The National Food Consumption Survey IV SCAI: Nutrient Intakes and Related Dietary Sources in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Data Entry, Food, and Nutrient Databases
2.3. Data Analysis
3. Results
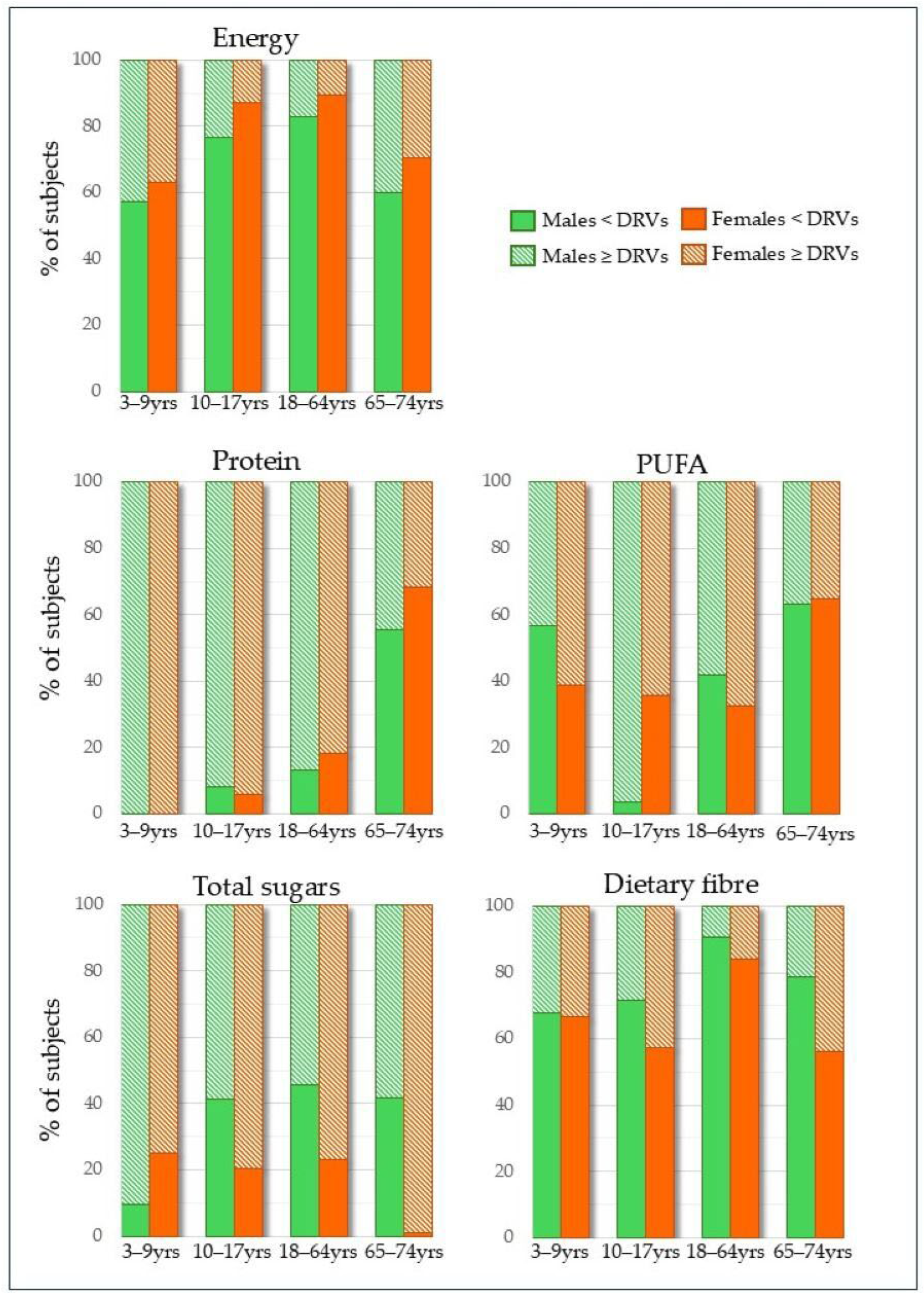
3.1. Nutrient Intake and Adequacy
3.2. Major Dietary Sources of Nutrients
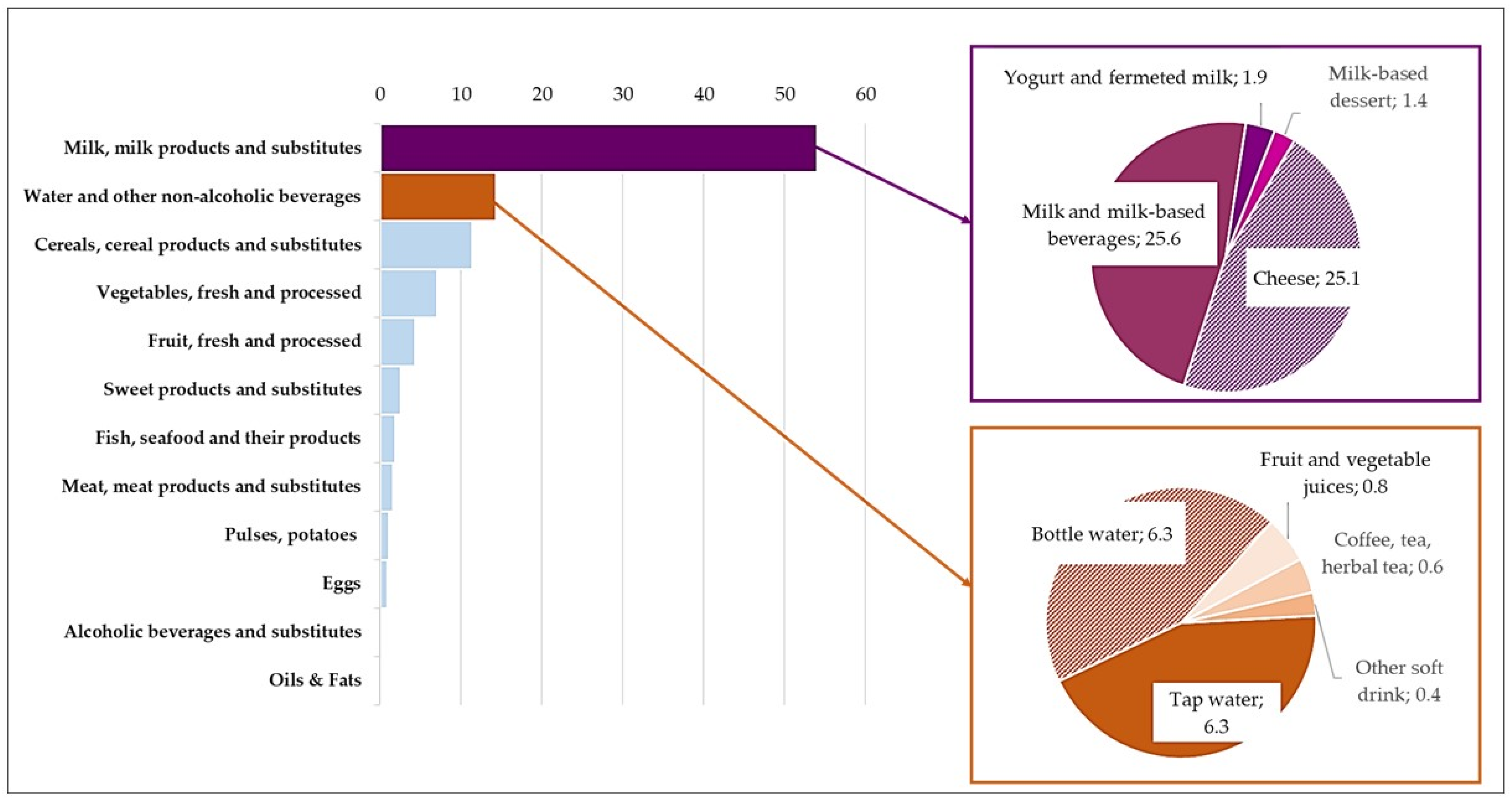
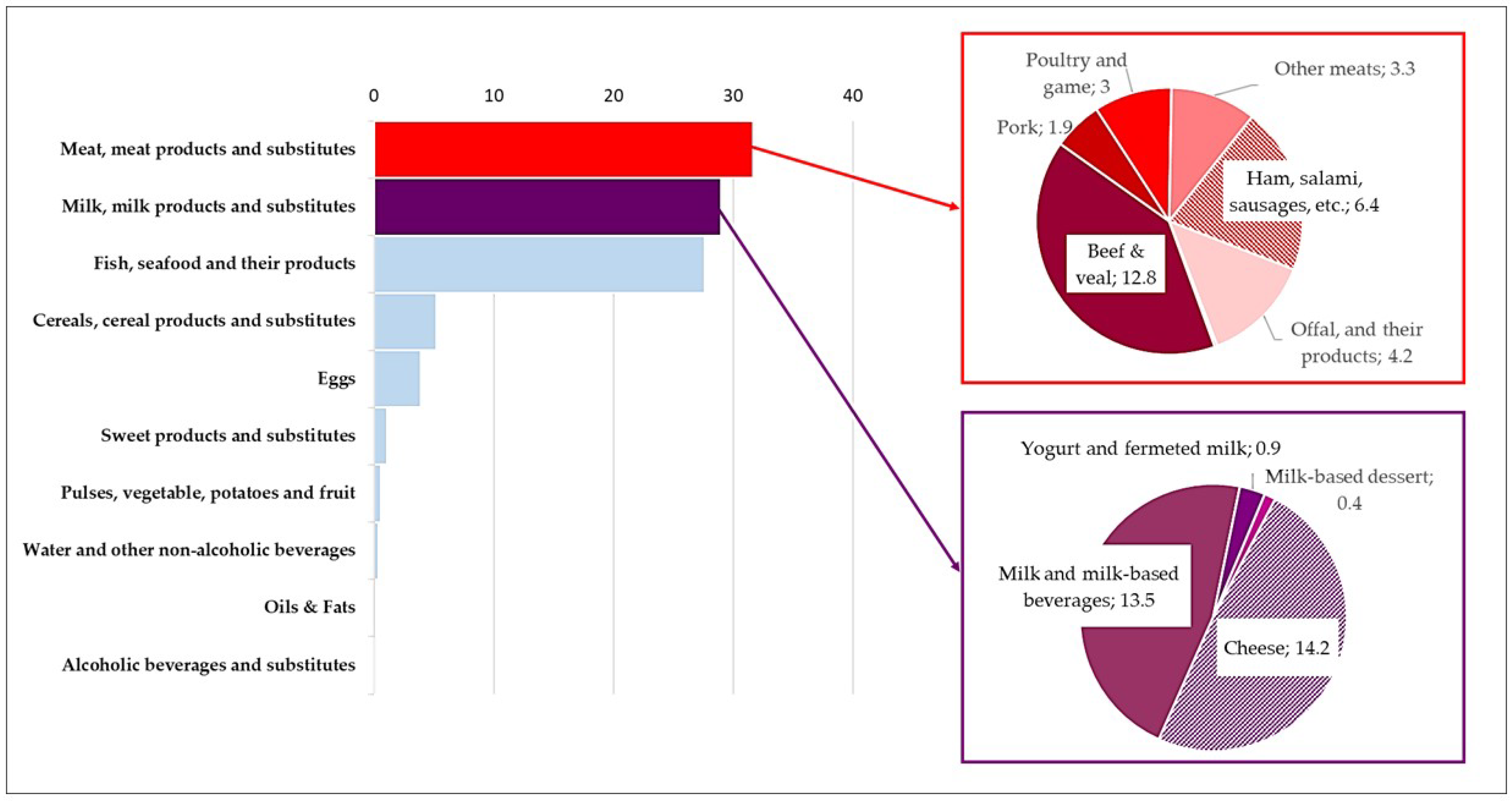
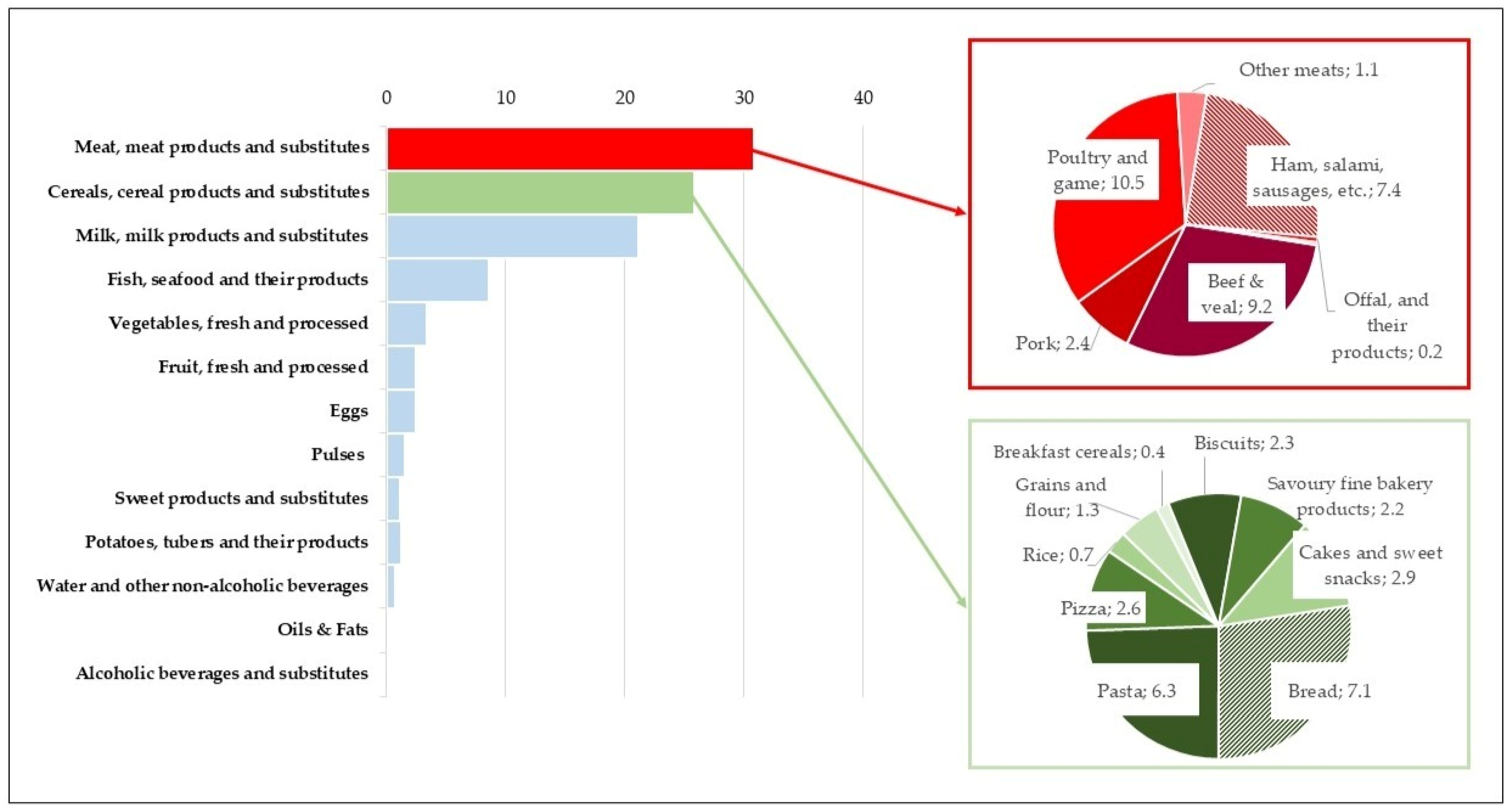
3.2.1. Energy, Macronutrients, and Dietary Fibre
3.2.2. Minerals and Vitamins
4. Discussion
4.1. Energy and Nutrient Assessment
4.2. Food Source Assessment
4.3. Implications of the Study: Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Adequate Intake |
| AR | Average Requirement |
| BMI | Body Mass Index |
| BMR | Basal Metabolic Rate |
| Ca | Calcium |
| CHO | Carbohydrates |
| CREA | Consiglio Per La Ricerca In Agricoltura E L’analisi Dell’economia Agraria |
| DFE | Dietary Folate Equivalents |
| DRVs | Dietary Reference Values |
| EFSA | European Food Safety Authority |
| En | Energy Intake |
| Fe | Iron |
| INRAN-SCAI | Third Italian National Food Consumption Survey |
| IV SCAI | Fourth Italian National Food Consumption Survey |
| K | Potassium |
| Mg | Magnesium |
| MJ | Megajoule |
| MSM | Multiple Source Method |
| MUFA | Monounsaturated Fatty Acids |
| NCDs | Non-Communicable Diseases |
| P | Phosphorus |
| PAL | Physical Activity Level |
| PRI | Population Reference Intake |
| PUFA | Polyunsaturated Fatty Acids |
| RI | Reference Intake Range for macronutrients |
| SDT | Suggested Dietary Target |
| SFA | Saturated Fatty Acids |
| WHO | World Health Organization |
| Zn | Zinc |
Appendix A
| Nicole Acquaviva | Maria Albini |
| Rosaria Amabile | Enrico Apreda |
| Alice Baganha Sabatino | Cristina Baggio |
| Eliane Denise Bahbouth | Rossella Ballotta |
| Francesca Barberi | Sandra Bassini |
| Lauretta Bianco | Lucia Bonadies |
| Francesca Borghi | Giuseppa Bruno |
| Filomena Capasso | Sabrina Capineri |
| Rosa Carbone | Roberta Carli |
| Liliana Cassano | Vincenza Castiglia |
| Maurizio Cavallaro | Ketty Ceccarelli |
| Sara Ciacci | Rosalba Cipresso |
| Lisa Colladet | Stefania Corradi |
| Anna Maria Covarino | Alessandra Covino |
| Maria Cristina Cucugliato | Marta D’Ambrosio |
| Sara Dattoli | Maria De Marinis |
| Ignazio Dei | Federica Del Genio |
| Giulia Dellacostanza | Maria Assunta Di Cesare |
| Flora Di Tommaso | Emanuela Alessandra Donghi |
| Roberta Falcone | Federica Falvo |
| Elena Felloni | Anna Ferrante |
| Antonella Ferrigno | Antonella Foglia |
| Paola Golzio | Silvana Grasso |
| Daniele Grumiro | Emilia Guberti |
| Marina Infante | Gianna Lia Innocenti |
| Domenica Iofrida | Marina La Rocca |
| Valeria Laganà | Patrizia Lamberti |
| Elisa Lazzarino | Carmela Legorano |
| Silvia Lisciani | Teresa Loiacono |
| Rosanna Macaluso | Manuela Maione |
| Monica Maj | Lara Marangoni |
| Cecilia Mari | Valeria Marmo |
| Domenico Marotta | Piero Maruccia |
| Nicola Marulla | Marika Massaro |
| Guido Antonello Mattera Ricigliano | Maria Rita Milone |
| Antonio Molinaro | Erika Mollo |
| Mariantonia Monni | Laura Morisi |
| Patrizia Orsini | Giuseppa Pacella |
| Michele Parmato | Laura Parravicini |
| Angela Pasinato | Brunella Pasquini |
| Franca Pasticci | Emma Petrella |
| Alessandro Pinto | Clorinda Pittalà |
| Angelica Pizzolante | Carolina Poli |
| Luigi Polverino | Lucia Pomaro |
| Paola Pozzo | Antonio Pratesi |
| Angela Pugliese | Sofia Pugnaloni |
| Marina Putzolu | Sara Quattrini |
| Lisa Randisi | Valeria Rebonato |
| Vittoria Rocchino | Paola Rossi |
| Gaia Rovai | Monica Ruotolo |
| Daniela Russo | Carmen Santangelo |
| Sara Santilli | Agata Rita Santonocito |
| Sabrina Scelfo | Egeria Scoditti |
| Angela Silvestri | Gabriella Siniscalchi |
| Giuseppa Smeralda | Vincenzo Sofia |
| Silvia Soligon | Erminia Solomita |
| Ottavia Sorace | Angela Spadafranca |
| Susanna Tardonato | Paola Tei |
| Paride Travaglini | Francesca Trinchella |
| Maria Trippa | Silvia Tulone |
| Salvatore Vaccaro | Anna Valente |
| Viviana Vecchio | Lorella Vicari |
| Sara Vignozzi | Laura Zangari |
Appendix B
| Food Groups | Single Food Items and Composite Food Items Merged into | Minor Ingredients from Other Food Groups Present in Composite Foods | Subgroups Merged into |
|---|---|---|---|
| Cereals, cereal products and substitutes | |||
| Bread | All types of bread prepared with any type of flour (wheat, whole wheat, soya, maize, etc.), speciality breads, sponge bread, excl. breadcrumbs and toasted bread | Milk and fats in speciality breads; soya in soya bread | |
| Pasta & pasta substitutes | All types of pasta, incl. rice noodles, fresh pasta with eggs, tortellini and ravioli (fresh pasta with meat filling), puff pastry dough; Pasta for infants, also fortified | Meat, vegetables, cheese in fresh pasta filling; eggs in fresh pasta; butter in puff pastry dough | Including Infant food–pasta |
| Pizza | Plain white pizza, plain tomato pizza, and pizza doughs | Tomato in plain tomato pizza; oil in plain white and tomato pizza | |
| Rice | All types of rice, white and brown, excl. rice in commercial rice pudding | ||
| Grains and flour | Wheat flour and whole wheat flour used in recipes, wheat germ, couscous, breadcrumbs; All types of flour (corn, oat, millet, barley, rice, etc.) used in recipes; Instant cereal-based preparations, cereal-based baby foods, also fortified | Fruit in some cereal-based baby foods | Including Wheat flours; Other cereals & flours, Infant food–other cereals |
| Breakfast cereals | All types of ready-to-eat cereals (generally used at breakfast with milk): corn flakes, puffed wheat, dried and toasted rice, muesli, etc. | Dried fruit and nuts in muesli; sugar; cocoa | |
| Biscuits | All types of sweet biscuits, incl. sugar-free biscuits, gluten-free biscuits; Biscuits for infants, granulated biscuits, also fortified | Sugar; eggs; fats; cocoa; dried fruit and nuts; | Including Infant food–biscuits |
| Savoury fine bakery products | All types of crackers, breadsticks, rusk, popcorn, salty appetizers and savoury biscuits | Fats, tomatoes, cheese, seeds, etc. | |
| Cakes and sweet snacks | Plain cakes without chocolate and chocolate coatings, without cream and custard and jam, etc., sweet cereal- based snacks (e.g., bars); Sweet rolls, all types of cakes with chocolate and chocolate coatings, with fruit, with cream, etc | Fats; eggs; fruit; milk; cocoa; cream | Including Cakes and sweet snacks without and with creams |
| Pulses | |||
| Pulses, fresh and processed, dried | All types of pulses fresh and processed: lentils, peas, chickpeas, soyabeans, all types of beans excl. green beans; All types of pulses dried and processed: lentils, peas, chickpeas, soyabeans, all types of beans excl. green beans; Legume-based baby foods, powdered preparations based on legumes | Including Pulses, dried; Infant food–pulses | |
| Vegetables, fresh and processed | |||
| Leafy vegetables, fresh | Chicory, lettuce, spinach, etc. | ||
| Tomatoes, fresh | Fresh tomatoes used in salad and other recipes (e.g., tomato sauce) | ||
| Other fruiting vegetables, fresh | Aubergine, pepper, cucumber, pumpkin, courgette, etc. | ||
| Roots and onions, fresh | Onion, garlic, turnip-rooted celery, beetroot, daikon | ||
| Other vegetables, fresh | All other types of fresh vegetables: broccoli, cabbage, cauliflower, artichokes, asparagus, fennel, mushroom, green beans and palm heart | ||
| Vegetables, processed | Tomato sauce canned, bottled etc., tomato paste; Vegetable preserves in vinegar, oil or brine; Vegetable soup dehydrated, dried seaweed; Industrial mixed salad with mayonnaise, mixed vegetable preparations for rice salad, vegetable broth; Vegetables-based baby foods | Oil (in oil preserves); vinegar (in oil and vinegar preserves); Cereals and potatoes (in dehydrated soup); Eggs (in mayonnaise) | Including Tomatoes, canned; Other vegetables, canned; Vegetables, dried; Other vegetables, packaged products; Infant food–vegetables |
| Spices and herbs | Parsley, basil, rosemary, oregano, curry, ginseng, etc. | ||
| Potatoes, tubers and their products | |||
| Potatoes and potato products, excl. potato chips | Potatoes raw, sweet potatoes, potato croquettes, potato flakes dehydrated; Tapioca, yam root | Cheese in some speciality potato; breading in potato croquettes | Including Other tubers |
| Potato chips and french fries | All potato chips, frozen french fries | Fats in all potato chips; cheese in some speciality potato chips | |
| Fruit, fresh and processed | |||
