Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Clearance and Protocol Registry
2.2. Participants and Interventions
2.3. BP Measurements
2.4. Lipidemic Profile
2.5. CVD Risk Stratification
2.6. Dietary Assesment and Calculation of Nutritional Indexes
2.6.1. MedDiet Score
2.6.2. DASH Index
2.6.3. Dietary Inflammatory Index (DII)
2.7. Anthropometry
2.8. Assessment of PA Levels
2.9. Statistical Analyses
3. Results
3.1. Baseline Group Comparison
3.2. Blood Lipids Profile
3.3. PA Level and Anthropometry Changes
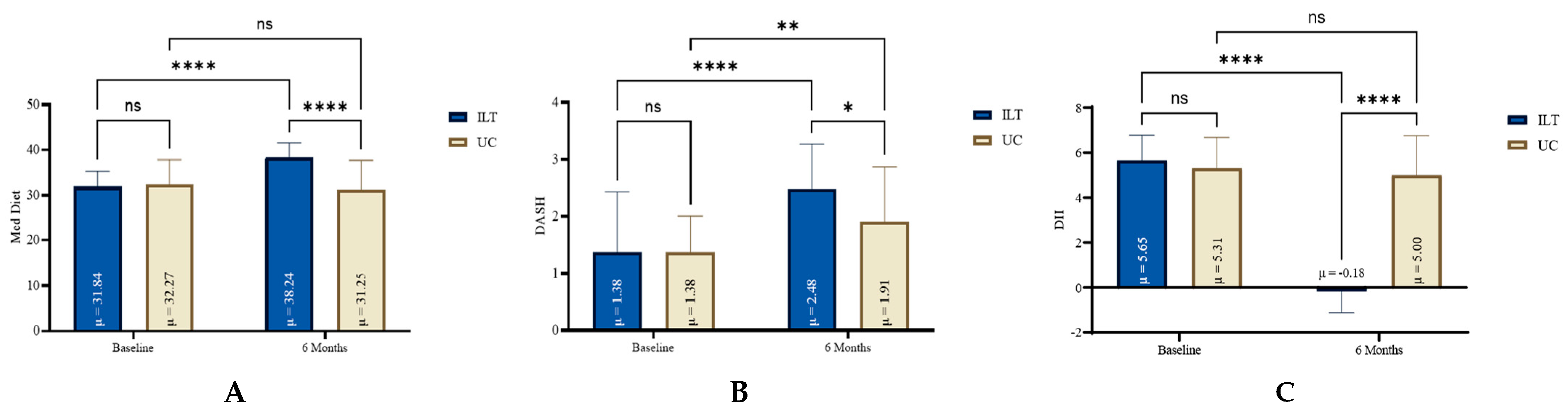
3.4. Dietary Indexes Alterations
3.5. Regression Analysis
4. Discussion
4.1. Overall Study Results
4.2. Mediterranean Diet
4.3. DASH Diet
4.4. DII
4.5. Intensive Nutritional Treatment
4.6. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ABPM | Ambulatory Blood Pressure Monitoring |
| ASCVD | Atherosclerotic Cardiovascular Disease |
| BMI | Body Mass Index |
| BP | Blood Pressure |
| BW | Body Weight |
| CVD | Cardiovascular Disease |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | Diastolic Blood Pressure |
| DII | Dietary Inflammatory Index |
| DM | Diabetes Mellitus |
| EH | Essential Hypertension |
| ESH | European Society of Hypertension |
| HC | Hip Circumference |
| HDL | High Density Lipoprotein |
| HRS | Hellenic Risk Score |
| HTN | Hypertension |
| ILT | Intensive Lifestyle Treatment |
| LDL | Low Density Lipoprotein |
| MedDiet | Mediterranean Diet |
| MUFA | Monounsaturated Fatty Acids |
| Na | Sodium |
| PA | Physical Activity |
| PUFA | Polyunsaturated Fatty Acids |
| RCT | Randomized Controlled Trial |
| SBP | Systolic Blood Pressure |
| SFA | Saturated Fatty Acids |
| TC | Total Cholesterol |
| TG | Triglycerides |
| UC | Usual Care |
| WC | Waist Circumference |
References
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, Regional, and National Age-Sex-Specific Mortality for 282 Causes of Death in 195 Countries and Territories, 1980–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, Regional, and National Comparative Risk Assessment of 84 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- British Heart Foundation. European Cardiovascular Disease Statistics 2017. 15 February 2017. Available online: https://www.bhf.org.uk/informationsupport/publications/statistics/european-cardiovascular-disease-statistics-2017 (accessed on 30 May 2025).
