Evaluating the Therapeutic Potential of Exercise in Hypoxia and Low-Carbohydrate, High-Fat Diet in Managing Hypertension in Elderly Type 2 Diabetes Patients: A Novel Intervention Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
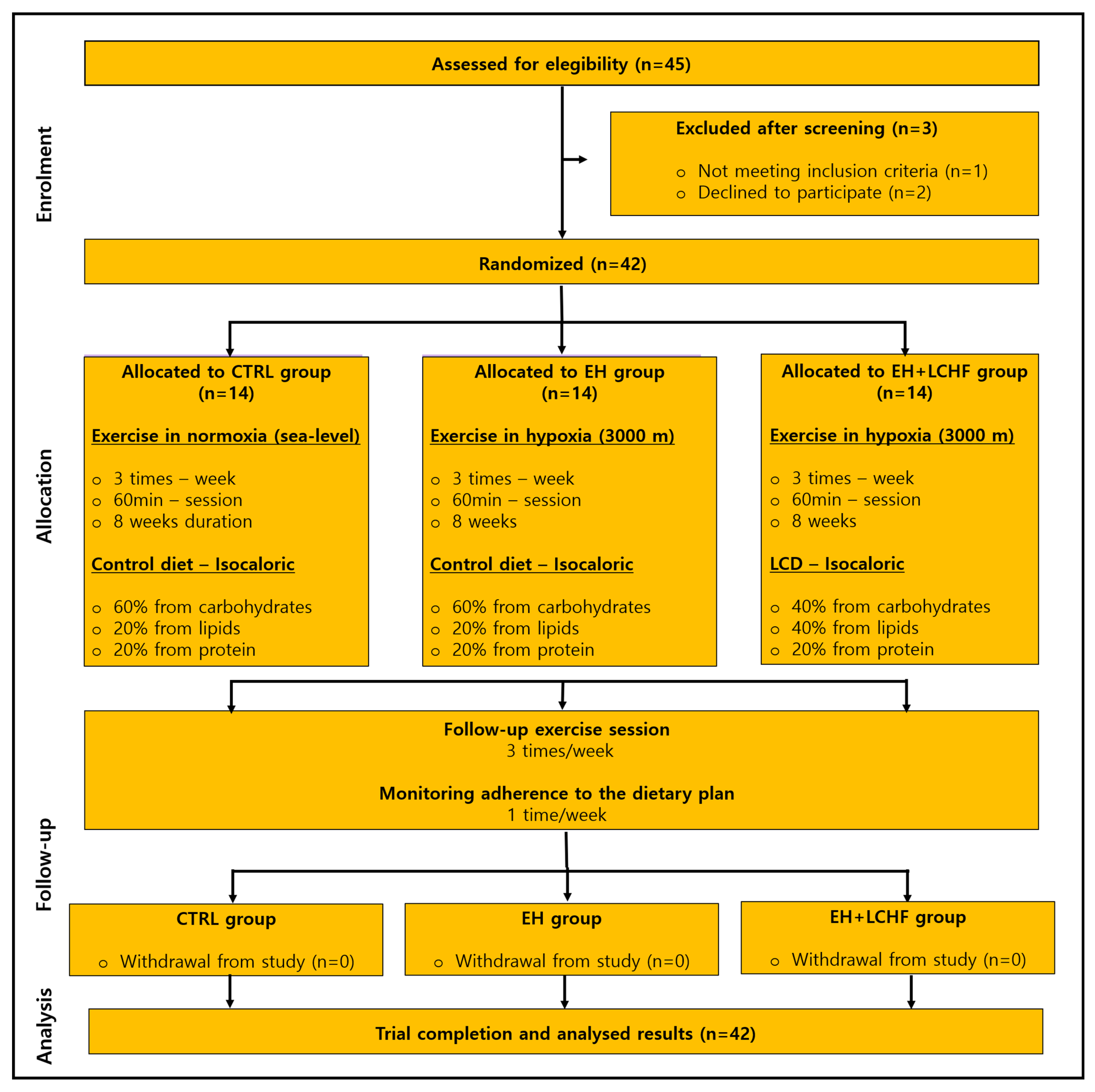
2.2. Study Design
2.3. Participants
2.4. Dietary Plan
2.5. Exercise Protocol
2.6. Measurements
2.7. Blood Samples Analyses
2.8. Blood Pressure
2.9. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Dietary and Exercise Interventions
3.3. Cardiovascular Risk Factors
3.4. Hematological Parameters
3.5. Blood Pressure
4. Discussion
4.1. Strengths and Limitations
4.2. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Magliano, D.J.; Boyko, E.J. IDF DIABETES ATLAS, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. Available online: https://www.ncbi.nlm.nih.gov/pubmed/35914061 (accessed on 5 June 2024).
