The Effect of Portion Size Interventions on Energy Intake and Risk of Obesity in School-Aged Children: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Extraction
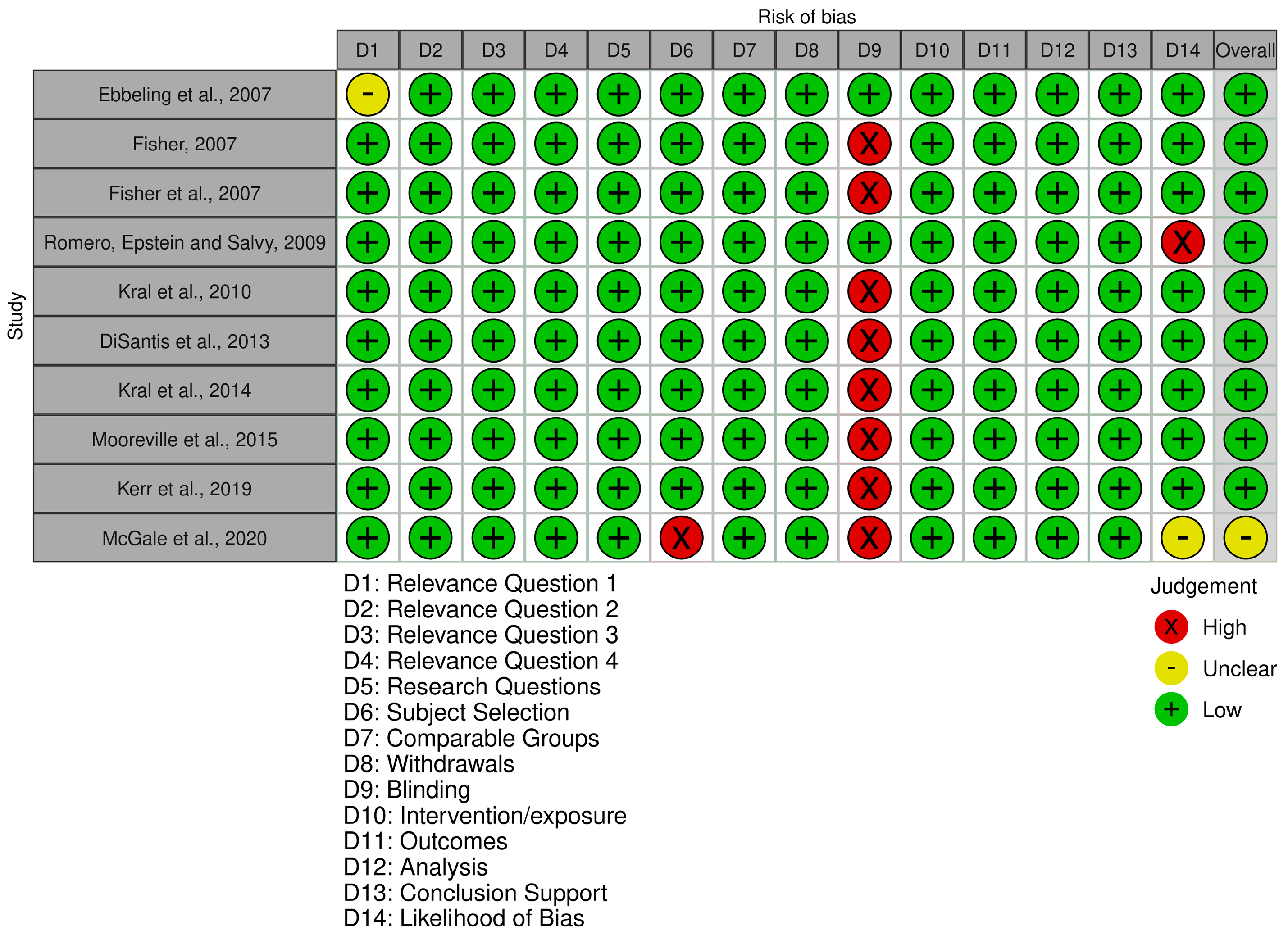
2.4. Risk of Bias Assessment
2.5. Synthesis of Results, Heterogeneity, and Reporting Bias Assessment
3. Results
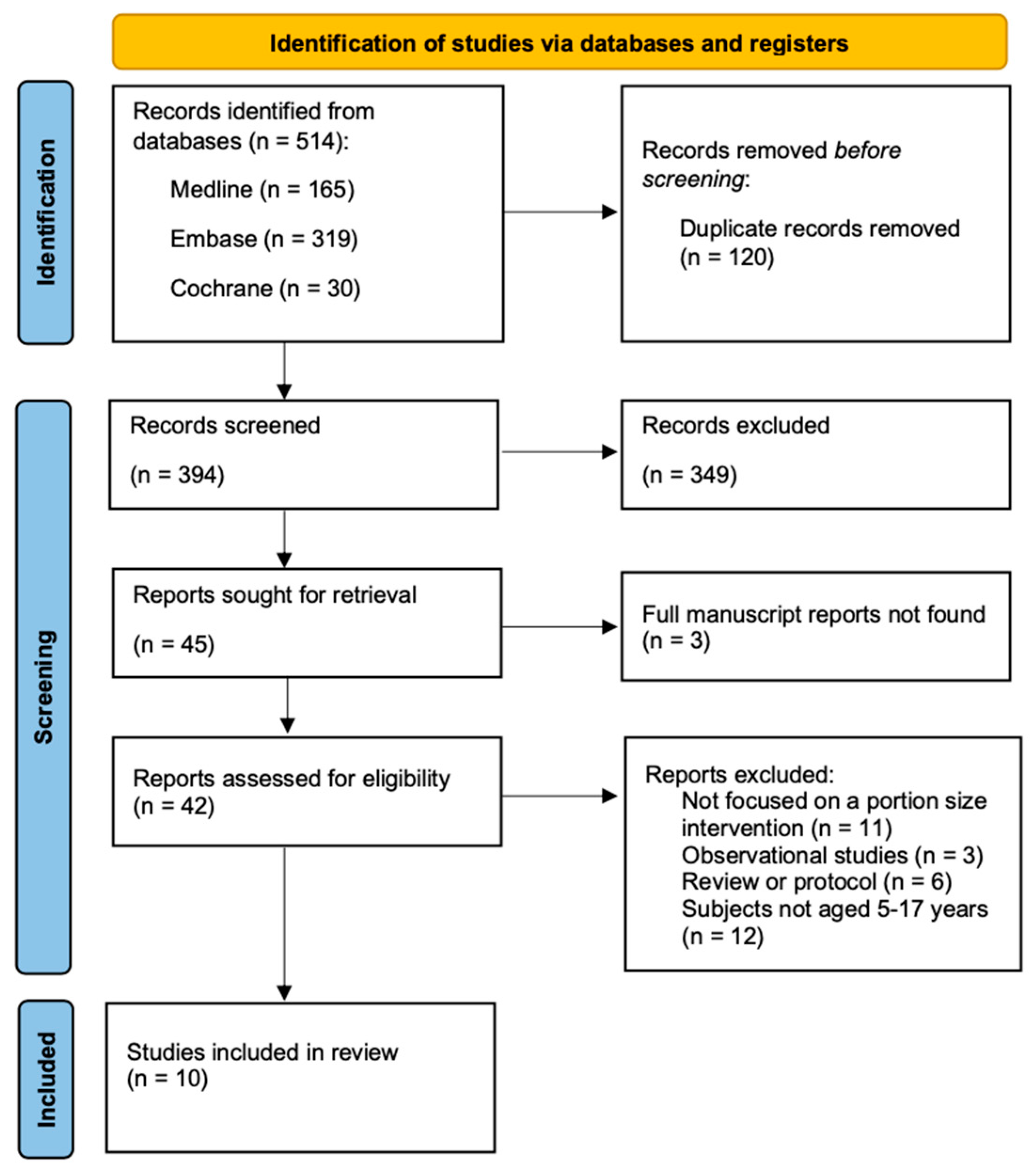
3.1. Results of Study Selection
3.2. Results of Quality Assessment
3.3. Characteristics of Studies
3.4. The Effect of Portion Size Intervention on Energy Intake in School-Aged Children
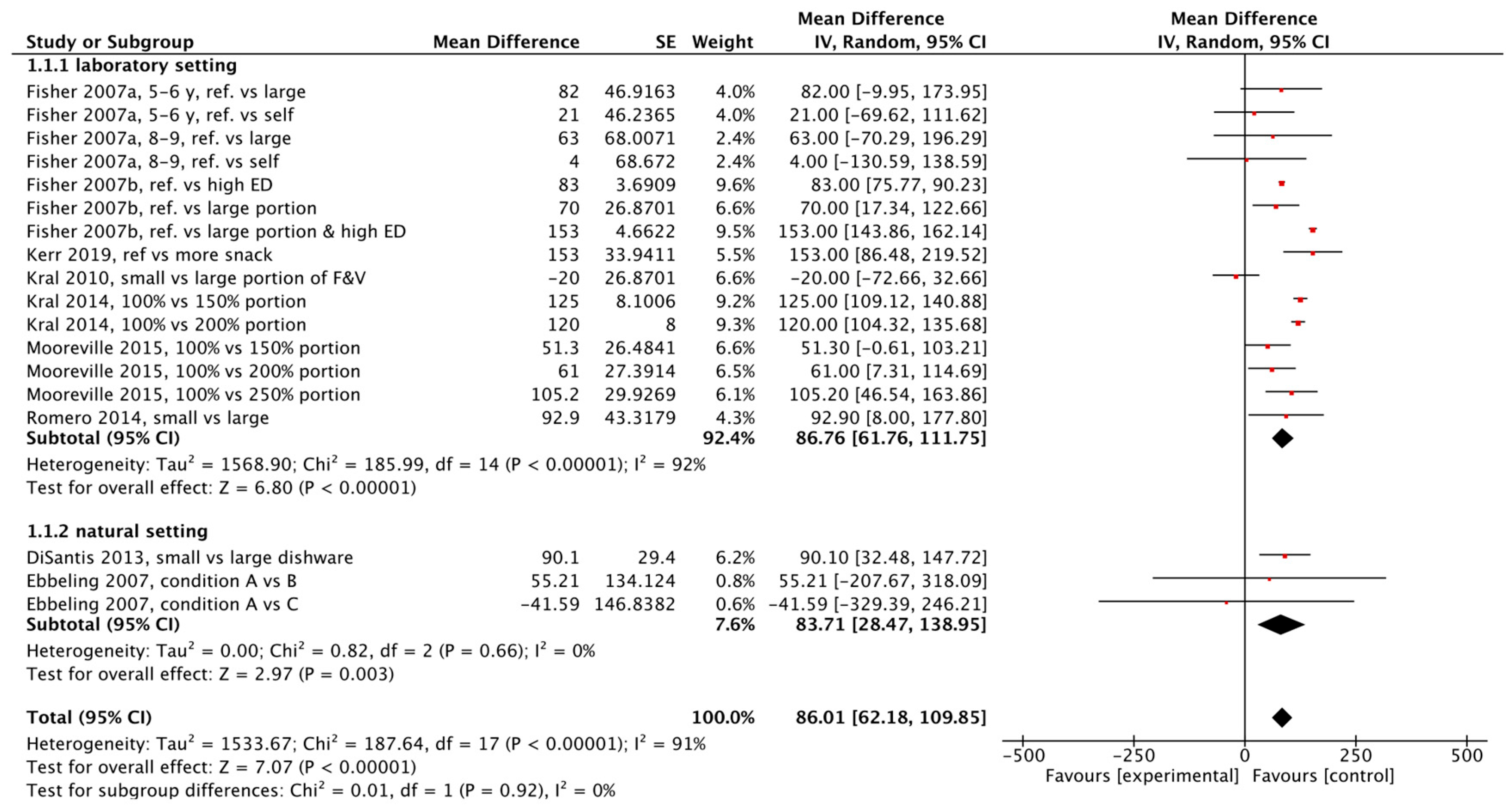
3.5. Results of Meta-Analysis
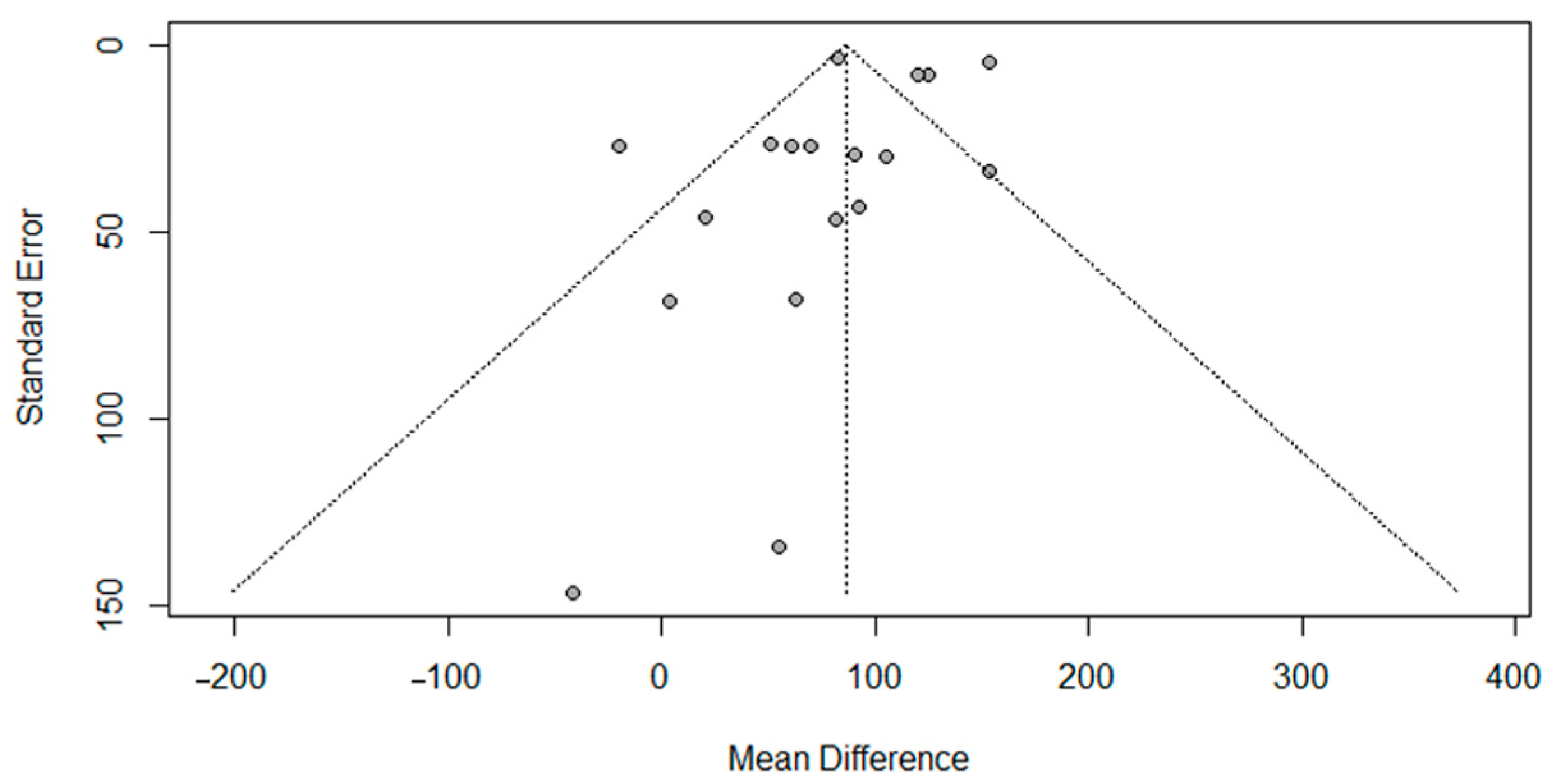
3.6. Results of Reporting Bias Assessment
4. Discussion
4.1. Summary of Main Findings
4.2. The Portion Size Effect on Energy Intake in School-Aged Children
4.3. Factors Affecting Susceptibility to Larger Portion Sizes
5. Strengths and Limitations
5.1. Strengths and Limitations of Included Studies
5.2. Strengths and Limitations of This Review
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 30 July 2024).
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The Epidemiological Burden of Obesity in Childhood: A Worldwide Epidemic Requiring Urgent Action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in Children and Adolescents: Epidemiology, Causes, Assessment, and Management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.D.; Fu, E.; Kobayashi, M.A. Prevention and Management of Childhood Obesity and Its Psychological and Health Comorbidities. Annu. Rev. Clin. Psychol. 