Vaccine Production to Protect Animals Against Pathogenic Clostridia
Abstract
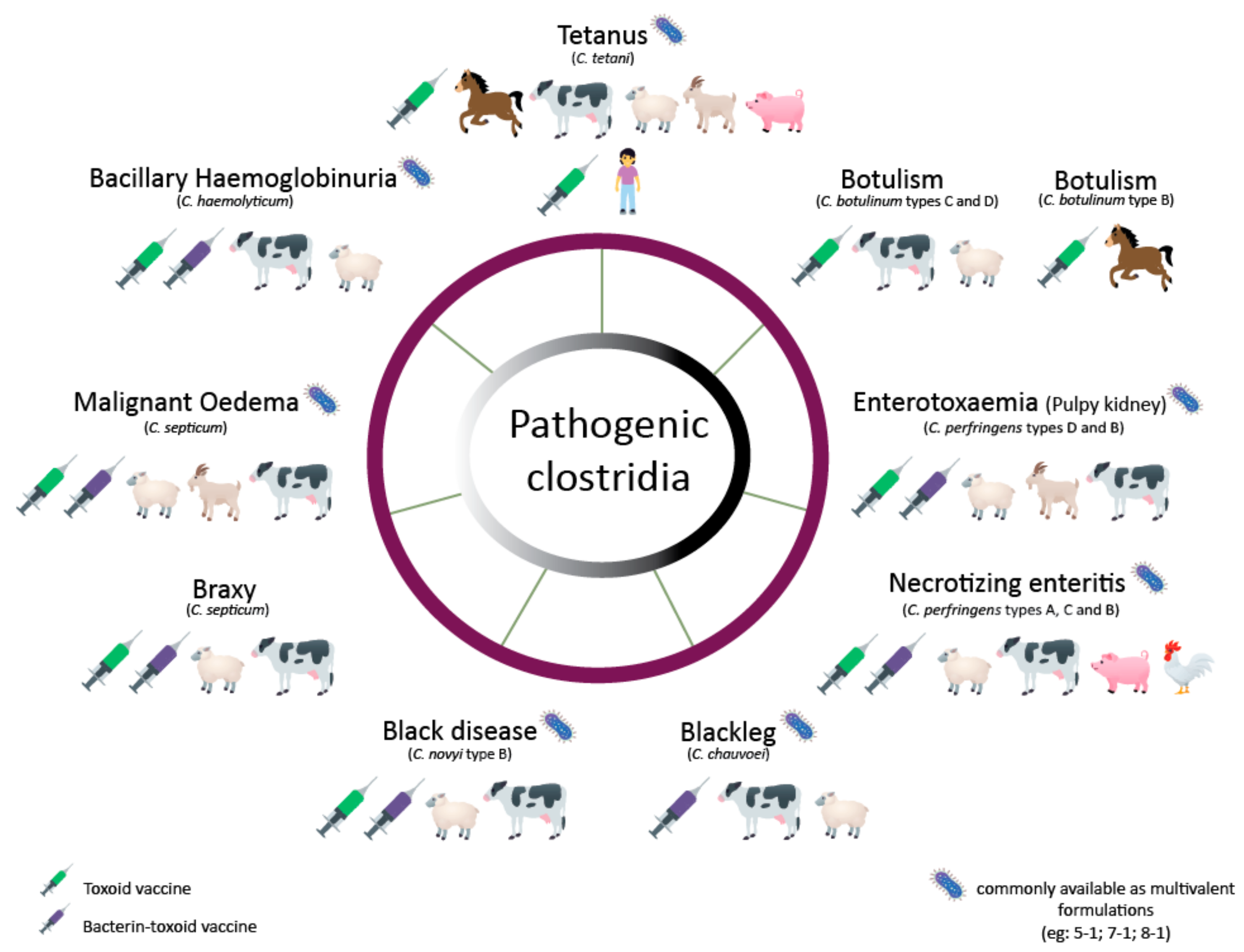
1. Introduction
2. Clostridium botulinum
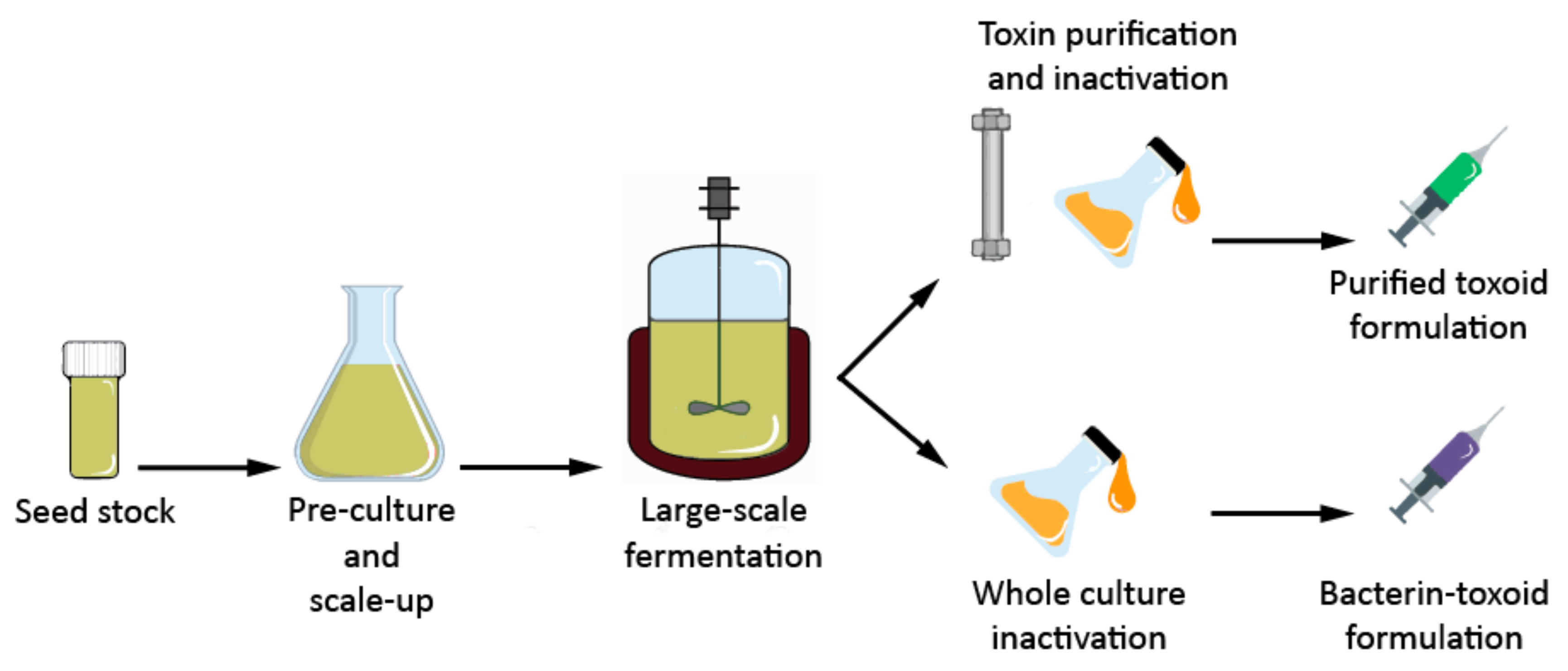
C. botulinum Vaccine Production
3. Clostridium tetani
C. tetani Vaccine Production
4. Clostridium perfringens
4.1. Alpha Toxin (CPA)
4.2. Beta Toxin (CPB)
4.3. Epsilon Toxin (ETX)
4.4. Iota Toxin (ITX)
4.5. C. perfringens Enterotoxin (CPE)
4.6. Necrotic Enteritis Beta-Like Toxin (NetB)
4.7. C. perfringens Vaccines
5. Clostridium chauvoei
C. chauvoei Vaccine Production
6. Clostridium septicum
C. septicum Vaccine Production
7. Clostridium novyi
C. novyi Vaccine Production
8. Clostridium hemolyticum
C. hemolyticum Vaccine Production
9. Concluding Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Cook, T.M.; Protheroe, R.T.; Handel, J.M. Tetanus: A review of the literature. Br. J. Anaesth. 2001, 87, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Lund, B.M. Foodborne disease due to Bacillus and Clostridium species. Lancet 1990, 336, 982–986. [Google Scholar] [CrossRef]
- Stevens, D.L.; Aldape, M.J.; Bryant, A.E. Life-threatening clostridial infections. Anaerobe 2012, 18, 254–259. [Google Scholar] [CrossRef]
- Lotfollahzadeh, S.; Heydari, M.; Mohebbi, M.R.; Hashemian, M. Tetanus outbreak in a sheep flock due to ear tagging. Vet. Med. Sci. 2019, 5, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Wells, C.L.; Balish, E. Clostridium tetani growth and toxin production in the intestines of germfree rats. Infect. Immun. 1983, 41, 826–828. [Google Scholar] [PubMed]
- Uzal, F.A.; Songer, J.G. Diagnosis of Clostridium perfringens intestinal infections in sheep and goats. J. Vet. Diagn. Investig. 2008, 20, 253–265. [Google Scholar] [CrossRef]
- Carter, G.P.; Cheung, J.K.; Larcombe, S.; Lyras, D. Regulation of toxin production in the pathogenic clostridia. Mol. Microbiol. 2014, 91, 221–231. [Google Scholar] [CrossRef]
- Singh, B.R.; Li, B.; Read, D. Botulinum versus tetanus neurotoxins: Why is botulinum neurotoxin but not tetanus neurotoxin a food poison? Toxicon 1995, 33, 1541–1547. [Google Scholar] [CrossRef]
- Kiu, R.; Hall, L.J. An update on the human and animal enteric pathogen Clostridium perfringens. Emerg. Microbes Infect. 2018, 7, 1–15. [Google Scholar] [CrossRef]
- Songer, J.G. Clostridia as agents of zoonotic disease. Vet. Microbiol. 2010, 140, 399–404. [Google Scholar] [CrossRef]
- Borriello, S.P. Clostridial disease of the Gut. Clin. Infect. Dis. 1995, 20, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Songer, J.G. Clostridial enteric diseases of domestic animals. Clin. Microbiol. Rev. 1996, 9, 216–234. [Google Scholar] [CrossRef] [PubMed]
- Hatheway, C.L. Toxigenic clostridia. Clin. Microbiol. Rev. 1990, 3, 66–98. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Tetanus Vaccines: WHO Position Paper, February 2017—Recommendations; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Brynestad, S.; Granum, P.E. Clostridium perfringens and foodborne infections. Int. J. Food Microbiol. 2002, 74, 195–202. [Google Scholar] [CrossRef]
- Rupnik, M.; Wilcox, M.H.; Gerding, D.N. Clostridium difficile infection: New developments in epidemiology and pathogenesis. Nat. Rev. Microbiol. 2009, 7, 526–536. [Google Scholar] [CrossRef] [PubMed]
- Bernard, W.; Divers, T.; Whitlock, R.; Messick, J.; Tulleners, E. Botulism as a sequel to open castration in a horse. J. Am. Vet. Med. Assoc. 1987, 191, 73–74. [Google Scholar] [PubMed]
- Critchley, E.M. A comparison of human and animal botulism: A review. J. R. Soc. Med. 1991, 84, 295–298. [Google Scholar] [CrossRef]
- Heller, H.H. Etiology of acute gangrenous infections of animals: A discussion of blackleg, braxy, malignant edema and whale septicemia. J. Infect. Dis. 1920, 27, 385–451. [Google Scholar] [CrossRef]
- Davies, J.L.; Uzal, F.A.; Whitehead, A.E. Necrotizing hepatitis associated with Clostridium novyi in a pony in western Canada. Can. Vet. J. 2017, 58, 285–288. [Google Scholar]
- Williams, R.B. Intercurrent coccidiosis and necrotic enteritis of chickens: Rational, integrated disease management by maintenance of gut integrity. Avian Pathol. 2005, 34, 159–180. [Google Scholar] [CrossRef]
- Dempster, R. The manufacture of veterinary Clostridial vaccines. Microbiol. Aust. 2015, 36, 120–121. [Google Scholar] [CrossRef]
- Cruz-Morales, P.; Orellana, C.A.; Moutafis, G.; Moonen, G.; Rincon, G.; Nielsen, L.K.; Marcellin, E. Revisiting the evolution and taxonomy of Clostridia, a phylogenomic update. Genome Biol. Evol. 2019, 11, 2035–2044. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.; Williamson, C.H.D.; Hill, K.; Sahl, J.; Keim, P. Botulinum Neurotoxin-Producing Bacteria. Isn’t It Time that We Called a Species a Species? MBio 2018, 9, e01469-18. [Google Scholar] [CrossRef]
- Stringer, S.C.; Carter, A.T.; Webb, M.D.; Wachnicka, E.; Crossman, L.C.; Sebaihia, M.; Peck, M.W. Genomic and physiological variability within Group II (non-proteolytic) Clostridium botulinum. BMC Genom. 2013, 14, 333. [Google Scholar] [CrossRef] [PubMed]
- Carter, A.T.; Peck, M.W. Genomes, neurotoxins and biology of Clostridium botulinum Group I and Group II. Res. Microbiol. 2015, 166, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Skarin, H.; Håfström, T.; Westerberg, J.; Segerman, B. Clostridium botulinum group III: A group with dual identity shaped by plasmids, phages and mobile elements. BMC Genomics 2011, 12, 185. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M.; Korkeala, H. Laboratory diagnostics of botulism. Clin. Microbiol. Rev. 2006, 19, 298–314. [Google Scholar] [CrossRef]
- Maslanka, S.E.; Lúquez, C.; Dykes, J.K.; Tepp, W.H.; Pier, C.L.; Pellett, S.; Raphael, B.H.; Kalb, S.R.; Barr, J.R.; Rao, A.; et al. A novel botulinum neurotoxin, previously reported as Serotype H, has a hybrid-like structure with regions of similarity to the structures of serotypes A and F and is neutralized with Serotype A antitoxin. J. Infect. Dis. 2016, 213, 379–385. [Google Scholar] [CrossRef]
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Henriksson, L.; Miyashita, S.I.; Martínez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef]
- Dover, N.; Barash, J.R.; Hill, K.K.; Xie, G.; Arnon, S.S. Molecular characterization of a novel botulinum neurotoxin type H gene. J. Infect. Dis. 2014, 209, 192–202. [Google Scholar] [CrossRef]
- Sobel, J. Botulism. Clin. Infect. Dis. 2005, 41, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Cagan, E.; Peker, E.; Dogan, M.; Caksen, H. Infant botulism. Eurasian J. Med. 2010, 42, 92–94. [Google Scholar] [CrossRef] [PubMed]
- Woudstra, C.; Skarin, H.; Anniballi, F.; Fenicia, L.; Bano, L.; Drigo, I.; Koene, M.; Bäyon-Auboyer, M.H.; Buffereau, J.P.; De Medici, D.; et al. Neurotoxin gene profiling of Clostridium botulinum types C and D native to different countries within Europe. Appl. Environ. Microbiol. 2012, 78, 3120–3127. [Google Scholar] [CrossRef] [PubMed]
- Steinman, A.; Galon, N.; Arazi, A.; Bar-Giora, Y.; Shpigel, N.Y. Cattle immune response to botulinum type D toxoid: Results of a vaccination study. Vaccine 2007, 25, 7636–7640. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Tighe, A.P.; Schiavo, G. Botulinum neurotoxins: Mechanism of action. Toxicon 2013, 67, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Raffestin, S.; Dupuy, B.; Marvaud, J.C.; Popoff, M.R. BotR/A and TetR are alternative RNA polymerase sigma factors controlling the expression of the neurotoxin and associated protein genes in Clostridium botulinum type A and Clostridium tetani. Mol. Microbiol. 2004, 55, 235–249. [Google Scholar] [CrossRef]
- Cooksley, C.M.; Davis, I.J.; Winzer, K.; Chan, W.C.; Peck, M.W.; Minton, N.P. Regulation of Neurotoxin Production and Sporulation by a Putative agrBD Signaling System in Proteolytic Clostridium botulinum. Appl. Environ. Microbiol. 2010, 76, 4448–4460. [Google Scholar] [CrossRef]
- Zhang, Z.; Korkeala, H.; Dahlsten, E.; Sahala, E.; Heap, J.T.; Minton, N.P.; Lindström, M. Two-Component Signal Transduction System CBO0787/CBO0786 Represses Transcription from Botulinum Neurotoxin Promoters in Clostridium botulinum ATCC 3502. PLoS Pathog. 2013, 9, e1003252. [Google Scholar] [CrossRef]
