Hemoglobin-Geriatric Nutritional Risk Index Predicts Major Adverse Cardiovascular Events After Transcatheter Aortic Valve Implantation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.2.1. Clinical Variables, Functional Assessments, and Definitions
2.2.2. GNRI
2.2.3. H-GNRI
2.2.4. Definition of MACEs
2.2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
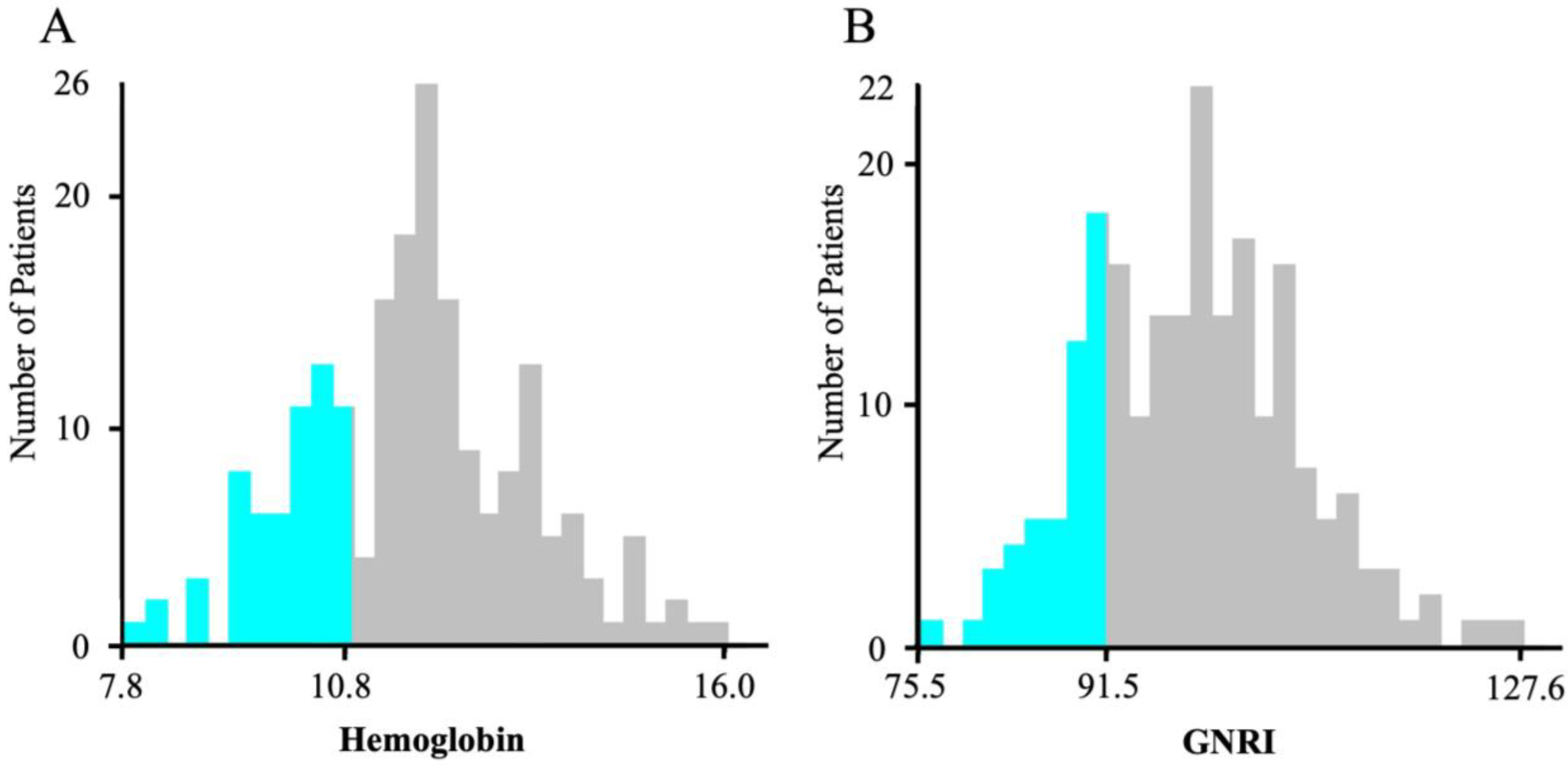
3.2. H-GNRI Cutoff Values
3.3. Comparison of the Three Groups on the Basis of H-GNRI
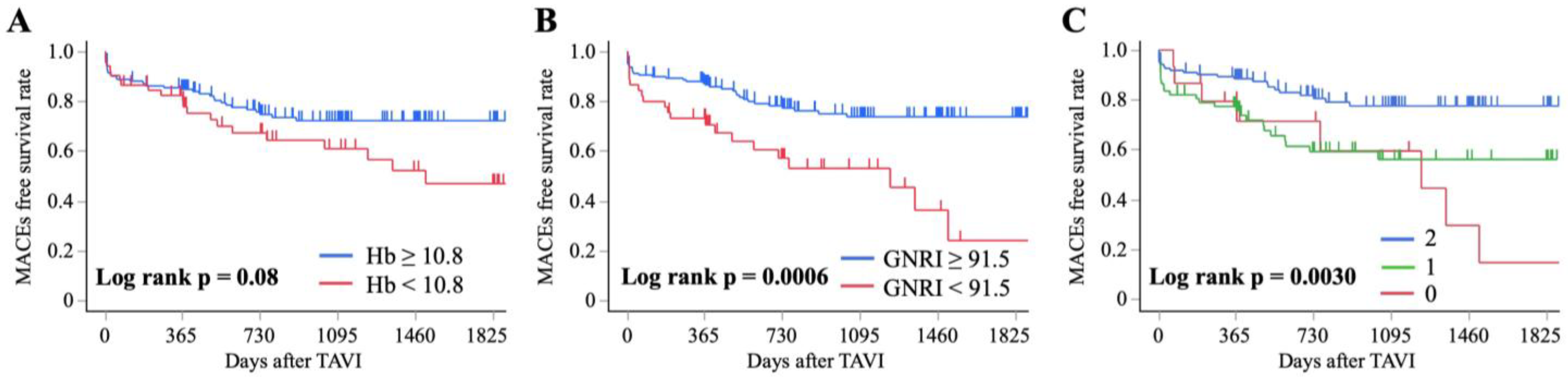
3.4. Kaplan–Meier Survival Curves for MACEs Using the Hb Level, GNRI, and H-GNRI
3.5. Factors Associated with MACEs Using Cox Proportional-Hazard Model: Univariate and Multivariate Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TAVI | Transcatheter aortic valve implantation |
| AS | Aortic stenosis |
| MACEs | Major adverse cardiovascular events |
| GNRI | Geriatric Nutritional Risk Index |
| Alb | Serum albumin |
| Hb | Hemoglobin |
| H-GNRI | Hemoglobin-GNRI |
| BMI | Body mass index |
| NYHA | New York Heart Association |
| STS-PROM | Society of Thoracic Surgeons Predicted Risk of Mortality |
| SPPB | Short Physical Performance Battery |
| BADL | Basic activities of daily living |
| HR | Hazard ratio |
| CI | Confidence interval |
| IQR | Interquartile ranges |
| WHO | World Health Organization |
References
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Piazza, N.; Alu, M.C.; Nazif, T.; Hahn, R.T.; Pibarot, P.; Bax, J.J.; Leipsic, J.A.; Blanke, P.; Blackstone, E.H.; et al. Valve Academic Research Consortium 3: Updated Endpoint Definitions for Aortic Valve Clinical Research. J. Am. Coll. Cardiol. 2021, 77, 2717–2746. [Google Scholar] [CrossRef] [PubMed]
- Eftychiou, C.; Eteocleous, N.; Zittis, I.; Simamonian, K.; Ioannou, A.; Loukaidou, P.; Ntaka, A.; Hadjigregoriou, A.; Vasiliades, V.; Adamou, M.; et al. Outcomes of transfemoral transcatheter aortic valve implantation (TAVI) and predictors of thirty-day major adverse cardiovascular events (MACE) and one-year mortality. Hell. J. Cardiol. 2021, 62, 57–64. [Google Scholar] [CrossRef]
- Ishizu, K.; Shirai, S.; Isotani, A.; Hayashi, M.; Kawaguchi, T.; Taniguchi, T.; Ando, K.; Yashima, F.; Tada, N.; Yamawaki, M.; et al. Long-Term Prognostic Value of the Society of Thoracic Surgery Risk Score in Patients Undergoing Transcatheter Aortic Valve Implantation (From the OCEAN-TAVI Registry). Am. J. Cardiol. 2021, 149, 86–94. [Google Scholar] [CrossRef]
