Nutritional Risk, Micronutrient Status and Clinical Outcomes: A Prospective Observational Study in an Infectious Disease Clinic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Data Collection
2.3. Assessment of Malnutrition Risk
2.4. Laboratory Analysis
2.5. Statistical Analysis
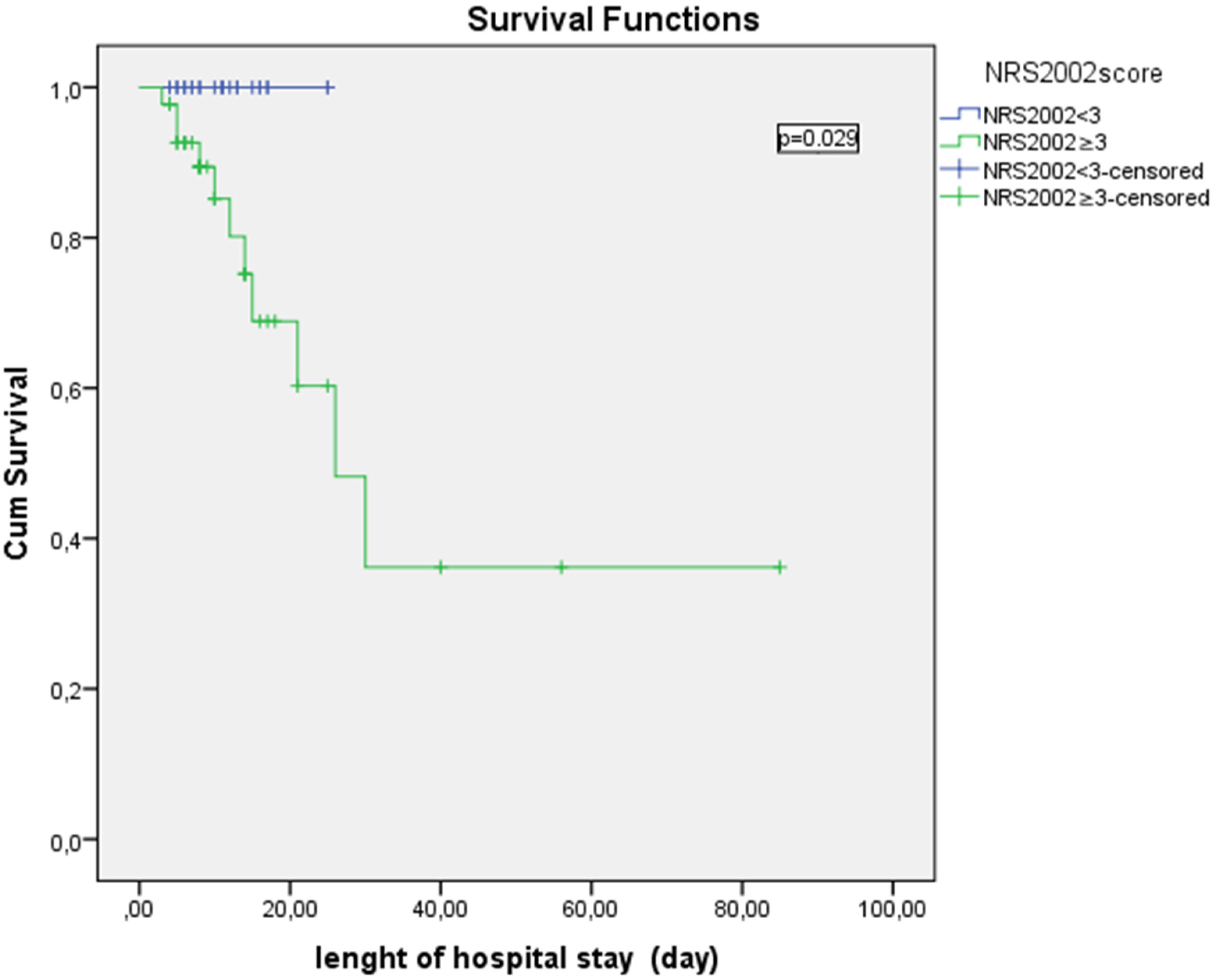
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mercadal-Orfila, G.; Lluch-Taltavull, J.; Campillo-Artero, C.; Torrent-Quetglas, M. Association between nutritional risk based on the NRS-2002 test and hospital morbidity and mortality. Nutr. Hosp. 2012, 27, 1248–1254. [Google Scholar] [PubMed]
- Edington, J.; Boorman, J.; Durrant, E.R.; Perkins, A.; Giffin, C.V.; James, R.; Thomson, J.M.; Oldroyd, J.C.; Smith, J.C.; Torrance, A.D.; et al. Prevalence of malnutrition on admission to four hospitals in England. Clin. Nutr. 2000, 19, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Waitzberg, D.L.; Caiaffa, W.T.; Correia, M.I.T.D. Hospital malnutrition: The Brazilian National Survey (IBRANUTRI): A study of 4000 patients. Nutrition 2001, 17, 573–580. [Google Scholar] [CrossRef]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Kondrup, J.; Prokopowicz, J.; Schiesser, M.; Krähenbühl, L.; Meier, R.; Liberda, M. EuroOOPS: An international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin. Nutr. 2008, 27, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Stratton, R.J.; Hackston, A.; Longmore, D.; Dixon, R.; Price, S.; Stroud, M.; King, C.; Elia, M. Malnutrition in hospital outpatients and inpatients: Prevalence, concurrent validity and ease of use of the “malnutrition universal screening tool” (“MUST”) for adults. Br. J. Nutr. 2004, 92, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Pirlich, M.; Schutz, T.; Norman, K.; Gastell, S.; Lubke, H.J.; Bischoff, S.C.; Bolder, U.; Frieling, T.; Güldenzoph, H.; Hahn, K.; et al. The German hospital malnutrition study. Clin. Nutr. 2006, 25, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Caccialanza, R.; Klersy, C.; Cereda, E.; Cameletti, B.; Bonoldi, A.; Bonardi, C.; Marinelli, M.; Dionigi, P. Nutritional parameters associated with prolonged hospital stay among ambulatory adult patients. CMAJ 2010, 182, 1843–1849. [Google Scholar] [CrossRef] [PubMed]
- Keusch, G.T. The history of nutrition: Malnutrition, infection and immunity. J. Nutr. 2003, 133, 336–340. [Google Scholar]
- Chandra, R.K. Nutrition and the immune system: An introduction. Am. J. Clin. Nutr. 1997, 66, 460–463. [Google Scholar]
- Bhaskaram, P. Micronutrient malnutrition, infection, and immunity: An overview. Nutr. Rev. 2002, 60, 40–45. [Google Scholar] [CrossRef]