- Zhang, Z.; Dahlsten, E.; Korkeala, H.; Lindström, M. Positive Regulation of Botulinum Neurotoxin Gene Expression by CodY in Clostridium botulinum ATCC 3502. Appl. Environ. Microbiol. 2014, 80, 7651–7658. [Google Scholar] [CrossRef]
- Smith, L.A. Botulism and vaccines for its prevention. Vaccine 2009, 27, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Sundeen, G.; Barbieri, J.T. Vaccines against Botulism. Toxins 2017, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.A.; Mahon, B.E.; Copeland, J.; Fagan, R.P. Botulism mortality in the USA, 1975-2009. Botulinum J. 2015, 3, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, P.; Chan, E.; Poon, M.; Tu, H.T.H.; Davis, J.M.; Eisen, D.; Marriott, M. Adult food borne botulism in Australia: The only 2 cases from the last 15 years. J. Clin. Neurosci. 2017, 41, 86–87. [Google Scholar] [CrossRef]
- Chen, S. Clinical uses of botulinum neurotoxins: Current indications, limitations and future developments. Toxins 2012, 4, 913–939. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M.; Nevas, M.; Kurki, J.; Sauna-aho, R.; Latvala-Kiesilä, A.; Pölönen, I.; Korkeala, H. Type C Botulism Due to Toxic Feed Affecting 52,000 Farmed Foxes and Minks in Finland. J. Clin. Microbiol. 2004, 42, 4718–4725. [Google Scholar] [CrossRef] [PubMed]
- Espelund, M.; Klaveness, D. Botulism outbreaks in natural environments—An update. Front. Microbiol. 2014, 5, 287. [Google Scholar] [CrossRef] [PubMed]
- Frey, J.; Eberle, S.; Stahl, C.; Mazuet, C.; Popoff, M.; Schatzmann, E.; Gerber, V.; Dungu, B.; Straub, R. Alternative vaccination against equine botulism (BoNT/C). Equine Vet. J. 2007, 39, 516–520. [Google Scholar] [CrossRef]
- Woudstra, C.; Le Maréchal, C.; Souillard, R.; Bayon-Auboyer, M.-H.; Mermoud, I.; Desoutter, D.; Fach, P. New Insights into the Genetic Diversity of Clostridium botulinum Group III through Extensive Genome Exploration. Front. Microbiol. 2016, 7, 757. [Google Scholar] [CrossRef][Green Version]
- Krüger, M.; Skau, M.; Shehata, A.A.; Schrödl, W. Efficacy of Clostridium botulinum types C and D toxoid vaccination in Danish cows. Anaerobe 2013, 23, 97–101. [Google Scholar] [CrossRef]
- Mecitoglu, Z.; Temizel, E.M.; Ozyigit, O.; Akgul, G.; Kennerman, E. Immune response of cattle to botulinum Type C and D toxoid administered on three occasions. Pak. Vet. J. 2015, 25, 7636–7640. [Google Scholar]
- Anniballi, F.; Fiore, A.; Löfström, C.; Skarin, H.; Auricchio, B.; Woudstra, C.; Bano, L.; Segerman, B.; Koene, M.; Båverud, V.; et al. Management of Animal Botulism Outbreaks: From Clinical Suspicion to Practical Countermeasures to Prevent or Minimize Outbreaks. Biosecur. Bioterror. Biodef. Strateg. Pract. Sci. 2013, 11, S191–S199. [Google Scholar] [CrossRef] [PubMed]
- Kodihalli, S.; Emanuel, A.; Takla, T.; Hua, Y.; Hobbs, C.; LeClaire, R.; O’Donnell, D.C. Therapeutic efficacy of equine botulism antitoxin in Rhesus macaques. PLoS ONE 2017, 12, e0186892. [Google Scholar] [CrossRef] [PubMed]
- Donovan, S. Botullinum Toxin Production Method. US7189541B2, 13 March 2007. [Google Scholar]
- Pickett, A. Botulinum Toxin as a Clinical Product: Manufacture and Pharmacology. In Clinical Applications of Botulinum Neurotoxin; Springer: New York, NY, USA, 2014; pp. 7–49. [Google Scholar]
- Siegel, L.S.; Metzger, J.F. Toxin production by Clostridium botulinum type A under various fermentation conditions. Appl. Environ. Microbiol. 1979, 38, 606–611. [Google Scholar] [PubMed]
- Siegel, L.S.; Metzger, J.F. Effect of fermentation conditions on toxin production by Clostridium botulinum type B. Appl. Environ. Microbiol. 1980, 40, 1023–1026. [Google Scholar]
- Keller, J.E. Characterization of new formalin-detoxified botulinum neurotoxin toxoids. Clin. Vaccine Immunol. 2008, 15, 1374–1379. [Google Scholar] [CrossRef] [PubMed]
- Fredrick, C.M.; Lin, G.; Johnson, E.A. Regulation of botulinum neurotoxin synthesis and toxin complex formation by arginine and glucose in Clostridium botulinum ATCC 3502. Appl. Environ. Microbiol. 2017, 83, e00642-17. [Google Scholar] [CrossRef] [PubMed]
- Whitmer, M.E.; Johnson, E.A. Development of improved defined media for Clostridium botulinum serotypes A, B, and E. Appl. Environ. Microbiol. 1988, 54, 753–759. [Google Scholar]
- Strasdine, G.A.; Melville, J. Growth and Spore Production of Clostridium botulinum Type E in Chemically Defined Media. J. Fish. Res. Board Can. 1968, 25, 547–553. [Google Scholar] [CrossRef]
- Zichel, R.; Mimran, A.; Keren, A.; Barnea, A.; Steinberger-Levy, I.; Marcus, D.; Turgeman, A.; Reuveny, S. Efficacy of a potential trivalent vaccine based on Hc fragments of botulinum toxins A, B, and E produced in a cell-free expression system. Clin. Vaccine Immunol. 2010, 17, 784–792. [Google Scholar] [CrossRef]
- Karalewitz, A.P.A.; Barbieri, J.T. Vaccines against botulism. Curr. Opin. Microbiol. 2012, 15, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Brook, I. Current concepts in the management of Clostridium tetani infection. Expert Rev. Anti. Infect. Ther. 2008, 6, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Ergonul, O.; Egeli, D.; Kahyaoglu, B.; Bahar, M.; Etienne, M.; Bleck, T. An unexpected tetanus case. Lancet Infect. Dis. 2016, 16, 746–752. [Google Scholar] [CrossRef]
- Pearce, J.M. Notes on tetanus (lockjaw). J. Neurol. Neurosurg. Psychiatry 1996, 60, 332. [Google Scholar] [CrossRef] [PubMed][Green Version]
- World Health Organization. Tetanus Vaccines: WHO Position Paper—February 2017; World Health Organization: Geneva, Switzerland, 2017; Volume 92. [Google Scholar]
- Bytchenko, B. Geographical Distribution of Tetanus in the World, 1951-1960. Bull. Org. Mond. Sante Bull. 1966, 34, 71–104. [Google Scholar]
- Radjou, A.; Hanifah, M.; Govindaraj, V. Tetanus following dog bite. Indian J. Community Med. 2012, 37, 200–201. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.; White, J.; Ramsay, M.; Amirthalingam, G. The importance of tetanus risk assessment during wound management. IDCases 2015, 2, 3–5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Green, S.L.; Little, C.B.; Baird, J.D.; Tremblay, R.R.M.; Smith-Maxie, L.L. Tetanus in the Horse: A Review of 20 Cases (1970 to 1990). J. Vet. Intern. Med. 1994, 8, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Springer, D.A.; Phillippi-Falkenstein, K.; Smith, G. Retrospective Analysis of Wound Characteristics and Tetanus Development in Captive Macaques. J. Zoo Wildl. Med. 2009, 40, 95–102. [Google Scholar] [CrossRef]
- Wernery, U.; Ul-Haq, A.; Joseph, M.; Kinne, J. Tetanus in a camel (Camelus dromedarius)—A case report. Trop. Anim. Health Prod. 2004, 36, 217–224. [Google Scholar] [CrossRef]
- Popoff, M.R. Ecology of Neurotoxigenic Strains of Clostridia BT—Clostridial Neurotoxins: The Molecular Pathogenesis of Tetanus and Botulism; Montecucco, C., Ed.; Springer: Berlin/Heidelberg, Germany, 1995; pp. 1–29. [Google Scholar]
- Bizzini, B. Tetanus toxin. Microbiol. Rev. 1979, 43, 224–240. [Google Scholar] [PubMed]
- Schiavo, G.G.; Benfenati, F.; Poulain, B.; Rossetto, O.; De Laureto, P.P.; Dasgupta, B.R.; Montecucco, C. Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin. Nature 1992, 359, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Grumelli, C.; Verderio, C.; Pozzi, D.; Rossetto, O.; Montecucco, C.; Matteoli, M. Internalization and mechanism of action of clostridial toxins in neurons. Neurotoxicology 2005, 26, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Pellizzari, R.; Rossetto, O.; Schiavo, G.; Montecucco, C. Tetanus and botulinum neurotoxins: Mechanism of action and therapeutic uses. Philos. Trans. R. Soc. B Biol. Sci. 1999, 354, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Binz, T.; Rummel, A. Cell entry strategy of clostridial neurotoxins. J. Neurochem. 2009, 109, 1584–1595. [Google Scholar] [CrossRef] [PubMed]
- Montecucco, C.; Schiavo, G.; Rossetto, O. The Mechanism of Action of Tetanus and Botulinum Neurotoxins BT—Toxicology—From Cells to Man.; Seiler, J.P., Kroftová, O., Eybl, V., Eds.; Springer: Berlin/Heidelberg, Germany, 1996; pp. 342–354. [Google Scholar]
- Forbes, G.B.; Auld, M. Management of tetanus: Report of fifteen consecutive cases with recovery. Am. J. Med. 1955, 18, 947–960. [Google Scholar] [CrossRef]
- Bruggemann, H.; Baumer, S.; Fricke, W.F.; Wiezer, A.; Liesegang, H.; Decker, I.; Herzberg, C.; Martinez-Arias, R.; Merkl, R.; Henne, A.; et al. The genome sequence of Clostridium tetani, the causative agent of tetanus disease. Proc. Natl. Acad. Sci. USA 2003, 100, 1316–1321. [Google Scholar] [CrossRef]
