Hydration Responses to Pre-Exercise Sodium Hyperhydration at Rest and During Cycling in the Heat and Across Menstrual Cycle Phases
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Experimental Design and Procedures
2.2.1. Design
2.2.2. Participants
2.2.3. Familiarisation Session
2.2.4. Experimental Sessions
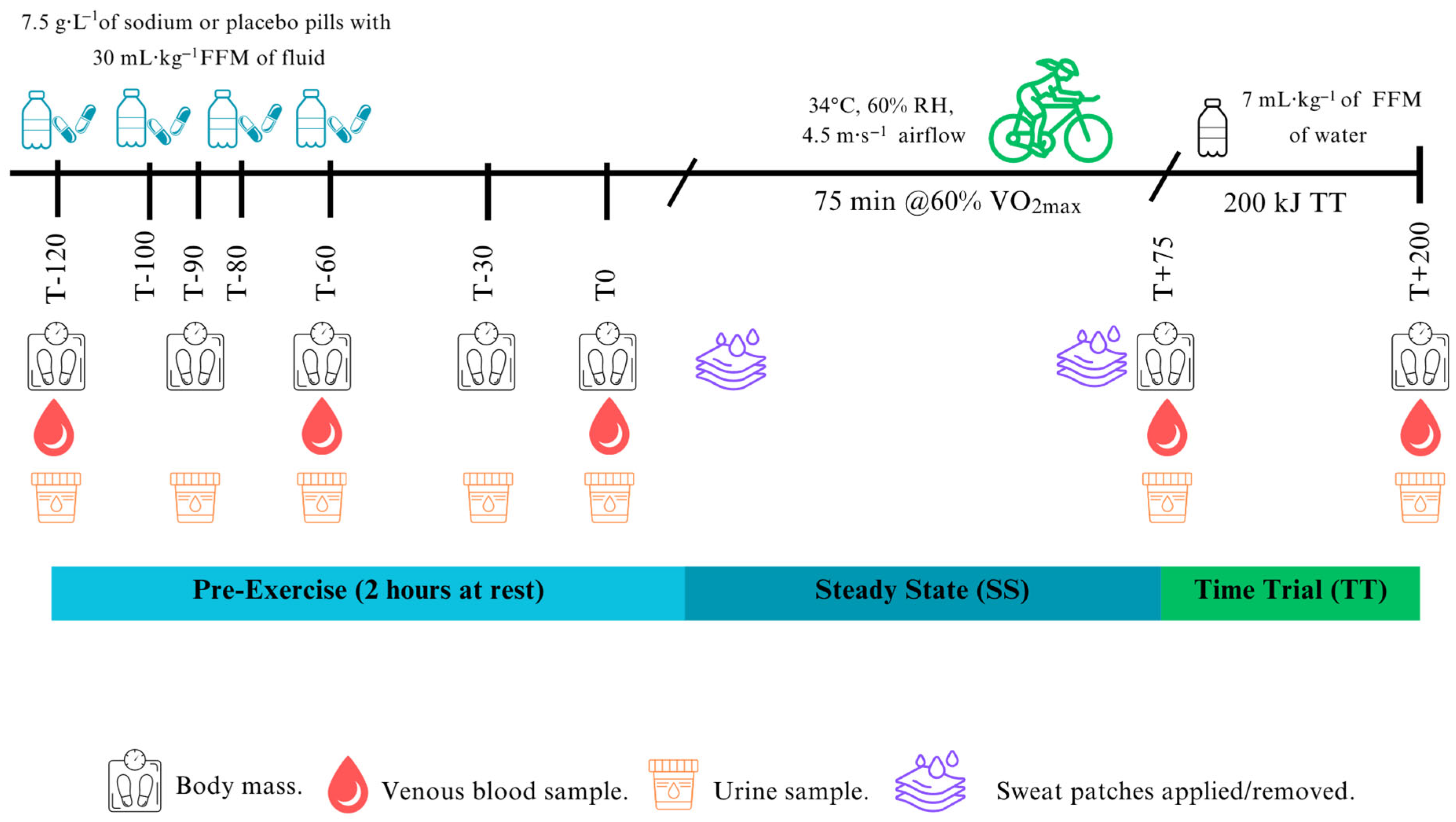
Hyperhydration Protocol
Exercise Protocol
2.2.5. Blood, Urine and Sweat Analysis
2.2.6. Derived Variables
2.3. Sample Size Estimation and Justification
2.4. Statistical Analysis
3. Results
3.1. Participants
3.2. Baseline
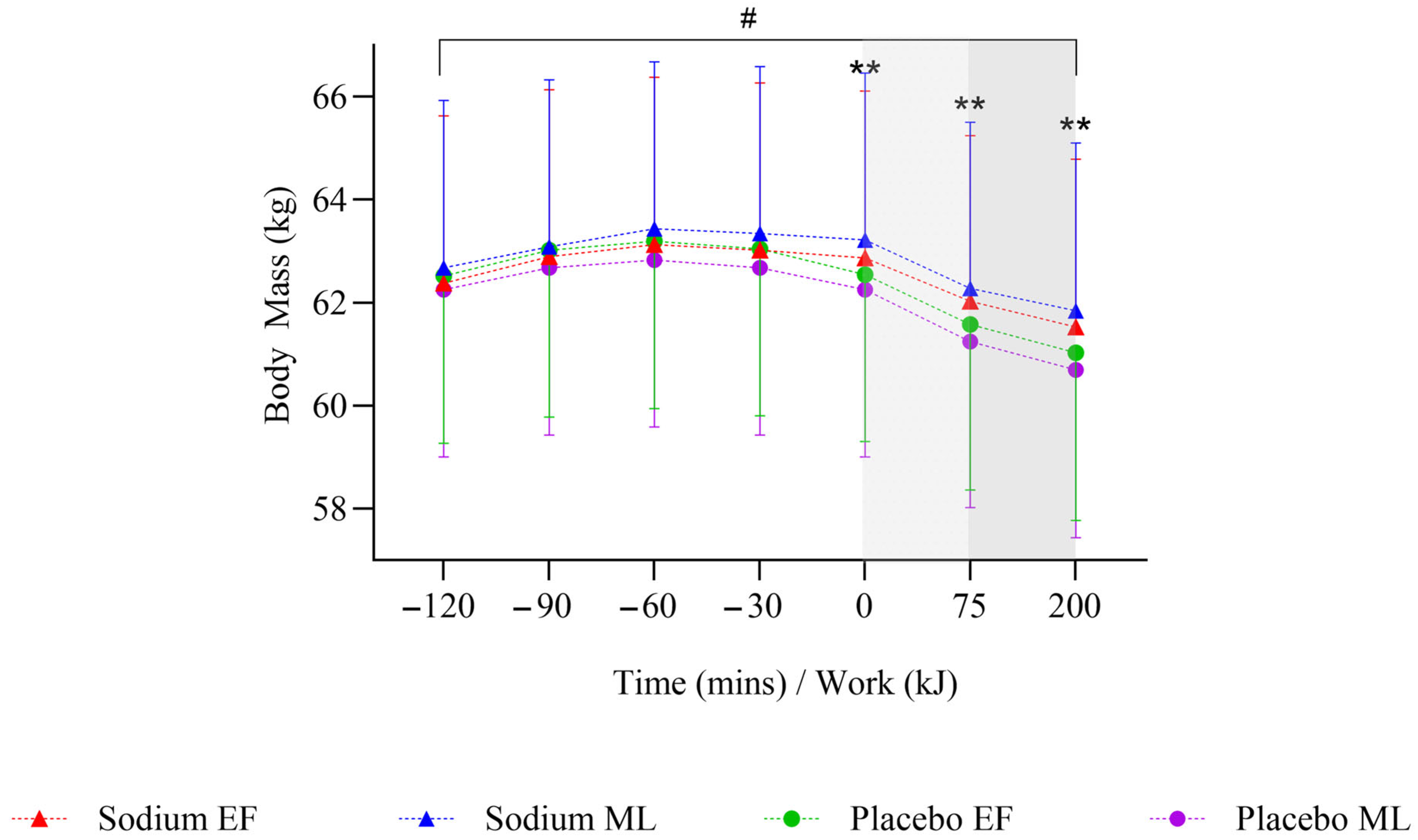
3.3. Pre-Exercise Hyperhydration (At Rest)
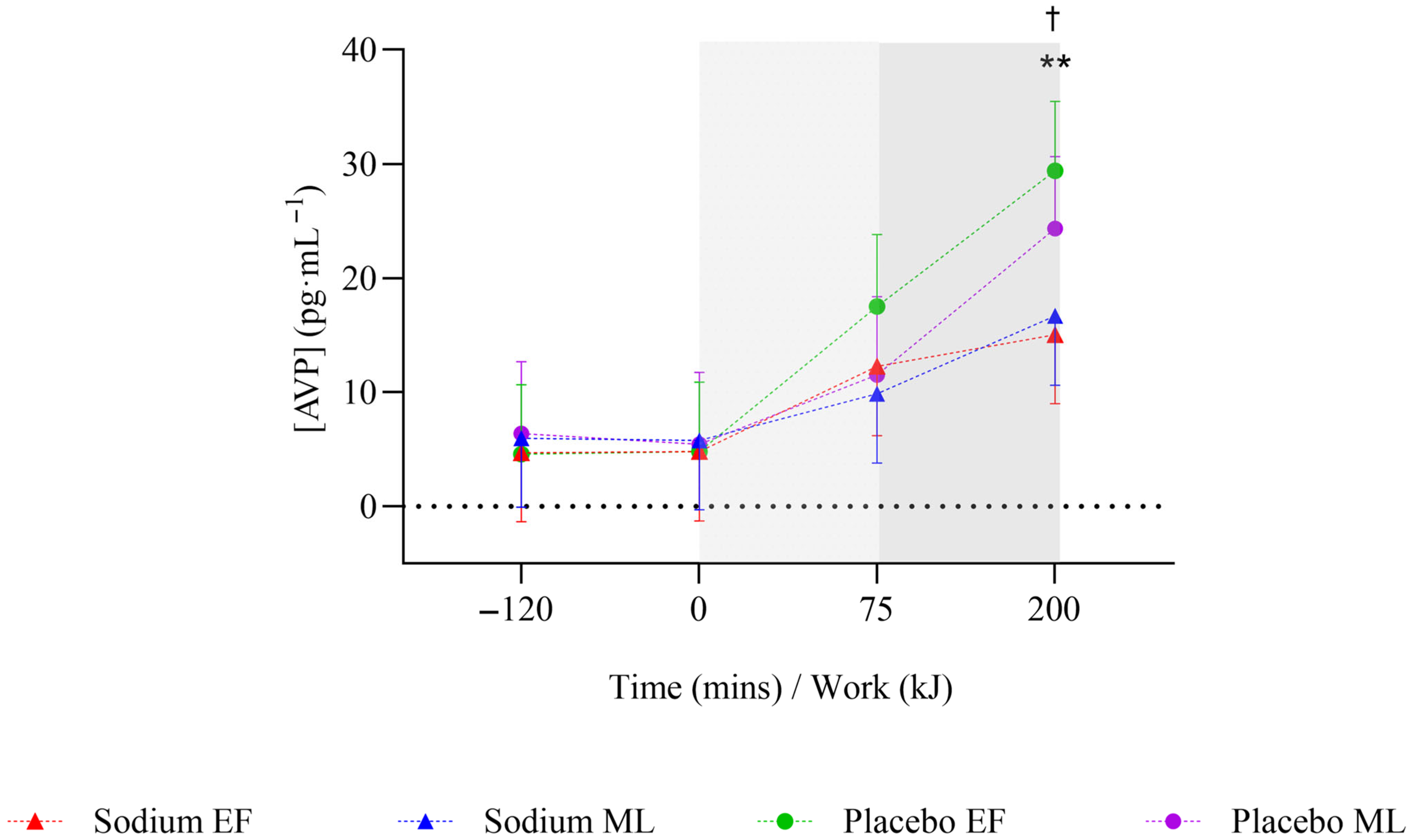
3.4. Steady State
3.5. Time Trial
3.6. Sensitivity Analysis
4. Discussion
4.1. Responses at Rest
4.2. Responses During Exercise
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Von Duvillard, S.P.; Braun, W.A.; Markofski, M.; Beneke, R.; Leithäuser, R. Fluids and hydration in prolonged endurance performance. Nutrition 2004, 20, 651–656. [Google Scholar] [CrossRef]
- Casa, D.J. Exercise in the heat. I. Fundamentals of thermal physiology, performance implications, and dehydration. J. Athl. Train. 1999, 34, 246. [Google Scholar] [PubMed]
- Périard, J.D.; Eijsvogels, T.M.; Daanen, H.A. Exercise under heat stress: Thermoregulation, hydration, performance implications and mitigation strategies. Physiol. Rev. 2021, 101, 1873–1979. [Google Scholar] [CrossRef]
- McCubbin, A.J.; Cort, M.M.; Crawshay, S.T.; Gaskell, S.K.; Jay, O.; Shaw, G.; Allanson, B.A.; Costa, R.J.S.; Desbrow, B.; Hughes, D.; et al. Sports Dietitians Australia Position Statement: Nutrition for Exercise in Hot Environments. Int. J. Sport Nutr. Exerc. Metab. 2020, 30, 83. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.; Deakin, V. Clinical Sports Nutrition, 4th ed.; Sports medicine series; McGraw-Hill: Columbus, OH, USA, 2015. [Google Scholar]
- Shirreffs, S.M.; Armstrong, L.E.; Cheuvront, S.N. Fluid and electrolyte needs for preparation and recovery from training and competition. In Food, Nutrition and Sports Performance II; Taylor & Francis: London, UK, 2004; Volume 22, pp. 57–63. [Google Scholar]
- Armstrong, L.E.; Curtis, W.C.; Hubbard, R.W.; Francesconi, R.P.; Moore, R.; Askew, E.W. Symptomatic hyponatremia during prolonged exercise in heat. Med. Sci. Sports Exerc. 1993, 25, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Rondon-Berrios, H.; Agaba, E.I.; Tzamaloukas, A.H. Hyponatremia: Pathophysiology, classification, manifestations and management. Int. Urol. Nephrol. 2014, 46, 2153–2165. [Google Scholar] [CrossRef]
