Dietary Habits and Obesity in Middle-Aged and Elderly Europeans—The Survey of Health, Ageing, and Retirement in Europe (SHARE)
Abstract
1. Introduction
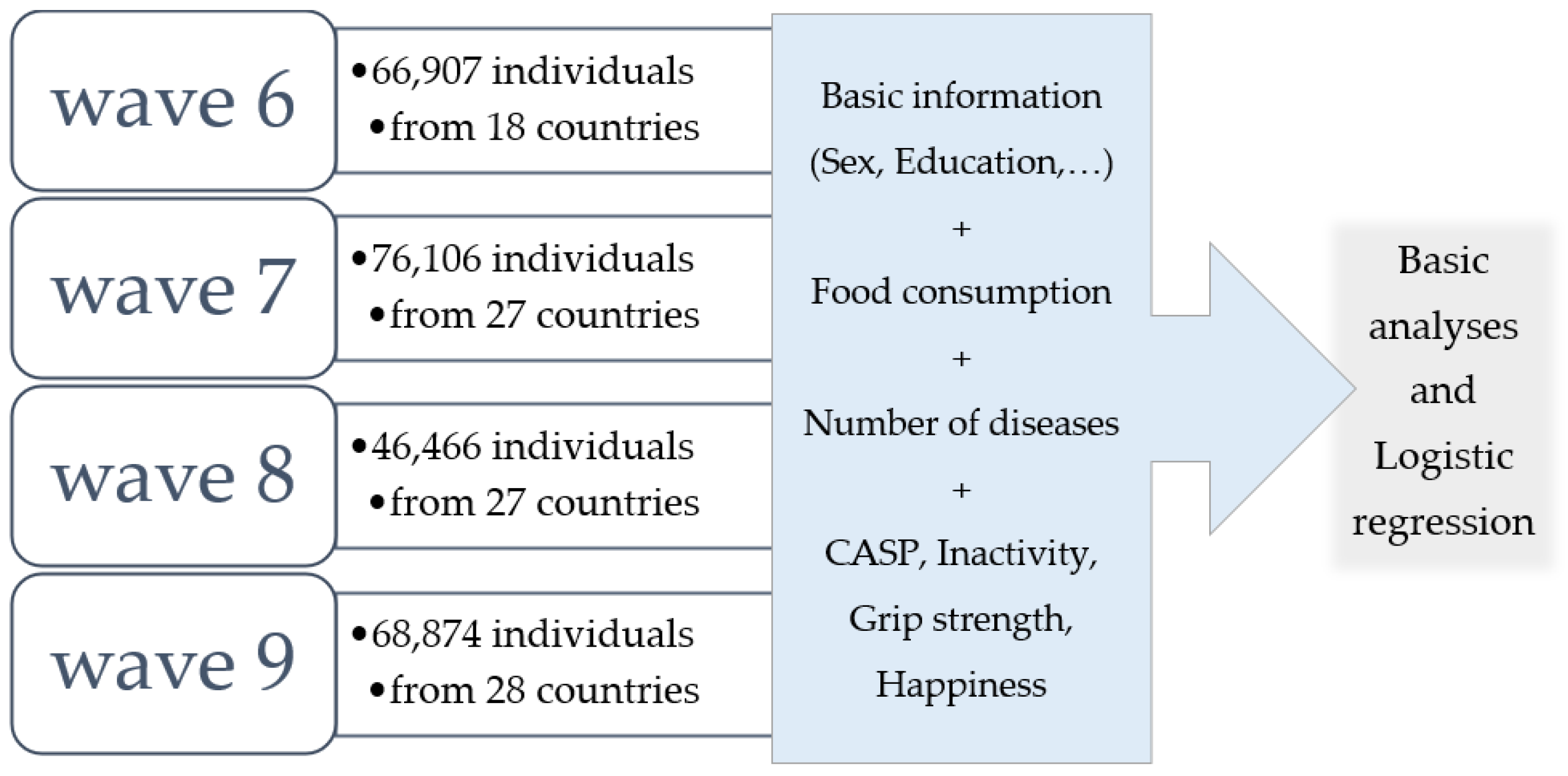
2. Materials and Methods
2.1. Study Population
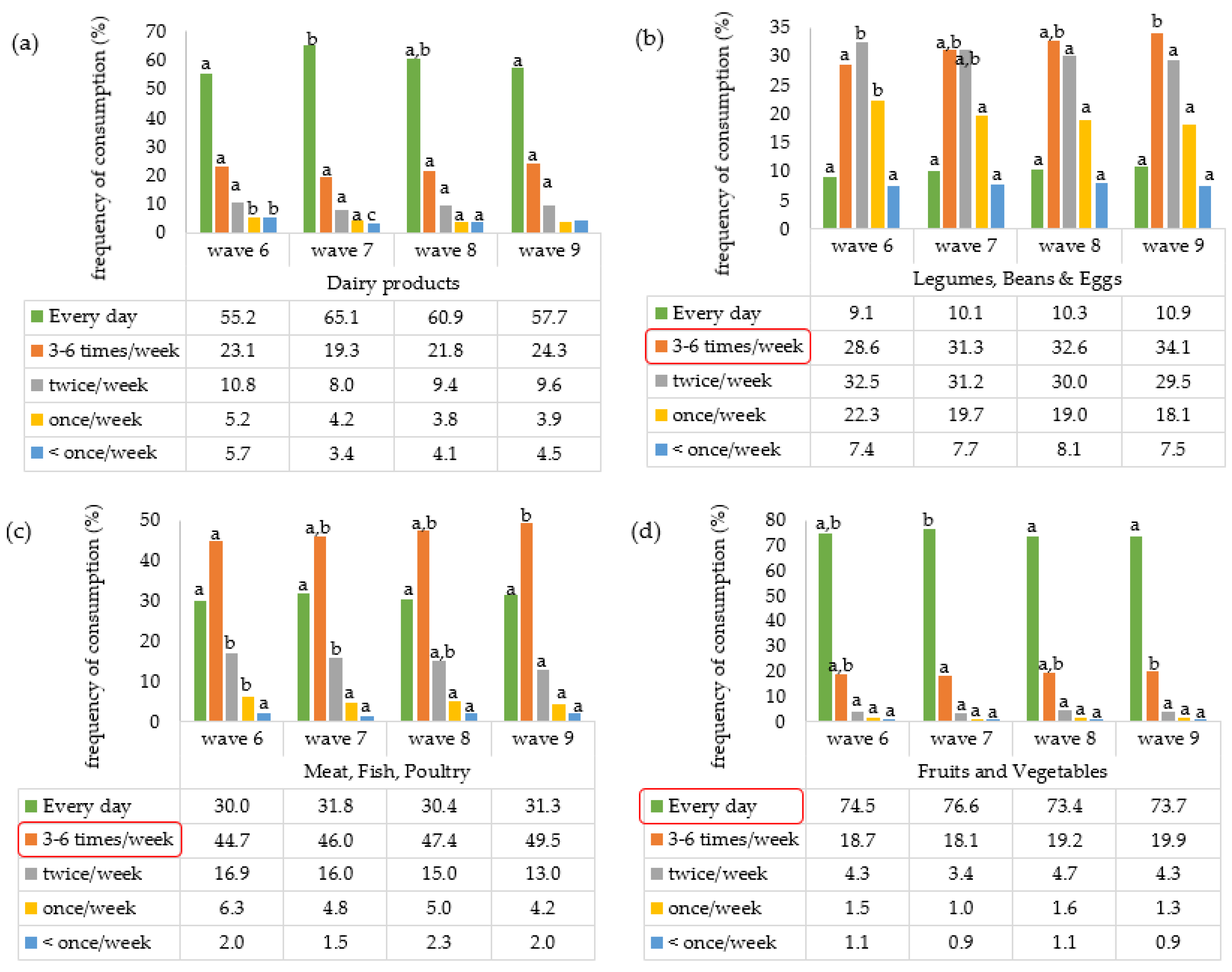
2.2. Mediterranean Diet Patterns (Note: Unvalidated Definition of MD Pattern)
- How frequently do you consume a serving of dairy products (e.g., a cup of yoghurt, cheese, a glass of milk, or a can of high-protein supplements) each week?