- Sobczak, A.I.S.; Stewart, A.J. Coagulatory Defects in Type-1 and Type-2 Diabetes. Int. J. Mol. Sci. 2019, 20, 6345. [Google Scholar] [CrossRef] [PubMed]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- Yen, F.-S.; Wei, J.C.-C.; Chiu, L.-T.; Hsu, C.-C.; Hwu, C.-M. Diabetes, hypertension, and cardiovascular disease development. J. Transl. Med. 2022, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Rapsomaniki, E.; Timmis, A.; George, J.; Pujades-Rodriguez, M.; Shah, A.D.; Denaxas, S.; White, I.R.; Caulfield, M.J.; Deanfield, J.E.; Smeeth, L.; et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014, 383, 1899–1911. [Google Scholar] [CrossRef]
- Chen, G.; McAlister, F.A.; Walker, R.L.; Hemmelgarn, B.R.; Campbell, N.R. Cardiovascular outcomes in framingham participants with diabetes: The importance of blood pressure. Hypertension 2011, 57, 891–897. [Google Scholar] [CrossRef]
- Dongway, A.C.; Faggad, A.S.; Zaki, H.Y.; Abdalla, B.E. C-reactive protein is associated with low-density lipoprotein cholesterol and obesity in type 2 diabetic Sudanese. Diabetes Metab. Syndr. Obes. 2015, 8, 427–435. [Google Scholar] [CrossRef]
- Cangelosi, G.; Grappasonni, I.; Nguyen, C.T.T.; Acito, M.; Pantanetti, P.; Benni, A.; Petrelli, F. Mediterranean Diet (MedDiet) and Lifestyle Medicine (LM) for support and care of patients with type II diabetes in the COVID-19 era: A cross-observational study. Acta Biomed. 2023, 94, e2023189. [Google Scholar] [CrossRef]
- Morrato, E.H.; Hill, J.O.; Wyatt, H.R.; Ghushchyan, V.; Sullivan, P.W. Physical activity in U.S. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care 2007, 30, 203–209. [Google Scholar] [CrossRef]
- Pan, B.; Ge, L.; Xun, Y.Q.; Chen, Y.J.; Gao, C.Y.; Han, X.; Zuo, L.Q.; Shan, H.Q.; Yang, K.H.; Ding, G.W.; et al. Exercise training modalities in patients with type 2 diabetes mellitus: A systematic review and network meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 72. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef]
- Gentzel, J.B. On “exercise assessment and prescription in patients with type 2 diabetes…” Hansen D, Peeters S, Zwaenepoel B; et al. Phys Ther. 2013;93:597-610. Phys. Ther. 2013, 93, 1141–1142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Colberg, S.R.; Sigal, R.J.; Fernhall, B.; Regensteiner, J.G.; Blissmer, B.J.; Rubin, R.R.; Chasan-Taber, L.; Albright, A.L.; Braun, B. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care 2010, 33, e147–e167. [Google Scholar] [CrossRef] [PubMed]
- Hordern, M.D.; Dunstan, D.W.; Prins, J.B.; Baker, M.K.; Singh, M.A.; Coombes, J.S. Exercise prescription for patients with type 2 diabetes and pre-diabetes: A position statement from Exercise and Sport Science Australia. J. Sci. Med. Sport. 2012, 15, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Ebrahim, H.; Fiseha, T.; Ebrahim, Y.; Bisetegn, H. Comparison of hematological parameters between type 2 diabetes mellitus patients and healthy controls at Dessie comprehensive specialized hospital, Northeast Ethiopia: Comparative cross-sectional study. PLoS ONE 2022, 17, e0272145. [Google Scholar] [CrossRef] [PubMed]
- Yatsutani, H.; Mori, H.; Ito, H.; Hayashi, N.; Girard, O.; Goto, K. Endocrine and Metabolic Responses to Endurance Exercise Under Hot and Hypoxic Conditions. Front. Physiol. 2020, 11, 932. [Google Scholar] [CrossRef]
