Topical Application of Apricot Kernel Extract Improves Dry Eye Symptoms in a Unilateral Exorbital Lacrimal Gland Excision Mouse
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Apricot Kernel Extract
2.2. Animals and Experimental Design
2.3. Tear Measurement
2.4. Corneal Fluorescein Staining
2.5. Corneal Irregularity Analysis
2.6. Immunohistochemistry
2.7. Western Blot Analysis
2.8. Statistical Analysis
3. Results
3.1. Standardization of AKE
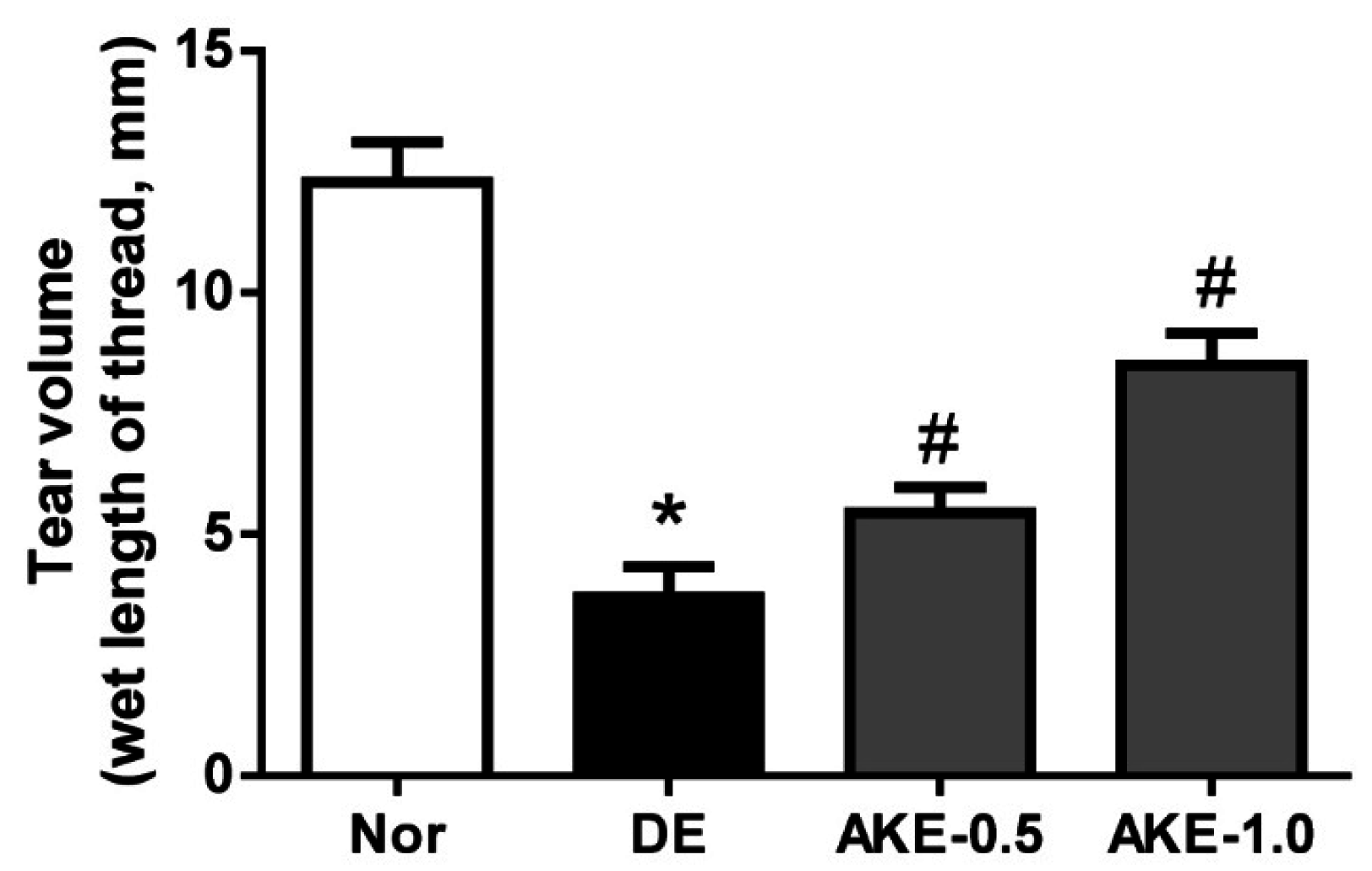
3.2. AKE Improves Tear Secretion
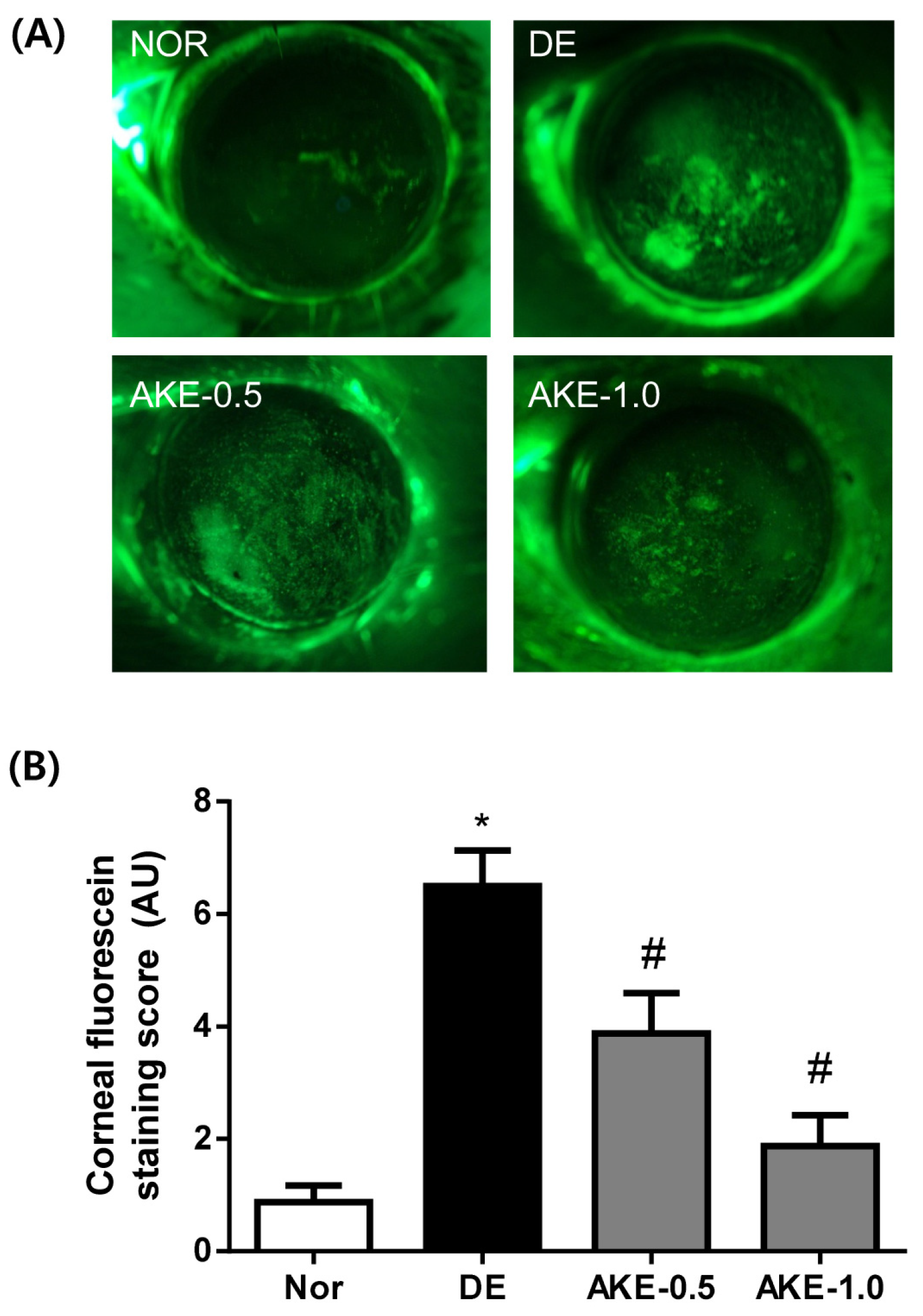
3.3. AKE Prevents Corneal Epithelial Damage
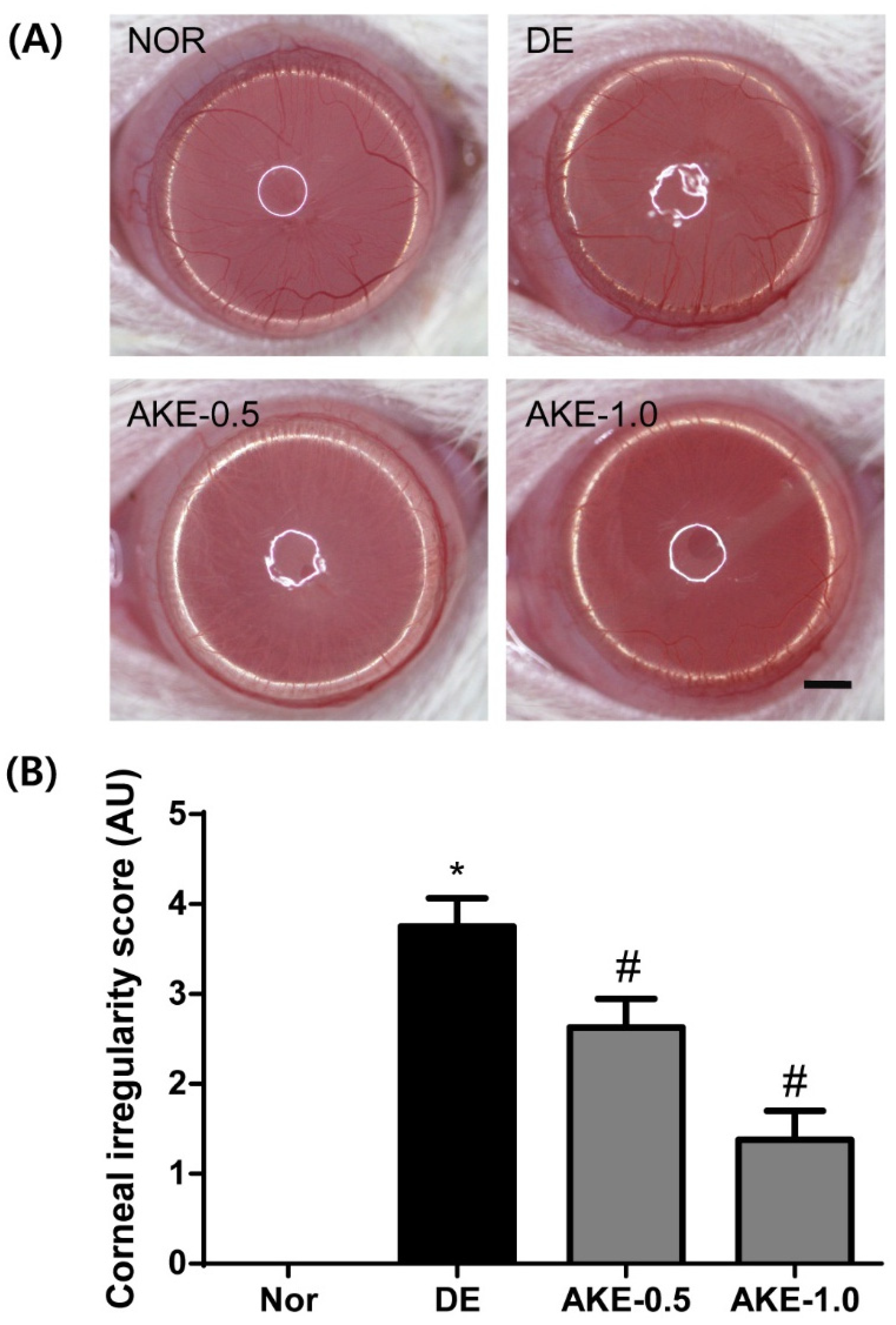
3.4. AKE Inhibits Corneal Regularization
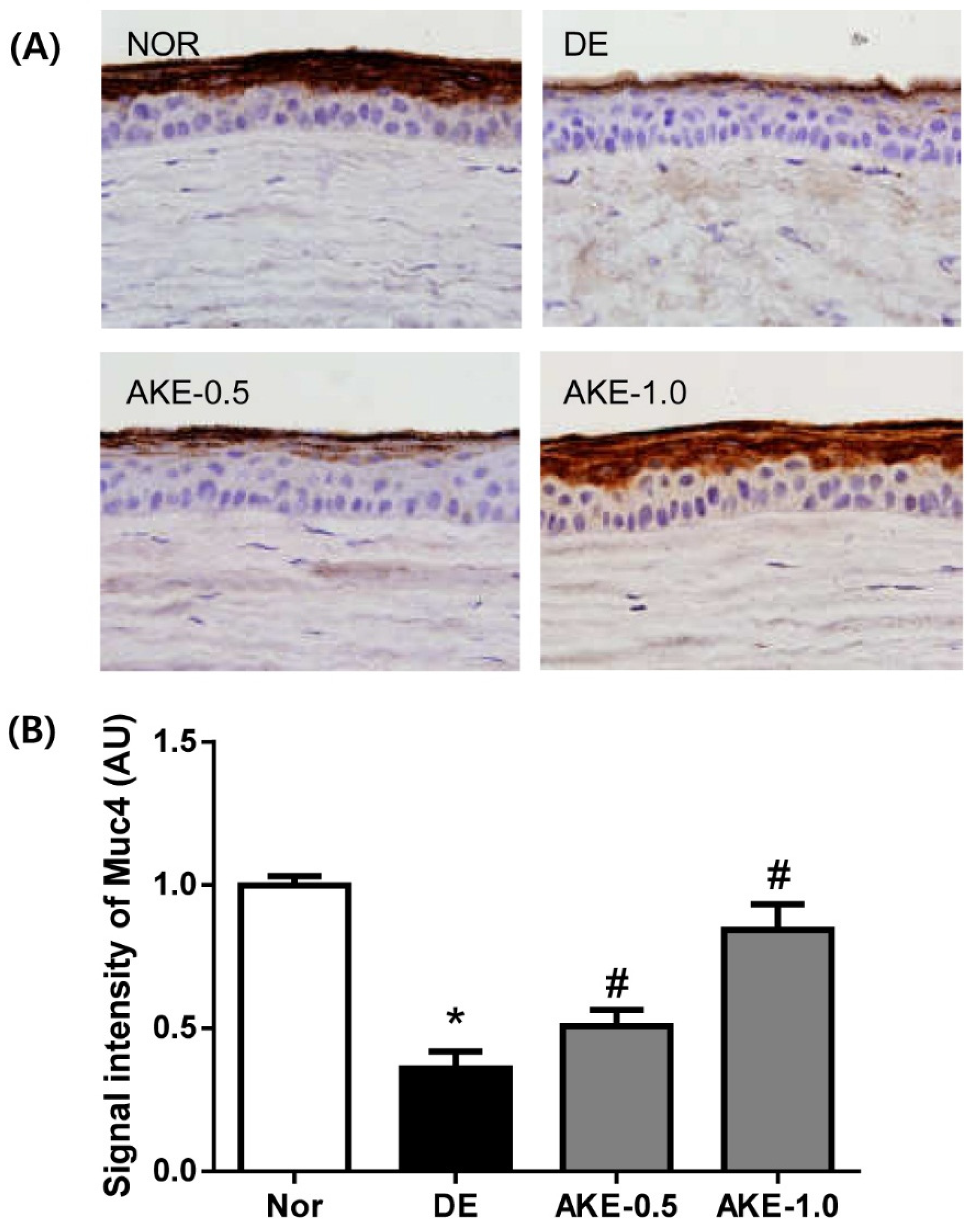
3.5. AKE Inhibits Corneal Mucin Alteration
3.6. AKE Suppresses the Expression of TNF-α
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Abelson, M.B.; Ousler, G.W., III; Maffei, C. Dry eye in 2008. Curr. Opin. Ophthalmol. 2009, 20, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Tavares Fde, P.; Fernandes, R.S.; Bernardes, T.F.; Bonfioli, A.A.; Soares, E.J. Dry eye disease. Semin. Ophthalmol. 