- Goulet, E.D.; De La Flore, A.; Savoie, F.A.; Gosselin, J. Salt+ Glycerol-Induced Hyperhydration Enhances Fluid Retention more than salt -or glycerol- induced hyperhydration. Int. J. Sport Nutr. 2018, 28, 246–252. [Google Scholar] [CrossRef]
- Goulet, E.D.B. Glycerol-induced hyperhydration: A method for estimating the optimal load of fluid to be ingested before exercise to maximize endurance performance. J. Strength Cond. Res. 2010, 24, 74–78. [Google Scholar] [CrossRef]
- Savoie, F.A.; Dion, T.; Asselin, A.; Goulet, E.D.B. Sodium-induced hyperhydration decreases urine output and improves fluid balance compared with glycerol- and water-induced hyperhydration. Appl. Physiol. Nutr. Metab. 2015, 40, 51–58. [Google Scholar] [CrossRef]
- Nelson, D.L.; Cox, M.M.; Lehninger, A.L. Principles of Biochemistry; Freeman New York: New York, NY, USA, 2008. [Google Scholar]
- Greenleaf, J.E. Problem: Thirst, drinking behavior, and involuntary dehydration. Med. Sci. Sports Exerc. 1992, 24, 645–656. [Google Scholar] [CrossRef]
- Goulet, E. Pre-exercise hyperhydration: Comments on the 2007 acsm position stand on exercise and fluid replacement. J. Exerc. Physiol. Online 2008, 11, 64–74. [Google Scholar]
- Goulet, E.D.; Rousseau, S.F.; Lamboley, C.R.; Plante, G.E.; Dionne, I.J. Pre-exercise hyperhydration delays dehydration and improves endurance capacity during 2 h of cycling in a temperate climate. J. Physiol. Anthropol. 2008, 27, 263–271. [Google Scholar] [CrossRef]
- Sims, S.T.; Rehrer, N.J.; Cotter, J.D.; Bell, M.L. Preexercise sodium loading aids fluid balance and endurance for women exercising in the heat. J. Appl. Physiol. 2007, 103, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Elliott-Sale, K.J.; Minahan, C.L.; de Jonge, X.A.K.J.; Ackerman, K.E.; Sipilä, S.; Constantini, N.W.; Lebrun, C.M.; Hackney, A.C. Methodological Considerations for Studies in Sport and Exercise Science with Women as Participants: A Working Guide for Standards of Practice for Research on Women. Sports Med. 2021, 51, 843. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B. Hydration in Physically Active Women. Sports Sci. Exch. 2023, 36, 1–10. [Google Scholar]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar]
