The Role of Diet in Women of Childbearing Age: Current Evidence Supporting Nutritional Recommendations
Abstract
1. Introduction
2. Nutritional Recommendations for Women of Childbearing Age
2.1. Importance of Nutritional Balance and Dietary Variety
2.2. Essential Macronutrients: Proteins, Carbohydrates, and Fats
2.3. Key Micronutrients: Vitamins and Minerals
2.4. Role of Dietary Supplements in Supporting Reproductive Health
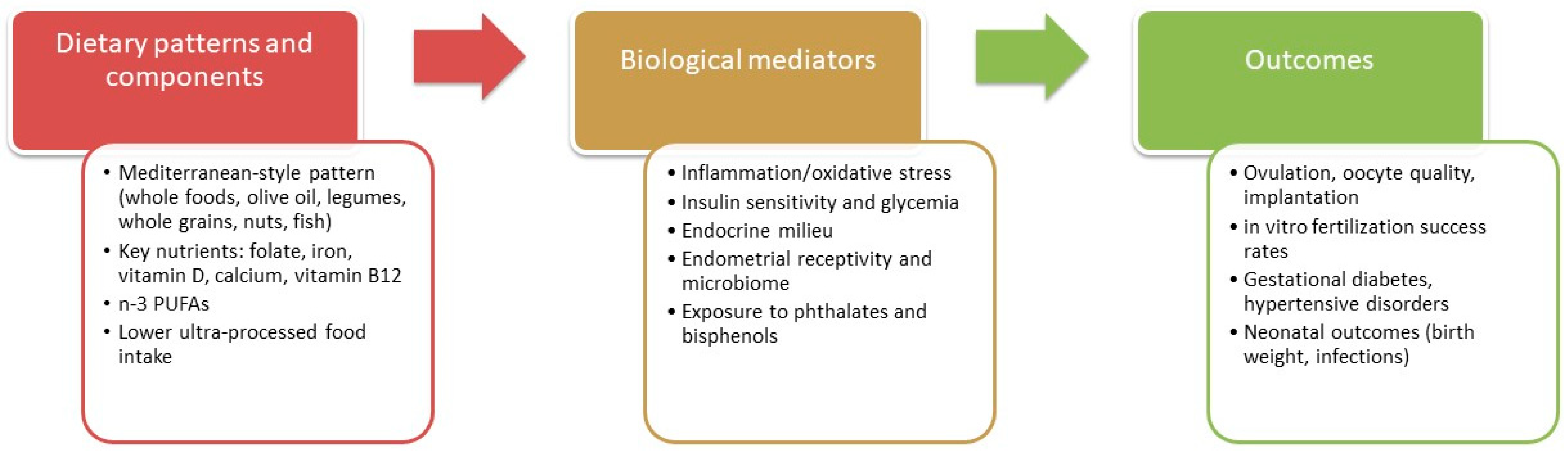
3. Impact of Dietary Patterns
3.1. Mediterranean Diet and Its Benefits
3.2. Comparison with Other Dietary Patterns
3.3. Importance of Preconception Nutrition
4. The Potential Role of Ultra-Processed Foods
5. Dietary Implications for General Health
5.1. Physiological Factors Influenced by Diet
5.2. Impact on Obesity and Weight Management
5.3. Cardiovascular Health Considerations
5.3.1. Glycemic Profile
5.3.2. Lipid Profile
5.3.3. Blood Pressure
5.4. Diet and Bone Health
5.4.1. Factors Influencing Bone Mass
5.4.2. Bone Health in Women of Childbearing Age
5.4.3. Mediterranean Diet and Bone Health
6. Diet and Reproductive Health
6.1. Influence of Diet on Menstrual Cycle
6.2. Hormonal Regulation and Fertility
6.3. Nutrients Essential for Promoting Fertility
6.4. Dietary Strategies to Optimize Reproductive Health
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lecorguillé, M.; Camier, A.; Kadawathagedara, M. Weight Changes, Nutritional Intake, Food Contaminants, and Supplements in Women of Childbearing Age, including Pregnant Women: Guidelines for Interventions during the Perinatal Period from the French National College of Midwives. J. Midwifery Womens Health 2022, 67 (Suppl. S1), S135–S148. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Grant, F.; Goldenberg, T.; Zongrone, A.; Martorell, R. Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: A systematic review. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. S1), 285–301. [Google Scholar] [CrossRef]
- Reifsnider, E.; Gill, S.L. Nutrition for the childbearing years. J. Obstet. Gynecol. Neonatal Nurs. 2000, 29, 43–55. [Google Scholar] [CrossRef]
- Islam, M.H.; Nayan, M.M.; Jubayer, A.; Amin, M.R. A review of the dietary diversity and micronutrient adequacy among the women of reproductive age in low- and middle-income countries. Food Sci. Nutr. 2024, 12, 1367–1379. [Google Scholar] [CrossRef]
- FAO. Minimum Dietary Diversity for Women (MDD-W). Rome: Food and Agriculture Organization of the United Nations. 2024. Available online: https://www.fao.org/nutrition/assessment/tools/minimum-dietary-diversity-women/en/ (accessed on 1 October 2025).