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- WHO. Global Report on Hypertension: The Race Against a Silent Killer; World Health Organization: Geneva, Switzerland, 2023; pp. 1–291. Available online: https://www.who.int/publications/i/item/9789240081062 (accessed on 30 May 2025).
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2019, 75, 285. [Google Scholar] [CrossRef] [PubMed]
- Malik, R.; Georgakis, M.K.; Vujkovic, M.; Damrauer, S.M.; Elliott, P.; Karhunen, V.; Giontella, A.; Fava, C.; Hellwege, J.N.; Shuey, M.M.; et al. Relationship Between Blood Pressure and Incident Cardiovascular Disease: Linear and Nonlinear Mendelian Randomization Analyses. Hypertension 2021, 77, 2004–2013. [Google Scholar] [CrossRef]
- Poznyak, A.V.; Sadykhov, N.K.; Kartuesov, A.G.; Borisov, E.E.; Melnichenko, A.A.; Grechko, A.V.; Orekhov, A.N. Hypertension as a Risk Factor for Atherosclerosis: Cardiovascular Risk Assessment. Front. Cardiovasc. Med. 2022, 9, 959285. [Google Scholar] [CrossRef]
- Libby, P. The Changing Landscape of Atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Huang, L.; Liu, Z.; Zhang, H.; Li, D.; Li, Z.; Huang, J.; He, J.; Lu, L.; Wen, H.; Yuan, H.; et al. The Association between Serum Lipid Profile Levels and Hypertension Grades: A Cross-Sectional Study at a Health Examination Center. High Blood Press. Cardiovasc. Prev. 2024, 32, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Yu, Z.; Huang, Q. Characteristics of Serum Lipid Levels in Patients with Hypertension: A Hospital-Based Retrospective Descriptive Study. BMJ Open 2022, 12, e054682. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Wang, L.; Chen, S. Differences in Lipid Profiles and Atherogenic Indices Between Hypertensive and Normotensive Populations: A Cross-Sectional Study of 11 Chinese Cities. Front. Cardiovasc. Med. 2022, 9, 887067. [Google Scholar] [CrossRef] [PubMed]
- Diószegi, Á.; Kovács, B.; Németh, Á.; Daróczy, B.; Maroda, L.; Karányi, Z.; Pall, D.; Harangi, M. Assessment of Hypertensive Patients’ Lipid Profile Using Data Mining Methods. Atherosclerosis 2024, 395, 117895. [Google Scholar] [CrossRef]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the Management of Elevated Blood Pressure and Hypertension: Developed by the Task Force on the Management of Elevated Blood Pressure and Hypertension of the European Society of Cardiology (ESC) and Endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO). Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the Management of Arterial Hypertension the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar] [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Keshani, M.; Feizi, A.; Askari, G.; Sharma, M.; Bagherniya, M. Effects of Therapeutic Lifestyle Change Diets on Blood Lipids, Lipoproteins, Glycemic Parameters, and Blood Pressure: A Systematic Review and Meta-Analysis of Clinical Trials. Nutr. Rev. 2024, 82, 176–192. [Google Scholar] [CrossRef]
- Dudum, R.; Juraschek, S.P.; Appel, L.J. Dose-Dependent Effects of Lifestyle Interventions on Blood Lipid Levels: Results from the PREMIER Trial. Patient Educ. Couns. 2019, 102, 1882–1891. [Google Scholar] [CrossRef]
