Locally Sustainable School Lunch Intervention Improves Hemoglobin and Hematocrit Levels and Body Mass Index among Elementary Schoolchildren in Rural West Java, Indonesia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area and Subjects
2.2. Research Design
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Subjects
3.2. Nutritional Value of the Provided School Lunch
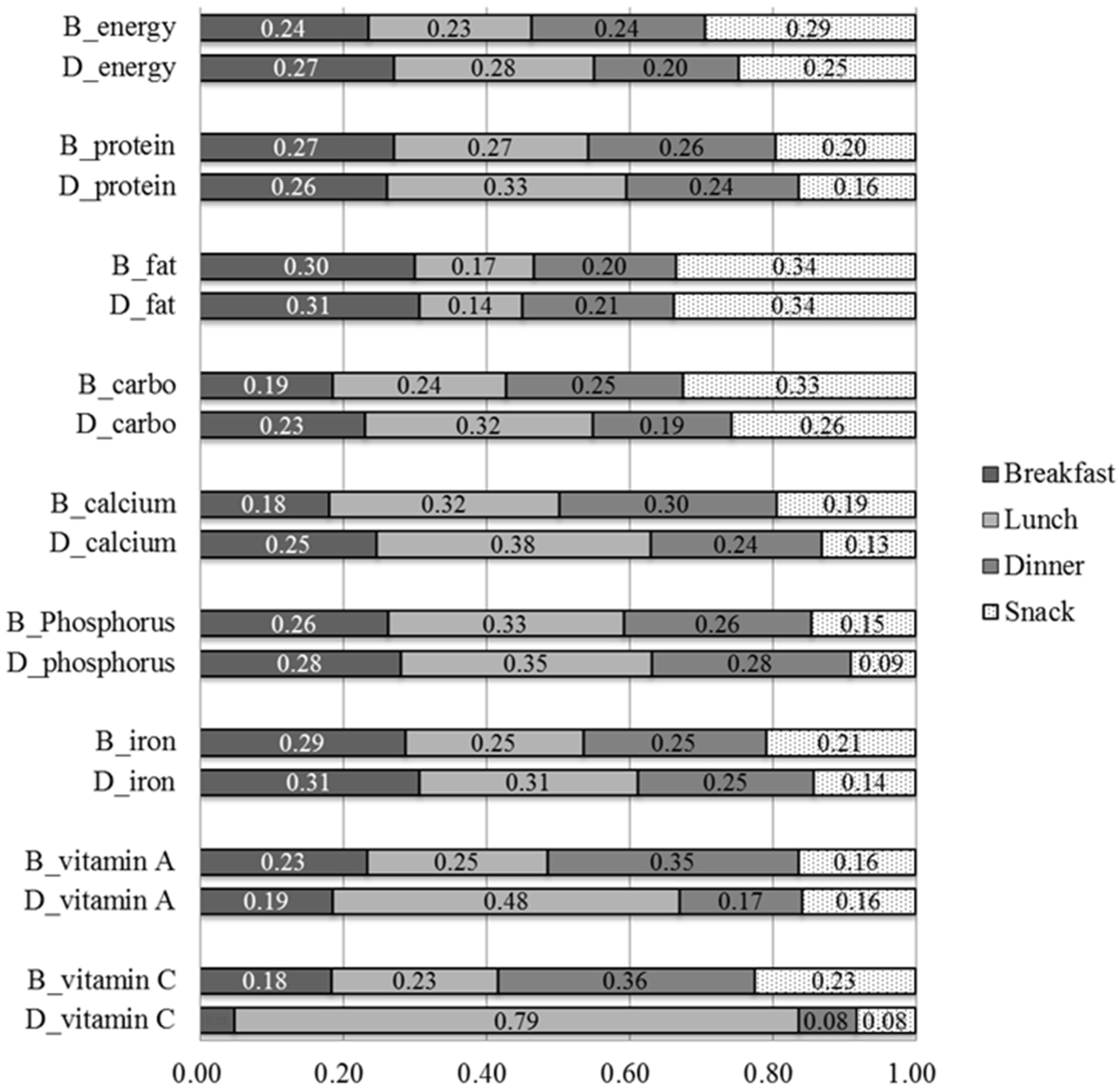
3.3. Nutritional Intakes Before and During the Intervention
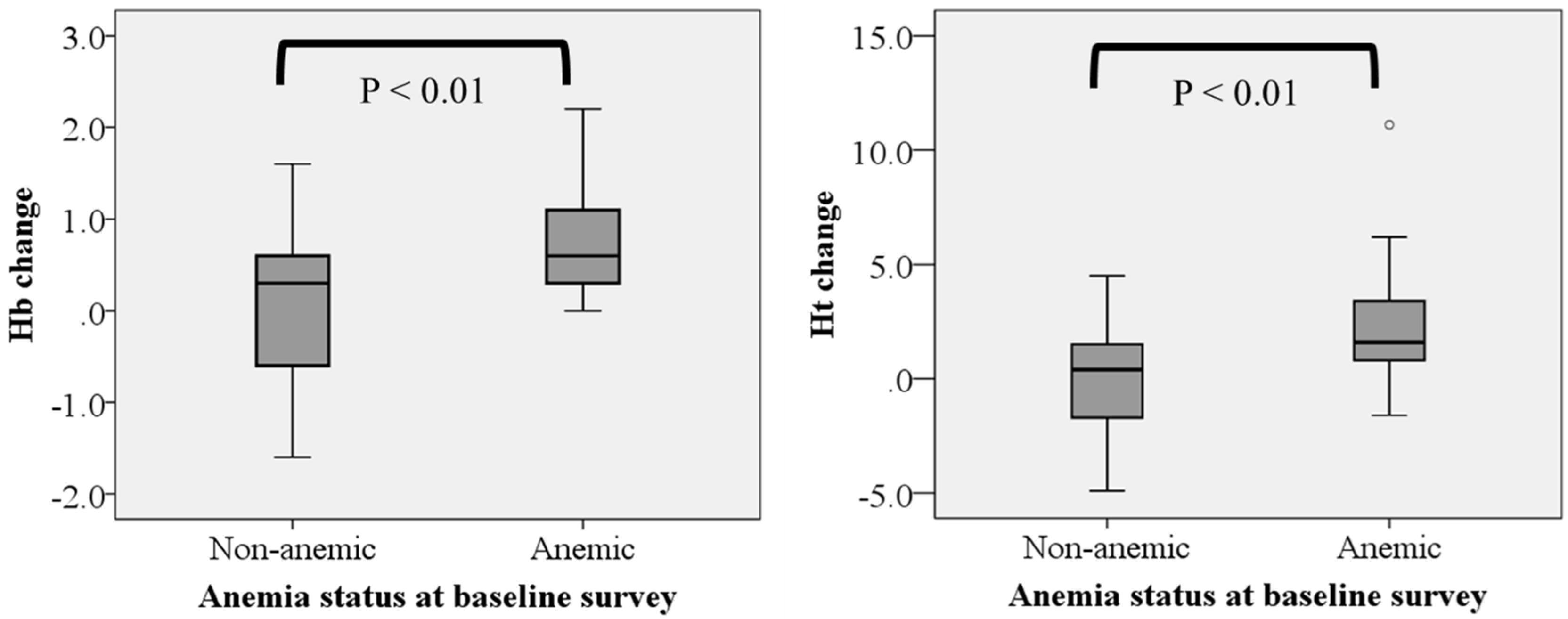
3.4. Hemoglobin and Hematocrit Levels and the Anemic Status Before and after the Intervention
