Exploring Body Composition and Eating Habits Among Nurses in Poland
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Measurements
- <7.1% body fat below norm;
- 7.1–20.0% body fat within norm;
- 20.0–25.0% excessive body fat;
- 25.0% obesity.
- <10.1% body fat below norm;
- 10.1–22.0% body fat within norm;
- 22.1–28.4% excessive body fat;
- 28.4% obesity.
- <20.9% body fat below norm;
- 20.9–33.0% body fat within norm;
- 33.1–39.5% excessive body fat;
- 39.5% obesity.
- <23.0% body fat below norm;
- 23.0–34.0% body fat within norm;
- 34.1–40.0% excessive body fat;
- 40.0% obesity [15].
- <0.96 WHR within normal limits;
- ≥0.96 abdominal obesity, increased risk of metabolic diseases.
- <0.83 WHR within normal limits;
- ≥0.83 abdominal obesity, increased risk of metabolic diseases [22].
2.3. Questionnaire
2.4. Statistical Analysis Applied
3. Results
3.1. Characteristics of Study Group
3.2. Findings
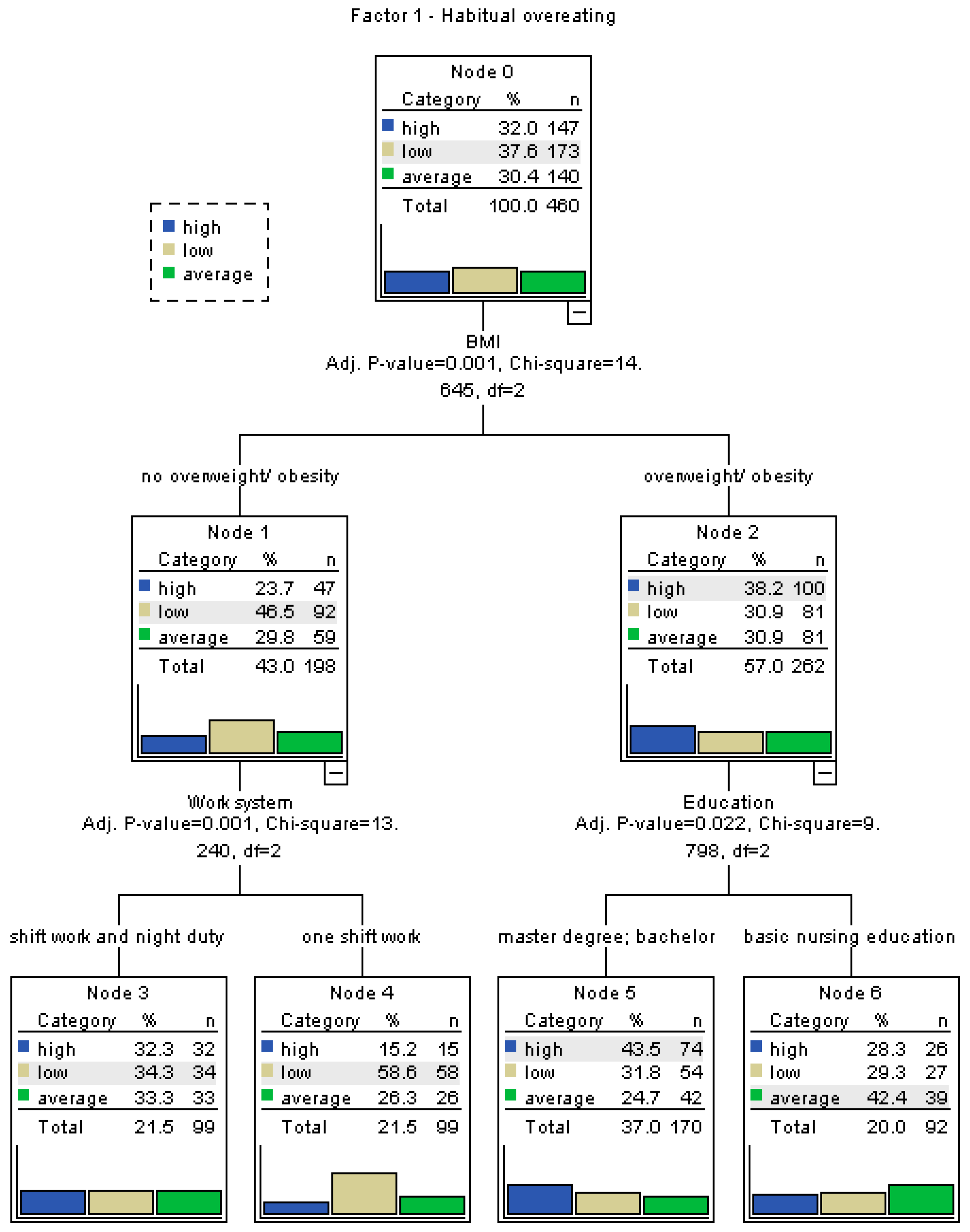
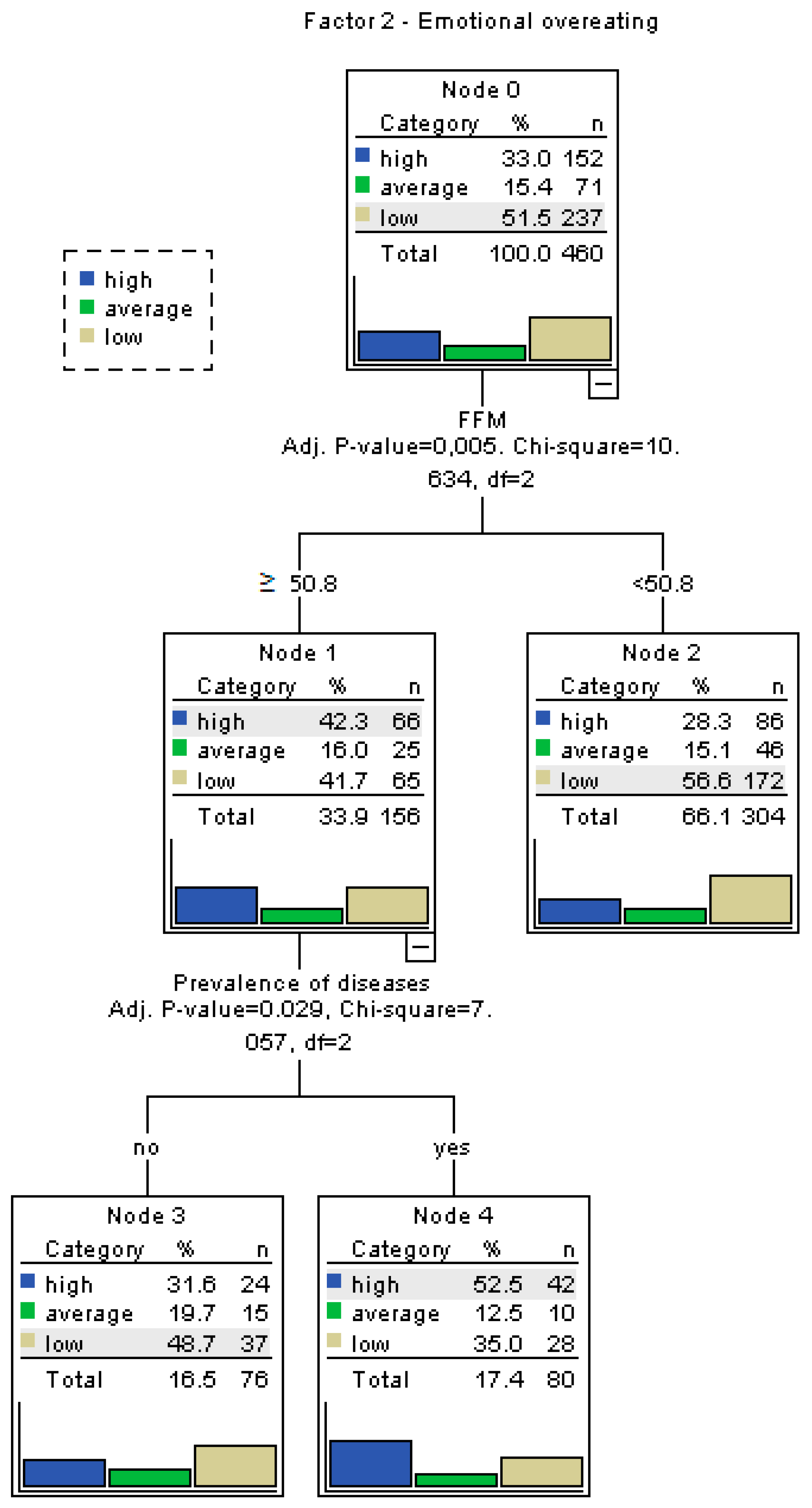
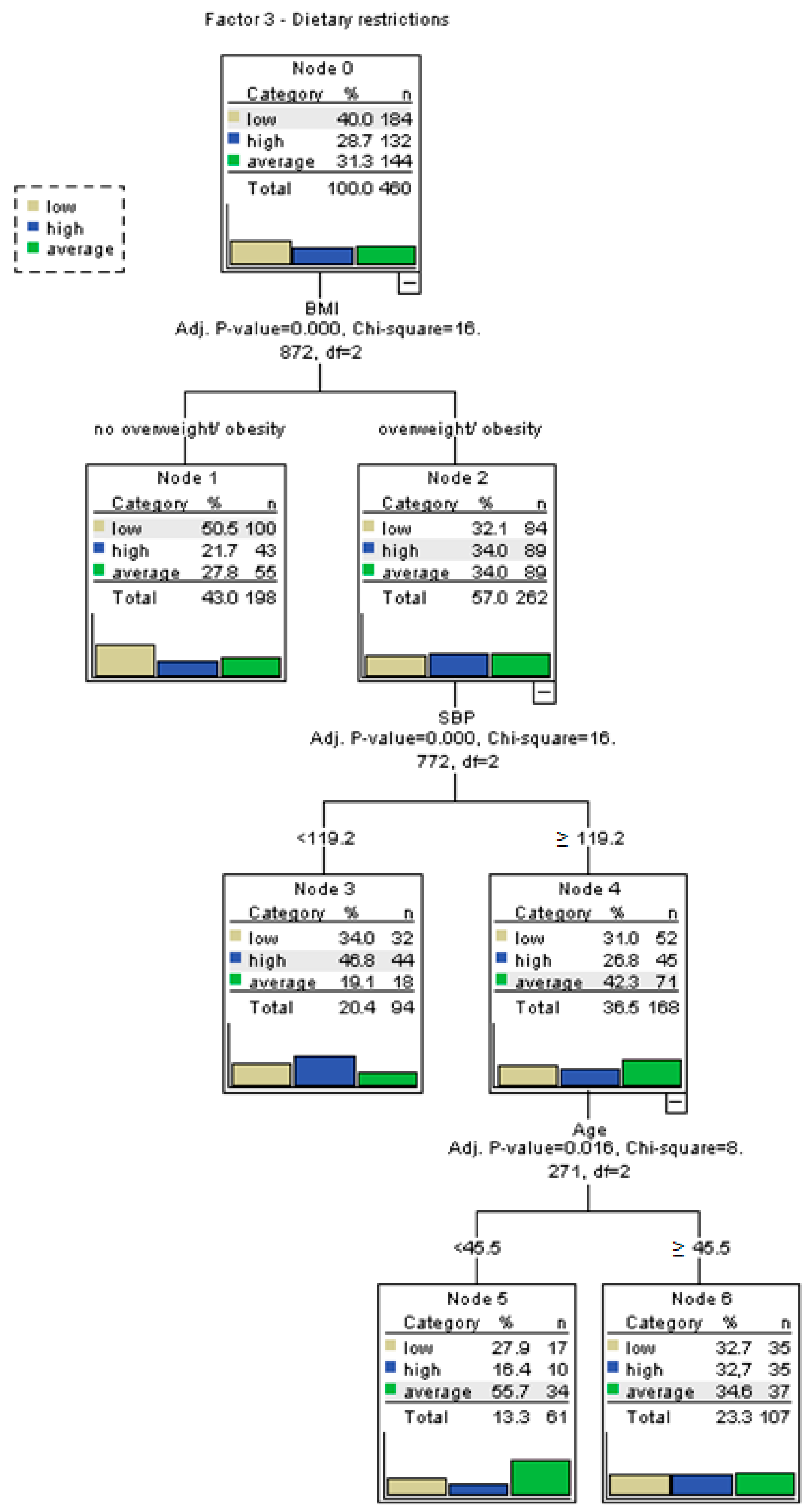
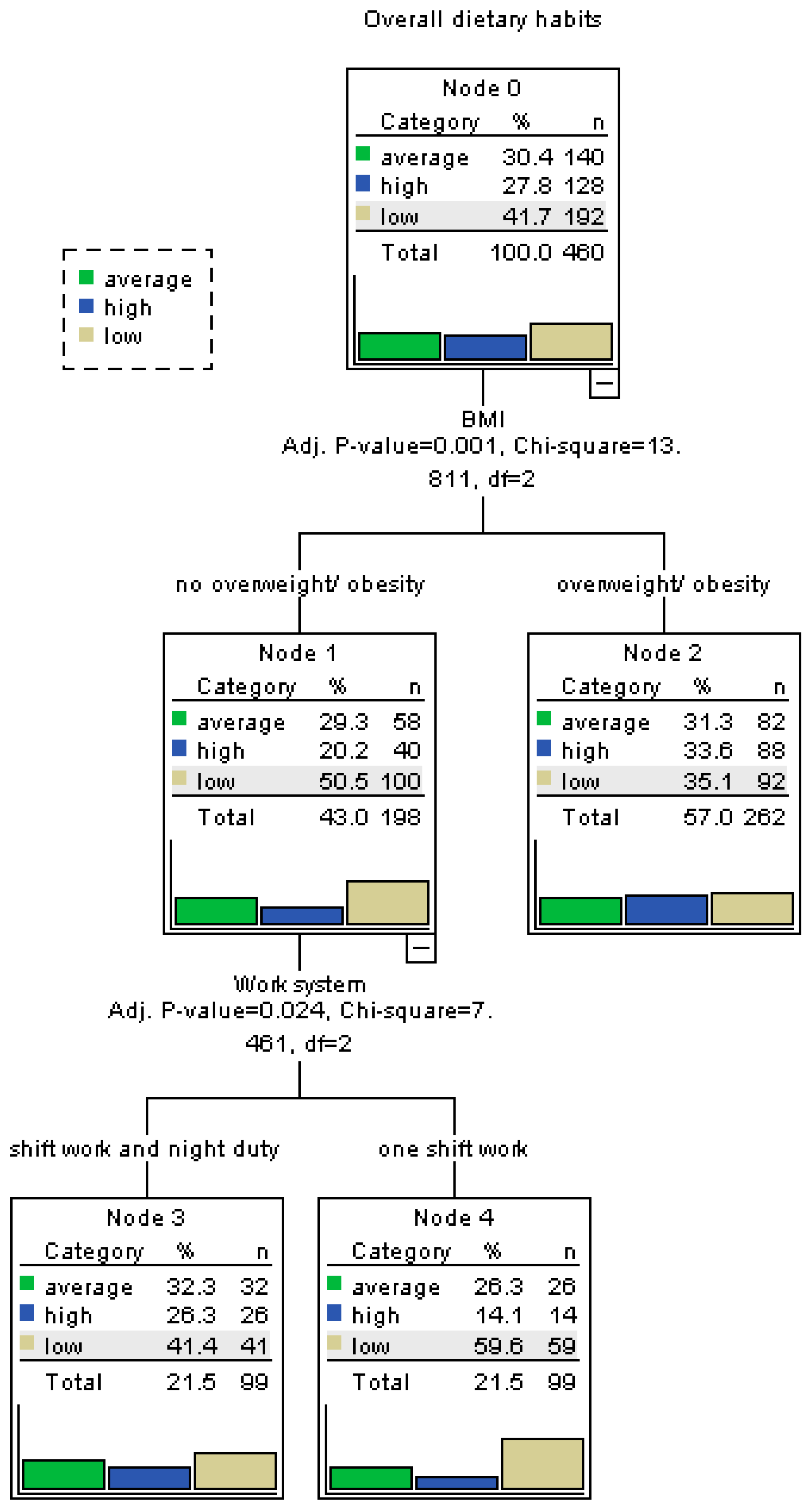
3.3. Decision Tree Analysis of Eating Behaviors
3.4. Heatmaps of Eating Behavior Factors by Key Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| FFM | Fat-Free Mass |
| FATM | Fat Mass |
| FATP | Body Fat Percentage |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| MEH | My Eating Habits |
| WHO | World Health Organization |
| OECD | Organisation for Economic Co-operation and Development |
| WHR | Waist-to-Hip Ratio |
| ROC | Receiver Operating Characteristic |
| M | Mean |
| Me | Median |
| SD | Standard Deviation |
| IQR; Q1–Q3 | Interquartile Range |
| CI | Confidence Interval |
| CART | Classification and Regression Tree |
| OR | Odds ratios |
References
- Phelps, N.H.; Singleton, R.K.; Zhou, B.; Heap, R.A.; Mishra, A.; Bennett, J.E.; Paciorek, C.J.; Lhoste, V.P.; Carrillo-Larco, R.M.; Stevens, G.A.; et al. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2030. Available online: https://www.who.int/publications/i/item/9789241506236 (accessed on 25 April 2025).