- How often do you eat a serving of eggs, beans, or legumes per week?
- How frequently do you consume a serving of poultry, meat, or fish on a weekly basis?
- How often do you eat a serving of fruits and vegetables each week?
2.3. Biomarker–Grip Strength
2.4. General Health Indicators
2.5. CASP-12 Index
2.6. Covariate Variables
2.7. Statistical Analysis
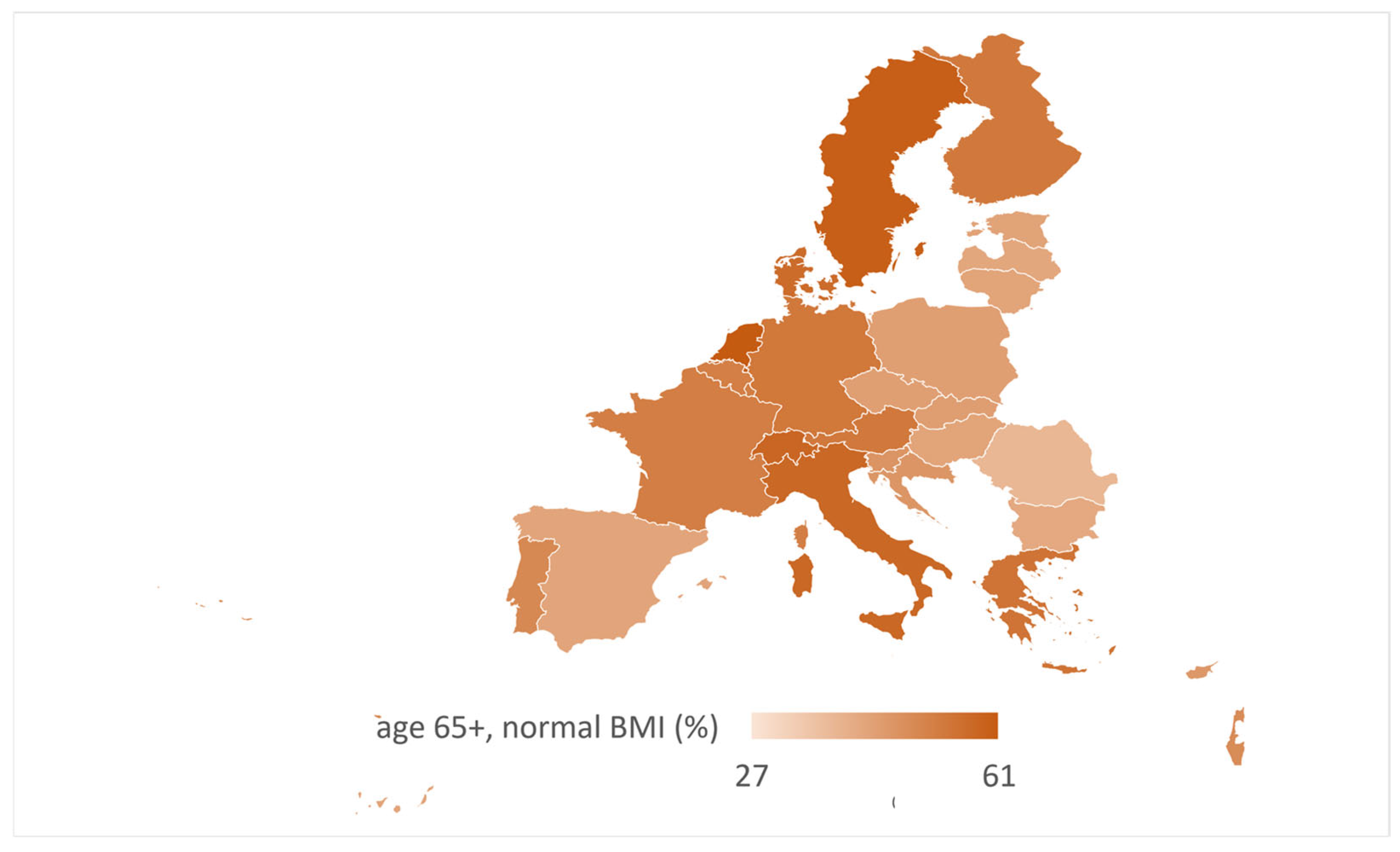
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CASP | Control, autonomy, self-realization, and pleasure scale |
| CVD | Cardiovascular diseases |
| CRM | Crude regression model |
| LDL/HDL | Low high-density lipoprotein cholesterol |
| MD | Mediterranean dietary pattern |
| OR | Odds ratios |
| SHARE | Survey of Health, Ageing and Retirement in Europe |
| SPHUS | Self-perceived health |
Appendix A
| Country | Mediterranean Diet Pattern (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| w6 | w7 | w8 | w9 | |||||
| No | Yes | No | Yes | No | Yes | No | Yes | |
| Austria | 82.5 | 17.5 | 78.3 | 21.7 | 78.1 | 21.9 | 75.5 | 24.5 |
| Germany | 72.1 | 27.9 | 81.8 | 18.2 | 77.6 | 22.4 | 78.1 | 21.9 |
| Sweden | 75.8 | 24.2 | 78.3 | 21.7 | 77.4 | 22.6 | 81.0 | 19.0 |
| Netherlands | n.a. | n.a. | 0.0 | 0.0 | 75.9 | 24.1 | 77.0 | 23.0 |
| Spain | 63.3 | 36.7 | 62.2 | 37.8 | 60.9 | 39.1 | 56.4 | 43.6 |
| Italy | 77.2 | 22.8 | 74.9 | 25.1 | 73.5 | 26.5 | 73.8 | 26.2 |
| France | 84.5 | 15.5 | 86.8 | 13.2 | 85.5 | 14.5 | 84.9 | 15.1 |
| Denmark | 80.4 | 19.6 | 88.3 | 11.7 | 85.7 | 14.3 | 83.4 | 16.6 |
| Greece | 81.2 | 18.8 | 75.6 | 24.4 | 81.5 | 18.5 | 79.5 | 20.5 |
| Switzerland | 73.6 | 26.4 | 75.2 | 24.8 | 75.5 | 24.5 | 75.2 | 24.8 |
| Belgium | 84.5 | 15.5 | 91.6 | 8.4 | 91.2 | 8.8 | 89.2 | 10.8 |
| Israel | 73.5 | 26.5 | 0.0 | 0.0 | 71.6 | 28.4 | 70.4 | 29.6 |
| Czech Republic | 88.1 | 11.9 | 77.5 | 22.5 | 86.6 | 13.4 | 83.7 | 16.3 |
| Poland | 74.6 | 25.4 | 78.0 | 22.0 | 79.7 | 20.3 | 67.3 | 32.7 |
| Luxembourg | 67.2 | 32.8 | 0.0 | 0.0 | 82.1 | 17.9 | 84.2 | 15.8 |
| Hungary | n.a. | n.a. | 0.0 | 0.0 | 65.8 | 34.2 | 64.7 | 35.3 |
| Portugal | 74.4 | 25.6 | 0.0 | 0.0 | 0.0 | 0.0 | 87.9 | 12.1 |
| Slovenia | 70.9 | 29.1 | 0.0 | 0.0 | 71.2 | 28.8 | 71.1 | 28.9 |
| Estonia | 87.6 | 12.4 | 0.0 | 0.0 | 85.7 | 14.3 | 86.1 | 13.9 |
| Croatia | 70.2 | 29.8 | 0.0 | 0.0 | 82.4 | 17.6 | 85.6 | 14.4 |
| Lithuania | n.a. | n.a. | 0.0 | 0.0 | 75.3 | 24.7 | 82.8 | 17.2 |