| Citrus fruit, fresh | Orange, lemon, grapefruit, tangerine, etc. | ||
| Berry fruit, fresch | Strawberries, raspberries, blueberries, blackberries, goji berries, etc | ||
| Exotic fruit, fresh | Banana, cherimoya, avocado, papaya, mango, lychee, etc | ||
| Other fruit, fresh | All other types of fruit: apple, pear, peach, apricot, grape, fig, melon, watermelon, pomegranate, plum, cherry, etc.; Fruit-based baby foods | Including Infant food–fruit | |
| Nuts, dried fruit, seeds, olives and their products | Nuts roasted, dried, in powder or in purée (almond, chestnut, walnut, coconut, pine nut, peanut, pistachio), seeds (pumpkin seed) and all dried fruit (figs, plum, raisin), olives | ||
| Processed fruit (in syrup, in purée, etc.) | All types of fruit in syrup (peach, apricot, pear, fruit cocktail. etc.), fruit purée, minced fruit | Sugar | |
| Meat, meat products and substitutes | |||
| Beef & veal, not preserved, excl. offal | Beef, veal, industrial meat sauce | Tomato in industrial meat sauce | |
| Pork, not preserved, excl. offal | Pork meat, roasted pork meat (porchetta), foot pork raw, excl. offal | ||
| Poultry and game, not preserved, excl. offal | Pheasant, chicken, roast chicken, goose, quail, turkey, ostrich | ||
| Other meats, not preserved, excl. offal | Lamb, goat, mutton, kid, horse, donkey, lean deer, boar, rabbit, frog, land snail, excl. offal | ||
| Ham, salami, sausages, excl. offal | Preserved meat from pork, chicken and turkey meat (ham, mortadella, sausages, wurstel, salami, etc.), dried beef or horse meat (bresaola); Corned beef, mixed wurstel stuffed with cheese or other ingredients; Meat-based baby foods | Cheese; Fats, cereals and tubers in meat-based baby foods | Including Other meats, preserved, excl. offal; Infant food_meat |
| Offal, and their products | Liver, kidney, brain, trotter, heart, tripe, tongue, sweetbreads, blood and liver pate’ | Fats in liver pate’ | |
| Meat substitutes | Seitan (wheat gluten), soya hamburger | Soya; wheat | |
| Fish, seafood and their products | |||
| Fish and seafood, fresh and frozen | All types of fish raw (fresh or frozen) and fish fingers; All types of molluscs (clams, oysters, mussels, octopus, squid, cuttlefish, etc.) crustaceans (shrimps, prawns, crabs, lobsters, crayfish, etc.), raw (fresh or frozen) | Breading on fish fingers | Including Seafood, fresh and frozen |
| Fish and seafood, preserved | All types of preserved fish, molluscs, crustaceans and fish eggs (caviar, anchovies brined or in oil, tuna brined or in oil, smoked salmon, canned crab meat, cod dried and salted, smoked herring, etc.); Fish-based baby foods | Oil in oil preserves; lemon; Fats, cereals, vegetables and tubers in fish-based baby foods | Including Infant food–fish |
| Milk, milk products and substitutes | |||
| Milk and milk-based beverages and substitutes | All types of milk (liquid, condensed and powder form), flavoured milk (e.g., packaged chocolate-flavoured milk); Milk substitutes (e.g., soya, rice, oat); Breast milk; Ready-to-feed liquid formula (growing up milk, follow- on milk) for infants; Powdered milk formulas (growing-up milk and follow- on milk) for infants | Sugar in flavoured milk beverages; cocoa in flavoured milk beverages | Including Milk substitutes plant-based; Human milk; Infant formula, liquid; Infant formula, powder |
| Yoghurt and fermented milk | All types of yoghurt, drinkable yoghurt, milk with ferments (e.g., kefir); Yoghurt-based dessert with fruit for infants | Sugar in yoghurt; fruit, cereals, chocolate or nuts in yoghurt; fruit | Including Infant food–yoghurt |
| Cheese and substitutes | All types of cheese (e.g., mozzarella, parmesan, edam, feta, fontina), cheese substitutes (e.g., tofu); Flavoured sweet cheese for children, cheese-based baby foods | Fruit or vegetables and sugar in flavoured cheese for children | Including Infant food–cheese |
| Milk-based desserts and substitutes | Commercial milk-based desserts (e.g., mousse chocolate, custard, Chantilly custard), incl. commercial creamy rice pudding (risolatte) | Sugar; milk cream; cocoa; rice in rice pudding | |
| Oils and fats | |||
| Olive oil | Extra-virgin olive oil, olive oil, incl. enriched type | ||
| Other vegetable oils | All type of vegetable oils, excl. olive oil | ||
| Butter & creams | Butter, cream, heavy cream | ||
| Other fats | Lard, tallow; All types of margarine, incl. soyabean butter; Mayonnaise, included light type | Eggs in mayonnaise | Including Margarine; Mayonnaise and fat-based sauces |
| Eggs | All types of eggs (chicken, duck, ostrich, etc.) excl. fish eggs | ||
| Sweet products and substitutes | |||
| Ice cream, ice lolly and substitutes | All types of ice creams (with all possible flavours and ingredients), ice lolly | Milk in ice cream; soya in soya ice cream; fruit; eggs | |
| Chocolate and substitutes | All types of chocolate (milk, white, cocoa 70–90%, with hazelnuts, etc.), spreadable chocolate cream with or without hazelnuts, chocolate bars filled with mou | Milk in milk chocolate; nuts in some chocolate creams or bars; rice in some chocolate bars | |
| Candies, jam and othersweet products (incl. sugar-free) | All types of candies (e.g., mou, fudge, fondant, different flavours), chewing gum, jam, marmalade, nougat with almonds, glazed chestnuts (marrons glacés), peanut brittle, sesame brittle, incl. sugar-free products | Nuts; seeds | |
| Sugar, fructose, honey | Honey, sugar, fructose, maple syrup, royal jelly | ||
| Cocoa and cocoa-based powder | Cocoa powder, mixed powder of cocoa with other ingredients, with or without sugar, with or without dehydrated milk | Sugar; milk | |
| Artificial sweeteners | All types of table-top products containing artificial sweeteners (e.g., aspartame, saccharin) in tablets, powder or liquid | ||
| Water and other non- alcoholic beverages | |||
| Tap water | Tap water (as such, in beverages or recipes) | ||
| Bottled water | All types of commercial bottled water | ||
| Coffee, tea, and substitutes (incl. decaffeinated) | All types of coffee (e.g., brewed, decaffeinated, espresso’), all types of tea (brewed, deteinated) with or without sugar, pearled barley coffee; Herbal tea in cup and ready to drink (e.g., chamomille) | Including Herbal tea | |
| Fruit and vegetable juices without artificial sweeteners | All types of fruit and vegetable juices (e.g., nectar, carrot juice, orange juice), with or without the addition of water, sugar, incl. fortified products; All types of fruit juices, ready to drink and powdered herbal teas for infant | Including Infant food_fruit juices and beverages (incl. powders) | |
| Non-alcoholic beverages | All types of carbonate beverages (e.g., cola, soda, ginger ale, orange, tonic water), energy drinks, sport drinks, syrups to be diluted, with sugar; All types of carbonate beverages (e.g., cola, soda, gingerale, orange, tonic water) sugar-free and with artificial sweeteners; All types of powdered and granulated drink preparations | Sugar in powders for the preparation of instant beverages | Including Non–alcoholic beverages without artificial sweeteners; Non–alcoholic beverages with artificial sweeteners; Non–alcoholic beverages, powder |
| Alcoholic beverages and substitutes | |||
| Regular wine and substitutes | All types of wine (red, white), non-alcoholic’ wine, excl. sparkling wine | ||
| Beer, cider and substitutes | Beer all types, non-alcoholic beer | ||
| Sweet wine, spumante, aperitif | Sparkling wine, aperitif (campari, aperol, bagardi, etc.) | ||
| Spirits & liquors | Fortified wine (e.g., porto, cherry, vermouth, dessert wine sweet or dry, appetizer), spirits (e.g., grappa, brandy, whiskey, rum), liquors (amaro, limoncello, etc.) | ||
| Meal substitutes | Meal replacements in liquid form and bar form | ||
| Miscellaneous | |||
| Non-fat-based sauces and condiments | Vinegar, ketchup, mustard sauce, soya sauce, etc.; Bouillon cubes, sodium bicarbonate (for food use), isinglass, baking powder, meat extract; Liquid cake flavourings | Tomato and sugar in ketchup, milk, cereal, vegetables; Meat in meat bouillon cubes | Including Broth cubes and other products; Flavors |
| Liquid foods | All water and beverages, milk in liquid state, drinkable yoghurt | ||
| Solid foods | All other food items incl. oil, dehydrated items (milk), powder for reconstitution of beverages, creamy desserts (yoghurt), sauces, etc. |
References
- Food and Agriculture Organization. Food and Diet Statistics on Dietary Data; FAOSTAT Analytical Briefs; Food and Agriculture Organization: Rome, Italy, 2024; Volume 82. [Google Scholar] [CrossRef]