2010, 25, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Shimmura, S.; Ono, M.; Shinozaki, K.; Toda, I.; Takamura, E.; Mashima, Y.; Tsubota, K. Sodium hyaluronate eyedrops in the treatment of dry eyes. Br. J. Ophthalmol. 1995, 79, 1007–1011. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Goto, E.; Fujita, H.; Ono, M.; Inoue, H.; Saito, I.; Shimmura, S. Treatment of dry eye by autologous serum application in Sjogren’s syndrome. Br. J. Ophthalmol. 1999, 83, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Condon, P.I.; McEwen, C.G.; Wright, M.; Mackintosh, G.; Prescott, R.J.; McDonald, C. Double blind, randomised, placebo controlled, crossover, multicentre study to determine the efficacy of a 0.1% (w/v) sodium hyaluronate solution (Fermavisc) in the treatment of dry eye syndrome. Br. J. Ophthalmol. 1999, 83, 1121–1124. [Google Scholar] [CrossRef] [PubMed]
- Takamura, E.; Tsubota, K.; Watanabe, H.; Ohashi, Y.; Diquafosol Ophthalmic Solution Phase 3 Study Group. A randomised, double-masked comparison study of diquafosol versus sodium hyaluronate ophthalmic solutions in dry eye patients. Br. J. Ophthalmol. 2012, 96, 1310–1315. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Awamura, S.; Oshiden, K.; Nakamichi, N.; Suzuki, H.; Yokoi, N.; Rebamipide Ophthalmic Suspension Phase II Study Group. Rebamipide (OPC-12759) in the treatment of dry eye: A randomized, double-masked, multicenter, placebo-controlled phase II study. Ophthalmology 2012, 119, 2471–2478. [Google Scholar] [CrossRef] [PubMed]
- Bernauer, W.; Thiel, M.A.; Kurrer, M.; Heiligenhaus, A.; Rentsch, K.M.; Schmitt, A.; Heinz, C.; Yanar, A. Corneal calcification following intensified treatment with sodium hyaluronate artificial tears. Br. J. Ophthalmol. 2006, 90, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.K.; Yang, H.Y.; Lee, T.H.; Shin, M.C.; Lee, M.H.; Shin, M.S.; Kim, C.J.; Kim, O.J.; Hong, S.P.; Cho, S. Armeniacae semen extract suppresses lipopolysaccharide-induced expressions of cyclooxygenase [correction of cycloosygenase]-2 and inducible nitric oxide synthase in mouse BV2 microglial cells. Biol. Pharm. Bull. 2005, 28, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.R.; Kang, Y.S.; Kim, S.S.; Kim, D.H.; Shin, M.K.; Song, H.J. Studies on the allergic asthma effect of semen Armeniaceae Amarum. Korea J. Herbol. 2003, 18, 201–208. [Google Scholar]