- Charchar, F.J.; Prestes, P.R.; Mills, C.; Ching, S.M.; Neupane, D.; Marques, F.Z.; Sharman, J.E.; Vogt, L.; Burrell, L.M.; Korostovtseva, L.; et al. Lifestyle Management of Hypertension: International Society of Hypertension Position Paper Endorsed by the World Hypertension League and European Society of Hypertension. J. Hypertens. 2023, 42, 23. [Google Scholar] [CrossRef] [PubMed]
- Saleem, K.; Iahtisham-Ul-Haq; Abdi, G.; Rabail, R.; Aadil, R.M. Dietary and Lifestyle Modifications for Effective Management of Hypertension: A Comprehensive Review. J. Agric. Food Res. 2025, 20, 101750. [Google Scholar] [CrossRef]
- Berisha, H.; Hattab, R.; Comi, L.; Giglione, C.; Migliaccio, S.; Magni, P. Nutrition and Lifestyle Interventions in Managing Dyslipidemia and Cardiometabolic Risk. Nutrients 2025, 17, 776. [Google Scholar] [CrossRef]
- Noerman, S.; Landberg, R. Blood Metabolite Profiles Linking Dietary Patterns with Health—Toward Precision Nutrition. J. Intern. Med. 2023, 293, 408–432. [Google Scholar] [CrossRef]
- Belardo, D.; Michos, E.D.; Blankstein, R.; Blumenthal, R.S.; Ferdinand, K.C.; Hall, K.; Klatt, K.; Natajaran, P.; Ostfeld, R.J.; Reddy, K.; et al. Practical, Evidence-Based Approaches to Nutritional Modifications to Reduce Atherosclerotic Cardiovascular Disease: An American Society for Preventive Cardiology Clinical Practice Statement. Am. J. Prev. Cardiol. 2022, 10, 100323. [Google Scholar] [CrossRef]
- Sikand, G.; Severson, T. Top 10 Dietary Strategies for Atherosclerotic Cardiovascular Risk Reduction. Am. J. Prev. Cardiol. 2020, 4, 100106. [Google Scholar] [CrossRef]
- McNaughton, S.A.; Mishra, G.D.; Brunner, E.J. Food Patterns Associated with Blood Lipids Are Predictive of Coronary Heart Disease: The Whitehall II Study. Br. J. Nutr. 2009, 102, 619. [Google Scholar] [CrossRef] [PubMed]
- Denova-Gutiérrez, E.; Tucker, K.L.; Flores, M.; Barquera, S.; Salmerón, J. Dietary Patterns Are Associated with Predicted Cardiovascular Disease Risk in an Urban Mexican Adult Population. J. Nutr. 2016, 146, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Chi Htun, N.; Suga, H.; Imai, S.R.; Shimizu, W.R.; Ishikawa-Takata, K.R.; Takimoto, H. Dietary Pattern and Its Association with Blood Pressure and Blood Lipid Profiles among Japanese Adults in the 2012 Japan National Health and Nutrition Survey. Asia Pac. J. Clin. Nutr. 2018, 27, 1048–1061. [Google Scholar] [CrossRef]
- Altawili, A.A.; Altawili, M.; Alwadai, A.M.; Alahmadi, A.S.; Alshehri, A.M.A.; Muyini, B.H.; Alshwwaf, A.R.; Almarzooq, A.M.; Alqarni, A.H.A.; Alruwili, Z.A.L.; et al. An Exploration of Dietary Strategies for Hypertension Management: A Narrative Review. Cureus 2023, 15, e50130. [Google Scholar] [CrossRef]
- Gomez-Delgado, F.; Katsiki, N.; Lopez-Miranda, J.; Perez-Martinez, P. Dietary Habits, Lipoprotein Metabolism and Cardiovascular Disease: From Individual Foods to Dietary Patterns. Crit. Rev. Food Sci. Nutr. 2021, 61, 1651–1669. [Google Scholar] [CrossRef]
