Orthorexia Nervosa: Prevalence Among Spanish University Students and Its Effects on Cardiometabolic Health
Abstract
1. Introduction
2. Materials and Methods
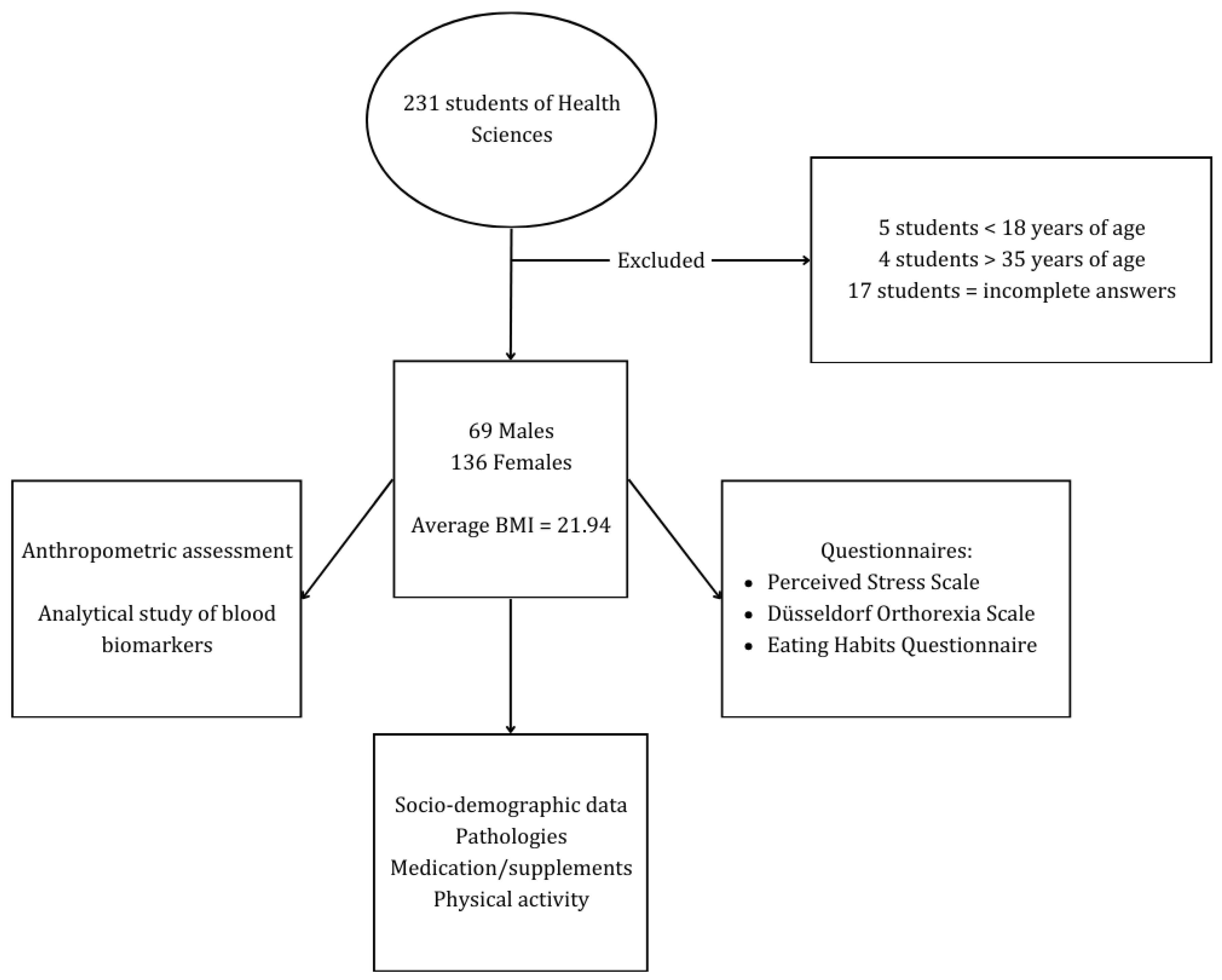
2.1. Study Design and Participants
2.2. Questionnaires
- Spanish version of the Perceived Stress Scale (PSS-ES) [28] used to assess the level of stress perceived during the last month. There is a positive correlation between higher scores and perceived stress levels;
- Spanish version of the Düsseldorf Orthorexia Scale (DOS-ES) [29] used to assess orthorexia behavior through ten statements about healthy eating. The scale is based on a 1 to 4 scoring system from ‘this does not apply to me [1]’ to ‘this does apply to me [4]’. The minimum score is 10 and the cut-off point used is a score > 30 as an indicator of ON. Scores between 25 and 29 indicate a high risk for ON;
- Spanish version of the Eating Habits Questionnaire (EHQ-ES) [30] used to provide a multidimensional measure of knowledge about healthy eating, problems associated with healthy eating and positive feelings about healthy eating. Items are rated on a 4-point scale and high scores indicate tendencies toward orthorexia, with the maximum score being 84.