- Connan, C.; Denève, C.; Mazuet, C.; Popoff, M.R. Regulation of toxin synthesis in Clostridium botulinum and Clostridium tetani. Toxicon 2013, 75, 90–100. [Google Scholar] [CrossRef]
- Marvaud, J.C.; Eisel, U.; Binz, T.; Niemann, H.; Popoff, M.R. TetR is a positive regulator of the tetanus toxin gene in Clostridium tetani and is homologous to BotR. Infect. Immun. 1998, 66, 5698–5702. [Google Scholar]
- Brüggemann, H.; Gottschalk, G. Insights in metabolism and toxin production from the complete genome sequence of Clostridium tetani. Anaerobe 2004, 10, 53–68. [Google Scholar] [CrossRef]
- Saltoglu, N.; Tasova, Y.; Midikli, D.; Burgut, R.; Dündar, I.H. Prognostic factors affecting deaths from adult tetanus. Clin. Microbiol. Infect. 2004, 10, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.G.; Nardi Júnior, G.D.; Megid, J.; Franco, M.M.J.; Guerra, S.T.; Portilho, F.V.R.; Rodrigues, S.A.; Paes, A.C. Tetanus in horses: An overview of 70 cases. Pesqui. Vet. Bras. 2018, 38, 285–293. [Google Scholar] [CrossRef]
- Smith, J.W.G. Diptheria and Tetanus toxoids. Br. Med. Bull. 1969, 25, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Scheibel, I. The uses and results of active tetanus immunization. Bull. World Health Organ. 1955, 13, 381–394. [Google Scholar] [PubMed]
- Licona-Cassani, C.; Steen, J.A.; Zaragoza, N.E.; Moonen, G.; Moutafis, G.; Hodson, M.P.; Power, J.; Nielsen, L.K.; Marcellin, E. Tetanus toxin production is triggered by the transition from amino acid consumption to peptides. Anaerobe 2016, 41, 113–124. [Google Scholar] [CrossRef]
- Brgles, M.; Prebeg, P.; Kurtović, T.; Ranić, J.; Marchetti-Deschmann, M.; Allmaier, G.; Halassy, B. Optimization of tetanus toxoid ammonium sulfate precipitation process using response surface methodology. Prep. Biochem. Biotechnol. 2016, 46, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Thomson, R.O.; Knight, P.; Stephen, J. The Immunopurification of Tetanus Toxoid. J. Appl. Bacteriol. 1974, 37, 603–621. [Google Scholar] [CrossRef]
- Ravetkar, S.D.; Rahalkar, S.B.; Kulkarni, C.G. Large Scale Processing of Tetanus Toxin from Fermentation Broth. J. Sci. Ind. Res. 2001, 60, 773–778. [Google Scholar]
- Muniandi, C.; Mani, K.R.; Subashkumar, R. Large scale recovery of tetanus toxin and toxoid from fermentation broth by microporous tangential flow filtration. Int. J. Biotechnol. Mol. Biol. Res. 2013, 4, 28–37. [Google Scholar]
- Stojićević, I.; Dimitrijević, L.; Dovezenski, N.; Živković, I.; Petrušić, V.; Marinković, E.; Inić-Kanada, A.; Stojanović, M. Tetanus toxoid purification: Chromatographic procedures as an alternative to ammonium-sulphate precipitation. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2011, 879, 2213–2219. [Google Scholar] [CrossRef]
- Mueller, J.H.; Miller, P.A. Variable factors influencing the production of tetanus toxin. J. Bacteriol. 1954, 67, 271–277. [Google Scholar] [PubMed]
- Latham, W.C.; Bent, D.F.; Levine, L. Tetanus toxin production in the absence of protein. Appl. Microbiol. 1962, 10, 146–152. [Google Scholar] [PubMed]
- Mellanby, J. The Effect of Glutamate on Toxin Production by Clostridium tetani. J. Gen. Microbiol. 1968, 54, 77–82. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tsunashima, I.; Sato, K.; Shoji, K.; Yoneda, M.; Amano, T. Excess Supplementation of Certain Amino Acids to Medium and Its Inhibitory Effect on Toxin Production by Clostridium Tetani. Biken J. 1964, 7, 161–163. [Google Scholar] [PubMed]
- Miller, P.A.; Mueller, J.H. Essential role of histidine peptides in tetanus toxin production. J. Biol. Chem. 1956, 223, 185–194. [Google Scholar] [PubMed]
- Porfírio, Z.; Prado, S.M.; Vancetto, M.D.C.; Fratelli, F.; Alves, E.W.; Raw, I.; Fernandes, B.L.; Camargo, A.C.M.; Lebrun, I. Specific peptides of casein pancreatic digestion enhance the production of tetanus toxin. J. Appl. Microbiol. 1997, 83, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Demain, A.L.; Gerson, D.F.; Fang, A. Effective levels of tetanus toxin can be made in a production medium totally lacking both animal (e.g., brain heart infusion) and dairy proteins or digests (e.g., casein hydrolysates). Vaccine 2005, 23, 5420–5423. [Google Scholar] [CrossRef] [PubMed]
- Demain, A.L.; George, S.; Kole, M.; Gerson, D.F.; Fang, A. Tetanus toxin production in soy-based medium: Nutritional studies and scale-up into small fermentors. Lett. Appl. Microbiol. 2007, 45, 635–638. [Google Scholar] [CrossRef]
- Chung, Y.J.; Jung, M.Y.; Lee, J.A.; Kim, T.Y.; Choe, Y.K.; Kim, I.H. Tetanus toxin production from Clostridium tetani, using a casein-based medium in a single-use bioreactor. Biotechnol. Bioprocess Eng. 2016, 21, 531–536. [Google Scholar] [CrossRef]
- Fratelli, F.; Siquini, T.J.; de Abreu, M.E.; Higashi, H.G.; Converti, A.; de Carvalho, J.C.M. Fed-batch production of tetanus toxin by Clostridium tetani. Biotechnol. Prog. 2010, 26, 88–92. [Google Scholar]
- Zacharias, B.; Björklund, M. Continuous production of Clostridium tetani toxin. Appl. Microbiol. 1968, 16, 69–72. [Google Scholar] [PubMed]
- Koch, W.; Kaplan, D. A simple method for obtaining highly potent tetanus toxin. J. Immunol. 1953, 70, 1–5. [Google Scholar] [PubMed]
- Feeney, R.E.; Mueller, J.H.; Miller, P.A. Growth requirements of clostridium tetani: II. Factors exhausted by growth of the organism. J. Bacteriol. 1943, 46, 559–562. [Google Scholar] [PubMed]
- Villarreal-Ramos, B.; Manser, J.M.; Collins, R.A.; Dougan, G.; Howard, C.J. Cattle immune responses to tetanus toxoid elicited by recombinant S. typhimurium vaccines or tetanus toxoid in alum or Freund’s adjuvant. Vaccine 2000, 18, 1515–1521. [Google Scholar] [CrossRef]
- Yu, R.; Ji, C.; Xu, J.; Wang, D.; Fang, T.; Jing, Y.; Kwang-Fu Shen, C.; Chen, W. The Immunogenicity of the C Fragment of Tetanus Neurotoxin in Production of Tetanus Antitoxin. Biomed Res. Int. 2018. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Hou, L.; Yu, C.; Liu, S.; Ren, J.; Fang, T.; Zhang, X.; Chen, W. Enhanced expression of soluble recombinant tetanus neurotoxin Hc in Escherichia coli as a tetanus vaccine candidate. Immunobiology 2011, 216, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Fang, T.; Liu, S.; Song, X.; Yu, C.; Li, J.; Fu, L.; Hou, L.; Xu, J.; Chen, W. Comparative immunogenicity of the tetanus toxoid and recombinant tetanus vaccines in mice, rats, and cynomolgus monkeys. Toxins 2016, 8, 194. [Google Scholar] [CrossRef]
- Johnston, L.; Mawas, F.; Tierney, R.; Qazi, O.; Fairweather, N.; Sesardic, D. Transcutaneous delivery of tetanus toxin Hc fragment induces superior tetanus toxin neutralizing antibody response compared to tetanus toxoid. Hum. Vaccin. 2009, 5, 230–236. [Google Scholar] [CrossRef]
- Tierney, R.; Nakai, T.; Parkins, C.J.; Caposio, P.; Fairweather, N.F.; Sesardic, D.; Jarvis, M.A. A single-dose cytomegalovirus-based vaccine encoding tetanus toxin fragment C induces sustained levels of protective tetanus toxin antibodies in mice. Vaccine 2012, 30, 3047–3052. [Google Scholar] [CrossRef]
- Freedman, J.C.; Theoret, J.R.; Wisniewski, J.A.; Uzal, F.A.; Rood, J.I.; McClane, B.A. Clostridium perfringens type A-E toxin plasmids. Res. Microbiol. 2015, 166, 264–279. [Google Scholar] [CrossRef]
- Li, J.; Uzal, F.A.; McClane, B.A. Clostridium perfringens sialidases: Potential contributors to intestinal pathogenesis and therapeutic targets. Toxins 2016, 8, 341. [Google Scholar] [CrossRef] [PubMed]
- Uzal, F.A. Clostridium Perfringens Toxins Involved in Mammalian Veterinary Diseases. Open Toxinol. J. 2010, 2, 24–42. [Google Scholar] [CrossRef] [PubMed]
- Niilo, L. Clostridium perfringens in animal disease: A review of current knowledge. Can. Vet. J. 1980, 21, 141–148. [Google Scholar] [PubMed]
