Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies
Abstract
1. Background
2. Materials and Methods
2.1. Protocol Registration
2.2. Search Strategy
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Data Extraction and Quality Assessment
2.6. Eligibility for Synthesis
2.7. Statistical Methods
3. Result
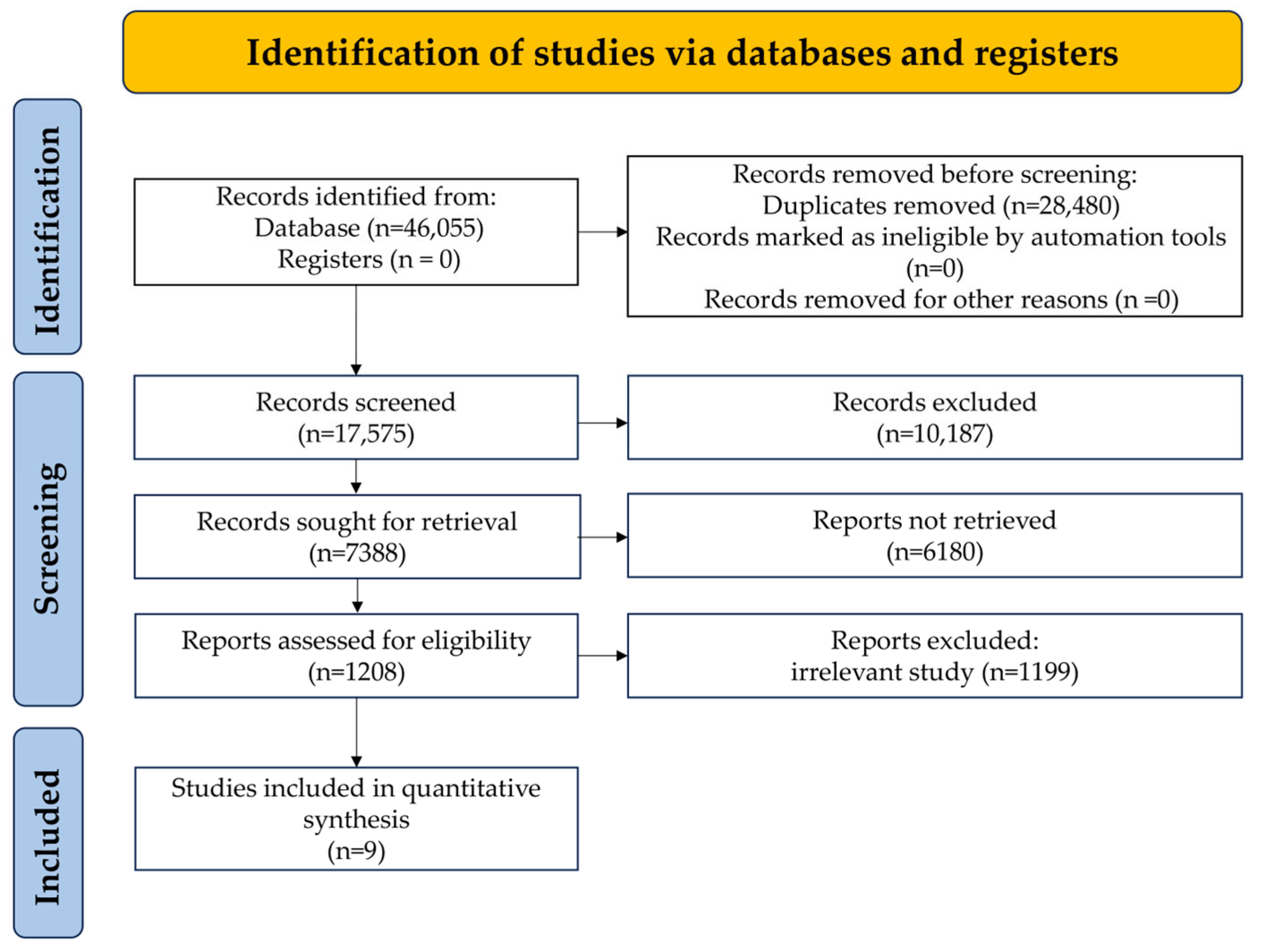
3.1. Research to Determine
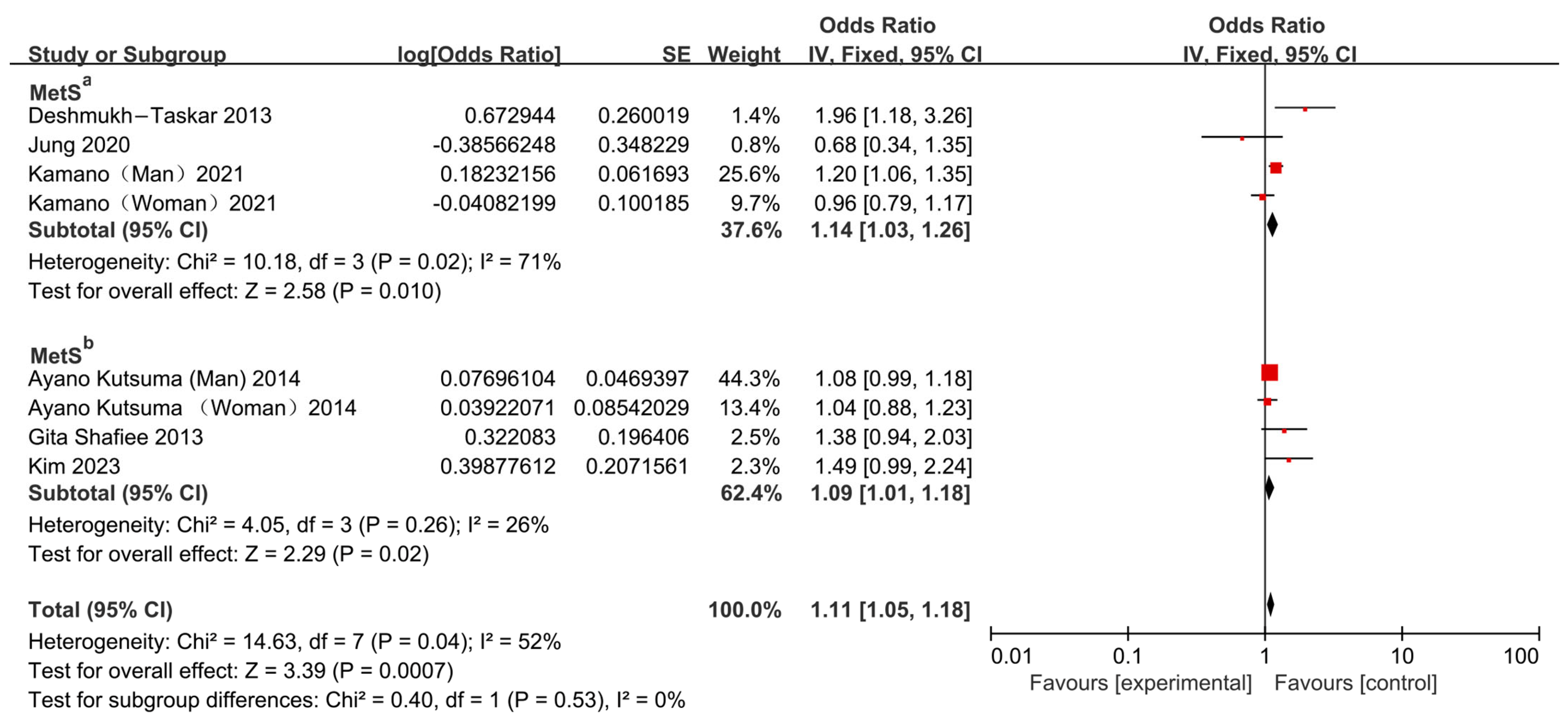
3.2. Association Between Skipping Breakfast and Risk of MetS
3.3. Association Between Skipping Breakfast and Risk of MetS Components
3.3.1. Association Between Skipping Breakfast and Risk of Abdominal Obesity
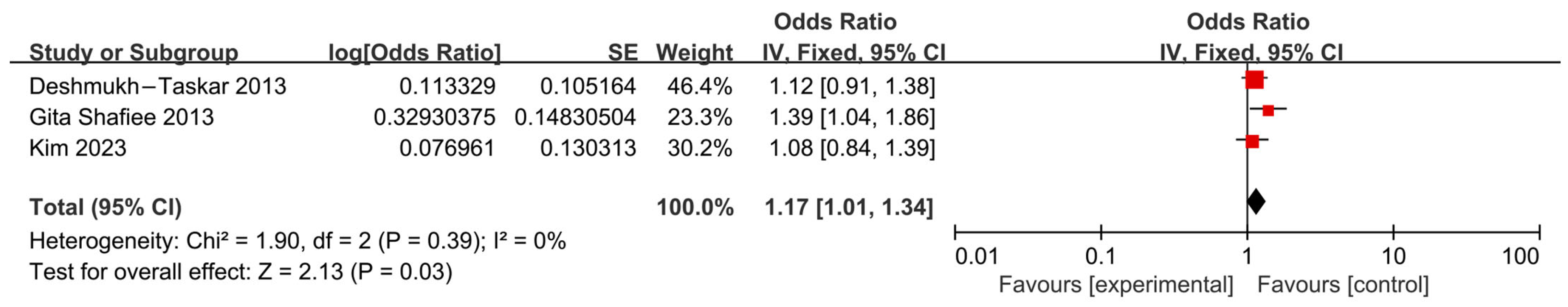
3.3.2. Association Between Skipping Breakfast and Risk of Hypertension
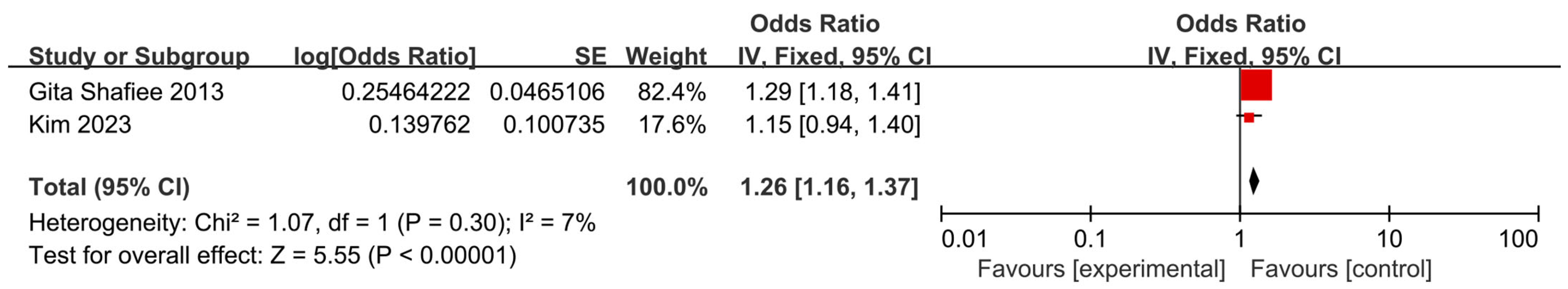
3.3.3. Association Between Skipping Breakfast and Risk of Hyperglycemia
| First Author | Publication Year | Study Design | Country | Male (%) | Age (Years) | Study Objective | Study Population | Outcome (%) | Frequency of Breakfast | OR (95% CI) | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jung [14] | 2020 | cross-sectional study | Korea | 49.1 | 20–64 | Evaluate the influence of skipping breakfast on the MetS. | 3864 | MetSa: 8.5 | 0 times/week 1–4 times/week 5–7 times/week | 0.68 (0.345–1.351) | 9 |
| Kamano [24] | 2021 | cohort study | Japan | 50.06 | 35–69 | Investigate sex-specific associations of skipping breakfast and short sleep duration with MetS and their interaction. | 29,780 | MetSa: 33.1 HTN: 87.5 (M); 87.9 (F) hyperglycemia: 77.7 (M); 69.5 (F) HLP: 68.6 (M); 55.5 (F) | Skipping breakfast | MetSa: 1.20 (1.06–1.35) (M) 0.96 (0.79–1.17) (F) HTN: 1.16(1.03–1.30) (M) 0.88 (0.77–1.00) (F) hyperglycemia: 1.05 (0.94–1.17) (M) 1.12 (0.96–1.30) (F) HLP: 1.18 (1.05–1.32) (M) 0.98 (0.82–1.18) (F) | 9 |
| Kutsuma [15] | 2014 | cross-sectional study | South Korea | 62.7 | 20–75 | Assess the association of breakfast skipping with MetS, proteinuria, obesity, and other cardiometabolic risk factors | 54,155 | MetSb: 12.1 | Skipping breakfast | 1.08 (0.99–1.19) (M) 1.04 (0.88–1.23) (F) | 8 |