- Lv, W.F.; Ding, M.Y.; Zheng, R. Isolation and quantitation of amygdalin in Apricot-kernel and Prunus Tomentosa Thunb. by HPLC with solid-phase extraction. J. Chromatogr. Sci. 2005, 43, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.C.; Ahn, K.Y.; Choi, W.; Li, Z.; Choi, J.S.; Lee, S.H.; Park, S.H. Tear production and ocular surface changes in experimental dry eye after elimination of desiccating stress. Investig. Ophthalmol. Vis. Sci. 2011, 52, 7267–7273. [Google Scholar] [CrossRef] [PubMed]
- Sohn, E.J.; Kim, C.S.; Kim, Y.S.; Jung, D.H.; Jang, D.S.; Lee, Y.M.; Kim, J.S. Effects of magnolol (5,5′-diallyl-2,2′-dihydroxybiphenyl) on diabetic nephropathy in type 2 diabetic Goto-Kakizaki rats. Life Sci. 2007, 80, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Barceloux, D.G. Cyanogenic foods (cassava, fruit kernels, and cycad seeds). Dis. Mon. 2009, 55, 336–352. [Google Scholar] [CrossRef] [PubMed]
- De Paiva, C.S.; Corrales, R.M.; Villarreal, A.L.; Farley, W.J.; Li, D.Q.; Stern, M.E.; Pflugfelder, S.C. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp. Eye Res. 2006, 83, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Kurose, M.; Meng, I.D. Dry eye modifies the thermal and menthol responses in rat corneal primary afferent cool cells. J. Neurophysiol. 