- Lee, H.L.; Cho, S.Y.; Lee, D.G.; Ko, Y.; Hyun, J.I.; Kim, B.K.; Seo, J.H.; Lee, J.W.; Lee, S. A fatal spontaneous gas gangrene due to Clostridium perfringens during neutropenia of allogeneic stem cell transplantation: Case report and literature review. Infect. Chemother. 2014, 46, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Bryant, A.E.; Stevens, D.L. Clostridial myonecrosis: New insights in pathogenesis and management. Curr. Infect. Dis. Rep. 2010, 12, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Goossens, E.; Verherstraeten, S.; Timbermont, L.; Valgaeren, B.R.; Pardon, B.; Haesebrouck, F.; Ducatelle, R.; Deprez, P.R.; Van Immerseel, F. Clostridium perfringens strains from bovine enterotoxemia cases are not superior in in vitro production of alpha toxin, perfringolysin O and proteolytic enzymes. BMC Vet. Res. 2014, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Keyburn, A.L.; Sheedy, S.A.; Ford, M.E.; Williamson, M.M.; Awad, M.M.; Rood, J.I.; Moore, R.J. Alpha-Toxin of Clostridium perfringens Is Not an Essential Virulence Factor in Necrotic Enteritis in Chickens. Infect. Immun. 2006, 74, 6496. [Google Scholar] [CrossRef] [PubMed]
- Keyburn, A.L.; Boyce, J.D.; Vaz, P.; Bannam, T.L.; Ford, M.E.; Parker, D.; Di Rubbo, A.; Rood, J.I.; Moore, R.J. NetB, a new toxin that is associated with avian necrotic enteritis caused by Clostridium perfringens. PLoS Pathog. 2008, 4, e26. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Miyakawa, M.E.; Fisher, D.J.; Poon, R.; Sayeed, S.; Adams, V.; Rood, J.I.; McClane, B.A.; Uzal, F.A. Both epsilon-toxin and beta-toxin are important for the lethal properties of Clostridium perfringens type B isolates in the mouse intravenous injection model. Infect. Immun. 2007, 75, 1443–1452. [Google Scholar] [CrossRef]
- Clarke, L.E.; Diekmann-Guiroy, B.; McNamee, W.; Java, D.J., Jr.; Weiss, S.M. Enteritis Necroticans with Midgut Necrosis Caused by Clostridium perfringens. JAMA Surg. 1994, 129, 557–560. [Google Scholar] [CrossRef]
- Nagahama, M.; Ochi, S.; Oda, M.; Miyamoto, K.; Takehara, M.; Kobayashi, K. Recent insights into Clostridium perfringens beta-toxin. Toxins 2015, 7, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Miclard, J.; Van Baarlen, J.; Wyder, M.; Grabscheid, B.; Posthaus, H. Clostridium perfringens β-toxin binding to vascular endothelial cells in a human case of enteritis necroticans. J. Med. Microbiol. 2009, 59, 826–828. [Google Scholar] [CrossRef] [PubMed]
- Uzal, F.A.; Freedman, J.C.; Shrestha, A.; Theoret, J.R.; Garcia, J.; Awad, M.M.; Adams, V.; Moore, R.J.; Rood, J.I.; Mcclane, B.A. Towards an understanding of the role of Clostridium perfringens toxins in human and animal disease. Future Microbiol. 2014, 9, 361–377. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.J.; Fernandez-Miyakawa, M.E.; Sayeed, S.; Poon, R.; Adams, V.; Rood, J.I.; Uzal, F.A.; McClane, B.A. Dissecting the contributions of Clostridium perfringens type C toxins to lethality in the mouse intravenous injection model. Infect. Immun. 2006, 74, 5200–5210. [Google Scholar] [CrossRef] [PubMed]
- Gui, L.; Subramony, C.; Fratkin, J.; Hughson, M.D. Fatal enteritis necroticans (Pigbel) in a diabetic adult. Mod. Pathol. 2002, 15, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Niilo, L. Clostridium perfringens Type C Enterotoxemia. Can. Vet. J. 1988, 29, 658–664. [Google Scholar]
- Garcia, J.P.; Adams, V.; Beingesser, J.; Hughes, M.L.; Poon, R.; Lyras, D.; Hill, A.; McClane, B.A.; Rood, J.I.; Uzal, F.A. Epsilon Toxin Is Essential for the Virulence of Clostridium perfringens Type D Infection in Sheep, Goats, and Mice. Infect. Immun. 2013, 81, 2405–2414. [Google Scholar] [CrossRef] [PubMed]
- Alves, G.G.; de Ávila, R.A.M.; Chávez-Olórtegui, C.D.; Lobato, F.C.F. Clostridium perfringens epsilon toxin: The third most potent bacterial toxin known. Anaerobe 2014, 30, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Berger, T.; Eisenkraft, A.; Bar-Haim, E.; Kassirer, M.; Aran, A.A.; Fogel, I. Toxins as biological weapons for terror—Characteristics, challenges and medical countermeasures: A mini-review. Disaster Mil. Med. 2016, 2, 7. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Kim, S.; Oh, J.Y.; Kim, H.R.; Jang, I.; Lee, H.S.; Kwon, Y.K. Characterization of Clostridium perfringens isolates obtained from 2010 to 2012 from chickens with necrotic enteritis in Korea. Poult. Sci. 2015, 94, 1158–1164. [Google Scholar] [CrossRef] [PubMed]
- Popoff, M.R. Epsilon toxin: A fascinating pore-forming toxin. FEBS J. 2011, 278, 4602–4615. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, J.; Nagahama, M.; Oda, M.; Tsuge, H.; Kobayashi, K. Clostridium perfringens iota-toxin: Structure and function. Toxins 2009, 1, 208–228. [Google Scholar] [CrossRef] [PubMed]
- Gibert, M.; Petit, L.; Raffestin, S.; Okabe, A.; Popoff, M.R. Clostridium perfringens iota-toxin requires activation of both binding and enzymatic components for cytopathic activity. Infect. Immun. 2000, 68, 3848–3853. [Google Scholar] [CrossRef] [PubMed]
- Takehara, M.; Takagishi, T.; Seike, S.; Oda, M.; Sakaguchi, Y.; Hisatsune, J.; Ochi, S.; Kobayashi, K.; Nagahama, M. Cellular Entry of Clostridium perfringens Iota-Toxin and Clostridium botulinum C2 Toxin. Toxins 2017, 9, 247. [Google Scholar] [CrossRef] [PubMed]
- Stiles, B.G.; Hale, M.L.; Marvaud, J.C.; Popoff, M.R. Clostridium perfringens iota toxin: Binding studies and characterization of cell surface receptor by fluorescence-activated cytometry. Infect. Immun. 2000, 68, 3475–3484. [Google Scholar] [CrossRef]
- Redondo, L.M.; Carrasco, J.M.D.; Redondo, E.A.; Delgado, F.; Fernández Miyakawa, M.E. Clostridium perfringens type E virulence traits involved in gut colonization. PLoS ONE 2015, 10, e0121305. [Google Scholar] [CrossRef] [PubMed]
- Songer, J.G.; Miskimmins, D.W. Clostridium perfringens type E enteritis in calves: Two cases and a brief review of the literature. Anaerobe 2004, 10, 239–242. [Google Scholar] [CrossRef]
- Lindström, M.; Heikinheimo, A.; Lahti, P.; Korkeala, H. Novel insights into the epidemiology of Clostridium perfringens type A food poisoning. Food Microbiol. 2011, 28, 192–198. [Google Scholar] [CrossRef]
- Grass, J.E.; Gould, L.H.; Mahon, B.E. Epidemiology of Foodborne Disease Outbreaks Caused by Clostridium perfringens, United States, 1998–2010. Foodborne Pathog. Dis. 2013, 10, 131–136. [Google Scholar] [CrossRef]
- Freedman, J.C.; Shrestha, A.; McClane, B.A. Clostridium perfringens enterotoxin: Action, genetics, and translational applications. Toxins 2016, 8, 73. [Google Scholar] [CrossRef]
- Yan, X.X.; Porter, C.J.; Hardy, S.P.; Steer, D.; Ian Smith, A.; Quinsey, N.S.; Hughes, V.; Cheung, J.K.; Keyburn, A.L.; Kaldhusdal, M.; et al. Structural and functional analysis of the pore-forming toxin NetB from clostridium perfringens. MBio 2013, 4, e00019-13. [Google Scholar] [CrossRef] [PubMed]
- Rood, J.I.; Keyburn, A.L.; Moore, R.J. NetB and necrotic enteritis: The hole movable story. Avian Pathol. 2016, 45, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Zahoor, I.; Ghayas, A.; Basheer, A. Genetics and genomics of susceptibility and immune response to necrotic enteritis in chicken: A review. Mol. Biol. Rep. 2018, 45, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Paiva, D.; McElroy, A. Necrotic enteritis: Applications for the poultry industry. J. Appl. Poult. Res. 2014, 23, 557–566. [Google Scholar] [CrossRef]
- Moore, R.J. Necrotic enteritis predisposing factors in broiler chickens. Avian Pathol. 2016, 45, 275–281. [Google Scholar] [CrossRef] [PubMed]
- To, H.; Suzuki, T.; Kawahara, F.; Uetsuka, K.; Nagai, S.; Nunoya, T. Experimental induction of necrotic enteritis in chickens by a netB-positive Japanese isolate of Clostridium perfringens. J. Vet. Med. Sci. 2016, 79, 350–358. [Google Scholar] [CrossRef]
- Timbermont, L.; Haesebrouck, F.; Ducatelle, R.; Van Immerseel, F. Necrotic enteritis in broilers: An updated review on the pathogenesis. Avian Pathol. 2011, 40, 341–347. [Google Scholar] [CrossRef]
- Wang, H.; Ni, X.; Qing, X.; Liu, L.; Lai, J.; Khalique, A.; Li, G.; Pan, K.; Jing, B.; Zeng, D. Probiotic enhanced intestinal immunity in broilers against subclinical necrotic enteritis. Front. Immunol. 2017, 8, 1592. [Google Scholar] [CrossRef]
- Caly, D.L.; D’Inca, R.; Auclair, E.; Drider, D. Alternatives to antibiotics to prevent necrotic enteritis in broiler chickens: A microbiologist’s perspective. Front. Microbiol. 2015, 6, 1336. [Google Scholar] [CrossRef]
- Mot, D.; Timbermont, L.; Haesebrouck, F.; Ducatelle, R.; Van Immerseel, F. Progress and problems in vaccination against necrotic enteritis in broiler chickens. Avian Pathol. 2014, 43, 290–300. [Google Scholar] [CrossRef]