- Maggini, S.; Wintergerst, E.S.; Beveridge, S.; Hornig, D.H. Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. Br. J. Nutr. 2007, 98, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Cunningham-Rundles, S.; Ahrn, S.; Abuav-Nussbaum, R.; Dnistrian, A. Development of immunocompetence: Role of micronutrients and microorganisms. Nutr. Rev. 2002, 60, 68–72. [Google Scholar] [CrossRef]
- Dellinger, R.P.; Levy, M.M.; Carlet, J.M.; Bion, J.; Parker, M.M.; Jaeschke, R.; Reinhart, K.; Angus, D.C.; Brun-Buisson, C.; Beale, R.; et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit. Care Med. 2008, 36, 296–327. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z.; Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Velasco, C.; Garcia, E.; Rodriguez, V.; Frias, L.; Garriga, R.; Alvarez, J.; García-Peris, P.; León, M. Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: A multicentre study. Eur. J. Clin. Nutr. 2011, 65, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Bo, M.; Massaia, M.; Raspo, S.; Bosco, F.; Cena, P.; Molaschi, M.; Fabris, F. Predictive factors of in-hospital mortality in older patients admitted to a medical intensive care unit. J. Am. Geriatr. Soc. 2003, 51, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S.; et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.; Cull, W.; Henderson, W.; Daley, J.; Hur, K.; Khuri, S.F. Preoperative serum albumin level as a predictor of operative mortality and morbidity: Results from the National VA Surgical Risk Study. Arch. Surg. 1999, 134, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Kuzuya, M.; Izawa, S.; Enoki, H.; Okada, K.; Iguchi, A. Is serum albumin a good marker for malnutrition in the physically impaired elderly? Clin. Nutr. 2007, 26, 84–90. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Izaola, O.; Cuellar, L.; Terroba, M.C.; Cabezas, G.; Rojo, S.; Aller, R.; Sagrado, M.G. Nutritional assessment: Predictive variables at hospital admission related with length of stay. Ann. Nutr. Metab. 2006, 50, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Gariballa, S.; Forster, S. Effects of acute-phase response on nutritional status and clinical outcome of hospitalized patients. Nutrition 2006, 22, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Rodríguez, M.; Medina-Cuadros, M.; Gómez-Ortega, A.; Martínez-Gallego, G.; Mariscal-Ortiz, M.; Martinez-Gonzalez, M.A.; Sillero-Arenas, M. Cholesterol and serum albumin levels as predictors of cross infection, death, and length of hospital stay. Arch. Surg. 2002, 137, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Erez, A.; Shental, O.; Tchebiner, J.Z.; Laufer-Perl, M.; Wasserman, A.; Sella, T.; Guzner-Gur, H. Diagnostic and prognostic value of very high serum lactate dehydrogenase in admitted medical patients. Isr. Med. Assoc. J. 2014, 16, 439–443. [Google Scholar] [PubMed]
