Vitamin D Supplementation in the Czech Republic: Socioeconomic Determinants and Public Awareness Gaps
Abstract
1. Introduction
2. Materials and Methods
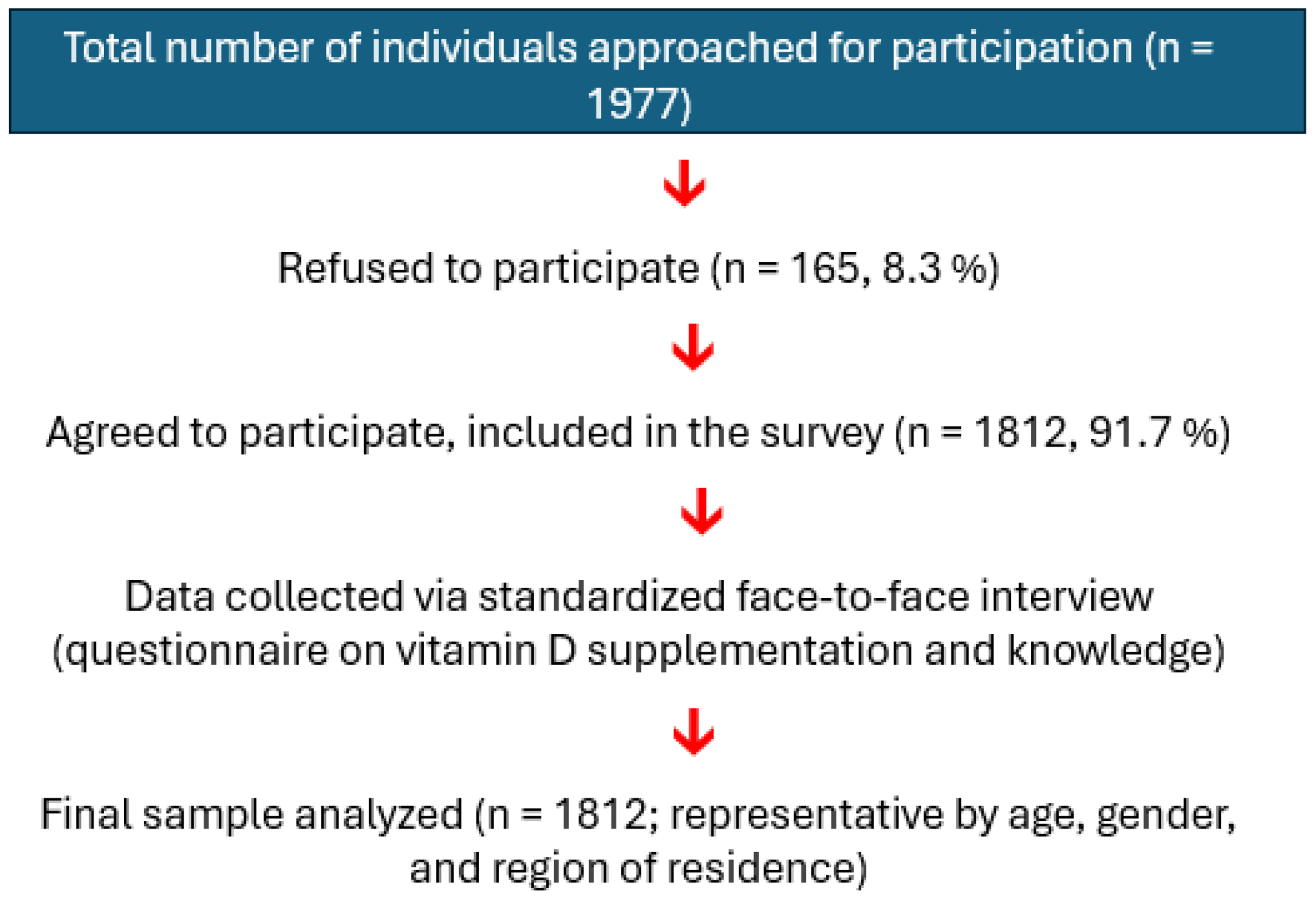
2.1. Study Design and Participants
2.2. The Questionnaire
2.3. Statistics
3. Results
3.1. Demographic Data
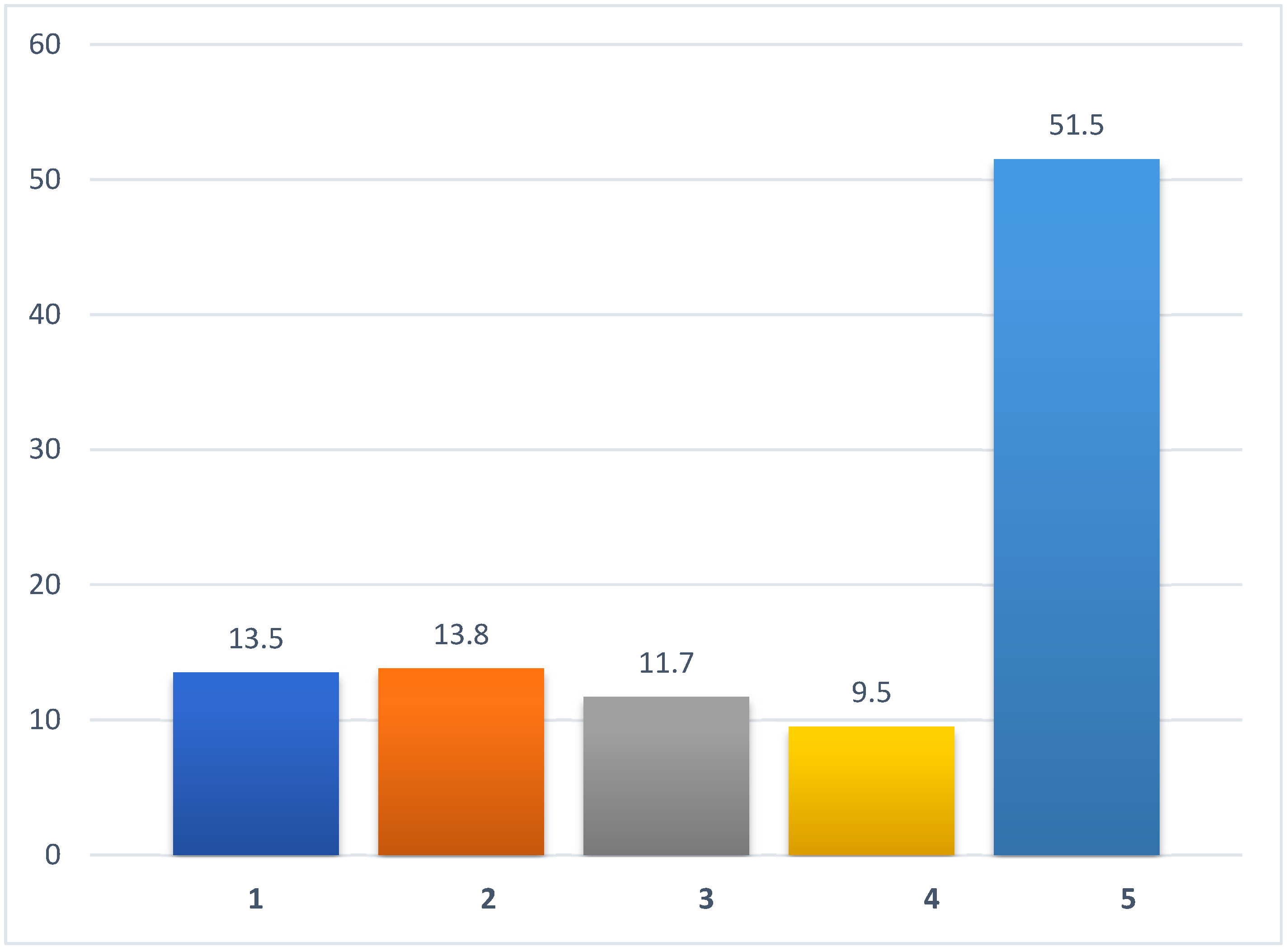
3.2. Intake of Vitamin D Supplements and Association Between Supplementation and Sociodemographic Data
3.3. Dependence of Vitamin D Supplementation on Socioeconomic Factors
3.4. Trends in Vitamin D Supplementation, Pre-Pandemic and Post-Pandemic, and Association with Socioeconomic Factors
3.5. Association Between Period (Before, During, and After the COVID-19 Pandemic) of Vitamin D Use and Socioeconomic Characteristics
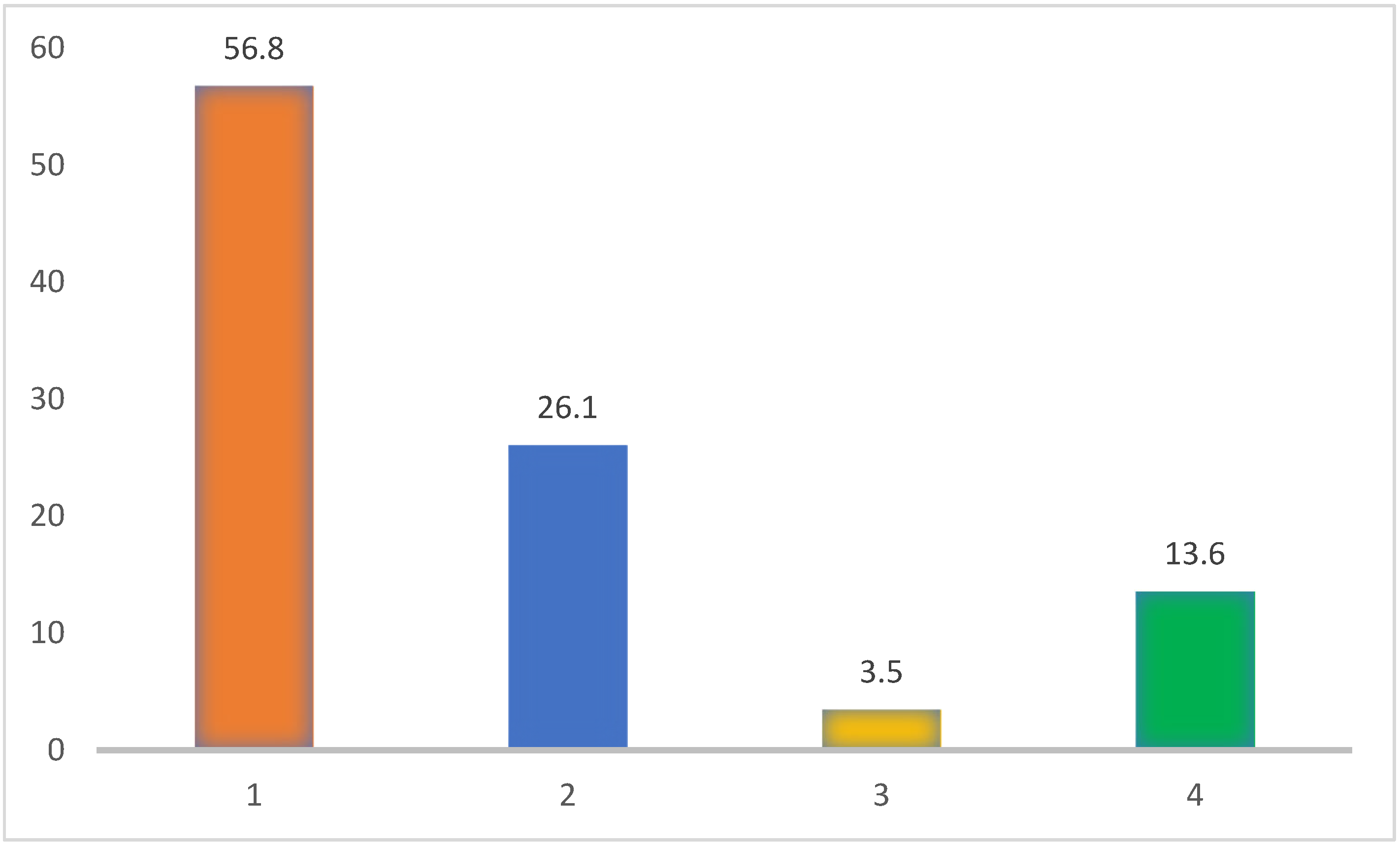
3.6. Reasons for Vitamin D Supplementation
3.7. Association Between Reasons for Vitamin D Supplementation and Sociodemographic Data
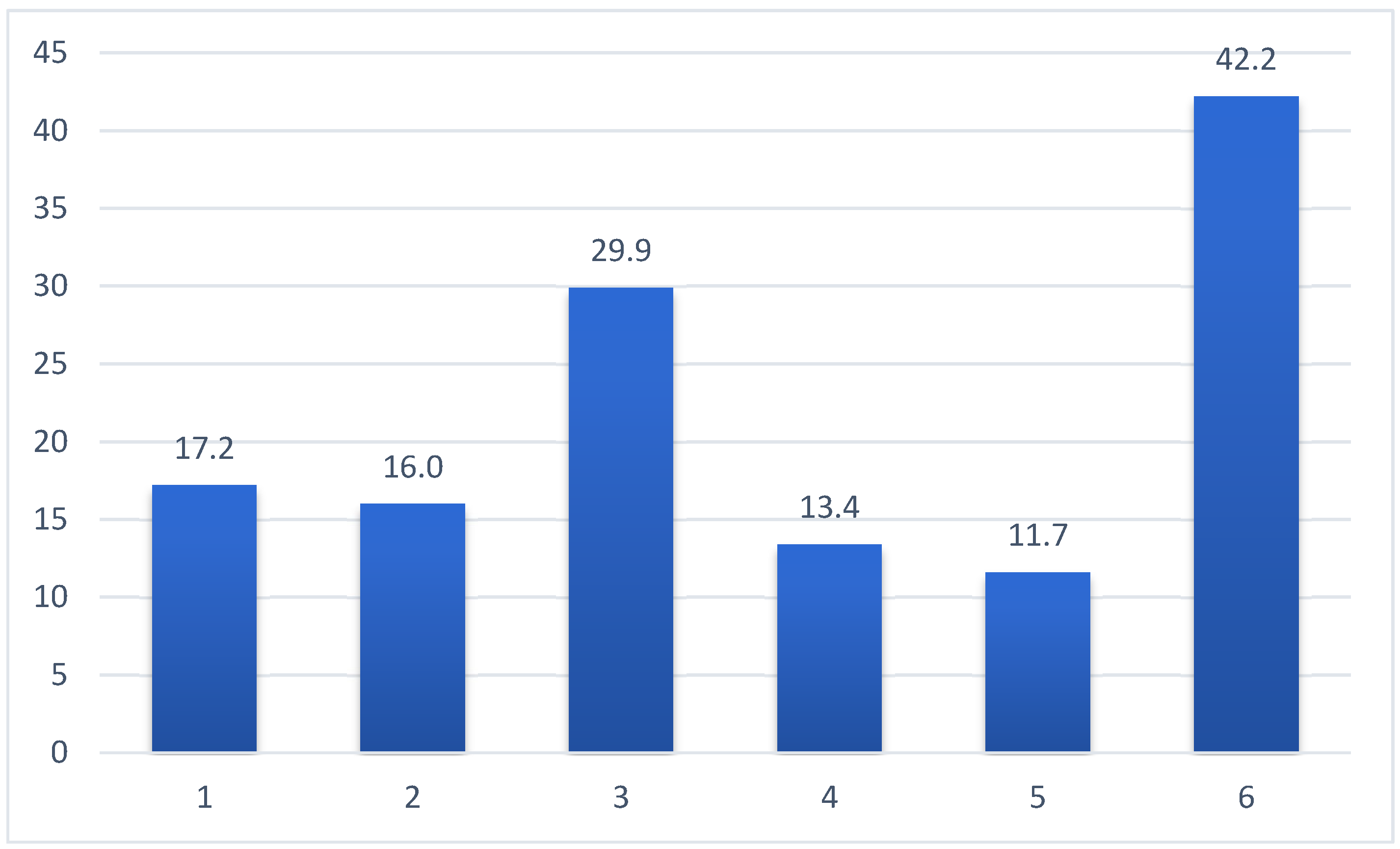
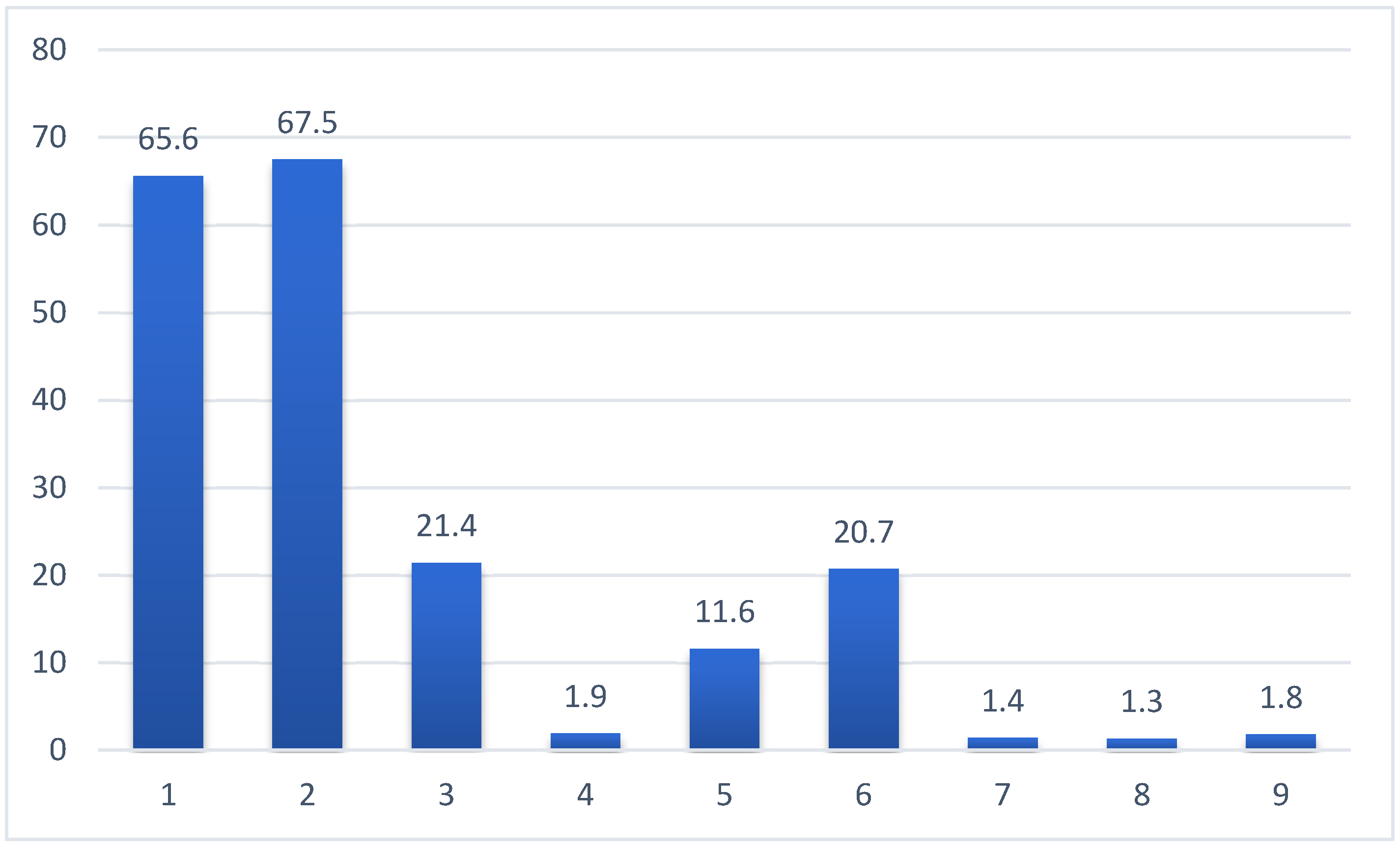
3.8. Participants’ Knowledge of the Importance of Vitamin D for Human Health
3.9. The Association Between Knowledge About the Effect of Vitamin D on the Human Body and Sociodemographic Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, S.; Miller, D.D.; Li, W.; Slominski, A.; Cucchiarini, M. Non-Musculoskeletal Benefits of Vitamin D beyond the Musculoskeletal System. Int. J. Mol. Sci. 2021, 22, 2128. [Google Scholar] [CrossRef]