| Kim [13] | 2023 | cross-sectional study | Japan | 53.4 | 18–39 | Assess the association between breakfast frequency and MetS. | 12,302 | MetSb: 2.6 AO: 9.1 HTN: 9.8 hyperglycemia: 10.2 HLP: 8.3 | Non-skipping,4–6 days, and 0–3 days | 1.49 (0.99–2.23) 1.08 (0.84–1.40) 1.34 (1.09–1.65) 1.15 (0.95–1.41) 1.09 (0.87–1.37) | 8 |
| Deshmukh-Taskar [23] | 2013 | cross-sectional study | USA | 26.1 | - | Examine the association between breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and MetS. | 5316 | MetSa: 20.7 AO: 36.8 HTN: 20.3 Hyperglycemia: 21.7 | Skipping breakfast, ready-to-eat cereal | 1.38 (0.94–2.03) 1.12 (0.95–1.38) 1.21 (0.98–1.48) 1.29 (0.95–1.14) | 9 |
| Tae Sic Lee [25] | 2016 | cross-sectional study | Korea | 39.4 | 14–68 | Investigate the relationship between the habit of eating breakfast and hypertension. | 3880 | HTN: 25.9 | Skipping breakfast | 1.065 (1.057–1.073) | 7 |
| Sung-Eun Park [26] | 2024 | cross-sectional study | Korea | 30.3 | 19–64 | Examine the association of breakfast habits with hypertension and obesity risk. | 2779 | HTN: 13.7 | Regular breakfast, skip breakfast every day | 1.239 (0.995–1.543) (M) 1.625 (1.228–2.148) (F) | 7 |
| Gita Shafiee [22] | 2013 | cross-sectional study | Iran | - | 10–18 | Evaluate the association of breakfast intake with cardiometabolic risk factors. | 5625 | MetSb: 5.25 HLP: 9.76 AO: 19.61 HTN: 4.89 Hyperglycemia: 14.02 | None, 1–2 days, 3–6 days, every day | 1.96 (1.18–3.27) 1.41 (1.03–1.93) 1.39 (1.04–1.86) 0.79 (0.54–1.14) 0.83 (0.64–1.08) | 8 |
| Fabiana A Silva [27] | 2018 | cross-sectional study | Brazil | - | 7–14 | Investigated the demographic, anthropometric, clinical, biochemical and behavioral factors associated with populations who missed breakfast. | 684 | HLP: 11.4 | Skipping breakfast | 0.79 (0.29–2.15) | 8 |
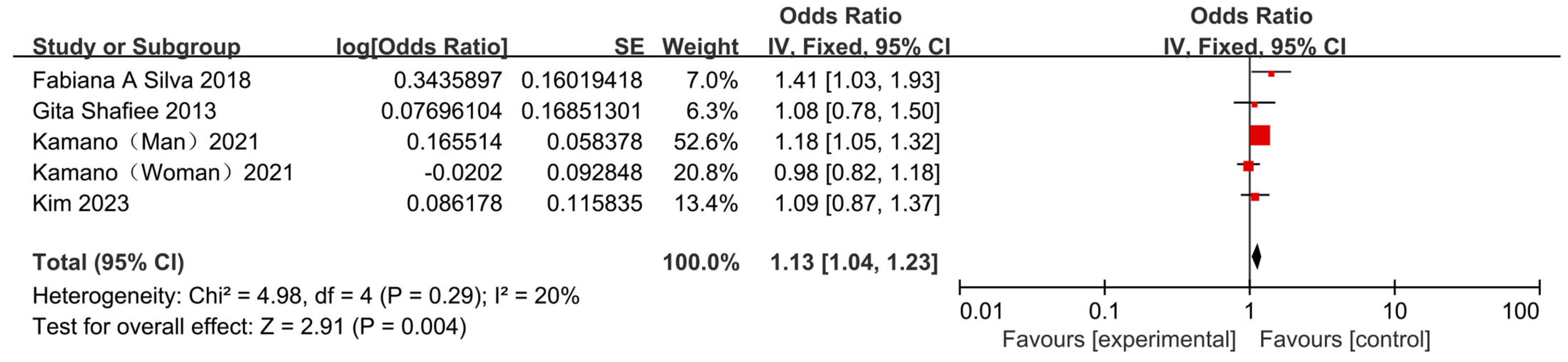
3.3.4. Association Between Skipping Breakfast and Risk of Hyperlipemia
4. Discussion
4.1. Skipping Breakfast Increase MetS Risk
4.2. Skipping Breakfast and Abdominal Obesity
4.3. Skipping Breakfast Increase Hypertension Risk