- Ishizu, K.; Shirai, S.; Tashiro, H.; Kitano, K.; Tabata, H.; Nakamura, M.; Morofuji, T.; Murakami, N.; Morinaga, T.; Hayashi, M.; et al. Prevalence and Prognostic Significance of Malnutrition in Older Japanese Adults at High Surgical Risk Undergoing Transcatheter Aortic Valve Implantation. J. Am. Heart Assoc. 2022, 11, e026294. [Google Scholar] [CrossRef]
- Kazemian, S.; Tavolinejad, H.; Rashedi, S.; Yarahmadi, P.; Farrokhpour, H.; Kolte, D. Meta-Analysis on the Association Between Nutritional Status and Outcomes After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2023, 186, 109–116. [Google Scholar] [CrossRef]
- Emami, S.; Rudasill, S.; Bellamkonda, N.; Sanaiha, Y.; Cale, M.; Madrigal, J.; Christian-Miller, N.; Benharash, P. Impact of Malnutrition on Outcomes Following Transcatheter Aortic Valve Implantation (from a National Cohort). Am. J. Cardiol. 2020, 125, 1096–1101. [Google Scholar] [CrossRef]
- Mas-Peiro, S.; Papadopoulos, N.; Walther, T.; Zeiher, A.M.; Fichtlscherer, S.; Vasa-Nicotera, M. Nutritional risk index is a better predictor of early mortality than conventional nutritional markers after transcatheter aortic valve replacement: A prospective cohort study. Cardiol. J. 2021, 28, 312–320. [Google Scholar] [CrossRef]
- Jiménez-Xarrié, E.; Asmarats, L.; Roqué-Figuls, M.; Millán, X.; Li, C.H.P.; Fernández-Peregrina, E.; Sánchez-Ceña, J.; van Roessel, A.M.; Hittinger, M.L.M.; Paniagua, P.; et al. Impact of Baseline Anemia in Patients Undergoing Transcatheter Aortic Valve Replacement: A Prognostic Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 6025. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, S.; Yamamoto, M.; Kagase, A.; Tokuda, T.; Koyama, Y.; Shimura, T.; Adachi, Y.; Yamaguchi, R.; Otsuka, T.; Yashima, F.; et al. The Usefulness of the Modified Essential Frailty Toolset to Predict Late Bleeding Events after Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2022, 184, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Xu, C.; Ying, K.; Chu, J.; Geng, W. Prognostic value of hemoglobin combined with Geriatric Nutritional Risk Index scores in patients undergoing postoperative radiotherapy for esophageal squamous cell carcinoma. Future Oncol. 2021, 18, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Onoda, H.; Ueno, H.; Imamura, T.; Ueno, Y.; Kuwahara, H.; Sobajima, M.; Kinugawa, K.; Tada, N.; Naganuma, T.; Yamawaki, M.; et al. Identification of Anemia for Predicting Mid-Term Prognosis After Transcatheter Aortic Valve Implantation in Japanese Patients—Insights From the OCEAN-TAVI Registry. Circ. Rep. 2021, 3, 286–293. [Google Scholar] [CrossRef]