| Bulgaria | n.a. | n.a. | 0.0 | 0.0 | 79.7 | 20.3 | 75.7 | 24.3 |
| Cyprus | n.a. | n.a. | 0.0 | 0.0 | 55.8 | 44.2 | 59.8 | 40.2 |
| Finland | n.a. | n.a. | 0.0 | 0.0 | 85.5 | 14.5 | 86.3 | 13.7 |
| Latvia | n.a. | n.a. | 0.0 | 0.0 | 74.7 | 25.3 | 79.3 | 20.7 |
| Malta | n.a. | n.a. | 0.0 | 0.0 | 54.5 | 45.5 | 57.1 | 42.9 |
| Romania | n.a. | n.a. | 0.0 | 0.0 | 65.1 | 34.9 | 50.8 | 49.2 |
| Slovakia | n.a. | n.a. | 0.0 | 0.0 | 84.1 | 15.9 | 81.7 | 18.3 |
| Total | 77.9 | 22.1 | 79.1 | 20.9 | 78.1 | 21.9 | 77.6 | 22.4 |
| Country | Max Grip in Three Categories (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| w6 | w7 | w8 | w9 | |||||||||
| L | M | H | L | M | H | L | M | H | L | M | H | |
| Austria | 28.4 | 63.0 | 8.6 | 29.5 | 63.6 | 6.9 | 37.2 | 56.8 | 5.8 | 26.3 | 66.5 | 7.2 |
| Germany | 19.8 | 68.1 | 12.1 | 21.4 | 67.8 | 10.8 | 24.9 | 67.3 | 7.6 | 18.9 | 72.4 | 8.6 |
| Sweden | 25.0 | 64.1 | 10.9 | 27.3 | 63.5 | 9.3 | 30.2 | 62.5 | 7.3 | 23.6 | 68.7 | 7.7 |
| Netherlands | n.a. | n.a. | n.a. | 0.0 | 0.0 | 0.0 | 22.9 | 68.1 | 8.9 | 20.7 | 72.0 | 7.2 |
| Spain | 42.8 | 54.3 | 2.9 | 45.2 | 52.1 | 2.7 | 49.1 | 48.3 | 2.6 | 39.6 | 58.1 | 2.2 |
| Italy | 29.9 | 63.3 | 6.8 | 31.6 | 63.7 | 4.6 | 38.2 | 58.2 | 3.4 | 31.4 | 65.8 | 2.6 |
| France | 30.6 | 62.3 | 7.1 | 31.0 | 61.8 | 7.3 | 33.2 | 60.1 | 6.7 | 26.9 | 64.9 | 8.2 |
| Denmark | 18.4 | 64.3 | 17.3 | 18.9 | 65.4 | 15.6 | 21.2 | 65.8 | 13.0 | 19.0 | 68.7 | 12.3 |
| Greece | 33.9 | 59.1 | 6.9 | 35.1 | 60.2 | 4.8 | 35.8 | 60.7 | 3.5 | 29.2 | 67.3 | 3.4 |
| Switzerland | 24.0 | 67.0 | 8.9 | 26.2 | 65.4 | 8.3 | 29.5 | 62.9 | 7.6 | 25.0 | 68.0 | 6.9 |
| Belgium | 25.4 | 63.7 | 10.9 | 26.1 | 64.3 | 9.6 | 29.5 | 61.0 | 9.5 | 24.2 | 66.3 | 9.4 |
| Israel | 49.8 | 47.9 | 2.1 | 45.8 | 52.0 | 1.9 | 46.3 | 52.1 | 1.3 | 36.4 | 61.9 | 1.5 |
| Czech Republic | 24.9 | 67.2 | 7.9 | 28.1 | 65.2 | 6.6 | 28.2 | 64.8 | 6.9 | 26.7 | 67.9 | 5.3 |
| Poland | 28.3 | 63.1 | 8.6 | 28.3 | 63.1 | 8.6 | 28.3 | 65.3 | 6.3 | 24.0 | 71.0 | 4.9 |
| Luxembourg | 23.9 | 65.9 | 10.3 | 25.5 | 64.8 | 9.7 | 25.3 | 67.1 | 7.5 | 19.7 | 73.3 | 6.7 |
| Hungary | n.a. | n.a. | n.a. | 38.1 | 56.6 | 5.3 | 39.0 | 55.2 | 5.4 | 33.7 | 61.4 | 5.0 |
| Portugal | 43.8 | 53.9 | 2.3 | 42.1 | 56.4 | 1.5 | 0.0 | 0.0 | 0.0 | 33.5 | 63.0 | 2.9 |
| Slovenia | 26.6 | 62.2 | 11.2 | 27.3 | 63.3 | 9.4 | 28.9 | 62.6 | 8.4 | 20.8 | 68.6 | 10.4 |
