A Scoping Review of Contextual and Individual Factors for Hospital-Acquired Malnutrition Development in Adult Hospital Inpatients: Guiding a Proactive Preventative Approach
Abstract
1. Introduction
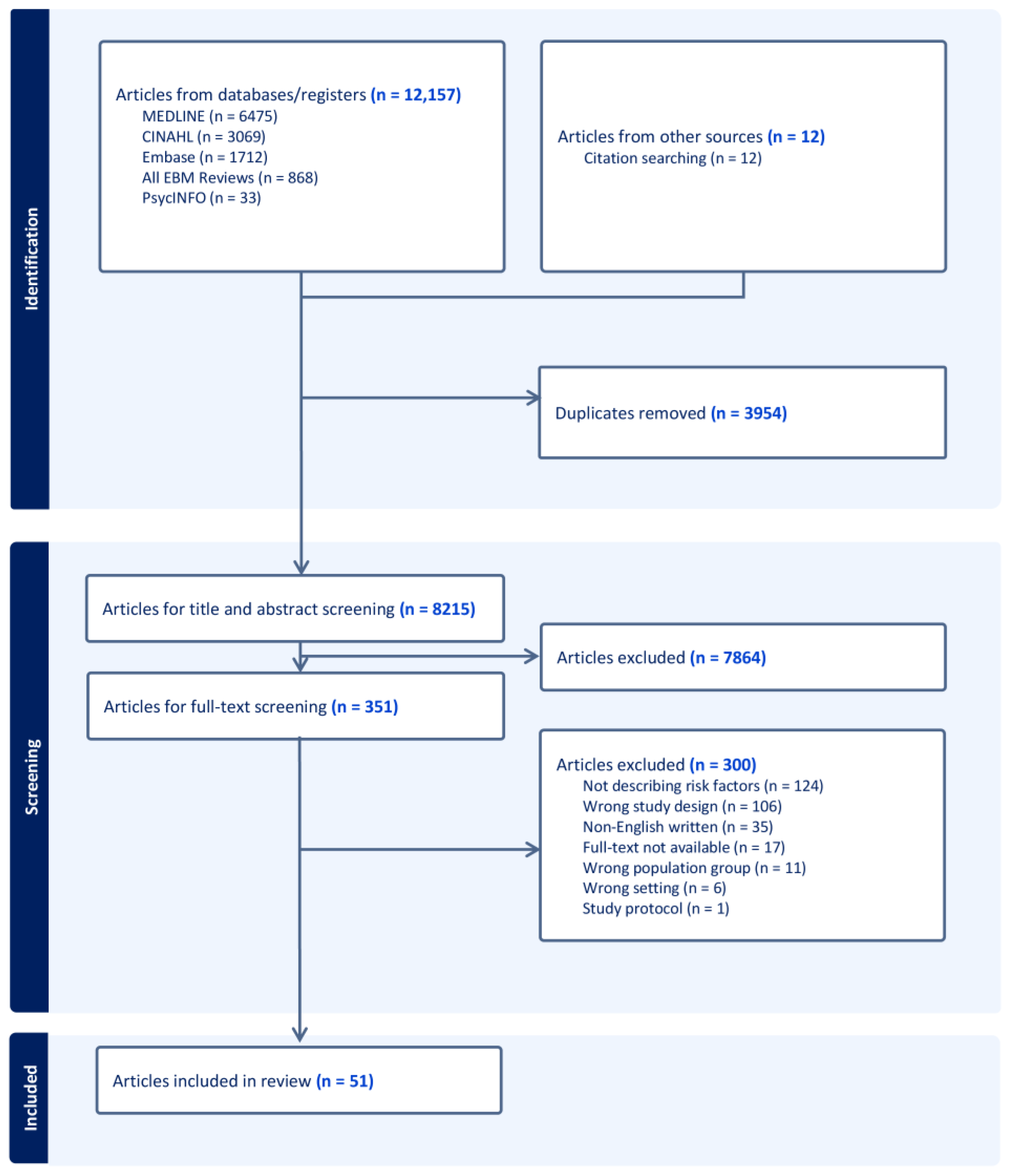
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Data Extraction
2.4. Data Analysis
3. Results
3.1. Main Characteristics of the Included Studies
3.2. Contextual Factors
3.2.1. Ward Type
3.2.2. Food Service Satisfaction
3.2.3. Medical-Related Mealtime Interruption
3.2.4. Nutrition Care Collaboration
3.3. Individual Factors
3.3.1. Nutritional Status Prior Admission
3.3.2. Hospital Length of Stay
3.3.3. Multimorbidity
3.3.4. Disease Acuity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheng, J.; Witney-Cochrane, K.; Cunich, M.; Ferrie, S.; Carey, S. Defining and quantifying preventable and non-preventable hospital-acquired malnutrition—A cohort study. Nutr. Diet. 2019, 76, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Hiesmayr, M.; Tarantino, S.; Moick, S.; Laviano, A.; Sulz, I.; Mouhieddine, M.; Schuh, C.; Volkert, D.; Simon, J.; Schindler, K. Hospital Malnutrition, a Call for Political Action: A Public Health and NutritionDay Perspective. J. Clin. Med. 2019, 8, 2048. [Google Scholar] [CrossRef]
- Cass, A.R.; Charlton, K.E. Prevalence of hospital-acquired malnutrition and modifiable determinants of nutritional deterioration during inpatient admissions: A systematic review of the evidence. J. Hum. Nutr. Diet. 2022, 35, 1043–1058. [Google Scholar] [CrossRef] [PubMed]
- Botero, L.; Young, A.M.; Banks, M.D.; Bauer, J. Incidence and criteria used in the diagnosis of hospital-acquired malnutrition in adults: A systematic review and pooled incidence analysis. Eur. J. Clin. Nutr. 2023, 77, 23–35. [Google Scholar] [CrossRef]
- Chen, B.; Yang, Y.; Cai, F.; Zhu, C.; Lin, S.; Huang, P.; Zhang, L. Nutritional status as a predictor of the incidence of pressure injury in adults: A systematic review and meta-analysis. J. Tissue Viability 2023, 32, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Australian Commission on Safety and Quality in Health Care, Hospital-Acquired Complications (HACs). Available online: https://www.safetyandquality.gov.au/our-work/indicators/hospital-acquired-complications (accessed on 1 May 2025).