2013, 110, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Meng, I.D.; Barton, S.T.; Mecum, N.E.; Kurose, M. Corneal sensitivity following lacrimal gland excision in the rat. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3347–3354. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, W.; Chen, Y.; Lee, S.M.; Lee, H.S.; Hua, J.; Dohlman, T.; Shiang, T.; Dana, R. Extraorbital lacrimal gland excision: A reproducible model of severe aqueous tear-deficient dry eye disease. Cornea 2014, 33, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Hata, Y.; Nagata, M.; Yokoi, N.; Yamaguchi, S.; Kaku, T.; Kinoshita, S. JBP485 promotes tear and mucin secretion in ocular surface epithelia. Sci. Rep. 2015, 5, 10248. [Google Scholar] [CrossRef] [PubMed]
- Gipson, I.K.; Hori, Y.; Argueso, P. Character of ocular surface mucins and their alteration in dry eye disease. Ocul. Surf. 2004, 2, 131–148. [Google Scholar] [CrossRef]
- Inatomi, T.; Spurr-Michaud, S.; Tisdale, A.S.; Gipson, I.K. Human corneal and conjunctival epithelia express MUC1 mucin. Investig. Ophthalmol. Vis. Sci. 1995, 36, 1818–1827. [Google Scholar]
- Pflugfelder, S.C.; Liu, Z.; Monroy, D.; Li, D.Q.; Carvajal, M.E.; Price-Schiavi, S.A.; Idris, N.; Solomon, A.; Perez, A.; Carraway, K.L. Detection of sialomucin complex (MUC4) in human ocular surface epithelium and tear fluid. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1316–1326. [Google Scholar]
- Danjo, Y.; Watanabe, H.; Tisdale, A.S.; George, M.; Tsumura, T.; Abelson, M.B.; Gipson, I.K. Alteration of mucin in human conjunctival epithelia in dry eye. Investig. Ophthalmol. Vis. Sci. 1998, 39, 2602–2609. [Google Scholar]
- Argueso, P.; Balaram, M.; Spurr-Michaud, S.; Keutmann, H.T.; Dana, M.R.; Gipson, I.K. Decreased levels of the goblet cell mucin MUC5AC in tears of patients with Sjogren syndrome. Investig. Ophthalmol. Vis. Sci. 2002, 43, 1004–1011. [Google Scholar]
- Cui, X.; Hong, J.; Wang, F.; Deng, S.X.; Yang, Y.; Zhu, X.; Wu, D.; Zhao, Y.; Xu, J. Assessment of corneal epithelial thickness in dry eye patients. Optom. Vis. Sci. 2014, 91, 1446–1454. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.A.; Hyun, L.C.; Jung, S.H.; Yang, S.J. The leaves of Diospyros kaki exert beneficial effects on a benzalkonium chloride-induced murine dry eye model. Mol. Vis. 2016, 22, 284–293. [Google Scholar] [PubMed]