- Tareke, A.A.; Melak, E.G.; Mengistu, B.K.; Hussen, J.; Molla, A. Association between maternal dietary diversity during pregnancy and birth outcomes: Evidence from a systematic review and meta-analysis. BMC Nutr. 2024, 10, 151. [Google Scholar] [CrossRef]
- Gómez, G.; Nogueira Previdelli, Á.; Fisberg, R.M.; Kovalskys, I.; Fisberg, M.; Herrera-Cuenca, M.; Cortés Sanabria, L.Y.; Yépez García, M.C.; Rigotti, A.; Liria-Domínguez, M.R.; et al. Dietary Diversity and Micronutrients Adequacy in Women of Childbearing Age: Results from ELANS Study. Nutrients 2020, 12, 1994. [Google Scholar] [CrossRef]
- Devarshi, P.P.; Legette, L.L.; Grant, R.W.; Mitmesser, S.H. Total estimated usual nutrient intake and nutrient status biomarkers in women of childbearing age and women of menopausal age. Am. J. Clin. Nutr. 2021, 113, 1042–1052. [Google Scholar] [CrossRef]
- Lander, R.L.; Hambidge, K.M.; Westcott, J.E.; Tejeda, G.; Diba, T.S.; Mastiholi, S.C.; Khan, U.S.; Garcés, A.; Figueroa, L.; Tshefu, A.; et al. Pregnant Women in Four Low-Middle Income Countries Have a High Prevalence of Inadequate Dietary Intakes That Are Improved by Dietary Diversity. Nutrients 2019, 11, 1560. [Google Scholar] [CrossRef] [PubMed]
- Ziso, D.; Chun, O.K.; Puglisi, M.J. Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities. Nutrients 2022, 14, 2278. [Google Scholar] [CrossRef]
- Chen, Y.; Michalak, M.; Agellon, L.B. Importance of Nutrients and Nutrient Metabolism on Human Health. Yale J. Biol. Med. 2018, 91, 95–103. [Google Scholar]
- Herring, C.M.; Bazer, F.W.; Johnson, G.A.; Wu, G. Impacts of maternal dietary protein intake on fetal survival, growth, and development. Exp. Biol. Med. 2018, 243, 525–533. [Google Scholar] [CrossRef]
- Lowensohn, R.I.; Stadler, D.D.; Naze, C. Current Concepts of Maternal Nutrition. Obstet. Gynecol. Surv. 2016, 71, 413–426. [Google Scholar] [CrossRef]
- Lapolla, A.; Dalfrà, M.G.; Marelli, G.; Parrillo, M.; Sciacca, L.; Sculli, M.A.; Succurro, E.; Torlone, E.; Vitacolonna, E. Medical nutrition therapy in physiological pregnancy and in pregnancy complicated by obesity and/or diabetes: SID-AMD recommendations. Acta Diabetol. 2025; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Hart, T.L.; Petersen, K.S.; Kris-Etherton, P.M. Nutrition recommendations for a healthy pregnancy and lactation in women with overweight and obesity—Strategies for weight loss before and after pregnancy. Fertil. Steril. 2022, 118, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Miketinas, D.; Luo, H.; Firth, J.A.; Bailey, A.; Bender, T.; Gross, G.; Brink, L. Macronutrient and Micronutrient Intake Among US Women Aged 20 to 44 Years. JAMA Netw. Open 2024, 7, e2438460. [Google Scholar] [CrossRef]
- Xue, L.; Chen, X.; Sun, J.; Fan, M.; Qian, H.; Li, Y.; Wang, L. Maternal Dietary Carbohydrate and Pregnancy Outcomes: Quality over Quantity. Nutrients 2024, 16, 2269. [Google Scholar] [CrossRef]
- Andreu, A.; Casals, G.; Vinagre, I.; Flores, L. Obesity management in women of reproductive age. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2023, 70 (Suppl. S1), 85–94. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization of the United Nations. Fats and Fatty Acids in Human Nutrition; Report of an expert consultation; FAO Food and Nutrition Paper; Food and Agriculture Organization of the United Nations: Rome, Italy, 2010; Volume 91, pp. 1–166. [Google Scholar]
- Cetin, I.; Carlson, S.E.; Burden, C.; da Fonseca, E.B.; di Renzo, G.C.; Hadjipanayis, A.; Harris, W.S.; Kumar, K.R.; Olsen, S.F.; Mader, S.; et al. Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth. Am. J. Obstet. Gynecol. MFM 2024, 6, 101251. [Google Scholar] [CrossRef]
- Trop-Steinberg, S.; Gal, M.; Azar, Y.; Kilav-Levin, R.; Heifetz, E.M. Effect of omega-3 supplements or diets on fertility in women: A meta-analysis. Heliyon 2024, 10, e29324. [Google Scholar] [CrossRef]
- Zaçe, D.; La Gatta, E.; Petrella, L.; Orfino, A.; Viteritti, A.M.; Di Pietro, M.L. Diet and lifestyles of young women of childbearing age: An Italian survey. Ann. Dell’istituto Super. Sanità 2024, 60, 89–97. [Google Scholar] [CrossRef]
- Milman, N.; Taylor, C.L.; Merkel, J.; Brannon, P.M. Iron status in pregnant women and women of reproductive age in Europe. Am. J. Clin. Nutr. 2017, 106, 1655S–1662S. [Google Scholar] [CrossRef] [PubMed]
- Peña-Rosas, J.P.; De-Regil, L.M.; Garcia-Casal, M.N.; Dowswell, T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2015, 2015, CD004736. [Google Scholar] [CrossRef]
- Busso, D.; David, A.; Penailillo, R.; Echeverría, G.; Rigotti, A.; Kovalskys, I.; Gómez, G.; Cortés Sanabria, L.Y.; Yépez García, M.C.; Pareja, R.G.; et al. Intake of Vitamin E and C in Women of Reproductive Age: Results from the Latin American Study of Nutrition and Health (ELANS). Nutrients 2021, 13, 1954. [Google Scholar] [CrossRef]