- Burke, L.M. Practical Issues in Evidence-Based Use of Performance Supplements: Supplement Interactions, Repeated Use and Individual Responses. Sports Med. 2017, 47, 79–100. [Google Scholar] [CrossRef]
- Stachenfeld, N.S. Sex hormone effects on body fluid regulation. Exerc. Sport Sci. Rev. 2008, 36, 152. [Google Scholar] [CrossRef]
- Nose, Y.; Fujita, K.; Wada, T.; Nishimura, K.; Hakoda, M. Effects of menstrual cycle phase on fluid regulation during walking exercise. J. Sports Sci. Med. 2020, 19, 556–563. [Google Scholar]
- Stachenfeld, N.S.; Taylor, H.S. Sex hormone effects on body fluid and sodium regulation in women with and without exercise-associated hyponatremia. J. Appl. Physiol. 2009, 107, 864–872. [Google Scholar] [CrossRef]
- Convit, L.; Orellana, L.; Périard, J.D.; Carr, A.J.; Warmington, S.; Beaugeois, M.; Abraham, A.; Snipe, R.M. Sodium Hyperhydration Improves Performance With No Change in Thermal and Cardiovascular Strain in Female Cyclists Exercising in the Heat Across the Menstrual Cycle. Int. J. Sport Nutr. Exerc. Metab. 2025, 35, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, A.; Fujii, N.; Tsuji, B.; Watanabe, K.; Niwa, T.; Nishiyasu, T. Hypervolemia induced by fluid ingestion at rest: Effect of sodium concentration. Eur. J. Appl. Physiol. 2014, 114, 2139–2145. [Google Scholar] [CrossRef] [PubMed]
- Savoie, F.A.; Asselin, A.; Goulet, E.D.B. Comparison of sodium chloride tablets--induced, sodium chloride solution-induced, and glycerol-induced hyperhydration on fluid balance responses in healthy men. J. Strength Cond. Res. 2016, 30, 2880–2891. [Google Scholar] [CrossRef]
- Earhart, E.L.; Weiss, E.P.; Rahman, R.; Kelly, P.V. Effects of oral sodium supplementation on indices of thermoregulation in trained, endurance athletes. J. Sports Sci. Med. 2015, 14, 172–178. [Google Scholar]
- McKay, A.K.; Stellingwerff, T.; Smith, E.S.; Martin, D.T.; Mujika, I.; Goosey-Tolfrey, V.L.; Sheppard, J.; Burke, L.M. Defining training and performance caliber: A participant classification framework. Int. J. Sports Physiol. Perform. 2021, 17, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Decroix, L.; De Pauw, K.; Foster, C.; Meeusen, R. Guidelines to classify female subject groups in sport-science research. Int. J. Sports Physiol. Perform. 2016, 11, 204–213. [Google Scholar] [CrossRef]
- Commonwealth of Australia BoM. Climate Statistics for Australian Location. Summary Statistics Melbourne Regional Office. Period 1991–2020. Available online: https://www.bom.gov.au/climate/averages/tables/cw_086071.shtml (accessed on 17 January 2025).
