Impact of Phosphate Variability in Patients Undergoing Hemodialysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Population
2.2. Study Variables
2.3. Statistical Analyses
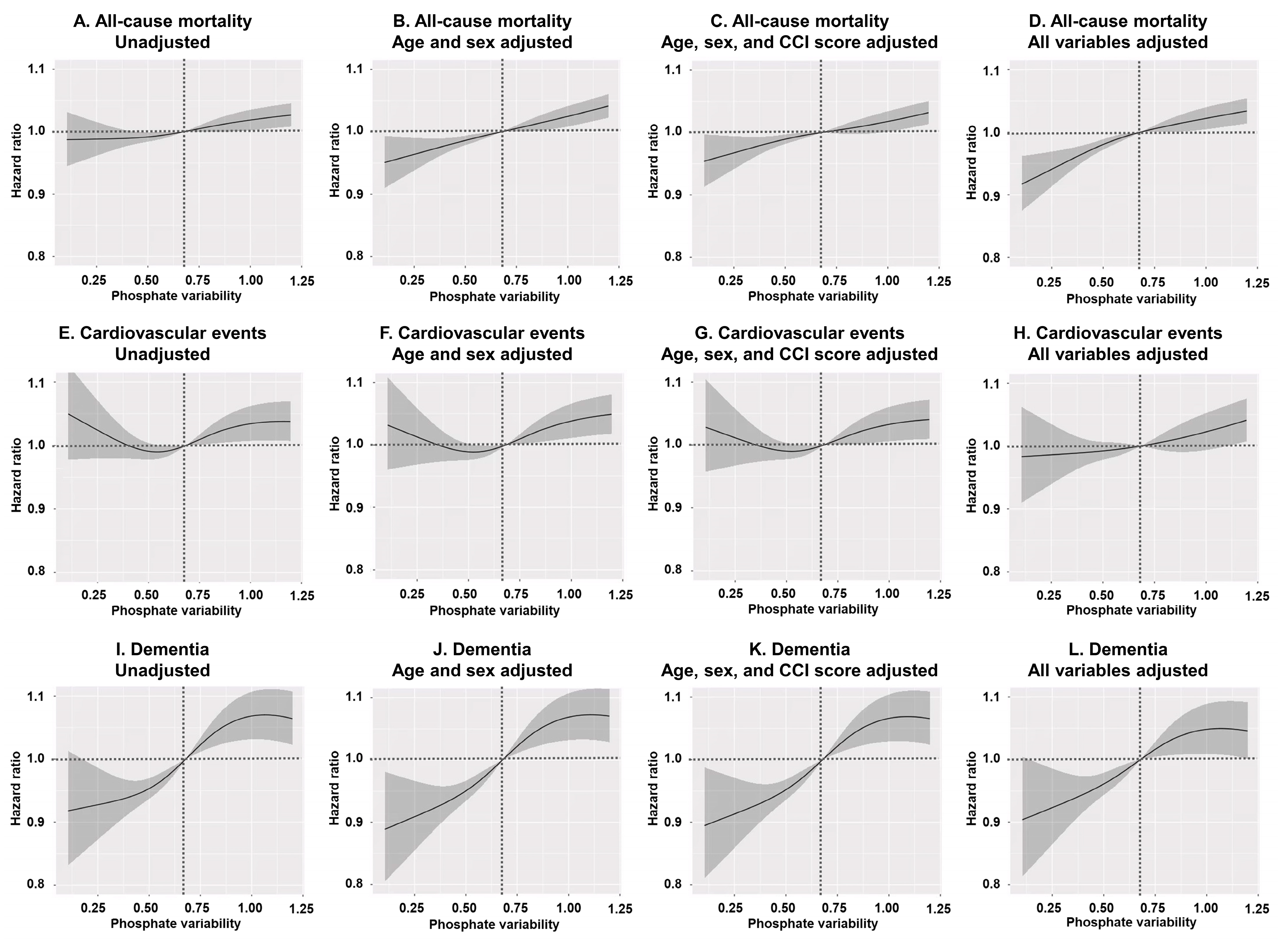
3. Results
3.1. Baseline Characteristics
3.2. Patient Status as Stratified by Phosphate Variability
3.3. Group-Specific Survival Analyses
3.4. Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Htay, H.; Cho, Y.; Jha, V.; See, E.; Arruebo, S.; Caskey, F.J.; Damster, S.; Donner, J.A.; Levin, A.; Nangaku, M.; et al. Global structures, practices, and tools for provision of hemodialysis. Nephrol. Dial. Transplant. 2024, 39 (Suppl. S2), ii11–ii17. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.A.; Polkinghorne, K.R.; McDonald, S.P.; Ierino, F.L. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am. J. Kidney Dis. 2011, 58, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Vervloet, M.G.; van Ballegooijen, A.J. Prevention and treatment of hyperphosphatemia in chronic kidney disease. Kidney Int. 2018, 93, 1060–1072. [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar]
- Fouque, D.; Horne, R.; Cozzolino, M.; Kalantar-Zadeh, K. Balancing nutrition and serum phosphate in maintenance dialysis. Am. J. Kidney Dis. 2014, 64, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Murray, S.L.; Wolf, M. Calcium and Phosphate Disorders: Core Curriculum 2024. Am. J. Kidney Dis. 2024, 83, 241–256. [Google Scholar] [CrossRef]
- Cozzolino, M.; Dusso, A.S.; Slatopolsky, E. Role of calcium-phosphate product and bone-associated proteins on vascular calcification in renal failure. J. Am. Soc. Nephrol. 2001, 12, 2511–2516. [Google Scholar] [CrossRef]
- Yang, W.; Israni, R.K.; Brunelli, S.M.; Joffe, M.M.; Fishbane, S.; Feldman, H.I. Hemoglobin variability and mortality in ESRD. J. Am. Soc. Nephrol. 2007, 18, 3164–3170. [Google Scholar] [CrossRef]
- Di Iorio, B.; Di Micco, L.; Torraca, S.; Sirico, M.L.; Guastaferro, P.; Chiuchiolo, L.; Nigro, F.; De Blasio, A.; Romano, P.; Pota, A.; et al. Variability of blood pressure in dialysis patients: A new marker of cardiovascular risk. J. Nephrol. 2013, 26, 173–182. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, N.; Nie, L.; Lu, C.; Chen, H.; He, W.; Li, M.; Wang, Y.; Zhao, J.; Xiong, J. Visit-to-visit ultrafiltration volume variability predicts all-cause mortality in patients receiving hemodialysis. Ren. Fail. 2023, 45, 2194439. [Google Scholar] [CrossRef]