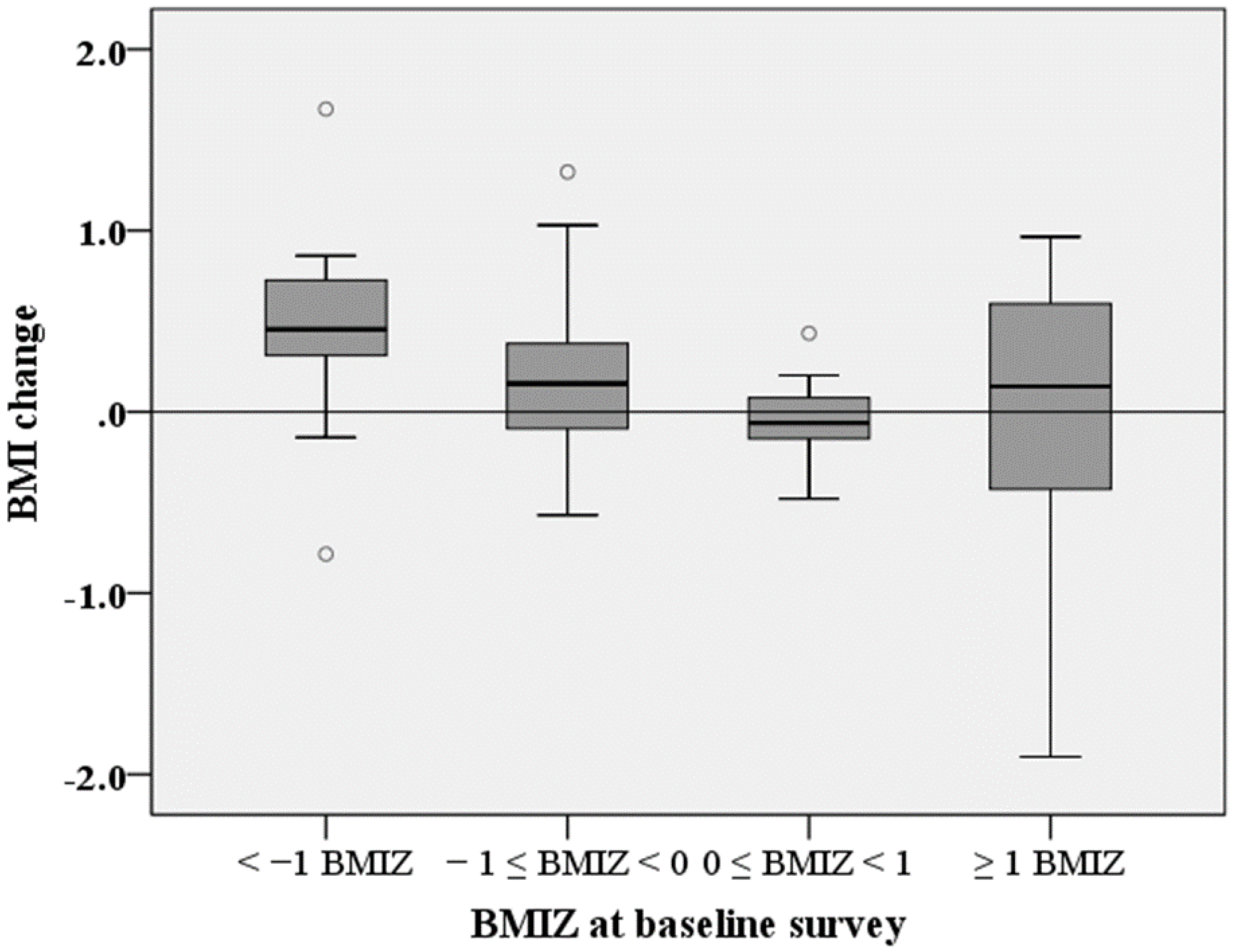
3.5. BMI and BMIZ Before and after the Intervention
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Badan Penelitian dan Pengembangan Kesehatan (Internet). Riset Kesehatan Dasar; Badan Penelitian dan Pengembangan Kesehatan: Jakarta, Indonesia, 2013; Available online: http://www.depkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf (accessed on 16 May 2017).
- Delisle, H.F.; Receveur, O.; Agueh, V.; Nishida, C. Pilot project of the Nutrition-Friendly School Initiative (NFSI) in Ouagadougou, Burkina Faso and Cotonou, Benin, in West Africa. Glob. Health Promot. 2013, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Skinner, J.D.; Carruth, B.R.; Wendy, B.; Ziegler, P.J. Children’s food preferences: A longitudinal analysis. J. Am. Diet. Assoc. 2002, 102, 1638. [Google Scholar] [CrossRef]
- World Health Organization (Internet). Report of the Brainstorming Meeting on the Development of a Framework on the Nutrition-Friendly Schools Initiative; World Health Organization: Geneva, Switzerland, 2006; Available online: http://www.who.int/nutrition/publications/Montreux_Meeting_Report.pdf (accessed on 25 April 2017).