- Kouchoukos, N.T.; Ebert, P.A.; Grover, F.L.; Lindesmith, G.G. Report of the ad hoc committee on risk-factors for coronary-artery bypass-surgery. Ann. Thorac. Surg. 1988, 45, 348–349. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Van Mourik, M.S.; Velu, J.F.; Lanting, V.R.; Limpens, J.; Bouma, B.J.; Piek, J.J.; Baan, J.; Henriques, J.P.S.; Vis, M.M. Preoperative frailty parameters as predictors for outcomes after transcatheter aortic valve implantation: A systematic review and meta-analysis. Neth. Heart J. 2020, 28, 280–292. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontrol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Gonçalves, R.S.d.S.A.; Ribeiro, K.M.O.B.d.F.; Fernandes, S.G.G.; de Andrade, L.E.L.; Lira, M.d.G.d.A.; Nascimento, R.A.D.; Vieira, M.C.A.; Maciel, Á.C.C. Diagnostic Accuracy of the Short Physical Performance Battery in Detecting Frailty and Prefrailty in Community-Dwelling Older Adults: Results from the PRO-EVA Study. J. Geriatr. Phys. Ther. 2023, 46, E127–E136. [Google Scholar] [CrossRef]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef]
- Kinugasa, Y.; Kato, M.; Sugihara, S.; Hirai, M.; Yamada, K.; Yanagihara, K.; Yamamoto, K. Geriatric Nutritional Risk Index Predicts Functional Dependency and Mortality in Patients with Heart Failure with Preserved Ejection Fraction. Circ. J. 2013, 77, 705–711. [Google Scholar] [CrossRef]
- Camp, R.L.; Dolled-Filhart, M.; Rimm, D.L. X-tile: A new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin. Cancer Res. 2004, 10, 7252–7259. [Google Scholar] [CrossRef]
- Ying, J.; Zhu, S.; Cheng, Y.; Wang, B.; Wang, Y. Prognostic Role of Hemoglobin Combined with Geriatric Nutritional Risk Index in Patients with Vater Ampulla Carcinoma Undergoing Pancreaticoduodenectomy. Cancer Med. 2024, 13, e70334. [Google Scholar] [CrossRef] [PubMed]
- Baştuğ, S.; Çöteli, C.; Çelik, M.C.; Kasapkara, H.A.; Bayram, N.A.; Akcay, M.; Durmaz, T. Baseline Anemia Is an Independent Predictor of Long-Term Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation. Angiology 2022, 73, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cen, K.; Sun, W.; Feng, B. Prognostic value of geriatric nutritional risk index in elderly patients with heart failure: A meta-analysis. Aging Clin. Exp. Res. 2021, 33, 1477–1486. [Google Scholar] [CrossRef]
- Tohyama, M.; Shirai, Y.; Shimizu, M.; Kato, Y.; Kokura, Y.; Momosaki, R. Predictive Value of the Hemoglobin-Geriatric Nutritional Risk Index in Patients with Heart Failure. Nutrients 2023, 15, 4789. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V. Epidemiology of Anemia in Older Adults. Semin. Hematol. 2008, 45, 210–217. [Google Scholar] [CrossRef]