- Diego, J.L.; Bidikov, L.; Pedler, M.G.; Kennedy, J.B.; Quiroz-Mercado, H.; Gregory, D.G.; Petrash, J.M.; McCourt, E.A. Effect of human milk as a treatment for dry eye syndrome in a mouse model. Mol. Vis. 2016, 22, 1095–1102. [Google Scholar] [PubMed]
- Hirayama, M.; Ogawa, M.; Oshima, M.; Sekine, Y.; Ishida, K.; Yamashita, K.; Ikeda, K.; Shimmura, S.; Kawakita, T.; Tsubota, K.; et al. Functional lacrimal gland regeneration by transplantation of a bioengineered organ germ. Nat. Commun. 2013, 4, 2497. [Google Scholar] [CrossRef] [PubMed]
- Nabavizadeh, F.; Alizadeh, A.M.; Sadroleslami, Z.; Adeli, S. Gastroprotective effects of amygdalin on experimental gastric ulcer: Role of NO and TNF. J. Med. Plants Res. 2011, 5, 3122–3127. [Google Scholar]
- Capper, R.; Guo, L.; Pearson, J.P.; Birchall, J.P. Effect of nitric oxide donation on mucin production in vitro. Clin. Otolaryngol. Allied Sci. 2003, 28, 51–54. [Google Scholar] [CrossRef] [PubMed]
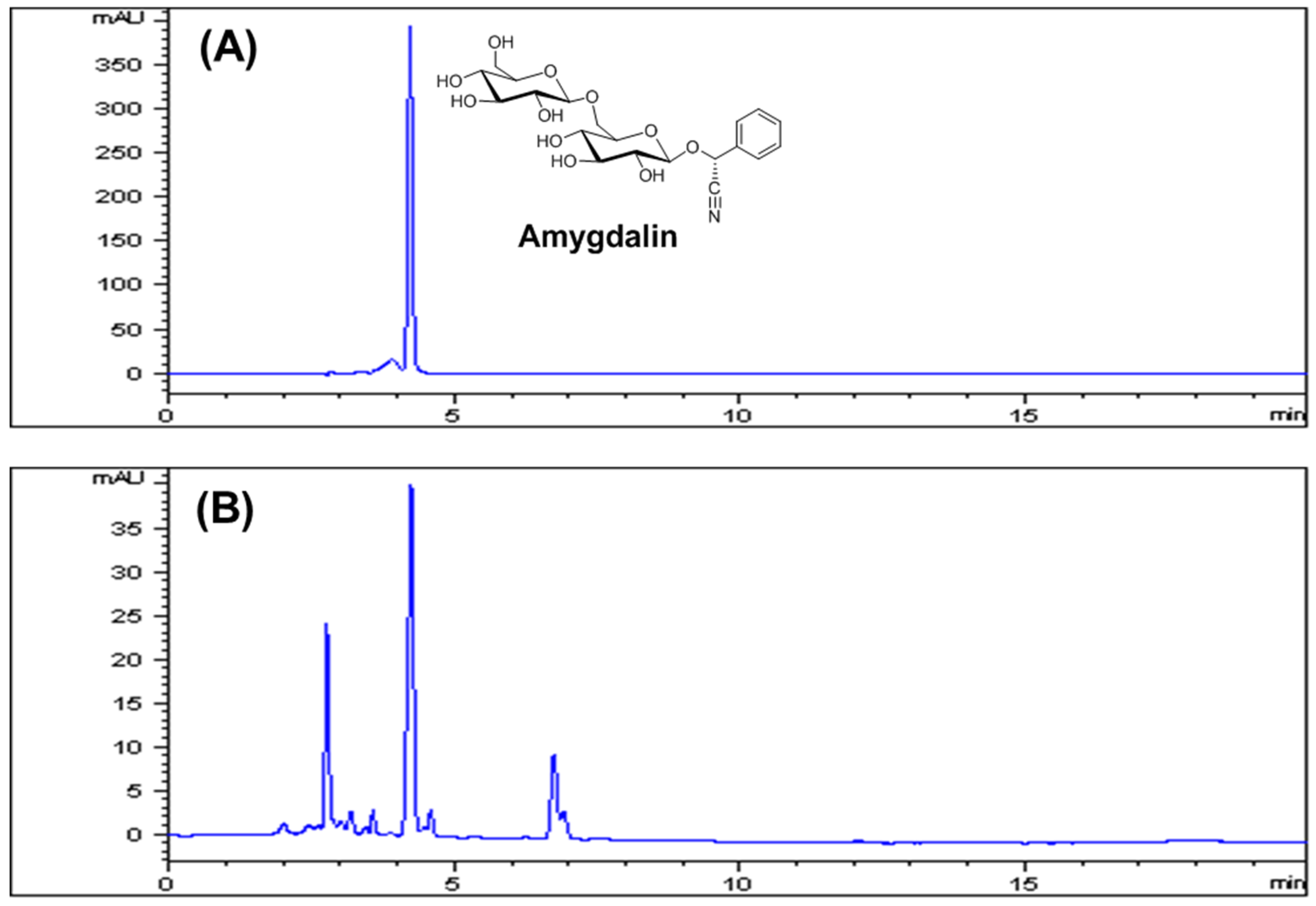

| Compound | Linear Range (μg/mL) | Regression Equation a | Correlation Coefficient (R2) |
