Relationship Between Dietary Inflammatory Index, Diets, and Cardiovascular Medication
Abstract
:1. Introduction
2. Materials and Methods
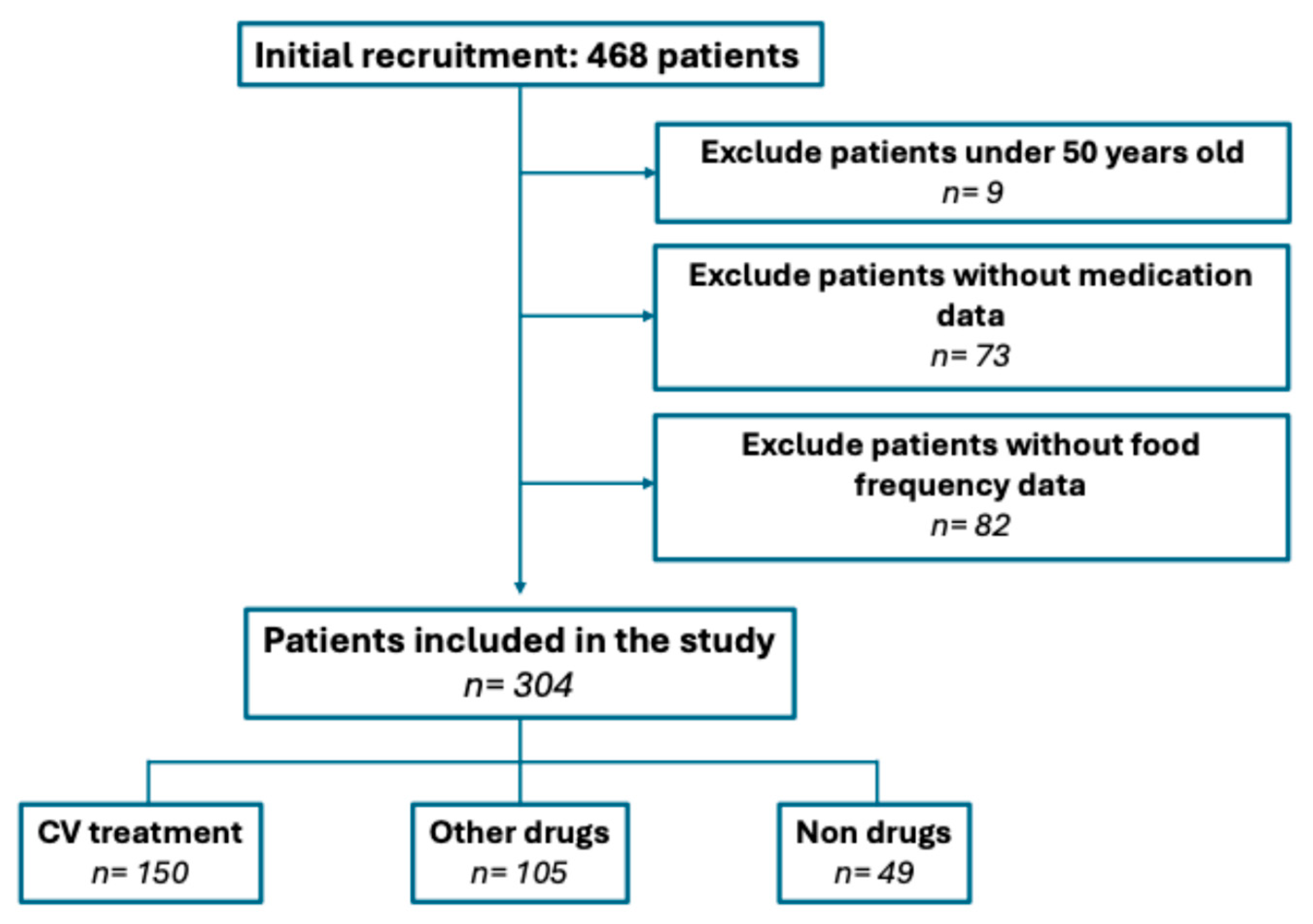
2.1. Study Design
2.2. Participants and Data Collection
2.3. Statistical Inference
2.4. Ethical Approval and Data Protection
3. Results
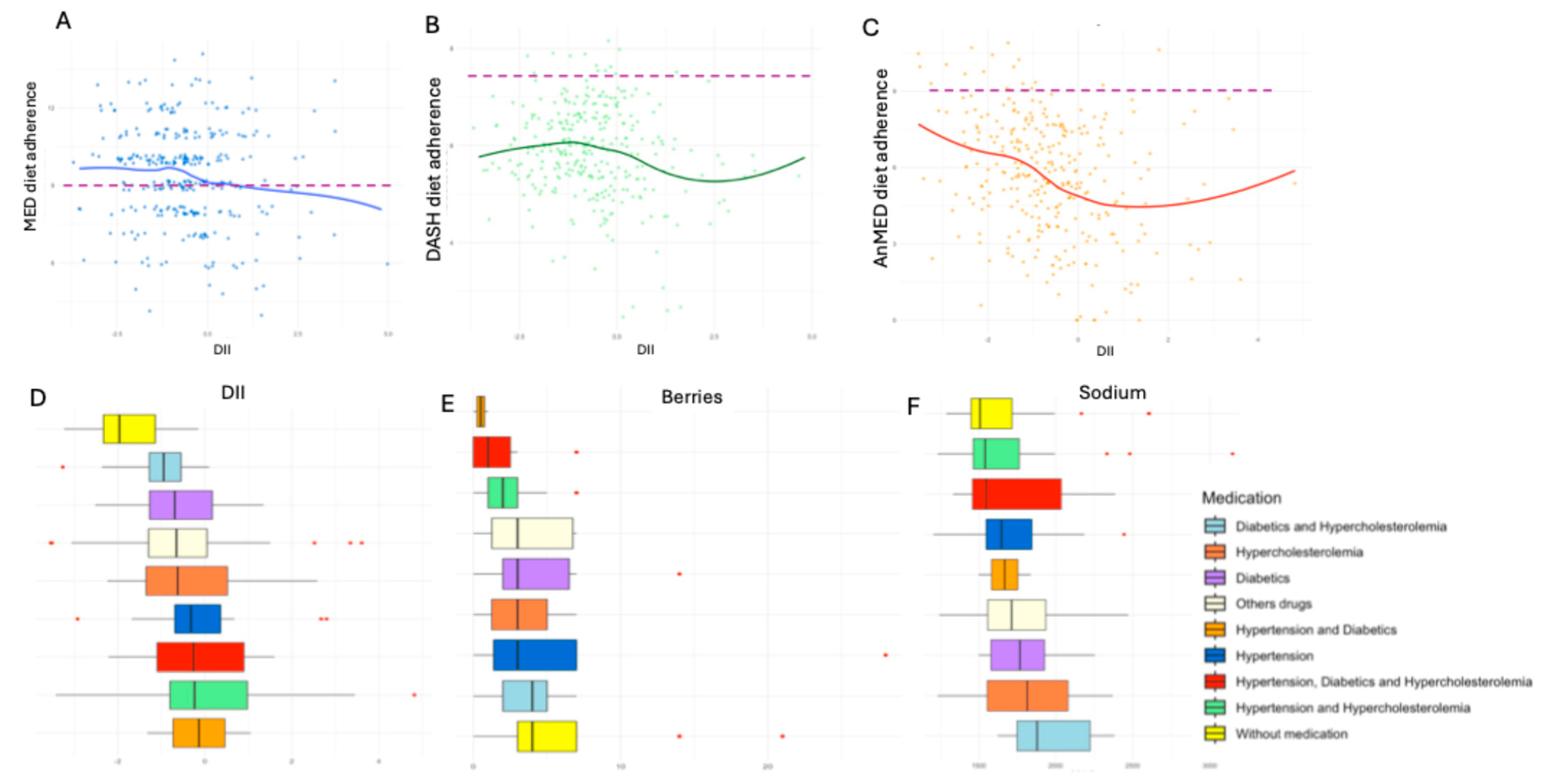
3.1. Medication Consumption, Diets, and DII
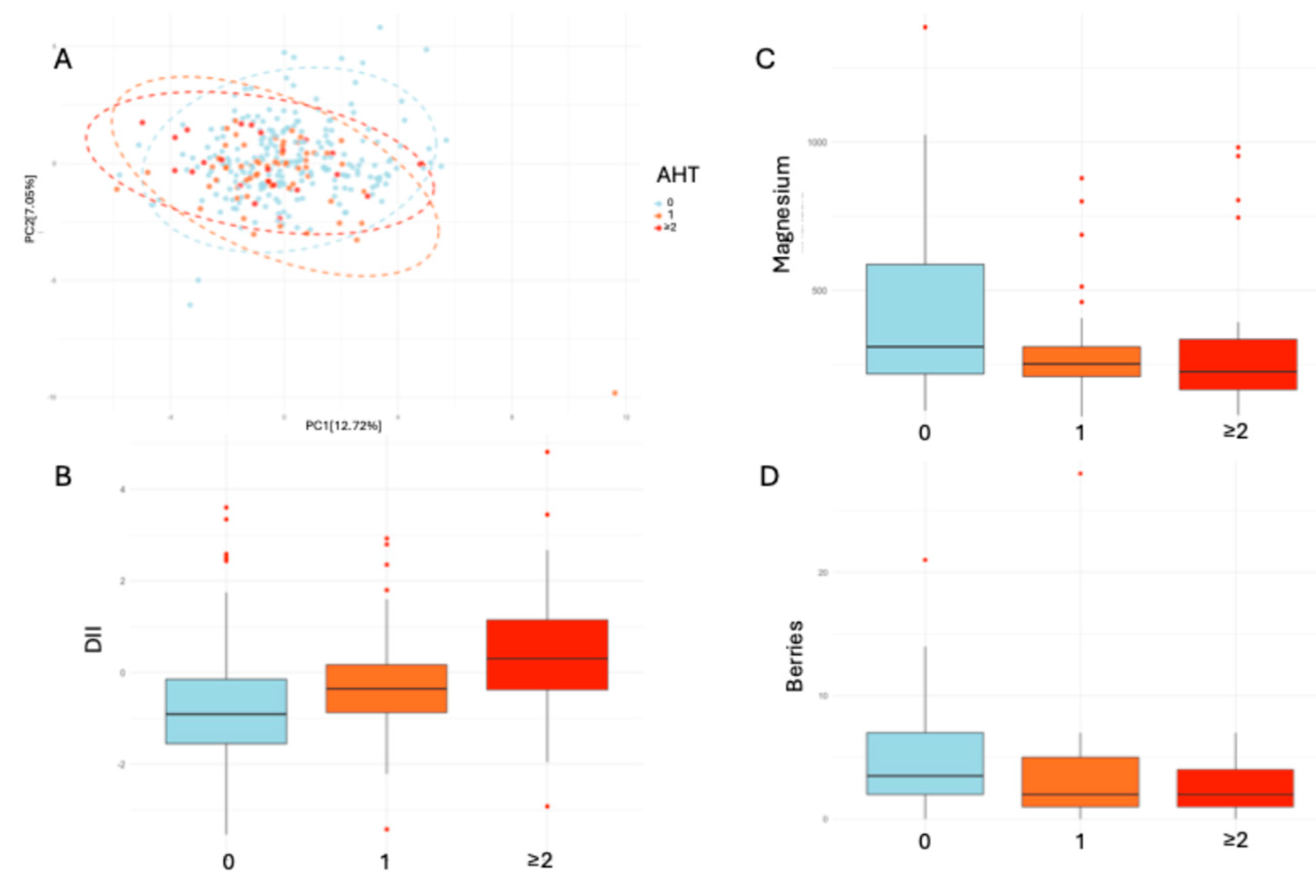
3.2. Antihypertensive Use and Dietary Intake
3.3. Predicting Antihypertensive Use with DII
3.4. DII Categorization and Micronutrient Intake
3.5. Dietary Micronutrient Intake and Modeled Diets
- MED adherence showed no significant association with micronutrient intake.