| Estonia | 30.1 | 60.2 | 9.6 | 30.5 | 61.0 | 8.4 | 32.1 | 59.9 | 7.9 | 24.9 | 65.6 | 9.4 |
| Croatia | 26.6 | 62.1 | 11.2 | 24.9 | 62.6 | 12.5 | 27.5 | 62.2 | 10.1 | 22.5 | 67.8 | 9.6 |
| Lithuania | n.a. | n.a. | n.a. | 26.6 | 65.0 | 8.4 | 28.3 | 63.4 | 8.3 | 28.3 | 66.5 | 5.1 |
| Bulgaria | n.a. | n.a. | n.a. | 41.7 | 55.2 | 3.1 | 44.7 | 54.7 | 0.6 | 35.3 | 60.4 | 4.2 |
| Cyprus | n.a. | n.a. | n.a. | 50.2 | 46.7 | 3.1 | 58.6 | 40.3 | 0.6 | 40.8 | 58.2 | 0.9 |
| Finland | n.a. | n.a. | n.a. | 20.5 | 66.6 | 12.9 | 23.6 | 67.6 | 8.9 | 20.4 | 70.6 | 9.0 |
| Latvia | n.a. | n.a. | n.a. | 26.1 | 61.6 | 12.4 | 25.0 | 65.9 | 9.2 | 21.5 | 70.8 | 7.7 |
| Malta | n.a. | n.a. | n.a. | 42.8 | 55.1 | 2.0 | 43.5 | 54.3 | 2.1 | 34.4 | 63.7 | 1.8 |
| Romania | n.a. | n.a. | n.a. | 33.7 | 61.5 | 4.7 | 34.3 | 62.0 | 3.8 | 26.6 | 70.6 | 2.8 |
| Slovakia | n.a. | n.a. | n.a. | 25.4 | 62.7 | 11.9 | 44.4 | 47.9 | 7.6 | 32.5 | 64.8 | 2.6 |
| Total | 28.8 | 62.2 | 8.9 | 30.4 | 61.8 | 7.8 | 32.0 | 61.2 | 6.8 | 25.6 | 67.4 | 6.9 |
| Score (Abbreviation) | Components that Are Scored | Score Range | Cut-Offs * | Source (Reference) |
|---|---|---|---|---|
| Mediterranean Diet Score (MDS) | Vegetables, legumes, fruits/nuts, cereals, fish, meat, dairy, alcohol, MUFA/SFA ratio | 0–9 | Low: 0–3 Moderate: 4–5 High: 6–9 | Trichopoulou, et al. [51] |
| Alternate Mediterranean Diet Score (aMED) | Vegetables, legumes, fruits, nuts, whole grains, fish, red/processed meats, alcohol, fats | 0–9 | Low: 0–3 Moderate: 4–5 High: 6–9 | Fung, et al. [52] |
| Mediterranean Diet Adherence Screener (MEDAS) | Olive oil, vegetables, fruits, red meats, butter/cream, sugary drinks, legumes, wine, etc. | 0–14 | Low: 0–5 Moderate: 6–9 High: ≥10 | Martínez-González, et al. [50] |
| Mediterranean-Style Dietary Pattern Score (MSDPS) | 13 food groups: whole grains, fruits, vegetables, dairy, olive oil, fish, legumes, alcohol | 0–100 | Low: <50 Moderate: 50–75 High: >75 | Rumawas, et al. [53] |
| Mediterranean Diet Quality Index for Children and Adolescents (KIDMED) | Fruits, vegetables, fast food, sweets, breakfast habits, dairy, cereals, nuts | −4 to +12 | Low: ≤3 Moderate: 4–7 High: ≥8 | Serra-Majem, et al. [54] |
References
- Eurostat. Ageing Europe-Statistics on Population Developments. 2025. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments (accessed on 3 March 2025).