2.3. Anthropometric Measurements
2.4. Blood Parameters
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bratman, S.; Knight, D. Health Food Junkies: Overcoming the Obsession with Healthful Eating; Broadway Books: New York, NY, USA, 2000; ISBN 978-0-7679-0630-2. [Google Scholar]
- Bratman, S. Health Food Junkie: Obsession with Dietary Perfection Can Sometimes Do More Harm than Good, Says One Who Has Been There. Yoga J. 1997, 136, 42–50. [Google Scholar]
- Chenkov, Y.; Hristova, D.N. A Brief Literature Overview on Orthorexia Nervosa—One New Representative in Cluster of Eating Disorders. J. IMAB 2021, 27, 3568–3571. [Google Scholar] [CrossRef]
- Dunn, T.M.; Bratman, S. On Orthorexia Nervosa: A Review of the Literature and Proposed Diagnostic Criteria. Eat. Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef]
- Parra-Fernández, M.L.; Rodríguez-Cano, T.; Onieva-Zafra, M.-D.; Perez-Haro, M.J.; Casero-Alonso, V.; Fernández-Martinez, E.; Notario-Pacheco, B. Prevalence of Orthorexia Nervosa in University Students and Its Relationship with Psychopathological Aspects of Eating Behaviour Disorders. BMC Psychiatry 2018, 18, 364. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychological Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. International Classification of Diseases 11th Revision; World Health Organization: Genève, Switzerland, 2019; ISBN 978-92-4-154455-9. [Google Scholar]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia Nervosa: Validation of a Diagnosis Questionnaire. Eat. Weight. Disord. 2005, 10, e28–e32. [Google Scholar] [CrossRef]
- Niedzielski, A.; Kaźmierczak-Wojtaś, N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools—A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Koven, N.; Abry, A. The Clinical Basis of Orthorexia Nervosa: Emerging Perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef]
- Varga, M.; Thege, B.K.; Dukay-Szabó, S.; Túry, F.; Van Furth, E.F. When Eating Healthy Is Not Healthy: Orthorexia Nervosa and Its Measurement with the ORTO-15 in Hungary. BMC Psychiatry 2014, 14, 59. [Google Scholar] [CrossRef]
- Missbach, B.; Dunn, T.M.; König, J.S. We Need New Tools to Assess Orthorexia Nervosa. A Commentary on “Prevalence of Orthorexia Nervosa among College Students Based on Bratman’s Test and Associated Tendencies”. Appetite 2017, 108, 521–524. [Google Scholar] [CrossRef]
- Roncero, M.; Barrada, J.R.; Perpiñá, C. Measuring Orthorexia Nervosa: Psychometric Limitations of the ORTO-15. Span. J. Psychol. 2017, 20, E41. [Google Scholar] [CrossRef]
- Barrada, J.R.; Meule, A. Orthorexia Nervosa: Research Based on Invalid Measures Is Invalid. J. Glob. Health 2024, 14, 03007. [Google Scholar] [CrossRef]
- Barrada, J.R.; Roncero, M. Bidimensional Structure of the Orthorexia: Development and Initial Validation of a New Instrument. Ann. Psychol. 2018, 34, 283–291. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Düesseldorf orthorexia scale–construction and evaluation of a questionnaire measuring orthorexic eating behavior. Z. Für Klin. Psychol. Und Psychother. 2015, 44, 97–105. [Google Scholar] [CrossRef]