2020, 16, 351–378. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting Adult Obesity from Childhood Obesity: A Systematic Review and Meta-Analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Morales Camacho, W.J.; Molina Díaz, J.M.; Plata Ortiz, S.; Plata Ortiz, J.E.; Morales Camacho, M.A.; Calderón, B.P. Childhood Obesity: Aetiology, Comorbidities, and Treatment. Diabetes Metab. Res. Rev. 2019, 35, e3203. [Google Scholar] [CrossRef] [PubMed]
- Benton, D. Portion Size: What We Know and What We Need to Know. Crit. Rev. Food Sci. Nutr. 2015, 55, 988–1004. [Google Scholar] [CrossRef]
- Zlatevska, N.; Dubelaar, C.; Holden, S.S. Sizing Up the Effect of Portion Size on Consumption: A Meta-Analytic Review. J. Mark. 2014, 78, 140–154. [Google Scholar] [CrossRef]
- Reale, S.; Hamilton, J.; Akparibo, R.; Hetherington, M.M.; Cecil, J.E.; Caton, S.J. The Effect of Food Type on the Portion Size Effect in Children Aged 2–12 Years: A Systematic Review and Meta-Analysis. Appetite 2019, 137, 47–61. [Google Scholar] [CrossRef]
- Higgins, K.A.; Hudson, J.L.; Hayes, A.M.R.; Braun, E.; Cheon, E.; Couture, S.C.; Gunaratna, N.S.; Hill, E.R.; Hunter, S.R.; McGowan, B.S.; et al. Systematic Review and Meta-Analysis on the Effect of Portion Size and Ingestive Frequency on Energy Intake and Body Weight among Adults in Randomized Controlled Feeding Trials. Adv. Nutr. 2022, 13, 248–268. [Google Scholar] [CrossRef]
- Small, L.; Lane, H.; Vaughan, L.; Melnyk, B.; Mcburnett, D. A Systematic Review of the Evidence: The Effects of Portion Size Manipulation with Children and Portion Education/Training Interventions on Dietary Intake with Adults. Worldviews Evid. Based Nurs. 2013, 10, 69–81. [Google Scholar] [CrossRef]
- Albar, S.A.; Alwan, N.A.; Evans, C.E.L.; Cade, J.E. Is There an Association between Food Portion Size and BMI among British Adolescents? Br. J. Nutr. 2014, 112, 841–851. [Google Scholar] [CrossRef]
- Dobrescu, A.T.; Porter, A.; Ferriday, D.; Rogers, P.J. A systematic review of the relationship between portion size and indexes of adiposity in children. Appetite 2025, 26, e13928. [Google Scholar] [CrossRef] [PubMed]
- Marteau, T.M.; Hollands, G.J.; Shemilt, I.; Jebb, S.A. Downsizing: Policy Options to Reduce Portion Sizes to Help Tackle Obesity. BMJ 2015, 351, h5863. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Limiting Portion Sizes to Reduce the Risk of Childhood Overweight and Obesity 2014. Available online: https://www.who.int/tools/elena/bbc/portion-childhood-obesity (accessed on 30 July 2024).