- Daryabor, G.; Gholijani, N.; Kahmini, F.R. A Review of the Critical Role of Vitamin D Axis on the Immune System. Exp. Mol. Pathol. 2023, 132–133, 104866. [Google Scholar] [CrossRef]
- Dunlop, E.; Pham, N.M.; Van Hoang, D.; Mazahery, H.; Neo, B.; Shrapnel, J.; Kalmpourtzidou, A.; Chai, K.E.K.; Ng, L.; Black, L.J. A Systematic Review and Meta-Analysis of Circulating 25-Hydroxyvitamin D Concentration and Vitamin D Status Worldwide. J. Public Health 2025, fdaf080. [Google Scholar] [CrossRef]
- Cui, A.; Zhang, T.; Xiao, P.; Fan, Z.; Wang, H.; Zhuang, Y. Global and Regional Prevalence of Vitamin D Deficiency in Population-Based Studies from 2000 to 2022: A Pooled Analysis of 7.9 Million Participants. Front. Nutr. 2023, 10, 1070808. [Google Scholar] [CrossRef] [PubMed]
- Raymond-Lezman, J.R.; Riskin, S.I. Benefits and Risks of Sun Exposure to Maintain Adequate Vitamin D Levels. Cureus 2023, 15, e38578. [Google Scholar] [CrossRef] [PubMed]
- Mertens, E.; Kuijsten, A.; Dofková, M.; Mistura, L.; D’Addezio, L.; Turrini, A.; Dubuisson, C.; Favret, S.; Havard, S.; Trolle, E.; et al. Geographic and Socioeconomic Diversity of Food and Nutrient Intakes: A Comparison of Four European Countries. Eur. J. Nutr. 2019, 58, 1475–1493. [Google Scholar] [CrossRef] [PubMed]