- Gleaves, D.H.; Graham, E.C.; Ambwani, S. Measuring “Orthorexia”: Development of the Eating Habits Questionnaire. Int. J. Educ. Psychol. Assess. 2013, 12, 1–18. [Google Scholar]
- López-Gil, J.F.; Tárraga-López, P.J.; Soledad Hershey, M.; López-Bueno, R.; Gutiérrez-Espinoza, H.; Soler-Marín, A.; Fernández-Montero, A.; Victoria-Montesinos, D. Overall Proportion of Orthorexia Nervosa Symptoms: A Systematic Review and Meta-Analysis Including 30 476 Individuals from 18 Countries. J. Glob. Health 2023, 13, 04087. [Google Scholar] [CrossRef]
- Scarff, J.R. Orthorexia Nervosa: An Obsession with Healthy Eating. Fed. Pract. 2017, 34, 36–39. [Google Scholar]
- Horovitz, O.; Argyrides, M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients 2023, 15, 3851. [Google Scholar] [CrossRef]
- Korinth, A.; Schiess, S.; Westenhoefer, J. Eating Behaviour and Eating Disorders in Students of Nutrition Sciences. Public Health Nutr. 2010, 13, 32–37. [Google Scholar] [CrossRef]
- Trindade, A.P.; Appolinario, J.C.; Mattos, P.; Treasure, J.; Nazar, B.P. Eating Disorder Symptoms in Brazilian University Students: A Systematic Review and Meta-Analysis. Braz. J. Psychiatry 2019, 41, 179–187. [Google Scholar] [CrossRef]
- Varga, M.; Dukay-Szabó, S.; Túry, F.; Van Furth Eric, F. Evidence and Gaps in the Literature on Orthorexia Nervosa. Eat. Weight. Disord. 2013, 18, 103–111. [Google Scholar] [CrossRef]
- Cartwright, M. Eating Disorder Emergencies: Understanding the Medical Complexities of the Hospitalized Eating Disordered Patient. Crit. Care Nurs. Clin. N. Am. 2004, 16, 515–530. [Google Scholar] [CrossRef]
- Moroze, R.M.; Dunn, T.M.; Craig Holland, J.; Yager, J.; Weintraub, P. Microthinking About Micronutrients: A Case of Transition from Obsessions About Healthy Eating to Near-Fatal “Orthorexia Nervosa” and Proposed Diagnostic Criteria. Psychosomatics 2015, 56, 397–403. [Google Scholar] [CrossRef]
- Villa, M.; Opawsky, N.; Manriquez, S.; Ananías, N.; Vergara-Barra, P.; Leonario-Rodriguez, M. Orthorexia Nervosa Risk and Associated Factors among Chilean Nutrition Students: A Pilot Study. J. Eat. Disord. 2022, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam. Fisioter. Kinesiol. 2007, 10, 48–52. [Google Scholar] [CrossRef]
- Remor, E. Psychometric Properties of a European Spanish Version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Parra-Fernández, M.L.; Onieva-Zafra, M.D.; Fernández-Muñoz, J.J.; Fernández-Martínez, E. Adaptation and Validation of the Spanish Version of the DOS Questionnaire for the Detection of Orthorexic Nervosa Behavior. PLoS ONE 2019, 14, e0216583. [Google Scholar] [CrossRef]
- Parra-Fernández, M.L.; Onieva-Zafra, M.D.; Fernández-Muñoz, J.J.; Głębocka, A.; Fernández-Martínez, E.; Brytek-Matera, A. The Spanish Version of the Eating Habits Questionnaire (EHQ-ES) and Its Links to Symptoms and Concerns Characteristic of Eating Disorders among Young Adults. Nutrients 2021, 13, 1993. [Google Scholar] [CrossRef]
- World Health Organization. A Healthy Lifestyle—WHO Recommendations. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 25 April 2024).