- National Diet and Nutrition Survey. NDNS. National Diet and Nutrition Survey 2019 to 2023: Report. Available online: https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-2019-to-2023/national-diet-and-nutrition-survey-2019-to-2023-report (accessed on 20 November 2025).
- Tang, K.; Adams, K.P.; Ferguson, E.L.; Woldt, M.; Yourkavitch, J.; Pedersen, S.; Broadley, M.R.; Dary, O.; Louise Ander, E.; Joy, E.J.M. Systematic Review of Metrics Used to Characterise Dietary Nutrient Supply from Household Consumption and Expenditure Surveys. Public Health Nutr. 2022, 25, 1153–1165. [Google Scholar] [CrossRef]
- Rippin, H.L.; Hutchinson, J.; Evans, C.E.L.; Jewell, J.; Breda, J.J.; Cade, J.E. National Nutrition Surveys in Europe: A Review on the Current Status in the 53 Countries of the WHO European Region. Food Nutr. Res. 2018, 62, 10-29219. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for Europe. European Food and Nutrition Action Plan 2015–2020; DK-2100 Copenhagen; World Health Organization: Geneva, Switzerland, 2015. Available online: https://www.who.int/europe/publications/i/item/9789289051231 (accessed on 31 October 2025).
- Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee Advisory, Report to the Secretary of Agriculture and Secretary of Health and Human Services; U.S. Department of Agriculture, Agricultural Research Service: Washington, DC, USA, 2020.
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health Effects of Dietary Risks in 195 Countries, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO. Healthy Diet; World Health Organization: Geneva, Switzerland, 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 20 November 2025).
- Montenegro, C.R.; Gomez, G.; Hincapie, O.; Dvoretskiy, S.; DeWitt, T.; Gracia, D.; Misas, J.D. The Pediatric Global Burden of Stunting: Focus on Latin America. Lifestyle Med. 2022, 3, e67. [Google Scholar] [CrossRef]
- Espinosa-Salas, S.; Gonzalez-Arias, M. Nutrition: Macronutrient Intake, Imbalances, and Interventions. Available online: https://www.ncbi.nlm.nih.gov/books/NBK594226/ (accessed on 6 November 2025).
- United States Department of Agriculture. USDA. Scientific Report of the 2025 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and Secretary of Agriculture; United States Department of Agriculture: Washington, DC, USA, 2024. [CrossRef]
- Beal, T.; Ortenzi, F. Priority Micronutrient Density in Foods. Front. Nutr. 2022, 9, 806566. [Google Scholar] [CrossRef]
- Sette, S.; Le Donne, C.; Piccinelli, R.; Arcella, D.; Turrini, A.; Leclercq, C. The Third Italian National Food Consumption Survey, INRAN-SCAI 2005-06—Part 1: Nutrient Intakes in Italy. Nutr. Metab. Cardiovasc Dis. 2011, 21, 922–932. [Google Scholar] [CrossRef]
- Rossi, L.; Berni Canani, S.; Censi, L.; Gennaro, L.; Leclercq, C.; Scognamiglio, U.; Sette, S.; Ghiselli, A. The 2018 Revision of Italian Dietary Guidelines: Development Process, Novelties, Main Recommendations, and Policy Implications. Front. Nutr. 2022, 9, 861526. [Google Scholar] [CrossRef] [PubMed]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2025—Addressing High Food Price Inflation for Food Security and Nutrition; WHO: Geneva, Switzerland, 2025. [CrossRef]
- Benvenuti, L.; Sette, S.; De Santis, A.; Riso, P.; Petroni, K.; Crosatti, C.; Losa, A.; Martone, D.; Martini, D.; Cattivelli, L.; et al. Simulation of Daily Iron Intake by Actual Diet Considering Future Trends in Wheat and Rice Biofortification, Environmental, and Dietary Factors: An Italian Case Study. Nutrients 2024, 16, 4097. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Fanzo, J.; Covic, N.; Dobermann, A.; Henson, S.; Herrero, M.; Pingali, P.; Staal, S. A Research Vision for Food Systems in the 2020s: Defying the Status Quo. Glob. Food Secur. 2020, 26, 100397. [Google Scholar] [CrossRef]
- Tilman, D.; Clark, M. Global Diets Link Environmental Sustainability and Human Health. Nature 2014, 515, 518–522. [Google Scholar] [CrossRef]
- Clark, M.A.; Springmann, M.; Hill, J.; Tilman, D. Multiple Health and Environmental Impacts of Foods. Proc. Natl. Acad. Sci. USA 2019, 116, 23357–23362. [Google Scholar] [CrossRef]
- García-Leal, J.; Espinoza Pérez, A.T.; Vásquez, Ó.C. Sustainable Diets Optimal Design for the Massive Food Services: Economic versus Environmental Aspects. Int. J. Life Cycle Assess 2023, 28, 1481–1494. [Google Scholar] [CrossRef]
- Tucci, M.; Martini, D.; Marino, M.; Del Bo’, C.; Vinelli, V.; Biscotti, P.; Parisi, C.; De Amicis, R.; Battezzati, A.; Bertoli, S.; et al. The Environmental Impact of an Italian-Mediterranean Dietary Pattern Based on the EAT-Lancet Reference Diet (EAT-IT). Foods 2022, 11, 3352. [Google Scholar] [CrossRef]
- Arrieta, E.M.; Aguiar, S. Healthy Diets for Sustainable Food Systems: A Narrative Review. Environ. Sci. Adv. 2023, 2, 684–694. [Google Scholar] [CrossRef]
- SINU. Società Italiana di Nutrizione Umana. LARN—Livelli Di Assunzione Di Riferimento Di Nutrienti Ed Energia per La Popolazione Italiana; V Revisione; BioMedia srl: Milano, Italy, 2024. [Google Scholar]
- Turrini, A.; Sette, S.; Le Donne, C.; Piccinelli, R.; D’Addezio, L.; Mistura, L.; Ferrari, M.; Catasta, G.; Martone, D. Italian National Dietary Survey on Children Population from Three Months up to Nine Years Old—IV SCAI CHILD. EFSA Support. Publ. 2021, 18, 7087E. [Google Scholar] [CrossRef]
- Turrini, A.; Le Donne, C.; Piccinelli, R.; D’Addezio, L.; Mistura, L.; Sette, S.; Martone, D.; Comendador Azcarraga, F.J.; Ferrari, M.; Catasta, G. Italian National Dietary Survey on Adult Population from 10 up to 74 Years Old—IV SCAI ADULT. EFSA Support. Publ. 2022, 19, 7559E. [Google Scholar] [CrossRef]
- Le Donne, C.; Piccinelli, R.; Sette, S.; Martone, D.; Catasta, G.; Censi, L.; Comendador Azcarraga, F.J.; D’Addezio, L.; Ferrari, M.; Mistura, L.; et al. Dietary Assessment Training: The Italian IV SCAI Study on 10–74 Year-Old Individuals’ Food Consumption. Front. Nutr. 2022, 9, 954939. [Google Scholar] [CrossRef] [PubMed]
- Mistura, L.; Donne, C.L.; D’Addezio, L.; Ferrari, M.; Comendador, F.J.; Piccinelli, R.; Martone, D.; Sette, S.; Catasta, G.; Turrini, A. The Italian IV SCAI Dietary Survey: Main Results on Food Consumption. Nutr. Metab. Cardiovasc. Dis. 2025, 37, 103863. [Google Scholar] [CrossRef]
- Turrini, A.; Catasta, G.; Censi, L.; Comendador Azcarraga, F.J.; D’Addezio, L.; Ferrari, M.; Le Donne, C.; Martone, D.; Mistura, L.; Pettinelli, A.; et al. A Dietary Assessment Training Course Path: The Italian IV SCAI Study on Children Food Consumption. Front. Public Health 2021, 9, 590315. [Google Scholar] [CrossRef]
- European Food Safety Authority. EFSA. Guidance on the EU Menu Methodology. EFSA J. 2014, 12, 3944. [Google Scholar] [CrossRef]
- Trolle, E.; Vandevijvere, S.; Ruprich, J.; Ege, M.; Dofková, M.; De Boer, E.; Ocké, M. Validation of a Food Quantification Picture Book Targeting Children of 0-10 Years of Age for Pan-European and National Dietary Surveys. Br. J. Nutr. 2013, 110, 2298–2308. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, F.; Vineis, P.; Cravanzola, D.; Pisani, P.; Xompero, G.; Riboli, E.; Kaaks, R. Validation of a Method for the Estimation of Food Portion Size. Epidemiology 1992, 3, 379–382. [Google Scholar] [CrossRef]
- Pisani, P.; Faggiano, F.; Krogh, V.; Palli, D.; Vineis, P.; Berrino, F. Relative Validity and Reproducibility of a Food Frequency Dietary Questionnaire for Use in the Italian EPIC Centres. Int. J. Epidemiol. 1997, 26, 152S–160S. [Google Scholar] [CrossRef]
- Slimani, N.; Ferrari, P.; Ocke, M.; Welch, A.; Boeing, H.; Van Liere, M.; Pala, V.; Amiano, P.; Lagiou, A.; Mattisson, I.; et al. Standardization of the 24-Hour Diet Recall Calibration Method Used in the European Prospective Investigation into Cancer and Nutrition (EPIC): General Concepts and Preliminary Results. Eur. J. Clin. Nutr. 2000, 54, 900–917. [Google Scholar] [CrossRef]
- Pala, V.; Sieri, S.; Palli, D.; Salvini, S.; Berrino, F.; Bellegotti, M.; Frasca, G.; Tumino, R.; Sacerdote, C.; Fiorini, L.; et al. Diet in the Italian EPIC Cohorts: Presentation of Data and Methodological Issues. Tumori 2003, 89, 594–607. [Google Scholar] [CrossRef]
- Istituto Scotti Bassani. Atlante Pediatrico Delle Porzioni Degli Alimenti (Pediatric Atlas of Food Portions). Available online: https://www.scottibassani.it/atlante-pediatrico/ (accessed on 31 October 2025).
- WHO. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; WHO: Geneva, Switzerland, 1995; World Health Organization Technical Report Series; Volume 854.