- Arvanitis, M.; Lowenstein, C.J. Dyslipidemia. Ann. Intern. Med. 2023, 176, ITC81–ITC96. [Google Scholar] [CrossRef]
- OECD. Health at A Glance 2023: OECD Indicators; OECD Publishing: Paris, France, 2023. [Google Scholar] [CrossRef]
- Yan, Y.; Wu, T.; Zhang, M.; Li, C.; Liu, Q.; Li, F. Prevalence, Awareness and Control of Type 2 Diabetes Mellitus and Risk Factors in Chinese Elderly Population. BMC Public Health 2022, 22, 1382. [Google Scholar] [CrossRef]
- Bilal, A.; Pratley, R. Diabetes and cardiovascular disease in older adults. Ann. N. Y. Acad. Sci. 2025, 1543, 42–67. [Google Scholar] [CrossRef] [PubMed]
- Mensah, G.; Fuster, V.; Roth, G. A Heart-Healthy and Stroke-Free World: Using Data to Inform Global Action. JACC 2023, 82, 2343–2349. [Google Scholar] [CrossRef] [PubMed]
- Jebari-Benslaiman, S.; Galicia-García, U.; Larrea-Sebal, A.; Olaetxea, J.R.; Alloza, I.; Vandenbroeck, K.; Benito-Vicente, A.; Martín, C. Pathophysiology of Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 3346. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, G.; Giosuè, A.; Calabrese, I.; Vaccaro, O. Dietary recommendations for prevention of atherosclerosis. Cardiovasc. Res. 2022, 118, 1188–1204. [Google Scholar] [CrossRef]
- Lusis, A.J.; Björkegren, J.L.M. Atherosclerosis: Recent Developments. Cell 2022, 185, 1630–1645. [Google Scholar] [CrossRef]
- Ajoolabady, A.; Pratico, D.; Lin, L.; Mantzoros, C.S.; Bahijri, S.; Tuomilehto, J.; Ren, J. Inflammation in atherosclerosis: Pathophysiology and mechanisms. Cell Death Dis. 2024, 15, 817. [Google Scholar] [CrossRef]
- Gaur, A.; Carr, F.; Warriner, D. Cardiogeriatrics: The current state of the art. Heart 2024, 110, 933–939. [Google Scholar] [CrossRef]
- Sciacqua, A.; Succurro, E.; Armentaro, G.; Miceli, S.; Pastori, D.; Rengo, G.; Sesti, G. Pharmacological treatment of type 2 diabetes in elderly patients with heart failure: Randomized trials and beyond. Heart Fail. Rev. 2023, 28, 667–681. [Google Scholar] [CrossRef]
- Grajower, M.M.; LeRoith, D. Management of Type 2 Diabetes Mellitus in the Very Elderly: One Practice’s Experience. Endocr. Pract. 2023, 29, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Gadó, K.; Tabák, G.Á.; Vingender, I.; Domján, G.; Dörnyei, G. Treatment of type 2 diabetes mellitus in the elderly-Special considerations. Physiol. Int. 2024, 111, 143–164. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 13. Older Adults: Standards of Care in Diabetes—2025. Diabetes Care 2025, 48 (Suppl. 1), S266–S282. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Hu, M.; Qin, X.; Qiu, L.; Wang, P.; Zhang, X.; Liu, R.; Wang, X. The Roles of Lipid Metabolism in the Pathogenesis of Chronic Diseases in the Elderly. Nutrients 2023, 15, 3433. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Katsiki, N.; Kolovou, G.; Perez-Martinez, P.; Mikhailidis, D.P. Dyslipidaemia in the Elderly: To Treat or Not to Treat? Expert Rev. Clin. Pharmacol. 2018, 11, 259–278. [Google Scholar] [CrossRef]
- Gielen, E.; Dupont, J.; Dejaeger, M.; Laurent, M.R. Sarcopenia, osteoporosis and frailty. Metab. Clin. Exp. 2023, 145, 155638. [Google Scholar] [CrossRef]
- Xu, J.; Wan, C.S.; Ktoris, K.; Reijnierse, E.M.; Maier, A.B. Sarcopenia is Associated with Mortality in Adults: A Systematic Review and Meta-Analysis. Gerontology 2022, 68, 361–376. [Google Scholar] [CrossRef]
- Shu, X.; Lin, T.; Wang, H.; Zhao, Y.; Jiang, T.; Peng, X.; Yue, J. Diagnosis, prevalence, and mortality of sarcopenia in dialysis patients: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2022, 13, 145–158. [Google Scholar] [CrossRef]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker for Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef]
- Zhao, X.; An, X.; Yang, C.; Sun, W.; Ji, H.; Lian, F. The crucial role and mechanism of insulin resistance in metabolic disease. Front. Endocrinol. 2023, 14, 1149239. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension. J. Hypertens. 2023, 41, 1874–1921. [Google Scholar] [CrossRef]
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Obeidat, A.A.; Ahmad, M.N.; Ghabashi, M.A.; Alazzeh, A.Y.; Habib, S.M.; Abu Al-Haijaa, D.; Azzeh, F.S. Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review. J. Clin. Med. 2025, 14, 2402. [Google Scholar] [CrossRef]
- Santos, C.A.; Maia, H.F.; Pitanga, F.J.G.; de Almeida, M.D.C.C.; da Fonseca, M.J.M.; de Aquino, E.M.L.; Cardoso, L.O.; Griep, R.H.; Barreto, S.M.; Suemoto, C.K.; et al. Hand Grip Strength Cut-Off Points as a Discriminator of Sarcopenia and Sarcopenic Obesity: Results from the ELSA-Brasil Cohort. J. Cachexia Sarcopenia Muscle 2025, 16, e13723. [Google Scholar] [CrossRef] [PubMed]
- Furbatto, M.; Lelli, D.; Antonelli Incalzi, R.; Pedone, C. Mediterranean Diet in Older Adults: Cardiovascular Outcomes and Mortality from Observational and Interventional Studies—A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 3947. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, S.; Di Chiara, T.; Daidone, M.; Tuttolomondo, A. Effects of the Mediterranean Diet on the Components of Metabolic Syndrome Concerning the Cardiometabolic Risk. Nutrients 2025, 17, 358. [Google Scholar] [CrossRef] [PubMed]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S.; SHARE Central Coordination Team. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef]
- Bergmann, M.; Scherpenzeel, A.; Börsch-Supan, A. SHARE Wave 7 Methodology: Panel Innovations and Life Histories; Max Planck Institute for Social Law and Social Policy: Munich, Germany, 2019; Available online: https://share-eric.eu/fileadmin/user_upload/SHARE_Working_Paper/SHARE_WP_69-2021.pdf (accessed on 15 November 2024).
- Börsch-Supan, A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8; Release Version: 8.0.0; Data Set; SHARE-ERIC: Berlin, Germany, 2022. [Google Scholar] [CrossRef]
- Maltarić, M.; Ruščić, P.; Kolak, M.; Bender, D.V.; Kolarić, B.; Ćorić, T.; Hoejskov, P.S.; Bošnir, J.; Kljusurić, J.G. Adherence to the Mediterranean Diet Related to the Health Related and Well-Being Outcomes of European Mature Adults and Elderly, with an Additional Reference to Croatia. Int. J. Environ. Res. Public Health 2023, 20, 4893. [Google Scholar] [CrossRef]
- Alves, R.; Perelman, J. European mature adults and elderly are moving closer to the Mediterranean diet—A longitudinal study, 2013–2019. Eur. J. Public Health 2022, 32, 600–605. [Google Scholar] [CrossRef]
- Alves, R. Mediterranean Diet in Europe: How are mature adults and elderly moving closer to this diet pattern? Eur. J. Public Health 2021, 31, ckab164.447. [Google Scholar] [CrossRef]
- Lee, M.T.; Howe, T.H.; Chen, C.C.; Wu, C.Y.; Hsieh, Y.W. Grip strength differences in middle-aged and older adults and individuals with stroke. Eur. J. Phys. Rehabil. Med. 2023, 59, 294–302. [Google Scholar] [CrossRef] [PubMed]
- CDC. Adult BMI Categories. 2024. Available online: https://www.cdc.gov/bmi/adult-calculator/bmi-categories.html (accessed on 14 April 2025).