- Viana Brandi, I.; Domenici Mozzer, O.; Vander Jorge, E.; Vieira Passos, F.J.; Lopes Passos, F.M.; Cangussu, A.S.R.; Macedo Sobrinho, E. Growth conditions of clostridium perfringens type B for production of toxins used to obtain veterinary vaccines. Bioprocess Biosyst. Eng. 2014, 37, 1737–1742. [Google Scholar] [CrossRef]
- Moreira, G.M.S.G.; Salvarani, F.M.; Da Cunha, C.E.P.; Mendonça, M.; Moreira, Â.N.; Gonçalves, L.A.; Pires, P.S.; Lobato, F.C.F.; Conceição, F.R. Immunogenicity of a Trivalent Recombinant Vaccine Against Clostridium perfringens Alpha, Beta, and Epsilon Toxins in Farm Ruminants. Sci. Rep. 2016, 23, 22816. [Google Scholar] [CrossRef]
- Goossens, E.; Verherstraeten, S.; Valgaeren, B.R.; Pardon, B.; Timbermont, L.; Schauvliege, S.; Rodrigo-Mocholí, D.; Haesebrouck, F.; Ducatelle, R.; Deprez, P.R.; et al. The C-terminal domain of Clostridium perfringens alpha toxin as a vaccine candidate against bovine necrohemorrhagic enteritis. Vet. Res. 2016, 47, 52. [Google Scholar] [CrossRef]
- Titball, R.W. Clostridium perfringens vaccines. Vaccine 2009, 27, D44–D47. [Google Scholar] [CrossRef]
- Duke, T.; Poka, H.; Myers, S.; Radcliffe, J.; Pavlin, B.I. Pigbel in the 21st century: Still here, and still in need of an effective surveillance system. PNG Med J 2013, 56, 136–140. [Google Scholar]
- Kennedy, K.K.; Norris, S.J.; Beckenhauer, W.H.; White, R.G. Vaccination of cattle and sheep with a combined Clostridium perfringens types C and D toxoid. Am. J. Vet. Res. 1977, 38, 1515–1517. [Google Scholar]
- Schäfer, K.; Wyder, M.; Gobeli, S.; Candi, A.; Doherr, M.G.; Zehnder, B.; Zimmermann, W.; Posthaus, H. Detection of Clostridium perfringens type C in pig herds following disease outbreak and subsequent vaccination. Vet. Rec. 2012, 171, 503. [Google Scholar] [CrossRef]
- Springer, S.; Selbitz, H.J. The control of necrotic enteritis in sucking piglets by means of a Clostridium perfringens toxoid vaccine. FEMS Immunol. Med. Microbiol. 1999, 24, 333–336. [Google Scholar] [CrossRef]
- Uzal, F.A.; Wong, J.P.; Kelly, W.R.; Priest, J. Antibody response in goats vaccinated with liposome-adjuvanted Clostridium perfringens type D epsilon toxoid. Vet. Res. Commun. 1999, 23, 143–150. [Google Scholar] [CrossRef]
- Giri, B.; Kole, L. Combating the Perilous Consequence of Clostridial Gas Gangrene: An Overview. Toxinology 2014. [Google Scholar] [CrossRef]
- Fernandes da Costa, S.P.; Mot, D.; Geeraerts, S.; Bokori-Brown, M.; Van Immerseel, F.; Titball, R.W. Variable protection against experimental broiler necrotic enteritis after immunization with the C-terminal fragment of Clostridium perfringens alpha-toxin and a non-toxic NetB variant. Avian Pathol. 2016, 45, 381–388. [Google Scholar] [CrossRef]
- Boyd, M.J.; Logan, M.A.; Tytell, A.A. The growth requirements of Clostridium perfringens (welchii) BP6K. J. Biol. Chem. 1948, 174, 1013–1025. [Google Scholar]
- Goldner, S.B.; Solberg, M.; Post, L.S. Development of a minimal medium for Clostridium perfringens by using an anaerobic chemostat. Appl. Environ. Microbiol. 1985, 50, 202–206. [Google Scholar]
- Nakamura, M.; Cook, J.A.; Cross2, W.R. Lecithinase Production by Clostridium perfringens in Chemically Defined Media. Appl. Microbiol. 1968, 16, 1420–1421. [Google Scholar]
- Fernandez-Miyakawa, M.E.; Marcellino, R.; Uzal, F.A. Clostridium Perfringens type A Toxin Production in 3 Commonly Used Culture Media. J. Vet. Diagn. Investig. 2007, 19, 184–186. [Google Scholar] [CrossRef]
- Murata, R.; Yamamoto, A.; Soda, S.; Ito, A. Nutritional requirements of clostridium perfringens pb6k for alpha toxin production. Jpn. J. Med. Sci. Biol. 1965, 18, 189–202. [Google Scholar] [CrossRef]
- Chou, G. Medium for toxin production by Clostridium perfringens in continuous culture. Appl. Microbiol. 1971, 21, 794–798. [Google Scholar]
- Pivnick, H.; Habeeb, A.F.S.A.; Gorenstein, B.; Stuart, P.F.; Hauschild, A.H.W. Effect of ph on toxinogenesis by clostridium perfringens type C. Can. J. Microbiol. 1964, 10, 329–344. [Google Scholar] [CrossRef]
- Duncan, C.L. Effect of Carbohydrates and Control of Culture pH on Beta Toxin Production by Clostridium perfringens Type C. Microbiol. Immunol. 1979, 23, 313–318. [Google Scholar]
- Hauschild, A.H.W.; Pivnick, H. Effect of carbohydrates on toxinogenesis by clostridium perfringens type D. Can. J. Microbiol. 1965, 11, 15–22. [Google Scholar] [CrossRef]
- Ohtani, K.; Shimizu, T. Regulation of toxin production in clostridium perfringens. Toxins 2016, 8, 207. [Google Scholar] [CrossRef]
- Ma, M.; Vidal, J.; Saputo, J.; McClane, B.A.; Uzal, F. The VirS/VirR two-component system regulates the anaerobic cytotoxicity, intestinal pathogenicity, and enterotoxemic lethality of Clostridium perfringens type C isolate CN3685. MBio 2011, 2, e00338-10. [Google Scholar] [CrossRef]
- Chen, J.; Ma, M.; Uzal, F.A.; McClane, B.A. Host cell-induced signaling causes Clostridium perfringens to upregulate production of toxins important for intestinal infections. Gut Microbes 2014, 5, 96–107. [Google Scholar] [CrossRef]
- Yu, Q.; Lepp, D.; Gohari, I.M.; Wu, T.; Zhou, H.; Yin, X.; Yu, H.; Prescott, J.F.; Nie, S.P.; Xie, M.Y.; et al. The Agr-like quorum sensing system is required for pathogenesis of necrotic enteritis caused by Clostridium perfringens in poultry. Infect. Immun. 2017, 85, e00975-16. [Google Scholar] [CrossRef]
- Lyristis, M.; Bryant, A.E.; Sloan, J.; Awad, M.M.; Nisbet, I.T.; Stevens, D.L.; Rood, J.I. Identification and molecular analysis of a locus that regulates extracellular toxin production in Clostridium perfringens. Mol. Microbiol. 1994, 12, 761–777. [Google Scholar] [CrossRef]
- Chen, J.; Rood, J.I.; McClane, B.A. Epsilon-Toxin Production by Clostridium perfringens Type D Strain CN3718 Is Dependent upon the Operon but Not the VirS/VirR Two-Component Regulatory System. MBio 2011, 2, e00275-11. [Google Scholar] [CrossRef]
- Lobato, F.C.F.; Lima, C.G.R.D.; Assis, R.A.; Pires, P.S.; Silva, R.O.S.; Salvarani, F.M.; Carmo, A.O.; Contigli, C.; Kalapothakis, E. Potency against enterotoxemia of a recombinant Clostridium perfringens type D epsilon toxoid in ruminants. Vaccine 2010, 28, 6125–6127. [Google Scholar] [CrossRef]
- Pilehchian Langroudi, R.; Shamsara, M.; Aghaiypour, K. Expression of Clostridium perfringens epsilon-beta fusion toxin gene in E. coli and its immunologic studies in mouse. Vaccine 2013, 31, 3295–3299. [Google Scholar] [CrossRef]
- Hosomi, K.; Hinenoya, A.; Suzuki, H.; Nagatake, T.; Nishino, T.; Tojima, Y.; Hirata, S.I.; Matsunaga, A.; Kondoh, M.; Yamasaki, S.; et al. Development of a bivalent food poisoning vaccine: Augmented antigenicity of the C-terminus of Clostridium perfringens enterotoxin by fusion with the B subunit of Escherichia coli Shiga toxin 2. Int. Immunol. 2019, 31, 91–100. [Google Scholar] [CrossRef]
- Williamson, E.D.; Titball, R.W. A genetically engineered vaccine against the alpha-toxin of Clostridium perfringens protects mice against experimental gas gangrene. Vaccine 1993, 11, 1253–1258. [Google Scholar] [CrossRef]
- Nagahama, M.; Oda, M.; Kobayashi, K.; Ochi, S.; Takagishi, T.; Shibutani, M.; Sakurai, J. A recombinant carboxy-terminal domain of alpha-toxin protects mice against Clostridium perfringens. Microbiol. Immunol. 2013, 57, 340–345. [Google Scholar] [CrossRef]
- Cooper, K.K.; Trinh, H.T.; Songer, J.G. Immunization with recombinant alpha toxin partially protects broiler chicks against experimental challenge with Clostridium perfringens. Vet. Microbiol. 2009, 133, 92–97. [Google Scholar] [CrossRef]
- Salvarani, F.M.; Conceição, F.R.; Cunha, C.E.P.; Moreira, G.M.S.G.; Pires, P.S.; Silva, R.O.S.; Alves, G.G.; Lobato, F.C.F. Vaccination with recombinant Clostridium perfringens toxoids α and β promotes elevated antepartum and passive humoral immunity in swine. Vaccine 2013, 31, 4152–4155. [Google Scholar] [CrossRef]
- Keyburn, A.L.; Portela, R.W.; Sproat, K.; Ford, M.E.; Bannam, T.L.; Yan, X.; Rood, J.I.; Moore, R.J. Vaccination with recombinant NetB toxin partially protects broiler chickens from necrotic enteritis. Vet. Res. 2013, 44, 54. [Google Scholar] [CrossRef]
- Ferreira, M.R.A.; Moreira, G.M.S.G.; Da Cunha, C.E.P.; Mendonça, M.; Salvarani, F.M.; Moreira, Â.N.; Conceição, F.R. Recombinant Alpha, Beta, and Epsilon toxins of Clostridium perfringens: Production strategies and applications as veterinary vaccines. Toxins 2016, 8, 340. [Google Scholar] [CrossRef]