- Leclercq, C.; Berardi, D.; Sorbillo, M.R.; Lambe, J. Intake of Saccharin, Aspartame, Acesulfame K and Cyclamate in Italian Teenagers: Present Levels and Projections. Food Addit. Contam. 1999, 16, 99–109. [Google Scholar] [CrossRef]
- Leclercq, C.; Arcella, D.; Armentia, A.; Boon, P.E.; Kruizinga, A.G.; Gilsenan, M.B.; Thompson, R.L. Development of Databases for Use in Validation Studies of Probabilistic Models of Dietary Exposure to Food Chemicals and Nutrients. Food Addit. Contam. 2003, 20, S27–S35. [Google Scholar] [CrossRef] [PubMed]
- Leclercq, C.; Arcella, D.; Piccinelli, R.; Sette, S.; Le Donne, C. The Italian National Food Consumption Survey INRAN-SCAI 2005-06: Main Results: In Terms of Food Consumption. Public Health Nutr. 2009, 12, 2504–2532. [Google Scholar] [CrossRef]
- Pounis, G.; Bonanni, A.; Ruggiero, E.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; Bonaccio, M.; Cerletti, C.; Riccardi, G.; Donati, M.; et al. Food Group Consumption in an Italian Population Using the Updated Food Classification System FoodEx2: Results from the Italian Nutrition & HEalth Survey (INHES) Study. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 307–328. [Google Scholar] [CrossRef]
- Magliulo, L.; Bondi, D.; Pietrangelo, T.; Fulle, S.; Piccinelli, R.; Jandova, T.; Di Blasio, G.; Taraborrelli, M.; Verratti, V. Serum Ferritin and Vitamin D Evaluation in Response to High Altitude Comparing Italians Trekkers vs Nepalese Porters. Eur. J. Sport. Sci. 2021, 21, 1792559. [Google Scholar] [CrossRef] [PubMed]
- Mistura, L.; Azcarraga, F.J.C.; D’Addezio, L.; Le Donne, C.; Martone, D.; Piccinelli, R.; Sette, S. Comparing Self-Administered Web-Based to Interviewer-Led 24-h Dietary Recall (FOODCONS): An Italian Pilot Case Study. Dietetics 2025, 4, 17. [Google Scholar] [CrossRef]
- European Food Safety Authority. The Food Classification and Description System FoodEx 2 (Revision 2). EFSA Support. Publ. 2015, 12, 804E. [Google Scholar] [CrossRef]
- Salfinger, A.; Gibin, D.; Niforou, K.; Ioannidou, S. FoodEx2 Maintenance 2022. EFSA Support. Publ. 2023, 20, 7900E. [Google Scholar] [CrossRef]
- D’Addezio, L.; Sette, S.; Piccinelli, R.; Le Donne, C.; Turrini, A. FoodEx2 Harmonization of the Food Consumption Database from the Italian IV SCAI Children’s Survey. Nutrients 2024, 16, 1065. [Google Scholar] [CrossRef]
- European Food Safety Authority. EFSA. The EFSA Comprehensive European Food Consumption Database. 15 2022. Available online: https://www.efsa.europa.eu/en/data-report/food-consumption-data (accessed on 31 October 2025).
- Harttig, U.; Haubrock, J.; Knüppel, S.; Boeing, H. The MSM Program: Web-Based Statistics Package for Estimating Usual Dietary Intake Using the Multiple Source Method. Eur. J. Clin. Nutr. 2011, 65, S87–S91. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Growth Reference Data for 5–19 Years. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years (accessed on 3 November 2025).
- World Health Organization. Body Mass Index-for-Age (BMI-for-Age). Available online: https://www.who.int/toolkits/child-growth-standards/standards/body-mass-index-for-age-bmi-for-age (accessed on 19 November 2025).
- Turck, D.; Michaelsen, K.F.; Shamir, R.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Kolacek, S.; et al. World Health Organization 2006 Child Growth Standards and 2007 Growth Reference Charts: A Discussion Paper by the Committee on Nutrition of the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 258–264. [Google Scholar] [CrossRef]
- World Health Organization. Growth Reference Data for 5–19 Years. WHO AnthroPlus Software. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/application-tools (accessed on 3 November 2025).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000; WHO technical report series; Volume 894. Available online: https://iris.who.int/handle/10665/42330 (accessed on 3 November 2025).
- Hörnell, A.; Lagström, H.; Lande, B.; Thorsdottir, I. Protein Intake from 0 to 18 Years of Age and Its Relation to Health: A Systematic Literature Review for the 5th Nordic Nutrition Recommendations. Food Nutr. Res. 2013, 57, 21083. [Google Scholar] [CrossRef]
- Stokes, A.; Campbell, K.J.; Yu, H.J.; Szymlek-Gay, E.A.; Abbott, G.; He, Q.Q.; Zheng, M. Protein Intake from Birth to 2 Years and Obesity Outcomes in Later Childhood and Adolescence: A Systematic Review of Prospective Cohort Studies. Adv. Nutr. 2021, 12, 1863–1876. [Google Scholar] [CrossRef]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D Deficiency 2.0: An Update on the Current Status Worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef]
- Pludowski, P.; Holick, M.F.; Pilz, S.; Wagner, C.L.; Hollis, B.W.; Grant, W.B.; Shoenfeld, Y.; Lerchbaum, E.; Llewellyn, D.J.; Kienreich, K.; et al. Vitamin D Effects on Musculoskeletal Health, Immunity, Autoimmunity, Cardiovascular Disease, Cancer, Fertility, Pregnancy, Dementia and Mortality-A Review of Recent Evidence. Autoimmun. Rev. 2013, 12, 976–989. [Google Scholar] [CrossRef]
- Burns, J.L.; Miller, C.H.; Fontaine-Bisson, B.; Connor, K.L. Iron Deficiency and Iron Deficiency Anaemia in Women of Reproductive Age: Sex- and Gender-Based Risk Factors and Inequities. J. Trace Elem. Med. Biol. 2025, 90. [Google Scholar] [CrossRef]
- Sette, S.; Le Donne, C.; Piccinelli, R.; Mistura, L.; Ferrari, M.; Leclercq, C.; Arcella, D.; Bevilacqua, N.; Buonocore, P.; Capriotti, M.; et al. The Third National Food Consumption Survey, INRAN-SCAI 2005-06: Major Dietary Sources of Nutrients in Italy. Int. J. Food Sci. Nutr. 2013, 64, 1014–1021. [Google Scholar] [CrossRef] [PubMed]
- López-Valenciano, A.; Mayo, X.; Liguori, G.; Copeland, R.J.; Lamb, M.; Jimenez, A. Changes in Sedentary Behaviour in European Union Adults between 2002 and 2017. BMC Public Health 2020, 20, 1206. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development/World Health Oraganization. Step Up! Tackling the Burden of Insufficient Physical Activity in Europe; OECD Publishing: Paris, France, 2023. [Google Scholar] [CrossRef]
- Koliaki, C.; Dalamaga, M.; Liatis, S. Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten? Curr. Obes. Rep. 2023, 12, 514–527. [Google Scholar] [CrossRef] [PubMed]
- Valsta, L.M.; Tapanainen, H.; Kortetmäki, T.; Sares-Jäske, L.; Paalanen, L.; Kaartinen, N.E.; Haario, P.; Kaljonen, M. Disparities in Nutritional Adequacy of Diets between Different Socioeconomic Groups of Finnish Adults. Nutrients 2022, 14, 1347. [Google Scholar] [CrossRef]
- Kehoe, L.; Buffini, M.; McNulty, B.A.; Kearney, J.M.; Flynn, A.; Walton, J. Food and Nutrient Intakes and Compliance with Recommendations in School-Aged Children in Ireland: Findings from the National Children’s Food Survey II (2017–2018) and Changes since 2003–2004. Br. J. Nutr. 2023, 129, 2011–2024. [Google Scholar] [CrossRef] [PubMed]
- Milešević, J.; Zeković, M.; Šarac, I.; Knez, M.; Krga, I.; Takić, M.; Martačić, J.D.; Stevanović, V.; Vidović, N.; Ranković, S.; et al. Energy and Macronutrient Dietary Intakes of Serbian Adults 18–64 Years Old: EFSA EU Menu Food Consumption Survey in Serbia (2017–2022). Foods 2025, 14, 1228. [Google Scholar] [CrossRef]
- Gregorič, M.; Hristov, H.; Blaznik, U.; Koroušić Seljak, B.; Delfar, N.; Pravst, I. Dietary Intakes of Slovenian Adults and Elderly: Design and Results of the National Dietary Study SI.Menu 2017/18. Nutrients 2022, 14, 3618. [Google Scholar] [CrossRef]
- López-Sobaler, A.M.; Aparicio, A.; Rubio, J.; Marcos, V.; Sanchidrián, R.; Santos, S.; Pérez-Farinós, N.; Dal-Re, M.Á.; Villar-Villalba, C.; Yusta-Boyo, M.J.; et al. Adequacy of Usual Macronutrient Intake and Macronutrient Distribution in Children and Adolescents in Spain: A National Dietary Survey on the Child and Adolescent Population, ENALIA 2013–2014. Eur. J. Nutr. 2019, 58, 705–719. [Google Scholar] [CrossRef]
- Sofi, F.; Martini, D.; Angelino, D.; Cairella, G.; Campanozzi, A.; Danesi, F.; Dinu, M.; Erba, D.; Iacoviello, L.; Pellegrini, N.; et al. Mediterranean Diet: Why a New Pyramid? An Updated Representation of the Traditional Mediterranean Diet by the Italian Society of Human Nutrition (SINU). Nutr. Metab. Cardiovasc. Dis. 2025, 35, 103919. [Google Scholar] [CrossRef]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for the Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef]
- Fouillet, H.; Dussiot, A.; Perraud, E.; Wang, J.; Huneau, J.F.; Kesse-Guyot, E.; Mariotti, F. Plant to Animal Protein Ratio in the Diet: Nutrient Adequacy, Long-Term Health and Environmental Pressure. Front. Nutr. 2023, 10, 1178121. [Google Scholar] [CrossRef]
- Health Council of the Netherlands. A Healthy Protein Transition_Executive Summary. Available online: https://www.healthcouncil.nl/documents/2023/12/13/a-healthy-protein-transition (accessed on 11 December 2025).
- Toujgani, H.; Brunin, J.; Perraud, E.; Allès, B.; Touvier, M.; Lairon, D.; Mariotti, F.; Pointereau, P.; Baudry, J.; Kesse-Guyot, E. The Nature of Protein Intake as a Discriminating Factor of Diet Sustainability: A Multi-Criteria Approach. Sci. Rep. 2023, 13, 17850. [Google Scholar] [CrossRef] [PubMed]
- Daas, M.C.; van ’t Veer, P.; Temme, E.H.M.; Kuijsten, A.; Gurinović, M.; Biesbroek, S. Diversity of Dietary Protein Patterns across Europe—Impact on Nutritional Quality and Environmental Sustainability. Curr. Res. Food Sci. 2025, 10, 101019. [Google Scholar] [CrossRef]
- Osadchiy, T.; Poliakov, I.; Olivier, P.; Rowland, M.; Foster, E. Progressive 24-Hour Recall: Usability Study of Short Retention Intervals in Web-Based Dietary Assessment Surveys. J. Med. Internet Res. 2020, 22, e13266. [Google Scholar] [CrossRef] [PubMed]
- CREA Centro di Ricerca Alimenti e Nutrizione. Linee Guida per una Sana Alimentazione. Revisione 2018. Available online: https://www.crea.gov.it/web/alimenti-e-nutrizione/-/linee-guida-per-una-sana-alimentazione-2018 (accessed on 13 November 2025).