- Delrue, C.; Speeckaert, M.M. Vitamin D and Vitamin D-Binding Protein in Health and Disease. Int. J. Mol. Sci. 2023, 24, 4642. [Google Scholar] [CrossRef]
- Sha, S.; Gwenzi, T.; Chen, L.J.; Brenner, H.; Schöttker, B. About the Associations of Vitamin D Deficiency and Biomarkers of Systemic Inflammatory Response with All-Cause and Cause-Specific Mortality in a General Population Sample of Almost 400,000 UK Biobank Participants. Eur. J. Epidemiol. 2023, 38, 957. [Google Scholar] [CrossRef]
- Desai, S.R.; Ko, Y.A.; Liu, C.; Hafeez, Z.; Park, J.; Faaborg-Andersen, C.; Alvi, Z.; Alras, Z.; Alkhoder, A.A.; Martini, A.; et al. Vitamin D Deficiency, Inflammation, and Diminished Endogenous Regenerative Capacity in Coronary Heart Disease. JACC Adv. 2024, 3, 100804. [Google Scholar] [CrossRef]
- Holmannova, D.; Borsky, P.; Kremlacek, J.; Krejsek, J.; Hodacova, L.; Cizkova, A.; Fiala, Z.; Borska, L. High Prevalence of Low Vitamin D Status in the Czech Republic: A Retrospective Study of 119,925 Participants. Eur. J. Clin. Nutr. 2025, 79, 641–652. [Google Scholar] [CrossRef]
- Pludowski, P.; Grant, W.B.; Karras, S.N.; Zittermann, A.; Pilz, S. Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 Μg) of Vitamin D for Adults in the General Population. Nutrients 2024, 16, 391. [Google Scholar] [CrossRef]
- Zittermann, A.; Trummer, C.; Theiler-Schwetz, V.; Pilz, S. Long-Term Supplementation with 3200 to 4000 IU of Vitamin D Daily and Adverse Events: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. J. Nutr. 2023, 62, 1833. [Google Scholar] [CrossRef]