- Tinker, S.C.; Cogswell, M.E.; Devine, O.; Berry, R.J. Folic acid intake among U.S. women aged 15-44 years, National Health and Nutrition Examination Survey, 2003–2006. Am. J. Prev. Med. 2010, 38, 534–542. [Google Scholar] [CrossRef]
- Pop, M.S.; Cheregi, D.C.; Onose, G.; Munteanu, C.; Popescu, C.; Rotariu, M.; Turnea, M.A.; Dogaru, G.; Ionescu, E.V.; Oprea, D.; et al. Exploring the Potential Benefits of Natural Calcium-Rich Mineral Waters for Health and Wellness: A Systematic Review. Nutrients 2023, 15, 3126. [Google Scholar] [CrossRef]
- Willemse, J.P.M.M.; Meertens, L.J.E.; Scheepers, H.C.J.; Achten, N.M.J.; Eussen, S.J.; van Dongen, M.C.; Smits, L.J.M. Calcium intake from diet and supplement use during early pregnancy: The Expect study I. Eur. J. Nutr. 2020, 59, 167–174. [Google Scholar] [CrossRef]
- da Silveira, E.A.; Moura, L.A.N.E.; Castro, M.C.R.; Kac, G.; Hadler, M.C.C.M.; Noll, P.R.E.S.; Noll, M.; Rezende, A.T.O.; Delpino, F.M.; Oliveira, C. Prevalence of Vitamin D and Calcium Deficiency and Insufficiency in Women of Childbearing Age and Associated Risk Factors: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 4351. [Google Scholar] [CrossRef]
- Mavar, M.; Sorić, T.; Bagarić, E.; Sarić, A.; Matek Sarić, M. The Power of Vitamin D: Is the Future in Precision Nutrition through Personalized Supplementation Plans? Nutrients 2024, 16, 1176. [Google Scholar] [CrossRef]
- Bohon, T.M.; Goolsby, M.A. The Role of Vitamin D Supplements in Women’s Health. Clin. Med. Insights Womens Health 2013, 6, 67–70. [Google Scholar] [CrossRef]
- Garner, T.B.; Hester, J.M.; Carothers, A.; Diaz, F.J. Role of zinc in female reproduction. Biol. Reprod. 2021, 104, 976–994. [Google Scholar] [CrossRef]
- Fernandes, S.; Oliveira, L.; Pereira, A.; Costa, M.D.C.; Raposo, A.; Saraiva, A.; Magalhães, B. Exploring Vitamin B12 Supplementation in the Vegan Population: A Scoping Review of the Evidence. Nutrients 2024, 16, 1442. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- Marangoni, F.; Cetin, I.; Verduci, E.; Canzone, G.; Giovannini, M.; Scollo, P.; Corsello, G.; Poli, A. Maternal Diet and Nutrient Requirements in Pregnancy and Breastfeeding. An Italian Consensus Document. Nutrients 2016, 8, 629. [Google Scholar] [CrossRef]
- Bibbins-Domingo, K.; Grossman, D.C.; Curry, S.J.; Davidson, K.W.; Epling, J.W.; García, F.A.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; Landefeld, C.S.; et al. Folic Acid Supplementation for the Prevention of Neural Tube Defects: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 183–189. [Google Scholar] [CrossRef]
- WHO. Antenatal Iron Supplementation; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Ahmed, A.; Saleem, M.A.; Saeed, F.; Afzaal, M.; Imran, A.; Akram, S.; Hussain, M.; Khan, A.; Al Jbawi, E. A comprehensive review on the impact of calcium and vitamin D insufficiency and allied metabolic disorders in females. Food Sci. Nutr. 2023, 11, 5004–5027. [Google Scholar] [CrossRef]
- Coletta, J.M.; Bell, S.J.; Roman, A.S. Omega-3 Fatty acids and pregnancy. Rev. Obstet. Gynecol. 2010, 3, 163–171. [Google Scholar]
- Brink, L.R.; Bender, T.M.; Davies, R.; Luo, H.; Miketinas, D.; Shah, N.; Loveridge, N.; Gross, G.; Fawkes, N. Optimizing Maternal Nutrition: The Importance of a Tailored Approach. Curr. Dev. Nutr. 2022, 6, nzac118. [Google Scholar] [CrossRef]
- Silvestris, E.; Lovero, D.; Palmirotta, R. Nutrition and Female Fertility: An Interdependent Correlation. Front. Endocrinol. 2019, 10, 346. [Google Scholar] [CrossRef]
- Grieger, J.A.; Grzeskowiak, L.E.; Clifton, V.L. Preconception dietary patterns in human pregnancies are associated with preterm delivery. J. Nutr. 2014, 144, 1075–1080. [Google Scholar] [CrossRef]
- Vujkovic, M.; de Vries, J.H.; Lindemans, J.; Macklon, N.S.; van der Spek, P.J.; Steegers, E.A.; Steegers-Theunissen, R.P. The preconception Mediterranean dietary pattern in couples undergoing in vitro fertilization/intracytoplasmic sperm injection treatment increases the chance of pregnancy. Fertil. Steril. 2010, 94, 2096–2101. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Chavarro, J.E. Diet and fertility: A review. Am. J. Obstet. Gynecol. 2018, 218, 379–389. [Google Scholar] [CrossRef]
- Grieger, J.A. Preconception diet, fertility, and later health in pregnancy. Curr. Opin. Obstet. Gynecol. 2020, 32, 227–232. [Google Scholar] [CrossRef]
- Fabiani, R.; Naldini, G.; Chiavarini, M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2056. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità (ISS). Linea Guida: La Dieta Mediterranea. Istituto Superiore di Sanità. 2025. Available online: https://www.iss.it/documents/20126/10024898/LG+C0035-SINPE+et+al.pdf/da49883e-c0ce-ba5f-062791a02b0f2bfd?t=1744374219082 (accessed on 1 October 2025).