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.; Sobotka, L.; et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin. Nutr. 2022, 41, 958–989. [Google Scholar] [CrossRef] [PubMed]
- SHARE. Release Guide 9.0.0. 2024. Available online: https://share-eric.eu/fileadmin/user_upload/Release_Guides/SHARE_release_guide_9-0-0.pdf (accessed on 5 December 2024).
- Heymans, M.W.; Twisk, J.W.R. Handling missing data in clinical research. J. Clin. Epidemiol. 2022, 151, 185–188. [Google Scholar] [CrossRef] [PubMed]
- IEssien, U.A.; Amechi, K.U.; Madu, K.A.; Ede, O.; Iyidobi, E.C.; Anyaehie, U.E.; Obadaseraye, O.R.; Ogbonnaya, I.S.; Ogbu, D.C.; Ngwangwa, C.L. Assessment of handgrip strength in healthy african subjects: Establishing age and gender stratified reference values. Niger. J. Clin. Pract. 2023, 26, 1029–1035. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Andersen, L.L.; Casaña, J.; Koyanagi, A.; Cruz, B.d.P.; Smith, L. Dose–response association of handgrip strength and risk of depression: A longitudinal study of 115 601 older adults from 24 countries. Br. J. Psychiatry 2023, 222, 135–142. [Google Scholar] [CrossRef]
- Lin, H.; Ren, H. The Influence of Interpersonal Behaviors and Population Density on Grip Strength of Elderly People: An Analysis of the Direct vs. Indirect Effects via Social Participation. Front. Public Health 2021, 9, 755695. [Google Scholar] [CrossRef]
- Ghosh, T.S.; Rampelli, S.; Jeffery, I.B.; Santoro, A.; Neto, M.; Capri, M.; Giampieri, E.; Jennings, A.; Candela, M.; Turroni, S.; et al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: The NU-AGE 1-year dietary intervention across five European countries. Gut 2020, 69, 1218–1228. [Google Scholar] [CrossRef]
- Chaaya, C.; Raad, E.; Kahale, F.; Chelala, E.; Ziade, N.; Maalouly, G. Adherence to Mediterranean Diet and Ocular Dryness Severity in Sjögren’s Syndrome: A Cross-Sectional Study. Med. Sci. 2025, 13, 64. [Google Scholar] [CrossRef]
- Castelló, J.V.; Tubianosa, C. Linking Mediterranean Diet and Lifestyle with Cardio Metabolic Disease and Depressive Symptoms: A Study on the Elderly in Europe. Int. J. Environ. Res. Public Health 2020, 17, 7053. [Google Scholar] [CrossRef]
- Mazza, E.; Ferro, Y.; Maurotti, S.; Micale, F.; Boragina, G.; Russo, R.; Lascala, L.; Sciacqua, A.; Gazzaruso, C.; Montalcini, T.; et al. Association of dietary patterns with sarcopenia in adults aged 50 years and older. Eur. J. Nutr. 2024, 63, 1651–1662. [Google Scholar] [CrossRef]
- Cacciatore, S.; Gava, G.; Calvani, R.; Marzetti, E.; Coelho-Junior, H.J.; Picca, A.; Esposito, I.; Ciciarello, F.; Salini, S.; Russo, A.; et al. Lower Adherence to A Mediterranean Diet is Associated with High Adiposity in Community-Dwelling Older Adults: Results from the Longevity Check-Up (Lookup) 7+ Project. Nutrients 2023, 15, 4892. [Google Scholar] [CrossRef]
- Marcos-Pardo, P.J.; González-Gálvez, N.; López-Vivancos, A.; Espeso-García, A.; Martínez-Aranda, L.M.; Gea-García, G.M.; Orquín-Castrillón, F.J.; Carbonell-Baeza, A.; Jiménez-García, J.D.; Velázquez-Díaz, D.; et al. Sarcopenia, Diet, Physical Activity and Obesity in European Middle-Aged and Older Adults: The LifeAge Study. Nutrients 2020, 13, 8. [Google Scholar] [CrossRef]
- Coelho-Júnior, H.J.; Trichopoulou, A.; Panza, F. Protein Intake and Physical Activity in Relation to Grip Strength Decline: A Pooled Analysis of Four Longitudinal Ageing Cohorts. Clin. Nutr. 2023, 42, 1234–1245. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-Item Mediterranean Diet Assessment Tool and Obesity Indexes among High-Risk Subjects: The PREDIMED Trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-Quality Scores and Plasma Concentrations of Markers of Inflammation and Endothelial Dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef][Green Version]
- Rumawas, M.E.; Dwyer, J.T.; McKeown, N.M.; Meigs, J.B.; Rogers, G.; Jacques, P.F. The Development of the Mediterranean-Style Dietary Pattern Score and Its Application to the American Diet in the Framingham Offspring Cohort. J. Nutr. 2009, 139, 1150–1156. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Zhang, S.; Gu, Y.; Rayamajhi, S.; Thapa, A.; Meng, G.; Zhang, Q.; Liu, L.; Wu, H.; Zhang, T.; Wang, X.; et al. Ultra-processed food intake is associated with grip strength decline in middle-aged and older adults: A prospective analysis of the TCLSIH study. Eur. J. Nutr. 2022, 61, 1331–1341. [Google Scholar] [CrossRef]
- Ma, Z.; Yang, H.; Meng, G.; Zhang, Q.; Liu, L.; Wu, H.; Gu, Y.; Zhang, S.; Wang, X.; Zhang, J.; et al. Anti-inflammatory dietary pattern is associated with handgrip strength decline: A prospective cohort study. Eur. J. Nutr. 2023, 62, 3207–3216. [Google Scholar] [CrossRef]