- Scientific Advisory Committee on Nutrition. Feeding Young Children Aged 1 to 5 Years—Summary Report 2024. Available online: https://www.gov.uk/government/publications/sacn-report-feeding-young-children-aged-1-to-5-years/feeding-young-children-aged-1-to-5-years-summary-report (accessed on 30 July 2024).
- Parasuraman, S.R.; Ghandour, R.M.; Kogan, M.D. Epidemiological Profile of Health and Behaviors in Middle Childhood. Pediatrics 2020, 145, e20192244. [Google Scholar] [CrossRef]
- Handu, D.; Moloney, L.; Wolfram, T.; Ziegler, P.; Acosta, A.; Steiber, A. Academy of Nutrition and Dietetics Methodology for Conducting Systematic Reviews for the Evidence Analysis Library. J. Acad. Nutr. Diet. 2016, 116, 311–318. [Google Scholar] [CrossRef]
- Ebbeling, C.B.; Garcia-Lago, E.; Leidig, M.M.; Seger-Shippee, L.G.; Feldman, H.A.; Ludwig, D.S. Altering Portion Sizes and Eating Rate to Attenuate Gorging during a Fast Food Meal: Effects on Energy Intake. Pediatrics 2007, 119, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.O. Effects of Age on Children’s Intake of Large and Self-Selected Food Portions. Obesity 2007, 15, 403–412. [Google Scholar] [CrossRef]
- Fisher, J.O.; Liu, Y.; Birch, L.L.; Rolls, B.J. Effects of Portion Size and Energy Density on Young Children’s Intake at a Meal. Am. J. Clin. Nutr. 2007, 86, 174–179. [Google Scholar] [CrossRef]
- Romero, N.D.; Epstein, L.H.; Salvy, S.J. Peer Modeling Influences Girls’ Snack Intake. J. Am. Diet. Assoc. 2009, 109, 133–136. [Google Scholar] [CrossRef]
- Kral, T.V.E.; Kabay, A.C.; Roe, L.S.; Rolls, B.J. Effects of Doubling the Portion Size of Fruit and Vegetable Side Dishes on Children’s Intake at a Meal. Obesity 2010, 18, 521–527. [Google Scholar] [CrossRef]
- DiSantis, K.I.; Birch, L.L.; Davey, A.; Serrano, E.L.; Zhang, J.; Bruton, Y.; Fisher, J.O. Plate Size and Children’s Appetite: Effects of Larger Dishware on Self-Served Portions and Intake. Pediatrics 2013, 131, e1451–e1458. [Google Scholar] [CrossRef] [PubMed]
- Kral, T.V.E.; Remiker, A.M.; Strutz, E.M.; Moore, R.H. Role of Child Weight Status and the Relative Reinforcing Value of Food in Children’s Response to Portion Size Increases. Obesity 2014, 22, 1716–1722. [Google Scholar] [CrossRef] [PubMed]
- Mooreville, M.; Davey, A.; Orloski, A.; Hannah, E.L.; Mathias, K.C.; Birch, L.L.; Kral, T.V.E.; Zakeri, I.F.; Fisher, J.O. Individual Differences in Susceptibility to Large Portion Sizes among Obese and Normal-Weight Children. Obesity 2015, 23, 808–814. [Google Scholar] [CrossRef]
- Kerr, J.A.; Jansen, P.W.; Mensah, F.K.; Gibbons, K.; Olds, T.S.; Carlin, J.B.; Clifford, S.A.; Burgner, D.; Gold, L.; Baur, L.A.; et al. Child and Adult Snack Food Intake in Response to Manipulated Pre-Packaged Snack Item Quantity/Variety and Snack Box Size: A Population-Based Randomized Trial. Int. J. Obes. 2019, 43, 1891–1902. [Google Scholar] [CrossRef]
- McGale, L.S.; Smits, T.; Halford, J.C.G.; Harrold, J.A.; Boyland, E.J. The Influence of Front-of-Pack Portion Size Images on Children’s Serving and Intake of Cereal. Pediatr. Obes. 2020, 15, e12583. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (Robvis): An R Package and Shiny Web App for Visualizing Risk-of-bias Assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Van Den Berg, S.W.; Boer, J.M.A.; Scholtens, S.; De Jongste, J.C.; Brunekreef, B.; Smit, H.A.; Wijga, A.H. Quantification of the Energy Gap in Young Overweight Children. the PIAMA Birth Cohort Study. BMC Public Health 2011, 11, 326. [Google Scholar] [CrossRef]
- Plachta-Danielzik, S.; Landsberg, B.; Bosy-Westphal, A.; Johannsen, M.; Lange, D.; Müller, M.J. Energy Gain and Energy Gap in Normal-Weight Children: Longitudinal Data of the KOPS. Obesity 2008, 16, 777–783. [Google Scholar] [CrossRef]
- Hall, K.D.; Butte, N.F.; Swinburn, B.A.; Chow, C.C. Dynamics of Childhood Growth and Obesity: Development and Validation of a Quantitative Mathematical Model. Lancet Diabetes Endocrinol. 2013, 1, 97–105. [Google Scholar] [CrossRef]
- Norman, J.; Kelly, B.; McMahon, A.T.; Boyland, E.; Baur, L.A.; Chapman, K.; King, L.; Hughes, C.; Bauman, A. Sustained Impact of Energy-Dense TV and Online Food Advertising on Children’s Dietary Intake: A within-Subject, Randomised, Crossover, Counter-Balanced Trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- Steenhuis, I.; Poelman, M. Portion Size: Latest Developments and Interventions. Curr. Obes. Rep. 2017, 6, 10–17. [Google Scholar] [CrossRef]
- English, L.; Lasschuijt, M.; Keller, K.L. Mechanisms of the Portion Size Effect. What Is Known and Where Do We Go from Here? Appetite 2015, 88, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Cruwys, T.; Bevelander, K.E.; Hermans, R.C.J. Social Modeling of Eating: A Review of When and Why Social Influence Affects Food Intake and Choice. Appetite 2015, 86, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.L.; Kral, T.V.E.; Rolls, B.J. Impacts of Energy Density and Portion Size on Satiation and Satiety. In Satiation, Satiety and the Control of Food Intake; Elsevier: Amsterdam, The Netherlands, 2013; pp. 115–127. [Google Scholar]
- Klos, B.; Cook, J.; Crepaz, L.; Weiland, A.; Zipfel, S.; Mack, I. Impact of Energy Density on Energy Intake in Children and Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. J. Nutr. 2023, 62, 1059–1076. [Google Scholar] [CrossRef]
- Johnson, F.; Wardle, J. Variety, Palatability, and Obesity. Adv. Nutr. 2014, 5, 851–859. [Google Scholar] [CrossRef]
- Miller, N.; Reicks, M.; Redden, J.P.; Mann, T.; Mykerezi, E.; Vickers, Z. Increasing Portion Sizes of Fruits and Vegetables in an Elementary School Lunch Program Can Increase Fruit and Vegetable Consumption. Appetite 2015, 91, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Roe, L.S.; Sanchez, C.E.; Smethers, A.D.; Keller, K.L.; Rolls, B.J. Portion Size Can Be Used Strategically to Increase Intake of Vegetables and Fruits in Young Children over Multiple Days: A Cluster-Randomized Crossover Trial. Am. J. Clin. Nutr. 2022, 115, 272–283. [Google Scholar] [CrossRef]
- Rolls, B.J.; Roe, L.S.; Meengs, J.S. Portion Size Can Be Used Strategically to Increase Vegetable Consumption in Adults. Am. J. Clin. Nutr. 2010, 91, 913–922. [Google Scholar] [CrossRef]