- Rich-Edwards, J.W.; Spiegelman, D.; Garland, M.; Hertzmark, E.; Hunter, D.J.; Colditz, G.A.; Willett, W.C.; Wand, H.; Manson, J.E. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology 2002, 13, 184–190. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet. Gynecol. 2007, 110, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Cetin, I.; Berti, C.; Calabrese, S. Role of micronutrients in the periconceptional period. Hum. Reprod. Update 2010, 16, 80–95. [Google Scholar] [CrossRef]
- Haider, B.A.; Olofin, I.; Wang, M.; Spiegelman, D.; Ezzati, M.; Fawzi, W.W.; Nutrition Impact Model Study Group (aneamia). Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 2013, 346, f3443. [Google Scholar] [CrossRef]
- Agarwal, A.; Aponte-Mellado, A.; Premkumar, B.J.; Shaman, A.; Gupta, S. The effects of oxidative stress on female reproduction: A review. Reprod. Biol. Endocrinol. 2012, 10, 49. [Google Scholar] [CrossRef]
- Wolfson, J.A.; Tucker, A.C.; Leung, C.W.; Rebholz, C.M.; Garcia-Larsen, V.; Martinez-Steele, E. Trends in Adults’ Intake of Un-processed/Minimally Processed, and Ultra-processed foods at Home and Away from Home in the United States from 2003–2018. J. Nutr. 2025, 155, 280–292. [Google Scholar] [CrossRef]
- Lane, M.M.; Gamage, E.; Du, S.; Ashtree, D.N.; McGuinness, A.J.; Gauci, S.; Baker, P.; Lawrence, M.; Rebholz, C.M.; Srour, B.; et al. Ultra-processed food exposure and adverse health outcomes: Umbrella review of epidemiological meta-analyses. BMJ 2024, 384, e077310. [Google Scholar] [CrossRef]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef]
- Monteiro, C.A. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009, 12, 729–731. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Touvier, M.; da Costa Louzada, M.L.; Mozaffarian, D.; Baker, P.; Juul, F.; Srour, B. Ultra-processed foods and cardiometabolic health: Public health policies to reduce consumption cannot wait. BMJ 2023, 383, e075294. [Google Scholar] [CrossRef] [PubMed]
- Martini, D.; Godos, J.; Bonaccio, M.; Vitaglione, P.; Grosso, G. Ultra-Processed Foods and Nutritional Dietary Profile: A Meta-Analysis of Nationally Representative Samples. Nutrients 2021, 13, 3390. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, E.; Esposito, S.; Costanzo, S.; Di Castelnuovo, A.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Bonaccio, M. Ultra-processed food consumption and its correlates among Italian children, adolescents and adults from the Italian Nutrition & Health Survey (INHES) cohort study. Public Health Nutr. 2021, 24, 6258–6271. [Google Scholar] [CrossRef]
- Bonaccio, M.; Iacoviello, L.; Donati, M.B.; de Gaetano, G. The tenth anniversary as a UNESCO world cultural heritage: An unmissable opportunity to get back to the cultural roots of the Mediterranean diet. Eur. J. Clin. Nutr. 2022, 76, 179–183. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef]
- Visioli, F.; Marangoni, F.; Fogliano, V.; Del Rio, D.; Martinez, J.A.; Kuhnle, G.; Buttriss, J.; Da Costa Ribeiro, H.; Bier, D.; Poli, A. The ultra-processed foods hypothesis: A product processed well beyond the basic ingredients in the package. Nutr. Res. Rev. 2023, 36, 340–350. [Google Scholar] [CrossRef]
- Gibney, M.J. Ultra-processed foods in public health nutrition: The unanswered questions. Br. J. Nutr. 2023, 129, 2191–2194. [Google Scholar] [CrossRef]
- Talebi, S.; Mehrabani, S.; Ghoreishy, S.M.; Wong, A.; Moghaddam, A.; Feyli, P.R.; Amirian, P.; Zarpoosh, M.; Kermani, M.A.H.; Moradi, S. The association between ultra-processed food and common pregnancy adverse outcomes: A dose-response systematic review and meta-analysis. BMC Pregnancy Childbirth 2024, 24, 369. [Google Scholar] [CrossRef]
- Morales-Suarez-Varela, M.; Rocha-Velasco, O.A. Impact of ultra-processed food consumption during pregnancy on maternal and child health outcomes: A comprehensive narrative review of the past five years. Clin. Nutr. ESPEN 2025, 65, 288–304. [Google Scholar] [CrossRef]
- Tristan Asensi, M.; Napoletano, A.; Sofi, F.; Dinu, M. Low-Grade Inflammation and Ultra-Processed Foods Consumption: A Review. Nutrients 2023, 15, 1546. [Google Scholar] [CrossRef]
- Ameho, S.; Klutstein, M. The effect of chronic inflammation on female fertility. Reproduction 2025, 169, e240197. [Google Scholar] [CrossRef] [PubMed]
- Han, V.X.; Patel, S.; Jones, H.F.; Nielsen, T.C.; Mohammad, S.S.; Hofer, M.J.; Gold, W.; Brilot, F.; Lain, S.J.; Nassar, N.; et al. Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: A systematic review. Transl. Psychiatry 2021, 11, 71. [Google Scholar] [CrossRef]
- Mouanness, M.; Nava, H.; Dagher, C.; Merhi, Z. Contribution of Advanced Glycation End Products to PCOS Key Elements: A Narrative Review. Nutrients 2022, 14, 3578. [Google Scholar] [CrossRef]
- Dennett, C.C.; Simon, J. The role of polycystic ovary syndrome in reproductive and metabolic health: Overview and approaches for treatment. Diabetes Spectr. 2015, 28, 116–120. [Google Scholar] [CrossRef]
- Laws, M.J.; Neff, A.M.; Brehm, E.; Warner, G.R.; Flaws, J.A. Endocrine disrupting chemicals and reproductive disorders in women, men, and animal models. Adv. Pharmacol. 2021, 92, 151–190. [Google Scholar] [CrossRef]
- Blaauwendraad, S.M.; Dykgraaf, R.H.M.; Gaillard, R.; Liu, M.; Laven, J.S.; Jaddoe, V.W.V.; Trasande, L. Associations of bisphenol and phthalate exposure and anti-Müllerian hormone levels in women of reproductive age. eClinicalMedicine 2024, 74, 102734. [Google Scholar] [CrossRef]