- Bresson, J.L.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.I.; Mangelsdorf, I.; McArdle, H.; Naska, A.; Neuhäuser-Berthold, M.; et al. Dietary Reference Values for Vitamin D. EFSA J. 2016, 14, e04547. [Google Scholar] [CrossRef]
- Griffin, G.; Hewison, M.; Hopkin, J.; Kenny, R.A.; Quinton, R.; Rhodes, J.; Subramanian, S.; Thickett, D. Preventing Vitamin D Deficiency during the COVID-19 Pandemic: UK Definitions of Vitamin D Sufficiency and Recommended Supplement Dose Are Set Too Low. Clin. Med. 2021, 21, e48–e51. [Google Scholar] [CrossRef]
- Age Structure of the Population—2022|Products. Available online: https://csu.gov.cz/produkty/age-structure-of-the-population-2022 (accessed on 4 February 2025).
- Mendes, M.M.; Gomes, A.P.O.; Araújo, M.M.; Coelho, A.S.G.; Carvalho, K.M.B.; Botelho, P.B. Prevalence of Vitamin D Deficiency in South America: A Systematic Review and Meta-Analysis. Nutr. Rev. 2023, 81, 1290–1309. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Pu, R.; Li, N.; Chen, C.; Li, J.; Dai, W.; Wang, Y.; Hu, J.; Zhu, D.; Yu, Q.; et al. High Prevalence of Vitamin D Deficiency in Asia: A Systematic Review and Meta-Analysis. Crit. Rev. Food Sci. Nutr. 2023, 63, 3602–3611. [Google Scholar] [CrossRef] [PubMed]