- Roman Viñas, B.; Ribas Barba, L.; Ngo, J.; Gurinovic, M.; Novakovic, R.; Cavelaars, A.; De Groot, L.C.P.G.M.; Van’T Veer, P.; Matthys, C.; Serra Majem, L. Projected Prevalence of Inadequate Nutrient Intakes in Europe. Ann. Nutr. Metab. 2011, 59, 84–95. [Google Scholar] [CrossRef]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C.; et al. Vitamin D Deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef]
- Poslusna, K.; Ruprich, J.; de Vries, J.H.; Jakubikova, M.; van’t Veer, P. Misreporting of Energy and Micronutrient Intake Estimated by Food Records and 24 Hour Recalls, Control and Adjustment Methods in Practice. Br. J. Nutr. 2009, 101, S73–S85. [Google Scholar] [CrossRef]
- Lopes, T.S.; Luiz, R.R.; Hoffman, D.J.; Ferriolli, E.; Pfrimer, K.; Moura, A.S.; Sichieri, R.; Pereira, R.A. Misreport of Energy Intake Assessed with Food Records and 24-h Recalls Compared with Total Energy Expenditure Estimated with DLW. Eur. J. Clin. Nutr. 2016, 70, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Kaczkowski, C.H.; Jones, P.J.H.; Feng, J.; Bayley, H.S. Human Nutrition and Metabolism-Research Communication Four-Day Multimedia Diet Records Underestimate Energy Needs in Middle-Aged and Elderly Women as Determined by Doubly-Labeled Water 1. J. Nutr. 2000, 130, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Hébert, J.R.; Hurley, T.G.; Steck, S.E.; Miller, D.R.; Tabung, F.K.; Peterson, K.E.; Kushi, L.H.; Frongillo, E.A. Considering the Value of Dietary Assessment Data in Informing Nutrition-Related Health Policy. Adv. Nutr. 2014, 5, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Springmann, M. Estimates of Energy Intake, Requirements and Imbalances Based on Anthropometric Measurements at Global, Regional and National Levels and for Sociodemographic Groups: A Modelling Study. BMJ Public Health 2025, 3, e002244. [Google Scholar] [CrossRef]
- Serra, M.; Alceste, D.; Hauser, F.; Hulshof, P.J.M.; Meijer, H.A.J.; Thalheimer, A.; Steinert, R.E.; Gerber, P.A.; Spector, A.C.; Gero, D.; et al. Assessing Daily Energy Intake in Adult Women: Validity of a Food-Recognition Mobile Application Compared to Doubly Labelled Water. Front. Nutr. 2023, 10, 1255499. [Google Scholar] [CrossRef]
- Forrestal, S.G. Energy Intake Misreporting among Children and Adolescents: A Literature Review. Matern. Child. Nutr. 2011, 7, 112–127. [Google Scholar] [CrossRef] [PubMed]
| Weight (kg) | Height (cm) | BMI (kg/m2) | BMI Class (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex | Age Groups (ys) | n | Mean (SD) | Mean (SD) | Mean (SD) | Underweight | Normal | Overweight | Obese |
| Male | 3–11 (months) | 75 | 9.2 (1.6) | 71.9 (4.9) | 17.8 (2.2) | 1.3 | 66.7 | 21.3 | 10.7 |
| 1–2 | 162 | 13.2 (2.0) | 89.1 (6.9) | 16.6 (1.7) | 3.5 | 63.8 | 23.4 | 9.4 | |
| 3–9 | 168 | 23.9 (9.0) | 117.0 (15.1) | 17.0 (3.1) | 1.2 | 58.5 | 22.1 | 18.2 | |
| 10–17 | 138 | 58.4 (14.3) | 165.2 (13.7) | 21.2 (3.7) | 0.9 | 86.8 | 9.8 | 2.5 | |
| 18–64 | 346 | 80.7 (14.2) | 176.4 (6.9) | 25.9 (4.4) | 0.2 | 49.0 | 37.8 | 12.9 | |
| 65–74 | 65 | 81.6 (13.9) | 169.3 (6.6) | 28.4 (4.1) | 0.0 | 19.2 | 52.8 | 28.0 | |
| Female | 3–11 (months) | 75 | 8.3 (1.4) | 70.1 (4.7) | 16.7 (1.5) | 1.3 | 84.0 | 10.7 | 4.0 |
| 1–2 | 160 | 12.5 (2.1) | 87.7 (7.1) | 16.2 (2.0) | 0.4 | 75.4 | 17.3 | 6.9 | |
| 3–9 | 171 | 23.9 (8.1) | 117.7 (13.8) | 16.8 (2.9) | 2.0 | 63.7 | 21.2 | 13.2 | |
| 10–17 | 138 | 54.8 (13.1) | 159.5 (8.5) | 21.4 (4.2) | 0.0 | 90.5 | 6.8 | 2.7 | |
| 18–64 | 380 | 64.2 (13) | 162.9 (6.2) | 24.2 (4.8) | 5.1 | 63.1 | 19.7 | 12.2 | |
| 65–74 | 91 | 69.5 (15.6) | 157.6 (7.5) | 28.1 (6.7) | 0.8 | 42.0 | 28.0 | 29.2 | |
| Total | 3–11 (months) | 150 | 8.7 (1.5) | 71.0 (4.9) | 17.2 (1.9) | 1.3 | 75.3 | 16.0 | 7.3 |
| 1–2 | 322 | 12.8 (2.1) | 88.4 (7.0) | 16.4 (1.8) | 2.0 | 69.5 | 20.4 | 8.1 | |
| 3–9 | 339 | 23.9 (8.5) | 117.4 (14.4) | 16.9 (3.0) | 1.6 | 61.1 | 21.7 | 15.6 | |
| 10–17 | 276 | 56.6 (13.8) | 162.4 (11.8) | 21.3 (3.9) | 0.5 | 88.7 | 8.3 | 2.6 | |
| 18–64 | 726 | 72.0 (15.9) | 169.2 (9.4) | 25.0 (4.7) | 2.8 | 56.5 | 28.2 | 12.5 | |
| 65–74 | 156 | 74.6 (16.0) | 162.5 (9.1) | 28.2 (5.8) | 0.5 | 32.5 | 38.4 | 28.7 | |
| Males (n = 954) | Females (n = 1015) | Total (n = 1969) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | |
| Energy (kcal/day) | 1828.2 | 648.8 | 896.5 | 1311 | 1792 | 2273.5 | 2955.3 | 1515.1 | 419.4 | 863.8 | 1209.5 | 1499.8 | 1782.5 | 2251 | 1666.8 | 562.3 | 871.5 | 1237.9 | 1598 | 2017.2 | 2661.2 |
| Energy (MJ/day) | 7.65 | 2.71 | 3.75 | 5.49 | 7.50 | 9.51 | 12.36 | 6.34 | 1.75 | 3.61 | 5.06 | 6.28 | 7.46 | 9.42 | 6.97 | 2.35 | 3.65 | 5.18 | 6.69 | 8.44 | 11.13 |
| Protein (g/day) | 73.6 | 30.1 | 29.5 | 51.3 | 71.4 | 91.8 | 123.2 | 60.3 | 19 | 30.3 | 46.9 | 59.5 | 73.1 | 92.9 | 66.7 | 25.8 | 29.3 | 48.4 | 64.6 | 81.8 | 111.4 |
| Protein (g/kg bw) | 2.0 | 1.1 | 0.8 | 1.2 | 1.7 | 2.7 | 4.3 | 1.9 | 1.0 | 0.7 | 1.1 | 1.5 | 2.6 | 3.9 | 2.0 | 1.1 | 0.7 | 1.1 | 1.6 | 2.6 | 4.1 |
| Animal protein (g/day) | 48.8 | 21.2 | 20.3 | 33.8 | 45.8 | 60.3 | 89.0 | 39.4 | 13.4 | 19.2 | 29.6 | 38.6 | 47.8 | 63.5 | 44.0 | 17.9 | 19.3 | 31.4 | 41.5 | 53.8 | 76.1 |
| Animal protein (% on total) | 66.7 | 7.9 | 53.8 | 62.5 | 67.2 | 71.7 | 77.9 | 65.7 | 8.6 | 51.1 | 61.2 | 66.3 | 71.1 | 77.3 | 66.2 | 8.3 | 52.3 | 61.7 | 66.8 | 71.4 | 77.6 |
| Fat (g/day) | 76.8 | 29.2 | 37.3 | 52.9 | 73.8 | 96.1 | 132.3 | 64.6 | 19.2 | 36.0 | 50.0 | 63.4 | 77.7 | 98.4 | 70.5 | 24.9 | 36.3 | 51.6 | 67.5 | 85.2 | 116.8 |
| SFAs (a) (g/day) | 24.8 | 9.0 | 13.2 | 17.8 | 23.3 | 29.8 | 41.7 | 20.9 | 6.0 | 11.9 | 16.3 | 20.5 | 25.0 | 30.9 | 22.8 | 7.8 | 12.3 | 17.1 | 21.8 | 27.3 | 36.9 |
| MUFA s (b) (g/day) | 35.2 | 14.1 | 16.1 | 23.9 | 33.6 | 44.0 | 60.7 | 29.6 | 9.3 | 16.1 | 22.8 | 28.9 | 35.7 | 47.3 | 32.4 | 12 | 16.00 | 23.2 | 30.7 | 39.4 | 54.5 |
| PUFAs (c) (g/day) | 10.6 | 5.1 | 4.5 | 6.9 | 9.7 | 13.3 | 19.6 | 9.0 | 3.6 | 4.4 | 6.4 | 8.5 | 10.9 | 15.0 | 9.8 | 4.4 | 4.4 | 6.6 | 9.0 | 12.1 | 17.4 |
| Cholesterol (mg/day) | 273.8 | 121.3 | 107.4 | 190.9 | 256.3 | 337.8 | 506.9 | 220.6 | 72.7 | 108.1 | 172.5 | 214.0 | 263.5 | 350.4 | 246.4 | 100.7 | 105.8 | 177.6 | 232.8 | 301.1 | 426.6 |
| Carbohydrates (g/day) | 211.6 | 71.5 | 109.3 | 157.8 | 204 | 256 | 339.1 | 178.1 | 50.2 | 104.1 | 142 | 173.6 | 208.1 | 268.7 | 194.3 | 63.4 | 105.5 | 148.5 | 186.4 | 233.3 | 306.5 |
| Starch (g/day) | 119.7 | 50.3 | 47.5 | 81.8 | 116.1 | 151.1 | 207.7 | 96.7 | 34.6 | 43.7 | 73.3 | 95.5 | 120.9 | 156.4 | 107.8 | 44.2 | 43.6 | 76.6 | 103.5 | 136.1 | 185.6 |
| Total sugars (g/day) | 79.4 | 26.4 | 42.6 | 60.9 | 75.5 | 93.5 | 126.8 | 71.2 | 20.8 | 41.1 | 56.7 | 67.9 | 83.8 | 109.5 | 75.2 | 23.9 | 42.1 | 58.5 | 71.7 | 87.9 | 119.2 |
| Dietary fibre (g/day) | 15.4 | 7.5 | 5.8 | 9.7 | 13.9 | 19.6 | 29.4 | 13.9 | 6.1 | 5.7 | 9.3 | 12.9 | 17.8 | 24.4 | 14.6 | 6.8 | 5.8 | 9.5 | 13.3 | 18.7 | 27.0 |
| Dietary fibre (g/1000 kcal/day) | 8.4 | 2.6 | 4.8 | 6.6 | 8.2 | 9.9 | 13.4 | 9.2 | 2.9 | 5.2 | 7.1 | 8.9 | 11.0 | 14.6 | 8.8 | 2.8 | 5.0 | 6.9 | 8.5 | 10.4 | 13.9 |
| % Total energy from | |||||||||||||||||||||
| Protein (%En) | 16 | 3 | 12 | 14 | 16 | 18 | 20 | 16 | 3 | 12 | 14 | 16 | 18 | 21 | 16 | 3 | 12 | 14 | 16 | 18 | 21 |
| Fat (%En) | 38 | 4 | 31 | 35 | 37 | 40 | 45 | 38 | 4 | 32 | 35 | 38 | 41 | 45 | 38 | 4 | 31 | 35 | 38 | 41 | 45 |
| SFAs (a) (%En) | 12 | 2 | 9 | 11 | 12 | 14 | 16 | 12 | 2 | 9 | 11 | 12 | 14 | 16 | 12 | 2 | 9 | 11 | 12 | 14 | 16 |
| MUFAs (b) (%En) | 17 | 3 | 13 | 15 | 17 | 19 | 22 | 18 | 3 | 14 | 16 | 17 | 19 | 22 | 17 | 3 | 13 | 16 | 17 | 19 | 22 |
| PUFAs (c) (%En) | 5 | 1 | 4 | 4 | 5 | 6 | 7 | 5 | 1 | 4 | 5 | 5 | 6 | 7 | 5 | 1 | 4 | 4 | 5 | 6 | 7 |
| Carbohydrates (%En) | 44 | 6 | 35 | 40 | 44 | 48 | 54 | 45 | 5 | 36 | 41 | 45 | 48 | 52 | 45 | 5 | 36 | 41 | 45 | 48 | 53 |
| Total sugars (%En) | 19 | 6 | 11 | 15 | 18 | 22 | 30 | 20 | 5 | 13 | 16 | 19 | 23 | 29 | 19 | 6 | 11 | 15 | 19 | 22 | 29 |
| Vitamins | |||||||||||||||||||||
| Vitamin A (REs µg/day) | 787.8 | 319.6 | 383.4 | 581.2 | 741.7 | 936.7 | 1317 | 730.6 | 266.7 | 387.4 | 554.5 | 688.9 | 867.7 | 1180.3 | 758.3 | 293.9 | 384.5 | 570.7 | 711.8 | 900.3 | 1248 |
| β-carotene (µg/day) | 2915.9 | 1742 | 832.6 | 1685.7 | 2491.9 | 3839.6 | 6235.9 | 2842.6 | 1521.9 | 913.3 | 1749.6 | 2580.6 | 3609 | 5715.2 | 2878.3 | 1632.1 | 874.7 | 1723.9 | 2544.6 | 3703.8 | 5984.9 |
| Total folate (µg/day) | 258.3 | 112.4 | 111.2 | 174.4 | 237.7 | 327.1 | 456.2 | 230.0 | 95.5 | 109.1 | 160.4 | 214.3 | 283.4 | 398.7 | 248.6 | 104.9 | 114.9 | 172.6 | 229.7 | 311.7 | 431.5 |
| Dietary folate equivalent (e) (µg/day) | 263.4 | 112.0 | 118.3 | 180 | 243.7 | 331.8 | 458.4 | 234.7 | 96.1 | 113.7 | 164.7 | 219.3 | 288.4 | 402.8 | 243.8 | 104.5 | 111.2 | 167.5 | 224.6 | 306.1 | 428.2 |