- Mazza, E.; Troiano, E.; Ferro, Y.; Lisso, F.; Tosi, M.; Turco, E.; Pujia, R.; Montalcini, T. Obesity, Dietary Patterns, and Hormonal Balance Modulation: Gender-Specific Impacts. Nutrients 2024, 16, 1629. [Google Scholar] [CrossRef]
- Barrea, L.; Caprio, M.; Camajani, E.; Verde, L.; Perrini, S.; Cignarelli, A.; Prodam, F.; Gambineri, A.; Isidori, A.M.; Colao, A.; et al. Ketogenic nutritional therapy (KeNuT)-a multi-step dietary model with meal replacements for the management of obesity and its related metabolic disorders: A consensus statement from the working group of the Club of the Italian Society of Endocrinology (SIE)-diet therapies in endocrinology and metabolism. J. Endocrinol. Investig. 2024, 47, 487–500. [Google Scholar] [CrossRef]
- Somogyi, V.; Gyorffy, A.; Scalise, T.J.; Kiss, D.S.; Goszleth, G.; Bartha, T.; Frenyo, V.L.; Zsarnovszky, A. Endocrine factors in the hypothalamic regulation of food intake in females: A review of the physiological roles and interactions of ghrelin, leptin, thyroid hormones, oestrogen and insulin. Nutr. Res. Rev. 2011, 24, 132–154. [Google Scholar] [CrossRef]
- Wohlgemuth, K.J.; Arieta, L.R.; Brewer, G.J.; Hoselton, A.L.; Gould, L.M.; Smith-Ryan, A.E. Sex differences and considerations for female specific nutritional strategies: A narrative review. J. Int. Soc. Sports Nutr. 2021, 18, 27. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Hao, T.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 2011, 364, 2392–2404. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Ferraro, R.; Lillioja, S.; Fontvieille, A.M.; Rising, R.; Bogardus, C.; Ravussin, E. Lower sedentary metabolic rate in women compared with men. J. Clin. Investig. 1992, 90, 780–784. [Google Scholar] [CrossRef]
- Taylor, R.W.; Grant, A.M.; Williams, S.M.; Goulding, A. Sex differences in regional body fat distribution from pre- to postpuberty. Obesity 2010, 18, 1410–1416. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Fernández-Ballart, J.; Ros, E.; Martínez-González, M.A.; Fitó, M.; Estruch, R.; Corella, D.; Fiol, M.; Gómez-Gracia, E.; Arós, F.; et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: One-year results of the PREDIMED randomized trial. Arch. Intern. Med. 2008, 168, 2449–2458. [Google Scholar] [CrossRef]
- Esposito, K.; Kastorini, C.M.; Panagiotakos, D.B.; Giugliano, D. Mediterranean diet and weight loss: Meta-analysis of randomized controlled trials. Metab Syndr. Relat. Disord. 2011, 9, 1–12. [Google Scholar] [CrossRef]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N. Engl. J. Med. 2008, 359, 229–241. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Bairey Merz, C.N.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Moscucci, F.; Sciomer, S.; Maffei, S.; Nasi, M.; Pinti, M.; Bucciarelli, V.; Dei Cas, A.; Parati, G.; Ciccone, M.M.; et al. Cardiovascular prevention in women: An update by the Italian Society of Cardiology working group on ‘Prevention, hypertension and peripheral disease’. J. Cardiovasc. Med. 2023, 24, e147–e155. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar] [CrossRef]
- Garcia, M.; Mulvagh, S.L.; Merz, C.N.; Buring, J.E.; Manson, J.E. Cardiovascular Disease in Women: Clinical Perspectives. Circ. Res. 2016, 118, 1273–1293. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Health effects of dietary risks in 195 countries, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart. J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD). Evidence-based European recommendations for the dietary management of diabetes. Diabetologia 2023, 66, 965–985. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Carbohydrate Intake for Adults and Children: WHO Guideline. 2023. Available online: https://www.who.int/publications/i/item/9789240073593 (accessed on 1 October 2025).
- World Health Organization. Guideline: Sugars Intake for Adults and Children. 2015. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 1 October 2025).
- Atkinson, F.S.; Brand-Miller, J.C.; Foster-Powell, K.; Buyken, A.E.; Goletzke, J. International tables of glycemic index and glycemic load values 2021: A systematic review. Am. J. Clin. Nutr. 2021, 114, 1625–1632. [Google Scholar] [CrossRef]
- World Health Organization. Use of Non-Sugar Sweeteners: WHO Guideline. 2023. Available online: https://www.who.int/publications/i/item/9789240073616 (accessed on 1 October 2025).
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- World Health Organization. Saturated Fatty Acid and Trans-Fatty Acid Intake for Adults and Children: WHO Guideline. 2023. Available online: https://www.who.int/publications/i/item/9789240073630 (accessed on 1 October 2025).
- Bhat, S.; Marklund, M.; Henry, M.E.; Appel, L.J.; Croft, K.D.; Neal, B.; Wu, J.H.Y. A Systematic Review of the Sources of Dietary Salt Around the World. Adv. Nutr. 2020, 11, 677–686. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Sodium Intake for Adults and Children. 2012. Available online: https://www.who.int/publications/i/item/9789241504836 (accessed on 1 October 2025).
- World Health Organization. Guideline: Potassium Intake for Adults and Children. 2012. Available online: https://www.who.int/publications/i/item/9789241504829 (accessed on 1 October 2025).