- Vamvakis, A.; Gkaliagkousi, E.; Lazaridis, A.; Grammatikopoulou, M.G.; Triantafyllou, A.; Nikolaidou, B.; Koletsos, N.; Anyfanti, P.; Tzimos, C.; Zebekakis, P.; et al. Impact of Intensive Lifestyle Treatment (Diet plus Exercise) on Endothelial and Vascular Function, Arterial Stiffness and Blood Pressure in Stage 1 Hypertension: Results of the Hintreat Randomized Controlled Trial. Nutrients 2020, 12, 1326. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Tölle, M.; Zidek, W.; van der Giet, M. Validation of the Mobil-O-Graph: 24 h-Blood Pressure Measurement Device. Blood Press. Monit. 2010, 15, 225–228. [Google Scholar] [CrossRef]
- Franssen, P.M.; Imholz, B.P. Evaluation of the Mobil-O-Graph New Generation ABPM Device Using the ESH Criteria. Blood Press. Monit. 2010, 15, 229–231. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Magriplis, E.; Zampelas, A.; Mitsopoulou, A.V.; Karageorgou, D.; Dimakopoulos, I.; Bakogianni, I.; Chourdakis, M.; Micha, R.; Michas, G.; et al. The Recalibrated HellenicSCORE Based on Newly Derived Risk Factors from the Hellenic National Nutrition and Health Survey (HNNHS); The HellenicSCORE II. Hell. J. Cardiol. 2021, 62, 285–290. [Google Scholar] [CrossRef]
- Katsiki, N.; Filippatos, T.; Vlachopoulos, C.; Panagiotakos, D.; Milionis, H.; Tselepis, A.; Garoufi, A.; Rallidis, L.; Richter, D.; Nomikos, T.; et al. Executive Summary of the Hellenic Atherosclerosis Society Guidelines for the Diagnosis and Treatment of Dyslipidemias—2023. Atheroscler. Plus 2024, 55, 74–92. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Arvaniti, F.; Stefanadis, C. Adherence to the Mediterranean Food Pattern Predicts the Prevalence of Hypertension, Hypercholesterolemia, Diabetes and Obesity, among Healthy Adults; The Accuracy of the MedDietScore. Prev. Med. 2007, 44, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Andrade, F.C.D. Diagnostic Status of Hypertension on the Adherence to the Dietary Approaches to Stop Hypertension (DASH) Diet. Prev. Med. Rep. 2016, 4, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hébert, J.R. Designing and Developing a Literature-Derived, Population-Based Dietary Inflammatory Index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef] [PubMed]
- Marfell-Jones, M.J.; Stewart, A.D.; Olds, T.; De Ridder, J.H. International Standards for Anthropometric Assessment; ISAK: Wellington, New Zealand, 2012. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Brown, W.J.; Clemes, S.A.; De Cocker, K.; Giles-Corti, B.; Hatano, Y.; Inoue, S.; Matsudo, S.M.; Mutrie, N.; et al. How Many Steps/Day Are Enough? For Adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 79. [Google Scholar] [CrossRef]
- Franczyk, B.; Gluba-Brzózka, A.; Ciałkowska-Rysz, A.; Ławiński, J.; Rysz, J. The Impact of Aerobic Exercise on HDL Quantity and Quality: A Narrative Review. Int. J. Mol. Sci. 2023, 24, 4653. [Google Scholar] [CrossRef]
- Mann, S.; Beedie, C.; Jimenez, A. Differential Effects of Aerobic Exercise, Resistance Training and Combined Exercise Modalities on Cholesterol and the Lipid Profile: Review, Synthesis and Recommendations. Sports Med. 2013, 44, 211. [Google Scholar] [CrossRef]
- Álvarez-Álvarez, I.; Martínez-González, M.Á.; Sánchez-Tainta, A.; Corella, D.; Díaz-López, A.; Fitó, M.; Vioque, J.; Romaguera, D.; Martínez, J.A.; Wärnberg, J.; et al. Adherence to an Energy-Restricted Mediterranean Diet Score and Prevalence of Cardiovascular Risk Factors in the PREDIMED-Plus: A Cross-Sectional Study. Rev. Española Cardiol. (Engl. Ed.) 2019, 72, 925–934. [Google Scholar] [CrossRef]