- Nuis, R.-J.; Sinning, J.-M.; Rodés-Cabau, J.; Gotzmann, M.; van Garsse, L.; Kefer, J.; Bosmans, J.; Yong, G.; Dager, A.E.; Revilla-Orodea, A.; et al. Prevalence, Factors Associated With, and Prognostic Effects of Preoperative Anemia on Short- and Long-Term Mortality in Patients Undergoing Transcatter Aortic Valve Implantation. Circ. Cardiovasc. Interv. 2013, 6, 625–634. [Google Scholar] [CrossRef]
- Abushouk, A.; Agrawal, A.; Hariri, E.; Dykun, I.; Kansara, T.; Saad, A.; Abdelfattah, O.; Badwan, O.; Jaggi, C.; Farwati, M.; et al. Association between haematological parameters and outcomes following transcatheter aortic valve implantation at mid-term follow-up. Open Heart 2022, 9, e002108. [Google Scholar] [CrossRef]
- Shibata, K.; Yamamoto, M.; Kano, S.; Koyama, Y.; Shimura, T.; Kagase, A.; Yamada, S.; Kobayashi, T.; Tada, N.; Naganuma, T.; et al. Importance of Geriatric Nutritional Risk Index assessment in patients undergoing transcatheter aortic valve replacement. Am. Heart J. 2018, 202, 68–75. [Google Scholar] [CrossRef]

| Variables | Overall (n = 205) |
|---|---|
| Demographics | |
| Male sex, n (%) | 67 (35.2) |
| Age, years | 83.0 (80.0–87.0) |
| BMI, kg/m2 | 22.4 (20.4–25.1) |
| NYHA functional class 3/4 (%) | 87 (42.4) |
| Surgical risk score | |
| STS–PROM score, % | 5.0 (3.3–7.1) |
| Echocardiographic data | |
| Ejection fraction, % | 65.0 (60.0–71.0) |
| Aortic valve area, cm2 | 0.60 (0.50–0.77) |
| Aortic peak velocity (m/s) | 4.3 (4.0–4.8) |
| Aortic valve mean pressure gradient, mmHg | 43.6 (35.7–55.5) |
| Nutrition | |
| GNRI score | 99.2 (91.8–104.4) |
| Preprocedural laboratory data | |
| Hb level, g/dL | 11.8 (10.6–12.7) |
| Alb level, g/dL | 3.7 (3.5–4.0) |
| eGFRcys, mL/min/1.73 m2 | 59.7 (48.1–69.0) |
| BNP level, pg/mL | 93.1 (47.7–286.9) |
| Physical function | |
| Grip power, kg | 19.7 (15.6–24.1) |
| SPPB score | 12 (9–12) |
| SPPB ≤ 9, n (%) | 61 (29.7) |
| Cognitive function MMSE score | 26 (24–28) |
| BADL dependency (Katz Index) | |
| Dependent (≥1 item), n (%) | 28 (13.6) |
| Comorbidity | |
| Hypertension, n (%) | 155 (75.2) |
| Diabetes mellitus, n (%) | 65 (31.6) |
| Dyslipidemia, n (%) | 109 (52.9) |
| Atrial fibrillation, n (%) | 56 (27.2) |
| Anemia, n (%) | 36 (17.5) |
| Chronic kidney disease, n (%) | 50 (24.3) |
| Cardiovascular disease, n (%) | 53 (25.7) |
| Arrhythmia, n (%) | 59 (28.6) |
| Chronic heart failure, n (%) | 45 (21.8) |
| Cerebral infarction, n (%) | 29 (14.1) |