- Van De Wouw, M.; Sichetti, M.; Long-Smith, C.M.; Ritz, N.L.; Moloney, G.M.; Cusack, A.-M.; Berding, K.; Dinan, T.G.; Cryan, J.F. Acute Stress Increases Monocyte Levels and Modulates Receptor Expression in Healthy Females. Brain Behav. Immun. 2021, 94, 463–468. [Google Scholar] [CrossRef]
- Akoglu, H. User’s Guide to Correlation Coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Parra-Fernández, M.L.; Onieva-Zafra, M.D.; Fernández-Martínez, E.; Abreu-Sánchez, A.; Fernández-Muñoz, J.J. Assessing the Prevalence of Orthorexia Nervosa in a Sample of University Students Using Two Different Self-Report Measures. Int. J. Environ. Res. Public Health 2019, 16, 2459. [Google Scholar] [CrossRef]
- Aiello, P.; Toti, E.; Villaño, D.; Raguzzini, A.; Peluso, I. Overlap of Orthorexia, Eating Attitude and Psychological Distress in Some Italian and Spanish University Students. World J. Psychiatry 2022, 12, 1298–1312. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Maciá, A.; Quiles Marcos, Y. Prevalencia de La Ortorexia Nerviosa En Estudiantes Universitarios Españoles: Relación Con La Imagen Corporal y Con Los Trastornos Alimentarios. Ann. Psychol. 2021, 37, 493–499. [Google Scholar] [CrossRef]
- Dunn, T.M.; Gibbs, J.; Whitney, N.; Starosta, A. Prevalence of Orthorexia Nervosa Is Less than 1%: Data from a US Sample. Eat. Weight. Disord. 2017, 22, 185–192. [Google Scholar] [CrossRef]
- He, J.; Ma, H.; Barthels, F.; Fan, X. Psychometric Properties of the Chinese Version of the Düsseldorf Orthorexia Scale: Prevalence and Demographic Correlates of Orthorexia Nervosa among Chinese University Students. Eat. Weight. Disord. 2019, 24, 453–463. [Google Scholar] [CrossRef]
- McInerney, E.G.; Stapleton, P.; Baumann, O. A Systematic Review on the Prevalence and Risk of Orthorexia Nervosa in Health Workers and Students. Int. J. Environ. Res. Public Health 2024, 21, 1103. [Google Scholar] [CrossRef]
- Yılmaz, M.N.; Dundar, C. The Relationship between Orthorexia Nervosa, Anxiety, and Self-Esteem: A Cross-Sectional Study in Turkish Faculty Members. BMC Psychol. 2022, 10, 82. [Google Scholar] [CrossRef]
- Awad, E.; Salameh, P.; Sacre, H.; Malaeb, D.; Hallit, S.; Obeid, S. Association between Impulsivity and Orthorexia Nervosa/Healthy Orthorexia: Any Mediating Effect of Depression, Anxiety, and Stress? BMC Psychiatry 2021, 21, 604. [Google Scholar] [CrossRef]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia Nervosa: A Behavioral Complex or a Psychological Condition? J. Behav. Addict. 2018, 7, 1143–1156. [Google Scholar] [CrossRef]
- Casuso-Holgado, M.J.; Moreno-Morales, N.; Labajos-Manzanares, M.T.; Montero-Bancalero, F.J. The Association between Perceived Health Symptoms and Academic Stress in Spanish Higher Education Students. Eur. J. Educ. Psychol. 2019, 12, 109–123. [Google Scholar] [CrossRef]
- Tamres, L.K.; Janicki, D.; Helgeson, V.S. Sex Differences in Coping Behavior: A Meta-Analytic Review and an Examination of Relative Coping. Personal. Soc. Psychol. Rev. 2002, 6, 2–30. [Google Scholar] [CrossRef]