- Rolls, B.J.; Morris, E.L.; Roe, L.S. Portion Size of Food Affects Energy Intake in Normal-Weight and Overweight Men and Women. Am. J. Clin. Nutr. 2002, 76, 1207–1220. [Google Scholar] [CrossRef]
- Smethers, A.D.; Roe, L.S.; Sanchez, C.E.; Zuraikat, F.M.; Keller, K.L.; Kling, S.M.R.; Rolls, B.J. Portion Size Has Sustained Effects over 5 Days in Preschool Children: A Randomized Trial. Am. J. Clin. Nutr. 2019, 109, 1361–1372. [Google Scholar] [CrossRef]
- Smith, L.; Conroy, K.; Wen, H.; Rui, L.; Humphries, D. Portion Size Variably Affects Food Intake of 6-Year-Old and 4-Year-Old Children in Kunming, China. Appetite 2013, 69, 31–38. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCrickerd, K.; Leong, C.; Forde, C.G. Preschool Children’s Sensitivity to Teacher-Served Portion Size Is Linked to Age Related Differences in Leftovers. Appetite 2017, 114, 320–328. [Google Scholar] [CrossRef]
- Blundell-Birtill, P.; Hetherington, M.M. Determinants of Portion Size in Children and Adolescents: Insights from the UK National Diet and Nutrition Survey Rolling Programme (2008–2016). Nutrients 2019, 11, 2957. [Google Scholar] [CrossRef]
- Langfield, T.; Clarke, K.; Marty, L.; Jones, A.; Robinson, E. Socioeconomic Position and the Influence of Food Portion Size on Daily Energy Intake in Adult Females: Two Randomized Controlled Trials. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 53. [Google Scholar] [CrossRef]
- Tsoi, M.-F.; Li, H.-L.; Feng, Q.; Cheung, C.-L.; Cheung, T.T.; Cheung, B.M.Y. Prevalence of Childhood Obesity in the United States in 1999–2018: A 20-Year Analysis. Obes. Facts 2022, 15, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J.; Roe, L.S.; Meengs, J.S. Larger Portion Sizes Lead to a Sustained Increase in Energy Intake over 2 Days. J. Am. Diet. Assoc. 2006, 106, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J.; Roe, L.S.; Meengs, J.S. The Effect of Large Portion Sizes on Energy Intake Is Sustained for 11 Days. Obesity 2007, 15, 1535–1543. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | School-aged children (5–17 years old) | Pre-school children (<5 years) or adults |
| Children without underlying medical conditions | Children with other diseases | |
| Intervention | Focus on the interventions that affect portion size | No intervention on portion size variation |
| Outcome | The outcome variable was the quantitative assessment of dietary intake (gram), energy intake (kcal or kJ), body weight (kg), or body mass index (BMI) | The outcome variable was not the quantitative assessment of dietary intake, energy intake, body weight, or BMI |
| Study Types | Experimental trials (randomised), controlled studies, quasi-randomised trials, or a crossover design | Non-experimental or non-controlled studies, reviews, or qualitative studies |
| Original articles written in English | Original articles written in other languages |
| Citation, Title, Location, Design | Objective, Sample Size, Intervention Method, Eating Setting | Intervention Period, Outcome Evaluation, Follow-Up | Main Findings 1 | Strengths and Limitations |
|---|---|---|---|---|
| ① Ebbeling et al., 2007 [19] Title: “Altering portion sizes and eating rate to attenuate gorging during a fast-food meal: Effects on energy intake” Location: Boston, Massachusetts Design: Randomised crossover design | Objective: To evaluate whether reducing portion sizes and slower eating rate can decrease energy intake when children are offered a fast-food meal. Sample size: 18 adolescents (14 female, 4 male) aged 13–17 years who reported consuming fast food ≥1 x per week. Intervention method: Fast food meals (chicken nuggets, French fries, ketchup, sweet and sour sauce, and cola) were presented in 3 conditions at different time points: 1 large serving (condition A), portioned into 4 smaller servings (condition B), and portioned into 4 smaller servings served at every 15 min intervals (condition C). The total amounts of foods and beverage given was the same over the study period (5691 kJ). Eating setting: Lunch meal in food court. | Intervention period: 4 sessions over the summer of 2005 (exact period not given). Outcome evaluation: Energy intake (kJ) and meal size rating of each meal. Follow-up: Dietary and physical activity data were collected by telephone 2 days after each visit. | Children consumed different amounts of energy in the 3 different conditions (mean ± SEM: condition A = 5552 ± 357 kJ; condition B = 5321 ± 433 kJ; condition C = 5762 ± 500 kJ), but the difference was not statistically significant (p = 0.5). However, they consumed ~5460 kJ (~50% of energy needs) under all conditions which indicates that the children were overeating. | Strengths: (1) Natural eating setting which minimised confounding factors; (2) Participant conditioning before intervention: eating a standard breakfast of cereal and cold milk, abstaining from foods and drinks until the time of the study visit; (3) Blinding of the interviewer. Limitations: (1) Small sample size which limits generalisability of findings; (2) Only evaluated 1 combination of fast-food items; (3) Homogenous study sample (majority were of black ethnicity). |
| ② Fisher, 2007 [20] Title: “Effects of age on children’s intake of large and self-selected food portions” Location: Houston, Texas Design: Between-subjects design (age group) with a within-subject component (portion size). Each child in three age groups was randomly assigned into three portion size sequences. | Objective: To determine the effects of age on children’s responsiveness to large and self-selected portions. Sample size: 75 children (44 boys, 31 girls) in 3 age groups: 2–3, 5–6, and 8–9 years old. Intervention method: Children were served with main entrée of macaroni and cheese that varied across 3 portion sizes: a reference condition, a large condition (portion was doubled), and a self-selected condition (portion was doubled but served in an individual serving dish). Portion sizes of other foods and drinks were held constant. Eating setting: Dinner meal in “USDA Children’s Nutrition Research Center’s Children’s Eating Laboratory”. | Intervention period: Once a week for 3 weeks Outcome evaluation: Energy intake (kcal) of each meal, children’s comment on portion size, children’s bite size and frequency. Follow-up: No follow-up (intake was estimated immediately after each meal). |