| Vitamin B12 (µg/day) | 4.8 | 2.8 | 1.8 | 3.1 | 4.2 | 5.7 | 9.7 | 3.8 | 1.8 | 1.6 | 2.7 | 3.6 | 4.5 | 6.9 | 4.3 | 2.3 | 1.7 | 2.9 | 3.9 | 5.1 | 8.3 |
| Vitamin C (mg/day) | 104.2 | 56.6 | 36.7 | 65.7 | 94.1 | 132.2 | 209.1 | 98.2 | 50.4 | 35.1 | 62.3 | 87.1 | 123.9 | 199.7 | 101.1 | 53.4 | 36.2 | 63.7 | 90.7 | 127.1 | 203.2 |
| Vitamin D (µg/day) | 2.9 | 1.9 | 1.0 | 1.7 | 2.4 | 3.6 | 6.6 | 2.4 | 1.5 | 0.8 | 1.4 | 2.0 | 2.8 | 5.5 | 2.6 | 1.7 | 0.9 | 1.6 | 2.2 | 3.2 | 6.0 |
| Vitamin E (mg/day) | 11.5 | 4.9 | 4.7 | 8 | 10.7 | 14.4 | 20.7 | 10.2 | 3.7 | 4.9 | 7.4 | 9.7 | 12.5 | 16.8 | 10.8 | 4.4 | 4.7 | 7.7 | 10.2 | 13.5 | 19 |
| Minerals | |||||||||||||||||||||
| Calcium (mg/day) | 774.7 | 232.9 | 427.9 | 614.4 | 756.7 | 911.5 | 1181.7 | 694.9 | 208.8 | 375.2 | 548 | 678.5 | 826.9 | 1055.8 | 733.6 | 224.1 | 399.9 | 575.6 | 716.6 | 864.8 | 1124.9 |
| Iron (mg/day) | 10.4 | 4.0 | 4.8 | 7.3 | 9.9 | 13.1 | 17.6 | 8.7 | 3.0 | 4.6 | 6.5 | 8.5 | 10.7 | 14.1 | 9.5 | 3.6 | 4.6 | 6.9 | 9.1 | 11.8 | 15.9 |
| Magnesium (mg/day) | 275.2 | 130.8 | 96.9 | 174.8 | 260.9 | 353.9 | 518.6 | 234.1 | 93.9 | 100.1 | 168.1 | 219.5 | 293 | 404.4 | 254.1 | 114.8 | 97.6 | 170.5 | 236.6 | 323.2 | 457.5 |
| Potassium (mg/day) | 2640.4 | 1087.4 | 1049.4 | 1792.5 | 2564.6 | 3363 | 4491.6 | 2341.4 | 835.5 | 1065.3 | 1738.9 | 2249.3 | 2908.6 | 3795.5 | 2485.9 | 975.9 | 1049.5 | 1757.1 | 2395.1 | 3110 | 4262.4 |
| Zinc (mg/day) | 10.0 | 3.8 | 4.8 | 7.2 | 9.5 | 12.2 | 17.1 | 8.3 | 2.5 | 4.8 | 6.6 | 8.1 | 9.7 | 13 | 9.1 | 3.3 | 4.7 | 6.8 | 8.7 | 11 | 15.2 |
| Males (n = 168) | Females (n = 171) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | |
| Energy (kcal/day) | 1519.3 | 341.0 | 1066.6 | 1274.4 | 1495.4 | 1717.7 | 2144.5 | 1380–1790 (f) | 1413.9 | 217.0 | 1077.1 | 1242.5 | 1414.8 | 1564.1 | 1741.6 | 1280–1650 (f) |
| Energy (MJ/day) | 6.36 | 1.43 | 4.46 | 5.33 | 6.26 | 7.19 | 8.97 | 5.77–7.49 (f) | 5.92 | 0.91 | 4.51 | 5.20 | 5.92 | 6.54 | 7.29 | 5.36–6.90 (f) |
| Protein (g/day) | 58.6 | 12.3 | 40.9 | 50.6 | 57.5 | 65.7 | 83.1 | 14.8–29.3 | 54.5 | 8.1 | 41.5 | 49.3 | 53.8 | 60.5 | 68.2 | 14.6–29.7 |
| Protein (g/kg bw) | 2.6 | 0.8 | 1.5 | 2.1 | 2.6 | 3.2 | 4.1 | 0.97–0.99 | 2.4 | 0.6 | 1.5 | 2.0 | 2.4 | 2.8 | 3.3 | 0.97–0.99 |
| Animal protein (g/day) | 39.0 | 9.8 | 24.8 | 32.4 | 37.9 | 45.3 | 55.9 | 36.2 | 6.6 | 25.3 | 32.2 | 35.5 | 40.7 | 47.9 | ||
| Animal protein (% on total) | 66.7 | 8.1 | 52.9 | 62.4 | 67.4 | 72.3 | 77.9 | 67.0 | 6.2 | 57.5 | 63.1 | 66.7 | 71.0 | 76.7 | ||
| Fats (g/day) | 63.3 | 16.1 | 41.0 | 50.4 | 62.6 | 74.4 | 90.9 | 59.7 | 10.7 | 43.5 | 51.0 | 59.2 | 66.5 | 76.8 | ||
| SFAs (a) (g/day) | 21.4 | 6.4 | 13.1 | 16.5 | 20.5 | 26.0 | 31.6 | 20.2 | 4.0 | 13.4 | 17.5 | 20.1 | 22.8 | 27.4 | ||
| MUFAs (b) (g/day) | 28.0 | 6.6 | 18.5 | 23.1 | 27.8 | 32.2 | 38.9 | 26.0 | 4.6 | 18.1 | 23.1 | 26.2 | 28.8 | 33.3 | ||
| PUFAs (c) (g/day) | 8.5 | 2.4 | 5.3 | 6.8 | 8.0 | 9.5 | 13.2 | 8.5 | 2.4 | 5.1 | 6.9 | 8.2 | 9.6 | 13.2 | ||
| Cholesterol (mg/day) | 250.7 | 72.9 | 148.4 | 205.2 | 234.6 | 292.1 | 387.3 | 221.3 | 18.1 | 191.1 | 209.3 | 220.2 | 232.7 | 254.2 | ||
| Carbohydrates (g/day) | 189.3 | 46.5 | 127.8 | 154.6 | 183.7 | 218.7 | 263.5 | 174.0 | 29.2 | 128.6 | 157.3 | 171.5 | 195.4 | 223.5 | ||
| Starch (g/day) | 101.2 | 26.3 | 65.9 | 81.8 | 99.2 | 119.1 | 145.2 | 94.2 | 19.5 | 62.5 | 80.3 | 93.0 | 106.9 | 126.5 | ||
| Total sugars (g/day) | 76.6 | 26.6 | 37.6 | 58.8 | 74.5 | 88.3 | 123.9 | 69.6 | 21.6 | 37.3 | 53.9 | 66.7 | 82.4 | 110.3 | ||
| Dietary fibre (g/day) | 11.6 | 4.2 | 6.1 | 8.8 | 11.1 | 13.7 | 18.6 | 10.9 | 3.0 | 6.5 | 8.6 | 10.4 | 12.6 | 17.2 | ||
| Dietary fibre (g/1000 kcal/day) | 7.7 | 2.2 | 4.6 | 6.2 | 7.5 | 8.9 | 11.0 | 8.4 (i) | 7.8 | 2.1 | 5.1 | 6.5 | 7.5 | 8.9 | 12.1 | 8.4 (i) |
| % Total energy from | ||||||||||||||||
| Protein (% En) | 16 | 2 | 13 | 15 | 16 | 17 | 19 | 10–15 | 16 | 0.0 | 15 | 16 | 16 | 16 | 16 | 10–15 |
| Fat (% En) | 37 | 4 | 32 | 35 | 37 | 40 | 44 | 20–35 (g) | 38 | 4 | 32 | 35 | 38 | 40 | 43 | 20–35 (g) |
| SFAs (a) (% En) | 13 | 2 | 10 | 11 | 13 | 14 | 16 | <10 (h) | 13 | 2 | 10 | 12 | 13 | 14 | 15 | <10 (h) |
| MUFAs (b) (% En) | 17 | 2 | 14 | 15 | 16 | 18 | 20 | 17 | 2 | 13 | 15 | 17 | 18 | 19 | ||
| PUFAs (c) (% En) | 5 | 1 | 4 | 5 | 5 | 5 | 6 | 5–10 (g) | 5 | 1 | 4 | 5 | 5 | 6 | 7 | 5–10 (g) |
| Carbohydrates (% En) | 47 | 4 | 40 | 44 | 47 | 50 | 53 | 45–60 (g) | 46 | 4 | 40 | 44 | 46 | 49 | 52 | 45–60 (g) |
| Total sugars (% En) | 21 | 4 | 14 | 17 | 20 | 23 | 29 | <15 (h) | 20 | 6 | 12 | 15 | 20 | 24 | 29 | <15 (h) |
| Vitamins | ||||||||||||||||
| Vitamin A (REs µg/day) | 642.0 | 233.8 | 278.5 | 482.3 | 609.4 | 765.9 | 1081.6 | 250–400 | 644.4 | 194.7 | 378.6 | 524.1 | 609.0 | 751.1 | 947.8 | 250–400 |
| β-carotene (µg/day) | 2384.5 | 1320.0 | 771.0 | 1476.5 | 2116.6 | 3170.0 | 4904.1 | 2343.6 | 985.6 | 1022.7 | 1691.9 | 2195.8 | 2919.0 | 4113.4 | ||
| Total folate (µg/day) | 195.5 | 58.5 | 114.8 | 156.9 | 188.6 | 231.2 | 289.0 | 120–200 | 182.7 | 37.8 | 130.8 | 156.8 | 179.6 | 205.2 | 251.1 | 120–200 |
| Dietary folate equivalent (µg/day) (l) | 200.5 | 62.9 | 114.7 | 157.5 | 190.7 | 238.5 | 312.3 | 187.0 | 41.7 | 130.1 | 157.2 | 183.3 | 212.2 | 259.1 | ||
| Vitamin B12 (µg/day) | 3.4 | 1.2 | 1.8 | 2.7 | 3.2 | 4.1 | 5.3 | 1.4–2.5 (i) | 3.4 | 1.0 | 2.2 | 2.9 | 3.4 | 3.8 | 4.6 | 1.4–2.5 (i) |
| Vitamin C (mg/day) | 71.8 | 37.0 | 28.0 | 44.9 | 61.5 | 96.2 | 142.6 | 35–60 | 71.3 | 31.7 | 25.9 | 50.3 | 66.3 | 86.6 | 130.7 | 35–60 |
| Vitamin D (µg/day) | 1.7 | 0.6 | 0.9 | 1.3 | 1.6 | 1.9 | 2.5 | 15 | 1.7 | 0.5 | 0.9 | 1.4 | 1.7 | 2.0 | 2.6 | 15 |
| Vitamin E (mg/day) | 8.8 | 2.0 | 5.8 | 7.3 | 8.7 | 9.8 | 13.1 | 5–8 (i) | 8.5 | 1.9 | 5.7 | 7.3 | 8.3 | 9.7 | 11.7 | 5–8 (i) |
| Minerals | ||||||||||||||||
| Calcium (mg/day) | 702.0 | 207.9 | 376.5 | 575.1 | 697.1 | 808.8 | 1018.0 | 510–1040 | 631.4 | 171.9 | 383.6 | 504.2 | 624.9 | 731.1 | 978.8 | 510–1040 |
| Iron (mg/day) | 7.7 | 1.9 | 4.7 | 6.5 | 7.6 | 8.6 | 11.4 | 8–13 | 7.1 | 1.3 | 5.3 | 6.1 | 6.9 | 8.1 | 9.3 | 8–13 |
| Magnesium (mg/day) | 199.6 | 47.2 | 131.2 | 168.5 | 193.1 | 227.7 | 285.0 | 120–220 (i) | 190.8 | 39.5 | 136.4 | 163.4 | 188.7 | 213.0 | 254.6 | 120–220 (i) |
| Potassium (mg/day) | 2040.5 | 581.8 | 1199.8 | 1627.7 | 1995.9 | 2365.0 | 3045.3 | 1900–2700 (h) | 1939.5 | 373.7 | 1354.7 | 1672.1 | 1903.7 | 2149.9 | 2640.8 | 1900–2700 (h) |
| Zinc (mg/day) | 7.8 | 1.6 | 5.3 | 6.6 | 7.7 | 8.7 | 10.4 | 5–8 | 7.2 | 1.1 | 5.5 | 6.5 | 7.2 | 8.0 | 9.0 | 5–8 |
| Males (n = 138) | Females (n = 138) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | |
| Energy (kcal/day) | 2230.1 | 477.4 | 1508.9 | 1934.6 | 2226.7 | 2456.4 | 2996.2 | 1900–2870 (f) | 1801.3 | 377.4 | 1213.6 | 1544.2 | 1773 | 2041.2 | 2415.9 | 1170–2310 (f) |
| Energy (MJ/day) | 9.33 | 2.00 | 6.31 | 8.09 | 9.32 | 10.28 | 12.54 | 7.95–12.01 (f) | 7.54 | 1.58 | 5.08 | 6.46 | 7.42 | 8.54 | 10.11 | 4.9–9.67 (f) |
| Protein (g/day) | 92.7 | 23.9 | 58 | 77.2 | 90.1 | 105.1 | 144.8 | 32.2–61.5 | 73.6 | 12.3 | 54 | 64.2 | 72 | 82.5 | 96.4 | 33.3–50.7 |
| Protein (g/kg bw) | 1.6 | 0.5 | 0.9 | 1.2 | 1.6 | 1.9 | 2.6 | 0.98–0.93 | 1.4 | 0.4 | 0.9 | 1.1 | 1.4 | 1.6 | 2.1 | 0.98–0.90 |
| Animal protein (g/day) | 62.2 | 21.1 | 32 | 47.2 | 59 | 72 | 102.7 | 48.6 | 10.5 | 32 | 41.8 | 47.6 | 56.6 | 67.2 | ||
| Animal protein (% on total) | 66.2 | 7.6 | 52.2 | 61.6 | 66.5 | 70.5 | 78.0 | 65.8 | 7.3 | 52.8 | 61.2 | 66.1 | 70.8 | 76.3 | ||
| Fat (g/day) | 98 | 25.1 | 60 | 78.9 | 96 | 112.3 | 140.8 | 76.9 | 16.3 | 53.7 | 65 | 74.8 | 85.3 | 106.4 | ||
| SFAs (a) (g/day) | 32 | 8.9 | 18.7 | 25.6 | 31.6 | 37.4 | 48.6 | 25.2 | 5.6 | 16.5 | 21.6 | 25 | 28.8 | 36.1 | ||
| MUFAs (b) (g/day) | 44.3 | 12.6 | 25.3 | 35.3 | 42.1 | 51.3 | 68 | 34.3 | 6.4 | 24.2 | 29.6 | 33.4 | 38.5 | 45.8 | ||
| PUFAs (c) (g/day) | 13.8 | 3.6 | 8.7 | 11.8 | 13.4 | 15.7 | 21.2 | 11.1 | 3.9 | 6.1 | 8.6 | 10.6 | 12.5 | 18.3 | ||
| Cholesterol (mg/day) | 356.9 | 122.1 | 194.7 | 269.7 | 337.9 | 421.9 | 585.8 | 295 | 34.5 | 234.5 | 270.1 | 295.4 | 314.1 | 351.6 | ||
| Carbohydrates (g/day) | 257.5 | 58.7 | 166.1 | 213.4 | 256.1 | 291.7 | 370.1 | 213.9 | 54 | 129.5 | 175 | 209.8 | 252.5 | 308.8 | ||
| Starch (g/day) | 155.4 | 38.9 | 94 | 132.5 | 152.1 | 176.8 | 222.9 | 123.3 | 29 | 75.4 | 104.7 | 125.8 | 142.3 | 170.7 | ||
| Total sugars (g/day) | 86.8 | 25 | 51.1 | 67.9 | 82 | 99.8 | 135.9 | 78.9 | 25.1 | 45.2 | 59.7 | 73.5 | 95.1 | 129.1 | ||
| Dietary fibre (g/day) | 16.4 | 5.1 | 9.1 | 12.8 | 15.6 | 19.3 | 26 | 14.5 | 4.2 | 8.3 | 11.3 | 14.1 | 17.3 | 22.4 | ||
| Dietary fibre (g/1000 kcal/day) | 7.5 | 2.3 | 4.7 | 5.8 | 7.3 | 8.7 | 12.1 | 8.4 (i) | 8.3 | 2.2 | 5.1 | 6.8 | 8.1 | 9.6 | 11.8 | 8.4 (i) |
| % Total energy from | ||||||||||||||||
| Protein (% En) | 17 | 2 | 13 | 15 | 17 | 18 | 21 | 15 | 17 | 2 | 14 | 15 | 16 | 18 | 20 | 15 |