- DASH adherence was significantly related to increased sodium (p-value: 0.006) and potassium intake (p-value: 0.031).
- AnMED adherence showed a significant relationship with all micronutrients analyzed in a linear model: calcium and magnesium (p-value < 0.001), followed by sodium (p-value: 0.002) and potassium (p-value: 0.039).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADM | Antidiabetic medication |
| AHT | Antihypertensive treatment |
| AnMED | Anti-inflammatory diet |
| ARBs | Angiotensin receptor blockers |
| CRP | C-reactive protein |
| CV | Cardiovascular |
| DASH | Dietary Approaches to Stop Hypertension |
| DII | Dietary Inflammatory Index |
| DM | Diabetes mellitus |
| EVOO | Extra virgin olive oil |
| FFQ | Food Frequency Questionnaire |
| HT | Hypertension |
| IL-6 | Interleukin-6 |
| LLT | Lipid-lowering therapy |
| MED | Mediterranean diet |
| MUFA | Monounsaturated fatty acid |
| PCA | Principal Component Analysis |
| PUFA | Polyunsaturated fatty acid |
| SFA | Saturated fatty acid |
| TNF-α | Tumor necrosis factor-alpha |
References
- De Pergola, G.; D’Alessandro, A. Influence of Mediterranean Diet on Blood Pressure. Nutrients 2018, 10, 1700. [Google Scholar] [CrossRef] [PubMed]
- The WHO, in Its Inaugural Report on Hypertension, Outlines the Severe Impact of the Condition and Strategies for Its Effective Management. Who.int. Available online: https://www.who.int/es/news/item/19-09-2023-first-who-report-details-devastating-impact-of-hypertension-and-ways-to-stop-it (accessed on 1 April 2025).