- Donnino, M.W.; Carney, E.; Cocchi, M.N.; Barbash, I.; Chase, M.; Joyce, N.; Chou, P.P.; Ngo, L. Thiamine deficiency in critically ill patients with sepsis. J. Crit. Care 2010, 25, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Costa, N.A.; Gut, A.L.; de Souza Dorna, M.; Pimentel, J.A.; Cozzolino, S.M.; Azevedo, P.S.; Fernandes, A.A.; Zornoff, L.A.; de Paiva, S.A.; Minicucci, M.F. Serum thiamine concentration and oxidative stress as predictors of mortality in patients with septic shock. J. Crit. Care 2014, 29, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Cruickshank, A.M.; Telfer, A.B.; Shenkin, A. Thiamine deficiency in the critically ill. Intensive Care Med. 1988, 14, 384–387. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, T.; O’Neill, M.; Webb, S.A.; Ho, K.M. Prevalence of vitamin deficiencies on admission: Relationship to hospital mortality in critically ill patients. Anaesth. Intensive Care 2009, 37, 254–260. [Google Scholar] [PubMed]
- Forceville, X.; Vitoux, D.; Gauzit, R.; Combes, A.; Lahilaire, P.; Chappuis, P. Selenium, systemic immune response syndrome, sepsis, and outcome in critically ill patients. Crit. Care Med. 1998, 26, 1536–1544. [Google Scholar] [CrossRef] [PubMed]
- Manzanares, W.; Biestro, A.; Galusso, F.; Torre, M.H.; Mañay, N.; Pittini, G.; Facchin, G.; Hardy, G. Serum selenium and glutathione peroxidase-3 activity: Biomarkers of systemic inflammation in the critically ill? Intensive Care Med. 2009, 35, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Sakr, Y.; Reinhart, K.; Bloos, F.; Marx, G.; Russwurm, S.; Bauer, M.; Brunkhorst, F. Time course and relationship between plasma selenium concentrations, systemic inflammatory response, sepsis, and multiorgan failure. Br. J. Anaesth. 2007, 98, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Rayman, M.P. The importance of selenium to human health. Lancet 2000, 356, 233–241. [Google Scholar] [CrossRef]
- Berger, M.M. Can oxidative damage be treated nutritionally? Clin. Nutr. 2005, 24, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.H.; Prasad, A.S. Zinc and immune function: The biological basis of altered resistance to infection. Am. J. Clin. Nutr. 1998, 68, 447–463. [Google Scholar]
- Wolman, S.L.; Anderson, G.H.; Marliss, E.B.; Jeejeebhoy, K.N. Zinc in total parenteral nutrition: Requirements and metabolic effects. Gastroenterology 1979, 76, 458–467. [Google Scholar] [PubMed]