- Baker, J.M.; Parise, G. Skeletal Muscle Erythropoietin Expression Is Responsive to Hypoxia and Exercise. Med. Sci. Sports Exerc. 2016, 48, 1294–1301. [Google Scholar] [CrossRef]
- Glazachev, O.S.; Kryzhanovskaya, S.Y.; Zapara, M.A.; Dudnik, E.N.; Samartseva, V.G.; Susta, D. Safety and Efficacy of Intermittent Hypoxia Conditioning as a New Rehabilitation/Secondary Prevention Strategy for Patients with Cardiovascular Diseases: A Systematic Review and Meta-analysis. Curr. Cardiol. Rev. 2021, 17, e051121193317. [Google Scholar] [CrossRef]
- Kindlovits, R.; Pereira, A.; Sousa, A.C.; Viana, J.L.; Teixeira, V.H. Effects of Acute and Chronic Exercise in Hypoxia on Cardiovascular and Glycemic Parameters in Patients with Type 2 Diabetes: A Systematic Review. High. Alt. Med. Biol. 2022, 23, 301–312. [Google Scholar] [CrossRef]
- Sato, T.; Takeda, N. The roles of HIF-1alpha signaling in cardiovascular diseases. J. Cardiol. 2023, 81, 202–208. [Google Scholar] [CrossRef]
- Lindholm, M.E.; Rundqvist, H. Skeletal muscle hypoxia-inducible factor-1 and exercise. Exp. Physiol. 2016, 101, 28–32. [Google Scholar] [CrossRef]
- Weidemann, A.; Johnson, R.S. Biology of HIF-1alpha. Cell Death Differ. 2008, 15, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Kong, Z.; Zang, Y.; Hu, Y. Normobaric hypoxia training causes more weight loss than normoxia training after a 4-week residential camp for obese young adults. Sleep. Breath. 2014, 18, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Morishima, T.; Hasegawa, Y.; Sasaki, H.; Kurihara, T.; Hamaoka, T.; Goto, K. Effects of different periods of hypoxic training on glucose metabolism and insulin sensitivity. Clin. Physiol. Funct. Imaging 2015, 35, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Muniesa, P.; Lopez-Pascual, A.; de Andres, J.; Lasa, A.; Portillo, M.P.; Aros, F.; Duran, J.; Egea, C.J.; Martinez, J.A. Impact of intermittent hypoxia and exercise on blood pressure and metabolic features from obese subjects suffering sleep apnea-hypopnea syndrome. J. Physiol. Biochem. 2015, 71, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Schobersberger, W.; Schmid, P.; Lechleitner, M.; von Duvillard, S.P.; Hortnagl, H.; Gunga, H.C.; Klingler, A.; Fries, D.; Kirsch, K.; Spiesberger, R.; et al. Austrian Moderate Altitude Study 2000 (AMAS 2000). The effects of moderate altitude (1700 m) on cardiovascular and metabolic variables in patients with metabolic syndrome. Eur. J. Appl. Physiol. 2003, 88, 506–514. [Google Scholar] [CrossRef]
- Sakagami, H.; Makino, Y.; Mizumoto, K.; Isoe, T.; Takeda, Y.; Watanabe, J.; Fujita, Y.; Takiyama, Y.; Abiko, A.; Haneda, M. Loss of HIF-1alpha impairs GLUT4 translocation and glucose uptake by the skeletal muscle cells. Am. J. Physiol. Endocrinol. Metab. 2014, 306, E1065–E1076. [Google Scholar] [CrossRef]
- Arauz-Pacheco, C.; Parrott, M.A.; Raskin, P.; American Diabetes Association. Hypertension management in adults with diabetes. Diabetes Care 2004, 27 (Suppl. 1), S65–S67. [Google Scholar] [CrossRef]
- Eckel, R.H.; Jakicic, J.M.; Ard, J.D.; de Jesus, J.M.; Houston Miller, N.; Hubbard, V.S.; Lee, I.M.; Lichtenstein, A.H.; Loria, C.M.; Millen, B.E.; et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S76–S99. [Google Scholar] [CrossRef]
- Evert, A.B.; Dennison, M.; Gardner, C.D.; Garvey, W.T.; Lau, K.H.K.; MacLeod, J.; Mitri, J.; Pereira, R.F.; Rawlings, K.; Robinson, S.; et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care 2019, 42, 731–754. [Google Scholar] [CrossRef]