- Wang, M.; Li, H.; You, L.; Yu, X.; Zhang, M.; Zhu, R.; Hao, C.; Zhang, Z.; Chen, J. Association of serum phosphorus variability with coronary artery calcification among hemodialysis patients. PLoS ONE 2014, 9, e93360. [Google Scholar]
- Hruska, K.A.; Mathew, S.; Lund, R.; Qiu, P.; Pratt, R. Hyperphosphatemia of chronic kidney disease. Kidney Int. 2008, 74, 148–157. [Google Scholar] [PubMed]
- Kang, S.H.; Kim, B.Y.; Son, E.J.; Kim, G.O.; Do, J.Y. Comparison of Patient Survival According to Erythropoiesis-Stimulating Agent Type of Treatment in Maintenance Hemodialysis Patients. J. Clin. Med. 2023, 12, 625. [Google Scholar] [CrossRef] [PubMed]
- Health Insurance Review & Assessment Service. 6th Hemodialysis Quality Assessment Program. Available online: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=6619#none (accessed on 15 March 2025).
- Daugirdas, J.T. Second generation logarithmic estimates of single-pool variable volume Kt/V: An analysis of error. J. Am. Soc. Nephrol. 1993, 4, 1205–1213. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1039–1130. [Google Scholar]
- Kang, S.H.; Kim, B.Y.; Son, E.J.; Kim, G.O.; Do, J.Y. Influence of Different Types of β-Blockers on Mortality in Patients on Hemodialysis. Biomedicines 2023, 11, 2838. [Google Scholar] [CrossRef]
- Levitt, H.; Smith, K.G.; Rosner, M.H. Variability in calcium, phosphorus, and parathyroid hormone in patients on hemodialysis. Hemodial. Int. 2009, 13, 518–525. [Google Scholar] [CrossRef]
- Ter Meulen, K.J.; Ye, X.; Wang, Y.; Usvyat, L.A.; van der Sande, F.M.; Konings, C.J.; Kotanko, P.; Kooman, J.P.; Maddux, F.W. Variability of Serum Phosphate in Incident Hemodialysis Patients: Association with All-Cause Mortality. Kidney360 2023, 4, 374–380. [Google Scholar]
- Zhu, M.; Dou, L.; Zhu, M.; Liu, S.; Zhan, Y.; Lu, J.; Ni, Z.; Qian, J.; Cai, H.; Zhang, W. Variability of serum phosphorus and its association with mortality among hemodialysis patients. Clin. Nephrol. 2018, 90, 79–86. [Google Scholar] [CrossRef]
- Mathur, A.; Ahn, J.B.; Sutton, W.; Chu, N.M.; Gross, A.L.; Segev, D.L.; McAdams-DeMarco, M. Secondary hyperparathyroidism (CKD-MBD) treatment and the risk of dementia. Nephrol. Dial. Transplant. 2022, 37, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Drew, D.A.; Tighiouart, H.; Scott, T.M.; Lou, K.V.; Fan, L.; Shaffi, K.; Weiner, D.E.; Sarnak, M.J. FGF-23 and cognitive performance in hemodialysis patients. Hemodial. Int. 2014, 18, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Yano, Y. Visit-to-Visit Blood Pressure Variability-What is the current challenge? Am. J. Hypertens. 2017, 30, 112–114. [Google Scholar] [CrossRef] [PubMed]