| Fat (% En) | 39 | 4 | 33 | 37 | 39 | 41 | 46 | 20–35 (g) | 38 | 4 | 32 | 36 | 38 | 40 | 45 | 20–35 (g) |
| SFAs (a) (% En) | 13 | 2 | 10 | 12 | 13 | 14 | 15 | <10 (h) | 12 | 2 | 9 | 11 | 12 | 14 | 16 | <10 (h) |
| MUFAs (b) (% En) | 18 | 3 | 13 | 16 | 18 | 19 | 23 | 17 | 2 | 14 | 16 | 17 | 18 | 20 | ||
| PUFAs (c) (% En) | 6 | 0 | 5 | 5 | 5 | 6 | 6 | 5–10 (g) | 5 | 1 | 4 | 5 | 5 | 6 | 8 | 5–10 (g) |
| Carbohydrates (% En) | 44 | 6 | 34 | 41 | 44 | 47 | 52 | 45–60 (g) | 45 | 4 | 36 | 42 | 45 | 48 | 52 | 45–60 (g) |
| Total sugars (% En) | 16 | 4 | 10 | 13 | 16 | 18 | 22 | <15 (h) | 18 | 3 | 14 | 16 | 17 | 19 | 23 | <15 (h) |
| Vitamins | ||||||||||||||||
| Vitamin A (REs µg/day) | 762.7 | 282.3 | 377.9 | 577.8 | 704.8 | 941.6 | 1262.1 | 400–750 | 701.2 | 240 | 366.2 | 537 | 668.5 | 859.7 | 1087.4 | 400–650 |
| β-carotene (µg/day) | 2892.1 | 1624.6 | 1014.6 | 1641.6 | 2456 | 3750.1 | 5986 | 2762.3 | 1221 | 1110.8 | 1965 | 2689.3 | 3305.7 | 4910.3 | ||
| Total folate (µg/day) | 280.5 | 85.6 | 169.9 | 216.8 | 261.4 | 327.7 | 432.6 | 270–330 | 238.6 | 64.4 | 149.7 | 196.7 | 232.6 | 271.8 | 364.8 | 270–330 |
| Dietary folate equivalent (µg/day) (l) | 286.7 | 90 | 171.4 | 220.8 | 264.5 | 335.1 | 452.7 | 244.3 | 67.4 | 151.3 | 198.6 | 237.5 | 274.7 | 367.7 | ||
| Vitamin B12 (µg/day) | 5.7 | 1.6 | 3.4 | 4.5 | 5.5 | 6.4 | 9.2 | 2.5–4 (i) | 4.6 | 1.3 | 2.9 | 3.9 | 4.5 | 5.2 | 7.1 | 2.5–4 (i) |
| Vitamin C (mg/day) | 90.2 | 44.2 | 33.3 | 58.1 | 78.9 | 115.3 | 181.8 | 60–105 | 86.9 | 45.3 | 30.5 | 56 | 77.4 | 113.8 | 163.4 | 60–85 |
| Vitamin D (µg/day) | 2.9 | 1.6 | 1.2 | 1.9 | 2.5 | 3.5 | 5.8 | 15 | 2.1 | 0.4 | 1.4 | 1.8 | 2 | 2.3 | 2.8 | 15 |
| Vitamin E (mg/day) | 13.3 | 3.8 | 7.8 | 10.5 | 12.6 | 15.9 | 20.3 | 8–13 (i) | 10.9 | 3.3 | 6.5 | 8.6 | 10.5 | 13 | 17.3 | 8–12 (i) |
| Minerals | ||||||||||||||||
| Calcium (mg/day) | 868.3 | 244.8 | 503.4 | 701.1 | 856.2 | 1018.5 | 1217.9 | 1040–1150 | 708.8 | 169 | 431.5 | 582 | 697.7 | 832.4 | 1019.3 | 1040–1150 |
| Iron (mg/day) | 11.5 | 2.7 | 7.6 | 9.5 | 11.5 | 13.2 | 16.1 | 13 | 9.8 | 2.1 | 6.4 | 8.5 | 9.9 | 11.1 | 14.1 | 13–18 |
| Magnesium (mg/day) | 294.5 | 65.1 | 202.5 | 250.6 | 288 | 335.9 | 398.7 | 220–380 (i) | 248.8 | 56.2 | 169.6 | 203.9 | 244 | 288.4 | 350 | 220–310 (i) |
| Potassium (mg/day) | 2886.3 | 639.6 | 1745.3 | 2499.5 | 2830.9 | 3320.9 | 3924.1 | 4500 (h) | 2494 | 562.9 | 1677.8 | 2086 | 2428.2 | 2780 | 3559.4 | 4500 (h) |
| Zinc (mg/day) | 12.0 | 3.3 | 7.4 | 9.4 | 11.7 | 13.7 | 18.8 | 8–12 | 9.8 | 2.2 | 6.5 | 8.2 | 9.7 | 11.1 | 13.8 | 8–9 |
| Males (n = 346) | Females (n = 380) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | |
| Energy (kcal/day) | 2271.5 | 396.9 | 1633.2 | 2024.8 | 2242 | 2511.8 | 2951.9 | 2630 (f) | 1737 | 270.5 | 1325.6 | 1552.1 | 1715.9 | 1903.3 | 2197.8 | 2120 (f) |
| Energy (MJ/day) | 9.50 | 1.66 | 6.83 | 8.47 | 9.38 | 10.51 | 12.35 | 11.00 | 7.27 | 1.13 | 5.55 | 6.49 | 7.18 | 7.96 | 9.20 | 8.87 |
| Protein (g/day) | 93.8 | 18.7 | 64.5 | 82.2 | 92 | 104.2 | 125.2 | 63 | 70.8 | 11.9 | 51.3 | 62.3 | 70.3 | 78.4 | 92.3 | 54 |
| Protein (g/kg bw) | 1.2 | 0.3 | 0.7 | 1.0 | 1.2 | 1.3 | 1.7 | 0.9 | 1.1 | 0.3 | 0.8 | 0.9 | 1.1 | 1.3 | 1.6 | 0.9 |
| Animal protein (g/day) | 61 | 16.4 | 36.8 | 50 | 58.5 | 69.1 | 87.7 | 45.1 | 11.5 | 26 | 37.6 | 44.9 | 52.6 | 65.1 | ||
| Animal protein (% on total) | 64.4 | 7.2 | 52.7 | 60.4 | 64.5 | 69.5 | 74.5 | 63.4 | 9.2 | 45.7 | 58.8 | 64.7 | 69.7 | 76.8 | ||
| Fat (g/day) | 95 | 18.3 | 65.2 | 82.5 | 94.5 | 105.9 | 127.2 | 75.1 | 13.2 | 52.8 | 66.2 | 74.6 | 83.8 | 96.8 | ||
| SFAs (a) (g/day) | 29.2 | 6.2 | 20 | 25 | 28.4 | 33.4 | 40.4 | 22.9 | 4.9 | 15.2 | 19.2 | 23.1 | 26.5 | 30.6 | ||
| MUFAs (b) (g/day) | 44.3 | 9 | 29.9 | 38.4 | 43.7 | 50.4 | 58.9 | 35.5 | 6.8 | 24.9 | 30.6 | 34.9 | 40.1 | 47.9 | ||
| PUFAs (c) (g/day) | 13.6 | 3.8 | 8 | 11 | 13.4 | 15.4 | 20.1 | 10.7 | 2.7 | 6.9 | 8.8 | 10.5 | 12.2 | 15.2 | ||
| Cholesterol (mg/day) | 328.6 | 90.7 | 192.4 | 270.9 | 320.9 | 373.6 | 512.7 | 244.2 | 42.2 | 175.9 | 217.4 | 242.1 | 271.6 | 315.2 | ||
| Carbohydrates (g/day) | 251.8 | 54.2 | 163.8 | 216.4 | 247.7 | 280.8 | 346.8 | 195.9 | 40.2 | 132.7 | 168.6 | 192.9 | 224.9 | 263.5 | ||
| Starch (g/day) | 149.7 | 35.1 | 95.1 | 125.4 | 147.7 | 171.7 | 212.3 | 109.7 | 26.1 | 68.4 | 92.2 | 107.7 | 127.2 | 151.6 | ||
| Total sugars (g/day) | 87.2 | 27.4 | 50.6 | 68.8 | 83.9 | 103.7 | 131.5 | 75.2 | 19.9 | 46.2 | 60.6 | 73.6 | 89 | 108.9 | ||
| Dietary fibre (g/day) | 20.2 | 6.2 | 11.1 | 15.8 | 19.6 | 23.8 | 32.1 | 25 (h) | 17.2 | 5.1 | 10.1 | 13.2 | 16.9 | 20.5 | 25.7 | 25 (h) |
| Dietary fibre (g/1000 kcal/day) | 9.1 | 2.5 | 5.5 | 7.4 | 8.9 | 10.6 | 14.2 | 12.6–16.7 (l) | 10.2 | 2.4 | 6.7 | 8.5 | 10.1 | 11.8 | 14.3 | 12.6–16.7 (l) |
| % Total energy from | ||||||||||||||||
| Protein (% En) | 17 | 2 | 14 | 16 | 17 | 18 | 20 | 15 | 17 | 3 | 13 | 15 | 16 | 18 | 21 | 15 |
| Fat (% En) | 37 | 4 | 31 | 35 | 37 | 40 | 44 | 25–30 (g) | 39 | 2 | 35 | 37 | 38 | 40 | 43 | 25–30 (g) |
| SFAs (a) (% En) | 11 | 1 | 10 | 11 | 11 | 12 | 14 | <10 (h) | 12 | 1 | 9 | 11 | 12 | 13 | 14 | <10 (h) |
| MUFAs (b) (% En) | 18 | 3 | 14 | 16 | 17 | 19 | 22 | 18 | 2 | 15 | 17 | 18 | 20 | 22 | ||
| PUFAs (c) (% En) | 5 | 1 | 4 | 5 | 5 | 6 | 7 | 5–10 (g) | 6 | 1 | 4 | 5 | 5 | 6 | 7 | 5–10 (g) |
| Carbohydrates (% En) | 42 | 5 | 35 | 39 | 42 | 45 | 50 | 45–60 (g) | 42 | 5 | 35 | 40 | 43 | 45 | 49 | 45–60 (g) |
| Total sugars (% En) | 16 | 4 | 10 | 13 | 16 | 18 | 22 | <15 (h) | 18 | 4 | 12 | 15 | 17 | 20 | 23 | <15 (h) |
| Vitamins | ||||||||||||||||
| Vitamin A (REs µg/day) | 940.8 | 310 | 529.1 | 739.6 | 898.5 | 1081.4 | 1397.6 | 750 | 832.2 | 280.7 | 452.8 | 655.2 | 783.5 | 968.2 | 1288.1 | 650 |
| β-carotene (µg/day) | 3772.8 | 1511.3 | 1743.3 | 2694.4 | 3540.9 | 4529.1 | 6617.4 | 3485.1 | 1526.3 | 1481.8 | 2410.8 | 3229.6 | 4268.2 | 6087.7 | ||
| Total folate (µg/day) | 341.8 | 76.9 | 227.8 | 284.7 | 339 | 389.6 | 483.9 | 330 | 289.4 | 80.5 | 180.4 | 229.5 | 283.2 | 337.1 | 419.5 | 330 (i) |
| Dietary folate equivalent (µg/day) (o) | 344.3 | 78.5 | 227.9 | 287.1 | 340.4 | 392.1 | 491.8 | 292.3 | 82.4 | 180.9 | 230.8 | 285.2 | 339.5 | 424.7 | ||
| Vitamin B12 (µg/day) | 6.2 | 2.8 | 3.1 | 4.7 | 5.5 | 7.1 | 10.7 | 4 (l) | 4.6 | 1.2 | 2.9 | 3.8 | 4.5 | 5.3 | 6.7 | 4 (l) |
| Vitamin C (mg/day) | 129.3 | 50.8 | 63.2 | 92.8 | 121.2 | 153.8 | 225.9 | 105 | 120.4 | 50.5 | 52.4 | 81 | 113.8 | 150.2 | 213.8 | 85 |
| Vitamin D (µg/day) | 3.2 | 0.3 | 2.8 | 3 | 3.2 | 3.4 | 3.7 | 15 | 2.5 | 1 | 1.3 | 1.8 | 2.4 | 3 | 4.5 | 15 |
| Vitamin E (mg/day) | 14.5 | 3.9 | 8.8 | 11.7 | 14.3 | 16.8 | 21.5 | 13 (l) | 12.4 | 3.1 | 7.6 | 10.2 | 12.3 | 14.5 | 17.7 | 12 (l) |
| Minerals | ||||||||||||||||
| Calcium (mg/day) | 827.3 | 213.7 | 500.5 | 685.5 | 811 | 966.6 | 1205.5 | 950 | 731.4 | 218.6 | 413.8 | 574.5 | 706 | 871.1 | 1116.5 | 950 (m) |
| Iron (mg/day) | 13.2 | 2.5 | 9.5 | 11.4 | 13.2 | 14.7 | 17.6 | 10 | 10.4 | 2.2 | 7.1 | 8.8 | 10.3 | 11.8 | 14.2 | 18 (n) |
| Magnesium (mg/day) | 383.2 | 98 | 246.7 | 314.2 | 369.5 | 431.5 | 567.6 | 350 (l) | 299.6 | 74.6 | 193 | 245.1 | 292.4 | 344 | 431.7 | 350 (l) |
| Potassium (mg/day) | 3462.2 | 721.5 | 2291.7 | 2990.6 | 3404.5 | 3871.4 | 4755.5 | 4500 (h) | 2913.8 | 567.9 | 2007.8 | 2521.5 | 2864.7 | 3293.5 | 3953.9 | 4500 (h) |
| Zinc (mg/day) | 12.6 | 2.8 | 8.6 | 10.7 | 12.3 | 14.2 | 17.8 | 12 | 9.7 | 1.6 | 7.3 | 8.5 | 9.5 | 10.7 | 12.6 | 9 |
| Males (n = 65) | Females (n = 91) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | Mean | SD (d) | P5 | P25 | P50 | P75 | P95 | DRVs (e) | |
| Energy (kcal/day) | 2188.6 | 533.9 | 1578.9 | 1787.8 | 2100.3 | 2458.8 | 3184.1 | 2160 (f) | 1659 | 348.1 | 1094.5 | 1399.1 | 1586.6 | 1926.9 | 2222.4 | 1890 (f) |
| Energy (MJ/day) | 9.16 | 2.23 | 6.61 | 7.48 | 8.79 | 10.29 | 13.32 | 9.04 | 6.94 | 1.46 | 4.58 | 5.85 | 6.64 | 8.06 | 9.30 | 7.91 |
| Protein (g/day) | 87.3 | 22.3 | 58.7 | 71.4 | 85 | 96.3 | 118.9 | 77 (g) | 67.2 | 14.2 | 46.5 | 57 | 66.5 | 77.2 | 89.9 | 66 (g) |
| Protein (g/kg bw) | 1.1 | 0.3 | 0.6 | 0.8 | 1.1 | 1.3 | 1.8 | 1.1 (g) | 1 | 0.3 | 0.7 | 0.8 | 1 | 1.1 | 1.5 | 1.1 (g) |
| Animal protein (g/day) | 55.0 | 16.4 | 31.4 | 42.7 | 52.1 | 65.1 | 82.7 | 41.8 | 11.4 | 25.8 | 33.2 | 41.5 | 49.4 | 62.3 | ||
| Animal protein (% on total) | 61.6 | 7.7 | 48.1 | 57.8 | 62.8 | 66.4 | 72.6 | 61.4 | 6.6 | 50.2 | 57.1 | 61.8 | 66.1 | 71.1 | ||
| Fat (g/day) | 87.9 | 23.2 | 57.9 | 72.2 | 80.5 | 98.7 | 133.4 | 68.4 | 15.4 | 46.8 | 58.3 | 66.8 | 79.2 | 96.4 | ||
| SFAs (a) (g/day) | 25.5 | 7.2 | 15.5 | 20.8 | 24.4 | 29.5 | 37.8 | 21.4 | 6.2 | 13.5 | 16.4 | 21.2 | 25.8 | 31.5 | ||
| MUFAs (b) (g/day) | 42.9 | 11.7 | 24.8 | 34.8 | 41.7 | 51.3 | 60.6 | 32.4 | 7.1 | 22.1 | 28 | 32 | 36.7 | 46 | ||