- Carnevale, S.; Vitale, A.; Razzi, M.; Onori, C.; Cornacchia, G.; Grispo, O.; Corsinovi, E.; Rossl, L.; Spinetti, E.; Tosi, M.; et al. Non-Evidence-Based Dietary Restrictions in Hospital Nutrition and Their Impact on Malnutrition: A Narrative Review of International and National Guidelines. Dietetics 2024, 3, 568–587. [Google Scholar] [CrossRef]
- Cardenas, D.; Correia, M.I.T.D.; Hardy, G.; Gramlich, L.; Cederholm, T.; Van Ginkel-Res, A.; Remijnse, W.; Barrocas, A.; Gautier, J.B.O.; Ljungqvist, O.; et al. International Declaration on the Human Right to Nutritional Care: A global commitment to recognize nutrition care as a human right. Nutr. Clin. Pract. 2023, 38, 946–958. [Google Scholar] [CrossRef]
- Schuetz, P.; Seres, D.; Lobo, D.N.; Gomes, F.; Kaegi-Braun, N.; Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet 2021, 398, 1927–1938. [Google Scholar] [CrossRef]
- Schuetz, P.; Sulo, S.; Walzer, S.; Vollmer, L.; Brunton, C.; Kaegi-Braun, N.; Stanga, Z.; Mueller, B.; Gomes, F. Cost savings associated with nutritional support in medical inpatients: An economic model based on data from a systematic review of randomised trials. BMJ Open 2021, 11, e046402. [Google Scholar] [CrossRef]
- Buitrago, G.; Vargas, J.; Sulo, S.; Partridge, J.S.; Guevara-Nieto, M.; Gomez, G.; Misas, J.D.; Correia, M.I.T.D. Targeting malnutrition: Nutrition programs yield cost savings for hospitalized patients. Clin. Nutr. 2020, 39, 2896–2901. [Google Scholar] [CrossRef]
- Keller, H.H.; Vesnaver, E.; Davidson, B.; Allard, J.; Laporte, M.; Bernier, P.; Payette, H.; Jeejeebhoy, K.; Duerksen, D.; Gramlich, L. Providing quality nutrition care in acute care hospitals: Perspectives of nutrition care personnel. J. Hum. Nutr. Diet. 2014, 27, 192–202. [Google Scholar] [CrossRef]
- Botero, L.; Banks, M.D.; Gordon, E.H.; Bauer, J.; Young, A.M. Incidence and outcomes of in-hospital nutritional decline: A prospective observational cohort study in adult patients. Clin. Nutr. 2024, 43, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Abahuje, E.; Niyongombwa, I.; Karenzi, D.; Bisimwa, J.D.A.; Tuyishime, E.; Ntirenganya, F.; Rickard, J. Malnutrition in Acute Care Surgery Patients in Rwanda. World J. Surg. 2020, 44, 1361–1367. [Google Scholar] [CrossRef]
- Akazawa, N.; Kishi, M.; Hino, T.; Tsuji, R.; Tamura, K.; Hioka, A.; Moriyama, H. Higher malnutrition risk in older inpatients who are referred to the department of rehabilitation is related to increase of intramuscular adipose tissue: A prospective study. Clin. Nutr. 2022, 41, 2087–2093. [Google Scholar] [CrossRef]
- Allard, J.P.; Keller, H.; Teterina, A.; Jeejeebhoy, K.N.; Laporte, M.; Duerksen, D.R.; Gramlich, L.; Payette, H.; Bernier, P.; Davidson, B.; et al. Factors associated with nutritional decline in hospitalised medical and surgical patients admitted for 7 d or more: A prospective cohort study. Br. J. Nutr. 2015, 114, 1612–1622. [Google Scholar] [CrossRef]
- Álvarez Hernández, J.; Planas Vilá, M.; León Sanz, M.; Garcia de Lorenzo y Mateos, A.; Celaya Pérez, S.; García Lorda, P.; Araujo, K.; Sarto Guerri, B. Prevalence and costs of multinutrution in hospitalized patients; the PREDyCES study. Nutr. Hosp. 2012, 27, 1049–1059. [Google Scholar]
- Antonelli Incalzi, R.; Landi, F.; Cipriani, L.; Bruno, E.; Pagano, F.; Gemma, A.; Capparella, O.; Carbonin, P.U. Nutritional assessment: A primary component of multidimensional geriatric assessment in the acute care setting. J. Am. Geriatr. Soc. 1996, 44, 166–174. [Google Scholar] [CrossRef]
- Axelsson, K.; Asplund, K.; Norberg, A.; Alafuzoff, I. Nutritional status in patients with acute stroke. Acta Medica Scand. 1988, 224, 217–224. [Google Scholar] [CrossRef]
- Borrego Utiel, F.J.; Segura Torres, P.; Pérez del Barrio, M.P.; Sánchez Perales, M.C.; García Cortés, M.J.; Serrano Angeles, P.; Biechy Baldan, M.M.; Liébana Cañada, A. How do disorders related to hospitalisation influence haemodialysis patients’ nutrition? Nefrol. Publ. Of. Soc. Esp. Nefrol. 2011, 31, 471–483. [Google Scholar] [CrossRef]