| Interval of Residual SD of Phosphate Levels | Unweighted Cohort | Weighted Cohort | |||
|---|---|---|---|---|---|
| Mean Phosphate Levels | Residual SDs of Phosphate Levels | Mean Phosphate Levels | Residual SDs of Phosphate Levels | ||
| Q1 | ≤0.47 | 4.55 ± 1.07 | 0.34 ± 0.09 | 4.94 ± 0.01 | 0.35 ± 0.00 |
| Q2 | 0.47 < SD ≤ 0.68 | 4.78 ± 1.05 a | 0.57 ± 0.06 a | 4.95 ± 0.01 | 0.57 ± 0.00 a |
| Q3 | 0.68 < SD ≤ 0.94 | 5.08 ± 1.07 a,b | 0.80 ± 0.07 a,b | 4.99 ± 0.01 a,b | 0.79 ± 0.00 a,b |
| Q4 | >0.94 | 5.47 ± 1.09 a,b,c | 1.25 ± 0.29 a,b,c | 5.03 ± 0.01 a,b,c | 1.22 ± 0.00 a,b,c |
| Q1 (n = 48,817) | Q2 (n = 49,310) | Q3 (n = 49,158) | Q4 (n = 47,730) | p | |
|---|---|---|---|---|---|
| Age (years) | 61.8 ± 0.1 | 61.9 ± 0.1 | 61.8 ± 0.1 | 61.7 ± 0.1 | 0.612 |
| Sex (male, %) | 29,993 (61.4%) | 29,987 (60.8%) | 29,525 (60.1%) | 28,322 (59.3%) | 0.011 |
| HD (months) | 67 ± 1 | 67 ± 1 | 66 ± 1 | 67 ± 1 | 0.385 |
| Body mass index (kg/m2) | 22.8 ± 0.0 | 22.8 ± 0.0 | 22.8 ± 0.0 | 22.7 ± 0. | 0.305 |
| Diabetes (%) | 21,481 (44.0%) | 21,803 (44.2%) | 21,701 (44.1%) | 20,353 (42.6%) | 0.066 |
| CCI score | 8.8 ± 0.0 | 8.8 ± 0.0 | 8.8 ± 0.0 | 8.8 ± 0.0 | 0.079 |
| Arteriovenous fistula (%) | 42,385 (86.8%) | 42,665 (86.5%) | 42,450 (86.4%) | 41,046 (86.0%) | 0.353 |
| Kt/Vurea | 1.57 ± 0.00 | 1.57 ± 0.00 | 1.57 ± 0.00 | 1.58 ± 0.00 | 0.016 |
| UFV (L/session) | 2.31 ± 0.01 | 2.30 ± 0.01 | 2.32 ± 0.01 | 2.34 ± 0.01 | 0.001 |
| Hemoglobin (g/dL) | 10.7 ± 0.0 | 10.7 ± 0.0 | 10.7 ± 0.0 | 10.7 ± 0.0 | 0.765 |
| Serum albumin (g/dL) | 4.01 ± 0.0 | 4.01 ± 0.0 | 4.01 ± 0.0 | 4.01 ± 0.0 | 0.865 |
| Serum calcium (mg/dL) | 8.9 ± 0.0 | 8.9 ± 0.0 | 8.9 ± 0.0 | 8.9 ± 0.0 | 0.020 |
| Serum creatinine (mg/dL) | 9.5 ± 0.0 | 9.5 ± 0.0 | 9.6 ± 0.0 | 9.7 ± 0.0 | <0.001 |
| Use of RASB (%) | 32,055 (65.7%) | 32,912 (66.7%) | 32,757 (66.6%) | 31,874 (66.8%) | 0.249 |
| Use of aspirin (%) | 23,643 (48.4%) | 24,326 (49.3%) | 23,954 (48.7%) | 23,301 (48.8%) | 0.606 |
| Use of clopidogrel (%) | 12,639 (25.9%) | 12,752 (25.9%) | 12,561 (25.6%) | 12,596 (26.4%) | 0.570 |
| Use of statins (%) | 23,950 (49.1%) | 24,398 (49.5%) | 24,720 (50.3%) | 23,965 (50.2%) | 0.211 |
| Use of anti-HTN drugs (%) | 41,440 (84.9%) | 41,977 (85.1%) | 41,787 (85.0%) | 40,634 (85.1%) | 0.951 |