- Tanaka, N.; Miyoshi, M. School lunch program for health promotion among children in Japan. Asia Pac. J. Clin. Nutr. 2012, 21, 155. [Google Scholar] [PubMed]
- Wong, Y.; Chang, Y.J. The practices and needs of dietitian in school lunch program in Taiwan. Asia Pac. J. Clin. Nutr. 2012, 21, 134. [Google Scholar] [PubMed]
- Chutani, A.M. School lunch program in India: Background, objectives and components. Asia Pac. J. Clin. Nutr. 2012, 21, 151. [Google Scholar] [PubMed]
- Le, D.S. School meal program in Ho Chi Minh city, Vietnam: Reality and future plan. Asia Pac. J. Clin. Nutr. 2012, 21, 139. [Google Scholar] [PubMed]
- Studdert, L.J.; Soekirman Rasmussen, K.M.; Habicht, J.-P. Community-based school feeding during Indonesia’s economic crisis: Implementation, benefits, and sustainability. Food Nutr. Bull. 2004, 25, 156. [Google Scholar] [CrossRef] [PubMed]
- Bundy, D.; Burbano, C.; Grosh, M. Rethinking school deeding: Social safety nets, child development, and the education sector. In The International Bank for Reconstruction and Development/The World Bank; The World Bank: Washington, DC, USA, 2009. [Google Scholar]
- Sekiyama, M.; Roosita, K.; Ohtsuka, R. Snack foods consumption contributes to poor nutrition of rural children in West Java, Indonesia. Asia Pac. J. Clin. Nutr. 2012, 21, 558. [Google Scholar] [PubMed]
- Sekiyama, M.; Roosita, K.; Ohtsuka, R. Developmental stage-dependent influence of environmental factors on growth of rural Sundanese children in West Java, Indonesia. Am. J. Phys. Anthropol. 2015, 157, 94. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Hardinsyah, B.D. Judgement and Planning for Food Consumption; Faculty of Agriculture, Bogor Agricultural University: Bogor, Indonesia, 1990. [Google Scholar]
- Department of Health, Indonesia. Food Composition Table of Indonesia; Department of Health: Jakarta, Indonesia, 1995. [Google Scholar]
- Minister of Health Indonesia (Internet). Peraturan Menteri Kesehatan Republik Indonesia Nomor 75 Tahun 2013 Tentang Angka Kecukupan Gizi. 2013. Available online: http://gizi.depkes.go.id/download/Kebijakan%20Gizi/PMK%2075-2013.pdf (accessed on 30 April 2017).
- World Health Organization (Internet). Iron Deficiency Anaemia: Assessment, Prevention and Control. A Guide for Program Managers; World Health Organization: Geneva, Switzerland, 2001; Available online: http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf (accessed on 10 May 2017).
- Sekiyama, M.; Ohtsuka, R. Significant effects of birth-related biological factors on pre-adolescent nutritional status among rural Sundanese in West Java, Indonesia. J. Biosoc. Sci. 2004, 37, 413–426. [Google Scholar] [CrossRef]
- Jomaa, L.H.; McDonnell, E.; Probart, C. School feeding programs in developing countries: Impacts on children’s health and educational outcomes. Nutr. Rev. 2011, 69, 83. [Google Scholar] [CrossRef] [PubMed]
- United Nations (Internet). UN General Assembly. Road map towards implement of the United Nations Millennium Declaration. 2001. Available online: http://www.un.org/documents/ga/docs/56/a56326.pdf (accessed on 7 March 2017).