- Brouwer-Brolsma, E.M.; Vaes, A.M.M.; van der Zwaluw, N.L.; van Wijngaarden, J.P.; Swart, K.M.A.; Ham, A.C.; van Dijk, S.C.; Enneman, A.W.; Sohl, E.; van Schoor, N.M.; et al. Relative Importance of Summer Sun Exposure, Vitamin D Intake, and Genes to Vitamin D Status in Dutch Older Adults: The B-PROOF Study. J. Steroid Biochem. Mol. Biol. 2016, 164, 168–176. [Google Scholar] [CrossRef]
- Rabenberg, M.; Scheidt-Nave, C.; Busch, M.A.; Rieckmann, N.; Hintzpeter, B.; Mensink, G.B.M. Vitamin D Status among Adults in Germany—Results from the German Health Interview and Examination Survey for Adults (DEGS1). BMC Public Health 2015, 15, 715–728. [Google Scholar] [CrossRef] [PubMed]
- Shatylo, S.; Bogomaz, V.; Babych, O. Vitamin D Deficiency in Ukraine: A Multicentre Cross-Sectional Study. Glob. Epidemiol. 2024, 8, 100170. [Google Scholar] [CrossRef]
- Engelsen, O. The Relationship between Ultraviolet Radiation Exposure and Vitamin D Status. Nutrients 2010, 2, 482–495. [Google Scholar] [CrossRef]
- Religi, A.; Backes, C.; Chatelan, A.; Bulliard, J.L.; Vuilleumier, L.; Moccozet, L.; Bochud, M.; Vernez, D. Estimation of Exposure Durations for Vitamin D Production and Sunburn Risk in Switzerland. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 742–752. [Google Scholar] [CrossRef]
- USDA Description Measure Vitamin D (IU) per Measure. Available online: https://www.nal.usda.gov/sites/default/files/page-files/Vitamin%20DIU.pdf (accessed on 15 July 2025).