- Navaneethabalakrishnan, S.; Smith, H.L.; Arenaz, C.M.; Goodlett, B.L.; McDermott, J.G.; Mitchell, B.M. Update on Immune Mechanisms in Hypertension. Am. J. Hypertens. 2022, 35, 842–851. [Google Scholar] [CrossRef] [PubMed]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. Available online: https://www.nature.com/articles/s41586-021-03392-8 (accessed on 1 April 2025). [CrossRef] [PubMed]
- Erickson, S.R.; Bostwick, J.R.; Guthrie, S.K. Psychological symptoms associated with cardiovascular drugs; cardiac symptoms from psychiatric drugs; drug interactions. In Psychiatry and Heart Disease: The Mind, Brain, and Heart; Wiley: Honoken, NJ, USA, 2012; pp. 194–210. [Google Scholar] [CrossRef]
- Kelly, M.A. Neurological complications of cardiovascular drugs. Handb. Clin. Neurol. 2021, 177, 319–344. [Google Scholar] [CrossRef]
- Sato, R.; Koziolek, M.J.; von Haehling, S. Translating evidence into practice: Managing electrolyte imbalances and iron deficiency in heart failure. Eur. J. Intern. Med. 2025, 131, 15–26. [Google Scholar] [CrossRef]
- Tse, Y.-H.; Tuet, C.-Y.; Lau, K.-K.; Tse, H.-F. Dietary modification for prevention and control of high blood pressure. Postgrad. Med. J. 2023, 99, 1058–1067. [Google Scholar] [CrossRef]
- He, F.J.; Campbell, N.R.C.; Woodward, M.; A MacGregor, G. Salt reduction to prevent hypertension: The reasons of the controversy. Eur. Heart J. 2021, 42, 2501–2505. [Google Scholar] [CrossRef]
- Chen, H.; Leng, X.; Liu, S.; Zeng, Z.; Huang, F.; Huang, R.; Zou, Y.; Xu, Y. Association between dietary intake of omega-3 polyunsaturated fatty acids and all-cause and cardiovascular mortality among hypertensive adults: Results from NHANES 1999–2018. Clin. Nutr. 2023, 42, 2434–2442. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Badimon, L.; Estruch, R. Latest Evidence of the Effects of the Mediterranean Diet in Prevention of Cardiovascular Disease. Curr. Atheroscler. Rep. 2014, 16, 446. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Sánchez-Tainta, A. The Prevention of Cardiovascular Disease Through the Mediterranean Diet; Academic Press: San Diego, CA, USA, 2017. [Google Scholar]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Akhlaghi, M. Dietary Approaches to Stop Hypertension (DASH): Potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 2020, 33, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2014, 113, 1–15. [Google Scholar] [CrossRef]
- Sala-Climent, M.; de Coca, T.L.; Guerrero, M.D.; Muñoz, F.J.; López-Ruíz, M.A.; Moreno, L.; Alacreu, M.; Dea-Ayuela, M.A. The effect of an anti-inflammatory diet on chronic pain: A pilot study. Front. Nutr. 2023, 10, 1205526. [Google Scholar] [CrossRef]
- Tada, N. [Dietary therapy for prevention and treatment of atherosclerosis from the perspective of anti-inflammation. Nihon Rinsho 2011, 69, 110–118. [Google Scholar] [PubMed]
- Esposito, K.; Giugliano, D. Diet and inflammation: A link to metabolic and cardiovascular diseases. Eur. Heart J. 2006, 27, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Baudet, M.; Daugareil, C.; Ferrieres, J. Prévention des maladies cardiovasculaires et règles hygiéno-diététiques. Ann. Cardiol. d’Angéiol. 2012, 61, 93–98. [Google Scholar] [CrossRef]
- Calder, P.C. Dietary modification of inflammation with lipids. Proc. Nutr. Soc. 2002, 61, 345–358. [Google Scholar] [CrossRef]
- Montefusco, L.; D’addio, F.; Loretelli, C.; Ben Nasr, M.; Garziano, M.; Rossi, A.; Pastore, I.; Plebani, L.; Lunati, M.E.; Bolla, A.M.; et al. Anti-inflammatory effects of diet and caloric restriction in metabolic syndrome. J. Endocrinol. Investig. 2021, 44, 2407–2415. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef]
- Ji, M.; Hong, X.; Chen, M.; Chen, T.; Wang, J.; Zhang, N. Dietary inflammatory index and cardiovascular risk and mortality: A meta-analysis of cohort studies. Medicine 2020, 99, e20303. [Google Scholar] [CrossRef]
- Rahimlou, M.; Ahmadi, A.R.; Cheraghian, B.; Baghdadi, G.; Ghalishourani, S.S.; Nozarian, S.; Hashemi, S.J.; Rahimi, Z.; Jahromi, N.B.; Hosseini, S.A. The association between dietary inflammatory index with some cardio-metabolic risk indices among the patients with type 2 diabetes from Hoveyzeh cohort study: A cross-sectional study. BMC Endocr. Disord. 2024, 24, 91. [Google Scholar] [CrossRef] [PubMed]