- Kristjansson, E.A.; Robinson, V.; Petticrew, M.; MacDonald, B.; Krasevec, J.; Janzen, L.; Greenhalgh, T.; Wells, G.A.; MacGowan, J.; Farmer, A.P.; et al. School feeding for improving the physical and psychosocial health of disadvantaged students. Cochrane Database Syst. Rev. 2007, 1–144. [Google Scholar] [CrossRef]
- Ahmed, A.U. Impact of Feeding Children in School: Evidence from Bangladesh; International Food Policy Research Institute: Washington, DC, USA, 2004. [Google Scholar]
- Murphy, S.P.; Gewa, C.; Liang, L.J.; Grillenberger, M.; Bwibo, N.O.; Neumann, C.G. School snacks containing animal source foods improve dietary quality for children in rural Kenya. J. Nutr. 2003, 133, 3950S–3956S. [Google Scholar] [PubMed]
- Afridi, F. Child welfare programs and child nutrition: Evidence from a mandated school meal program in India. J. Dev. Econ. 2010, 92, 152–165. [Google Scholar] [CrossRef]
- Kruger, M.; Badenhorst, C.J.; Mansvelt, E.P.G.; Laubscher, J.A. Effects of iron fortification in a school feeding scheme and anthelmintic therapy on the iron status and growth of 6–8 year old school children. Food Nutr. Bull. 1996, 17, 11. [Google Scholar]
- Van Stuijvenberg, M.E.; Kvalsvig, J.D.; Faber, M.; Kruger, M.; Kenoyer, D.G.; Benadé, A.J. Effect of iron-, iodine-, and beta-carotene-fortified biscuits on the micronutrient status of primary school children: A randomized controlled trial. Am. J. Clin. Nutr. 1999, 69, 497. [Google Scholar] [PubMed]
- Arsenault, J.E.; Mora-plazas, M.; Forero, Y.; López-Arana, S.; Marín, C.; Baylin, A.; Villamor, E. Provision of a school snack is associated with Vitamin B-12 Status, linear growth, and morbidity in children from Bogota. J. Nutr. 2009, 139, 1744. [Google Scholar] [CrossRef] [PubMed]
- Simeon, D.T. School feeding in Jamaica: A review of its evaluation. Am. J. Clin. Nutr. 1998, 67, 790S–794S. [Google Scholar] [PubMed]
- Grillenberger, M.; Neumann, C.G.; Murphy, S.P.; Bwibo, N.O.; van’t Veer, P.; Hautvast, J.G.; West, C.E. Food supplements have a positive impact on weight gain and the addition of animal source foods increases lean body mass of Kenyan schoolchildren. J. Nutr. 2003, 133, 3957S–3964S. [Google Scholar] [PubMed]
- Hurrell, R.F. Preventing iron deficiency through food fortification. Nutr. Rev. 1997, 55, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S. Principles of Nutritional Assessment; Oxford University Press: New York, NY, USA, 2005. [Google Scholar]
- Ministry of Health of Republic of Indonesia. Total Diet Study: Individual Food Consumption Survey (Studi Diet Total: Survei Konsumsi Makanan Individu) Indonesia 2014; National Institute for Health Research and Development, Ministry of Health Republic of Indonesia: Jakarta, Indonesia, 2014. [Google Scholar]
- Soliman, A.T.; Al Dabbagh, M.M.; Habboub, A.H.; Adel, A.; Humaidy, N.A.; Abushahin, A. Linear growth in children with iron deficiency anemia before and after treatment. J. Trop. Pediatr. 2009, 55, 324–327. [Google Scholar] [CrossRef] [PubMed]

| n | Age (months) | Height (cm) | HAZ | Stunting (≤−2 HAZ) | Weight (kg) | BMI (kg/m2) | BMIZ | Underweight (≤−2 BMIZ) | Overweight or Obese (≥1 BMIZ) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | % | Mean ± SD | Mean ± SD | Mean ± SD | % | % | ||
| Boy | 43 | 115.2 ± 8.9 | 125.9 ± 5.4 | −1.55 ± 0.81 | 30.2 | 26.5 ± 5.9 | 16.6 ± 2.8 | −0.06 ± 1.19 | 4.7 | 20.9 |
| Girl | 25 | 113.6 ± 8.5 | 125.1 ± 6.2 | −1.66 ± 0.95 | 36.0 | 25.0 ± 4.1 | 15.9 ± 2.0 | −0.37 ± 0.99 | 0.0 | 13.6 |