- Organisation for Economic Co-Operation and Development (OECD). The Heavy Burden of Obesity: The Economics of Prevention; OECD: Paris, France, 2019. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Obesity and Overweight Factsheet. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 25 April 2025).
- Caballero, B. Humans against Obesity: Who Will Win? Adv. Nutr. 2019, 10, 4–9. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Wong, A.H.C.; Hon, K.L. Childhood Obesity: An Updated Review. Curr. Pediatr. Rev. 2024, 20, 2–26. [Google Scholar] [CrossRef]
- Magee, M.K.; Jones, M.T.; Fields, J.B.; Kresta, J.; Khurelbaatar, C.; Dodge, C.; Merfeld, B.; Ambrosius, A.; Carpenter, M.; Jagim, A.R. Body Composition, Energy Availability, Risk of Eating Disorder, and Sport Nutrition Knowledge in Young Athletes. Nutrients 2023, 15, 1502. [Google Scholar] [CrossRef]
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The Influence of Parental Dietary Behaviors and Practices on Children’s Eating Habits. Nutrients 2021, 13, 1138. [Google Scholar] [CrossRef]
- Van der Merwe, C.; Münch, M.; Kruger, R. Chronotype Differences in Body Composition, Dietary Intake and Eating Behavior Outcomes: A Scoping Systematic Review. Adv. Nutr. 2022, 13, 2357–2405. [Google Scholar] [CrossRef]
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic review of shift work and nurses’ health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, A.; Kabi, A.; Mohanty, A.P. Health problems in healthcare workers: A review. J. Fam. Med. Prim. Care 2019, 8, 2568. [Google Scholar] [CrossRef] [PubMed]
- Jankowska-Polańska, B.; Wijacka, K.; Lomper, K.; Uchmanowicz, I. Zachowania zdrowotne personelu pielęgniarskiego w profilaktyce nadciśnienia tętniczego. Współczesne Pielęgniarstwo Ochr. Zdrowia 2014, 3, 67–70. [Google Scholar]
- Kucharska, A.; Janiszewska, M.; Siński, B. Nurses’ health behaviours in the context of the prevention of circulatory system diseases. Żywienie Człowieka Metabolizm 2016, 43, 107–116. [Google Scholar]
- Supreme Chamber of Nurses and Midwives in Poland. Raport o Stanie Pielęgniarstwa i Położnictwa w Polsce. Available online: https://nipip.pl/wp-content/uploads/2023/12/RAPORT-O-STANIE-PIELEGNIARSTWA-I-P-OLOZNICTWA-W-POLSCE-MAJ-2023.pdf (accessed on 22 April 2024).
- Supreme Chamber of Nurses and Midwives in Poland. Raport: Katastrofa Kadrowa Pielęgniarek i Położnych. Available online: https://nipip.pl/wp-content/uploads/2021/09/2021-09-06_Raport_NIPiP_KRAJ.pdf (accessed on 22 April 2024).
- Organisation for Economic Co-Operation and Development (OECD). Health at a Glance 2019: OECD Indicators; OCED: Paris, France, 2019. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Global Strategic Directions for Nursing and Midwifery 2021–2025. Available online: https://www.who.int/publications/i/item/9789240033863 (accessed on 25 April 2025).
- Brennan, E.J. Towards resilience and wellbeing in nurses. Br. J. Nurs. 2017, 26, 43–47. [Google Scholar] [CrossRef]
- Kurth, A.E.; Jacob, S.; Squires, A.P.; Sliney, A.; Davis, S.; Stalls, S.; Portillo, C.J. Investing in Nurses is a Prerequisite for Ensuring Universal Health Coverage. J. Assoc. Nurses AIDS Care 2016, 27, 344–354. [Google Scholar] [CrossRef]
- Tanita. Professional Product. Guide. Available online: https://tanita.es/media/pdf/documents/professional/EN%20-%20Medical%20Product%20Guide%20DIGITAL.pdf (accessed on 22 April 2024).