- Mertens, K.; Lowes, D.A.; Webster, N.R.; Talib, J.; Hall, L.; Davies, M.J.; Beattie, J.H.; Galley, H.F. Low zinc and selenium concentrations in sepsis are associated with oxidative damage and inflammation. Br. J. Anaesth. 2015, 114, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Yakoob, M.Y.; Theodoratou, E.; Jabeen, A.; Imdad, A.; Eisele, T.P.; Ferguson, J.; Jhass, A.; Rudan, I.; Campbell, H.; Black, R.E.; et al. Preventive zinc supplementation in developing countries: Impact on mortality and morbidity due to diarrhea, pneumonia and malaria. BMC Public Health 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Richard, S.A.; Black, R.E. Zinc supplementation for the prevention of acute lower respiratory infection in children in developing countries: Meta-analysis and meta-regression of randomized trials. Int. J. Epidemiol. 2010, 39, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Barceloux, D.G. Copper. J. Toxicol. Clin. Toxicol. 1999, 37, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Songchitsomboon, S.; Komindr, S.; Komindr, A.; Kulapongse, S.; Puchaiwatananon, O.; Udomsubpayakul, U. Serum copper and zinc levels in Thai patients with various diseases. J. Med. Assoc. Thail. 1999, 82, 701–706. [Google Scholar]
- Lee, M.J.; Alvarez, J.A.; Smith, E.M.; Killilea, D.W.; Chmiel, J.F.; Joseph, P.M.; Grossmann, R.E.; Gaggar, A.; Ziegler, T.R.; Tangpricha, V. Vitamin D for enhancing the immune system in cystic fibrosis investigators. changes in mineral micronutrient status during and after pulmonary exacerbation in adults with cystic fibrosis. Nutr. Clin. Pract. 2015, 30, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Malavolta, M.; Giacconi, R.; Piacenza, F.; Santarelli, L.; Cipriano, C.; Costarelli, L.; Tesei, S.; Pierpaoli, S.; Basso, A.; Galeazzi, R.; et al. Plasma copper/zinc ratio: An inflammatory/nutritional biomarker as predictor of all-cause mortality in elderly population. Biogerontology 2010, 11, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, R.; Upreti, R.K.; Seth, P.K.; Chaturvedi, U.C. Effects of chromium on the immune system. FEMS Immunol. Med. Microbiol. 2002, 34, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gavin, I.M.; Gillis, B.; Arbieva, Z.; Prabhakar, B.S. Identification of human cell responses to hexavalent chromium. Environ. Mol. Mutagen. 2007, 48, 650–657. [Google Scholar] [CrossRef] [PubMed]
| Variables | All Patients n:68 | Male Patients (n:37) | Female Patients (n:31) |
|---|---|---|---|
| Age (year), mean ± SD | 62.8 ± 17.5 | 62 ± 15.9 | 63.8 ± 19.4 |
| Weight at admission (kg), mean ± SD | 69 ± 13.8 | 71.4 ± 14.1 | 66.3 ± 13.3 |
| Weight at discharge (kg), mean ± SD | 69.5 ± 14.1 | 72.2 ± 14.3 | 66.4 ± 13.6 |