- Bueno, N.B.; de Melo, I.S.; de Oliveira, S.L.; da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187. [Google Scholar] [CrossRef]
- Saslow, L.R.; Jones, L.M.; Sen, A.; Wolfson, J.A.; Diez, H.L.; O’Brien, A.; Leung, C.W.; Bayandorian, H.; Daubenmier, J.; Missel, A.L.; et al. Comparing Very Low-Carbohydrate vs DASH Diets for Overweight or Obese Adults with Hypertension and Prediabetes or Type 2 Diabetes: A Randomized Trial. Ann. Fam. Med. 2023, 21, 256–263. [Google Scholar] [CrossRef] [PubMed]
- McSwiney, F.T.; Doyle, L. Low-Carbohydrate Ketogenic Diets in Male Endurance Athletes Demonstrate Different Micronutrient Contents and Changes in Corpuscular Haemoglobin over 12 Weeks. Sports 2019, 7, 201. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, R.; Tabara, Y.; Kohara, K.; Miki, T.; Kusunoki, T.; Abe, M.; Katoh, T. Hematological parameters are associated with metabolic syndrome in Japanese community-dwelling persons. Endocrine 2013, 43, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Mansoori, A.; Sahranavard, T.; Hosseini, Z.S.; Soflaei, S.S.; Emrani, N.; Nazar, E.; Gharizadeh, M.; Khorasanchi, Z.; Effati, S.; Ghamsary, M.; et al. Prediction of type 2 diabetes mellitus using hematological factors based on machine learning approaches: A cohort study analysis. Sci. Rep. 2023, 13, 663. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.H.; White, C.R.; Patel, R.P. Vasoactivity of S-nitrosohemoglobin: Role of oxygen, heme, and NO oxidation states. Blood 2003, 101, 4408–4415. [Google Scholar] [CrossRef]
- Floras, J.S.; Meneilly, G. Insulin-mediated blood flow and glucose uptake. Can. J. Cardiol. 2001, 17 (Suppl. A), 7A–10A. Available online: https://www.ncbi.nlm.nih.gov/pubmed/11381287 (accessed on 27 June 2024).
- Crawford, J.H.; Chacko, B.K.; Kevil, C.G.; Patel, R.P. The red blood cell and vascular function in health and disease. Antioxid. Redox Signal 2004, 6, 992–999. [Google Scholar] [CrossRef]
- Goodyear, M.D.; Krleza-Jeric, K.; Lemmens, T. The Declaration of Helsinki. BMJ 2007, 335, 624–625. [Google Scholar] [CrossRef]
- Kindlovits, R.; Sousa, A.C.; Viana, J.L.; Milheiro, J.; Marques, F.; Teixeira, V.H. Combined low-carbohydrate diet and long-term exercise in hypoxia in type 2 diabetes: A randomized controlled trial protocol to assess glycemic control, cardiovascular risk factors and body composition. Nutr. Health 2024, 30, 5–13. [Google Scholar] [CrossRef]
- Kindlovits, R.; Sousa, A.C.; Viana, J.L.; Milheiro, J.; Oliveira, B.; Marques, F.; Santos, A.; Teixeira, V.H. Eight Weeks of Intermittent Exercise in Hypoxia, with or without a Low-Carbohydrate Diet, Improves Bone Mass and Functional and Physiological Capacity in Older Adults with Type 2 Diabetes. Nutrients 2024, 16, 1624. [Google Scholar] [CrossRef]
- Cioffi, I.; Marra, M.; Pasanisi, F.; Scalfi, L. Prediction of resting energy expenditure in healthy older adults: A systematic review. Clin. Nutr. 2021, 40, 3094–3103. [Google Scholar] [CrossRef] [PubMed]
- Sjostrom, M.; Ainsworth, B.E.; Bauman, A.; Bull, F.C.; Hamilton-Craig, C.R.; Sallis, J.F. Guidelines for data processing analysis of the International Physical Activity Questionnaire (IPAQ)—Short and long forms. 2005. Available online: https://sites.google.com/view/ipaq/score (accessed on 26 January 2025).