- Caccialanza, R.; Cereda, E.; Klersy, C.; Bonardi, C.; Cappello, S.; Quarleri, L.; Turri, A.; Montagna, E.; Iacona, I.; Valentino, F.; et al. Phase Angle and Handgrip Strength Are Sensitive Early Markers of Energy Intake in Hypophagic, Non-Surgical Patients at Nutritional Risk, with Contraindications to Enteral Nutrition. Nutrients 2015, 7, 1828–1840. [Google Scholar] [CrossRef] [PubMed]
- Chapple, L.-A.S.; Deane, A.M.; Heyland, D.K.; Lange, K.; Kranz, A.J.; Williams, L.T.; Chapman, M.J. Energy and protein deficits throughout hospitalization in patients admitted with a traumatic brain injury. Clin. Nutr. 2016, 35, 1315–1322. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.H.; Tang, S.T.; Wang, C.; Huang, G.-H. Trajectory and determinants of nutritional health in older patients during and six-month post-hospitalisation. J. Clin. Nurs. 2009, 18, 3299–3307. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.; Porter, J.; Truby, H.; Huggins, C.E. How does nutritional state change during a subacute admission? Findings and implications for practice. Eur. J. Clin. Nutr. 2016, 70, 607–612. [Google Scholar] [CrossRef]
- Crary, M.A.; Humphrey, J.L.; Carnaby-Mann, G.; Sambandam, R.; Miller, L.; Silliman, S. Dysphagia, nutrition, and hydration in ischemic stroke patients at admission and discharge from acute care. Dysphagia 2013, 28, 69–76. [Google Scholar] [CrossRef]
- Diendéré, J.; Millogo, A.; Preux, P.-M.; Jésus, P.; Desport, J.-C. Changes in nutritional state and dysphagia in stroke patients monitored during a 14-d period in a Burkina Faso hospital setting. Nutrition 2018, 48, 55–60. [Google Scholar] [CrossRef]
- Flury, I.; Mueller, G.; Perret, C. The risk of malnutrition in patients with spinal cord injury during inpatient rehabilitation-A longitudinal cohort study. Front. Nutr. 2023, 10, 1085638. [Google Scholar] [CrossRef]
- Fu, K.; Pan, H. Nutritional status and risk factors for malnutrition in CRC patients undergoing neoadjuvant therapy. Biomed. Res. 2017, 28, 4406–4412. [Google Scholar]
- Gayo, N.P.; Águila, M.d.C.P.; Martín, A.M.; Ribeiro, A. The importance of using a nutritional risk analysis scale in patients admitted to continued care. EWMA J. 2014, 14, 27–31. [Google Scholar]
- Gobel, P.; Dogan Guney, H. Nutritional Support in Geriatric Patients in Intensive Care: The Relationships Between Prealbumin, Albumin and Total Protein Levels and the Route of Nutrition Administration. Turk Geriatr. Derg. 2022, 25, 409–421. [Google Scholar] [CrossRef]
- Graeb, F.; Wolke, R. Malnutrition and Inadequate Eating Behaviour during Hospital Stay in Geriatrics-An Explorative Analyses of NutritionDay Data in Two Hospitals. Nurs. Rep. 2021, 11, 929–941. [Google Scholar] [CrossRef] [PubMed]
- Gubari, M.I.M.; Hosseinzadeh-Attar, M.J.; Hosseini, M.; Mohialdeen, F.A.; Norouzy, A. Association of High Serum Adiponectin with the Risk of Malnutrition and Worse Outcome in Head Trauma Patients; a Cohort study. Arch. Acad. Emerg. Med. 2019, 7, e43. [Google Scholar] [CrossRef]
- Hafsteinsdóttir, T.B.; Mosselman, M.; Schoneveld, C.; Riedstra, Y.D.; Kruitwagen, C.L.J.J. Malnutrition in hospitalised neurological patients approximately doubles in 10 days of hospitalisation. J. Clin. Nurs. 2010, 19, 639–648. [Google Scholar] [CrossRef]
- Incalzi, R.A.; Gemma, A.; Capparella, O.; Cipriani, L.; Landi, F.; Carbonin, P. Energy Intake and In-Hospital Starvation: A Clinically Relevant Relationship. Arch. Intern. Med. 1996, 156, 425–429. [Google Scholar] [CrossRef]
- Kagifuku, Y.; Tohara, H.; Wakasugi, Y.; Susa, C.; Nakane, A.; Toyoshima, M.; Nakakuki, K.; Kabasawa, Y.; Harada, H.; Minakuchi, S. What Factors Affect Changes in Body Composition and Swallowing Function in Patients Hospitalized for Oral Cancer Surgery? Clin. Interv. Aging 2020, 15, 1–7. [Google Scholar] [CrossRef]
- Liang, L.; Thomas, J.; Miller, M.; Puckridge, P. Nutritional issues in older adults with wounds in a clinical setting. J. Multidiscip. Healthc. 2008, 1, 63–71. [Google Scholar] [CrossRef]
- Lin, L.; Wang, S.; Chen, S.H.; Wang, T.; Chen, M.; Wu, S. Efficacy of swallowing training for residents following stroke. J. Adv. Nurs. 2003, 44, 469–478. [Google Scholar] [CrossRef]
- Lin, T.; Yang, J.; Hong, X.; Yang, Z.; Ge, T.; Wang, M. Nutritional status in patients with advanced lung cancer undergoing chemotherapy: A prospective observational study. Nutr. Cancer 2020, 72, 1225–1230. [Google Scholar] [CrossRef]