| Procedural variables | |
| Procedure time, min | 104.0 (90.0–121.8) |
| Approach route | |
| Transfemoral approach, n (%) | 196 (95.1) |
| Transapical approach, n (%) | 5 (2.4) |
| Transaortic approach, n (%) | 2 (1.0) |
| Trans-subclavian approach, n (%) | 2 (1.0) |
| Length of hospital stay after TAVI, days | 11.0 (11–16.5) |
| Factor | H-GNRI Score | |||
|---|---|---|---|---|
| 2 (n = 123) | 1 (n = 67) | 0 (n = 15) | p-Value | |
| MACEs, n (%) | 24 (19.5) | 25 (37.3) | 8 (53.3) | 0.0026 |
| Variables | ||||
| Male sex, n (%) | 41 (33.6) | 20 (30.0) | 6 (40.0) | 0.70 |
| Age, years | 83.0 (80.0, 86.0) | 84.0 (82.0, 88.0) | 85.0 (78.0, 87.0) | 0.06 |
| BMI, kg/m2 | 23.6 (21.3, 26.1) | 21.0 (19.0, 23.8) | 20.4 (19.0, 21.5) | <0.0001 |
| NYHA functional class 3/4 (%) | 41 (33.3) | 39 (58.2) | 7 (46.7) | 0.004 |
| STS-PROM score, % | 4.2 (3.0, 6.4) | 5.89 (4.1, 8.10) | 7.2 (5.3, 7.2) | 0.0003 |
| Echocardiographic data | ||||
| Ejection fraction, % | 63.8 (62.0, 65.8) | 64.1 (61.5, 66.7) | 58.5 (53.1, 64.0) | 0.14 |
| Aortic valve area, cm2 | 0.67 (0.54, 0.77) | 0.60 (0.46, 0.76) | 0.65 (0.53, 0.72) | 0.15 |
| Aortic peak velocity, m/s | 4.2 (4.0, 4.7) | 4.5 (4.0, 4.8) | 4.4 (4.0, 4.8) | 0.30 |
| Aortic valves mean pressure | 41.2 (35.6, 54.4) | 46.5 (35.4, 58.1) | 46.4 (37.3, 56.0) | 0.21 |
| gradient, mmHg | ||||
| Nutrition | ||||
| GNRI score | 101.5 (97.3, 106.9) | 92.2 (89.6, 100.7) | 87.7 (84.1, 89.6) | <0.0001 |
| Preprocedural laboratory data | ||||
| Hb level, g/dL | 12.1 (11.7, 13.3) | 10.5 (10.0, 11.7) | 9.7 (8.9, 10.3) | <0.0001 |
| Alb level, g/dL | 3.9 (3.6, 4.1) | 3.7 (3.5, 3.9) | 3.3 (3.0, 3.4) | <0.0001 |
| eGFRcys, mL/min/1.73 m2 | 53.9 (43.3, 64.0) | 47.7 (36.7, 58.1) | 42.1 (30.7, 47.2) | 0.0009 |
| BNP level, pg/mL | 62.7 (39.7, 185.4) | 141.1 (71.0, 393.6) | 98.0 (69.7, 369.8) | 0.0002 |
| Physical function | ||||
| Grip power, kg | 20.0 (16.2, 24.2) | 18.7 (14.0, 24.2) | 19.4 (12.0, 22.5) | 0.20 |
| SPPB, score | 12 (9, 12) | 11 (8, 12) | 9.5 (7.5, 12) | 0.26 |
| SPPB ≤ 9, n (%) | 33 (27.1) | 21 (31.3) | 7 (50.0) | 0.19 |
| Cognitive function | ||||
| MMSE | 26.0 (25.0, 29.0) | 26.0 (24.0, 28.0) | 25.0 (21, 27) | 0.03 |
| BADL dependency (Katz Index) | ||||
| Dependent (≥1 item) n (%) | 12 (9.8) | 14 (20.9) | 2 (14.3) | 0.10 |
| Procedural variables | ||||
| Procedure time, min | 103.5 (88.8, 120.0) | 104 (90.7, 122.8) | 109.0 (92.0, 118.0) | 0.74 |
| Approach route | ||||
| Transfemoral approach, n (%) | 120 (98.0) | 62 (93.0) | 14 (93.0) | 0.15 |
| Transapical approach, n (%) | 0 (0.0) | 4 (6.0) | 1 (6.7) | |