- Janse de Jonge, X.; Thompson, B.; Han, A. Methodological Recommendations for Menstrual Cycle Research in Sports and Exercise. Med. Sci. Sports Exerc. 2019, 51, 2610–2617. [Google Scholar] [CrossRef]
- Janse de Jonge, X.; Thompson, M.W.; Chuter, V.H.; Silk, L.N.; Thom, J.M. Exercise performance over the menstrual cycle in temperate and hot, humid conditions. Med. Sci. Sports Exerc. 2012, 44, 2190–2198. [Google Scholar] [CrossRef]
- Schaumberg, M.A.; Jenkins, D.G.; de Jonge, X.A.J.; Emmerton, L.M.; Skinner, T.L. Three-step method for menstrual and oral contraceptive cycle verification. J. Sci. Med. Sport 2017, 20, 965–969. [Google Scholar] [CrossRef]
- Tanner, R.; Gore, C. Physiological Tests for Elite Athletes; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Rodriguez-Giustiniani, P.; Rodriguez-Sanchez, N.; Galloway, S.D. Fluid and electrolyte balance considerations for female athletes. Eur. J. Sport Sci. 2022, 22, 697–708. [Google Scholar] [CrossRef]
- Pickering, C.; Kiely, J. What should we do about habitual caffeine use in athletes? Sports Med. 2019, 49, 833–842. [Google Scholar] [CrossRef]
- Morris, D.M.; Huot, J.R.; Jetton, A.M.; Collier, S.R.; Utter, A.C. Acute Sodium Ingestion Before Exercise Increases Voluntary Water Consumption Resulting in Preexercise Hyperhydration and Improvement in Exercise Performance in the Heat. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 456. [Google Scholar] [CrossRef]
- Che Jusoh, M.; Morton, R.; Stannard, S.; Mündel, T. A reliable preloaded cycling time trial for use in conditions of significant thermal stress. Scand. J. Med. Sci. Sports 2015, 25, 296–301. [Google Scholar] [CrossRef]
- Baker, L.B.; Ungaro, C.T.; Barnes, K.A.; Nuccio, R.P.; Reimel, A.J.; Stofan, J.R. Validity and reliability of a field technique for sweat Na+ and K+ analysis during exercise in a hot-humid environment. Physiol. Rep. 2014, 2, e12007. [Google Scholar] [CrossRef] [PubMed]
- Jardine, W.T.; Aisbett, B.; Kelly, M.K.; Burke, L.M.; Ross, M.L.; Condo, D.; Périard, J.D.; Carr, A.J. The Effect of Pre-Exercise Hyperhydration on Exercise Performance, Physiological Outcomes and Gastrointestinal Symptoms: A Systematic Review. Sports Med. 2023, 53, 2111–2134. [Google Scholar] [CrossRef] [PubMed]