- Wirth, M.D.; Hébert, J.R.; Shivappa, N.; Hand, G.A.; Hurley, T.G.; Drenowatz, C.; McMahon, D.; Shook, R.P.; Blair, S.N. Anti-inflammatory Dietary Inflammatory Index scores are associated with healthier scores on other dietary indices. Nutr. Res. 2016, 36, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Camargo-Ramos, C.M.; Correa-Bautista, J.E.; Correa-Rodríguez, M.; Ramírez-Vélez, R. Dietary Inflammatory Index and Cardiometabolic Risk Parameters in Overweight and Sedentary Subjects. Int. J. Environ. Res. Public Health 2017, 14, 1104. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Shivappa, N.; Hébert, J.R.; Huang, H.; Cai, L.; Liang, J.; Lin, W.; Zong, L.; Wang, N.; Li, L.; et al. Dietary inflammatory index and cardiorenal function in women with diabetes and prediabetes. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2319–2327. [Google Scholar] [CrossRef]
- Souci, S.; Fachmann, W.; Kraut, H. Food Composition and Nutrition Tables, 9th ed; MedPharm: Berlin, Germany, 2024; ISBN 9783804750937. [Google Scholar]
- Ferreira-Pêgo, C.; Nissensohn, M.; Kavouras, S.A.; Babio, N.; Serra-Majem, L.; Águila, A.M.; Mauromoustakos, A.; Pérez, J.Á.; Salas-Salvadó, J. Relative Validity and Repeatability in a Spanish Population with Metabolic Syndrome from the PREDIMED-PLUS Study. Nutrients 2016, 8, 475. [Google Scholar] [CrossRef]
- Nejati-Namin, S.; Ataie-Jafari, A.; Amirkalali, B.; Hosseini, S.; Fathollahi, M.S.; Najafi, M. Adherence to the Dietary Approaches to Stop Hypertension eating plan in candidates awaiting coronary artery bypass graft surgery, Tehran, Iran: Adherence to DASH diet in cardiovascular patients. Nutr. Diet. 2013, 70, 27–34. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; Guallar-Castillón, P.; Graciani, A.; López-García, E.; Mesas, A.E.; Aguilera, M.T.; Banegas, J.R.; Rodríguez-Artalejo, F. Adherence to the Mediterranean Diet Pattern Has Declined in Spanish Adults3. J. Nutr. 2012, 142, 1843–1850. [Google Scholar] [CrossRef]
- Hébert, J.R.; Shivappa, N.; Wirth, M.D.; Hussey, J.R.; Hurley, T.G. Perspective: The Dietary Inflammatory Index (DII)—Lessons Learned, Improvements Made, and Future Directions. Adv. Nutr. Int. Rev. J. 2019, 10, 185–195. [Google Scholar] [CrossRef]
- Shivappa, N.; Godos, J.; Hébert, J.R.; Wirth, M.D.; Piuri, G.; Speciani, A.F.; Grosso, G. Dietary Inflammatory Index and Cardiovascular Risk and Mortality—A Meta-Analysis. Nutrients 2018, 10, 200. [Google Scholar] [CrossRef]
- Jeong, J.; Shin, S. A higher dietary inflammatory index score is associated with an increased risk of developing dyslipidemia and its components only in women. Nutr. Res. 2024, 130, 67–80. [Google Scholar] [CrossRef]
- Behbahani, H.B.; Bazyar, H.; Aghamohammadi, V.; Ahangarpour, A.; Shivappa, N.; Hebert, J.R.; Alipour, M.; Nasab, M.S.; Moradi, F.; Bar, H.H. The Dietary Inflammatory Index is positively associated with cardiometabolic risk parameters in atherosclerosis patients. Nutr. Res. 2022, 107, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.M.; Shivappa, N.; Hébert, J.R.; Perry, I.J. Dietary Inflammatory Index and Biomarkers of Lipoprotein Metabolism, Inflammation and Glucose Homeostasis in Adults. Nutrients 2018, 10, 1033. [Google Scholar] [CrossRef]
- Sugiyama, T.; Tsugawa, Y.; Tseng, C.-H.; Kobayashi, Y.; Shapiro, M.F. Different Time Trends of Caloric and Fat Intake Between Statin Users and Nonusers Among US Adults: Gluttony in the Time of Statins? JAMA Intern. Med. 2014, 174, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Yang, K.; Cheng, C.; Hu, Q.; Zhao, F.; Lu, S.; Long, J.; Yang, H.; Chen, S. Higher dietary inflammatory index linked to increased risk of hypertension: A systematic review and dose-response meta-analysis. Eur. J. Clin. Nutr. 2024, 1–8. [Google Scholar] [CrossRef]
- Li, J.; Lee, D.H.; Hu, J.; Tabung, F.K.; Li, Y.; Bhupathiraju, S.N.; Rimm, E.B.; Rexrode, K.M.; Manson, J.E.; Willett, W.C.; et al. Dietary Inflammatory Potential and Risk of Cardiovascular Disease Among Men and Women in the U.S. J. Am. Coll. Cardiol. 2020, 76, 2181–2193. [Google Scholar] [CrossRef]
- Tessier, A.-J.; Wang, F.; Korat, A.A.; Eliassen, A.H.; Chavarro, J.; Grodstein, F.; Li, J.; Liang, L.; Willett, W.C.; Sun, Q.; et al. Optimal dietary patterns for healthy aging. Nat. Med. 2025, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Unanua, M.P.; Fernández, M.A.; Simarro, F.L.; Llora, T.S.; Martínez, I.P.; Romero, J.M. Adherencia a un estilo de vida saludable en pacientes con diabetes mellitus tipo 2 en España. Med. de Fam. SEMERGEN 2021, 47, 161–169. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; Guallar-Castillón, P.; Graciani, A.; Rodríguez-Artalejo, F.; Banegas, J.R. Self-Reported Adherence to Nonpharmacological Treatment and Association with Mortality over 6 Years: Population-Based Study in Older Persons with Hypercholesterolemia. J. Am. Geriatr. Soc. 2009, 57, 2287–2292. [Google Scholar] [CrossRef]
- Fao.org. Available online: https://www.fao.org/fileadmin/user_upload/nutrition/docs/requirements/fatsandfattacidsreport.pdf (accessed on 29 April 2025).