- Barlow, S.E.; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120 (Suppl. 4), S164–S192. [Google Scholar] [CrossRef]
- Nishida, C.; Ko, G.; Kumanyika, S. Body fat distribution and noncommunicable diseases in populations: Overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist–Hip Ratio. Eur. J. Clin. Nutr. 2010, 64, 2–5. [Google Scholar] [CrossRef]
- Ogińska-Bulik, N.; Putyński, L. Kwestionariusz Moje Zwyczaje Żywieniowe–konstrukcja i właściwości psychometryczne. Acta Univ. Lodziensis. Folia Psychol. 2000, 4, 25–31. [Google Scholar]
- Lazarus, J.; McIntyre, M.; Slater, H. Psychosocial Stress and Nutrition Among Nurses: A Systematic Review. Nutrients 2021, 13, 2934. [Google Scholar]
- Znyk, M.; Kaleta, D. Unhealthy Eating Habits and Determinants of Diet Quality in Primary Healthcare Professionals in Poland: A Cross-Sectional Study. Nutrients 2024, 16, 3367. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B.; Fung, T.T.; Manson, J.E.; Willett, W.C.; Hu, F.B. Dietary Patterns and Changes in Body Weight in Women. Obesity 2006, 14, 1444–1453. [Google Scholar] [CrossRef] [PubMed]
- Fruh, S.; Williams, S.; Hayes, K.; Hauff, C.; Hudson, G.M.; Sittig, S.; Graves, R.J.; Hall, H.; Barinas, J. A practical approach to obesity prevention: Healthy home habits. J. Am. Assoc. Nurse Pract. 2021, 33, 1055–1065. [Google Scholar] [CrossRef]
- Volpe, R.; Stefano, P.; Massimiliano, M.; Francesca, M.; Gianluca, S.; Federica, R. Healthy fats for healthy nutrition. An educational approach in the workplace to regulate food choices and improve prevention of non-communicable diseases. High Blood Press. Cardiovasc. Prev. 2015, 22, 395–401. [Google Scholar] [CrossRef]
- Samhat, Z.; Fares, S.; Sabbah, M. Association Between Night Shift and Nutritional Behavior in Nurses. J. Nurs. Manag. 2020, 28, 1045–1053. [Google Scholar]
- Chen, L.; Gao, X.; Tsai, Y. Impact of Meal Timing on Metabolic Outcomes in Nurses Working Night Shifts. Chronobiol. Int. 2023, 40, 95–108. [Google Scholar]
- US Department of Health and Human Services. Healthy people 2000: National health promotion and disease prevention objectives—Nutrition priority area. Nutr. Today 1990, 25, 29–39. [Google Scholar]
- Bielicki, J.A.; Duval, X.; Gobat, N.; Goossens, H.; Koopmans, M.; Tacconelli, E.; Van der Werf, S. Monitoring approaches for health-care workers during the COVID-19 pandemic. Lancet Infect. Dis. 2020, 20, e261–e267. [Google Scholar] [CrossRef]
- Persson, M.; Mårtensson, J. Situations influencing habits in diet and exercise among nurses working night shift. J. Nurs. Manag. 2006, 14, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Kieft, R.A.; De Brouwer, B.B.; Francke, A.L.; Delnoij, D.M. How nurses and their work environment affect patient experiences of the quality of care: A qualitative study. BMC Health Serv. Res. 2014, 14, 249. [Google Scholar] [CrossRef]
- Colditz, G.A.; Hankinsn, S.E. The Nurses’ Health Study: Lifestyle and health among women. Nat. Rev. Cancer 2005, 5, 388–396. [Google Scholar] [CrossRef]
- De Lucia, F.; Cocchiara, R.; La Torre, G. A Systematic Review of nurses’ eating habits on duty for a healthy workplace. Senses Sci. 2021, 8, 1304–1323. [Google Scholar]
- Pallesen, S.; Bjorvatn, B.; Waage, S.; Harris, A.; Sagoe, D. Prevalence of shift work disorder: A systematic review and meta-analysis. Front. Psychol. 2021, 12, 638252. [Google Scholar] [CrossRef]
- Gieniusz-Wojczyk, L.; Dąbek, J.; Kulik, H. Nutrition Habits of Polish Nurses: An Approach. Healthcare 2021, 9, 786. [Google Scholar] [CrossRef]
- Streng, A.A.; Loef, B.; Dollé, M.E.T.; Van der Horst, G.T.J.; Chaves, I.; Proper, K.I.; Van Kerkhof, L.W.M. Night shift work characteristics are associated with several elevated metabolic risk factors and immune cell counts in a cross-sectional study. Sci. Rep. 2022, 12, 2022. [Google Scholar] [CrossRef]
- Tran, H.; Stephens, R. Workload and emotional eating among nurses: A structural equation model. J. Nurs. Scholarsh. 2020, 52, 424–432. [Google Scholar]
- Panczyk, M.; Woynarowska-Sołdan, M.; Żmuda-Trzebiatowska, H.; Gotlib, J. Health-enhancing behaviours of nurses in Poland and their association with shift work and age. Collegian 2018, 25, 255–261. [Google Scholar] [CrossRef]