| PUFAs (c) (g/day) | 12.2 | 4.4 | 7.4 | 9.1 | 11.8 | 13.7 | 19.9 | 9.1 | 2.8 | 5.8 | 7.2 | 8.5 | 10.6 | 15.1 | ||
| Cholesterol (mg/day) | 296.6 | 88.1 | 183 | 227.8 | 292.1 | 357.1 | 447.9 | 220.4 | 46.6 | 156.8 | 184.6 | 215.8 | 253 | 300.8 | ||
| Carbohydrates (g/day) | 240.3 | 62.5 | 156.3 | 194.1 | 233 | 277.8 | 368.1 | 194.3 | 44.6 | 121.4 | 163.1 | 194.7 | 226.2 | 275.1 | ||
| Starch (g/day) | 141.2 | 43.4 | 75.9 | 111.2 | 135.4 | 168 | 221.8 | 105.9 | 31.1 | 61.1 | 82.2 | 103.2 | 129.7 | 168.4 | ||
| Total sugars (g/day) | 84.9 | 24.1 | 47.2 | 68.4 | 86.8 | 100.4 | 123.6 | 76.7 | 15.6 | 52.9 | 67.4 | 75.3 | 85.5 | 99.8 | ||
| Dietary fibre (g/day) | 23.5 | 7 | 13.2 | 18.6 | 23.1 | 26.2 | 37.6 | 25 (g) | 20.1 | 4.9 | 12.6 | 16.2 | 19.8 | 23.9 | 27.5 | 25 (g) |
| Dietary fibre (g/1000 kcal/day) | 11.2 | 2.1 | 7.6 | 9.9 | 11 | 12.2 | 15.4 | 12.6–16.7 (h) | 12.6 | 2.8 | 8.4 | 10.4 | 12.4 | 14.4 | 17.6 | 12.6–16.7 (h) |
| % Total energy from | ||||||||||||||||
| Protein (% En) | 16 | 2 | 13 | 15 | 16 | 17 | 19 | 15 | 16 | 2 | 14 | 15 | 16 | 18 | 20 | 15 |
| Fat (% En) | 36 | 4 | 29 | 33 | 35 | 39 | 42 | 20–30 (i) | 37 | 4 | 31 | 34 | 37 | 39 | 45 | 20–30 (i) |
| SFAs (a) (% En) | 10 | 2 | 7 | 10 | 11 | 12 | 13 | <10 (g) | 11 | 2 | 9 | 10 | 11 | 13 | 15 | <10 (g) |
| MUFAs (b) (% En) | 18 | 2 | 14 | 16 | 18 | 19 | 22 | 18 | 3 | 14 | 16 | 18 | 20 | 23 | ||
| PUFAs (c) (% En) | 5 | 1 | 4 | 4 | 5 | 5 | 6 | 5–10 (i) | 5 | 1 | 3 | 4 | 5 | 5 | 7 | 5–10 (i) |
| Carbohydrates (% En) | 42 | 5 | 34 | 38 | 42 | 45 | 49 | 45–60 (i) | 44 | 5 | 37 | 41 | 45 | 47 | 51 | 45–60 (i) |
| Total sugars (% En) | 16 | 4 | 11 | 13 | 16 | 19 | 22 | <15 (g) | 19 | 2 | 16 | 18 | 19 | 20 | 22 | <15 (g) |
| Vitamins | ||||||||||||||||
| Vitamin A (REs µg/day) | 1165.5 | 325.3 | 609.1 | 1019.5 | 1157.2 | 1347.2 | 1512.3 | 750 | 920.1 | 234.3 | 540.3 | 787.3 | 918.4 | 1046.9 | 1247.5 | 650 |
| β-carotene (µg/day) | 4334 | 1317.6 | 2314.1 | 3331.3 | 4460.8 | 5352.7 | 6618 | 4038.1 | 586.2 | 2949.7 | 3653 | 4044.3 | 4417.1 | 4945.1 | ||
| Total folate (µg/day) | 335.4 | 95.7 | 199 | 261.6 | 325.5 | 389.5 | 509.6 | 330 | 299.8 | 75.3 | 177.4 | 250.9 | 289.1 | 353.5 | 417 | 330 |
| Dietary folate equivalent (µg/day) (m) | 335.5 | 95.9 | 198.9 | 261.5 | 325.5 | 389.5 | 509.7 | 301.7 | 76.4 | 177.4 | 251.4 | 289.9 | 354 | 417.9 | ||
| Vitamin B12 (µg/day) | 7.2 | 1.8 | 5 | 6.1 | 7 | 8 | 10.4 | 4 (h) | 4.3 | 1.5 | 2.2 | 3.3 | 4.2 | 4.8 | 7 | 4 (h) |
| Vitamin C (mg/day) | 163.8 | 85.4 | 59.6 | 96.1 | 157.2 | 211.1 | 292.4 | 105 | 138.4 | 54.1 | 74.7 | 93.3 | 129.6 | 174.2 | 246.4 | 85 |
| Vitamin D (µg/day) | 2.6 | 0.1 | 2.3 | 2.5 | 2.6 | 2.6 | 2.7 | 15 | 2 | 0.6 | 1.1 | 1.7 | 2.1 | 2.3 | 2.9 | 15 |
| Vitamin E (mg/day) | 15.1 | 4.2 | 8.7 | 12.5 | 14.8 | 18 | 21.8 | 13 (h) | 11.8 | 2.2 | 8.2 | 10.3 | 11.9 | 13.1 | 15.5 | 12 (h) |
| Minerals | ||||||||||||||||
| Calcium (mg/day) | 818 | 238.6 | 511.9 | 649.3 | 805.2 | 916.1 | 1332.6 | 1100 | 778.2 | 174.6 | 467.5 | 664.4 | 809.5 | 885.7 | 1062.1 | 1100 (l) |
| Iron (mg/day) | 14.3 | 3.2 | 9.8 | 12.4 | 13.8 | 16 | 19.8 | 10 | 10.4 | 2 | 7 | 9 | 10.6 | 11.9 | 13.6 | 10 |
| Magnesium (mg/day) | 365.4 | 112.2 | 224.1 | 285.6 | 346.7 | 428.8 | 557.4 | 350 (h) | 291.4 | 61.8 | 199.6 | 243.4 | 285.9 | 337.2 | 397 | 350 (h) |
| Potassium (mg/day) | 3616.9 | 890.1 | 2235.5 | 3047.1 | 3547.6 | 4055.5 | 5140.8 | 3900 (g) | 3011.3 | 420.8 | 2299.4 | 2755.4 | 3007.8 | 3245.9 | 3820.6 | 3900 (g) |
| Zinc (mg/day) | 12.3 | 2.5 | 8.6 | 10.4 | 11.9 | 14.2 | 16.9 | 12 | 9.4 | 1.2 | 7.3 | 8.5 | 9.4 | 10.3 | 11.3 | 9 |
| Food Groups | Energy | Protein | Animal Protein | Plant Protein | Fat | SFAs (a) | MUFAs (b) | PUFAs (c) | Cholesterol | Carbohydrates | Total Sugars | Dietary Fibre |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | % | % | % | % | % | |
| Cereals, cereal products and substitutes | 38.8 | 25.9 | 2.8 | 69.8 | 18.6 | 19.4 | 14.5 | 25.1 | 22.1 | 62.5 | 22.7 | 42.3 |
| Pulses | 0.8 | 1.6 | 0.0 | 4.6 | 0.2 | 0.1 | 0.1 | 0.5 | 0.0 | 1.1 | 0.4 | 5.0 |
| Vegetables, fresh and processed | 1.9 | 3.4 | 0.0 | 9.9 | 0.7 | 0.4 | 0.2 | 2.2 | 0.0 | 2.4 | 5.8 | 19.1 |
| Potatoes, tubers, and their products | 2.2 | 1.2 | 0.0 | 3.5 | 1.2 | 1.0 | 0.5 | 4.0 | 0.0 | 3.5 | 0.2 | 4.3 |
| Fruit, fresh and processed | 5.8 | 2.5 | 0.0 | 7.3 | 3.3 | 1.2 | 3.1 | 8.0 | 0.0 | 9.3 | 21.8 | 23.8 |
| Meat, meat products, and substitutes | 10.0 | 30.9 | 47.0 | 0.3 | 13.0 | 14.8 | 11.4 | 14.0 | 28.1 | 0.3 | 0.4 | 0.3 |
| Fish, seafood, and their products | 2.3 | 8.6 | 13.1 | 0.1 | 2.0 | 1.3 | 1.3 | 4.5 | 8.1 | 0.3 | 0.3 | 0.0 |
| Milk, milk products, and substitutes | 14.9 | 21.2 | 32.0 | 0.6 | 21.1 | 35.4 | 13 | 8.1 | 18.1 | 7.9 | 18.6 | 1.8 |
| Oils and fats | 12.9 | 0.1 | 0.1 | 0.0 | 33.7 | 18.4 | 51.1 | 28.4 | 1.6 | 0.0 | 0.1 | 0.0 |
| Eggs | 1.2 | 2.5 | 3.8 | 0.0 | 2.0 | 2.0 | 1.7 | 2.0 | 20.1 | 0.0 | 0.0 | 0.0 |
| Sweet products and substitutes | 4.7 | 1.2 | 1.0 | 1.5 | 3.7 | 5.6 | 2.8 | 2.1 | 1.7 | 7.2 | 16.6 | 2.2 |
| Water and other non-alcoholic beverages | 2.3 | 0.7 | 0.1 | 2.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.0 | 4.8 | 11.5 | 0.9 |
| Alcoholic beverages and substitutes | 2.0 | 0.1 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 1.6 | 0.0 |
| Meal substitutes | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0 | 0.1 |
| Miscellaneous | 0.2 | 0.1 | 0.0 | 0.3 | 0.4 | 0.3 | 0.3 | 0.9 | 0.1 | 0.1 | 0.1 | 0.1 |
| Food Groups | Ca | Fe | Mg | K | Zn | Vit A Eq | β-Carotene | Folate Eq | Vit B12 | Vit C | Vit D | Vit E |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | |||||||||||
| Cereals, cereal products, and substitutes | 11.4 | 34.2 | 25.7 | 14.1 | 22.0 | 6.4 | 1.7 | 28.5 | 5.2 | 2.3 | 13.5 | 12.6 |
| Pulses | 0.6 | 3.6 | 3.2 | 2.0 | 1.3 | 0.3 | 0.5 | 5.4 | 0.0 | 1.3 | 0.0 | 0.3 |
| Vegetables, fresh and processed | 7.1 | 11.9 | 9.7 | 16.1 | 8.6 | 43.4 | 69.7 | 24.6 | 0.1 | 37.6 | 0.8 | 11.4 |
| Potatoes, tubers, and their products | 0.5 | 2.3 | 3.9 | 8.3 | 4.5 | 0.1 | 0.2 | 5.1 | 0.0 | 5.2 | 0.0 | 1.1 |
| Fruit, fresh and processed | 4.3 | 8.3 | 9.8 | 16.1 | 3.5 | 11.9 | 19.1 | 9.7 | 0.5 | 31.7 | 0.1 | 10.1 |
| Meat, meat products, and substitutes | 1.6 | 14.9 | 9.0 | 12.8 | 24.3 | 6.4 | 0.7 | 4.6 | 31.7 | 0.3 | 17.1 | 1.6 |
| Fish, seafood, and their products | 1.9 | 5.1 | 3.5 | 4.0 | 5.4 | 1.2 | 0.0 | 1.1 | 27.6 | 0.2 | 32.3 | 3.8 |
| Milk, milk products, and substitutes | 54.0 | 6.9 | 12.2 | 13.1 | 23.3 | 20.0 | 2.2 | 12.7 | 29.0 | 7.4 | 25.4 | 7.1 |
| Oils and Fats | 0.2 | 0.4 | 0.0 | 0.0 | 0.1 | 1.5 | 0.3 | 0.0 | 0.1 | 0.0 | 0.7 | 46.2 |
| Eggs | 0.9 | 2.1 | 0.7 | 0.7 | 1.7 | 3.7 | 0.4 | 2.7 | 3.9 | 0.0 | 8.8 | 1.9 |
| Sweet products and substitutes | 2.6 | 3.4 | 2.6 | 2.1 | 1.6 | 1.8 | 0.3 | 0.7 | 1.1 | 0.7 | 0.9 | 0.7 |
| Water and other non-alcoholic beverages | 14.3 | 3.5 | 16.8 | 9.0 | 3.2 | 2.9 | 4.6 | 3.8 | 0.4 | 13.1 | 0.3 | 1.8 |
| Alcoholic beverages and substitutes | 0.3 | 3.0 | 2.3 | 1.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.1 | 0.2 | 0.0 | 0.0 |
| Meal substitutes | 0.1 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 |
| Miscellaneous | 0.2 | 0.2 | 0.2 | 0.7 | 0.2 | 0.2 | 0.2 | 0.4 | 0.1 | 0.0 | 0.0 | 1.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Le Donne, C.; Ferrari, M.; Mistura, L.; D’Addezio, L.; Comendador Azcarraga, F.J.; Martone, D.; Piccinelli, R.; Sette, S.; Catasta, G.; Turrini, A., on behalf of IV SCAI field work team. The National Food Consumption Survey IV SCAI: Nutrient Intakes and Related Dietary Sources in Italy. Nutrients 2026, 18, 88. https://doi.org/10.3390/nu18010088
Le Donne C, Ferrari M, Mistura L, D’Addezio L, Comendador Azcarraga FJ, Martone D, Piccinelli R, Sette S, Catasta G, Turrini A on behalf of IV SCAI field work team. The National Food Consumption Survey IV SCAI: Nutrient Intakes and Related Dietary Sources in Italy. Nutrients. 2026; 18(1):88. https://doi.org/10.3390/nu18010088
Chicago/Turabian StyleLe Donne, Cinzia, Marika Ferrari, Lorenza Mistura, Laura D’Addezio, Francisco Javier Comendador Azcarraga, Deborah Martone, Raffaela Piccinelli, Stefania Sette, Giovina Catasta, and Aida Turrini on behalf of IV SCAI field work team. 2026. "The National Food Consumption Survey IV SCAI: Nutrient Intakes and Related Dietary Sources in Italy" Nutrients 18, no. 1: 88. https://doi.org/10.3390/nu18010088
APA StyleLe Donne, C., Ferrari, M., Mistura, L., D’Addezio, L., Comendador Azcarraga, F. J., Martone, D., Piccinelli, R., Sette, S., Catasta, G., & Turrini, A., on behalf of IV SCAI field work team. (2026). The National Food Consumption Survey IV SCAI: Nutrient Intakes and Related Dietary Sources in Italy. Nutrients, 18(1), 88. https://doi.org/10.3390/nu18010088