- Follis, S.; Cook, A.; Bea, J.W.; Going, S.B.; Laddu, D.; Cauley, J.A.; Shadyab, A.H.; Stefanick, M.L.; Chen, Z. Association Between Sarcopenic Obesity and Falls in a Multiethnic Cohort of Postmenopausal Women. J. Am. Geriatr. Soc. 2018, 66, 2314–2320. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, S.; Brau, F.; Galluzzo, V.; Santagada, D.A.; Loreti, C.; Biscotti, L.; Laudisio, A.; Zuccalà, G.; Bernabei, R. Falls among Older Adults: Screening, Identification, Rehabilitation and Management. Appl. Sci. 2022, 12, 7934. [Google Scholar] [CrossRef]
- Aballay, L.R.; Eynard, A.R.; del Pilar Díaz, M.; Navarro, A.; Muñoz, S.E. Overweight and obesity: A review of their relationship to metabolic syndrome, cardiovascular disease, and cancer in South America. Nutr. Rev. 2013, 71, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Huemer, M.-T.; Kluttig, A.; Fischer, B.; Ahrens, W.; Castell, S.; Ebert, N.; Gastell, S.; Jöckel, K.-H.; Kaaks, R.; Karch, A.; et al. Grip strength values and cut-off points based on over 200,000 adults of the German National Cohort-a comparison to the EWGSOP2 cut-off points. Age Ageing 2023, 52, afac324. [Google Scholar] [CrossRef]
- Huang, L.; Shen, X.; Zou, Y.; Wang, Y. Effects of BMI and grip strength on older adults’ falls-A longitudinal study based on CHARLS. Front. Public Health 2024, 12, 1415360. [Google Scholar] [CrossRef]
- Liu, S.; He, Y.; Yu, G.; Song, C.; Wang, D.; Liu, L.; Liang, H.; Wan, H.; Shen, J. Association of muscle mass, grip strength and fat-to-muscle ratio and metabolic dysfunction-associated steatotic liver disease in a middle-to-elderly aged population. Ann. Med. 2024, 56, 2390169. [Google Scholar] [CrossRef]
- Romagnolo, D.F.; Selmin, O.I. Mediterranean Diet and Prevention of Chronic Diseases. Nutr. Today 2017, 52, 208–222. [Google Scholar] [CrossRef]
- Sarpdaği, Y.; Yiğit, M.F.; Aydin, M.A.; Yildirim, M.S.; Çiftci, N.; Yildiz, M. Mediating role of psychological well-being in the effect of spirituality on attitudes toward death in the elderly. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2025, 25, e13236. [Google Scholar] [CrossRef]
- Pallazola, V.A.; Davis, D.M.; Whelton, S.P.; Cardoso, R.; Latina, J.M.; Michos, E.D.; Sarkar, S.; Blumenthal, R.S.; Arnett, D.K.; Stone, N.J.; et al. A Clinician’s Guide to Healthy Eating for Cardiovascular Disease Prevention. Mayo Clin. Proc. Innov. Qual. Outcomes 2019, 3, 251–267. [Google Scholar] [CrossRef]
- Rippe, J.M. Lifestyle Medicine: The Health Promoting Power of Daily Habits and Practices. Am. J. Lifestyle Med. 2018, 12, 499–512. [Google Scholar] [CrossRef]
- Jurek, J.M.; Zablocka-Sowinska, K.; Clavero Mestres, H.; Reyes Gutiérrez, L.; Camaron, J.; Auguet, T. The Impact of Dietary Interventions on Metabolic Outcomes in Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and Comorbid Conditions, Including Obesity and Type 2 Diabetes. Nutrients 2025, 17, 1257. [Google Scholar] [CrossRef]
| Variables | Mediterranean Dietary Pattern (MD) | Maximum Grip Strength Measure | |||||
|---|---|---|---|---|---|---|---|
| No (n = 201,967) | Yes (n = 56,386) | p-Value | Low (n = 75,439) | Medium (n = 163,149) | High (n = 19,635) | p-Value | |
| Sex (%) | 0.731 | <0.001 | |||||
| Male | 43.9 | 42.2 | 9.1 | 52.7 | 99.4 | ||
| Female | 56.1 | 57.8 | 90.9 | 47.3 | 0.6 | ||
| Age (%) | 0.997 | <0.001 | |||||
| 51–64 | 26.7 | 26.5 | 20.3 | 37.6 | 62.2 | ||
| 65–74 | 34.9 | 35.7 | 32.2 | 38.3 | 32.0 | ||
| 75–85 | 23.5 | 23.3 | 33.1 | 19.1 | 4.7 | ||
| >85 | 8.5 | 8.0 | 13.9 | 3.6 | 0.1 | ||
| BMI (%) | 0.900 | 0.006 | |||||
| Normal (under 65 years) | 33.1 | 33.7 | 36.1 | 32.9 | 20.9 | ||
| Normal (>65 years) | 50.5 | 51.0 | 48.6 | 52.2 | 46.2 | ||
| Marital status (%) | 0.636 | 0.128 | |||||
| Living with a partner | 59.5 | 61.8 | 51.0 | 68.8 | 75.2 | ||
| Not living with a partner | 40.4 | 38.1 | 48.9 | 31.2 | 24.6 | ||
| Education level (%) | 0.929 | 0.028 | |||||
| Primary | 32.4 | 33.7 | 41.7 | 25.0 | 15.4 | ||
| Secondary | 35.6 | 33.9 | 33.5 | 40.0 | 43.5 | ||
| Tertiary | 31.0 | 31.6 | 23.8 | 34.3 | 40.3 | ||
| 2+ chronic diseases (%) | 0.809 | 0.035 | |||||
| Less than 2 diseases | 46.1 | 47.3 | 37.2 | 53.4 | 63.5 | ||
| 2+ chronic diseases | 53.8 | 52.6 | 62.7 | 46.6 | 36.4 | ||
| Physical inactivity (%) | 0.901 | 0.003 | |||||
| Other | 86.4 | 86.1 | 80.9 | 93.1 | 97.6 | ||
| Never vigorous nor moderate physical activity | 13.4 | 13.8 | 19.1 | 6.9 | 2.4 | ||
| Self-perceived health (SPHUS-1) (%) | 0.999 | 0.200 | |||||
| Excellent | 5.8 | 5.7 | 3.5 | 7.2 | 9.8 | ||
| Very good | 16.5 | 17.4 | 11.6 | 19.3 | 24.5 | ||
| Good | 37.9 | 37.9 | 33.9 | 40.8 | 41.4 | ||
| Fair | 28.8 | 28.4 | 36.0 | 26.4 | 19.6 | ||