- Fishbein, A.B.; Knutson, K.L.; Zee, P.C. Circadian disruption and human health. J. Clin. Investig. 2021, 7, 131. [Google Scholar] [CrossRef]
- Brzeźniak, H.; Rotter, I.; Żułtak-Bączowska, K. Ocena wpływu wybranych czynników stresogennych na funkcjonowanie zawodowe pielęgniarek w zależności od wieku i stażu pracy. Zdr. Publ. 2011, 121, 43–46. [Google Scholar]
- Warchoł-Stawińska, E.; Włoch, K. Zachowania zdrowotne pielęgniarek. Zdr. Publ. 2003, 113, 156–159. [Google Scholar]
- Terada, T.; Mistura, M.; Tulloch, H.; Pipe, A.; Reed, J. Dietary Behaviour is Associated with Cardiometabolic and Psychological Risk Indicators in Female Hospital Nurses—A Post-Hoc, Cross-Sectional Study. Nutrients 2019, 11, 2054. [Google Scholar] [CrossRef]
- Monaghan, T.; Dinour, L.; Liou, D.; Shefchik, M. Factors Influencing the Eating Practices of Hospital Nurses During Their Shifts. Workplace Health Saf. 2017, 66, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Almajwal, A.M. Correlations of Physical Activity, Body Mass Index, Shift Duty, and Selected Eating Habits among Nurses in Riyadh, Saudi Arabia. Ecol. Food Nutr. 2015, 54, 397–417. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Choi-Kwon, S.; Kim, K.S. Poor dietary behaviors among hospital nurses in Seoul, South Korea. Appl. Nurs. Res. 2016, 30, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Dias, C.H.; Dawson, R.M. Hospital and Shift Work Influences on Nurses’ Dietary Behaviors. Workplace Health Saf. 2020, 68, 374–383. [Google Scholar] [CrossRef]
- Pi-Sunyer, X. The Medical Risks of Obesity. Postgrad. Med. 2009, 121, 21–33. [Google Scholar] [CrossRef]
- Gieniusz-Wojczyk, L.; Dąbek, J.; Kulik, H. Risky behaviour among nurses in Poland: An analysis of nurses’ physical condition, mental health, and resilience. Int. J. Environ. Res. Public Health 2021, 18, 1807. [Google Scholar] [CrossRef]
- Amani, R.; Gill, T. Shiftworking, nutrition and obesity: Implications for workforce health—A systematic review. Asia Pac. J. Clin. Nutr. 2013, 22, 698–708. [Google Scholar] [CrossRef]
- Nicholls, R.; Perry, L.; Duffield, C.; Gallagher, R.; Pierce, H. Barriers and facilitators to healthy eating for nurses in the workplace: An integrative review. J. Adv. Nurs. 2017, 73, 1051–1065. [Google Scholar] [CrossRef] [PubMed]
- Samhat, Z.; Attieh, R.; Sacre, Y. Relationship between night shift work, eating habits and BMI among nurses in Lebanon. BMC Nurs. 2020, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Bilski, B. Higiena Pracy dla Pielęgniarek: Wybrane Zagadnienia; Wydawnictwo Naukowe, Akademia Medycyny: Poznań, Poland, 2004. [Google Scholar]
- Bilski, B. Wpływ pracy zmianowej na sposób odżywania się i patologię przewodu pokarmowego wśród pielęgniarek–wyniki badania pilotażowego. Med. Pracy 2006, 57, 15–19. [Google Scholar]
- Nejman, M.; Gotlib, J. Wpływ pracy zmianowej pielęgniarek na ich postawy żywieniowe. Pielęg. Pol. 2017, 1, 13–19. [Google Scholar] [CrossRef]
- Macht, M. How emotions affect eating: A five-way model. Appetite 2008, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; McSweeney, L.; Spence, S. Availability of Healthy Food and Beverages in Hospital Outlets and Interventions in the UK and USA to Improve the Hospital Food Environment: A Systematic Narrative Literature Review. Nutrients 2022, 14, 1566. [Google Scholar] [CrossRef]
- Den Hamer-Jordaan, G.; Groenendijk-van Woudenbergh, G.J.; Kroeze, W.; Troost, E.; Haveman-Nies, A. Nurse-related behavioural determinants associated with healthy eating support provided by Dutch community nurses: A cross-sectional study. BMC Nurs. 2024, 23, 774. [Google Scholar] [CrossRef] [PubMed]
- Main Chamber of Nurses and Midwifes in Poland. Report: Nurse, Midwife, Shortage Professions in the Polish Health Care System. Available online: https://nipip.pl/wp-content/uploads/2022/06/2022_Raport-NIPiP-struktura-wiekowa-kadr.pdf (accessed on 22 April 2024).
- Cheong, Z.Y.; Lopez, V.; Tam, W.S. Barriers to healthy eating among nurses working in hospitals: A meta-synthesis. J. Adv. Nurs. 2022, 78, 314–331. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Total (n = 460) | ||
|---|---|---|---|
| n | % | ||
| Sex * | female | 420 | 91.3% |
| male | 40 | 8.7% | |
| Type of work * | hospital ward | 386 | 83.9% |