- Abreu, C.C.; Edwards, E.E.; Edwards, J.F.; Gibbons, P.M.; Leal de Araújo, J.; Rech, R.R.; Uzal, F.A. Blackleg in cattle: A case report of fetal infection and a literature review. J. Vet. Diagn. Investig. 2017, 29, 612–621. [Google Scholar] [CrossRef]
- Frey, J.; Johansson, A.; Bürki, S.; Vilei, E.M.; Redhead, K. Cytotoxin CctA, a major virulence factor of Clostridium chauvoei conferring protective immunity against myonecrosis. Vaccine 2012, 30, 5500–5505. [Google Scholar] [CrossRef]
- Rychener, L.; Albon, S.I.; Djordjevic, S.P.; Chowdhury, P.R.; Ziech, R.E.; de Vargas, A.C.; Frey, J.; Falquet, L. Clostridium chauvoei, an evolutionary dead-end pathogen. Front. Microbiol. 2017, 8, 1054. [Google Scholar] [CrossRef]
- Ziech, R.E.; Gressler, L.T.; Frey, J.; Vargas, A.C. de Blackleg in cattle: Current understanding and future research needs. Ciência Rural 2018, 120, 176–180. [Google Scholar]
- Thomas, P.; Semmler, T.; Eichhorn, I.; Lübke-Becker, A.; Werckenthin, C.; Abdel-Glil, M.Y.; Wieler, L.H.; Neubauer, H.; Seyboldt, C. First report of two complete Clostridium chauvoei genome sequences and detailed in silico genome analysis. Infect. Genet. Evol. 2017, 54, 287–298. [Google Scholar] [CrossRef]
- Nicholson, P.; Furrer, J.; Hässig, M.; Strauss, C.; Heller, M.; Braga-Lagache, S.; Frey, J. Production of neutralizing antibodies against the secreted Clostridium chauvoei toxin A (CctA) upon blackleg vaccination. Anaerobe 2019, 56, 78–87. [Google Scholar] [CrossRef]
- Frey, J.; Falquet, L. Patho-genetics of Clostridium chauvoei. Res. Microbiol. 2015, 166, 384–392. [Google Scholar] [CrossRef]
- Useh, N.M.; Esievo, K.A.N.; Nok, A.J. Pathogenesis and pathology of blackleg in ruminants: The role of toxins and neuraminidase. A short review. Vet. Q. 2003, 25, 155–159. [Google Scholar] [CrossRef]
- Uzal, F.A. Evidence-Based Medicine Concerning Efficacy of Vaccination against Clostridium chauvoei Infection in Cattle. Vet. Clin. N. Am. Food Anim. Pract. 2012, 28, 71–77. [Google Scholar] [CrossRef]
- Cortiñas, T.I.; Micalizzi, B.; de Guzman, A.M.S. Influence of culture conditions on growth and protective antigenicity of Clostridium chauvoei. J. Appl. Bacteriol. 1994, 77, 382–387. [Google Scholar] [CrossRef]
- Tanaka, M.; Hirayama, N.; Tamura, Y. Production, characterization, and protective effect of monoclonal antibodies to Clostridium chauvoei flagella. Infect. Immun. 1987, 55, 1779–1783. [Google Scholar]
- Chandler, H.M.; Gulasekharam, J. The Protective Antigen of a Highly Immunogenic Strain of Clostridium chauvoei Including an Evaluation of Its Flagella as a Protective Antigen. J. Gen. Microbiol. 1974, 84, 128–134. [Google Scholar] [CrossRef]
- Mattar, M.; Cortiñas, T.; Stefanini, A. Extracellular proteins of Clostridium chauvoei are protective in a mouse model. Acta Vet. Hung. 2007, 55, 159–170. [Google Scholar] [CrossRef]
- Aldape, M.J.; Bayer, C.R.; Rice, S.N.; Bryant, A.E.; Stevens, D.L. Comparative efficacy of antibiotics in treating experimental Clostridium septicum infection. Int. J. Antimicrob. Agents 2018, 52, 469–473. [Google Scholar] [CrossRef]
- Gazioglu, A.; Karagülle, B.; Yüksel, H.; Nuri Açlk, M.; Keçeci, H.; Dörtbudak, M.B.; Çetinkaya, B. Sudden death due to gas gangrene caused by Clostridium septicum in goats. BMC Vet. Res. 2018, 14, 406. [Google Scholar] [CrossRef]
- Silva, R.O.S.; Uzal, F.A.; Oliveira, C.A., Jr.; Lobato, F.C.F. Gas Gangrene (Malignant Edema). In Clostridial Diseases of Animals; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2016; pp. 243–254. ISBN 9781118728291. [Google Scholar]
- Lighty, M.E.; Elvinger, F.; Evans, R.D.; Sriranganathan, N.; Leroith, T.; Pierson, F.W. Incidence of clostridial dermatitis (cellulitis) and factors for development of the disease in turkeys. J. Appl. Poult. Res. 2015, 5, 104–112. [Google Scholar] [CrossRef]
- Li, G.; Lillehoj, H.S.; Lee, K.W.; Jang, S.I.; Marc, P.; Gay, C.G.; Ritter, G.D.; Bautista, D.A.; Phillips, K.; Neumann, A.P.; et al. An outbreak of gangrenous dermatitis in commercial broiler chickens. Avian Pathol. 2010, 39, 247–253. [Google Scholar] [CrossRef]
- D’avil Farias, L.; Azevedo, M.D.S.; Trost, M.E.; De La Côrte, F.D.; Irigoyen, L.F.; de Vargas, A.C. Acute myonecrosis in horse caused by Clostridium novyi type A. Braz. J. Microbiol. 2014, 45, 221–224. [Google Scholar] [CrossRef]
- Srivastava, I.; Aldape, M.J.; Bryant, A.E.; Stevens, D.L. Spontaneous C. septicum gas gangrene: A literature review. Anaerobe 2017, 48, 165–171. [Google Scholar] [CrossRef]
- KJessamy, K.; Ojevwe, F.O.; Ubagharaji, E.; Sharma, A.; Anozie, O.; Gilman, C.A.; Rawlins, S. Clostridium septicum: An Unusual Link to a Lower Gastrointestinal Bleed. Case Rep. Gastroenterol. 2016, 10, 489–493. [Google Scholar] [CrossRef]
- Macfarlane, S.; Hopkins, M.J.; Macfarlane, G.T. Toxin synthesis and mucin breakdown are related to swarming phenomenon in Clostridium septicum. Infect. Immun. 2001, 69, 1120–1126. [Google Scholar] [CrossRef]
- Zurmeyer, S.; Fotopoulou, C.; Sehouli, J.; Braicu, E.; Schlichting, U. Clostridium septicum can cause distant myonecrosis in patients with ovarian cancer. Anticancer Res. 2013, 33, 1585–1589. [Google Scholar]
- Nanjappa, S.; Shah, S.; Pabbathi, S. Clostridium septicum Gas Gangrene in Colon Cancer: Importance of Early Diagnosis. Case Rep. Infect. Dis. 2015, 2015, 694247. [Google Scholar]
- Forrester, J.D.; Shkolyar, E.; Gregg, D.; Spain, D.A.; Weiser, T.G. Nontraumatic Clostridium septicum Myonecrosis in Adults: Case Report and a 15-Year Systematic Literature Review. Infect. Dis. Clin. Pract. 2016, 24, 318–323. [Google Scholar] [CrossRef]
- Cullinane, C.; Earley, H.; Tormey, S. Deadly combination: Clostridium septicum and colorectal malignancy. BMJ Case Rep. 2017. [Google Scholar] [CrossRef]
- Salvarani, F.M.; Lobato, Z.I.P.; Assis, R.A.; Lima, C.G.R.D.; Silva, R.O.S.; Pires, P.S.; Lobato, F.C.F. In vitro evaluation of Clostridium septicum alpha toxoid. Arq. Bras. Med. Vet. Zootec. 2011, 62, 778–783. [Google Scholar] [CrossRef]
- Morris, W.E.; Uzal, F.A.; Fattorini, F.R.; Terzolo, H. Malignant oedema associated with blood-sampling in sheep. Aust. Vet. J. 2002, 80, 280–281. [Google Scholar] [CrossRef]
- Odani, J.S.; Blanchard, P.C.; Adaska, J.M.; Moeller, R.B.; Uzal, F.A. Malignant edema in postpartum dairy cattle. J. Vet. Diagn. Investig. 2009, 21, 920–924. [Google Scholar] [CrossRef]
- Clark, S.; Porter, R.; McComb, B.; Lippert, R.; Olson, S.; Nohner, S.; Shivaprasad, H. Clostridial Dermatitis and Cellulitis: An Emerging Disease of Turkeys. Avian Dis. Dig. 2010, 54, 788–794. [Google Scholar] [CrossRef]
- Neumann, A.P.; Rehberger, T.G. MLST analysis reveals a highly conserved core genome among poultry isolates of Clostridium septicum. Anaerobe 2009, 15, 99–106. [Google Scholar] [CrossRef]
- Kennedy, C.L.; Krejany, E.O.; Young, L.F.; O’Connor, J.R.; Awad, M.M.; Boyd, R.L.; Emmins, J.J.; Lyras, D.; Rood, J.I. The α-toxin of Clostridium septicum is essential for virulence. Mol. Microbiol. 2005, 57, 1357–1366. [Google Scholar] [CrossRef]
- Kennedy, C.L.; Lyras, D.; Cordner, L.M.; Melton-Witt, J.; Emmins, J.J.; Tweten, R.K.; Rood, J.I. Pore-Forming activity of Alpha-Toxin is essential for clostridium septicum-mediated myonecrosis. Infect. Immun. 2009, 77, 943–951. [Google Scholar] [CrossRef]
- Chakravorty, A.; Awad, M.M.; Cheung, J.K.; Hiscox, T.J.; Lyras, D.; Rood, J.I. The pore-forming α-toxin from Clostridium septicum activates the MAPK pathway in a Ras-c-Raf-dependent and independent manner. Toxins 2015, 7, 516–534. [Google Scholar] [CrossRef]
- Ballard, J.; Crabtree, J.; Roe, B.A.; Tweten, R.K. The primary structure of Clostridium septicum alpha-toxin exhibits similarity with that of Aeromonas hydrophila aerolysin. Infect. Immun. 1995, 63, 340–344. [Google Scholar]
- Amimoto, K.; Ohgitani, T.; Sasaki, O.; Oishi, E.; Katayama, S.; Isogai, M.; Ota, S. Protective Effect of Clostridium septicum Alpha-Toxoid Vaccine against Challenge with Spores in Guinea Pigs. J. Vet. Med. Sci. 2002, 64, 67–69. [Google Scholar] [CrossRef]
- Thachil, A.J.; McComb, B.; Kromm, M.; Nagaraja, K.V. Vaccination of Turkeys with Clostridium septicum Bacterin-Toxoid: Evaluation of Protection against Clostridial Dermatitis. Avian Dis. 2013, 57, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Prescott, J.F.; Menzies, P.I.; Fraser, R.S. Clostridial Abomasitis. In Clostridial Diseases in Animals; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; ISBN 9781118728291. [Google Scholar]