- Dyson, P.A.; Twenefour, D.; Breen, C.; Duncan, A.; Elvin, E.; Goff, L.; Hill, A.; Kalsi, P.; Marsland, N.; McArdle, P.; et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet. Med. 2018, 35, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Silverii, G.A.; Botarelli, L.; Dicembrini, I.; Girolamo, V.; Santagiuliana, F.; Monami, M.; Mannucci, E. Low-carbohydrate diets and type 2 diabetes treatment: A meta-analysis of randomized controlled trials. Acta Diabetol. 2020, 57, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Idrose, A.M.; Juliana, N.; Azmani, S.; Yazit, N.A.A.; Muslim, M.S.A.; Ismail, M.; Amir, S.N. Singing Improves Oxygen Saturation in Simulated High-Altitude Environment. J. Voice 2022, 36, 316–321. [Google Scholar] [CrossRef]
- Scherr, J.; Wolfarth, B.; Christle, J.W.; Pressler, A.; Wagenpfeil, S.; Halle, M. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur. J. Appl. Physiol. 2013, 113, 147–155. [Google Scholar] [CrossRef]
- van Zuuren, E.J.; Fedorowicz, Z.; Kuijpers, T.; Pijl, H. Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: A systematic review including GRADE assessments. Am. J. Clin. Nutr. 2018, 108, 300–331. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Hein, M.; Chobanyan-Jurgens, K.; Tegtbur, U.; Engeli, S.; Jordan, J.; Haufe, S. Effect of normobaric hypoxic exercise on blood pressure in old individuals. Eur. J. Appl. Physiol. 2021, 121, 817–825. [Google Scholar] [CrossRef]
- Stewart, K.J.; Bacher, A.C.; Turner, K.L.; Fleg, J.L.; Hees, P.S.; Shapiro, E.P.; Tayback, M.; Ouyang, P. Effect of exercise on blood pressure in older persons: A randomized controlled trial. Arch. Intern. Med. 2005, 165, 756–762. [Google Scholar] [CrossRef]
- Gatterer, H.; Haacke, S.; Burtscher, M.; Faulhaber, M.; Melmer, A.; Ebenbichler, C.; Strohl, K.P.; Hogel, J.; Netzer, N.C. Normobaric Intermittent Hypoxia over 8 Months Does Not Reduce Body Weight and Metabolic Risk Factors—A Randomized, Single Blind, Placebo-Controlled Study in Normobaric Hypoxia and Normobaric Sham Hypoxia. Obes. Facts 2015, 8, 200–209. [Google Scholar] [CrossRef]
- Millet, G.P.; Roels, B.; Schmitt, L.; Woorons, X.; Richalet, J.P. Combining hypoxic methods for peak performance. Sports Med. 2010, 40, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.A.; Quod, M.J.; Clark, M.A.; Martin, D.T.; Saunders, P.U.; Gore, C.J. Time course of haemoglobin mass during 21 days live high:train low simulated altitude. Eur. J. Appl. Physiol. 2009, 106, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yang, C.; Zhang, X.; Ye, R.; Li, X.; Zhang, Z.; Jia, S.; Sun, L.; Meng, Q.; Chen, X. Association between hemoglobin concentration and hypertension risk in native Tibetans at high altitude. J. Clin. Hypertens. 2024, 26, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Neya, M.; Enoki, T.; Ohiwa, N.; Kawahara, T.; Gore, C.J. Increased hemoglobin mass and VO2max with 10 h nightly simulated altitude at 3000 m. Int. J. Sports Physiol. Perform 2013, 8, 366–372. [Google Scholar] [CrossRef]
- Billett, H.H. Hemoglobin and Hematocrit. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21250102 (accessed on 5 June 2024).