| Height (cm), mean ± SD | 167.8 ± 10.9 | 175.1 ± 7.9 | 159.2 ± 7.1 |
| BMI (kg/m2), median (Q1 and Q3) | 23.9 (20.9–27.7) | 22.1 (20.4–25.3) | 25 (22.3–29.4) |
| SIRS, n (%) | 28 (41.2) | 15 (40.5) | 13 (41.9) |
| Sepsis, n (%) | 18 (26.5) | 9 (24.3) | 9 (29) |
| Length of hospital stay (day), median (range) | 10 (3–85) | 8 (3–85) | 10 (4–26) |
| Death, n (%) | 11(16.2) | 6 (16.2) | 5 (16.1) |
| Types of infection, n (%) | |||
| Urinary infections | 16 (23.5) | 6 (16.2) | 10 (32.3) |
| Pneumonia | 15 (22.1) | 9 (24.3) | 6 (19.4) |
| Soft tissue infections | 11 (16.2) | 7 (18.9) | 4 (12.9) |
| Pneumonia plus urinary infections | 5 (7.4) | 3 (8.1) | 2 (6.5) |
| Foreign body infections | 5 (7.4) | 1 (2.7) | 4 (12.9) |
| Tuberculosis | 4 (5.9) | 3 (8.1) | 1 (3.2) |
| Meningitis | 2 (2.9) | 1 (2.7) | 1 (3.2) |
| Protozoal infections | 2 (2.9) | 2 (5.4) | - |
| Abscess | 2 (2.9) | 1 (2.7) | 1 (3.2) |
| Other bacterial infections | 6 (8.8) | 4 (10.8) | 2 (6.5) |
| Nutrition type during hospital stay, n (%) | |||
| Oral | 51 (75) | 29 (78.4) | 22 (71) |
| Parenteral | 5 (7.4) | 3 (8.1) | 2 (6.5) |
| Enteral | 1 (1.5) | - | 1 (3.2) |
| Oral plus parenteral | 8 (11.8) | 5 (13.5) | 3 (9.7) |
| Oral plus enteral | 2 (2.9) | - | 2 (6.5) |
| Enteral plus parenteral | 1 (1.5) | - | 1 (3.2) |
| NRS-2002 score, median (range) | |||
| on admission | 3 (1–7) | 3 (1–7) | 3 (1–7) |
| at first week | 2 (1–7) | 3 (1–7) | 2 (1–7) |
| at discharge | 2 (1–7) | 2 (1–7) | 2 (1–7) |
| Ceruloplasmin level (g/L), mean ± SD | 0.89 ± 4.5 | 1.28 ± 5.8 | 0.3 ± 0.8 |
| Micronutrients levels | |||
| Zinc (µg/dL), median (Q1 and Q3) | 64 (50.5–81.7) | 65 (53.5–77.5) | 62 (47.8–91.8) |
| Copper (µg/dL), mean ± SD | 141.9 ± 41.9 | 139.9 ± 40.3 | 144.9 ± 44.9 |
| Thiamine (ng/mL), median (Q1 and Q3) | 39.1 (26.7–78.1) | 37.7 (26.8–69.2) | 42.2 (25.1–93.2) |
| Selenium (µg/L), median (Q1 and Q3) | 49.9 (39.5–62.3) | 49.3 (37.6–62.7) | 50.5 (42–62.3) |
| Chromium (µg/L), mean ± SD | 11.4 ± 6 | 11.7 ± 6.5 | 11 ± 5.5 |
| Vitamin B6 (ng/mL), median (Q1 and Q3) | 6.4 (3.1–15.5) | 4.8 (2.6–11.2) | 8 (4.6–27.3) |
| Vitamin B12 (pg/mL), median (Q1 and Q3) | 260 (151.5–469.5) | 249 (142–419) | 304 (174–608) |
| Variables | SIRS | p | Sepsis | p | Death | p | |||
|---|---|---|---|---|---|---|---|---|---|
| Positive Negative (n:28) (n:40) | Positive Negative (n:18) (n:50) | Positive Negative (n:11) (n:57) | |||||||
| Thiamine (ng/mL) | 37.8 (19.6–66.5) | 42.2 (30.1–95.7) | 0.044 | 28.3 (18.7–58.3) | 42.2 (29.6–88.9) | 0.032 | 29.6 (24.1–53.3) | 42 (27.7–81.6) | 0.247 |
| Vitamin B6 (ng/mL) | 6.1 (2.3–17.4) | 6.4 (3.5–14.8) | 0.596 | 8.6 (2.1–21.7) | 6 (3.5–14.1) | 0.813 | 10.6 (2.2–21.1) | 5.8 (3.1–15.4) | 0.696 |