- Costill, D.; Fink, W. Plasma volume changes following exercise and thermal dehydration. J. Appl. Physiol. 1974, 37, 521–525. [Google Scholar] [CrossRef]
- Barley, O.R.; Chapman, D.W.; Abbiss, C.R. Reviewing the current methods of assessing hydration in athletes. J. Int. Soc. Sports Nutr. 2020, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.J.; Galloway, S.D.; Nimmo, M.A. Variations in regional sweat composition in normal human males. Exp. Physiol. 2000, 85, 869–875. [Google Scholar] [CrossRef]
- Gelman, A. Data Analysis Using Regression and Multilevel/Hierarchical Models; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Sims, S.T.; Rehrer, N.J.; Bell, M.L.; Cotter, J.D. Endogenous and exogenous female sex hormones and renal electrolyte handling: Effects of an acute sodium load on plasma volume at rest. J. Appl. Physiol. 2008, 105, 121–127. [Google Scholar] [CrossRef]
- Szmuilowicz, E.D.; Adler, G.K.; Williams, J.S.; Green, D.E.; Yao, T.M.; Hopkins, P.N.; Seely, E.W. Relationship between Aldosterone and Progesterone in the Human Menstrual Cycle. J. Clin. Endocrinol. Metab. 2006, 91, 3981–3987. [Google Scholar] [CrossRef]
- Baker, F.C.; Siboza, F.; Fuller, A. Temperature regulation in women: Effects of the menstrual cycle. Temperature 2020, 7, 226–262. [Google Scholar] [CrossRef] [PubMed]
- Janse de Jonge, X. Effects of the menstrual cycle on exercise performance. Sports Med. 2003, 33, 833–851. [Google Scholar] [CrossRef]
- Giersch, G.E.; Morrissey, M.C.; Katch, R.K.; Colburn, A.T.; Sims, S.T.; Stachenfeld, N.S.; Casa, D.J. Menstrual cycle and thermoregulation during exercise in the heat: A systematic review and meta-analysis. J. Sci. Med. Sport 2020, 23, 1134–1140. [Google Scholar] [CrossRef]
- Vokes, T.; Weiss, N.; Schreiber, J.; Gaskill, M.; Robertson, G. Osmoregulation of thirst and vasopressin during normal menstrual cycle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1988, 254, R641–R647. [Google Scholar] [CrossRef]
- Sims, S.T.; Van Vliet, L.; Cotter, J.D.; Rehrer, N.J. Sodium loading aids fluid balance and reduces physiological strain of trained men exercising in the heat. Med. Sci. Sports Exerc. 2007, 39, 123–130. [Google Scholar] [CrossRef]
- Stachenfeld, N.S.; Keefe, D.L. Estrogen effects on osmotic regulation of AVP and fluid balance. Am. J. Physiol. Endocrinol. Metab. 2002, 283, E711–E721. [Google Scholar] [CrossRef]
- Stachenfeld, N.S.; Taylor, H.S. Effects of estrogen and progesterone administration on extracellular fluid. J. Appl. Physiol. 2004, 96, 1011–1018. [Google Scholar] [CrossRef]