- Alkhaldy, H.Y.; Awan, Z.A.; Abouzaid, A.A.; Elbahaey, H.M.; Al Amoudi, S.M.; Shehata, S.F.; Saboor, M. Effect of Altitude on Hemoglobin and Red Blood Cell Indices in Adults in Different Regions of Saudi Arabia. Int. J. Gen. Med. 2022, 15, 3559–3565. [Google Scholar] [CrossRef]
- Yan, Y.; Mao, Z.; Jia, Q.; Zhao, X.J.; Yang, S.H. Changes in blood pressure, oxygen saturation, hemoglobin concentration, and heart rate among low-altitude migrants living at high altitude (5380 m) for 360 days. Am. J. Hum. Biol. 2023, 35, e23913. [Google Scholar] [CrossRef]
- Burtscher, M.; Pachinger, O.; Ehrenbourg, I.; Mitterbauer, G.; Faulhaber, M.; Puhringer, R.; Tkatchouk, E. Intermittent hypoxia increases exercise tolerance in elderly men with and without coronary artery disease. Int. J. Cardiol. 2004, 96, 247–254. [Google Scholar] [CrossRef]
- Nishiwaki, M.; Kawakami, R.; Saito, K.; Tamaki, H.; Takekura, H.; Ogita, F. Vascular adaptations to hypobaric hypoxic training in postmenopausal women. J. Physiol. Sci. 2011, 61, 83–91. [Google Scholar] [CrossRef]
- Urdampilleta, A.; Gonzalez-Muniesa, P.; Portillo, M.P.; Martinez, J.A. Usefulness of combining intermittent hypoxia and physical exercise in the treatment of obesity. J. Physiol. Biochem. 2012, 68, 289–304. [Google Scholar] [CrossRef]
- Ladage, D.; Braunroth, C.; Lenzen, E.; Berghofer, S.; Graf, C.; Bloch, W.; Brixius, K. Influence of intermittent hypoxia interval training on exercise-dependent erythrocyte NOS activation and blood pressure in diabetic patients. Can. J. Physiol. Pharmacol. 2012, 90, 1591–1598. [Google Scholar] [CrossRef]
- Jain, T.; Nikolopoulou, E.A.; Xu, Q.; Qu, A. Hypoxia inducible factor as a therapeutic target for atherosclerosis. Pharmacol. Ther. 2018, 183, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, J.C.; Hoiland, R.L.; Howe, C.A.; Coombs, G.B.; Vizcardo-Galindo, G.A.; Figueroa-Mujica, R.J.; Bermudez, D.; Gibbons, T.D.; Stacey, B.S.; Bailey, D.M.; et al. Global REACH 2018: High Blood Viscosity and Hemoglobin Concentration Contribute to Reduced Flow-Mediated Dilation in High-Altitude Excessive Erythrocytosis. Hypertension 2019, 73, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- Zidek, V.; Fucikova, A.; Musilova, A.; Bila, V.; Kren, V.; Pravenec, M. Hematocrit and hemoglobin values are negatively correlated with insulin resistance in spontaneous hypertension. Folia. Biol. 1999, 45, 247–251. Available online: https://www.ncbi.nlm.nih.gov/pubmed/10732721 (accessed on 7 June 2024).
- McKay, A.K.A.; Peeling, P.; Pyne, D.B.; Welvaert, M.; Tee, N.; Leckey, J.J.; Sharma, A.P.; Ross, M.L.R.; Garvican-Lewis, L.A.; Swinkels, D.W.; et al. Chronic Adherence to a Ketogenic Diet Modifies Iron Metabolism in Elite Athletes. Med. Sci. Sports Exerc. 2019, 51, 548–555. [Google Scholar] [CrossRef]
- Yu, J.G.; Javorschi, S.; Hevener, A.L.; Kruszynska, Y.T.; Norman, R.A.; Sinha, M.; Olefsky, J.M. The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 2002, 51, 2968–2974. [Google Scholar] [CrossRef]
- Kutlu, M.; Sonmez, A.; Genc, H.; Erdem, G.; Tapan, S.; Celebi, G.; Haymana, C.; Taslipinar, A.; Uckaya, G.; Erbil, M.K. Relationship between hemoglobin and CD40 ligand in prediabetes. Clin. Investig. Med. 2009, 32, E244. [Google Scholar] [CrossRef]