- Ahmed, F.S.; Wade, A.T.; Guenther, B.A.; Murphy, K.J.; Elias, M.F. Adherence to a Mediterranean Diet Associated with Lower Blood Pressure in a US Sample: Findings from the Maine-Syracuse Longitudinal Study. J. Clin. Hypertens. 2020, 22, 2276. [Google Scholar] [CrossRef]
- Zeenny, R.M.; Haddad, C.; Hajj, A.; Zeidan, R.K.; Salameh, P.; Ferrières, J. Adherence to the Mediterranean Diet and Cardiovascular Risk Factors among the Lebanese Population: A Nationwide Cross-Sectional Post Hoc Study. Nutrients 2024, 16, 2426. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Chrysoula, L.; Leonida, I.; Kotzakioulafi, E.; Theodoridis, X.; Chourdakis, M. Impact of the Level of Adherence to the Mediterranean Diet on Blood Pressure: A Systematic Review and Meta-Analysis of Observational Studies. Clin. Nutr. 2021, 40, 5771–5780. [Google Scholar] [CrossRef]
- Daidone, M.; Di Chiara, T.; Del Cuore, A.; Casuccio, A.; Salamone, G.; Di Raimondo, D.; Tuttolomondo, A. Mediterranean Diet and Hypertension: Relationship between Adherence to a Mediterranean Diet and Arterial Hypertension. BMC Nutr. 2025, 11, 44. [Google Scholar] [CrossRef]
- Hernáez, Á.; Castañer, O.; Elosua, R.; Pintó, X.; Estruch, R.; Salas-Salvadó, J.; Corella, D.; Arós, F.; Serra-Majem, L.; Fiol, M.; et al. Mediterranean Diet Improves High-Density Lipoprotein Function in High-Cardiovascular-Risk Individuals. Circulation 2017, 135, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Doménech, M.; Roman, P.; Lapetra, J.; García De La Corte, F.J.; Sala-Vila, A.; De La Torre, R.; Corella, D.; Salas-Salvadó, J.; Ruiz-Gutiérrez, V.; Lamuela-Raventós, R.M.; et al. Mediterranean Diet Reduces 24-Hour Ambulatory Blood Pressure, Blood Glucose, and Lipids: One-Year Randomized, Clinical Trial. Hypertension 2014, 64, 69–76. [Google Scholar] [CrossRef]
- Scaglione, S.; Di Chiara, T.; Daidone, M.; Tuttolomondo, A. Effects of the Mediterranean Diet on the Components of Metabolic Syndrome Concerning the Cardiometabolic Risk. Nutrients 2025, 17, 358. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yuan, H.; Yuan, J.; Zhang, Y. Study of The Mediterranean Diet and Its Significance for Hypertension Prevention. Highlights Sci. Eng. Technol. 2022, 19, 81–88. [Google Scholar] [CrossRef]
- Yu, E.; Ruiz-Canela, M.; Hu, F.B.; Clish, C.B.; Corella, D.; Salas-Salvadó, J.; Hruby, A.; Fitó, M.; Liang, L.; Toledo, E.; et al. Plasma Arginine/Asymmetric Dimethylarginine Ratio and Incidence of Cardiovascular Events: A Case-Cohort Study. J. Clin. Endocrinol. Metab. 2017, 102, 1879–1888. [Google Scholar] [CrossRef]
- Gkaliagkousi, E.; Gavriilaki, E.; Triantafyllou, A.; Nikolaidou, B.; Anyfanti, P.; Koletsos, N.; Vamvakis, A.; Dipla, K.; Lazaridis, A.; Douma, S. Asymmetric Dimethylarginine Levels Are Associated with Augmentation Index across Naïve Untreated Patients with Different Hypertension Phenotypes. J. Clin. Hypertens. 2018, 20, 680. [Google Scholar] [CrossRef]