- Ballard, J.; Bryant, A.; Stevens, D.; Tweten, R.K. Purification and characterization of the lethal toxin (alpha-toxin) of Clostridium septicum. Infect. Immun. 1992, 57, 214–219. [Google Scholar]
- Roth, F.; Jansen, K.; Petzke, S. Detection of neutralizing antibodies against α-toxin of different Clostridium septicum strains in cell culture. FEMS Immunol. Med. Microbiol. 1999, 24, 353–359. [Google Scholar] [CrossRef]
- Hasan, S.M.; Hall, J.B. Growth of Clostridium tertium and Clostridium septicum in chemically defined media. Appl. Environ. Microbiol. 1976, 31, 442–443. [Google Scholar] [PubMed]
- Hnátková, Z.; Vraný, B.; Hnátek, J.; Lettl, A. Preparation of Clostridium septicum antigen for hyperimmunization of horses using a dialyzed culture. Folia Microbiol. 1986, 31, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Cortiñas, T.I.; Mattar, M.A.; Stefanini de Guzmán, A.M. Alpha-toxin production by Clostridium septicum at different culture conditions. Anaerobe 1997, 3, 199–202. [Google Scholar] [CrossRef]
- Lancto, C.A.; Foster, L.K.; Kromm, M.M.; McComb, B.; Williams, J.; Luke, J.; Carnes, A.; Hodgson, C.P.; Foster, D.N. A Noncytolytic α Toxin Recombinant Protein Protects Turkeys against Clostridium septicum Challenge. Avian Dis. 2014, 58, 566–571. [Google Scholar] [CrossRef]
- Navarro, M.; Uzal, F.A. Infectious Necrotic Hepatitis. In Clostridial Diseases in Animals; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; ISBN 9781118728291. [Google Scholar]
- Garía, A.; Ayuso, D.; Benítez, J.M.; García, W.L.; Martínez, R.; Sánchez, S. Clostridium novyi infection causing sow mortality in an iberian pig herd raised in an outdoor rearing system in Spain. J. Swine Health Prod. 2009, 17, 264–268. [Google Scholar]
- Sweeney, H.J.; Greig, A. Infectious necrotic hepatitis in a horse. Equine Vet. J. 1986, 18, 150–151. [Google Scholar] [CrossRef]
- Whitfield, L.; Cypher, E.; Gordon, S.; Pauwels, F.; Ling, J.; Collett, M.; Uzal, F. Necrotic hepatitis associated with Clostridium novyi infection (black disease) in a horse in New Zealand. N. Z. Vet. J. 2015, 63, 177–179. [Google Scholar] [CrossRef]
- Abdel-Haq, N.M.; Chearskul, P.; Salimnia, H.; Asmar, B.I. Clostridial liver abscess following blunt abdominal trauma: Case report and review of the literature. Scand. J. Infect. Dis. 2007, 39, 734–737. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.; Boyd, J.T.; Trinh, H.T.; Coombs, J.W.; Fermann, G.J. Fatal myocarditis due to Clostridium novyi type B in a previously healthy woman: Case report and literature review. Scand. J. Infect. Dis. 2007, 39, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Oakley, C.L.; Warrack, G.H.; Clarke, P.H. The Toxins of Clostridium oedematiens (Cl. novyi). J. Gen. Microbiol. 2009, 1, 91–107. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McGuigan, C.; Roworth, M. Clostridium novyi type A infection: A sporadic fatal case. Scand. J. Infect. Dis. 2002, 34, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Herrera, C.; Meehan, R.; Podduturi, V.; Eastman, A.L.; Nelson, D.B. Maternal Death Due to Clostridium novyi in an Injection Drug User. Obstet. Gynecol. 2016, 128, 876–879. [Google Scholar] [CrossRef]
- McGuigan, C.C.; Penrice, G.M.; Gruer, L.; Ahmed, S.; Goldberg, D.; Black, M.; Salmon, J.E.; Hood, J. Lethal outbreak of infection with Clostridium novyi type A and other spore-forming organisms in Scottish injecting drug users. J. Med. Microbiol. 2002, 51, 971–977. [Google Scholar] [CrossRef]
- Majumdar, S.; Woodcock, S.; Cheesbrouch, J. Severe sepsis following wound infection by an unusual organism - Clostridium novyi. Int. J. Clin. Pract. 2004, 58, 892–893. [Google Scholar] [CrossRef]
- Watanabe, N.; Kobayashi, K.; Hashikita, G.; Taji, Y.; Ishibashi, N.; Sakuramoto, S.; Mitsutake, K.; Ikebuchi, K.; Ebihara, Y. Hepatic gas gangrene caused by Clostridium novyi. Anaerobe 2019, 57, 90–92. [Google Scholar] [CrossRef]
- Choi, Y.-K.; Kang, M.-S.; Yoo, H.-S.; Lee, D.-Y.; Lee, H.-C.; Kim, D.-Y. Clostridium perfringens type A Myonecrosis in a Horse in Korea. J. Vet. Med. Sci. 2003, 65, 1245–1247. [Google Scholar] [CrossRef]
- Pires, P.S.; Ecco, R.; Silva, R.O.S.; de Araújo, M.R.; Salvarani, F.M.; Heneine, L.G.D.; de Oliveira Júnior, C.A.; Lobato, F.C.F. A retrospective study on the diagnosis of clostridial myonecrosis in ruminants in Brazil. Ciência Rural 2016, 47. [Google Scholar] [CrossRef]
- Peek, S.F.; Semrad, S.D. Clostridial myonecrosis in horses. Equine Vet. Educ. 2010, 35, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Nyaoke, A.C.; Navarro, M.A.; Beingesser, J.; Uzal, F.A. Infectious necrotic hepatitis caused by Clostridium novyi type B in a horse: Case report and review of the literature. J. Vet. Diagn. Investig. 2018, 30, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Busch, C.; Schomig, K.; Hofmann, F.; Aktories, K. Characterization of the catalytic domain of Clostridium novyi alpha-toxin. Infect. Immun. 2000, 68, 6378–6383. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, F.; Herrmann, A.; Habermann, E.; von Eichel-Streiber, C. Sequencing and analysis of the gene encoding the α-toxin of Clostridium novyi proves its homology to toxins A and B of Clostridium difficile. MGG Mol. Gen. Genet. 1995, 247, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Oksche, A.; Nakov, R.; Habermann, E. Morphological and biochemical study of cytoskeletal changes in cultured cells after extracellular application of Clostridium novyi alpha-toxin. Infect. Immun. 1992, 60, 3002–3006. [Google Scholar] [PubMed]
- Selzer, J.; Hofmann, F.; Rex, G.; Wilm, M.; Mann, M.; Just, I.; Aktories, K. Clostridium novyi α-toxin-catalyzed incorporation of GlcNAc into Rho subfamily proteins. J. Biol. Chem. 1996, 271, 25173–25177. [Google Scholar] [CrossRef] [PubMed]
- Hauer, P.J.; Yeary, T.J.; Rosenbusch, R.F. Cloning and molecular characterization of the beta toxin (phospholipase C) gene of Clostridium haemolyticum. Anaerobe 2004, 10, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Skarin, H.; Segerman, B. Plasmidome interchange between Clostridium botulinum, Clostridium novyiand Clostridium haemolyticum converts strains of independent lineages into distinctly different pathogens. PLoS ONE 2014, 9, e107777. [Google Scholar] [CrossRef]
- Eklund, M.W.; Poysky, F.T.; Peterson, M.E.; Meyers, J.A. Relationship of bacteriophages to alpha toxin production in Clostridium novyi types A and B. Infect. Immun. 1976, 14, 793–803. [Google Scholar]
- Fortier, L.C. The Contribution of Bacteriophages to the Biology and Virulence of Pathogenic Clostridia. Adv. Appl. Microbiol. 2017, 101, 169–200. [Google Scholar]
- Aquino, P.L.M.; Fonseca, F.S.; Mozzer, O.D.; Giordano, R.C.; Sousa, R. Optimization of the Production of Inactivated Clostridium novyi Type B Vaccine Using Computational Intelligence Techniques. Appl. Biochem. Biotechnol. 2016, 179, 895–909. [Google Scholar] [CrossRef] [PubMed]
- Obana, N.; Nakamura, K. A novel toxin regulator, the CPE1446-CPE1447 protein heteromeric complex, controls toxin genes in Clostridium perfringens. J. Bacteriol. 2011, 193, 4417–4424. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Boyd, N.A.; Thomson, R.O.; Walker, P.D. The prevention of experimental Clostridium novyi and Cl. perfringens gas gangrene in high-velocity missile wounds by active immunisation. J. Med. Microbiol. 1972, 5, 467–472. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tytell, A.A.; Logan, M.A.; Tytell, A.G.; Tepper, J. Immunization of humans and animals with gas gangrene toxoids. J. Immunol. 1947, 55, 233–244. [Google Scholar] [PubMed]
- Robertson, M.; Keppie, J. Gas gangrene active immunisation by means of concentrated toxoids. Lancet 1943, 242, 311–314. [Google Scholar] [CrossRef]
- Walbum, L.E.; Reymann, G.C. The production of toxin by Clostridium œdematiens (B. novyi). J. Pathol. Bacteriol. 1937, 44, 379–387. [Google Scholar] [CrossRef]
- Moore, W.B. Solidified Media Suitable for the Cultivation of Clostridium novyi Type B. J. Gen. Microbiol. 1968, 53, 415–423. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nishida, S.; Nakagawara, G. Isolation of toxigenic strains of clostridium novyi from soil. J. Bacteriol. 1964, 88, 1636–1640. [Google Scholar] [PubMed]