- Spiro, A.; Buttriss, J.L. Vitamin D: An Overview of Vitamin D Status and Intake in Europe. Nutr. Bull. 2014, 39, 322–350. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.D. 100 Years of Vitamin D: Global Differences in Vitamin D Status and Dietary Intake: A Review of the Data. Endocr. Connect. 2022, 11, e210282. [Google Scholar] [CrossRef] [PubMed]
- Bischofova, S.; Dofkova, M.; Blahova, J.; Kavrik, R.; Nevrla, J.; Rehurkova, I.; Ruprich, J. Dietary Intake of Vitamin D in the Czech Population: A Comparison with Dietary Reference Values, Main Food Sources Identified by a Total Diet Study. Nutrients 2018, 10, 1452. [Google Scholar] [CrossRef] [PubMed]
- Stachoń, M.; Lachowicz, K. Assessment of Determinants of Dietary Vitamin D Intake in a Polish National Sample of Male Adolescents. Nutrients 2025, 17, 2024. [Google Scholar] [CrossRef]
- Saternus, R.; Vogt, T.; Reichrath, J. A Critical Appraisal of Strategies to Optimize Vitamin D Status in Germany, a Population with a Western Diet. Nutrients 2019, 11, 2682. [Google Scholar] [CrossRef]
- Grønborg, I.M.; Tetens, I.; Ege, M.; Christensen, T.; Andersen, E.W.; Andersen, R. Modelling of Adequate and Safe Vitamin D Intake in Danish Women Using Different Fortification and Supplementation Scenarios to Inform Fortification Policies. Eur. J. Nutr. 2019, 58, 227–232. [Google Scholar] [CrossRef]
- Sha, S.; Nguyen, T.M.N.; Kuznia, S.; Niedermaier, T.; Zhu, A.; Brenner, H.; Schöttker, B. Real-World Evidence for the Effectiveness of Vitamin D Supplementation in Reduction of Total and Cause-Specific Mortality. J. Intern. Med. 2023, 293, 384–397. [Google Scholar] [CrossRef]
- Tanna, N.K.; Karki, M.; Webber, I.; Alaa, A.; El-Costa, A.; Blair, M. Knowledge, Attitudes, and Practices Associated with Vitamin D Supplementation: A Cross-Sectional Online Community Survey of Adults in the UK. PLoS ONE 2023, 18, e0281172. [Google Scholar] [CrossRef]
- Paparodis, R.D.; Bantouna, D.; Karvounis, E.; Zoupas, I.; Livadas, S.; Angelopoulos, N.; Imam, S.; Papadimitriou, D.T.; Jaume, J.C. Intense Testing and Use of Vitamin D Supplements Leads to Slow Improvement in Vitamin D Adequacy Rates: A Cross-Sectional Analysis of Real-World Data. Nutrients 2023, 16, 111. [Google Scholar] [CrossRef]
- Zaremba, S.M.M.; Conduit-Turner, K. Knowledge of Vitamin D and Practices of Vitamin D Supplementation in a Scottish Adult Population: A Cross-Sectional Study. Nutr. Health 2025, 31, 715–728. [Google Scholar] [CrossRef]
- Mishra, S.; Stierman, B.; Gahche, J.J.; Potischman, N. Dietary Supplement Use among Adults: United States, 2017–2018. NCHS Data Brief. 2021, 1–8. [Google Scholar] [CrossRef]
- McCormack, D.; Mai, X.; Chen, Y. Determinants of Vitamin D Supplement Use in Canadians. Public Health Nutr. 2017, 20, 1768–1774. [Google Scholar] [CrossRef]
- Reinert, A.; Rohrmann, S.; Becker, N.; Linseisen, J. Lifestyle and Diet in People Using Dietary Supplements: A German Cohort Study. Eur. J. Nutr. 2007, 46, 165–173. [Google Scholar] [CrossRef]
- Mahdavi-Roshan, M.; Rezazadeh, A.; Joukar, F.; Khorshidi, Y.; Naghipour, M.; Mansour-Ghanaei, F. Dietary Supplements Consumption and Its Association with Socioeconomic Factors, Obesity and Main Non-Communicable Chronic Diseases in the North of Iran: The PERSIAN Guilan Cohort Study (PGCS). BMC Nutr. 2021, 7, 84. [Google Scholar] [CrossRef] [PubMed]
- Wei, N.; Sun, D. Children’s Education and Parents’ Dietary Nutrient Intake: An Empirical Study Based on Rural China. Humanit. Soc. Sci. Commun. 2023, 10, 336. [Google Scholar] [CrossRef]
- Chiba, T.; Kobayashi, E.; Okura, T.; Sekimoto, M.; Mizuno, H.; Saito, M.; Umegaki, K. An Educational Intervention Improved Knowledge of Dietary Supplements in College Students. BMC Public Health 2020, 20, 633. [Google Scholar] [CrossRef] [PubMed]
- COVID-19: Doplňky Stravy Při Pandemii|NZIP. Available online: https://www.nzip.cz/clanek/1082-covid-19-doplnky-stravy-pri-pandemii (accessed on 6 February 2025).