- Thomazella, M.C.D.; Góes, M.F.S.; Andrade, C.R.; Debbas, V.; Barbeiro, D.F.; Correia, R.L.; Marie, S.K.N.; Cardounel, A.J.; Daluz, P.L.; Laurindo, F.R.M. Effects of High Adherence to Mediterranean or Low-Fat Diets in Medicated Secondary Prevention Patients. Am. J. Cardiol. 2011, 108, 1523–1529. [Google Scholar] [CrossRef]
- Davis, C.R.; Hodgson, J.M.; Woodman, R.; Bryan, J.; Wilson, C.; Murphy, K.J. A Mediterranean Diet Lowers Blood Pressure and Improves Endothelial Function: Results from the MedLey Randomized Intervention Trial. Am. J. Clin. Nutr. 2017, 105, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Pant, A.; Chew, D.P.; Mamas, M.A.; Zaman, S. Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses. Nutrients 2024, 16, 570. [Google Scholar] [CrossRef]
- Chiu, S.; Bergeron, N.; Williams, P.T.; Bray, G.A.; Sutherland, B.; Krauss, R.M. Comparison of the DASH (Dietary Approaches to Stop Hypertension) Diet and a Higher-Fat DASH Diet on Blood Pressure and Lipids and Lipoproteins: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2015, 103, 341. [Google Scholar] [CrossRef] [PubMed]
- Zare, P.; Bideshki, M.V.; Sohrabi, Z.; Behzadi, M.; Sartang, M.M. Effect of Dietary Approaches to Stop Hypertension (DASH) Diet on Lipid Profile in Individuals with Overweight/Obesity: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials. Nutr. Metab. Cardiovasc. Dis. 2025, 35, 104057. [Google Scholar] [CrossRef]
- Tyson, C.C.; Nwankwo, C.; Lin, P.H.; Svetkey, L.P. The Dietary Approaches to Stop Hypertension (DASH) Eating Pattern in Special Populations. Curr. Hypertens. Rep. 2012, 14, 388. [Google Scholar] [CrossRef]
- Obarzanek, E.; Sacks, F.M.; Vollmer, W.M.; Bray, G.A.; Miller, E.R.; Lin, P.H.; Karanja, N.M.; Most-Windhauser, M.M.; Moore, T.J.; Swain, J.F.; et al. Effects on Blood Lipids of a Blood Pressure-Lowering Diet: The Dietary Approaches to Stop Hypertension (DASH) Trial. Am. J. Clin. Nutr. 2001, 74, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Hou, C.; Yao, L.; Li, J.; Gui, M.; Wang, M.; Zhou, X.; Lu, B.; Fu, D. Dietary Inflammation Index Is Associated with Dyslipidemia: Evidence from National Health and Nutrition Examination Survey, 1999–2019. Lipids Health Dis. 2023, 22, 149. [Google Scholar] [CrossRef]
- Zeb, F.; Osaili, T.; Naqeeb, H.; Faris, M.A.E.; Cheikh Ismail, L.; Obaid, R.S.; Naja, F.; Radwan, H.; Hasan, H.; Hashim, M.; et al. Scientific Basis of Dietary Inflammatory Index (DII): A Dietary Tool to Metabolic Syndrome Risk. Clin. Nutr. Open Sci. 2025, 61, 138–161. [Google Scholar] [CrossRef]
- Jiang, R.; Wang, T.; Han, K.; Peng, P.; Zhang, G.; Wang, H.; Zhao, L.; Liang, H.; Lv, X.; Du, Y. Impact of Anti-Inflammatory Diets on Cardiovascular Disease Risk Factors: A Systematic Review and Meta-Analysis. Front. Nutr. 2025, 12, 1549831. [Google Scholar] [CrossRef] [PubMed]
- Sepehrinia, M.; Pourmontaseri, H.; Naghizadeh, M.M.; Vahid, F.; Hebert, J.R.; Homayounfar, R.; Alkamel, A. The Association between Energy-Adjusted Dietary Inflammatory Index and 10-Year Cardiovascular Risk: Fasa Adult Cohort Study. Food Sci. Nutr. 2024, 12, 5530–5537. [Google Scholar] [CrossRef] [PubMed]


| Baseline | |||||
|---|---|---|---|---|---|
| ILT (n = 33) | UC (n = 28) | ||||
| Mean ± SD | Mean ± SD | p | Cohens’ d | ||
| Anthropometric Indices | |||||