| Strengths: (1) Relatively large sample size; (2) Clear age grouping; (3) Portions are age-appropriate; (4) Participant conditioning before intervention: abstaining from foods and drinks for prior 2 h. Limitations: (1) Conducted in a laboratory setting; (2) No follow-up data collected; (3) 14 children were excluded from the analysis because of zero intake of the main entrée; (4) Homogenous study sample (all children were non-Hispanic white). |
| ③ Fisher et al., 2007 [21] Title: “Effects of portion size and energy density on young children’s intake at a meal” Location: Houston, Texas Design: 2 (portion size) x 2 (energy density) within-subjects factorial design. Randomisation of feeding condition sequences. | Objective: To investigate the effects of entrée portion size and energy density on satiation in children. Sample size: 53 children (28 girls, 25 boys) aged 5–6 years old. Intervention method: Children were served a single meal with macaroni and cheese as main entrée in 4 conditions with variation in the portion size (250 or 500 g), and energy density (1.3 or 1.8 kcal/g). Other foods were constant. Eating setting: Dinner time in “USDA Children’s Nutrition Research Center’s Children’s Eating Laboratory”. | Intervention period: Once a week for 4 weeks. Outcome evaluation: Food intake (g) and energy intake (kcal) of each meal. Follow-up: No follow up (intake was estimated immediately after each meal). |
| Strengths: (1) Familiarisation of laboratory setting before testing; (2) Children’s conditioning before intervention: abstaining from foods and drinks for the prior 2 h; (3) Food quantitative sensory tests before testing; (4) Diverse ethnicity of study participants. Limitations: (1) Small age range of children; (2) Conducted in laboratory setting; (3) No follow-up data collected. |
| ④ Romero, Epstein, and Salvy, 2009 [22] Title: “Peer Modelling influences girls’ snack intake” Location: New York, NY, USA Design: 2 (weight status) × 2 (portion size) between-group factorial design. Randomisation of participants to intervention condition. | Objective: To assess how peer modelling influences eating in preadolescent girls with normal weight and overweight. Sample size: 44 girls (22 overweight, 22 normal weight) aged 8–12 years. Intervention method: Portion sizes were varied by showing a video in which a model consumed either a small (29 g/1 oz, 10 bite-sized cookies) or a large (223 g/8 oz, 77 bite-sized cookies) serving. Each participant was provided with the same amount of cookies (8 oz). 1 cookie (2.9 g) = 14.03 kcal. Eating setting: Snack meal in laboratory. | Intervention period: One visit (exact period not given) Outcome evaluation: Cookie intake (gram), hunger, and food-liking rating. Follow-up: No follow up (intake was estimated immediately after each meal). | Girls with overweight consumed significantly more cookies than girls with normal weight (60.5 ± 35.1 g vs. 41.7 ± 23.2 g; p < 0.05). Furthermore, girls exposed to the small portion size condition consumed fewer cookies than girls exposed to the large portion size (41.5 ± 27.2 g vs. 60.7 ± 32.0; p < 0.05). However, the interaction of weight status by portion size condition was not statistically significant (p = 0.2) which indicates that video model affects both girls with normal weight and those with overweight. | Strengths: (1) Comparison of individual variance (weight status); (2) Children’s conditioning before intervention: abstain from food and drinks for 2 h; (3) Blinding of the experimenter. Limitations: (1) Homogenous sample (all females, most were white); (2) Eating time limitation (10 min) for participant might affect eating behaviour; (3) Not involving a “no video” comparison group; (4) Not assessing energy intake; (5) Only analysing 1 type of food. |
| ⑤ Kral et al., 2010 [23] Title: “Effects of doubling the portion size of fruit and vegetable side dishes on children’s intake at a meal” Location: Philadelphia, Pennsylvania Design: Randomised crossover design | Objective: (1) To evaluate the impacts of doubling the fruit and vegetable portion size on children’s fruit and vegetable consumption; (2) To determine how fruit and vegetable portion size variation affects total meal energy intake. Sample size: 43 children (21 girls, 22 boys), aged 5–6 years. Intervention method: Children were served dinner meal which consisted of pasta with tomato sauce, fruit and vegetable side dishes (broccoli, carrots, and applesauce), and milk. The fruit and vegetable portion size was doubled between the experimental conditions, while other foods remained constant. Eating Setting: Dinner time in “Centre for Weight and Eating Disorders at the University of Pennsylvania”. | Intervention period: Once a week for 2 weeks. Outcome evaluation: Food intake (g), energy intake (kcal), and energy density (kcal/g) at each meal; taste preference. Follow-up: No follow up (intake was estimated immediately after each meal). | (1) Doubling the portion size of fruit and vegetable side dish increased the intake of apple sauce (43%, 36.1 ± 9.9 g, p = 0.001), but not broccoli (p = 0.7) and carrots (p = 0.6). There was no significant interaction between weight status and fruit and vegetable portion size. (2) The difference in total meal energy intake between doubled fruit and vegetable portion and reference was not statistically significant (446 ± 19 kcal vs. 426 ± 19 kcal; p = 0.2), but there was a significant decrease in the overall energy density when fruit and vegetable portion was doubled (from 0.95 ± 0.02 to 0.89 ± 0.02 kcal/g; p = 0.005). Furthermore, girls had significantly less total energy intake than boys when served large fruit and vegetable portion (p = 0.01). Food preferences may moderate the effect of portion size and fruit & vegetable intake. | Strengths: (1) Adjusting fruit and vegetable intake analysis with preference and liking of foods; (2) Familiarisation of setting for children before testing; (3) Children conditioning before intervention: abstain from food and drinks for 2 h. Limitations: (1) Using puree fruit (apple sauce) instead of solid fruit which may influence preference and satiety; (2) Narrow age range of children and exclusion of children who disliked most foods which limits generalisability of findings; (3) Homogenous study sample (majority were Black or African American). |