- Missiou, A.; Wolf, D.; Platzer, I.; Ernst, S.; Walter, C.; Rudolf, P.; Zirlik, K.; Kostlin, N.; Willecke, F.K.; Munkel, C.; et al. CD40L induces inflammation and adipogenesis in adipose cells—A potential link between metabolic and cardiovascular disease. Thromb. Haemost. 2010, 103, 788–796. [Google Scholar] [CrossRef]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef]
| Variables | CTRL Group | EH Group | EH+LCHF Group | p-Value |
|---|---|---|---|---|
| Gender (male:female) | 7:7 | 8:6 | 9:5 | 0.747 |
| Age (years) | 74.4 (3.6) | 71.6 (3.8) | 70.7 (4.0) | 0.110 |
| Body mass index (kg/m2) | 29.4 (4.1) | 28.3 (4.0) | 29.3 (3.4) | 0.707 |
| Hemoglobin A1c (%) | 6.9 (0.8) | 7.1 (0.7) | 6.8 (0.5) | 0.647 |
| Fasting glucose (mg/dL) | 118.7 (27.8) | 117.9 (22.3) | 108.2 (19.7) | 0.435 |
| Systolic blood pressure (mmHg) | 154.7 (20.9) | 142.3 (18.2) | 148.0 (18.9) | 0.254 |
| Diastolic blood pressure (mmHg) | 77.5 (8.1) | 76.3 (11.7) | 82.9 (16.3) | 0.347 |
| Mean arterial blood pressure (mmHg) | 107.9 (16.9) | 98.7 (13.6) | 107.1 (15.8) | 0.234 |
| Variables | CTRL Group | EH Group | EH+LCHF Group | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | Pre | Post | Δ | Moments | Groups | |
| Cholesterol (mmol/L) | 181.2 (49.5) | 188.1 (51.8) | 2.4 (17.7) | 178.9 (30.1) | 161.9 (23.2) | 7.1 (6.7) | 158.5 (46.4) | 143.2 (42.7) | 7.3 (16.4) | 0.082 | 0.135 |
| HDL-c (mmol/L) | 53.8 (11.7) | 52.5 (10.6) | 0.5 (2.2) | 52.3 (13.1) | 52.0 (9.4) | 0.1 (2.8) | 56.2 (14.0) | 57.2 (13.9) | 0.4 (1.4) | 0.987 | 0.511 |
| LDL-c (mmol/L) | 100.4 (43.2) | 112.5 (48.4) | 3.6 (14.3) | 104.5 (29.2) | 93.8 (19.1) | 3.3 (6.4) | 87.7 (36.6) | 77.7 (28.4) | 3.5 (8.3) | 0.501 | 0.119 |
| TAG (mmol/L) | 134.6 (61.5) | 133.8 (46.4) | 1.2 (9.4) | 136.5 (59.6) | 126.8 (47.1) | 2.1 (9.0) | 96.2 (29.8) | 91.2 (29.6) | 2.5 (9.9) | 0.435 | 0.518 |
| CRP (mg/dL) | 1.8 (2.4) | 3.3 (6.4) | 0.1 (0.3) | 1.9 (2.1) | 1.6 (1.7) | 0.1 (0.1) | 3.4 (4.7) | 1.7 (1.3) | 0.2 (0.3) | 0.155 | 0.19 |
| Variables | CTRL Group | EH Group | EH+LCHF Group | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | Pre | Post | Δ | Moments | Groups | |
| Erythrocytes (L) | 4.7 (0.4) | 4.7 (0.5) | 0.1 (0.1) | 4.5 (0.4) | 4.5 (0.5) | 0.1 (0.2) | 4.6 (0.51) | 4.7 (0.5) | 0.1 (0.2) | 0.585 | 0.122 |
| Hemoglobin (g/dL) | 14.2 (1.0) | 14.2 (1.2) | 0.1 (0.5) | 13.9 (1.3) | 13.7 (1.4) | 0.1 (0.6) | 13.8 (1.6) | 13.7 (1.7) | 0.1 (0.5) | 0.355 | 0.668 |
| Hematocrit (%) | 42.7 (3.1) | 42.7 (3.5) | 0.1 (1.3) | 41.7 (3.6) | 41.1 (4.3) | 0.5 (1.9) | 41.9 (4.1) | 41.9 (5.0) | 0.1 (1.6) | 0.460 | 0.611 |
| MCH (pg) | 29.9 (2.2) | 29.2 (2.2) | 0.7 (2.7) | 30.2 (1.2) | 31.3 (1.7) | 1.1 (1.3) | 29.7 (1.8) | 29.6 (1.8) | 0.1 (0.3) | 0.733 | 0.027 # |
| MCHC (g/dL) | 33.3 (1.3) | 33.4 (1.3) | 0.1 (0.3) | 33.3 (1.1) | 33.4 (1.3) | 0.1 (0.3) | 32.9 (0.9) | 32.6 (0.8) | 0.2 (0.5) | 0.669 | 0.046 # |
| RDW (%) | 12.5 (0.5) | 12.6 (0.7) | 0.1 (0.3) | 12.8 (0.5) | 12.8 (0.5) | 0.1 (0.1) | 13.4 (0.6) | 13.5 (0.6) | 0.1 (0.4) | 0.059 | 0.911 |
| Leukocytes (L) | 7.4 (2.1) | 7.1 (1.9) | 0.2 (1.0) | 6.1 (1.3) | 6.3 (1.1) | 0.2 (1.0) | 6.1 (1.4) | 5.8 (1.1) | 0.3 (0.9) | 0.999 | 0.156 |