4.4. Skipping Breakfast Increase Hyperglycemia Risk
4.5. Breakfast Increase Hyperlipidemia Risk
4.6. Skipping Breakfast vs. Intermittent Fasting
4.7. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Alemany, M. The Metabolic Syndrome, a Human Disease. Int. J. Mol. Sci. 2024, 25, 2251. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef]
- Moore, K.J.; Shah, R. Introduction to the Obesity, Metabolic Syndrome and CVD Compendium. Circ. Res. 2020, 126, 1475–1476. [Google Scholar] [CrossRef]
- Muszalska, A.; Wiecanowska, J.; Michałowska, J.; Pastusiak-Zgolińska, K.M.; Polok, I.; Łompieś, K.; Bogdański, P. The Role of the Planetary Diet in Managing Metabolic Syndrome and Cardiovascular Disease: A Narrative Review. Nutrients 2025, 17, 862. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Bo, Y.; Zhao, L.; Li, Y.; Ju, L.; Fang, H.; Piao, W.; Yu, D.; Lao, X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients 2021, 13, 4475. [Google Scholar] [CrossRef] [PubMed]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011–2016. JAMA 2020, 323, 2526–2528. [Google Scholar] [CrossRef] [PubMed]
- Uzhova, I. The Importance of Breakfast in Atherosclerosis Disease. J. Am. Coll. Cardiol. 2017, 70, 1833–1842. [Google Scholar] [CrossRef]
- Zou, Y.; Zhang, R.H.; Huang, L.C.; Su, D.T.; Fang, Y.Q.; Meng, J.; Gu, F.; Zhao, D. Adult breakfast habits and nutritional status: A household based cross-sectional study in Zhejiang Province, China. Asia Pac. J. Clin. Nutr. 2020, 29, 372–381. [Google Scholar] [CrossRef]
- Manolis, A.A.; Manolis, T.A.; Melita, H.; Manolis, A.S. Features of a Balanced Healthy Diet with Cardiovascular and OtherBenefits. Curr. Vasc. Pharmacol. 2023, 21, 163–184. [Google Scholar] [CrossRef]
- Santos, H.O.; Genario, R.; Macedo, R.C.O.; Pareek, M.; Tinsley, G.M. Association of breakfast skipping with cardiovascular outcomes and cardiometabolic risk factors: An updated review of clinical evidence. Crit. Rev. Food Sci. Nutr. 2022, 62, 466–474. [Google Scholar] [CrossRef]