| administrative position | 74 | 16.1% | |
| Work system * | one shiftwork | 223 | 48.5% |
| shift work and night duty | 237 | 51.5% | |
| More than one job * | No | 325 | 70.7% |
| Yes | 135 | 29.3% | |
| Education * | basic nursing education | 138 | 30.0% |
| bachelor | 104 | 22.6% | |
| master’s degree | 218 | 47.4% | |
| WHR * | normal | 243 | 52.8% |
| abdominal obesity | 217 | 47.2% | |
| BMI * | underweight | 8 | 1.7% |
| normal body weight | 190 | 41.3% | |
| overweight | 154 | 33.5% | |
| first-degree obesity | 72 | 15.7% | |
| second-degree obesity | 23 | 5.0% | |
| third-degree obesity | 13 | 2.8% | |
| Fat mass * | normal | 325 | 70.7% |
| excessive body fat | 91 | 19.8% | |
| obesity | 44 | 9.6% | |
| Prevalence of diseases * | No | 237 | 51.5 |
| Yes | 223 | 48.5 | |
| Prevalence of diseases * | diabetes | 29 | 6.3 |
| hypertension | 69 | 15.0 | |
| circulatory system diseases | 20 | 4.3 | |
| thyroid diseases | 63 | 13.7 | |
| kidney disease | 10 | 2.2 | |
| digestive system diseases | 22 | 4.8 | |
| degenerative disease of joints/spine | 48 | 10.4 | |
| diseases of the nervous system | 7 | 1.5 | |
| cancer | 6 | 1.3 | |
| eating disorders: anorexia | 4 | 0.9 | |
| bulimia | 8 | 1.7 | |
| compulsive overeating syndrome | 22 | 4.8 | |
| other | 45 | 9.8 | |
| Parameter | M (95% CI) | Me (Q1–Q3) | SD (Min–Max) |
|---|---|---|---|
| BMI [kg/m2] | 26.77 (26.28; 27.26) | 25.8 (23.1; 29.5) | 5.39 (16.6; 54.6) |
| FATP [%] | 30.29 (29.62; 30.96) | 30.4 (25.35; 35.3) | 7.34 (10; 52.4) |
| FATM [kg] | 22.58 (21.67; 23.49) | 20.85 (16; 26.85) | 9.9 (4.6; 75.7) |
| FFM [kg] | 49.43 (48.7; 50.15) | 47.9 (44; 53.1) | 7.88 (32.4; 80.8) |
| WHR [cm] | 0.83 (0.83; 0.84) | 0.83 (0.78; 0.89) | 0.08 (0.52; 1.10) |
| SBP [mmHg] | 124.08 (121.99; 126.17) | 122 (111.75; 132.00) | 22.81 (90.67; 198.00) |
| DBP [mmHg] | 77.45 (75.62; 79.29) | 75.83 (71; 81) | 20.04 (56.67; 118.00) |
| Factors of MEH Questionnaire | M (95% CI) | Me (Q1–Q3) | SD (Min–Max) |
|---|---|---|---|
| Factor 1—Habitual overeating | 4.66 (4.42; 4.9) | 4 (3; 7) | 2.6 (0; 10) |
| Factor 2—Emotional overeating | 4.71 (4.46; 4.96) | 4.5 (3; 7) | 2.76 (0; 10) |
| Factor 3—Dietary restrictions | 4.47 (4.28; 4.67) | 4 (3; 6) | 2.17 (0; 10) |
| Overall dietary habits | 13.85 (13.28; 14.41) | 13 (9; 18) | 6.15 (0; 28) |
| Factors of MEH Questionnaire | Level of Clusters | n | % |
|---|---|---|---|
| Factor 1—Habitual overeating | High | 147 | 32.0 |
| Low | 173 | 37.6 | |
| Medium | 140 | 30.4 | |
| Factor 2—Emotional overeating | High | 152 | 33.0 |
| Medium | 71 | 15.4 | |
| Low | 237 | 51.5 | |
| Factor 3—Dietary restrictions | Low | 184 | 40.0 |
| High | 132 | 28.7 | |
| Medium | 144 | 31.3 | |
| Overall dietary habits | Medium | 140 | 30.4 |
| High | 128 | 27.8 | |
| Low | 192 | 41.7 |
| Variables | Overall Dietary Habits [MEH] | p | ||||||
|---|---|---|---|---|---|---|---|---|
| Average | High | Low | ||||||
| n | % | n | % | n | % | |||
| Sex | female | 129 | 30.7% | 118 | 28.1% | 173 | 41.2% | Χ2 = 0.598; p(χ2) = 0.7415 |
| male | 11 | 27.5% | 10 | 25.0% | 19 | 47.5% | ||
| Type of work | hospital ward | 113 | 29.3% | 107 | 27.7% | 166 | 43.0% | χ2 = 1.992; p(χ2) = 0.3693 |
| administrative position | 27 | 36.5% | 21 | 28.4% | 26 | 35.1% | ||
| Work system | shiftwork | 73 | 32.7% | 52 | 23.3% | 98 | 43.9% | χ2 = 4.418; p(χ2) = 0.1098 |
| shift work and night duty | 67 | 28.3% | 76 | 32.1% | 94 | 39.7% | ||
| More than one job | no | 103 | 31.7% | 78 | 24.0% | 144 | 44.3% | χ2 = 8.152; p(χ2) = 0.0170 |
| yes | 37 | 27.4% | 50 | 37.0% | 48 | 35.6% | ||
| Education | basic nursing education | 40 | 29.0% | 30 | 21.7% | 68 | 49.3% | χ2 = 7.540; p(χ2) = 0.1100 |
| Bachelor | 31 | 29.8% | 37 | 35.6% | 36 | 34.6% | ||
| master’s degree | 69 | 31.7% | 61 | 28.0% | 88 | 40.4% | ||
| WHR | normal | 75 | 30.9% | 63 | 25.9% | 105 | 43.2% | χ2 = 0.967; p(χ2) = 0.6168 |
| abdominal obesity | 65 | 30.0% | 65 | 30.0% | 87 | 40.1% | ||
| BMI | normal | 99 | 30.5% | 81 | 24.9% | 145 | 44.6% | χ2 = 6.003; p(χ2) = 0.1989 |
| increased | 28 | 30.8% | 33 | 36.3% | 30 | 33.0% | ||
| excessive | 13 | 29.5% | 14 | 31.8% | 17 | 38.6% | ||
| BMI | no overweight/obesity | 58 | 29.3% | 40 | 20.2% | 100 | 50.5% | χ2 = 13.811; p(χ2) = 0.0010 |