| ⑥ DiSantis et al., 2013 [24] Title: “Plate size and children’s appetite: Effects of larger dishware on self-served portions and intake” Location: Philadelphia, Pennsylvania Design: Within-subjects experimental design. Randomisation of feeding condition order. | Objective: (1) Determine dishware size effects on self-served portion sizes and energy intake of young children; (2) Identify children’s characteristics who responded to more food with larger dishware. Sample size: 42 first-grade elementary students (exact age was not given). Intervention method: Children served themselves using either child or adult-size dishware (double in size and volume) in a buffet type line. Entrée of amorphous (pasta with meat sauce) and unit form (chicken nuggets) were served on separate days, whereas fruit and vegetable were self-served at all meals. Bread and milk were served in fixed portions. Eating setting: Lunch time in school classroom. | Intervention period: Once a week for 8 weeks Outcome evaluation: Energy intake (kcal) of each meal, food-liking assessment. Follow-up: No follow up (intake was estimated immediately after each meal) | There was a difference in total energy intake between the dishware sizes (p = 0.002). On average, children consumed 90.1 kcal (SE = 29.4 kcal) more when using adult-size dishware, and this effect was seen in 80% of children. Type of entrée also influenced the total energy intake, where children had higher energy intake when unit entrée was offered compared to amorphous entrée (p = 0.001). Based on each type of food, children served themselves more entrée (+57.6 kcal, SE = 19.7 kcal) and more fruit (+15.7 kcal, SE = 6.3 kcal) when using adult-size than child-size dishware (p < 0.05), but there was no effect on vegetable intake. Furthermore, food insecurity was a significant predictor of large portion size (p = 0.04), whereas sex and body mass index (BMI) showed no significant association. | Strengths: (1) Natural eating setting (school lunch); (2) Familiarisation of procedure for children before intervention; (3) Analysis models were adjusted for entrée type, child’s sex and weight status, food insecurity, and child’s food-liking. Limitations: (1) Randomisation of condition order only in the classroom level, not for individual children; (2) Children’s behaviour of self-serving food may vary; (3) Homogenous study sample (majority were African American). |
| ⑦ Kral et al., 2014 [25] Title: “Role of child weight status and the relative reinforcing value of food in children’s response to portion size increases” Location: Philadelphia, Pennsylvania Design: Randomised crossover design | Objective: To compare energy intake at a meal between children with normal-weight and children with obesity when the portion size of energy-dense foods was increased. Sample size: 50 children (25 normal-weight, 25 obese) aged 8–10 years old. Intervention method: Children were served dinner meal (chicken nuggets, hash browns, ketchup, green beans, brownies) which varied across 3 portion sizes (100%, 150%, 200%). Eating setting: Dinner in “Centre for Weight and Eating Disorders at University of Pennsylvania”. | Intervention period: Once a week for 3 weeks. Outcome evaluation: Energy intake (kcal) at each meal, taste preference of all foods given. Follow-up: No follow-up (intake was estimated immediately after each meal). | Total energy intake (mean ± SD) across the 100, 150, and 200% portion sizes, with children’s weight groups combined, were 921 ± 40, 1046 ± 41, and 1041 ± 40 kcal, respectively. While there was a trend suggesting that children with obesity were more responsive to portion size changes, this difference was not statistically significant (p = 0.1), meaning that children in all weight status consumed more calories in response to larger portion sizes (>50–60% of estimated energy requirements). | Strengths: (1) Assessing multiple components of children’s response to portion size; (2) Familiarisation and children’s conditioning: abstain from food and drinks for 2 h before testing. Limitations: (1) Relatively small sample size; (2) Conducted in laboratory setting; (3) No follow up or longitudinal data collected; (4) Children’s variation in hunger level which may impact intake at meals. |
| ⑧ Mooreville et al., 2015 [26] Title: “Individual differences in susceptibility to large portion sizes among obese and normal-weight children” Location: Philadelphia, Pennsylvania Design: Within-subjects design, with randomisation of feeding condition sequences. | Objective: To investigate the association of young children’s vulnerability to large portion sizes of foods with weight status and appetite regulation traits. Sample size: 100 children (66 with normal weight, 34 with obesity) aged 5–6 years. Intervention method: Children were served a dinner meal containing pasta, corn, applesauce, cookies, and 2% milk. All foods (except milk) varied across 4 portion size conditions: 100% (677 kcal), 150% (1015 kcal), 200% (1353 kcal), or 250% (1691 kcal). Eating setting: Dinner time in laboratory. | Intervention period: Once a week for 4 weeks. Outcome evaluation: Energy intake (kcal) of each meal, food preference, food responsiveness, satiety responsiveness, and enjoyment of food. Follow-up: No follow-up (intake was estimated immediately after each meal). | Children consumed higher total energy intake with increasing portion sizes across all conditions (p < 0.001). On average, children consumed 479.9 ± 167.8 kcal in 100% portion size condition, 531.2 ± 204.9 kcal in 150% condition, 540.9 ± 216.5 kcal in 200% condition, and 585.1 ± 247.8 kcal in 250% condition. The effect of portion size condition on total energy intake did not vary with children’s weight status (p = 0.6) but varied with satiety responsiveness (p < 0.05) and food responsiveness (p = 0.05). | Strengths: (1) Assessing individual variation in children’s susceptibility of large portion size; (2) Relatively high sample size; (3) Children’s conditioning: fasting for 2 h before testing. Limitations: (1) Homogenous study sample (all children were non-Hispanic black children, majority from low-income families); (2) No follow up or longitudinal data collected; (3) Laboratory setting; (4) Imbalanced proportion of children with normal weight and obesity. |