- Liu, G.; Yi, Y.; Wang, Y.; Feng, Y.; Lin, M.; Yan, X.; Wang, J.; Ning, X.; Ma, N. Assessment of the Risk of Malnutrition or Frailty Among Patients Undergoing Liver Transplantation: A Hospital-Based Prospective Study. Int. J. Gen. Med. 2024, 17, 2347–2354. [Google Scholar] [CrossRef]
- Liu, P.; Wang, B.; Yan, X.; Cai, J.J.; Wang, Y. Comprehensive evaluation of nutritional status before and after hematopoietic stem cell transplantation in 170 patients with hematological diseases. Chin. J. Cancer Res. 2016, 28, 626–633. [Google Scholar] [CrossRef]
- Matsumoto, A.; Yoshimura, Y.; Nagano, F.; Bise, T.; Kido, Y.; Shimazu, S.; Shiraishi, A. Polypharmacy and Its Association with Dysphagia and Malnutrition among Stroke Patients with Sarcopenia. Nutrients 2022, 14, 4251. [Google Scholar] [CrossRef] [PubMed]
- Mosselman, M.J.; Kruitwagen, C.L.J.J.; Schuurmans, M.J.; Hafsteinsdóttir, T.B. Malnutrition and risk of malnutrition in patients with stroke: Prevalence during hospital stay. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurses 2013, 45, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Nematy, M.; Salami, H.; Norouzy, A.; Siadat, Z.; Shahsavan, N.; Tavallaie, S.; Ferns, G.; Ghayour-Mobarhan, M.; Soluti, S.S. Indices of malnutrition in patients admitted to general medical and chest medicine wards of an Iranian teaching hospital on admission and discharge. Mediterr. J. Nutr. Metab. 2013, 6, 53–57. [Google Scholar] [CrossRef]
- Padillo, F.J.; Rodriguez, M.; Gallardo, J.M.; Andicoberry, B.; Naranjo, A.; Minõ, G.; Sitges-Serra, A.; Pera-Madrazo, C. Changes in the pattern of visceral protein concentrations after internal biliary drainage in patients with obstructive jaundice. Eur. J. Surg. 1999, 165, 550–555. [Google Scholar] [CrossRef]
- Paillaud, E.; Caillet, P.; Campillo, B.; Bories, P.N. Increased risk of alteration of nutritional status in hospitalized elderly patients with advanced cancer. J. Nutr. Health Aging 2006, 10, 91–95. [Google Scholar]
- Patel, M.D.; Martin, F.C. Why don’t elderly hospital inpatients eat adequately? J. Nutr. Health Aging 2008, 12, 227–231. [Google Scholar] [CrossRef]
- Pavičić Žeželj, S.; Malec, D.; Janko-Labinac, D.; Šoić Vranić, T.; Mičetić Balog, G.; Schnurrer-Luke-Vrbanić, T.; Čaljkušić Mance, T.; Kovačević, D.; Cvijanović Peloza, O. Nutritional Risk Screening in Gastroenterological Patients at the Rijeka University Hospital Centre. Acta Clin. Croat. 2020, 59, 632–640. [Google Scholar] [CrossRef]
- Pekmezci, A.G.; Gundogan, K.; Dizdar, O.S.; Mese, E.A. Daily energy and protein intake in hospitalized patients in department of infectious diseases: A prospective observational study. Prog. Nutr. 2018, 20, 98–105. [Google Scholar] [CrossRef]
- Planas, M.; Álvarez-Hernández, J.; León-Sanz, M.; Celaya-Pérez, S.; Araujo, K.; García de Lorenzo, A. Prevalence of hospital malnutrition in cancer patients: A sub-analysis of the PREDyCES® study. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2016, 24, 429–435. [Google Scholar] [CrossRef]
- Pourhassan, M.; Babel, N.; Sieske, L.; Westhoff, T.H.; Wirth, R. Longitudinal Changes of Cytokines and Appetite in Older Hospitalized Patients. Nutrients 2021, 13, 2508. [Google Scholar] [CrossRef]
- Purnamasari, D.; Bunawan, N.C.; Suseno, D.; Rinaldi, I.; Dillon, D.H. In-hospital malnutrition among adult patients in a national referral hospital in Indonesia. Nutr. Res. Pract. 2023, 17, 218–227. [Google Scholar] [CrossRef]
- Roganovic, B.; Peric, S.; Petrovic, S.; Saric, A.R.; Roganovic, A. Risk factors for malnutrition among hospitalized gastroenterological patients. Vojnosanit. Pregl. 2022, 79, 48–54. [Google Scholar] [CrossRef]
- Sato, M.; Ido, Y.; Yoshimura, Y.; Mutai, H. Relationship of Malnutrition During Hospitalization with Functional Recovery and Postdischarge Destination in Elderly Stroke Patients. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2019, 28, 1866–1872. [Google Scholar] [CrossRef]
- Shim, H.; Cheong, J.H.; Lee, K.Y.; Lee, H.; Lee, J.G.; Noh, S.H. Perioperative nutritional status changes in gastrointestinal cancer patients. Yonsei Med. J. 2013, 54, 1370–1376. [Google Scholar] [CrossRef]