- Rutter, J.M. Study of the carbohydrate fermentation reactions of Clostridium oedematiens (Cl. novyi). J. Med. Microbiol. 1970, 3, 283–289. [Google Scholar] [CrossRef]
- Ball, D.W.; Van Tassell, R.L.; Roberts, M.D.; Hahn, P.E.; Lyerly, D.M.; Wilkins, T.D. Purification and characterization of alpha-toxin produced by Clostridium novyi type A. Infect. Immun. 1993, 61, 2912–2918. [Google Scholar]
- Navarro, M.A.; Dutra, F.; Briano, C.; Romero, A.; Persiani, M.; Freedman, J.C.; Morrell, E.; Beingesser, J.; Uzal, F.A. Pathology of Naturally Occurring Bacillary Hemoglobinuria in Cattle. Vet. Pathol. 2017, 54, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.C. The isolation of Clostridium haemolyticum from cattle in New Zealand. N. Z. Vet. J. 1959, 7, 115–119. [Google Scholar] [CrossRef]
- Shinozuka, Y.; Yamato, O.; Hossain, M.A.; Higaki, T.; Ishikawa, I.; Ichiba, S.; Takagi, M. Bacillary Hemoglobinuria in Japanese Black Cattle in Hiroshima, Japan: A Case Study. J. Vet. Med. Sci. 2010, 73, 255–258. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Randhawa, S.S.; Sharma, D.K.; Randhawa, C.S.; Gill, B.S.; Brar, R.S.; Singh, J. An outbreak of bacillary haemoglobinuria in sheep in India. Trop. Anim. Health Prod. 1995, 27, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Son, D.J.; Hong, J.Y.; Kim, K.H.; Jeong, Y.H.; Myung, D.S.; Cho, S.B.; Lee, W.S.; Kang, Y.J.; Kim, J.W.; Joo, Y.E. Liver abscess caused by Clostridium haemolyticum infection after transarterial chemoembolization for hepatocellular carcinoma: A case report. Medicine 2018, 97. [Google Scholar] [CrossRef] [PubMed]
- Saeb, A.T.; Abouelhoda, M.; Selvaraju, M.; Althawadi, S.I.; Mutabagani, M.; Adil, M.; Al Hokail, A.; Tayeb, H.T. The Use of Next-Generation Sequencing in the Identification of a Fastidious Pathogen: A Lesson from a Clinical Setup. Evol. Bioinform. Online 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Navarro, M.; Quintela, F.D.; Uzal, F.A. Bacillary Hemoglobinuria. In Clostridial Diseases of Animals; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 265–274. ISBN 9781118728291. [Google Scholar]
- Hauer, P.J.; Yeary, T.J.; Rosenbusch, R.F. Evidence of the protective immunogenicity of native and recombinant Clostridium haemolyticum phospholipase C (beta toxin) in guinea pigs. Vaccine 2006, 24, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Takagi, M.; Yamato, O.; Sasaki, Y.; Mukai, S.; Fushimi, Y.; Yoshida, T.; Mizukami, K.; Shoubudani, T.; Amimoto, K.; Chuma, T.; et al. Successful Treatment of Bacillary Hemoglobinuria in Japanese Black Cows. J. Vet. Med. Sci. 2009, 71, 1105–1108. [Google Scholar] [CrossRef] [PubMed]
- Takagi, M.; Kohyama, M.; Ono, T.; Adachi, S.; Shirao, D.; Tamura, H.; Taniguchi, M.; Yabuki, A.; Yamato, O. Recovery with a regular dose of antibiotics from bacillary hemoglobinuria in a Holstein cow. J. Vet. Med. Sci. 2016, 78, 1737–1740. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sasaki, Y.; Takikawa, N.; Kojima, A.; Norimatsu, M.; Suzuki, S.; Tamura, Y. Phylogenetic positions of Clostridium novyi and Clostridium haemolyticum based on 16S rDNA sequences. Int. J. Syst. Evol. Microbiol. 2001, 51, 901–904. [Google Scholar] [CrossRef][Green Version]
- Roberts, R.S.; Güven, S.; Worrall, E.E. Studies on clostridium oedematiens. J. Comp. Pathol. 1970, 80, 9–18. [Google Scholar] [CrossRef]
- Darakhshan, H.; Lauerman, L.H. Some properties of beta toxin produced by Clostridium haemolyticum strain IRP-135. Comp. Immunol. Microbiol. Infect. Dis. 1981, 4, 307–316. [Google Scholar] [CrossRef]
- Rappuoli, R. Glycoconjugate vaccines: Principles and mechanisms. Sci. Transl. Med. 2018, 10, eaat4615. [Google Scholar] [CrossRef] [PubMed]
- Colombo, C.; Pitirollo, O.; Lay, L. Recent Advances in the Synthesis of Glycoconjugates for Vaccine Development. Molecules 2018, 23, 1712. [Google Scholar] [CrossRef] [PubMed]
- Pizarro-Guajardo, M.; Chamorro-Veloso, N.; Vidal, R.M.; Paredes-Sabja, D. New insights for vaccine development against Clostridium difficile infections. Anaerobe 2019, 58, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, H.; Kett, V. Current prospects and future challenges for nasal vaccine delivery. Hum. Vaccin. Immunother. 2017, 13, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, R.; Kohda, T.; Kataoka, K.; Ihara, H.; Kozaki, S.; Pascual, D.W.; Staats, H.F.; Kiyono, H.; McGhee, J.R.; Fujihashi, K. A Novel Neurotoxoid Vaccine Prevents Mucosal Botulism. J. Immunol. 2005, 174, 2190–2195. [Google Scholar] [CrossRef] [PubMed]
- Nochi, T.; Yuki, Y.; Takahashi, H.; Sawada, S.; Mejima, M.; Kohda, T.; Harada, N.; Kong, I.G.; Sato, A.; Kataoka, N.; et al. Nanogel antigenic protein-delivery system for adjuvant-free intranasal vaccines. Nat. Mater. 2010, 9, 572. [Google Scholar] [CrossRef] [PubMed]
| Pathogenic Strain | Type | Toxin | Disease | Commercial Toxoid or Bacterin-Toxoid Vaccine | Recombinant Vaccine Research |
|---|---|---|---|---|---|
| C. botulinum | Group I | BoNT serotypes A, B, E, and F | Botulism (human and animal) | Pentavalent BoNT/A–E toxoids (for people at high risk or exposed to the toxin). Discontinued. BoNT/B toxoid (horses) | rBV A/B Withdrawn from human clinical trial. rHC BoNT/A/B/E |
| Group II | BoNT serotypes B, E, and F | Botulism (human and animal) | - | - | |
| Group III | BoNT serotypes C and D | Botulism (human and animal) | Bivalent BoNT/C-D toxoids (livestock) | rHC BoNT/C | |
| C. tetani | - | TeNT | Tetanus (human and animal) | TeNT toxoid (human and animal) | TeNT-HC |
| C. perfringens | Type A | CPA | CPA: Myonecrosis (human and animal). | Monovalent CPA toxoid vaccine (cattle and poultry). | rCPA |
| Type B | CPA, CPB, ETX | CPB: Necrohemorrhagic enteritis (animal) ETX: Dysentery (lambs) and enterotoxemia or pulpy kidney (domestic ruminants) | CPB and ETX toxoid(s) or bacterin-toxoid(s) vaccine (animal) | rCPB rETX r- fused ETX-CPB vaccine | |
| Type C | CPA, CPB, | CPB: Enteritis necroticans or pigbel (human) and necrotic enteritis, enterotoxemia (animal) | Experimental CPB toxoid vaccine (for people in Papua New Guinea). Discontinued. CPB toxoid or bacterin-toxoid (animals) | rCPB | |
| Type D | CPA, ETX, | ETX: Enterotoxemia or pulpy kidney (domestic ruminants) | ETX toxoid or bacterin-toxoid (animal) | rETX | |
| Type E | CPA, ITX, | ITX: Hemorrhagic enteritis (ruminants) and enterotoxemia (rabbits). Not confirmed. | - | - | |
| Type F | CPA, CPE | CPE: food poisoning, antibiotic-associated diarrhea, sporadic diarrhea, and sudden infant death syndrome (SIDS) (humans), and gastrointestinal disease (animals) | - | rC-terminal CPE r-fused C-terminal CPE with Shiga toxin B subunit | |
| Type G | CPA, NetB | NetB: Necrotic enteritis (poultry) | - | rNetB | |
| C. chauvoei | - | CctA | Blackleg (cattle, sheep, and other small ruminants) | Bacterin-toxoid vaccine (animal) | rCctA |
| C. septicum | - | ATX | Spontaneous myonecrosis (human) Braxy (sheep and calves) Malignant edema (ruminants) Gangrenous dermatitis (poultry) | Toxoid or bacterin-toxoid vaccine (animal) | rATX |
| C. novyi | A | TcnA | Myonecrosis (human and animal) | - | - |
| B | Beta toxin | Black disease (ruminants, pigs, and horses) | Toxoid vaccine (animal) | - | |
| C. hemolyticum | - | Beta toxin | Bacillary hemoglobinuria (cattle and occasionally in sheep and goats) | Bacterin-toxoid vaccine (animal) | r-beta toxin |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaragoza, N.E.; Orellana, C.A.; Moonen, G.A.; Moutafis, G.; Marcellin, E. Vaccine Production to Protect Animals Against Pathogenic Clostridia. Toxins 2019, 11, 525. https://doi.org/10.3390/toxins11090525
Zaragoza NE, Orellana CA, Moonen GA, Moutafis G, Marcellin E. Vaccine Production to Protect Animals Against Pathogenic Clostridia. Toxins. 2019; 11(9):525. https://doi.org/10.3390/toxins11090525
Chicago/Turabian StyleZaragoza, Nicolas E., Camila A. Orellana, Glenn A. Moonen, George Moutafis, and Esteban Marcellin. 2019. "Vaccine Production to Protect Animals Against Pathogenic Clostridia" Toxins 11, no. 9: 525. https://doi.org/10.3390/toxins11090525
APA StyleZaragoza, N. E., Orellana, C. A., Moonen, G. A., Moutafis, G., & Marcellin, E. (2019). Vaccine Production to Protect Animals Against Pathogenic Clostridia. Toxins, 11(9), 525. https://doi.org/10.3390/toxins11090525