|---|---|---|---|
| Amygdalin | 12.5–200 | y = 2.1113x + 7.35 | 0.9999 |
| Sample | Amygdalin Content (mg/g) a |
|---|---|
| Apricot kernel extract | 127.34 ± 0.99 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.-S.; Jo, K.; Lee, I.-S.; Kim, J. Topical Application of Apricot Kernel Extract Improves Dry Eye Symptoms in a Unilateral Exorbital Lacrimal Gland Excision Mouse. Nutrients 2016, 8, 750. https://doi.org/10.3390/nu8110750
Kim C-S, Jo K, Lee I-S, Kim J. Topical Application of Apricot Kernel Extract Improves Dry Eye Symptoms in a Unilateral Exorbital Lacrimal Gland Excision Mouse. Nutrients. 2016; 8(11):750. https://doi.org/10.3390/nu8110750
Chicago/Turabian StyleKim, Chan-Sik, Kyuhyung Jo, Ik-Soo Lee, and Junghyun Kim. 2016. "Topical Application of Apricot Kernel Extract Improves Dry Eye Symptoms in a Unilateral Exorbital Lacrimal Gland Excision Mouse" Nutrients 8, no. 11: 750. https://doi.org/10.3390/nu8110750
APA StyleKim, C.-S., Jo, K., Lee, I.-S., & Kim, J. (2016). Topical Application of Apricot Kernel Extract Improves Dry Eye Symptoms in a Unilateral Exorbital Lacrimal Gland Excision Mouse. Nutrients, 8(11), 750. https://doi.org/10.3390/nu8110750