- Shimazu, S.; Yoshimura, Y.; Kudo, M.; Nagano, F.; Bise, T.; Shiraishi, A.; Sunahara, T. Frequent and personalized nutritional support leads to improved nutritional status, activities of daily living, and dysphagia after stroke. Nutrition 2021, 83, 111091. [Google Scholar] [CrossRef] [PubMed]
- Sidenvall, B.; Ek, A.C. Long-term care patients and their dietary intake related to eating ability and nutritional needs: Nursing staff interventions. J. Adv. Nurs. 1993, 18, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Sunaga, A.; Hikoso, S.; Yamada, T.; Yasumura, Y.; Tamaki, S.; Yano, M.; Hayashi, T.; Nakagawa, Y.; Nakagawa, A.; Seo, M.; et al. Change in Nutritional Status during Hospitalization and Prognosis in Patients with Heart Failure with Preserved Ejection Fraction. Nutrients 2022, 14, 4345. [Google Scholar] [CrossRef]
- Venzin, R.M.; Kamber, N.; Keller, W.C.F.; Suter, P.M.; Reinhart, W.H. How important is malnutrition? A prospective study in internal medicine. Eur. J. Clin. Nutr. 2009, 63, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.; Shankar, B.; Marshall, S.; Pearcy, J.; Somani, A.; Agarwal, E. Prevalence of malnutrition risk and poor food intake in older adults in Indian hospitals: A prospective observational nutritionDay study with novel mapping of malnutrition risk to the Malnutrition Screening Tool. Nutr. Diet. J. Dietit. Assoc. Aust. 2021, 78, 135–144. [Google Scholar] [CrossRef]
- Yeung, S.E.; Hilkewich, L.; Gillis, C.; Heine, J.A.; Fenton, T.R. Protein intakes are associated with reduced length of stay: A comparison between Enhanced Recovery After Surgery (ERAS) and conventional care after elective colorectal surgery. Am. J. Clin. Nutr. 2017, 106, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.; Zhou, X.r.; He, S.L. A multicentre study to implement nutritional risk screening and evaluate clinical outcome and quality of life in patients with cancer. Eur. J. Clin. Nutr. 2013, 67, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhao, X.; Wang, A.; Zhou, Y.; Yang, B.; Wei, N.; Yu, D.; Lu, J.; Chen, S.; Wang, Y.; et al. Emerging malnutrition during hospitalisation independently predicts poor 3-month outcomes after acute stroke: Data from a Chinese cohort. Asia Pac. J. Clin. Nutr. 2015, 24, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Li, Y.; Fang, J.; Lu, Q.; He, L. Risk factors for malnutrition in stroke patients: A meta-analysis. Clin. Nutr. 2019, 38, 127–135. [Google Scholar] [CrossRef]
- Tuffaha, H.W.; Roberts, S.; Chaboyer, W.; Gordon, L.G.; Scuffham, P.A. Cost-effectiveness Analysis of Nutritional Support for the Prevention of Pressure Ulcers in High-Risk Hospitalized Patients. Adv. Ski. Wound Care 2016, 29, 261–267. [Google Scholar] [CrossRef]
- Bell, J.J.; Young, A.M.; Hill, J.M.; Banks, M.D.; Comans, T.A.; Barnes, R.; Keller, H.H. Systematised, Interdisciplinary Malnutrition Program for impLementation and Evaluation delivers improved hospital nutrition care processes and patient reported experiences—An implementation study. Nutr. Diet. 2021, 78, 466–475. [Google Scholar] [CrossRef]
- Keller, H.; Koechl, J.M.; Laur, C.; Chen, H.; Curtis, L.; Dubin, J.A.; Gramlich, L.; Ray, S.; Valaitis, R.; Yang, Y.; et al. More-2-Eat implementation demonstrates that screening, assessment and treatment of malnourished patients can be spread and sustained in acute care; a multi-site, pretest post-test time series study. Clin. Nutr. 2021, 40, 2100–2108. [Google Scholar] [CrossRef]
- Keller, H.; Laur, C.; Atkins, M.; Bernier, P.; Butterworth, D.; Davidson, B.; Hotson, B.; Nasser, R.; Laporte, M.; Marcell, C.; et al. Update on the Integrated Nutrition Pathway for Acute Care (INPAC): Post implementation tailoring and toolkit to support practice improvements. Nutr. J. 2018, 17, 2. [Google Scholar] [CrossRef]
- Porter, J.; Hanna, L. Evidence-Based Analysis of Protected Mealtime Policies on Patient Nutrition and Care. Risk Manag. Healthc. Policy 2020, 13, 713–721. [Google Scholar] [CrossRef]
- Trinca, V.; Duizer, L.; Keller, H. Putting quality food on the tray: Factors associated with patients’ perceptions of the hospital food experience. J. Hum. Nutr. Diet. 2022, 35, 81–93. [Google Scholar] [CrossRef]