- Maki, K.C.; Phillips-Eakley, A.K.; Smith, K.N. The Effects of Breakfast Consumption and Composition on Metabolic Wellness with a Focus on Carbohydrate Metabolism. Adv. Nutr. 2016, 7, 613S–621S. [Google Scholar] [CrossRef]
- Gong, W.-J.; Fong, D.Y.-T.; Wang, M.-P.; Lam, T.-H.; Chung, T.W.-H.; Ho, S.-Y. Skipping Breakfast and Eating Breakfast Away from Home Were Prospectively Associated with Emotional and Behavioral Problems in 115,217 Chinese Adolescents. J. Epidemiol. 2022, 32, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.M.; Kang, H.J.; Lee, D.H.; Jeong, S.-M.; Joh, H.-K. Association between breakfast frequency and metabolic syndrome among young adults in South Korea. Sci. Rep. 2023, 13, 16826. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Kim, A.-S.; Ko, H.-J.; Choi, H.-I.; Hong, H.-E. Association between Breakfast Skipping and the Metabolic Syndrome: The Korea National Health and Nutrition Examination Survey, 2017. Medicina 2020, 56, 396. [Google Scholar] [CrossRef]
- Kutsuma, A.; Nakajima, K.; Suwa, K. Potential Association between Breakfast Skipping and Concomitant Late-Night-Dinner Eating with Metabolic Syndrome and Proteinuria in the Japanese Population. Scientifica 2014, 2014, 253581. [Google Scholar] [CrossRef]
- Grech, V.; Eldawlatly, A.A. STROBE, CONSORT, PRISMA, MOOSE, STARD, SPIRIT, and other guidelines—Overview and application. Saudi J. Anaesth. 2024, 18, 137–141. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Brach, C.; Borsky, A. How the U.S. Agency for Healthcare Research and Quality Promotes Health Literate Health Care. Stud. Health Technol. Inform. 2020, 269, 313–323. [Google Scholar] [CrossRef]
- Oremus, M.; Oremus, C.; Hall, G.B.C.; McKinnon, M.C. Inter-rater and test–retest reliability of quality assessments by novice student raters using the Jadad and Newcastle–Ottawa Scales. BMJ Open 2012, 2, e001368. [Google Scholar] [CrossRef]
- Moskalewicz, A.; Oremus, M. No clear choice between Newcastle–Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J. Clin. Epidemiol. 2020, 120, 94–103. [Google Scholar] [CrossRef]