| Weight (kg) | 86.4 ± 16.7 | 85.9 ± 14.5 | 0.891 | 0.04 | |
| Height (cm) | 1.7 ± 0.1 | 1.7 ± 0.1 | 0.387 | 0.22 | |
| BMI (kg/m2) | 29.8 ± 5.2 | 28.9 ± 4.3 | 0.475 | 0.19 | |
| WC (cm) | 97.9 ± 13.6 | 100.0 ± 12.1 | 0.540 | 0.16 | |
| HC (cm) | 105.3 ± 8.8 | 100.6 ± 7.3 | 0.029 | 0.58 | |
| WC/HC | 0.9 ± 0.1 | 1.0 ± 0.1 | 0.035 | 0.56 | |
| Nutritional Indexes Scores | |||||
| DASH | 1.4 ± 1.1 | 1.4 ± 0.6 | 0.986 | 0.00 | |
| DII | 5.7 ± 1.1 | 5.3 ± 1.4 | 0.284 | 0.28 | |
| MedDiet | 31.8 ± 3.4 | 32.3 ± 5.6 | 0.724 | 0.1 | |
| Physical Activity | Effect size | ||||
| Pedometer PA categories * | |||||
| 1 | 0.8% | 0.7% | 0.266 | 0.21 a | |
| 2 | 18.2% | 0.2% | |||
| 3 | 0.0% | 0.1% | |||
| IPAQ PA categories ** | |||||
| 1 | 51.5% | 57.1% | 0.054 | 0.28 b | |
| 2 | 39.4% | 17.9% | |||
| 3 | 9.1% | 25.0% | |||
| Cohens’ d | |||||
| Mean steps per day (pedometer) | 6573 ± 231 | 6168 ± 1929 | 0.471 | 0.19 | |
| Blood Pressure | |||||
| Office BP | SBP (mmHg) | 143.2 ± 5.5 | 138.5 ± 8.6 | 0.013 | 0.66 |
| DBP (mmHg) | 90.3 ± 9.1 | 88.2 ± 7.1 | 0.316 | 0.26 | |
| ABPM | Daytime SBP (mmHg) | 139.8 ± 8.9 | 135.1 ± 6.3 | 0.022 | 0.61 |
| Daytime DBP (mmHg) | 92.5 ± 9.8 | 88.2 ± 7.4 | 0.063 | 0.49 | |
| Lipidemic Profile and CVD HRS | |||||
| TC (mg/dL) | 213.3 ± 38.2 | 212.0 ± 37.3 | 0.880 | 0.04 | |
| TG (mg/dL) | 117.7 ± 52.1 | 124.3 ± 61.4 | 0.653 | 0.12 | |
| HDL (mg/dL) | 47.6 ± 11.2 | 44.5 ± 10.6 | 0.271 | 0.29 | |
| LDL-C (mg/dL) | 147.2 ± 35.6 | 138.6 ± 34.5 | 0.345 | 0.25 | |
| Effect size | |||||
| CVD HRS (%) | 3.2 ± 3.4 | 3.6 ± 4.0 | 0.699 | 0.1 | |
| CVD HRS Category *** | |||||
| 1 | 3.0% | 3.6% | 0.542 | 0.19 a | |
| 2 | 69.7% | 71.4% | |||
| 3 | 24.2% | 14.3% | |||
| 4 | 3.0% | 10.7% | |||
| Dyslipidemia **** | |||||
| 0 | 0.0% | 10.7% | 0.054 | 0.25 b | |
| 1 | 100.0% | 89.3% | |||
| ILT (n = 33) | UC (n = 28) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 Months | Baseline | 6 Months | |||||
| Variable | Mean Dif ± SEM | 95% CI | p | Cohen’s d | Mean Dif ± SEM | 95% CI | p | Cohen’s d |
| Anthropometry | ||||||||
| Weight (kg) | −6.6 ± 1.1 | [−8.7 to −4.4] | <0.001 | 1.08 | 0.4 ± 0.8 | [−1.2 to 2.0] | 0.618 | 0.10 |
| BMI (kg/m2) | −2.3 ± 0.4 | [−3.0 to −1.5] | <0.001 | 1.10 | 0.1 ± 0.3 | [−0.4 to 0.6] | 0.691 | 0.08 |
| WC (cm) | −8.4 ± 1.0 | [−10.5 to −6.3] | <0.001 | 1.43 | −0.6 ± 1.1 | [−2.8 to 1.6] | 0.580 | 0.11 |
| HC (cm) | −8.3 ± 0.9 | [−10.0 to −6.5] | <0.001 | 1.70 | −0.6 ± 0.8 | [−2.2 to 1.0] | 0.429 | 0.15 |
| Lipidemic Profile | ||||||||
| TC (mg/dL) | −35.4 ± 4.6 | [−44.8 to −26.0] | <0.0001 | 1.33 | −1.6 ± 6.4 | [−14.8 to 11.6] | 0.804 | 0.05 |
| TG (mg/dL) | −21.4 ± 5.0 | [−31.5 to −11.3] | <0.0001 | 0.75 | 0.8 ± 8.1 | [−15.8 to 17.3] | 0.927 | 0.02 |
| HDL (mg/dL) | 0.7 ± 1.0 | [−1.2 to 2.6] | 0.470 | 0.13 | −0.2 ± 1.0 | [−2.2 to 1.8] | 0.855 | 0.04 |
| LDL-C (mg/dL) | −27.8 ± 5.7 | [−39.0 to −16.1] | <0.0001 | 0.85 | −0.6 ± 5.7 | [−12.2 to 11.0] | 0.915 | 0.02 |
| CVD HRS (%) | −1.5 ± 0.3 | [−2.0 to −1.0] | <0.0001 | 1.00 | −0.5 ± 0.3 | [−1.1 to 0.1] | 0.114 | 0.31 |
| CVD HRS Category * (n) | Effect size | Effect size | ||||||
| 1 | 8 | <0.0001 | 4 | 0 | 0.180 | 1.34 | ||
| 2 | 0 | 1 | ||||||
| 3 | −8 | 1 | ||||||