- Trinca, V.; Duizer, L.; Paré, S.; Keller, H. Investigating the patient food experience: Understanding hospital staffs’ perspectives on what leads to quality food provision in Ontario hospitals. J. Hum. Nutr. Diet. 2022, 35, 980–994. [Google Scholar] [CrossRef] [PubMed]
- Golder, H.J.; Papalois, V. Enhanced Recovery after Surgery: History, Key Advancements and Developments in Transplant Surgery. J. Clin. Med. 2021, 10, 1634. [Google Scholar] [CrossRef] [PubMed]
- Rossoni, C.; Oliveira Magro, D.; Santos, Z.C.; Cambi, M.P.C.; Patias, L.; Bragança, R.; Pellizzaro, D.; Parmar, C.; Ribeiro, R. Enhanced Recovery After Surgery (ERAS) protocol in bariatric and metabolic surgery (BMS)—Analysis of practices in nutritional aspects from five continents. Obes. Surg. 2020, 30, 4510–4518. [Google Scholar] [CrossRef] [PubMed]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.G.; et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin. Nutr. 2021, 40, 4745–4761. [Google Scholar] [CrossRef]
- Beaulieu, B.; Lamarche, Y.; Rousseau-Saine, N.; Ferland, G. Adequacy of oral intakes after cardiac surgery within an ERAS pathway: A prospective observational study. Nutr. Clin. Pract. 2025, 40, 605–615. [Google Scholar] [CrossRef]
- Ardito, F.; Lai, Q.; Rinninella, E.; Mimmo, A.; Vellone, M.; Panettieri, E.; Adducci, E.; Cintoni, M.; Mele, M.C.; Gasbarrini, A.; et al. The impact of personalized nutritional support on postoperative outcome within the enhanced recovery after surgery (ERAS) program for liver resections: Results from the NutriCatt protocol. Updates Surg. 2020, 72, 681–691. [Google Scholar] [CrossRef]
- Wunderle, C.; Siegenthaler, J.; Seres, D.; Owen-Michaane, M.; Tribolet, P.; Stanga, Z.; Mueller, B.; Schuetz, P. Adaptation of nutritional risk screening tools may better predict response to nutritional treatment: A secondary analysis of the randomized controlled trial Effect of early nutritional therapy on Frailty, Functional Outcomes, and Recovery of malnourished medical inpatients Trial (EFFORT). Am. J. Clin. Nutr. 2024, 119, 800–808. [Google Scholar] [CrossRef]

| Author, Year | Sample (n), Country | Study Design | Settings and Ward Types | Nutritional Status Measurement | Follow-Up Period | Risk Factors Examined |
|---|---|---|---|---|---|---|
| Abahuje, 2020 [16] | 279, Africa | Cohort | Surgical ward in a hospital | SGA | Weekly | Age, gender, disease diagnosis, multimorbidities, disease acuity, and length of stay |
| Akazawa, 2022 [17] | 200, Japan | Cohort | Subacute and rehabilitation wards in a hospital | Skinfold thickness | During hospital stay | Age, sex, disease diagnosis, and malnutrition risk at admission |
| Allard, 2015 [18] | 424, Canada | Cohort | Medical and surgical wards at multiple hospital sites | SGA | ≥7 days of hospitalisation | Age, sex, CCI, disease, disease acuity, appetite, and food service satisfaction |
| Alvarez Hernandez, 2012 [19] | 1707, Spain | Cohort | General, orthopedic, geriatric and rehabilitation wards at multiple hospital sites | NRS-2002 | During hospital stay | Age, BMI, polypharmacy and disease diagnosis |
| Antonelli Incalzi, 1996 [20] | 302, Italy | Cohort | Medical and geriatric wards in a hospital | SNA | Weekly | Age, BMI, number of comorbid diseases, disease diagnosis and ADL score |
| Axelsson, 1988 [21] | 100, Sweden | Cohort | Stroke unit in a hospital | Skinfold thickness | Weekly | Age, gender, disease diagnosis, disease acuity, and medical treatment |
| Borrego Utiel, 2011 [22] | 77, Spain | Case–control | Haemodialysis clinic at a hospital | Body weight | ≥4 days of hospitalisation | Age, gender, months on dialysis, CCI, disease acuity, length of stay, disease diagnosis, and medical treatment |
| Botero, 2024 [13] | 130, Australia | Cohort | Medical and surgical wards in a hospital | SGA | Weekly | Age, CCI, Frailty Index, delirium risk, and nutrition care plan prescribed or not |
| Caccialanza, 2015 [23] | 30, Italy | Case–control | Non-surgical wards in a hospital | Body weight | Not reported | Energy and protein intake, and nutritional supplementation |
| Chapple, 2016 [24] | 47, Australia | Cohort | Neuro-trauma clinic in a hospital | Body weight | Not reported | Type of nutritional support, and interruptions to dietary intake |