- Saraswathi, V.; Kumar, N.; Gopal, T.; Bhatt, S.; Ai, W.; Ma, C.; Talmon, G.A.; Desouza, C. Lauric Acid versus Palmitic Acid: Effects on Adipose Tissue Inflammation, Insulin Resistance, and Non-Alcoholic Fatty Liver Disease in Obesity. Biology 2020, 9, 346. [Google Scholar] [CrossRef]
- Sanders, T. Olive Oil and the Mediterranean Diet. Int. J. Vitam. Nutr. Res. 2001, 71, 179–184. [Google Scholar] [CrossRef]
- Korean Institute for Functional Medicine; Kim, Y.-S. The comprehension and utilization of omega-3 and -6 polyunsaturated fatty acid. Korean Inst. Funct. Med. 2024, 7, 39–45. [Google Scholar] [CrossRef]
- Mensink, R.P. Effects of stearic acid on plasma lipid and lipoproteins in humans. Lipids 2005, 40, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Mensink, R.P.; Temme, E.H.M.; Hornstra, G. Dietary Saturated and Trans Fatty Acids and Lipoprotein Metabolism. Ann. Med. 1994, 26, 461–464. [Google Scholar] [CrossRef]
- Kris-Etherton, P.; Mustad, V.; Derr, J. Effects of dietary stearic acid on plasma lipids and thrombosis. Nutrition Today. 1993, 28, 30–38. Available online: https://journals.lww.com/nutritiontodayonline/abstract/1993/05000/effects_of_dietary_stearic_acid_on_plasma_lipids.6.aspx (accessed on 29 April 2025). [CrossRef]
- Rio-Valle, J.S.; Quintana, F.C.; Gutiérrez, C.V.; Peña, D.P.; Caro, M.G.; Vinuesa, A.M.; Pappous, A. Adherencia terapéutica en hipertensos: Estudio cualitativo. Index de Enfermería 2006, 15, 25–29. [Google Scholar] [CrossRef]
- Rodriguez-Saldana, J. Patient adherence: Challenges, myths, and realities. In The Diabetes Textbook; Springer International Publishing: Cham, Switzerland, 2023; pp. 451–467. [Google Scholar]
- Zhang, L.; Muscat, J.E.; Chinchilli, V.M.; Kris-Etherton, P.M.; Al-Shaar, L.; Richie, J.P. Berry Consumption in Relation to Allostatic Load in US Adults: The National Health and Nutrition Examination Survey, 2003–2010. Nutrients 2024, 16, 403. [Google Scholar] [CrossRef]
- Severino, P.; Netti, L.; Mariani, M.V.; Maraone, A.; D’amato, A.; Scarpati, R.; Infusino, F.; Pucci, M.; Lavalle, C.; Maestrini, V.; et al. Prevention of Cardiovascular Disease: Screening for Magnesium Deficiency. Cardiol. Res. Pr. 2019, 2019, 4874921. [Google Scholar] [CrossRef]
- Appel, L.J. Potassium. In Encyclopedia of Human Nutrition, 4th ed.; Caballero, B., Ed.; Academic Press: Oxford, UK, 2023; pp. 362–367. [Google Scholar]
- McLean, R.M.; Wang, N.X. Potassium. Adv. Food Nutr. Res. 2021, 96, 89–121. [Google Scholar] [CrossRef]
- Pana, T.A.; Dehghani, M.; Baradaran, H.R.; Neal, S.R.; Wood, A.D.; Kwok, C.S.; Loke, Y.K.; Luben, R.N.; Mamas, M.A.; Khaw, K.-T.; et al. Calcium intake, calcium supplementation and cardiovascular disease and mortality in the British population: EPIC-norfolk prospective cohort study and meta-analysis. Eur. J. Epidemiol. 2021, 36, 669–683. [Google Scholar] [CrossRef]
- Chan, Q.; Wren, G.M.; E Lau, C.-H.; Ebbels, T.M.D.; Gibson, R.; Loo, R.L.; Aljuraiban, G.S.; Posma, J.M.; Dyer, A.R.; Steffen, L.M.; et al. Blood pressure interactions with the DASH dietary pattern, sodium, and potassium: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am. J. Clin. Nutr. 2022, 116, 216–229. [Google Scholar] [CrossRef]