- Cohen, J.F.; Chalumeau, M.; Cohen, R.; Korevaar, D.A.; Khoshnood, B.; Bossuyt, P.M.M. Cochran’s Q test was useful to assess heterogeneity in likelihood ratios in studies of diagnostic accuracy. J. Clin. Epidemiol. 2015, 68, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, G.; Kelishadi, R.; Qorbani, M.; Motlagh, M.E.; Taheri, M.; Ardalan, G.; Taslimi, M.; Poursafa, P.; Heshmat, R.; Larijani, B. Association of breakfast intake with cardiometabolic risk factors. J. Pediatr. 2013, 89, 575–582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Deshmukh-Taskar, P.; Nicklas, T.A.; Radcliffe, J.D.; O’Neil, C.E.; Liu, Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr. 2013, 16, 2073–2082. [Google Scholar] [CrossRef] [PubMed]
- Katsuura-Kamano, S.; Arisawa, K.; Uemura, H.; Van Nguyen, T.; Takezaki, T.; Ibusuki, R.; Suzuki, S.; Otani, T.; Okada, R.; Kubo, Y.; et al. Association of skipping breakfast and short sleep duration with the prevalence of metabolic syndrome in the general Japanese population: Baseline data from the Japan Multi-Institutional Collaborative cohort study. Prev. Med. Rep. 2021, 24, 101613. [Google Scholar] [CrossRef]
- Lee, T.S.; Kim, J.S.; Hwang, Y.J.; Park, Y.C. Habit of Eating Breakfast Is Associated with a Lower Risk of Hypertension. J. Lifestyle Med. 2016, 6, 64–67. [Google Scholar] [CrossRef]
- Park, S.-E.; Roh, S.-Y.; Kim, S.-Y. Relationship of Breakfast Habits with Hypertension and Obesity: A Cross-Sectional Study among Korean Adults and Older Adults. Int. J. Public Health 2025, 54, 175–185. [Google Scholar] [CrossRef]
- Silva, F.A.; Padez, C.; Sartorelli, D.S.; Oliveira, R.M.S.; Netto, M.P.; Mendes, L.L.; Cândido, A.P.C. Cross-sectional study showed that breakfast consumption was associated with demographic, clinical and biochemical factors in children and adolescents. Acta Paediatr. 2018, 107, 1562–1569. [Google Scholar] [CrossRef]
- Lujan-Barroso, L.; Iglesias, L.; Zamora-Ros, R.; Lasheras, C.; Sánchez, M.-J.; Cabrera-Castro, N.; Delfrad, J.; Amiano, P.; Molina-Montes, E.; Colorado-Yohar, S.; et al. Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort. Nutrients 2023, 15, 630. [Google Scholar] [CrossRef]