- Pal, R.; Banerjee, M.; Bhadada, S.K.; Shetty, A.J.; Singh, B.; Vyas, A. Vitamin D Supplementation and Clinical Outcomes in COVID-19: A Systematic Review and Meta-Analysis. J. Endocrinol. Investig. 2022, 45, 53. [Google Scholar] [CrossRef]
- Chen, J.; Lu, F.; Shen, B.; Xu, H.; Chen, Y.; Hu, Q.; Xu, A.; Tung, T.H.; Hong, D. Associations between Pre-Infection Serum Vitamin D Concentrations and Omicron COVID-19 Incidence, Severity and Reoccurrence in Elderly Individuals. Public Health Nutr. 2024, 27, e197. [Google Scholar] [CrossRef]
- Tariq, A.; Khan, S.R.; Basharat, A. Assessment of Knowledge, Attitudes and Practice towards Vitamin D among University Students in Pakistan. BMC Public Health 2020, 20, 355. [Google Scholar] [CrossRef]
- Alkalash, S.H.; Odah, M.; Alkenani, H.H.; Hibili, N.H.; Al-Essa, R.S.; Almowallad, R.T.; Aldabali, S. Public Knowledge, Attitude, and Practice Toward Vitamin D Deficiency in Al-Qunfudhah Governorate, Saudi Arabia. Cureus 2023, 15, e33756. [Google Scholar] [CrossRef]
- Zadka, K.; Pałkowska-Goździk, E.; Rosołowska-Huszcz, D. The State of Knowledge about Nutrition Sources of Vitamin D, Its Role in the Human Body, and Necessity of Supplementation among Parents in Central Poland. Int. J. Environ. Res. Public Health 2018, 15, 1489. [Google Scholar] [CrossRef]
- Alibrahim, H.; Swed, S.; Bohsas, H.; Abouainain, Y.; Jawish, N.; Diab, R.; Ishak, A.; Saleh, H.H.; Nasif, M.N.; Arafah, R.; et al. Assessment the Awareness of Vitamin D Deficiency among the General Population in Syria: An Online Cross-Sectional Study. BMC Public Health 2024, 24, 938. [Google Scholar] [CrossRef]
- Grużewska, A.; Grużewska-Piotrowska, K. Vitamin D—Knowledge among People about Its Properties and Effects Based on Anonymous Surveys. Qual. Sport 2023, 14, 113–125. [Google Scholar] [CrossRef]
- Kwabena, A.A.; Appiah, B.; Danso, S.A.; Agomuo, S.K.S.; Kwarteng, S.; Senu, E.; Effah, A.; Sakyi, S.A.; Fondjo, L.A. Knowledge, Attitude and Practices Regarding Vitamin D among Adults in Ghana: A Cross-Sectional Study. BMC Public Health 2025, 25, 212. [Google Scholar] [CrossRef] [PubMed]
- Zgliczyński, W.S.; Zgliczyński, Z.; Rostkowska, O.M.; Sarecka-Hujar, B.; Carlberg, C. Vitamin D Knowledge, Attitudes and Practices of Polish Medical Doctors. Nutrients 2021, 13, 2443. [Google Scholar] [CrossRef]
- Rasouli, M.A.; Darvishzadehdaledari, S.; Alizadeh, Z.; Moradi, G.; Gholami, F.; Mahmoudian, A. Vitamin D Supplementation and Cardiovascular Disease Risks in More Than 134,000 Individuals in 29 Randomized Clinical Trials and 157,000 Individuals in 30 Prospective Cohort Studies: An Updated Systematic Review and Meta-Analysis. J. Res. Health Sci. 2023, 23, e00594. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-J.; Sha, S.; Stocker, H.; Brenner, H.; Schöttker, B. The Associations of Serum Vitamin D Status and Vitamin D Supplements Use with All-Cause Dementia, Alzheimer’s Disease, and Vascular Dementia: A UK Biobank Based Prospective Cohort Study. Am. J. Clin. Nutr. 2024, 119, 1052–1064. [Google Scholar] [CrossRef]
- Tekeli, S.Ö.; Köse, Ö.; Yapar, D.; Tekeli, F.Y.; Asoğlu, M.M.; Kartal, E.M. Relationship between Serum Vitamin D Levels and the Prevalence of Knee Osteoarthritis: A Retrospective Study on 3424 Subjects. Technol. Health Care 2024, 32, 3649–3658. [Google Scholar] [CrossRef]
- Jung, H.; Kwon, Y.D.; Noh, J.W. Financial Burden of Catastrophic Health Expenditure on Households with Chronic Diseases: Financial Ratio Analysis. BMC Health Serv. Res. 2022, 22, 568. [Google Scholar] [CrossRef]
- Van De Ven, D.; Robroek, S.J.W.; Burdorf, A.; Schuring, M. Inequalities in the Impact of Having a Chronic Disease on Entering Permanent Paid Employment: A Registry-Based 10-Year Follow-up Study. J. Epidemiol. Community Health 2023, 77, 474–480. [Google Scholar] [CrossRef]
- de Rijk, A.; Carrasco-Negüe, K.; Houkes, I. The Cross-Country Comparison Model for Labor Participation (CCC Model for LP) of Persons with Chronic Diseases. J. Occup. Rehabil. 2022, 32, 225–240. [Google Scholar] [CrossRef]