| 4 | 0 | −2 | ||||||
| Dyslipidemia ** (n) | ||||||||
| 0 | 10 | 0.002 | 3.0 | 0 | 1.000 | 0.5 | ||
| 1 | −10 | 0 | ||||||
| Physical Activity | ||||||||
| Pedometer PA categories *** | (n) | |||||||
| 1 | −4 | 0.046 | 1.6 | 0 | 0.109 | 0.38 | ||
| 2 | 2 | 1 | ||||||
| 3 | 2 | −1 | ||||||
| IPAQ PA categories **** | (n) | 0.705 | 0.24 | |||||
| 1 | −5 | 0.808 | 2.0 | −1 | ||||
| 2 | 2 | 3 | ||||||
| 3 | 3 | −2 | ||||||
| Mean steps per day (pedometer) | 1096.7 ± 303.9 | [477.7 to 1715.7] | 0.001 | 0.69 | 175.1 ± 369.7 | [−583.5 to 933.6] | 0.640 | 0.90 |
| ILT (n = 33) | UC (n = 28) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 Months | Baseline | 6 Months | |||||
| Variable | Mean Dif ± SEM | 95% CI | p | Cohen’s d | Mean Dif ± SEM | 95% CI | p | Cohen’s d |
| DASH | 1.1 ± 0.2 | [0.7 to 1.6] | <0.0001 | 0.89 | 0.5 ± 0.2 | [0.2 to 0.9] | 0.005 | 0.58 |
| DII | −5.8 ± 0.2 | [−6.2 to −5.5] | <0.0001 | 6.10 | −0.3 ± 0.3 | [−0.9 to 0.3] | 0.312 | 0.20 |
| MedDiet | 6.4 ± 0.4 | [5.5 to 7.3] | <0.0001 | 2.55 | −1.0 ± 0.7 | [−2.4 to 0.3] | 0.131 | 0.30 |
| Unstandardized Coefficients | Standardized Coefficients | |||||||
|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | p | 95% C.I. for B | ||||
| ILT | CVD HRS | DII | 0.973 | 0.203 | 0.628 | 4.786 | <0.001 | [0.6 to 1.4] |
| TC | Med Diet | −7.238 | 1.383 | −0.684 | −5.235 | <0.001 | [−10.1 to −4.4] | |
| TG | Med Diet | −4.103 | 1.85 | −0.362 | −2.218 | 0.035 | [−7.9 to −0.3] | |
| TG | DASH | 9.913 | 3.618 | 0.433 | 2.74 | 0.010 | [2.5 to 17.3] | |
| LDL-C | Med Diet | −6.431 | 2.063 | −0.492 | −3.117 | 0.004 | [−10.7 to −2.2] | |
| UC | CVD HRS | DII | 0.05 | 0.215 | 0.048 | 0.232 | 0.819 | [−0.4 to 0.5] |
| TC | Med Diet | −3.581 | 1.722 | −0.365 | −2.08 | 0.048 | [−7.1 to 0.0] | |
| TG | Med Diet | 1.033 | 2.603 | 0.084 | 0.397 | 0.695 | [−4.4 to 6.4] | |
| TG | DASH | −6.92 | 9.157 | −0.151 | −0.756 | 0.457 | [−25.8 to 12.0] | |
| LDL-C | Med Diet | −3.974 | 1.505 | −0.46 | −2.641 | 0.014 | [−7.1 to −0.9] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vamvakis, A.; Lazaridis, A.; Grammatikopoulou, M.G.; Malliora, A.; Tsiroukidou, K.; Tzimos, C.; Blasio, A.D.; Izzicupo, P.; Gkaliagkousi, E. Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial. Nutrients 2025, 17, 2632. https://doi.org/10.3390/nu17162632
Vamvakis A, Lazaridis A, Grammatikopoulou MG, Malliora A, Tsiroukidou K, Tzimos C, Blasio AD, Izzicupo P, Gkaliagkousi E. Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial. Nutrients. 2025; 17(16):2632. https://doi.org/10.3390/nu17162632
Chicago/Turabian StyleVamvakis, Anastasios, Antonios Lazaridis, Maria G. Grammatikopoulou, Anastasia Malliora, Kyriaki Tsiroukidou, Christos Tzimos, Andrea Di Blasio, Pascal Izzicupo, and Eugenia Gkaliagkousi. 2025. "Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial" Nutrients 17, no. 16: 2632. https://doi.org/10.3390/nu17162632
APA StyleVamvakis, A., Lazaridis, A., Grammatikopoulou, M. G., Malliora, A., Tsiroukidou, K., Tzimos, C., Blasio, A. D., Izzicupo, P., & Gkaliagkousi, E. (2025). Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial. Nutrients, 17(16), 2632. https://doi.org/10.3390/nu17162632