| Both | 68 | 114.6 ± 8.8 | 125.6 ± 5.7 | −1.59 ± 0.86 | 32.4 | 25.9 ± 5.3 | 16.3 ± 2.6 | −0.17 ± 1.12 | 2.9 | 17.6 |
| Energy (kcal) | Protein (g) | Fat (g) | Carbohydrate (g) | Calcium (mg) | Phosphorus (mg) | Iron (mg) | Vitamin A (μgRE) | Vitamin C (mg) | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | 544.8 | 13.3 | 11.3 | 123.6 | 80.9 | 532.8 | 4.5 | 284.5 | 29.5 |
| SD | 68.4 | 2.5 | 4.3 | 132.8 | 30.3 | 745.2 | 1.8 | 170.7 | 21.9 |
| % RDA/day * | 29 | 27 | 16 | 49 | 8 | 107 | 45 | 57 | 66 |
| Before the Intervention | During the Intervention | Difference | |||
|---|---|---|---|---|---|
| Amount of Intake | NAR (%) | Amount of Intake | NAR (%) | ||
| (Mean ± SD) | (Mean ± SD) | ||||
| Energy (kcal) | 1654 ± 640 | 89.4 | 1660 ± 465 | 89.7 | ns |
| Protein (g) | 36.7 ± 16.6 | 75.0 | 41.7 ± 13.6 | 85.1 | p < 0.05 |
| Fat (g) | 47.3 ± 26.0 | 65.6 | 36.6 ± 15.9 | 50.9 | p < 0.001 |
| Carbohydrate (g) | 262 ± 98 | 103.2 | 298 ± 129 | 117.4 | ns |
| Calcium (mg) | 205 ± 185 | 20.5 | 240 ± 155 | 24.0 | p < 0.05 |
| Phosphorus (mg) | 418 ± 403 | 83.6 | 426 ± 207 | 85.3 | ns |
| Iron (mg) | 9.7 ± 5.6 | 97.2 | 10.2 ± 4.4 | 102.2 | ns |
| Vitamin A (μgRE) | 300 ± 230 | 60.0 | 279 ± 176 | 55.9 | ns |
| Vitamin C (mg) | 12.5 ± 21.5 | 27.8 | 64.0 ± 28.0 | 142.3 | p < 0.001 |
| Before Intervention | After Intervention | p (Baseline Anemia Status) | p (Time) | Interaction | |||
|---|---|---|---|---|---|---|---|
| Baseline Anemia (n = 17) | Baseline Non-Anemia (n = 34) | Baseline Anemia (n = 17) | Baseline Non-Anemia (n = 34) | ||||
| Hemoglobin (g/dL) a | 11.2 ± 0.9 | 12.6 ± 0.6 | 11.9 ± 0.9 | 12.6 ± 0.7 | p < 0.01 | p < 0.001 | p < 0.01 |
| Hematocrit (%) a | 31.7 ± 3.0 | 36.5 ± 1.6 | 34.0 ± 2.7 | 36.5 ± 1.9 | p < 0.01 | p < 0.001 | p < 0.01 |
| Before Intervention | After Intervention | p (Baseline BMIZ) | p (Time) | Interaction | |||
|---|---|---|---|---|---|---|---|
| Baseline <1 BMIZ (n = 54) | Baseline ≥1 BMIZ (n = 12) | Baseline <1 BMIZ (n = 54) | Baseline ≥1 BMIZ (n = 12) | ||||
| BMI (kg/m2) a | 15.4 ± 1. | 20.5 ± 3.4 | 15.7 ± 0.9 | 20.5 ± 3.8 | p < 0.001 | ns | ns |
| BMIZ b | −0.57 ± 0.68 | 1.70 ± 0.87 | −0.47 ± 0.62 | 1.61 ± 1.01 | p < 0.001 | ns | ns |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekiyama, M.; Roosita, K.; Ohtsuka, R. Locally Sustainable School Lunch Intervention Improves Hemoglobin and Hematocrit Levels and Body Mass Index among Elementary Schoolchildren in Rural West Java, Indonesia. Nutrients 2017, 9, 868. https://doi.org/10.3390/nu9080868
Sekiyama M, Roosita K, Ohtsuka R. Locally Sustainable School Lunch Intervention Improves Hemoglobin and Hematocrit Levels and Body Mass Index among Elementary Schoolchildren in Rural West Java, Indonesia. Nutrients. 2017; 9(8):868. https://doi.org/10.3390/nu9080868
Chicago/Turabian StyleSekiyama, Makiko, Katrin Roosita, and Ryutaro Ohtsuka. 2017. "Locally Sustainable School Lunch Intervention Improves Hemoglobin and Hematocrit Levels and Body Mass Index among Elementary Schoolchildren in Rural West Java, Indonesia" Nutrients 9, no. 8: 868. https://doi.org/10.3390/nu9080868
APA StyleSekiyama, M., Roosita, K., & Ohtsuka, R. (2017). Locally Sustainable School Lunch Intervention Improves Hemoglobin and Hematocrit Levels and Body Mass Index among Elementary Schoolchildren in Rural West Java, Indonesia. Nutrients, 9(8), 868. https://doi.org/10.3390/nu9080868