- Holman, H.R. The Relation of the Chronic Disease Epidemic to the Health Care Crisis. ACR Open Rheumatol. 2020, 2, 167–173. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Walli-Attaei, M.; Gray, A.; Torbica, A.; Maggioni, A.P.; Huculeci, R.; Bairami, F.; Aboyans, V.; Timmis, A.D.; Vardas, P.; et al. Economic Burden of Cardiovascular Diseases in the European Union: A Population-Based Cost Study. Eur. Heart J. 2023, 44, 4752–4767. [Google Scholar] [CrossRef]
| Years | Males | Females | ||||
|---|---|---|---|---|---|---|
| N | % | Deviation | N | % | Deviation | |
| 15–19 | 58 | 3.2 | 0.1 | 56 | 3.1 | 0.1 |
| 20–24 | 52 | 2.9 | 0.1 | 51 | 2.8 | 0.1 |
| 25–34 | 133 | 7.3 | 0.1 | 126 | 7 | 0.1 |
| 35–44 | 157 | 8.7 | −0.1 | 153 | 8.4 | 0 |
| 45–54 | 168 | 9.3 | −0.1 | 165 | 9.1 | 0 |
| 55–64 | 126 | 7 | −0.1 | 127 | 7 | −0.1 |
| >65 | 186 | 10.3 | 0.1 | 254 | 14 | −0.1 |
| Occupation | Number |
|---|---|
| Manager, Director, Executive | 87 |
| Mental Worker | 125 |
| Armed Forces Employee | 64 |
| Engineer, Technician | 94 |
| Clerk, Administrative Worker | 151 |
| Service Worker | 357 |
| Farmer, Agricultural Worker, Forester | 30 |
| Laborer, Worker | 109 |
| Craftsman | 56 |
| Self-employed | 47 |
| Entrepreneur | 33 |
| Student | 182 |
| Homemaker, Parental leave | 38 |
| Retiree, Pensioner, Disabled Pensioner | 426 |
| Unemployed | 13 |
| Income | |
| 0.0–20,000 | 129 |
| 20,001–30,000 | 291 |
| 30,001–40,000 | 354 |
| 40,001–50,000 | 308 |
| 50,001–60,000 | 269 |
| 60,001–70,000 | 198 |
| 70,001–80,000 | 263 |
| Marital status | |
| Single | 492 |
| Married | 859 |
| Divorced | 215 |
| Widower, Widow | 172 |
| Partner, Common-law Partner | 74 |
| Education | |
| Primary/Elementary | 121 |
| Vocational Training or Secondary Education without a Diploma | 512 |
| High School Diploma, Higher Vocational Education | 795 |
| Bachelor’s Degree, University Degree | 384 |
| Total | 1812 |
| Vitamin D Supplementation | Value X2 | df | p Value |
|---|---|---|---|
| Gender | 55.92 | 4 | <0.001 |
| Age | 38.81 | 24 | ˂0.05 |
| Marital status | 39.22 | 16 | ˂0.001 |
| Education | 51.90 | 12 | ˂0.001 |
| Size of place of residence | 17.96 | 20 | 0.590 n.s. |
| Monthly household income | 24.13 | 8 | ˂0.01 |
| Occupation | 44.60 | 12 | ˂0.001 |
| Value X2 | df | p Value | |
|---|---|---|---|
| Gender | 3.89 | 3 | 0.27 n.s. |
| Age | 43.96 | 18 | ˂0.001 |
| Marital status | 34.35 | 12 | ˂0.001 |
| Education | 15.37 | 9 | 0.08 n.s. |
| Size of place of residence | 18.12 | 15 | 0.25 n.s. |
| Monthly household income | 10.43 | 6 | 0.11 n.s. |
| Occupation | 16.61 | 9 | 0.06 n.s. |
| Value X2 | df | p Value | |
|---|---|---|---|
| Gender | 21.90 | 5 | ˂0.001 |
| Age | 84.28 | 30 | ˂0.001 |
| Marital status | 75.02 | 20 | ˂0.001 |
| Education | 41.42 | 15 | ˂0.001 |
| Size of place of residence | 46.20 | 25 | ˂0.01 |
| Monthly household income | 33.14 | 10 | ˂0.001 |
| Occupation | 80.65 | 15 | ˂0.001 |
| Value X2 | df | p Value | |
|---|---|---|---|
| Gender | 20.28 | 8 | ˂0.01 |
| Age | 35.48 | 48 | 0.91 n.s. |
| Marital status | 44.01 | 32 | 0.08 n.s. |
| Education | 18.42 | 24 | 0.78 n.s. |
| Size of place of residence | 64.26 | 40 | ˂0.01 |
| Monthly household income | 19.76 | 16 | 0.23 n.s. |
| Occupation | 26.70 | 24 | 0.32 n.s. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holmannova, D.; Hodac, J.; Borska, L.; Cermakova, E.; Hodacova, L. Vitamin D Supplementation in the Czech Republic: Socioeconomic Determinants and Public Awareness Gaps. Nutrients 2025, 17, 2623. https://doi.org/10.3390/nu17162623
Holmannova D, Hodac J, Borska L, Cermakova E, Hodacova L. Vitamin D Supplementation in the Czech Republic: Socioeconomic Determinants and Public Awareness Gaps. Nutrients. 2025; 17(16):2623. https://doi.org/10.3390/nu17162623
Chicago/Turabian StyleHolmannova, Drahomira, Jan Hodac, Lenka Borska, Eva Cermakova, and Lenka Hodacova. 2025. "Vitamin D Supplementation in the Czech Republic: Socioeconomic Determinants and Public Awareness Gaps" Nutrients 17, no. 16: 2623. https://doi.org/10.3390/nu17162623
APA StyleHolmannova, D., Hodac, J., Borska, L., Cermakova, E., & Hodacova, L. (2025). Vitamin D Supplementation in the Czech Republic: Socioeconomic Determinants and Public Awareness Gaps. Nutrients, 17(16), 2623. https://doi.org/10.3390/nu17162623