| Chen, 2009 [25] | 306, Taiwan | Cohort | Medical and surgical wards in a hospital | MNA | During hospital stay | Disease diagnosis, number of multimorbidities, polypharmacy, BI, length of stay, and surgical treatment |
| Cheng, 2019 [1] | 23, Australia | Cohort | In a quaternary hospital | SGA | Not reported | Age, gender, CCI, and disease diagnosis |
| Collins, 2016 [26] | 248, Australia | Cohort | Geriatric rehabilitation wards in a hospital | MNA | During hospital stay | Age, gender, functional independence, and disease diagnosis |
| Crary, 2013 [27] | 67, United States | Cohort | Stroke clinic in a hospital | MNA | Hospital stay up to 7 days | Disease diagnosis and disease acuity |
| Diendere, 2018 [28] | 222, Africa | Cohort | Stroke units in multiple hospitals | Skinfold thickness | Weekly | Age, gender, disease acuity, attempt to eat, and dietary support received |
| Flury, 2023 [29] | 252, Switzerland | Cohort | Rehabilitation ward at a hospital | SNST | Not reported | Age, gender, BMI, type of nutritional support, feeding assistance required, and disease diagnosis |
| Fu, 2017 [30] | 310, China | Cohort | Cancer ward in a hospital | NRS-2002 | Not reported | Disease acuity, appetite, and treatment-related side effects |
| Gayo, 2014 [31] | 76, Spain | Cohort | Special care clinic in a hospital | MNA | During hospital stay | Disease diagnosis, disease acuity and BI |
| Gobel, 2022 [32] | 112, Turkey | Cohort | Intensive care units at a hospital | NRS-2002 | 21 days | Age, dietary intake, and type of nutritional support |
| Graeb, 2021 [33] | 156, Germany | Cohort | Geriatric wards at 2 hospitals | MUST | During hospital stay | Age, gender, length of stay, BMI, reasons for admission, polypharmacy, multimorbidities, nutritional status prior to admission, dietary intake, reasons for reduced oral intake and nutritional support provided |
| Gubari, 2019 [34] | 64, Iran | Cohort | Intensive care unit in a hospital | SGA | Weekly | Disease acuity |
| Hafsteinsdottir, 2010 [35] | 196, Netherlands | Cohort | Neurological ward in a hospital | MNA | 10 days | Gender, disease diagnosis, polypharmacy, walking deficits, BI |
| Incalzi, 1996 [36] | 286, Italy | Cohort | Medical and geriatric wards in a hospital | Midarm circumference | During hospital stay | Dietitian support, appetite, and feedback on food service |
| Kagifuku, 2020 [37] | 26, Japan | Cohort | Cancer ward in a hospital | BIA | During hospital stay | Age, gender, perioperative BMI, cancer treatment |
| Liang, 2008 [38] | 31, Australia | Cohort | Vascular unit in a hospital | Body weight | Repeated at 5–6 days | Dietary intake and appetite |
| Lin, 2003 [39] | 61, Taiwan | Case–control | Patients at eight hospitals | Midarm circumference | Weekly | Swallowing ability and swallowing training provided |
| Lin, 2020 [40] | 465, China | Cohort | Cancer wards in a hospital | PG-SGA | Before and after chemotherapy | Treatment side effects, appetite, and disease acuity |
| Liu, 2024 [41] | 44, China | Cohort | Liver transplant ward in a hospital | NRS-2002 | Weekly | Age and frailty |
| Liu, 2016 [42] | 170, China | Cohort | Haematological ward in a hospital | NRS-2002 | Not reported | Unintentional weight loss and dietary intake changes after treatment |
| Matsumoto, 2022 [43] | 257, Japan | Cohort | Rehabilitation ward in a hospital | GNRI | During hospital stay | Nutritional status at admission, disease diagnosis, rehabilitation therapy performed, functional dependence, dietary intake, CCI, length of stay, polypharmacy, and swallowing function |
| Mosselman, 2013 [44] | 73, Netherlands | Cohort | Neurological ward in a hospital | MNA | 10 days | Gender, discharge destination, disease type, swallowing abilities, and BI |
| Nematy, 2013 [45] | 114, Iran | Cohort | Medical wards in a hospital | NRS-2002 | 7–10 days | Age, gender, disease diagnosis, and dietary intake |
| Padillo, 1999 [46] | 39, Spain | Cohort | Medical ward in a hospital | Skinfold thickness | During hospital stay | Disease acuity and dietary intake |
| Paillaud, 2006 [47] | 88, France | Cohort | Advanced cancer ward in a hospital | Skinfold thickness | Monthly | Dietary intake and physical functional status |