| Zinc (µg/dL) | 59 (47.2–67) | 69 (53.5–91.7 | 0.042 | 59 (46–69.2) | 65.5 (52.7–88.7) | 0.131 | 62 (47–78) | 65 (51–84) | 0.681 |
| Copper (µg/dL) | 140 (114.7–171.2) | 141 (110–158) | 0.699 | 137.2 ± 48.4 | 143.9 ± 39.2 | 0.577 | 131.3 ± 58.2 | 144.3 ± 37.6 | 0.493 |
| Selenium (µg/L) | 45.6 (36.9–60.4) | 52.6 (42.4–63.6) | 0.229 | 49.8 ± 14.6 | 51.9 ± 13.9 | 0.596 | 48.1 ± 11.7 | 51.9 ± 14.4 | 0.408 |
| Vitamin B12 (pg/mL) | 318 (191.2–533.5) | 218 (134.2–347) | 0.144 | 409.5 (145.7–650) | 235.5 (160.5–376.5) | 0.124 | 421 (127–609) | 228 (157–466.5) | 0.237 |
| Chromium (µg/L) | 12.4 ± 5 | 10.6 ± 6.5 | 0.193 | 14.4 (11.4–16.4) | 8.5 (5.1–16.4) | 0.027 | 14.3 ± 4.5 | 10.8 ± 6.1 | 0.043 |
| Multiple micronutrients deficiency | 13 (46.4) | 9 (22.5) | 0.07 | 8 (44.4) | 14 (28) | 0.325 | 5 (45.5) | 17 (29.8) | 0.508 |
| Cu/Zn ratio | 2.54 ± 1.00 | 2.06 ± 0.85 | 0.051 | 2.42 ± 0.93 | 2.23 ± 0.96 | 0.471 | 2.18 ± 0.99 | 2.31 ± 0.94 | 0.694 |
| NRS-2002 score on admission | 5 (3.25–6) | 2 (2–3) | <0.001 | 5 (4–6) | 3 (2–4) | <0.001 | 5 (5–7) | 3 (2–4) | <0.001 |
| Albumin | 2.86 ± 0.56 | 3.78 ± 0.53 | <0.001 | 2.69 ± 0.51 | 3.66 ± 0.58 | <0.001 | 2.52 ± 0.48 | 3.57 ± 0.61 | <0.001 |
| BMI | 23.2 (20.9–27.3) | 23.9 (20.8–27.8) | 0.861 | 23.2 (21.2–26.5) | 23.9 (20.6–27.7) | 0.868 | 24 (21.3–25.6) | 23.9 (20.8–27.8) | 0.920 |
| Risk Factors | OR | 95% CI | p |
|---|---|---|---|
| Univariate analysis | |||
| Thiamine level | 0.98 | 0.97–1.00 | 0.074 |
| Zinc level | 0.98 | 0.95–1.00 | 0.067 |
| Chromium level | 1.05 | 0.97–1.14 | 0.211 |
| Selenium level | 0.98 | 0.94–1.01 | 0.323 |
| Multiple micronutrients deficiency | 2.98 | 1.04–8.53 | 0.041 |
| NRS-2002 score on admission | 3.56 | 1.97–6.43 | <0.001 |
| Age | 1.03 | 1.005–1.07 | 0.022 |
| CRP | 1.01 | 1.004–1.019 | 0.002 |
| BMI | 0.97 | 0.87–1.08 | 0.589 |
| Gender | 0.94 | 0.35–2.48 | 0.907 |
| Glucose | 1.01 | 1.004–1.019 | 0.004 |
| Urea | 1.02 | 1.004–1.04 | 0.016 |
| Leukocyte count | 1.00 | 1.00–1.00 | 0.002 |
| Hemoglobin | 0.79 | 0.62–1.01 | 0.064 |
| Albumin | 0.06 | 0.01–0.21 | <0.001 |
| LDH | 1.00 | 0.99–1.007 | 0.183 |
| Multiple analysis | |||
| Albumin | 0.02 | 0.002–0.260 | 0.002 |
| NRS-2002 on admission | 2.74 | 1.23–6.08 | 0.013 |
| Glucose | 1.01 | 1.003–1.03 | 0.018 |
| Risk Factors | OR | 95% CI | p |
|---|---|---|---|
| Univariate analysis | |||
| Thiamine | 0.98 | 0.97–1.004 | 0.157 |
| Zinc | 0.98 | 0.95–1.006 | 0.145 |
| Chromium | 1.09 | 1.00–1.20 | 0.051 |
| Selenium | 0.98 | 0.95–1.02 | 0.590 |
| Multiple micronutrients deficiency | 0.48 | 0.15–1.48 | 0.205 |