| MI or CHF (%) | 28,416 (58.2%) | 28,571 (57.9%) | 28,634 (58.2%) | 27,978 (58.6%) | 0.795 |
| Atrial fibrillation (%) | 5922 (12.1%) | 6120 (12.4%) | 6154 (12.5%) | 5630 (11.8%) | 0.375 |
| PPB (%) | <0.001 | ||||
| Calcium-based PPB | 30,438 (62.4%) | 30,536 (61.9%) | 30,717 (62.5%) | 29,383 (61.6%) | |
| Non-calcium-based PPB | 13,154 (26.9%) | 13,535 (27.4%) | 13,706 (27.9%) | 14,313 (30.0%) | |
| No PPB | 5225 (10.7%) | 5239 (10.6%) | 4735 (9.6%) | 4034 (8.5%) | |
| Use of vitamin D agents (%) | 26,113 (53.5%) | 26,017 (52.8%) | 26,198 (53.3%) | 25,155 (52.7%) | 0.575 |
| Use of cinacalcet (%) | 5898 (12.1%) | 5950 (12.1%) | 5747 (11.7%) | 5592 (11.7%) | 0.688 |
| Use of CaS (%) | 1362 (2.8%) | 1499 (3.0%) | 1557 (3.2%) | 1528 (3.2%) | 0.270 |
| Univariable | Multivariable | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| All–cause mortality | ||||
| Q2 | 1.03 (1.00–1.05) | 0.022 | 1.03 (1.00–1.05) | 0.033 |
| Q3 | 1.04 (1.01–1.06) | 0.002 | 1.08 (1.05–1.10) | <0.001 |
| Q4 | 1.06 (1.04–1.09) | <0.001 | 1.08 (1.06–1.11) | <0.001 |
| Cardiovascular events | ||||
| Q2 | 0.97 (0.93–1.01) | 0.111 | 0.96 (0.93–1.00) | 0.085 |
| Q3 | 1.01 (0.97–1.04) | 0.752 | 1.01 (0.97–1.05) | 0.644 |
| Q4 | 1.01 (0.97–1.05) | 0.612 | 1.02 (0.98–1.07) | 0.243 |
| Dementia | ||||
| Q2 | 1.02 (0.97–1.07) | 0.526 | 0.99 (0.94–1.05) | 0.782 |
| Q3 | 1.06 (1.01–1.11) | 0.022 | 1.05 (0.99–1.11) | 0.079 |
| Q4 | 1.12 (1.06–1.18) | <0.001 | 1.08 (1.02–1.14) | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, S.-H.; Park, S.-Y.; Lim, Y.-J.; Kim, B.-Y.; Choi, J.-Y.; Do, J.-Y.; Kim, A.-Y. Impact of Phosphate Variability in Patients Undergoing Hemodialysis. Nutrients 2025, 17, 1528. https://doi.org/10.3390/nu17091528
Kang S-H, Park S-Y, Lim Y-J, Kim B-Y, Choi J-Y, Do J-Y, Kim A-Y. Impact of Phosphate Variability in Patients Undergoing Hemodialysis. Nutrients. 2025; 17(9):1528. https://doi.org/10.3390/nu17091528
Chicago/Turabian StyleKang, Seok-Hui, So-Young Park, Yu-Jeong Lim, Bo-Yeon Kim, Ji-Young Choi, Jun-Young Do, and A-Young Kim. 2025. "Impact of Phosphate Variability in Patients Undergoing Hemodialysis" Nutrients 17, no. 9: 1528. https://doi.org/10.3390/nu17091528
APA StyleKang, S.-H., Park, S.-Y., Lim, Y.-J., Kim, B.-Y., Choi, J.-Y., Do, J.-Y., & Kim, A.-Y. (2025). Impact of Phosphate Variability in Patients Undergoing Hemodialysis. Nutrients, 17(9), 1528. https://doi.org/10.3390/nu17091528