- Domínguez-Andrés, J.; Reinecke, H.; Sohrabi, Y. The Immune Hunger Games: The Effects of Fasting on Monocytes. Cell. Mol. Immunol. 2023, 20, 1098–1100. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, M.A.; Platt, A.M.; Potteaux, S.; Randolph, G.J. Monocyte Trafficking in Acute and Chronic Inflammation. Trends Immunol. 2011, 32, 470–477. [Google Scholar] [CrossRef] [PubMed]
- León-Pedroza, J.I.; González-Tapia, L.A.; Del Olmo-Gil, E.; Castellanos-Rodríguez, D.; Escobedo, G.; González-Chávez, A. Inflamación sistémica de grado bajo y su relación con el desarrollo de enfermedades metabólicas: De la evidencia molecular a la aplicación clínica. Cirugía Cir. 2015, 83, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Sirin, M.C.; Korkmaz, S.; Erturan, I.; Filiz, B.; Aridogan, B.C.; Cetin, E.S.; Yildirim, M. Evaluation of Monocyte to HDL Cholesterol Ratio and Other Inflammatory Markers in Patients with Psoriasis. An. Bras. Dermatol. 2020, 95, 575–582. [Google Scholar] [CrossRef]
- Ganjali, S.; Gotto, A.M.; Ruscica, M.; Atkin, S.L.; Butler, A.E.; Banach, M.; Sahebkar, A. Monocyte-to-HDL-cholesterol Ratio as a Prognostic Marker in Cardiovascular Diseases. J. Cell. Physiol. 2018, 233, 9237–9246. [Google Scholar] [CrossRef]
- Cetin, M.S.; Ozcan Cetin, E.H.; Kalender, E.; Aydin, S.; Topaloglu, S.; Kisacik, H.L.; Temizhan, A. Monocyte to HDL Cholesterol Ratio Predicts Coronary Artery Disease Severity and Future Major Cardiovascular Adverse Events in Acute Coronary Syndrome. Heart Lung Circ. 2016, 25, 1077–1086. [Google Scholar] [CrossRef]
- Tremelling, K.; Sandon, L.; Vega, G.L.; McAdams, C.J. Orthorexia Nervosa and Eating Disorder Symptoms in Registered Dietitian Nutritionists in the United States. J. Acad. Nutr. Diet. 2017, 117, 1612–1617. [Google Scholar] [CrossRef]
- Novara, C.; Maggio, E.; Piasentin, S.; Pardini, S.; Mattioli, S. Orthorexia Nervosa: Differences between Clinical and Non-Clinical Samples. BMC Psychiatry 2021, 21, 341. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Gkiouras, K.; Markaki, A.; Theodoridis, X.; Tsakiri, V.; Mavridis, P.; Dardavessis, T.; Chourdakis, M. Food Addiction, Orthorexia, and Food-Related Stress among Dietetics Students. Eat. Weight. Disord. 2018, 23, 459–467. [Google Scholar] [CrossRef]
- Abdullah, M.A.; Al Hourani, H.M.; Alkhatib, B. Prevalence of Orthorexia Nervosa among Nutrition Students and Nutritionists: Pilot Study. Clin. Nutr. ESPEN 2020, 40, 144–148. [Google Scholar] [CrossRef]
- Plichta, M.; Jezewska-Zychowicz, M.; Gębski, J. Orthorexic Tendency in Polish Students: Exploring Association with Dietary Patterns, Body Satisfaction and Weight. Nutrients 2019, 11, 100. [Google Scholar] [CrossRef] [PubMed]
- Yılmazel, G. Orthorexia Tendency and Social Media Addiction among Candidate Doctors and Nurses. Perspect. Psychiatr. Care 2021, 57, 1846–1852. [Google Scholar] [CrossRef] [PubMed]
| Variables | n (%)/Mean ± SD |
|---|---|
| Gender | |
| Male | 69 (33.7) |
| Female | 136 (66.3) |
| Age | |
| 18–23 | 182 (88.88) |
| 24–29 | 15 (7.3) |