| ⑨ Kerr et al., 2019 [27] Title: “Child and adult snack food intake in response to manipulated pre-packaged snack item quantity/variety and snack box size: a population-based randomised trial” Location: Australia (multi-cities) Design: Population-based randomised trial | Objective: To investigate how intake is affected by modification of pre-packaged snack food in terms of item quantity and variety dishware (boxed container) size. Sample size: 1299 children (11–12 years old) and 1274 parents from the Longitudinal Study of Australian Children (LSAC). Intervention method: Snack food items (savoury crackers, sweet biscuits, milk chocolate, cheese, muesli/granola bars, wheat fruit bites, and peaches in juice) were presented in one of four conditions: (1) small box, fewer items, (2) larger box, fewer items, (3) small box, more items, and (4) larger box, more items. Eating setting: “Food Stop” (snacking area) in the assessment centre. | Intervention period: One session between February 2015 and March 2016 (14 months). Outcome evaluation: Food intake (g) and energy intake (kJ) of snacks, hunger scale before eating. Follow-up: No follow-up (intake was estimated immediately after each meal). | Children’s intake increased by 10 g (95% CI 3–17 g) and 349 kJ (95% CI 282–416 kJ) when offered more variety/quantity of snacks (p < 0.01). Box size did not affect intake (p = 0.7, for grams consumed; p = 0.5, for kilojoules consumed). Based on children’s characteristics, boys consumed significantly more energy (kJ), but not amount in grams, of snacks compared to girls (p < 0.001). However, neither energy (kJ) nor consumption in grams differed by children’s weight and social-economic status. In adults, neither box size nor variety or quantity of snack items had significant effect on consumption. | Strengths: (1) Large sample size (population-based); (2) Although tightly controlled, the break time setting was more realistic than laboratory setting; (3) Adults and children were exposed to identical but separate manipulations. Limitations: (1) Distraction of other activities (e.g., reading) while the study participants having snacks; (2) Adults exposed to the information booklet prior testing which mention that food intake would be evaluated; (3) Children had fasted longer and were hungrier than adults at the Food Stop. |
| ⑩ McGale et al., 2020 [28] Title: “The influence of front-of-pack portion size images on children’s serving and intake of cereal” Location: UK Design: Between-subjects design, with randomisation of participants to intervention condition. | Objective: To investigate the effect of front-of-package portion size image on children self-served portions and consumption. Sample size: 41 children aged 7–11 years old. Intervention method: Children were exposed to cereal box condition depicting either a small visual cue of recommended cereal serving size (30 g), or a larger and more typical front-of-pack portion size (90 g). Eating setting: Breakfast meal in laboratory. | Intervention period: One session between February and November 2015 (10 months). Outcome evaluation: Cereal serving and intake (gram), children’s perception of the portion size, hunger scale. Follow-up: No follow-up (intake was estimated immediately after each meal). | Children served themselves (+7 g, 37%) and consumed (+6 g, 63%) more cereal when exposed to larger-portion-size visual cue compared to small-portion-size visual cue (p = 0.015 for cereal served, p = 0.002 for cereal consumed). The total meal consumed (cereal and milk) was higher in large compared to small portion size visual cue (mean ± SE: 73.4 ± 7.4 g vs. 47.1 ± 7.8 g). Furthermore, 63% of children accepted the image of portion as appropriate, regardless of condition, meaning that children might be susceptible to manipulations of external cues. | Strengths: (1) Using natural control of large portion size package which represent typical cereal package on the market; (2) The analysis accounted covariates (BMI, age, sex, hunger rating). Limitations: (1) Relatively small sample size; (2) Did not assess the effect on energy intake; (3) Fixed amount of milk provided (100 g) which create ceiling effect. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sani, S.L.; Alfaraidi, S.; Mu, Y.; Sinaga, G.H.P.; Singhal, A. The Effect of Portion Size Interventions on Energy Intake and Risk of Obesity in School-Aged Children: A Systematic Review and Meta-Analysis. Nutrients 2025, 17, 2911. https://doi.org/10.3390/nu17182911
Sani SL, Alfaraidi S, Mu Y, Sinaga GHP, Singhal A. The Effect of Portion Size Interventions on Energy Intake and Risk of Obesity in School-Aged Children: A Systematic Review and Meta-Analysis. Nutrients. 2025; 17(18):2911. https://doi.org/10.3390/nu17182911
Chicago/Turabian StyleSani, Salma Luthfiyah, Sara Alfaraidi, Yongqi Mu, Gideon Hot Partogi Sinaga, and Atul Singhal. 2025. "The Effect of Portion Size Interventions on Energy Intake and Risk of Obesity in School-Aged Children: A Systematic Review and Meta-Analysis" Nutrients 17, no. 18: 2911. https://doi.org/10.3390/nu17182911
APA StyleSani, S. L., Alfaraidi, S., Mu, Y., Sinaga, G. H. P., & Singhal, A. (2025). The Effect of Portion Size Interventions on Energy Intake and Risk of Obesity in School-Aged Children: A Systematic Review and Meta-Analysis. Nutrients, 17(18), 2911. https://doi.org/10.3390/nu17182911