| prevalence overweight/obesity | 82 | 31.3% | 88 | 33.6% | 92 | 35.1% | ||
| Prevalence of disease | no | 73 | 30.8% | 54 | 22.8% | 110 | 46.4% | χ2 = 7.046; p(χ2) = 0.0295 |
| yes | 67 | 30.0% | 74 | 33.2% | 82 | 36.8% | ||
| ROC | n | % | |
|---|---|---|---|
| Age (AUC = 0.546 sensitivity = 0.567 1-specificity = 0.400) | <45.5 | 206 | 44.8% |
| ≥45.5 | 254 | 55.2% | |
| FFM (AUC = 0.839 sensitivity = 0.875 1-specificity = 0.288) | <50.8 | 304 | 66.1% |
| ≥50.8 | 156 | 33.9% | |
| SBP (AUC = 0.698 sensitivity = 0.875 1-specificity = 0.533) | <119.2 | 200 | 43.5% |
| ≥119.2 | 260 | 56.5% | |
| DBP (AUC = 0.662 sensitivity = 0.875 1-specificity = 0.579) | <73.8 | 182 | 39.6% |
| ≥73.8 | 278 | 60.4% | |
| Variables | F1_High | F2_High | F3_High | MEH Overall |
|---|---|---|---|---|
| Sex | OR = 0.79 (0.38; 1.63); p = 0.5278 | OR = 0.56 (0.26; 1.21); p = 0.1424 | OR = 0.60 (0.27; 1.33); p = 0.2075 | OR = 0.85 (0.40; 1.80); p = 0.6766 |
| Type of work | OR = 0.95 (0.56; 1.63); p = 0.8601 | OR = 0.90 (0.53; 1.54); p = 0.6953 | OR = 0.98 (0.57; 1.70); p = 0.9475 | OR = 1.03 (0.59; 1.79); p = 0.9079 |
| Work system | OR = 1.58 (1.06; 2.34); p = 0.0247 | OR = 1.41 (0.95; 2.09); p = 0.0854 | OR = 1.19 (0.79; 1.78); p = 0.4106 | OR = 1.55 (1.03; 2.35); p = 0.0370 |
| More than one job | OR = 1.91 (1.25; 2.90); p = 0.0025 | OR = 1.07 (0.70; 1.63); p = 0.7620 | OR = 1.51 (0.98; 2.32); p = 0.0623 | OR = 1.86 (1.21; 2.87); p = 0.0048 |
| Basic nursing education | OR = 0.69 (0.43; 1.11); p = 0.1253 | OR = 0.70 (0.44; 1.11); p = 0.1268 | OR = 0.95 (0.59; 1.52); p = 0.8240 | OR = 0.71 (0.43; 1.18); p = 0.1893 |
| Bachelor | OR = 1.27 (0.78; 2.06); p = 0.3388 | OR = 1.01 (0.62; 1.65); p = 0.9642 | OR = 0.93 (0.55; 1.56); p = 0.7851 | OR = 1.42 (0.86; 2.34); p = 0.1669 |
| WHR | OR = 1.21 (0.81; 1.78); p = 0.3515 | OR = 1.39 (0.94; 2.05); p = 0.1000 | OR = 1.33 (0.89; 2.00); p = 0.1652 | OR = 1.22 (0.81; 1.84); p = 0.3362 |
| FAT excessive body fat | OR = 1.74 (1.07; 2.81); p = 0.0244 | OR = 1.20 (0.74; 1.96); p = 0.4602 | OR = 1.71 (1.05; 2.79); p = 0.0314 | OR = 1.71 (1.04; 2.81); p = 0.0332 |
| FAT obesity | OR = 1.13 (0.57; 2.23); p = 0.7242 | OR = 1.69 (0.89; 3.20); p = 0.1105 | OR = 0.80 (0.38; 1.70); p = 0.5682 | OR = 1.41 (0.71; 2.78); p = 0.3279 |
| BMI | OR = 1.98 (1.31; 2.99); p = 0.0011 | OR = 1.81 (1.21; 2.71); p = 0.0041 | OR = 1.85 (1.21; 2.83); p = 0.0043 | OR = 2.00 (1.3; 3.080); p = 0.0017 |
| Diseases | OR = 1.67 (1.12; 2.48); p = 0.0111 | OR = 1.44 (0.98; 2.13); p = 0.0652 | OR = 0.88 (0.59; 1.32); p = 0.5374 | OR = 1.68 (1.11; 2.54); p = 0.0133 |
| Age | OR = 0.99 (0.67; 1.47); p = 0.9728 | OR = 1.09 (0.73; 1.61); p = 0.6800 | OR = 1.56 (1.03; 2.35); p = 0.0367 | OR = 1.06 (0.70; 1.60); p = 0.7821 |
| FFM | OR = 1.70 (1.13; 2.55); p = 0.0106 | OR = 1.86 (1.24; 2.78); p = 0.0026 | OR = 1.16 (0.76; 1.78); p = 0.4814 | OR = 1.43 (0.94; 2.19); p = 0.0960 |
| SBP | OR = 1.04 (0.70; 1.54); p = 0.8539 | OR = 1.04 (0.71; 1.55); p = 0.8279 | OR = 0.72 (0.48; 1.08); p = 0.1143 | OR = 0.90 (0.60; 1.36); p = 0.6223 |
| DBP | OR = 0.78 (0.53; 1.17); p = 0.2329 | OR = 0.73 (0.49; 1.08); p = 0.1116 | OR = 0.68 (0.45; 1.02); p = 0.0650 | OR = 0.79 (0.52; 1.19); p = 0.2549 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartosiewicz, A.; Dereń, K.; Łuszczki, E.; Zielińska, M.; Nowak, J.; Lewandowska, A.; Sulikowski, P. Exploring Body Composition and Eating Habits Among Nurses in Poland. Nutrients 2025, 17, 2686. https://doi.org/10.3390/nu17162686
Bartosiewicz A, Dereń K, Łuszczki E, Zielińska M, Nowak J, Lewandowska A, Sulikowski P. Exploring Body Composition and Eating Habits Among Nurses in Poland. Nutrients. 2025; 17(16):2686. https://doi.org/10.3390/nu17162686
Chicago/Turabian StyleBartosiewicz, Anna, Katarzyna Dereń, Edyta Łuszczki, Magdalena Zielińska, Justyna Nowak, Anna Lewandowska, and Piotr Sulikowski. 2025. "Exploring Body Composition and Eating Habits Among Nurses in Poland" Nutrients 17, no. 16: 2686. https://doi.org/10.3390/nu17162686
APA StyleBartosiewicz, A., Dereń, K., Łuszczki, E., Zielińska, M., Nowak, J., Lewandowska, A., & Sulikowski, P. (2025). Exploring Body Composition and Eating Habits Among Nurses in Poland. Nutrients, 17(16), 2686. https://doi.org/10.3390/nu17162686