- Derkach, A.; Sampson, J.; Joseph, J.; Playdon, M.C.; Stolzenberg-Solomon, R.Z. Effects of dietary sodium on metabolites: The Dietary Approaches to Stop Hypertension (DASH)–Sodium Feeding Study. Am. J. Clin. Nutr. 2017, 106, 1131–1141. [Google Scholar] [CrossRef] [PubMed]
- Ginos, B.N.; Engberink, R.H.O. Estimation of Sodium and Potassium Intake: Current Limitations and Future Perspectives. Nutrients 2020, 12, 3275. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Andrade, F.C. Diagnostic status of hypertension on the adherence to the Dietary Approaches to Stop Hypertension (DASH) diet. Prev. Med. Rep. 2016, 4, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, W.M.; Sacks, F.M.; Ard, J.; Appel, L.J.; Bray, G.A.; Simons-Morton, D.G.; Conlin, P.R.; Svetkey, L.P.; Erlinger, T.P.; Moore, T.J.; et al. Effects of Diet and Sodium Intake on Blood Pressure: Subgroup Analysis of the DASH-Sodium Trial. Ann. Intern. Med. 2001, 135, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Filippou, C.; Tatakis, F.; Polyzos, D.; Manta, E.; Thomopoulos, C.; Nihoyannopoulos, P.; Tousoulis, D.; Tsioufis, K. Overview of salt restriction in the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean diet for blood pressure reduction. Rev. Cardiovasc. Med. 2022, 23, 36. [Google Scholar] [CrossRef]
- E Puddu, P.; Shivappa, N.; Menotti, A.; Hébert, J.R.; Tolonen, H.; Kafatos, A.; Adachi, H. Energy-adjusted Dietary Inflammatory Index scores predict long-term cardiovascular disease mortality and other causes of death in an ecological analysis of the Seven Countries Study. Eur. J. Prev. Cardiol. 2021, 28, 1342–1350. [Google Scholar] [CrossRef]

| MED | DASH | AnMED | |
|---|---|---|---|
| White meat | Preferential consumption over red meat. Non-consumption guidelines. | 2 or less per day. | 3 servings per week. |
| Red meat | Less than 1 per day. | Not recommended. | Not allowed. |
| Legumes | 3 or more servings per week. | 4–5 per week. | 3 or more servings per week. |
| Refined grains | No guidelines. | 7–8 servings per day, of which at least half are whole grains. | Not allowed. |
| Vegetables | 2 or more servings per day. | 4–5 servings per day. | Distinguishes between green vegetables, non-green vegetables, and other vegetables. A quantity of 100 g of each vegetable group daily. |
| Fruits | 3 or more servings per day. | 4–5 servings per day. | Differentiates between enzymatic, antioxidant, and other fruits. One piece of each type per day. |
| Fish | 3 or more times per week. | 2 or less per day. | Distinguishes between blue and white fish. Three or more servings of each type per week. |
| Fats and oils | EVOO primary oil use. Four or more tablespoons per day (60 mL). | 2–3 per day. | 3 EVOO tablespoons per day (approximately 45 mL). |
| Nuts | 3 or more times per week. | 4–5 per week. | 1 serving per day. |
| Dairy products | No guidelines. | 2–3 servings per day of low-fat dairy products. | Cow milk not allowed; cured cheese or goat/sheep cheese and natural yogurt or kefir are preferred. |
| Coffee | No guidelines. | No guidelines. | Maximum of 2 cups per day. |
| Alcohol | 7 glasses of red wine per week. | ≤1 drink for women. ≤2 drinks for men. | Not allowed. |
| Sugar and pastries | Less than 2 servings per week. | 5 or less per week. | Not allowed. |
| Saturated fats products | Less than 7 per week. | Not recommended. | Not allowed. |