| Neutrophils (%) | 62.2 (8.0) | 60.3 (10.1) | 1.8 (5.2) | 63.1 (7.2) | 63.9 (7.7) | 0.9 (5.4) | 61.5 (7.5) | 59.3 (7.4) | 2.1 (4.6) | 0.192 | 0.241 |
| Eosinophils (%) | 2.6 (1.4) | 2.5 (1.4) | 0.1 (0.4) | 2.2 (1.1) | 1.9 (1.1) | 0.2 (0.6) | 2.4 (1.4) | 2.8 (1.1) | 0.37 (1.1) | 0.863 | 0.118 |
| Basophils (%) | 0.5 (0.1) | 0.4 (0.1) | 0.1 (0.1) | 0.6 (0.2) | 0.7 (0.2) | 0.1 (0.2) | 0.6 (0.2) | 0.6 (0.3) | 0.1 (0.2) | 0.691 | 0.138 |
| Lymphocytes (%) | 28.6 (6.3) | 30.4 (9.1) | 1.7 (4.7) | 28.1 (6.9) | 27.1 (7.1) | 0.9 (5.1) | 28.7 (7.2) | 30.3 (8.1) | 1.6 (4.4) | 0.279 | 0.260 |
| Monocytes (%) | 5.9 (1.4) | 6.2 (1.6) | 0.2 (1.3) | 5.9 (1.1) | 6.1 (1.1) | 0.2 (0.6) | 6.7 (1.2) | 6.90 (1.6) | 0.1 (1.1) | 0.303 | 0.967 |
| Platelets (L) | 218.2 (38.0) | 212.8 (35.4) | 5.4 (13.8) | 213.5 (43.3) | 227.4 (31.2) | 13.8 (27.1) | 219.1 (35.2) | 223.2 (35.9) | 4.1 (32.0) | 0.105 | 0.066 |
| Variables | CTRL Group | EH Group | EH+LCHF Group | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | Pre | Post | Δ | Moments | Groups | |
| SBP (mmHg) | 154.7 (20.9) | 142.5 (16.6) | 12.2 (10.2) | 142.3 (18.2) | 124.5 (14.6) | 17.7 (15.6) | 148.0 (18.9) | 126.5 (18.6) | 21.5 (10.6) | <0.001 * | 0.151 |
| DBP (mmHg) | 77.5 (8.1) | 72.2 (7.7) | 5.4 (5.2) | 76.3 (11.7) | 71.8 (12.0) | 4.1 (6.6) | 82.9 (16.3) | 71.4 (8.4) | 9.0 (8.9) | <0.001 * | 0.124 |
| MAP (mmHg) | 107.9 (16.9) | 102.9 (10.2) | 5.0 (13.3) | 98.7 (13.6) | 87.0 (17.8) | 11.7 (15.6) | 107.1 (15.8) | 92.0 (12.1) | 15.1 (12.3) | <0.001 * | 0.158 |
| RHR (bpm) | 68.5 (9.5) | 69.0 (9.7) | 0.5 (5.2) | 64.7 (10.5) | 67.3 (10.1) | 2.4 (8.1) | 62.1 (8.1) | 65.0 (9.5) | 2.8 (8.3) | 0.090 | 0.660 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kindlovits, R.; Sousa, A.C.; Viana, J.L.; Milheiro, J.; Oliveira, B.M.P.M.; Marques, F.; Santos, A.; Teixeira, V.H. Evaluating the Therapeutic Potential of Exercise in Hypoxia and Low-Carbohydrate, High-Fat Diet in Managing Hypertension in Elderly Type 2 Diabetes Patients: A Novel Intervention Approach. Nutrients 2025, 17, 522. https://doi.org/10.3390/nu17030522
Kindlovits R, Sousa AC, Viana JL, Milheiro J, Oliveira BMPM, Marques F, Santos A, Teixeira VH. Evaluating the Therapeutic Potential of Exercise in Hypoxia and Low-Carbohydrate, High-Fat Diet in Managing Hypertension in Elderly Type 2 Diabetes Patients: A Novel Intervention Approach. Nutrients. 2025; 17(3):522. https://doi.org/10.3390/nu17030522
Chicago/Turabian StyleKindlovits, Raquel, Ana Catarina Sousa, João Luís Viana, Jaime Milheiro, Bruno M. P. M. Oliveira, Franklim Marques, Alejandro Santos, and Vitor Hugo Teixeira. 2025. "Evaluating the Therapeutic Potential of Exercise in Hypoxia and Low-Carbohydrate, High-Fat Diet in Managing Hypertension in Elderly Type 2 Diabetes Patients: A Novel Intervention Approach" Nutrients 17, no. 3: 522. https://doi.org/10.3390/nu17030522
APA StyleKindlovits, R., Sousa, A. C., Viana, J. L., Milheiro, J., Oliveira, B. M. P. M., Marques, F., Santos, A., & Teixeira, V. H. (2025). Evaluating the Therapeutic Potential of Exercise in Hypoxia and Low-Carbohydrate, High-Fat Diet in Managing Hypertension in Elderly Type 2 Diabetes Patients: A Novel Intervention Approach. Nutrients, 17(3), 522. https://doi.org/10.3390/nu17030522