- Sawka, M.N.; Coyle, E.F. Influence of body water and blood volume on thermoregulation and exercise performance in the heat. Exerc. Sport Sci. Rev. 1999, 27, 167–218. [Google Scholar] [CrossRef] [PubMed]
- Sawka, M.N.; Cheuvront, S.N.; Kenefick, R.W. Hypohydration and human performance: Impact of environment and physiological mechanisms. Sports Med. 2015, 45, 51–60. [Google Scholar] [CrossRef]
- Stachenfeld, N.S.; Keefe, D.L.; Palter, S.F. Estrogen and progesterone effects on transcapillary fluid dynamics. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001, 281, R1319–R1329. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T.; Loi, V.; Pani, A.; Rosner, M.H. Exercise-associated hyponatremia: 2017 update. Front. Med. 2017, 4, 21. [Google Scholar] [CrossRef]
- Hew-Butler, T. Arginine vasopressin, fluid balance and exercise: Is exercise-associated hyponatraemia a disorder of arginine vasopressin secretion? Sports Med. 2010, 40, 459–479. [Google Scholar] [CrossRef] [PubMed]
- Christ-Crain, M. Vasopressin and Copeptin in health and disease. Rev. Endocr. Metab. Disord. 2019, 20, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Morgenthaler, N.G.; Struck, J.; Jochberger, S.; Dünser, M.W. Copeptin: Clinical use of a new biomarker. Trends Endocrinol. Metab. 2008, 19, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, J.P.; Terker, A.S.; Zuchowski, Y.; Watts, J.A.; Bock, F.; Meyer, C.; Luo, W.; Kapp, M.E.; Gould, E.R.; Miranda, A.X. Kidney collecting duct cells make vasopressin in response to NaCl-induced hypertonicity. JCI Insight 2022, 7, e161765. [Google Scholar] [CrossRef]
- Agorastos, A.; Sommer, A.; Heinig, A.; Wiedemann, K.; Demiralay, C. Vasopressin surrogate marker copeptin as a potential novel endocrine biomarker for antidepressant treatment response in major depression: A pilot study. Front. Psychiatry 2020, 11, 453. [Google Scholar] [CrossRef]

| No-LPD (n = 8) | LPD (n = 4) | |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Age (years) | 35 ± 5 | 31 ± 1 |
| Height (cm) | 167 ± 7 | 160 ± 1 |
| Body mass (kg) | 61.7 ± 6.6 | 63.5 ± 6.1 |
| Fat-free mass (kg) | 46.2 ± 4.9 | 46.6 ± 4.0 |
| Body fat (%) | 27.1 ± 4.8 | 27.3 ± 1.2 |
| BSA (m2) | 6.9 ± 0.5 | 6.8 ± 0.5 |
| VO2peak (mL·kg−1 BM·min−1) | 56.6 ± 5.6 | 47.2 ± 8.7 |
| Baseline | Pre-Exercise (2 h at Rest) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sodium | Placebo | Difference p-Value | Interaction p-Value | Sodium | Placebo | Difference p-Value | Interaction p-Value | ||