| Poor | 10.9 | 10.6 | 15.0 | 6.3 | 3.7 | ||
| SPHUS-2 (%) | 0.867 | 0.064 | |||||
| Very good/excellent | 22.3 | 23.0 | 15.0 | 26.4 | 35.3 | ||
| Less than very good | 77.6 | 76.9 | 85.0 | 73.5 | 64.7 | ||
| CASP categories (%) | 0.965 | 0.082 | |||||
| Low | 2.7 | 2.9 | 5.6 | 1.8 | 0.8 | ||
| Medium | 27.9 | 28.9 | 35.5 | 23.3 | 16.3 | ||
| High | 69.4 | 68.2 | 60.3 | 75.3 | 83.2 | ||
| Current job situation (%) | 0.737 | <0.001 | |||||
| Retired | 66.9 | 65.3 | 70.3 | 62.9 | 43.1 | ||
| Not retired | 33.0 | 34.6 | 29.7 | 37.1 | 56.9 | ||
| Sex | BMI Categories (kg/m2) | Age (Years) | BMI Categories * (kg/m2) | Age (Years) | ||
|---|---|---|---|---|---|---|
| 51–64.9 | 65–74.9 | 75–85 | >85 | |||
| Male | <18.5—underweight | 0.6 | <18.5—severe underweight | 2.6 | 3.2 | 7.4 |
| 18.5–20.9—underweight | 2.4 | 3.4 | 5.3 | |||
| 18.5–24.9—normal | 25.2 | 21–27.49—normal | 49.4 | 55.8 | 59.0 | |
| 25–29.9—overweight | 45.7 | 27.5–30.9—overweight | 27.0 | 23.4 | 19.6 | |
| >30—obese | 26.5 | 31–39.9—obese | 17.2 | 13.7 | 8.5 | |
| >40—morbid obesity | 1.4 | 0.6 | 0.1 | |||
| Female | <18.5—underweight | 1.2 | <18.5—severe underweight | 4.5 | 7.0 | 14.3 |
| 18.5–20.9—underweight | 6.4 | 6.4 | 9.4 | |||
| 18.5–24.9—normal | 37.0 | 21–27.49—normal | 46.8 | 47.9 | 46.5 | |
| 25–29.9—overweight | 34.8 | 27.5–30.9—overweight | 21.4 | 20.6 | 16.9 | |
| >30—obese | 24.4 | 31–39.9—obese | 19.0 | 16.8 | 12.5 | |
| >40—morbid obesity | 2.0 | 1.3 | 0.5 | |||
| Crude Model | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| No. of chronic diseases | ||||||
| Less than 2 diseases | Reference | Reference | Reference | |||
| 2+ chronic diseases | 1.08 (1.03–1.12) | 0.001 | 1.12 (1.09–1.30) | <0.001 | 1.21 (1.11–1.32) | <0.001 |
| BMI | ||||||
| Underweight | Reference | Reference | Reference | |||
| Normal | 1.16 (1.16–1.69) | 0.001 | 1.28 (0.95–1.95) | 0.090 | 1.39 (1.00–1.94) | 0.048 |
| Overweight | 1.17 (0.99–1.40) | 0.059 | 1.29 (0.65–1.77) | 0.097 | 1.40 (1.00–1.94) | 0.049 |
| Obesity | 1.07 (0.91–1.28) | 1.17 (0.86–1.02) | 0.317 | 1.33 (0.95–1.87) | 0.094 | |
| CASP | ||||||
| Low | Reference | Reference | Reference | |||
| Medium | 0.69 (0.89–0.81) | <0.001 | 0.75 (0.56–1.00) | 0.049 | 0.92 (0.68–1.26) | 0.616 |
| High | 0.93 (0.89–0.97) | 0.001 | 0.94 (0.86–1.02) | 0.131 | 0.95 (0.87–1.04) | 0.240 |
| Physical inactivity | ||||||
| Never, nor moderate physical activity | Reference | Reference | Reference | |||
| Other | 0.79 (0.74–0.84) | <0.001 | 0.70 (0.61–0.79) | <0.001 | 0.63 (0.55–0.723) | <0.001 |
| Self-perceived health (SPHUS-1) | ||||||
| Poor | Reference | Reference | Reference | |||
| Fair | 0.96 (0.79–5.70) | 0.133 | 0.79 (0.09–6.62) | 0.825 | 0.84 (0.10–7.08) | 0.872 |
| Good | 1.14 (1.00–1.26) | 0.058 | 1.17 (0.94–1.44) | 0.154 | 1.21 (0.96–1.52) | 0.110 |
| Very good | 1.28 (1.15–1.39) | <0.001 | 1.35 (1.13–1.61) | 0.001 | 1.44 (1.19–1.75) | <0.001 |
| Excellent | 1.24 (1.13–1.34) | <0.001 | 1.26 (1.08–1.48) | 0.004 | 1.36 (1.14–1.62) | 0.001 |
| SPHUS-2 | ||||||
| Less than very good | Reference | Reference | Reference | |||
| Very good/excellent | 1.15 (1.08–1.26) | <0.001 | 1.29 (1.11–1.51) | 0.001 | 1.42 (1.20–1.69) | <0.001 |
| Maximal grip strength | ||||||
| Low | Reference | Reference | Reference | |||
| Medium | 1.33 (1.22–1.45) | <0.001 | 1.38 (1.15–1.65) | 0.001 | 1.36 (1.18–1.74) | <0.001 |
| High | 1.24 (1.14–1.34) | <0.001 | 1.23 (1.06–1.42) | 0.005 | 1.27 (1.10–1.48) | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maltarić, M.; Gajdoš Kljusurić, J.; Kolak, M.; Smolić, Š.; Kolarić, B.; Vranešić Bender, D. Dietary Habits and Obesity in Middle-Aged and Elderly Europeans—The Survey of Health, Ageing, and Retirement in Europe (SHARE). Nutrients 2025, 17, 2525. https://doi.org/10.3390/nu17152525
Maltarić M, Gajdoš Kljusurić J, Kolak M, Smolić Š, Kolarić B, Vranešić Bender D. Dietary Habits and Obesity in Middle-Aged and Elderly Europeans—The Survey of Health, Ageing, and Retirement in Europe (SHARE). Nutrients. 2025; 17(15):2525. https://doi.org/10.3390/nu17152525
Chicago/Turabian StyleMaltarić, Manuela, Jasenka Gajdoš Kljusurić, Mirela Kolak, Šime Smolić, Branko Kolarić, and Darija Vranešić Bender. 2025. "Dietary Habits and Obesity in Middle-Aged and Elderly Europeans—The Survey of Health, Ageing, and Retirement in Europe (SHARE)" Nutrients 17, no. 15: 2525. https://doi.org/10.3390/nu17152525
APA StyleMaltarić, M., Gajdoš Kljusurić, J., Kolak, M., Smolić, Š., Kolarić, B., & Vranešić Bender, D. (2025). Dietary Habits and Obesity in Middle-Aged and Elderly Europeans—The Survey of Health, Ageing, and Retirement in Europe (SHARE). Nutrients, 17(15), 2525. https://doi.org/10.3390/nu17152525