- Li, X.; Sun, Z. Circadian clock and temporal meal pattern. Med. Rev. 2021, 3, 85–101. [Google Scholar] [CrossRef]
- Harrison, S.; Couture, P.; Lamarche, B. Diet Quality, Saturated Fat and Metabolic Syndrome. Nutrients 2020, 12, 3232. [Google Scholar] [CrossRef]
- Wang, K.; Niu, Y.; Lu, Z.; Duo, B.; Effah, C.Y.; Guan, L. The effect of breakfast on childhood obesity: A systematic review and meta-analysis. Front. Nutr. 2023, 10, 1222536. [Google Scholar] [CrossRef]
- Li, Z.; Li, H.; Xu, Q.; Long, Y. Skipping Breakfast Is Associated with Hypertension in Adults: A Meta-Analysis. Int. J. Hypertens. 2022, 2022, 7245223. [Google Scholar] [CrossRef] [PubMed]
- Yin, T.; Zhang, J.-X.; Wang, F.-X.; Zhao, J.-H.; Zhao, Y.; Liu, L.; Liu, X.-Y.; Zhang, Y.-H.; Zhao, Y. The Association Between Sarcopenic Obesity and Hypertension, Diabetes, and Abnormal Lipid Metabolism in Chinese Adults. Diabetes Metab. Syndr. Obes. 2021, 14, 1963–1973. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, J.P.; Cardel, M.I.; Cellini, J.; Hu, F.B.; Guasch-Ferré, M. Breakfast Skipping, Body Composition, and Cardiometabolic Risk: A Systematic Review and Meta-Analysis of Randomized Trials. Obesity 2020, 28, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Naous, E.; Achkar, A.; Mitri, J. Intermittent Fasting and Its Effects on Weight, Glycemia, Lipids, and Blood Pressure: A Narrative Review. Nutrients 2023, 15, 3661. [Google Scholar] [CrossRef]
- Papakonstantinou, E.; Oikonomou, C.; Nychas, G.; Dimitriadis, G.D. Effects of Diet, Lifestyle, Chrononutrition and Alternative Dietary Interventions on Postprandial Glycemia and Insulin Resistance. Nutrients 2022, 14, 823. [Google Scholar] [CrossRef]
- Yao, Y.S.; Li, T.D.; Zeng, Z.H. Mechanisms underlying direct actions of hyperlipidemia on myocardium: An updated review. Lipids Health Dis. 2020, 19, 23. [Google Scholar] [CrossRef]
- Stewart, J.; McCallin, T.; Martinez, J.; Chacko, S.; Yusuf, S. Hyperlipidemia. Pediatr. Rev. 2020, 41, 393–402. [Google Scholar] [CrossRef]