- Watts, N.B.; Binkley, N.; Owens, C.D.; Al-Hendy, A.; Puscheck, E.E.; Shebley, M.; Schlaff, W.D.; Simon, J.A. Bone Mineral Density Changes Associated with Pregnancy, Lactation, and Medical Treatments in Premenopausal Women and Effects Later in Life. J. Womens Health 2021, 30, 1416–1430. [Google Scholar] [CrossRef]
- Bellavia, D.; Costa, V.; De Luca, A.; Maglio, M.; Pagani, S.; Fini, M.; Giavaresi, G. Vitamin D Level Between Calcium-Phosphorus Homeostasis and Immune System: New Perspective in Osteoporosis. Curr. Osteoporos. Rep. 2024, 22, 599–610. [Google Scholar] [CrossRef]
- Dytfeld, J.; Marcinkowska, M.; Drwęska-Matelska, N.; Michalak, M.; Horst-Sikorska, W.; Słomski, R. Association analysis of the COL1A1 polymorphism with bone mineral density and prevalent fractures in Polish postmenopausal women with osteoporosis. Arch. Med. Sci. 2016, 12, 288–294. [Google Scholar] [CrossRef]
- Tu, M.Y.; Han, K.Y.; Lan, Y.W.; Chang, K.Y.; Lai, C.W.; Staniczek, T.; Lai, C.Y.; Chong, K.Y.; Chen, C.M. Association of TGF-β1 and IL-10 Gene Polymorphisms with Osteoporosis in a Study of Taiwanese Osteoporotic Patients. Genes 2021, 12, 930. [Google Scholar] [CrossRef]
- Moran, J.M. Nutrition and Women’s Bone Health. Nutrients 2022, 14, 763. [Google Scholar] [CrossRef]
- Kim, D.; Han, A.; Park, Y. Association of Dietary Total Antioxidant Capacity with Bone Mass and Osteoporosis Risk in Korean Women: Analysis of the Korea National Health and Nutrition Examination Survey 2008–2011. Nutrients 2021, 13, 1149. [Google Scholar] [CrossRef]
- Ali, D.S.; Khan, A.A.; Brandi, M.L. Effective strategies for pregnancy and lactation-associated osteoporosis: Teriparatide use in focus. Endocrine 2024, 86, 459–469. [Google Scholar] [CrossRef]
- Curtis, E.M.; Moon, R.J.; D’Angelo, S.; Crozier, S.R.; Bishop, N.J.; Gopal-Kothandapani, J.S.; Kennedy, S.H.; Papageorghiou, A.T.; Fraser, R.; Gandhi, S.V.; et al. Pregnancy Vitamin D Supplementation and Childhood Bone Mass at Age 4 Years: Findings From the Maternal Vitamin D Osteoporosis Study (MAVIDOS) Randomized Controlled Trial. JBMR Plus 2022, 6, e10651. [Google Scholar] [CrossRef]
- Sheng, B.; Li, X.; Nussler, A.K.; Zhu, S. The relationship between healthy lifestyles and bone health: A narrative review. Medicine 2021, 100, e24684. [Google Scholar] [CrossRef]
- Kovacs, C.S. Calcium and Phosphate Metabolism and Related Disorders During Pregnancy and Lactation. In Endotext; Feingold, K.R., Ahmed, S.F., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., et al., Eds.; MDText.Com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Jones, G.; Riley, M.D.; Dwyer, T. Maternal diet during pregnancy is associated with bone mineral density in children: A longitudinal study. Eur. J. Clin. Nutr. 2000, 54, 749–756. [Google Scholar] [CrossRef]
- Zhou, L.; Deng, W.; Wu, Q.; Pan, Y.; Huang, H. Association between dietary folate intake and the risk of osteoporosis in adults: A cross-sectional study. BMC Musculoskelet. Disord. 2024, 25, 487. [Google Scholar] [CrossRef]
- Gattermann, N.; Muckenthaler, M.U.; Kulozik, A.E.; Metzgeroth, G.; Hastka, J. The Evaluation of Iron Deficiency and Iron Overload. Dtsch. Arztebl. Int. 2021, 118, 847–856. [Google Scholar] [CrossRef]
- Harris, M.M.; Houtkooper, L.B.; Stanford, V.A.; Parkhill, C.; Weber, J.L.; Flint-Wagner, H.; Weiss, L.; Going, S.B.; Lohman, T.G. Dietary iron is associated with bone mineral density in healthy postmenopausal women. J. Nutr. 2003, 133, 3598–3602. [Google Scholar] [CrossRef]
- Naselli, F.; Bellavia, D.; Costa, V.; De Luca, A.; Raimondi, L.; Giavaresi, G.; Caradonna, F. Osteoarthritis in the Elderly Population: Preclinical Evidence of Nutrigenomic Activities of Flavonoids. Nutrients 2023, 16, 112. [Google Scholar] [CrossRef]
- Blekkenhorst, L.C.; Hodgson, J.M.; Lewis, J.R.; Devine, A.; Woodman, R.J.; Lim, W.H.; Wong, G.; Zhu, K.; Bondonno, C.P.; Ward, N.C.; et al. Vegetable and Fruit Intake and Fracture-Related Hospitalisations: A Prospective Study of Older Women. Nutrients 2017, 9, 511. [Google Scholar] [CrossRef]
- Gambari, L.; Grigolo, B.; Grassi, F. Dietary organosulfur compounds: Emerging players in the regulation of bone homeostasis by plant-derived molecules. Front. Endocrinol. 2022, 13, 937956. [Google Scholar] [CrossRef]
- Godos, J.; Giampieri, F.; Chisari, E.; Micek, A.; Paladino, N.; Forbes-Hernández, T.Y.; Quiles, J.L.; Battino, M.; La Vignera, S.; Musumeci, G.; et al. Alcohol Consumption, Bone Mineral Density, and Risk of Osteoporotic Fractures: A Dose-Response Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1515. [Google Scholar] [CrossRef]