| NRS-2002 score on admission | 3.40 | 1.89–6.13 | <0.001 |
| Age | 1.04 | 1.009–1.08 | 0.015 |
| CRP | 1.00 | 1.001–1.01 | 0.022 |
| BMI | 0.99 | 0.88–1.11 | 0.924 |
| Gender | 0.78 | 0.26–2.31 | 0.662 |
| Glucose | 1.00 | 0.99–1.009 | 0.330 |
| Urea | 1.02 | 1.008–1.04 | 0.005 |
| Leukocyte count | 1.00 | 1.00–1.00 | 0.043 |
| Hemoglobin | 0.68 | 0.51–0.91 | 0.010 |
| Albumin | 0.05 | 0.01–0.23 | <0.001 |
| LDH | 1.00 | 1.00–1.002 | 0.199 |
| Multiple analysis | |||
| Albumin | 0.07 | 0.01–0.44 | 0.004 |
| NRS-2002 on admission | 2.92 | 1.43–5.97 | 0.003 |
| Risk Factors | HR | 95% CI | p |
|---|---|---|---|
| Univariate analysis | |||
| Age | 1.03 | 0.99–1.07 | 0.095 |
| BMI | 0.95 | 0.83–1.10 | 0.543 |
| Chromium | 1.057 | 0.95–1.16 | 0.276 |
| Thiamine | 0.99 | 0.98–1.009 | 0.436 |
| Zinc | 0.99 | 0.96–1.01 | 0.425 |
| Selenium | 0.99 | 0.95–1.04 | 0.864 |
| Multiple micronutrients deficiency | 0.61 | 0.18–2.03 | 0.424 |
| NRS-2002 score on admission | 2.79 | 1.55–5.03 | 0.001 |
| Urea | 1.01 | 1.001–1.019 | 0.037 |
| Hemoglobin | 0.64 | 0.44–0.92 | 0.018 |
| Albumin | 0.139 | 0.04–0.45 | 0.001 |
| LDH | 1.004 | 1.000–1.008 | 0.034 |
| Leukocyte count | 1.00 | 1.000–1.000 | 0.622 |
| Multiple analysis | |||
| Albumin | 0.133 | 0.02–0.86 | 0.035 |
| NRS-2002 score on admission | 6.105 | 1.49–24.95 | 0.012 |
| LDH | 1.004 | 1.001–1.008 | 0.011 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dizdar, O.S.; Baspınar, O.; Kocer, D.; Dursun, Z.B.; Avcı, D.; Karakükcü, C.; Çelik, İ.; Gundogan, K. Nutritional Risk, Micronutrient Status and Clinical Outcomes: A Prospective Observational Study in an Infectious Disease Clinic. Nutrients 2016, 8, 124. https://doi.org/10.3390/nu8030124
Dizdar OS, Baspınar O, Kocer D, Dursun ZB, Avcı D, Karakükcü C, Çelik İ, Gundogan K. Nutritional Risk, Micronutrient Status and Clinical Outcomes: A Prospective Observational Study in an Infectious Disease Clinic. Nutrients. 2016; 8(3):124. https://doi.org/10.3390/nu8030124
Chicago/Turabian StyleDizdar, Oguzhan Sıtkı, Osman Baspınar, Derya Kocer, Zehra Bestepe Dursun, Deniz Avcı, Cigdem Karakükcü, İlhami Çelik, and Kursat Gundogan. 2016. "Nutritional Risk, Micronutrient Status and Clinical Outcomes: A Prospective Observational Study in an Infectious Disease Clinic" Nutrients 8, no. 3: 124. https://doi.org/10.3390/nu8030124
APA StyleDizdar, O. S., Baspınar, O., Kocer, D., Dursun, Z. B., Avcı, D., Karakükcü, C., Çelik, İ., & Gundogan, K. (2016). Nutritional Risk, Micronutrient Status and Clinical Outcomes: A Prospective Observational Study in an Infectious Disease Clinic. Nutrients, 8(3), 124. https://doi.org/10.3390/nu8030124