| Sweet or carbonated beverages | Less than 1 per day. | Not recommended. | Not allowed. |
| Turmeric | No guidelines. | No guidelines. | 5 g per day. |
| Treated with | n | Mean Age | DII | MED | DASH | AnMED |
|---|---|---|---|---|---|---|
| CV treatments | 150 | 69.37 ± 9.44 | −0.29 ± 1.31 | 70.47 | 5.37 | 7.38 |
| AHT | 37 | 72.70 ± 8.57 | −0.20 ± 1.04 | 77.78 | 0 | 5.56 |
| ADM | 19 | 63.50 ± 9.97 | −0.62 ± 1.08 | 78.95 | 5.26 | 10.53 |
| LLT | 34 | 67.90 ± 9.05 | −0.31 ± 1.39 | 61.76 | 8.82 | 5.88 |
| AHT and ADM | 2 | 71.50 ± 10.6 | −0.14 ± 1.68 | 100 | 0 | 0 |
| AHT and LLT | 34 | 72.20 ± 8.33 | 0.08 ± 1.63 | 61.76 | 5.88 | 2.94 |
| LLT and ADM | 13 | 62.20 ± 8.06 | −1.09 ± 0.92 | 76.92 | 15.39 | 30.77 |
| AHT, ADM, and LLT | 11 | 72.50 ± 8.59 | −0.13 ± 1.24 | 72.73 | 0 | 0 |
| Other drugs | 105 | 65.60 ± 9.32 | −0.56 ± 1.18 | 65.09 | 2.83 | 6.60 |
| Non-drugs consumption | 49 | 57.70 ± 3.19 | −1.77 ± 0.75 | 73.47 | 10.20 | 2.04 |
| CV Treatments | Other Drugs | Non-Drugs | p-Value | p-Adjust | |
|---|---|---|---|---|---|
| Total proteins | 11.9% | 12.2% | 13.1% | 0.778 | 1.000 |
| Total carbohydrates | 30.6% | 32.9% | 35.3% | 0.518 | 1.000 |
| Total fats | 57.6% | 54.9% | 51.6% | 0.003 | 0.004 ** |
| SFA | 17.95 ± 6.70 (g) | 17.39 ± 6.98 (g) | 13.09 ± 3.32 (g) | <0.001 | <0.001 *** |
| PUFA | 12.47 ± 4.53 (g) | 12.05 ± 4.30 (g) | 10.18 ± 2.49 (g) | 0.005 | 0.043 * |
| MUFA | 72.48 ± 34.98 (g) | 66.90 ± 33.57 (g) | 52.32 ± 16.25 (g) | 0.001 | 0.011 * |
| Lauric acid | 0.20 ± 0.17 (g) | 0.21 ± 0.19 (g) | 0.11 ± 0.13 (g) | <0.001 | 0.001 ** |
| Miristic acid | 0.81 ± 0.58 (g) | 0.87 ± 0.62 (g) | 0.54 ± 0.39 (g) | 0.002 | 0.017 * |
| Palmitic acid | 3.74 ± 1.54 (g) | 4.04 ± 1.63 (g) | 3.21 ± 1.01 (g) | 0.010 | 0.091 |
| Stearic acid | 3.66 ± 1.35 (g) | 3.58 ± 1.38 (g) | 2.71 ± 0.66 (g) | <0.001 | <0.001 *** |
| Oleic acid | 65.77 ± 31.59 (g) | 60.84 ± 30.22 (g) | 47.66 ± 14.78 (g) | 0.001 | 0.009 ** |
| DII | Predicted Probability (Fit) | Lower Bound | Upper Bound |
|---|---|---|---|
| −2 | 0.168 | 0.061 | 0.275 |
| −1 | 0.311 | 0.235 | 0.387 |
| 0 | 0.454 | 0.373 | 0.535 |
| 1 | 0.597 | 0.480 | 0.713 |
| 2 | 0.739 4 | 0.575 | 0.904 |
| MED | DASH | AnMED | |
|---|---|---|---|
| Calcium | X | X | V |
| Magnesium | X | X | V |
| Potasium | X | V | V |
| Sodium | X | V | V |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez de Coca, T.; Maya, P.; Villagrasa, V.; Moreno, L. Relationship Between Dietary Inflammatory Index, Diets, and Cardiovascular Medication. Nutrients 2025, 17, 1570. https://doi.org/10.3390/nu17091570
Lopez de Coca T, Maya P, Villagrasa V, Moreno L. Relationship Between Dietary Inflammatory Index, Diets, and Cardiovascular Medication. Nutrients. 2025; 17(9):1570. https://doi.org/10.3390/nu17091570
Chicago/Turabian StyleLopez de Coca, Teresa, Pablo Maya, Victoria Villagrasa, and Lucrecia Moreno. 2025. "Relationship Between Dietary Inflammatory Index, Diets, and Cardiovascular Medication" Nutrients 17, no. 9: 1570. https://doi.org/10.3390/nu17091570
APA StyleLopez de Coca, T., Maya, P., Villagrasa, V., & Moreno, L. (2025). Relationship Between Dietary Inflammatory Index, Diets, and Cardiovascular Medication. Nutrients, 17(9), 1570. https://doi.org/10.3390/nu17091570