- Abrams, S.A. Bone Health in School Age Children: Effects of Nutritional Intake on Outcomes. Front. Nutr. 2021, 8, 773425. [Google Scholar] [CrossRef]
- Dobranowska, K.; Plińska, S.; Dobosz, A. Dietary and Lifestyle Management of Functional Hypothalamic Amenorrhea: A Comprehensive Review. Nutrients 2024, 16, 2967. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.M.; Ackerman, K.E.; Berga, S.L.; Kaplan, J.R.; Mastorakos, G.; Misra, M.; Murad, M.H.; Santoro, N.F.; Warren, M.P. Functional Hypothalamic Amenorrhea: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 1413–1439. [Google Scholar] [CrossRef]
- Miyamoto, M.; Shibuya, K. Exploring the relationship between nutritional intake and menstrual cycle in elite female athletes. PeerJ 2023, 11, e16108. [Google Scholar] [CrossRef]
- Kuryłowicz, A. Estrogens in Adipose Tissue Physiology and Obesity-Related Dysfunction. Biomedicines 2023, 11, 690. [Google Scholar] [CrossRef]
- Gitsi, E.; Livadas, S.; Argyrakopoulou, G. Nutritional and exercise interventions to improve conception in women suffering from obesity and distinct nosological entities. Front. Endocrinol. 2024, 15, 1426542. [Google Scholar] [CrossRef]
- Łagowska, K. The Relationship between Vitamin D Status and the Menstrual Cycle in Young Women: A Preliminary Study. Nutrients 2018, 10, 1729. [Google Scholar] [CrossRef]
- Kapper, C.; Oppelt, P.; Ganhör, C.; Gyunesh, A.A.; Arbeithuber, B.; Stelzl, P.; Rezk-Füreder, M. Minerals and the Menstrual Cycle: Impacts on Ovulation and Endometrial Health. Nutrients 2024, 16, 8. [Google Scholar] [CrossRef]
- Skoracka, K.; Ratajczak, A.E.; Rychter, A.M.; Dobrowolska, A.; Krela-Kaźmierczak, I. Female Fertility and the Nutritional Approach: The Most Essential Aspects. Adv. Nutr. 2021, 12, 2372–2386. [Google Scholar] [CrossRef]
- Kazemi, M.; Jarrett, B.Y.; Vanden Brink, H.; Lin, A.W.; Hoeger, K.M.; Spandorfer, S.D.; Lujan, M.E. Obesity, Insulin Resistance, and Hyperandrogenism Mediate the Link between Poor Diet Quality and Ovarian Dysmorphology in Reproductive-Aged Women. Nutrients 2020, 12, 1953. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Dietary fatty acid intakes and the risk of ovulatory infertility. Am. J. Clin. Nutr. 2007, 85, 231–237. [Google Scholar] [CrossRef]
- Kudesia, R.; Alexander, M.; Gulati, M.; Kennard, A.; Tollefson, M. Dietary Approaches to Women’s Sexual and Reproductive Health. Am. J. Lifestyle Med. 2021, 15, 414–424. [Google Scholar] [CrossRef]
- Chou, S.H.; Mantzoros, C. 20 years of leptin: Role of leptin in human reproductive disorders. J. Endocrinol. 2014, 223, T49–T62. [Google Scholar] [CrossRef]
- Greenberg, J.A.; Bell, S.J.; Guan, Y.; Yu, Y.H. Folic Acid supplementation and pregnancy: More than just neural tube defect prevention. Rev. Obstet. Gynecol. 2011, 4, 52–59. [Google Scholar]
- Barchitta, M.; Maugeri, A.; Magnano San Lio, R.; Favara, G.; La Mastra, C.; La Rosa, M.C.; Agodi, A. Dietary Folate Intake and Folic Acid Supplements among Pregnant Women from Southern Italy: Evidence from the “Mamma & Bambino” Cohort. Int. J. Environ. Res. Public Health 2020, 17, 638. [Google Scholar] [CrossRef]
- Skolmowska, D.; Głąbska, D. Effectiveness of Dietary Intervention with Iron and Vitamin C Administered Separately in Improving Iron Status in Young Women. Int. J. Environ. Res. Public Health 2022, 19, 11877. [Google Scholar] [CrossRef]
- Allen, L.H. Anemia and iron deficiency: Effects on pregnancy outcome. Am. J. Clin. Nutr. 2000, 71, 1280S–1284S. [Google Scholar] [CrossRef]
- Vašková, J.; Klepcová, Z.; Špaková, I.; Urdzík, P.; Štofilová, J.; Bertková, I.; Kľoc, M.; Rabajdová, M. The Importance of Natural Antioxidants in Female Reproduction. Antioxidants 2023, 12, 907. [Google Scholar] [CrossRef]
- Baroutis, D.; Kalampokas, T.; Katsianou, E.; Psarris, A.; Daskalakis, G.; Panoulis, K.; Eleftheriades, M. The Role of the Mediterranean Diet in Assisted Reproduction: A Literature Review. Nutrients 2024, 16, 2807. [Google Scholar] [CrossRef]
- Cristodoro, M.; Zambella, E.; Fietta, I.; Inversetti, A.; Di Simone, N. Dietary Patterns and Fertility. Biology 2024, 13, 131. [Google Scholar] [CrossRef] [PubMed]
- Çekici, H.; Akdevelioğlu, Y. The association between trans fatty acids, infertility and fetal life: A review. Hum. Fertil. 2019, 22, 154–163. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Caffeinated and alcoholic beverage intake in relation to ovulatory disorder infertility. Epidemiology 2009, 20, 374–381. [Google Scholar] [CrossRef] [PubMed]
| To Be Preferred | To Be Used in Moderation | To Be Chosen Occasionally Amounts | |