- Souza, M.R.; Neves, M.E.A.; Gorgulho, B.M.; Souza, A.M.; Nogueira, P.S.; Ferreira, M.G.; Rodrigues, P.R.M. Breakfast skipping and cardiometabolic risk factors in adolescents: Systematic review. Rev. Saude Publica 2021, 55, 107. [Google Scholar] [CrossRef]
- Blasetti, A.; Franchini, S.; Castorani, V.; Comegna, L.; Fornari, E.; Daniele, F.; Prezioso, G.; Piona, C.; Federico, V.; Zona, D.; et al. Skipping Breakfast Is Associated with an Atherogenic Lipid Profile in Overweight and Obese Prepubertal Children. Int. J. Endocrinol. 2020, 2020, 1849274. [Google Scholar] [CrossRef]
- Farshchi, H.R.; Taylor, M.A.; Macdonald, I.A. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am. J. Clin. Nutr. 2005, 81, 388–396. [Google Scholar] [CrossRef]
- Santos, H.O.; Tinsley, G.M. Is breakfast consumption detrimental, unnecessary, or an opportunity for health promotion? A review of cardiometabolic outcomes and functional food choices. Diabetes Metab. Res. 2024, 40, e3684. [Google Scholar] [CrossRef]
- Reddy, B.L.; Reddy, V.S.; Saier, M.H. Review Article: Health Benefits of Intermittent Fasting. Microb. Physiol. 2024, 34, 142–152. [Google Scholar] [CrossRef]
- Pérez-Gerdel, T.; Camargo, M.; Alvarado, M.; Ramírez, J.D. Impact of Intermittent Fasting on the Gut Microbiota: A Systematic Review. Adv. Biol. 2023, 7, 2200337. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, B.; Lian, L.; Xing, K.; Cen, Y.; Zhao, Y.; Zhang, Y. Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2025, 17, 3155. https://doi.org/10.3390/nu17193155
Yang B, Lian L, Xing K, Cen Y, Zhao Y, Zhang Y. Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2025; 17(19):3155. https://doi.org/10.3390/nu17193155
Chicago/Turabian StyleYang, Bowen, Linxi Lian, Kaijun Xing, Yangyang Cen, Yi Zhao, and Yannan Zhang. 2025. "Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies" Nutrients 17, no. 19: 3155. https://doi.org/10.3390/nu17193155
APA StyleYang, B., Lian, L., Xing, K., Cen, Y., Zhao, Y., & Zhang, Y. (2025). Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients, 17(19), 3155. https://doi.org/10.3390/nu17193155