| Transaortic approach, n (%) | 1 (0.8) | 1 (1.5) | 0 (0.0) | |
| Trans-subclavian approach, n (%) | 2 (1.6) | 0 (0.0) | 0 (0.0) | |
| Postprocedural variables | ||||
| Length of hospital stay after TAVI, days | 11.0 (11.0, 13.2) | 14.0 (11.0, 18.0) | 11.0 (10.0, 18.0) | 0.0002 |
| Factor | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Sex Male (Reference) | 1.00 | - | - | |||
| Female | 0.68 | 0.40–1.16 | 0.16 | |||
| Age | 1.03 | 0.97–1.09 | 0.31 | 0.99 | 0.94–1.06 | 0.99 |
| BMI | 0.92 | 0.84–0.99 | 0.03 | |||
| NYHA functional class 3/4 | 1.13 | 0.66–1.90 | 0.64 | 1.27 | 0.40–1.39 | 0.36 |
| SPPB ≤ 9 | 0.77 | 0.43–1.41 | 0.41 | 0.75 | 0.40–1.39 | 0.36 |
| MMSE | 1.04 | 0.95–1.15 | 0.37 | |||
| BADL Dependent (≥1 item) | 0.48 | 0.17–1.35 | 0.16 | |||
| Hb level | 0.83 | 0.70–0.99 | 0.03 | |||
| GNRI | 0.96 | 0.92–0.98 | 0.006 | |||
| H-GNRI score (baseline, H-GNRI score of 2) | 0.0063 | 0.024 | ||||
| H-GNRI score = 1 | 2.25 | 1.28–3.95 | 0.004 | 2.02 | 1.10–3.60 | 0.021 |
| H-GNRI score = 0 | 2.85 | 1.26–6.40 | 0.011 | 2.67 | 1.10–6.44 | 0.028 |
| Procedure time | 1.01 | 1.00–1.01 | <0.0001 | 1.00 | 1.00–1.01 | 0.0093 |
| Transfemoral approach (for Transapical) | 0.27 | 0.10–0.77 | 0.014 | 0.49 | 0.16–1.47 | 0.66 |
| Length of hospital stay after TAVI | 1.03 | 1.02v1.04 | <0.0001 | 1.02 | 1.01–1.04 | 0.0003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sasaki, T.; Miura, T.; Tamura, H.; Takakubo, Y.; Takagi, M.; Ebihara, S. Hemoglobin-Geriatric Nutritional Risk Index Predicts Major Adverse Cardiovascular Events After Transcatheter Aortic Valve Implantation. Nutrients 2025, 17, 3419. https://doi.org/10.3390/nu17213419
Sasaki T, Miura T, Tamura H, Takakubo Y, Takagi M, Ebihara S. Hemoglobin-Geriatric Nutritional Risk Index Predicts Major Adverse Cardiovascular Events After Transcatheter Aortic Valve Implantation. Nutrients. 2025; 17(21):3419. https://doi.org/10.3390/nu17213419
Chicago/Turabian StyleSasaki, Takeshi, Takahiro Miura, Harutoshi Tamura, Yuya Takakubo, Michiaki Takagi, and Satoru Ebihara. 2025. "Hemoglobin-Geriatric Nutritional Risk Index Predicts Major Adverse Cardiovascular Events After Transcatheter Aortic Valve Implantation" Nutrients 17, no. 21: 3419. https://doi.org/10.3390/nu17213419
APA StyleSasaki, T., Miura, T., Tamura, H., Takakubo, Y., Takagi, M., & Ebihara, S. (2025). Hemoglobin-Geriatric Nutritional Risk Index Predicts Major Adverse Cardiovascular Events After Transcatheter Aortic Valve Implantation. Nutrients, 17(21), 3419. https://doi.org/10.3390/nu17213419