| 30–35 | 8 (3.9) |
| Body Mass Index | |
| Healthy weight (18.5–24.9 kg/m2) | 158 (77.1) |
| Underweight (<18.5 kg/m2) | 17 (8.3) |
| Overweight (25–29.9 kg/m2) | 25 (12.2) |
| Obesity (≥30 kg/m2) | 5 (2.4) |
| IPAQ | |
| Low | 91 (44.4) |
| Moderate | 57 (27.8) |
| High | 57 (27.8) |
| Use of nutritional supplements | |
| Yes | 28 (13.7) |
| No | 177 (86.3) |
| Pathologies | |
| Yes | 41 (20) |
| No | 164 (80) |
| Use of medication | |
| Yes | 43 (21) |
| No | 162 (79) |
| Score in the Perceived Stress Scale | 25.74 ± 7.70 |
| Variables | OR 95% CI | p-Value |
|---|---|---|
| Gender | ||
| Females | Reference | |
| Males | 1.00 (0.94–1.07) | 0.93 |
| Age | ||
| 18–23 | Reference | |
| 24–29 | 1.01 (0.91–1.13) | 0.79 |
| 30–35 | 1.13 (0.99–1.28) | 0.65 |
| BMI | ||
| 18.5–24.9 | Reference | |
| <18.5 | 1.11 (1.01–1.22) | 0.03 |
| 25–29.9 | 0.98 (0.89–1.08) | 0.72 |
| ≥30 | 0.96 (0.77–1.19) | 0.70 |
| Total cholesterol | ||
| 150–199 | Reference | |
| <150 | 0.98 (0.89–1.08) | 0.71 |
| ≥200 | 0.99 (0.93–1.06) | 0.86 |
| HDL-c | ||
| ≥40 | Reference | |
| <40 | 1.00 (0.92–1.09) | 0.95 |
| LDL-c | ||
| <130 | Reference | |
| ≥130 | 0.96 (0.83–1.11) | 0.60 |
| TG | ||
| 150–200 | Reference | |
| <150 | 0.98 (0.88–1.08) | 0.70 |
| >200 | 1.06 (0.93–1.22) | 0.39 |
| Leucocytes | ||
| 4.5–11 × 103 cells/mcL | Reference | |
| <4.5 × 103 cells/mcL | 0.93 (0.76–1.14) | 0.50 |
| >11 × 103 cells/mcL | 1.13 (0.99–1.28) | 0.07 |
| Monocytes | ||
| 0.14–1.3 × 103 cells/mcL | Reference | |
| <0.14 × 103 cells/mcL | 1.05 (0.84–1.31) | 0.66 |
| >1.3 × 103 cells/mcL | 1.15 (1.05–1.26) | 0.02 |
| Lymphocytes | ||
| 0.77–4.5 × 103 cells/mcL | Reference | |
| >4.5 × 103 cells/mcL | 1.14 (0.93–1.39) | 0.22 |
| Eosinophils | ||
| 0–0.55 × 103 cells/mcL | Reference | |
| >0.55 × 103 cells/mcL | 1.05 (0.89–1.23) | 0.56 |
| Basophils | ||
| 0–0.22 × 103 cells/mcL | Reference | |
| >0.22 × 103 cells/mcL | 1.02 (0.68–1.53) | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manero-Higuera, S.; Garcés-Rimón, M.; Iglesias-López, M.T.; López-Moreno, M. Orthorexia Nervosa: Prevalence Among Spanish University Students and Its Effects on Cardiometabolic Health. Nutrients 2025, 17, 629. https://doi.org/10.3390/nu17040629
Manero-Higuera S, Garcés-Rimón M, Iglesias-López MT, López-Moreno M. Orthorexia Nervosa: Prevalence Among Spanish University Students and Its Effects on Cardiometabolic Health. Nutrients. 2025; 17(4):629. https://doi.org/10.3390/nu17040629
Chicago/Turabian StyleManero-Higuera, Sara, Marta Garcés-Rimón, María Teresa Iglesias-López, and Miguel López-Moreno. 2025. "Orthorexia Nervosa: Prevalence Among Spanish University Students and Its Effects on Cardiometabolic Health" Nutrients 17, no. 4: 629. https://doi.org/10.3390/nu17040629
APA StyleManero-Higuera, S., Garcés-Rimón, M., Iglesias-López, M. T., & López-Moreno, M. (2025). Orthorexia Nervosa: Prevalence Among Spanish University Students and Its Effects on Cardiometabolic Health. Nutrients, 17(4), 629. https://doi.org/10.3390/nu17040629