| Hydration Outcomes | |||||||||
| Fluid retention (mL) | Overall | - | - | - | - | 616.1 (443.5, 788.8) | 109.2 (−65.4, 283.7) | <0.001 | - |
| EF | - | - | - | - | 568.3 (362.7, 774) | 153.1 (−52.6, 358.8) | <0.001 | 0.252 | |
| ML | - | - | - | 666 (460.3, 871.7) | 63.3 (−149, 275.7) | <0.001 | |||
| Ingested fluid retained (%) | Overall | - | - | - | - | 44.4 (31.8, 57.0) | 7.6 (−5.1, 20.4) | <0.001 | - |
| EF | - | - | - | - | 40.5 (25.5, 55.6) | 10.8 (−4.2, 25.9) | <0.001 | 0.230 | |
| ML | - | - | - | 48.5 (33.4, 63.5) | 4.3 (−11.2, 19.9) | <0.001 | |||
| Urine Outcomes | |||||||||
| Urine Specific Gravity (au) | Overall | 1.015 (1.012, 1.018) | 1.013 (1.010, 1.016) | 0.340 | - | 1.007 (1.006, 1.008) | 1.005 (1.004, 1.006) | <0.001 | - |
| EF | 1.014 (1.010, 1.018) | 1.013 (1.009, 1.017) | 0.588 | 0.840 | 1.007 (1.006, 1.008) | 1.005 (1.004, 1.006) | 0.021 | 0.729 | |
| ML | 1.016 (1.012, 1.019) | 1.014 (1.010, 1.018) | 0.420 | 1.008 (1.006, 1.009) | 1.005 (1.004, 1.007) | 0.005 | |||
| Urine osmolality (mOsm·kgH2O−1) | Overall | 556 (436, 676) | 483 (359, 608) | 0.207 | - | 298.5 (255.6, 341.3) | 206.2 (163.1, 249.3) | <0.001 | - |
| EF | 541 (400, 683) | 481 (335, 628) | 0.448 | 0.829 | 288.5 (236.5, 340.5) | 207.7 (156.3, 259.1) | 0.007 | 0.604 | |
| ML | 570 (428, 712) | 486 (334, 637) | 0.301 | 308.7 (257.6, 359.8) | 204.6 (151.9, 257.3) | 0.001 | |||
| Urine Volume (mL) | Overall | 49.7 (32.4, 67.1) | 51.6 (32.7, 70.5) | 0.874 | - | 185.4 (144.6, 226.2) | 293.1 (251.9, 334.3) | <0.001 | - |
| EF | 54.1 (30.9, 77.3) | 60.4 (35, 85.8) | 0.705 | 0.722 | 204.4 (154.9, 253.8) | 289.9 (240.7, 339.2) | 0.003 | 0.257 | |
| ML | 45.3 (22.1, 68.5) | 43.3 (17.9, 68.6) | 0.902 | 166.9 (118.2, 215.7) | 296.3 (246, 346.7) | <0.001 | |||
| Urine Sodium (ppm) | Overall | 1525 (1139, 1910) | 1274 (868, 1680) | 0.255 | - | 989.4 (821.6, 1157.1) | 530.3 (360.8, 699.9) | <0.001 | - |
| EF | 1344 (871, 1817) | 1408 (917, 1899) | 0.830 | 0.127 | 891.5 (680, 1103) | 586.3 (376.6, 796) | 0.020 | 0.109 | |
| ML | 1705 (1232, 2178) | 1123 (611, 1635) | 0.057 | 1090 (881.5, 1298.5) | 473.8 (257.6, 690) | <0.001 | |||
| Steady State Cycling | Cycling Time Trial | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sodium | Placebo | Difference p-Value | Interaction p-Value | Sodium | Placebo | Difference p-Value | Interaction p-Value | ||
