jéssica Amaral Lopes, Weverson Luciano Pires, Sulamita da Silva Setúbal, Jaína Rodrigues Evangelista, Andreimar Martins Soares, and Juliana Pavan Zuliani. 2020. "Inflammasome Activation Induced by a Snake Venom Lys49-Phospholipase A2 Homologue" Toxins 12, no. 1: 22. https://doi.org/10.3390/toxins12010022
APA StyleBoeno, C. N., Paloschi, M. V., Lopes, J. A., Pires, W. L., Setúbal, S. d. S., Evangelista, J. R., Soares, A. M., & Zuliani, J. P. (2020). Inflammasome Activation Induced by a Snake Venom Lys49-Phospholipase A2 Homologue. Toxins, 12(1), 22. https://doi.org/10.3390/toxins12010022