| Patel, 2008 [48] | 100, United Kingdom | Cohort | Geriatric ward in a hospital | Body weight | Monthly | Disease acuity and reasons for inadequate dietary intake |
| Pavicic Zezelj, 2020 [49] | 160, Croatia | Cohort | Medical wards in a hospital | NRS-2002 | During hospital stay | Type of nutritional support and dietary intake |
| Pekmezci, 2018 [50] | 47, Turkey | Cohort | Infectious disease wards in a hospital | NRS-2002 | Weekly | Age, gender, dietary intake and length of hospital stay |
| Planas, 2016 [51] | 401, Spain | Cross-sectional | Oncological ward at multiple hospitals | NRS-2002 | During hospital stay | Age and BMI at admission |
| Pourhassan, 2021 [52] | 191, Germany | Cohort | Geriatric wards in a hospital | MNA-SF | During hospital stay | Age, gender, disease acuity, CCI, appetite and dietary intake |
| Purnamasari, 2023 [53] | 55, Indonesia | Cohort | Medical wards in a hospital | Body weight | During hospital stay | Reasons for fasting during hospitalisation and length of stay |
| Roganovic, 2022 [54] | 650, Serbia | Cohort | Medical wards in a hospital | Skinfold thickness | During hospital stay | Gender, disease diagnosis, disease acuity, length of stay, nutritional status at admission and mobility worsening |
| Sato, 2019 [55] | 205, Japan | Cohort | Acute wards in a hospital | GNRI | During hospital stay | Age, BI and disease diagnosis |
| Shim, 2013 [56] | 435, Korea | Cohort | Cancer wards in a hospital | PG-SGA | Weekly | Age, gender, preoperative weight loss, cancer type and treatment type |
| Shimazu, 2021 [57] | 426, Japan | Cohort | Rehabilitation ward in a hospital | BIA | During hospital stay | Age, gender, disease diagnosis, CCI, dietary intake, dietary prescription frequency, length of stay |
| Sidenvall, 1993 [58] | 18, Sweden | Cohort | Geriatric ward in a hospital | Body weight | During hospital stay | Nutritional support from a multidisciplinary team |
| Sunaga, 2022 [59] | 982, Japan | Cohort | Cardiac ward in multiple hospital sites | GNRI | During hospital stay | Age, gender, disease acuity, length of stay, frailty and disease diagnosis |
| Venzin, 2009 [60] | 211, Switzerland | Cohort | Medical ward in a hospital | Body weight | During hospital stay | Treatment type, fasting for diagnostic reasons, disease diagnosis, disease acuity, and nutritional treatment plan |
| Wright, 2021 [61] | 262, Indian | Cohort | Geriatric wards at five hospitals | MST | During hospital stay | Nutritional support received and nutritional status before admission |
| Yeung, 2017 [62] | 115, Canada | Cohort | Colorectal wards at two hospitals | MST | During hospital stay | Dietary intake and ERAS protocol implemented or not |
| Yu, 2013 [63] | 687, China | Cohort | Surgical wards at two hospitals | NRS-2002 | Two weeks or until the time of discharge | Disease type and disease acuity |
| Zhang, 2015 [64] | 760, China | Cohort | Stroke units at eight hospitals | BMI | Two weeks | Age, gender, disease diagnosis, type of nutritional support, disease acuity and dysphagia |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheung, V.H.I.; Wan, C.S. A Scoping Review of Contextual and Individual Factors for Hospital-Acquired Malnutrition Development in Adult Hospital Inpatients: Guiding a Proactive Preventative Approach. Nutrients 2025, 17, 2970. https://doi.org/10.3390/nu17182970
Cheung VHI, Wan CS. A Scoping Review of Contextual and Individual Factors for Hospital-Acquired Malnutrition Development in Adult Hospital Inpatients: Guiding a Proactive Preventative Approach. Nutrients. 2025; 17(18):2970. https://doi.org/10.3390/nu17182970
Chicago/Turabian StyleCheung, Vivien Hui In, and Ching Shan Wan. 2025. "A Scoping Review of Contextual and Individual Factors for Hospital-Acquired Malnutrition Development in Adult Hospital Inpatients: Guiding a Proactive Preventative Approach" Nutrients 17, no. 18: 2970. https://doi.org/10.3390/nu17182970
APA StyleCheung, V. H. I., & Wan, C. S. (2025). A Scoping Review of Contextual and Individual Factors for Hospital-Acquired Malnutrition Development in Adult Hospital Inpatients: Guiding a Proactive Preventative Approach. Nutrients, 17(18), 2970. https://doi.org/10.3390/nu17182970