| Hydration Outcomes | |||||||||
| Body Mass Loss (%) | Overall | 1.38 (1.21, 1.54) | 1.58 (1.41, 1.75) | 0.001 | - | 0.77 (0.59, 0.96) | 0.91 (0.73, 1.1) | 0.037 | - |
| EF | 1.31 (1.12, 1.5) | 1.57 (1.38, 1.76) | 0.004 | 0.395 | 0.82 (0.61, 1.03) | 0.92 (0.71, 1.13) | 0.332 | 0.466 | |
| ML | 1.44 (1.25, 1.63) | 1.59 (1.4, 1.79) | 0.105 | 0.72 (0.51, 0.92) | 0.91 (0.7, 1.13) | 0.050 | |||
| Sweat Rate (L·h−1) | Overall | 0.60 (0.52, 0.68) | 0.68 (0.61, 0.76) | 0.001 | - | 2.09 (1.80, 2.37) | 2.12 (1.84, 2.41) | 0.739 | - |
| EF | 0.57 (0.49, 0.66) | 0.67 (0.58, 0.75) | 0.003 | 0.457 | 2.16 (1.84, 2.48) | 2.12 (1.79, 2.44) | 0.788 | 0.479 | |
| ML | 0.64 (0.55, 0.72) | 0.70 (0.61, 0.79) | 0.062 | 2.01 (1.68, 2.33) | 2.13 (1.80, 2.46) | 0.468 | |||
| Sweat Sodium (ppm) | Overall | 1530 (1316, 1744) | 1430 (1215, 1646) | 0.109 | - | - | - | - | - |
| EF | 1551 (1321, 1782) | 1433 (1203, 1663) | 0.169 | 0.754 | - | - | - | - | |
| ML | 1507 (1277, 1737) | 1427 (1194, 1661) | 0.368 | - | - | - | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Convit, L.; Orellana, L.; Périard, J.D.; Carr, A.J.; Warmington, S.; Mruthunjaya, A.K.V.; Torriero, A.A.J.; Snipe, R.M.J. Hydration Responses to Pre-Exercise Sodium Hyperhydration at Rest and During Cycling in the Heat and Across Menstrual Cycle Phases. Nutrients 2025, 17, 3672. https://doi.org/10.3390/nu17233672
Convit L, Orellana L, Périard JD, Carr AJ, Warmington S, Mruthunjaya AKV, Torriero AAJ, Snipe RMJ. Hydration Responses to Pre-Exercise Sodium Hyperhydration at Rest and During Cycling in the Heat and Across Menstrual Cycle Phases. Nutrients. 2025; 17(23):3672. https://doi.org/10.3390/nu17233672
Chicago/Turabian StyleConvit, Lilia, Liliana Orellana, Julien D. Périard, Amelia J. Carr, Stuart Warmington, Ashwin K. V. Mruthunjaya, Angel A. J. Torriero, and Rhiannon M. J. Snipe. 2025. "Hydration Responses to Pre-Exercise Sodium Hyperhydration at Rest and During Cycling in the Heat and Across Menstrual Cycle Phases" Nutrients 17, no. 23: 3672. https://doi.org/10.3390/nu17233672
APA StyleConvit, L., Orellana, L., Périard, J. D., Carr, A. J., Warmington, S., Mruthunjaya, A. K. V., Torriero, A. A. J., & Snipe, R. M. J. (2025). Hydration Responses to Pre-Exercise Sodium Hyperhydration at Rest and During Cycling in the Heat and Across Menstrual Cycle Phases. Nutrients, 17(23), 3672. https://doi.org/10.3390/nu17233672