|---|---|---|---|
| Cereals | Whole grains | Refined bread and pasta, biscuits, corn flakes | Pastries, muffins, pies, croissants |
| Vegetables | Raw and cooked vegetables | Potatoes | Vegetables prepared in butter or cream |
| Legumes | Lentils, beans, fava beans, peas, chickpeas, soybean | ||
| Fruit | Fresh or frozen fruit | Dried fruit, jelly, jam, canned fruit, sorbets, ice lollies/popsicles, fruit juice | |
| Sweets and sweeteners | Sucrose, honey, chocolate | Cakes, ice creams, soft drinks, sweets/candies | |
| Meat and fish | Lean and oily fish, poultry without skin | Lean cuts of beef, lamb, pork, and veal, seafood, shellfish | Sausages, salami, bacon, spare ribs, hot dogs, organ meats |
| Dairy food and eggs | Skimmed milk and yogurt | Low-fat milk, low-fat cheese and other milk products, eggs | Regular cheese, cream, whole milk and yogurt |
| Cooking fat and dressing | Vinegar, mustard, Olive oil | non-tropical vegetable oils, soft margarines, salad dressing, mayonnaise, ketchup | Trans fats and hard margarines (better to avoid them), palm and coconut oils, butter, lard, bacon fat |
| Nuts/seeds | All, unsalted (except coconut) | Coconut | |
| Cooking procedures | Grilling, boiling, steaming | Stir-frying, roasting | Frying |
| Domain | Recommendation | Typical Targets | Rationale/Evidence |
|---|---|---|---|
| Dietary pattern | Mediterranean-style, minimally processed diet | Vegetables, fruits, legumes, whole grains, nuts; extra-virgin olive oil; fish 2–3/week | Improved fertility/IVF outcomes; better metabolic profiles; lower GDM; better neonatal outcomes [18,41,42,43,44,45] |
| Diet quality | Achieve dietary diversity (MDD—W ≥ 5 groups/day) | ≥5 of 10 FAO food groups/day | Higher likelihood of micronutrient adequacy and better reproductive outcomes [2,3,4,5,6,7] |
| UPFs | Reduce UPFs (NOVA) | Limit refined carbohydrates, added sugars, saturated/trans fats, sodium | Associations with adverse pregnancy outcomes and inflammation [53,54,55,56,57,58] |
| Folate | Supplement peri—conceptionally | 400 μg/day (higher if clinically indicated) | Prevents NTDs [5,26,35,36,50,116] |
| Iron | Ensure adequate intake; supplement per status | 18 mg/day (non—pregnant); 30–60 mg/day in pregnancy if indicated | Reduces anemia and adverse pregnancy outcomes [23,24,25,26,27,28,29] |
| Vitamin D | Assess and replete if low | ≈600 IU/day; dose to 25(OH)D status | Linked to preeclampsia risk and maternal–fetal outcomes [5,27,28,29,30,31] |
| Calcium | Meet daily intake; separate from iron | 1000–1200 mg/day | Bone health; synergy with vitamin D [5,27,28,29,30,31] |
| Vitamin B12 | Ensure adequacy (esp. vegetarian/vegan) | 2.4 μg/day (non—pregnant); 2.6 μg/day in pregnancy | Prevents anemia and neurologic complications [32,33,41] |
| n-3 PUFAs (DHA/EPA) | Encourage intake; consider DHA supplement | DHA ≥ 200–300 mg/day during conception/pregnancy | Benefits for implantation and offspring neurodevelopment [18,19,20,21,35,36] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maugeri, A.; Barchitta, M.; Favara, G.; Magnano San Lio, R.; Ojeda-Granados, C.; Alonzo, E.; Bellavia, D.; Bonaccio, M.; Di Nucci, A.; Donfrancesco, C.; et al. The Role of Diet in Women of Childbearing Age: Current Evidence Supporting Nutritional Recommendations. Nutrients 2025, 17, 3505. https://doi.org/10.3390/nu17223505
Maugeri A, Barchitta M, Favara G, Magnano San Lio R, Ojeda-Granados C, Alonzo E, Bellavia D, Bonaccio M, Di Nucci A, Donfrancesco C, et al. The Role of Diet in Women of Childbearing Age: Current Evidence Supporting Nutritional Recommendations. Nutrients. 2025; 17(22):3505. https://doi.org/10.3390/nu17223505
Chicago/Turabian StyleMaugeri, Andrea, Martina Barchitta, Giuliana Favara, Roberta Magnano San Lio, Claudia Ojeda-Granados, Elena Alonzo, Daniele Bellavia, Marialaura Bonaccio, Annalisa Di Nucci, Chiara Donfrancesco, and et al. 2025. "The Role of Diet in Women of Childbearing Age: Current Evidence Supporting Nutritional Recommendations" Nutrients 17, no. 22: 3505. https://doi.org/10.3390/nu17223505
APA StyleMaugeri, A., Barchitta, M., Favara, G., Magnano San Lio, R., Ojeda-Granados, C., Alonzo, E., Bellavia, D., Bonaccio, M., Di Nucci, A., Donfrancesco, C., Esposito, S., Gandullia, P., Giavaresi, G., Giroli, M., Grigolo, B., Grassi, F., Leonardi, F., Proietti, E., Sciacca, L., ... Agodi, A. (2025). The Role of Diet in Women of Childbearing Age: Current Evidence Supporting Nutritional Recommendations. Nutrients, 17(22), 3505. https://doi.org/10.3390/nu17223505











